A Quality Improvement Tool to Assess Self
advertisement

The Joint Commission Journal on Quality and Patient Safety
Research Methods
A Quality Improvement
Tool to Assess SelfManagement Support
in Primary Care
Carol A. Brownson, M.S.P.H.
Doriane Miller, M.D.
Richard Crespo, Ph.D.
Sally Neuner, R.N.
Joan Thompson, Ph.D., M.P.H., R.D., C.D.E.
Joseph C. Wall, M.H.A., C.H.E.
Seth Emont, Ph.D., M.S.
Patricia Fazzone, D.N.Sc., M.P.H., R.N.
Edwin B. Fisher, Ph. D.
Russell E. Glasgow, Ph. D.
S
elf management is an essential, central component
of effective care for diabetes and other chronic illnesses.1–5 Unfortunately, self-management support,
patient follow-up, and linkage to community resources are
also among the illness management activities conducted
least often in most health care settings.6–8
Very few instruments exist to assess delivery or consistency of self-management support. Patient self-report surveys have been designed to assess patient perceptions of
receipt of care congruent with the Chronic Care Model,8
of the “5 A’s” (Assess, Advise, Agree, Assist, Arrange) of
behavioral counseling recommended by the U.S.
Preventive Services Task Force,9,10 and of their health care
providers’ ability to be “autonomy supportive.”11,12 Perhaps
the gold standard for assessing self-management support is
direct observation measures of patient-provider interactions.13 Although helpful in research settings, such measures are not practical for widespread use, nor do they
reflect the importance of a system of planned, proactive
care and its contribution to self-management support.
This article reports on the development and use of a
quality improvement (QI) instrument that is completed
by primary health care teams to (1) help them self-evaluate their current delivery of resources and supports for self
management and (2) identify areas and ways in which they
could enhance these services. This scale, the Assessment of
Primary Care Resources and Supports for Chronic Disease
Self-Management (PCRS), is designed to apply to a variety of primary care settings and across different chronic ill-
408
July 2007
Article-at-a-Glance
Background: Self management is an essential, central
component of effective care for diabetes and other chronic illnesses, yet very few instruments exist to assess delivery
or consistency of self-management support. The
Assessment of Primary Care Resources and Supports for
Chronic Disease Self-Management (PCRS) tool assesses
both organizational infrastructure and delivery of selfmanagement support services.
Methods: The PCRS was developed by the Robert
Wood Johnson Foundation® Diabetes Initiative and
underwent several stages of development, including three
pilot tests, review by experts, and implementation by a
national quality improvement (QI) program.
Results: The development and testing of the instrument resulted in the current 16-item measure. Use of the
PCRS in a QI collaborative with 20 diverse health care
teams across the United States demonstrated that the
instrument is helpful in assessing areas for improvement.
Discussion: Initial experience suggests that the
PCRS is a user-friendly self-assessment tool that primary
care teams can use to assess their current capacity to support and implement consistent patient-centered self management. The initial evaluation indicates that the PCRS
has acceptable psychometric properties and is applicable
across different types of primary care teams and chronic
illness conditions.
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
The Joint Commission Journal on Quality and Patient Safety
nesses. It is modeled after an instrument based on the
Chronic Care Model—Assessment of Chronic Illness Care
(ACIC).6
Although the PCRS is consistent with and complementary to the ACIC, it differs from it in the following ways:
■ It focuses exclusively and more comprehensively on selfmanagement support.
■ It is based on a complementary, but different, conceptual model known as Resources and Support for Self
Management.5
■ The content is divided into two primary sections,
Patient Support and Organizational Support, rather than
the 6 areas of the Chronic Care Model.
■ The response options are different.
The PCRS was developed as a tool for teams participating in the Diabetes Initiative of the Robert Wood Johnson
Foundation (RWJF). This initiative funds self-management and community supports grants for diabetes care in
14 settings in the United States that serve diverse high-risk
audiences. On the basis of extensive research showing the
importance of self management both in diabetes care and
prevention,1–5 the Diabetes Initiative was developed in
2002 to demonstrate successful self-management program
models and stimulate their dissemination. Two programs
were launched:
1. Advancing Diabetes Self Management (ADSM) funded
projects to “demonstrate that comprehensive models for
diabetes self-management can be delivered in primary care
settings and can significantly improve patient outcomes.”14
2. Building Community Supports for Diabetes Care funded
projects to “extend support for diabetes management
beyond the clinical setting into the communities where
people with diabetes live.”15
In light of diabetes’ status as an ideal model for chronic disease care,14–16 the Diabetes Initiative’s projects also
were expected to serve as demonstrations of self-management support and community resources and policies, two
components of the Chronic Care Model17 that have
received somewhat less attention and proven more challenging to implement than the more ”structural” components of the model.
To guide development of demonstration projects in
these two areas, the Diabetes Initiative first needed to
define and develop a framework for addressing the broad
categories of self-management support and community
July 2007
resources. To do this, the initiative developed a model of
the needs of the individual with diabetes, known as
Resources and Supports for Self Management (RSSM).5
There are two important aspects of this model. First, it
views self-management support from the perspective of
the individual with diabetes. Second, and related to the
first, it takes an ecological perspective of self-management
support, recognizing the role of clinical care as well as family, community, and environmental supports for self-management. Thus, RSSM includes the needs of those with
diabetes for the following:
■ Individualized assessment
■ Collaborative goal setting
■ Instruction in key skills
■ Ongoing follow-up and support
■ Community resources
■ Continuity of quality clinical care
The PCRS tool is the work of the Organizational
Resources and Supports for Self Management (ORSSM)
work group of the Diabetes Initiative, originally composed
of representatives of the six ADSM sites. Work groups
consisted of grantees and experts whose focused collaboration led to a shared understanding of the issue, agreement
on approaches to QI, and, if applicable, the development
of tools or products to facilitate or improve practice.
Participating sites in the ORSSM work group represented
a variety of primary care settings (for example, a rural clinic, urban Federally Qualified Health Centers, a family
medicine residency training program) serving diverse populations. Their work focused on the organizational structures and processes needed to achieve high-quality
diabetes self management in primary care settings. The
resulting PCRS tool corresponds to the RSSM model in a
number of respects, specifically reflecting the role of primary care in providing or supporting the key resources
and supports needed by people with diabetes.
This article (1) describes the background for and development of the PCRS, (2) describes how the PCRS can be
used both for QI and research, and (3) presents preliminary data on and uses of the PCRS to date.
Methods
PCRS OVERVIEW
The intent of the PCRS is to promote self-assessment and
to stimulate discussion among primary care team mem-
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
409
The Joint Commission Journal on Quality and Patient Safety
bers about practice changes that can be made to more consistently deliver high-quality self-management resources
and supports to patients with one or more chronic illnesses. Its specific goals follow:
■ Function as a QI tool by helping to build consensus for
change
■ Identify strengths as well as gaps in resources, services,
and supports
■ Help teams integrate changes into their system by identifying standards for optimal performance, as well as suggestions and benchmarks for improvements
The PCRS, in the public domain and available on the
Web,18 is designed to help primary care teams assess the
level to which self management is integrated into their
practice. The survey is divided into two components—
Patient Support and Organizational Support. The Patient
Support section includes eight items, each corresponding
to a characteristic of service delivery found to enhance
patient self management in the areas of physical activity,
healthy eating, emotional health, medication management, and management of daily activities and roles.
The Organizational Support section includes eight
items corresponding to system design issues that primary
care organizations must address in their planning, resource
allocation, and evaluation to support the delivery of selfmanagement services. The two sections of the PCRS are
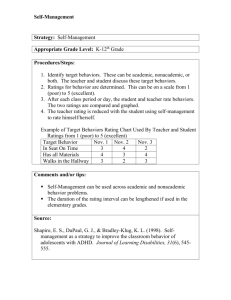
intended to complement each other. Figure 1 (below) lists
the characteristics of each section and reflects their interface, in particular the importance of organizational infrastructure in enabling patient support for self management.
The PCRS tool is to be used with multidisciplinary
teams representing frontline staff, clinicians, and administrative personnel. It is recommended that teams use it
periodically (for example, quarterly, semi-annually) as a
way to guide the integration of self management into their
system of health care over time.
Each member of the team is to fill out the assessment
independently taking into account an agreed-on period of
time (for example, previous quarter). When all members
have completed the tool, it is recommended that the team
meet to discuss their scores and any discrepancies among
scores. Discrepancies in scores offer an important opportunity for discussion that can lead to improved communication and team function. The tool’s value lies not so
much in the number each member assigns but in the
improvement process that is initiated by discovery of discrepancies or areas for improvement.
The PCRS defines four levels of performance for each
Characteristics of Resources and Supports for
Self Management in Primary Care and the Relationship Between
Organizational Support and Patient Support Categories
}
●
Continuity of care
●
Coordination of referrals
●
Ongoing quality improvement
●
System for documentation
●
Patient input
●
Integration of self management
into primary care
●
Team approach
●
Staff education and training
Organizational
Support
Patient
Support
{
●
Individualized assessment
●
Self-management education
●
Goal setting
●
Problem-solving skills
●
Emotional health
●
Patient involvement in
decision making
●
Social support
●
Links to community resources
Figure 1. The characteristics of the Organizational Support and Patient Support sections and their interface, in particular the
importance of organizational infrastructure in enabling patient support for self management, are shown.
410
July 2007
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
The Joint Commission Journal on Quality and Patient Safety
characteristic using “grades,” from a low level of development (D) to a level that reflects strong systems integration
(A). The levels are progressive. In general, the following
criteria were used to identify activities for each of the D–A
levels:
■ Level D: structure and/or process nonexistent or inadequate.
■ Level C: patient/provider level only. Implementation is
sporadic or inconsistent; patient-provider interaction is
passive.
■ Level B: microsystem level, that is, health care team or
coordination of services in a particular office are present.
At this level, implementation is done in an organized and
consistent manner, using a team approach; a system is in
place for coordinating services.
■ Level A: system level, that is, level B plus the health care
system, policies, and environmental or community supports. At this level, implementation is consistent, thorough, and part of a QI system that gives feedback to the
patient and the health care system.
With the exception of the D level, each level has a range
of 3 numbers from which to select. This allows users to
consider the degree to which their team is meeting the criteria described for that level and to score accordingly. For
example, if the criteria for Level B are being minimally
met, the score would be a 5, the lowest for that level. If, on
the other hand, the criteria were fully met then one might
score a 7, the highest rating for that level. Within each
level, scores can be adjusted up or down depending on
how much of the criteria are met and how consistently the
scorer perceives that their team meets it. Scoring sheets
and instructions are provided with the tool.
INSTRUMENT DEVELOPMENT
A number of factors contributed to the development of
the PCRS, as follows:
■ The aims of the ADSM Program—to advance diabetes
self management in primary care settings
■ The need for clarification and agreement on the role of
primary care in providing resources and supports for self
management
■ The desire for a means to assess organizational capacity
for providing self-management services and for articulating action steps that could serve as benchmarks for
improvement in the quality of self-management support
July 2007
in primary care
■ The desire to be congruent with and to further delineate
the self-management support component of the Chronic
Care Model
Table 1 (page 412) outlines the time frame and key
processes in the development of the PCRS. Initial discussion and formation of the ORSSM work group occurred
at the first Diabetes Initiative Collaborative Learning
Network meeting in April 2003. Expert consultation was
provided by a member of the Diabetes Initiative National
Advisory Committee [R.G.], who also serves as faculty to
the Quality Allies program, now known as “New Health
Partnerships: Improving Care by Engaging Patients,”* and
by the national director [D.M.]. The program follows
ambulatory care teams nationwide as they design, test,
refine and ultimately spread best practices in self-management support.19
Review and feedback were solicited throughout the
course of development from a number of experts, including staff of the Bureau of Primary Health Care Health
Disparities Collaboratives, Diabetes Initiative National
Advisory Committee members, other national RWJFfunded initiatives, and the Improving Chronic Illness Care
program. Key decisions included (1) using the ACIC format because of its familiarity and (2) increasing the tool’s
generalizability by not limiting it to diabetes but using language appropriate for a broad array of chronic conditions.
Testing and Improvement
The development process for the tool was iterative. A task
group of four primary care sites was heavily involved in
testing, retesting, and finally facilitating the piloting of a
final version. Testing was conducted in three pilots (Table
1, page 412).
Following the third pilot, the tool was shared with four
external potential users, whose feedback promoted specific changes. For example, language was broadened to be
more inclusive of cultural differences in self management
(e.g., inclusion of family in self management) based on
feedback from the Health Disparities Collaborative.
Prompted by queries from the Missouri Diabetes
Prevention and Control Program, the task group formu* New Health Partnerships is supported by funding from the Robert Wood
Johnson Foundation and the California HealthCare Foundation.
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
411
The Joint Commission Journal on Quality and Patient Safety
Table 1. Timetable of Primary Care Resources and Supports for
Chronic Disease Self-Management (PCRS)of Tool Development
April 2003
First meeting of grantees and initial face-to-face work group session
Periodically, beginning July 2003
Ongoing work via teleconferences
December 2003–March 2004
Face-to-face work group meetings in conjunction with the Collaborative Learning
Network (CLN) meeting
October 2004
Work group, with consultation from experts, established format, finalized
characteristics, and worked on scaling and internal consistency
November 2004
Work group solicited feedback on the tool at CLN meeting and planned pilot tests
December 2004
New draft finalized by work group
January–February 2005
Pilot 1: external review in work group sites for clarity, conciseness, completeness,
consistency across levels, flow, and ease of use
March 2005
Pilot 2: 9 Diabetes Initiative (DI) sites; 6 sites submitted data from 52 patient care
team members representing diverse roles
April 2005 (CLN)
Work group reviewed pilot data and planned next pilot
April–May 2005
Pilot 3: conducted in non-DI sites; tool sent for review to external consultants.
The teams found it clear and useful in initiating quality improvement processes.
June 2005
Work group call to review feedback and discuss need for final changes
August 2005
PCRS tool finalized and shared with potential users
December 2005
Tool used as “pre-work” for Quality Allies Learning Community teams
lated guidelines regarding expectations of teams who
would use the tool and performance measures for monitoring purposes. Those were added to the instructions.
Initial Evaluation Results
The PCRS was first tested and evaluated outside the
Diabetes Initiative with health care teams participating in
the Institute for Healthcare Improvement (IHI)’s threeyear collaborative QI program, Quality Allies. This collaborative responded to the growing demand for patient- and
family-centered approaches to care by teaching provider
organizations how to implement robust models of collaborative self-management support through an approach
known as a “learning network.”
At the Quality Allies initial group session, all 20 health
412
July 2007
care teams from across the United States completed the
PCRS in December 2005 as a baseline assessment. As can
be seen in Table 2 (page 413), the teams varied widely, for
example, in terms of disease area of focus, type of health
system, and urban versus rural setting.
A range of 1 to 28 participants at each site completed
the PCRS. As shown in Table 3 (page 414), most items
were scored around the midpoint of the response range.
There was variation in scoring across sites, and in every
case there was adequate room for improvement (that is, no
ceiling effects). Cronbach’s alpha for the individual and
organizational support subscales were .94 and .90, respectively, indicating a high level of reliability. On the Patient
Support subscale, the most frequently endorsed item was
“Linking to Community Resources,” and the lowest-rated
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
The Joint Commission Journal on Quality and Patient Safety
Table 2. Quality Allies Learning Community Sites: Site Characteristics*
System Type
Number of Learning
Percentage of Learning
Community Sites
Community Sites
■ Integrated
1
5%
■ FQHC
3
15%
■ Academic medical center
6
30%
■ Public health
3
15%
■ Community health center
5
25%
■ IPA
1
5%
■ Hospital-based clinic
1
5%
20
100%
■ Multiple chronic conditions
5
25%
■ Diabetes
7
35%
■ HIV
3
15%
■ Cystic fibrosis
1
5%
■ Pediatric obesity
1
5%
■ Depression
2
10%
■ Multiple sclerosis
1
5%
20
100%
■ Urban
6
30%
■ Rural
5
25%
■ Mix
9
45%
20
100%
Total Learning Community Sites
Population of Focus
Total Learning Community Sites
Patient Mix
Total Learning Community Sites
* FQHC, Federally Qualified Health Centers; HIV, human immunodeficiency virus; IPA, independent provider association.
item was “Individualized Assessment of Patient’s SelfManagement Educational Needs” (Table 3).
On the Organizational Support (infrastructure) subscale, the highest-rated item was “Ongoing QI,” and the
two lowest-rated items were “Patient Input” and
“Integration of Self-Management Support into Primary
Care.”
Feedback about the use of the PCRS for QI by each of
the 20 Quality Allies teams was assessed at both the baseline and follow-up administrations (September 2006) of
the survey. Teams were asked to provide feedback based
July 2007
on their group discussions about items they spent the most
time on and the ways in which they thought they could
improve the provision of self-management supports at
their respective clinics. User feedback indicated that teams
found the PCRS helpful in their QI efforts (Sidebar 1,
page 415).
Discussion
The PCRS, which underwent a fairly extensive and iterative development and piloting process, appears to be a
user-friendly self-assessment tool. Primary care teams can
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
413
The Joint Commission Journal on Quality and Patient Safety
Table 3. Quality Allies Demonstration Sites: Cross-Site Mean Self-Ratings on Primary Care Resources and
Supports for Chronic Disease Self-Management (PCRS) Measures*
Mean/S.D.
Possible
Score Range
Quality Level
(Possible Levels =
A, B, C, D)
Individualized Assessment of Patient’s
Self-Management Educational Needs
4.8/1.8
1–10
C
Patient Self-Management Education
5.5/2.1
1–10
B
Goal Setting
5.4/2.1
1–10
B
Problem-Solving Skills
(e.g., problem identification, listing of possible solutions,
selection of one to try, assessment of the results)
5.0/2.1
1–10
B
Emotional Health
(e.g., depression, anxiety, stress, family conflicts)
5.8/2.0
1–10
B
Patient Involvement
6.1/1.9
1–10
B
Organizational Support Measures
Patient Support Measures
Primary Care Resources and Supports for Chronic
Disease Self-Management (PCRS) Submeasure
Patient Social Support
5.9/1.6
1–10
B
Linking to Community Resources
6.0/2.1
1–10
B
Continuity of Care
7.0/1.7
1–10
B
Coordination of Referrals
6.3/1.6
1–10
B
Ongoing Quality Improvement (QI)
7.0/1.8
1–10
B
System for Documentation of Self-management
Support Services
5.0/2.0
1–10
B
Patient Input
5.2/2.0
1–10
B
Integration of Self-Management Support into Primary Care
4.1/1.8
1–10
C
Patient Care Team (internal to the practice)
6.4/1.9
1–10
B
Physician, Team, and Staff Self-Management
Education & Training
5.0/1.8
1–10
B
3.2
1–28
C
Average total score for Patient Support (8 submeasures)
44.4/12.1
8–80
B
Average total score for Organizational Support
(8 submeasures)
45.9/10.1
8–80
B
Average total score on PCRS
90.3/20.9
16–160
B
Average number of respondents per site
* S.D., standard deviation.
use it to assess their current capacity to support and implement consistent patient-centered self-management congruent with the Chronic Care Model, the Expanded
Chronic Care Model,20 and the model of Resources and
5
Supports for Self Management. The initial evaluation
indicates that the PCRS has acceptable psychometric
properties and is applicable across different types of pri414
July 2007
mary care teams and chronic illness conditions.
Data confirm some findings from primary care research
based on other assessment methods and identify areas for
future QI and developmental work. Among the areas rated
as occurring least often were problem-solving assistance
(“assist” in 5 A’s terminology),10 integrating self-management support into primary care, and self-management
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
The Joint Commission Journal on Quality and Patient Safety
Sidebar 1. Quotes from the Quality Allies Teams on
the Assessment of the Primary Care Resources and
Supports for Chronic Disease Self-Management
(PCRS) Tool (Following Baseline Assessment,
November 2005)
“Through...participation in the Bureau of Primary Care’s
Diabetes Collaborative, we have focused our efforts on
PDSAs [plan–do–study–act], electronic registry population, and key measures tracking. This survey helped us
to see that though our measure goals are being met,
there are still quality improvements that may be
addressed and achieved in individual components of the
Chronic Care Model, such as self-management goal-setting for our diabetic patients.”
“The [PCRS] helped us to better define the system being
discussed and to orient ourselves as to where we are in
relation to accomplishing our objectives in chronic disease self-management in the [site name]. It also helped
us to realize that we need to have more patient and family input regarding patient service delivery and practice
policies.”
“The [PCRS] showed that there were different views on
self-management support in the group. We probably
discussed the value of centralized vs. point-of-care
resources the most. We also identified that many
providers are not aware of all the resources and how to
refer to them…..”
“The [PCRS] was useful because we saw the viewpoint
of the patient, the staff, and management. We realized
that we need to become more standardized in how we
document patient goals.”
support education and training for staff. These findings
are congruent with prior research using different samples
8,21
and methods. It was also informative that individualized
assessment for self management was rated as occurring at
a low frequency, which is likely due to time constraints of
the primary care encounter and the general unavailability
of brief, practical instruments that are both validated and
useful for primary care.22,23
Although these initial data are encouraging, the PCRS
needs further assessment and evaluation, especially in the
context of either experimentally controlled trials or before-
July 2007
and-after QI initiatives to assess its sensitivity to change.6,24
It would also be of interest to compare PCRS results with
patient reports of self-management support (for example,
using the Patient Assessment of Chronic Illness Care)7,8
especially on issues such as the extent of patient involvement in care. Finally, future research should investigate (1)
the relationship of PCRS scores to patient status on independent measures of self-management behaviors, clinical
indicators, and quality of life; (2) the relationship of
changes in the PCRS over time to improvement in these
other measures; and (3) the impact of use of the PCRS
tool and related quality self-assessment and improvement
processes on practice staff ’s quality of work life.
The ORSSM work group recommended several potential uses for the PCRS. Because it delineates the self-management support component of the Chronic Care Model,
it is compatible with and complementary to other measures that might be used in QI efforts addressing other
aspects of that model. As already stated, individual primary care practices can use the tool for planning and
assessing progress in supporting patient self-management.
The PCRS could, for example, be administered quarterly
to review progress, patterns of change, and timeliness of
improvements in support. Networks containing several
practices could use PCRS results to identify practices that
have attained higher levels of performance to serve as
models and peer leaders to others in the network.
Researchers and leaders of QI collaboratives (for example,
the IHI’s Breakthrough Series collaboratives,25,26 the Health
Resources and Services Administration’s Bureau of
Primary Health Care Health Disparities Collaboratives27)
could use the tool to index the current state of performance at community, regional, or national levels. This
information could guide development and funding of
improvement programs and additional research. Finally, as
already stated, researchers could use the tool to identify
patterns in performance in relation to outcome measures
of interest.
Primary care teams working on diverse self-management issues and different conditions are encouraged to use
the PCRS and to provide feedback on its usefulness. Such
feedback could help determine the need for additional QI
work around the tool. J
Preparation of this article was supported by funds from the Robert Wood
Johnson Foundation.
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations
415
The Joint Commission Journal on Quality and Patient Safety
Carol A. Brownson, M.S.P.H., is Deputy Director, the
Robert Wood Johnson Foundation Diabetes Initiative
National Program Office, Washington University
School of Medicine, St. Louis. Doriane Miller, M.D., is
National Program Director, the Robert Wood Johnson
Foundation Quality Allies. Richard Crespo, Ph.D., is
Professor, Department of Family and Community
Health, Marshall University School of Medicine,
Huntington, West Virginia. Sally Neuner, R.N., is
Operations Director, Holyoke Health Center, Inc.,
Holyoke, Massachusetts. Joan Thompson, Ph.D.,
M.P.H., R.D., C.D.E., is Supervisor, Preventive
Medicine Department, La Clinica de La Raza Fruitvale
Health Project, Inc., Oakland, California. Joseph C.
Wall, M.H.A., C.H.E., is Administrator, Providence St.
Peter Family Practice Residence, Olympia,
Washington. Seth Emont, Ph.D., M.S., is Principal,
White Mountain Research Associates, L.L.C., Danbury,
New Hampshire. Patricia Fazzone D.N.Sc., M.P.H.,
R.N., is Professor and Department Chair, Family
Health and Community Health Nursing, Southern
Illinois University–Edwardsville School of Nursing,
Edwardsville, Illinois. Edwin B. Fisher, Ph.D., is
National Program Director, the Robert Wood Johnson
Foundation Diabetes Initiative. Russell E. Glasgow,
Ph.D., is Senior Scientist, Kaiser Permanente
Colorado, for the Clinical Research Unit, Penrose,
Colorado. Please address requests for reprints to
Carol Brownson, cbrownso@im.wustl.edu.
References
1. Lorig K.R., et al.: Chronic disease self-management program: Twoyear health status and health care utilization outcomes. Med Care
39:1217–1223, Nov. 2001.
2. Norris S.L., et al.: Self-management education for adults with type 2
diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care
25:2115–2116, Nov. 2002.
3. Wagner E.H., et al.: Improving outcomes in chronic illness. Manag
Care Q 4:12–25, Spring 1996.
4. Wagner E.H., et al.: Organizing care for patients with chronic illness.
Milbank Q 74:511–544, 1996.
5. Fisher E.B., et al.: Ecological approaches to self-management: The
case of diabetes. Am J Public Health 95:1523–1535, Sep. 2005.
6. Bonomi A.E., et al.: Assessment of Chronic Illness Care (ACIC): A
practical tool to measure quality improvement. Health Serv Res
37:791–820, Jun. 2002.
7. Glasgow R.E., et al.: Development and validation of the Patient
Assessment of Chronic Illness Care (PACIC). Med Care 43:436–444,
May 2005.
8. Glasgow R.E., et al.: Use of the Patient Assessment of Chronic Illness
Care (PACIC) with diabetic patients: Relationship to patient characteristics, receipt of care, and self-management. Diabetes Care
416
July 2007
28:2655–2661, Nov. 2005.
9. Glasgow R.E., et al.: Assessing delivery of the five “As” for patientcentered counseling. Health Promot Int 21:245–255, Sep. 2006.
10. Whitlock E.P., et al.: Evaluating primary care behavioral counseling
interventions: An evidence-based approach. Am J Prev Med
22:267–284, May 2002.
11. Williams G.C., et al.: Supporting autonomy to motivate patients
with diabetes for glucose control. Diabetes Care 21:1644–1651, Oct.
1998.
12. Williams G.C., et al.: Testing a self-determination theory process
model for promoting glycemic control through diabetes self-management. Health Psychol 23:58–66, Jan. 2004.
13. Roter D., Kinmonth A.-L.: What is the evidence that increasing participation of individuals in self-management improves the processes and
outcomes of care? In Williams R., Herman W., Kinmonth A.-L.,
Wareham M.J. (eds): The Evidence Base for Diabetes Care. Hoboken,
N.J.: John Wiley & Sons, Ltd., 2002, pp. 679–700.
14. Robert Wood Johnson Foundation: Call for Proposals: Advancing
Diabetes Self-Management. Princeton, N.J.: Robert Wood Johnson
Foundation, Jul. 2002.
15. Robert Wood Johnson Foundation: Call for Proposals: Building
Community Supports for Diabetes Care. Princeton, N.J.: Robert Wood
Johnson Foundation, Jul. 2002.
16. Fisher E.B., et al.: Psychological factors in diabetes and its treatment.
J Consult Clin Psychol 50:993–1003, Dec. 1982.
17. Wagner E.H., et al.: Quality improvement in chronic illness care: A
collaborative approach. Jt Comm J Qual Patient Saf 27:63–80, Feb.
2001.
18. Diabetes Initiative: Lessons Learned: Tools. http://diabetesnpo.im.
wustl.edu/lessons/tools.html (last accessed May 4, 2007).
19. Institute for Healthcare Improvement (IHI): New Health
Partnerships: Improving Care by Engaging Patients. http://www.ihi.org/
IHI/Programs/StrategicInitiatives/NewHealthPartnerships.htm (last
accessed May 7, 2007).
20. Barr V.J., et al.: The expanded Chronic Care Model: An integration
of concepts and strategies from population health promotion and the
Chronic Care Model. Hosp Q 7(1):73–82, 2003.
21. Glasgow R.E., et al.: Implementing practical interventions to support chronic illness self-management. Jt Comm J Qual Patient Saf
29:563–574, Nov. 2003.
22. Babor T.F., et al.: Assessing multiple risk behaviors in primary care:
Screening issues and related concepts. Am J Prev Med 27:42–53, Aug.
2004.
23. Østbye T., et al.: Is there time for management of patients with
chronic diseases in primary care? Ann Fam Med 3:209–214, May–Jun.
2005.
24. Glasgow R.E., et al.: Practical and relevant self-report measures of
patient health behaviors for primary care research. Ann Fam Med
3:73–81, Jan.–Feb. 2005.
25. Institute for Healthcare Improvement (IHI): The Breakthrough
Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement,
2003. http://www.ihi.org/IHI/Results/WhitePapers/The Breakthrough
SeriesIHIsCollaborativeModelforAchieving+Breakthrough
Improvement.htm (last accessed May 3, 2007).
26. Improving Chronic Illness Care. http://www.improvingchronic
care.org/improvement/collaboratives/index.html (last accessed May 3,
2007).
27. Health Disparities Collaboratives: Overview.
http://www.healthdisparities.net/hdc/html/collaboratives
Overview.aspx (last accessed May 3, 2007).f Tool Development
Volume 33 Number 7
Copyright 2007 Joint Commission on Accreditation of Healthcare Organizations