What is Septic Shock? - Queensland Ambulance Service
advertisement
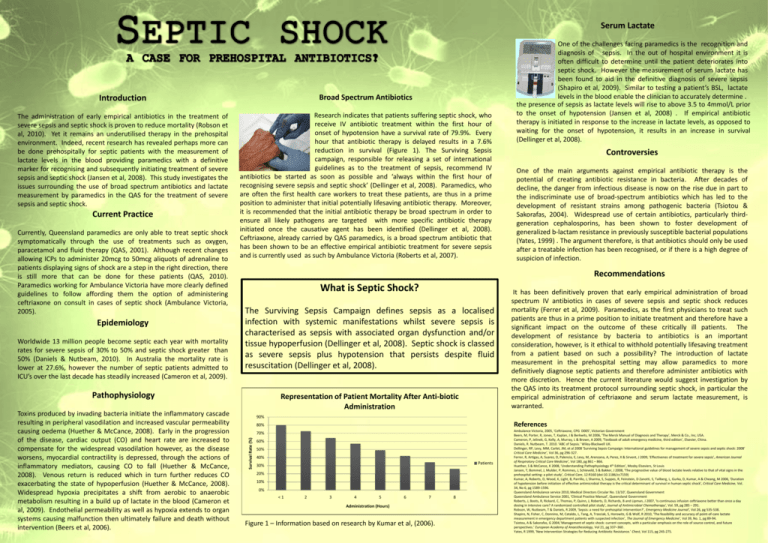
Serum Lactate Introduction Broad Spectrum Antibiotics The administration of early empirical antibiotics in the treatment of severe sepsis and septic shock is proven to reduce mortality (Robson et al, 2010). Yet it remains an underutilised therapy in the prehospital environment. Indeed, recent research has revealed perhaps more can be done prehospitally for septic patients with the measurement of lactate levels in the blood providing paramedics with a definitive marker for recognising and subsequently initiating treatment of severe sepsis and septic shock (Jansen et al, 2008). This study investigates the issues surrounding the use of broad spectrum antibiotics and lactate measurement by paramedics in the QAS for the treatment of severe sepsis and septic shock. Research indicates that patients suffering septic shock, who receive IV antibiotic treatment within the first hour of onset of hypotension have a survival rate of 79.9%. Every hour that antibiotic therapy is delayed results in a 7.6% reduction in survival (Figure 1). The Surviving Sepsis campaign, responsible for releasing a set of international guidelines as to the treatment of sepsis, recommend IV antibiotics be started as soon as possible and ‘always within the first hour of recognising severe sepsis and septic shock’ (Dellinger et al, 2008). Paramedics, who are often the first health care workers to treat these patients, are thus in a prime position to administer that initial potentially lifesaving antibiotic therapy. Moreover, it is recommended that the initial antibiotic therapy be broad spectrum in order to ensure all likely pathogens are targeted with more specific antibiotic therapy initiated once the causative agent has been identified (Dellinger et al, 2008). Ceftriaxone, already carried by QAS paramedics, is a broad spectrum antibiotic that has been shown to be an effective empirical antibiotic treatment for severe sepsis and is currently used as such by Ambulance Victoria (Roberts et al, 2007). Current Practice Currently, Queensland paramedics are only able to treat septic shock symptomatically through the use of treatments such as oxygen, paracetamol and fluid therapy (QAS, 2001). Although recent changes allowing ICPs to administer 20mcg to 50mcg aliquots of adrenaline to patients displaying signs of shock are a step in the right direction, there is still more that can be done for these patients (QAS, 2010). Paramedics working for Ambulance Victoria have more clearly defined guidelines to follow affording them the option of administering ceftriaxone on consult in cases of septic shock (Ambulance Victoria, 2005). Epidemiology Worldwide 13 million people become septic each year with mortality rates for severe sepsis of 30% to 50% and septic shock greater than 50% (Daniels & Nutbeam, 2010). In Australia the mortality rate is lower at 27.6%, however the number of septic patients admitted to ICU’s over the last decade has steadily increased (Cameron et al, 2009). Controversies One of the main arguments against empirical antibiotic therapy is the potential of creating antibiotic resistance in bacteria. After decades of decline, the danger from infectious disease is now on the rise due in part to the indiscriminate use of broad-spectrum antibiotics which has led to the development of resistant strains among pathogenic bacteria (Tsiotou & Sakorafas, 2004). Widespread use of certain antibiotics, particularly thirdgeneration cephalosporins, has been shown to foster development of generalized b-lactam resistance in previously susceptible bacterial populations (Yates, 1999) . The argument therefore, is that antibiotics should only be used after a treatable infection has been recognised, or if there is a high degree of suspicion of infection. Recommendations What is Septic Shock? The Surviving Sepsis Campaign defines sepsis as a localised infection with systemic manifestations whilst severe sepsis is characterised as sepsis with associated organ dysfunction and/or tissue hypoperfusion (Dellinger et al, 2008). Septic shock is classed as severe sepsis plus hypotension that persists despite fluid resuscitation (Dellinger et al, 2008). Pathophysiology Representation of Patient Mortality After Anti-biotic Administration It has been definitively proven that early empirical administration of broad spectrum IV antibiotics in cases of severe sepsis and septic shock reduces mortality (Ferrer et al, 2009). Paramedics, as the first physicians to treat such patients are thus in a prime position to initiate treatment and therefore have a significant impact on the outcome of these critically ill patients. The development of resistance by bacteria to antibiotics is an important consideration, however, is it ethical to withhold potentially lifesaving treatment from a patient based on such a possibility? The introduction of lactate measurement in the prehospital setting may allow paramedics to more definitively diagnose septic patients and therefore administer antibiotics with more discretion. Hence the current literature would suggest investigation by the QAS into its treatment protocol surrounding septic shock, in particular the empirical administration of ceftriaxone and serum lactate measurement, is warranted. 90% References 80% 70% Survival Rate (%) Toxins produced by invading bacteria initiate the inflammatory cascade resulting in peripheral vasodilation and increased vascular permeability causing oedema (Huether & McCance, 2008). Early in the progression of the disease, cardiac output (CO) and heart rate are increased to compensate for the widespread vasodilation however, as the disease worsens, myocardial contractility is depressed, through the actions of inflammatory mediators, causing CO to fall (Huether & McCance, 2008). Venous return is reduced which in turn further reduces CO exacerbating the state of hypoperfusion (Huether & McCance, 2008). Widespread hypoxia precipitates a shift from aerobic to anaerobic metabolism resulting in a build up of lactate in the blood (Cameron et al, 2009). Endothelial permeability as well as hypoxia extends to organ systems causing malfunction then ultimately failure and death without intervention (Beers et al, 2006). One of the challenges facing paramedics is the recognition and diagnosis of sepsis. In the out of hospital environment it is often difficult to determine until the patient deteriorates into septic shock. However the measurement of serum lactate has been found to aid in the definitive diagnosis of severe sepsis (Shapiro et al, 2009). Similar to testing a patient’s BSL, lactate levels in the blood enable the clinician to accurately determine . the presence of sepsis as lactate levels will rise to above 3.5 to 4mmol/L prior to the onset of hypotension (Jansen et al, 2008) . If empirical antibiotic therapy is initiated in response to the increase in lactate levels, as opposed to waiting for the onset of hypotension, it results in an increase in survival (Dellinger et al, 2008). 60% 50% 40% Patients 30% 20% 10% 0% <1 2 3 4 5 6 7 Administration (Hours) Figure 1 – Information based on research by Kumar et al, (2006). 8 Ambulance Victoria, 2005, ‘Ceftriaxone, CPG D005’, Victorian Government Beers, M, Porter, R, Jones, T, Kaplan, J & Berkwits, M 2006, ‘The Merck Manual of Diagnosis and Therapy’, Merck & Co., Inc, USA. Cameron, P, Jelinek, G, Kelly, A, Murray, L & Brown, A 2009, ‘Textbook of adult emergency medicine, third edition’, Elsevier, China. Daniels, R. Nutbeam, T. 2010. ‘ABC of Sepsis.’ Wiley-Blackwell UK. Dellinger, RP, Levy, MM, Carlet, JM, et al 2008 ‘Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008’ Critical Care Medicine’, Vol 36, pg 296-327. Ferrer, R, Artigas, A, Suarez, D, Palencia, E, Levy, M, Arenzana, A, Perez, X & Sirvent, J 2009, ‘Effectivenes of treatment for severe sepsis’, American Journal of Respiratory Critical Care Medicine’, Vol 180, pg 861 – 866. Huether, S & McCance, K 2008, ‘Understanding Pathophysiology 4th Edition’, Mosby Elseviers, St Louis Jansen, T, Bommel, J, Mulder, P, Rommes, J, Schieveld, S & Bakker, J 2008, ‘The prognostive value of blood lactate levels relative to that of vital signs in the prehospital setting: a pilot study’, Critical Care, 12:R160 (doi:10.1186/cc7159) Kumar, A, Roberts, D, Wood, K, Light, B, Parrillo, J, Sharma, S, Suppes, R, Feinstein, D Zanotti, S, Tailberg, L, Gurka, D, Kumar, A & Cheang, M 2006, ‘Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock’, Critical Care Medicine, Vol. 34, No 6, pg 1589-1596. Queensland Ambulance service 2010, Medical Directors Circular No. 13/10’, Queensland Government Queensland Ambulance Service 2001, ‘Clinical Practice Manual’, Queensland Government Roberts, J, Boots, R, Rickard, C, Thomas, P, Quinn, J, Roberts, D, Richards, B and Lipman, J 2007, ‘Is continuous infusion ceftriaxone better than once a day dosing in intensive care? A randomized controlled pilot study’, Journal of Antimicrobial Chemotherapy’, Vol. 59, pg 285 – 291. Robson, W, Nutbeam, T & Daniels, R 2009, ‘Sepsis: a need for prehospital intervention?’, Emergency Medicine Journal’, Vol 26, pg 535-538. Shapiro, N, Fisher, C, Donnino, M, Cataldo, L, Tang, A, Trzeciak, S, Horowitz, G & Wolf, R 2010, ‘The feasibility and accuracy of point-of-care lactate measurement in emergency department patients with suspected infection’, The Journal of Emergency Medicine’, Vol 39, No. 1, pg 89-94. Tsiotou, A & Sakorafas, G 2004,‘Management of septic shock: current concepts, with a particular emphasis on the role of source control, and future perspectives.’ European Academy of Anaesthesiology, Vol 21, pg 337–360 . Yates, R 1999, ‘New Intervention Strategies for Reducing Antibiotic Resistance.’ Chest, Vol 115, pg 24S-27S.







