pdf 23 click here
advertisement

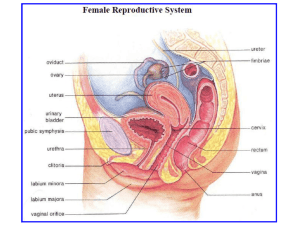
Chapter 28B Reproduction Part II: Female Reproduction Introduction: In this chapter you will learn the following: - The anatomy of the female reproductive system - The physiology of the female reproductive system - The female hormones: functions and control of secretion Lecture Materials Required: VanPutte/Seeley Text, Chapter 28 pages 1045 – 1065 CD ROM Media Phys • CD ROM, A and Revealed, Volume 4 Female Anatomy Refer to: Media Phys module 14.22 – 14.25 A&P Revealed, Reproductive System, Animations, Anatomy, Female I. Ovaries A. Describe the ovaries. B. List and describe the ligaments that attach to the ovaries. - Broad ligament: extension of peritoneum, spread out on both sides of uterus. Ovaries and uterine tubes are attached as well – Mesovarium: peritoneal fold attaches ovary to posterior surface of broad ligament (part of broad ligament) – Suspensory ligament: from mesovarium to body wall. Contains ovarian arteries, veins, and nerves – Ovarian ligament: from ovary to superior margin of uterus. Ovarian arteries, veins & nerves enter ovary through this ligament C. Histology: Describe each of the following features of the ovaries. 1. Germinal epithelium - Outermost covering: ovarian (germinal) epithelium 2. Tunica albuginea - capsule of dense fibrous connective tissue 3. Stroma - connective tissue of the ovary 4. Cortex: outer, dense. Contains follicles with oocytes 5. Medulla: inner, looser. Contains blood vessels, nerves, lymphatic vessels D. Oocyte development: Refer to Media Phys Module 14.27 – 14.28 • Oogenesis is the production of a secondary oocyte in ovaries • Oogonia are cells from which oocytes develop. Five million oogonia are produced by the 4th month of prenatal life. The oogonia divide by mitosis to produce other oogonia and primary oocytes. • Primary oocytes are surrounded by granulosa cells and are called primordial follicles – Between birth and puberty many undergo atresia – Primary oocytes begin first meiotic division but all stop at prophase I. All remain at this state until puberty (400,000) total. E. For each of the following ovarian structures: • Describe the structure • State which hormone, if any, stimulates its development • State which hormones, if any, are secreted by the structure • State which reproductive structure (for example primary oocyte), is present within the structure. 1. Primordial follicles - A primordial follicle becomes a primary follicle when the oocyte and granulosa cells enlarge – FSH- stimulates the follicular cells to divide – Several layers of granulosa cells surround follicle – Zona pellucida (glycoprotein layer) surrounds the primary oocyte – Stromal cells form a layer of thecal cells around the follicle – Thecal cells and granulosa cells secrete estrogen 2. Primary follicles - Primary follicle becomes a secondary follicle – Only a few primary follicles progress to this stage – Granulosa cells secrete follicular fluid – Fluid separates inner and outer layer of the follicle 3. Secondary follicles - Secondary follicle enlarges to form a mature or Graafian follicle - – LH increases – Primary oocyte completes meiosis I to form a secondary oocyte and a polar body – Meiosis II stops at metaphase II – Secondary oocyte and surrounding cells float free in the antrum – Some granular cells adhere to the zona pellucida as the corona radiata – As the follicle continues to develop, it forms a blister on the surface of the ovary 4. Tertiary (Graafian or mature) follicles - Graafian follicle becomes the corpus luteum - – Continued influence of LH – Empty follicle collapses, blood vessels bleed into the antrum – Granulosa cells develop into an endocrine structure which secretes estrogen and progesterone 5. Ovulation - release of a secondary oocyte from an ovary. Unlike spermatogenesis, the division of cytoplasm during meiosis is uneven and polar bodies are very small compared to the oocyte – Under influence of LH, the Graafian follicle releases secondary oocyte – Secondary oocyte and polar body are surrounded by the zona pellucidum and corona radiata 6. Corpus luteum - Fertilization: begins when a sperm cell binds the plasma membrane of a secondary oocyte and penetrates the cytoplasm. • Secondary oocyte completes meiosis II AFTER FERTILIZATION, forming another polar body. The fertilized egg is a zygote • Fate of corpus luteum – If fertilization occurs, the corpus luteum persists and secretes progesterone and estrogen 7. Corpus albicans If fertilization does not occur, the corpus luteum becomes a corpus albicans. Fibroblasts invade the corpus luteum to form scar tissue II. Uterine or fallopian tubes (oviducts) A. Describe the following structures associated with the fallopian tubes: 1. Infundibulum End closest to the ovary with numerous fimbriae, funnel shaped open distal end 2. Fimbriae Fingerlike projections surrounding infundibulum – Lined with cilia 3. Ampulla - widest and largest, where fertilization occurs 4. Isthmus - A short segment connected to the uterine wall 5. Uterine (Fallopian) Tubes - Three layers – outer serosa – middle muscular layer – inner mucosa • Mucosa: ciliated columnar epithelium with longitudinal folds – Provides nutrients for oocyte/embryonic mass – Cilia move fluid and oocyte/embryonic mass through the tube toward uterus - Fertilization occurs in uterine tube – 12-24 hours after ovulation B. Uterus Composed of 3 layers – Perimetrium: Serous membrane – Myometrium: Three layers of smooth muscle – Endometrium: Mucous membrane • Simple tubular glands • Functional layer: innermost. Replaced monthly during menstrual cycle • Basal layer: deepest and is not shed monthly 1. Describe each of the following regions of the uterus: - Fundus - Body - Uterine cavity - Isthmus - Cervix – More rigid and less contractile than rest of uterus – Cervical os (external orifice) – Cervical canal – Internal os (internal orifice) - Internal os - External os C. List the ligaments which attach to the uterus. broad, round, uterosacral – Round: from uterus through inguinal canals to labia majora – Uterosacral: attach lateral wall of uterus to sacrum D. What is the normal position of the uterus? anteflexion – Anterior and slightly superior to the bladder – Cervix enters vagina at a right angle – Vesicouterine pouch (over bladder) – Rectouterine pouch (Pouch of Douglas) over rectum E. Vessels and nerves 1. The uterine arteries branch from which major artery? – Internal iliacs - uterine arteries – Arcuate - within the myometrium – Radial – myometrium towards endometrium – Straight arteriole-basilar zone of the endometrium – Spiral arteriole - supplies the functionalis, changes during cycle t 2. Describe the sympathetic and parasympathetic innervation of the uterus. F. Histology 1. Perimetrium (serosa) - What are the vesicouterine and rectouterine pouches? 2. Myometrium 3. Endometrium - Describe the two layers of the endometrium. G. What is a Pap test? Why is it important? III. Vagina A. Describe the vagina. • Allows menstrual flow and childbirth • Receives the penis during sexual intercourse • Histology – Mucosa in transverse folds (rugae) – Longitudinal muscle capable of distention • Normal bacteria create an acid environment which inhibits infection but is hostile to sperm B. What is the fornix? superior domed portion is attached to sides of cervix Menses Proliferative Phase Secretory Phase IV. External genitalia (vulva, pudendum) A. Vestibule - cleft of labia minora 1. What two orifices are found in the vestibule? • Vaginal orifice • Urethral orifice 2. What two glands are found in the vestibule? • Paraurethral (Skene's) - embedded in walls of urethra, secrete mucus (homolog of prostate) • Greater vestibular (Bartholin's) - next to vaginal orifice, duct in a groove between hymen and labia minora, secretes mucus (homolog of bulbourethral glands B. Labia majora - scrotal homolog C. Labia minora – scrotal homolog – Medial surfaces covered with numerous sebaceous and sweat glands D. Clitoris – Erectile tissue – Prepuce formed by labia minora – Homolog of the penis E. Mons pubis (veneris) – adipose tissue, elevated area over the symphysis pubis V. Perineum A. Where is the clinical perineum found? B. What obstetrical procedure involves the clinical perineum? VI. Mammary glands A. Describe the mammary glands. • 15 - 25 lobes of glandular tissue • Lobes – contain secretory lobules – alveoli (milk-secreting cells) • Nipple is surrounded by areola • Suspensory ligaments – connective tissue surrounds ducts and portions between the lobes B. Trace the flow of milk from the alveoli to the nipple. Ducts from lobules --> lactiferous duct in each lobe Lactiferous duct --> lactiferous sinus --> nipple C. State the importance of breast self exam (BSE) and mammograms. VII. Female physiology A. Cycles 1. Uterine cycle - Describe the changes in the endometrium that occur during: • menstruation • Degeneration of functional layer • Spiral arteries constrict • Secretory cells and tissues deteriorate • Weakened arterioles rupture • Blood and degenerating tissues are sloughed off • proliferative phase – Epithelial cells of glands in basilar layer multiply – Restores functional layer – Requires estrogen • secretory phase – Endometrial glands enlarge – Arterioles elongate and spiral – Requires progesterone 2. Ovarian cycle ---------------------------------------------->> - Describe the changes that occur in the ovary that occur during: - follicular phase - ovulation - luteal phase B. Hormones: For each of the following hormones, give the following information: • the gland which secretes them • how the secretion is controlled • the function of the hormone 1. GnRH (hypothalamus) – Released in pulse cycles, each cycle has an amplitude and frequency – Changes in pulse frequency regulate the secretion FSH and LH – Low pulse frequency FSH – Higher pulse frequency LH 2. FSH (ant. pituitary) stimulates initial development of follicles and secretion of estrogen 3. LH (ant. pituitary) stimulates further development of follicles, ovulation, and secretion of estrogen and progesterone 4. Estrogens (Graafian follicle) Estradiol, estrone, estriol – Stimulate bone and muscle growth – Maintain secondary sex characteristics – Affect CNS activity – Maintain reproductive organs – Initiate growth and repair of the endometrium 5. Progesterone (corpus luteum) – Prepares endometrium for implantation and mammary glands for milk secretion – Increased progesterone inhibits GnRH which inhibits LH 6. Inhibin - inhibits FSH 7. Relaxin - at the end of pregnancy relaxes symphysis pubis and helps dilate cervix C. Cyclic relationships of the menstrual and ovarian cycles. 1. Follicular (preovulatory) phase (days 1 -13) – Increase in FSH causes primordial follicles to develop into primary follicles – Primary follicles secrete estrogen – Estrogen inhibits LH secretion – As secondary follicles develop, they secrete inhibin which causes FSH to decrease (not shown on graph) – Development of Graafian follicle maintained by the combination of estrogen, FSH and LH – Mature Graafian follicle produces a sharp increase in estrogen – Increasing estrogen causes GnRH pulse frequency to increase – Peak estrogen and maximum GnRH pulses causes a massive surge in LH – Surge in LH triggers the completion of meiosis I in graafian follicle. Meiosis proceeds to metaphase II 2. Ovulation - day 14 – Increase estrogen positive feedback on LH and GnRH. A surge in LH occurs due to high levels of estrogen and GnRH – Rupture of Graafian follicle • release of secondary oocyte and corona radiata 3. Luteal (post ovulatory) phase - days 15 – 28 – LH stimulates the remaining granulosa cells to form the corpus luteum – GnRH pulse rate increases to a level that stimulates more LH than FSH – Corpus luteum secretes progesterone and moderate amounts of estrogen – 12 days after ovulation, LH begins to decline, corpus luteum degenerates to a corpus albicans – Progesterone and estrogen levels decrease • Leads to an increase in GnRH pulse frequency and increase in FSH and LH. E. Fertilization:day 14 – 16 – Oocyte can be fertilized up to 24 hours after ovulation – Sperm cells can be viable for up to 6 days in female reproductive tract 1. What hormone secreted by the embryonic membranes functions to maintain the corpus luteum? • Embryonic membrane begins to secrete HCG (human chorionic gonadotrophin) • HCG acts like LH to maintain the corpus luteum • OTC pregnancy tests measure levels of HCG F. Cyclic relationships of the Uterus. 1. Menstrual phase (days 1 - 5) – Decrease in estrogen and progesterone – Functional layer degenerates, patchy areas of bleeding develop, discharge of functionalis 2. Proliferative phase (days 6 - 13) – Follicles are secreting large quantities of estrogen. – Rapid proliferation of endometrial cells, thickness doubles endometrial glands develop, arterioles coil & lengthen. 3. Secretory phase - days 15 – 28 – Increase LH causes the corpus luteum to increase secretion of progesterone and estrogen. – Increase progesterone prepares endometrium to receive a fertilized egg. Increase secretory activity of endometrial glands. Maximal one week after ovulation – As corpus luteum degenerates to a corpus albicans, levels of estrogen and progesterone decline, endometrium begins to degenerate, menstruation occurs G. Sexual behavior 1. Explain how sex drive regulated by hormonal and psychological factors. 2. Female fertility - What is capacitation? Activation of Sperm Cells - Once a secondary oocyte is ovulated, for how long is it capable of being fertilized? Oocyte 24 hrs. - Once deposited in the vaginal tract, how long do sperm remain viable? Sperm 72 hrs. (up to 6 days) - Where in the female reproductive tract does fertilization occur? H. Menopause 1. Describe the hormonal changes that occur during menopause. • Menstrual periods become less regular, ovulation stops – perimenopause-irregular periods • Cessation of menstrual cycles – menopause – 40-50 years of age – LH and FSH elevated, but the few remaining follicles become insensitive to LH and FSH – Ovaries stop producing estrogen and progesterone – Symptoms: hot flashes, irritability, night sweats, fatigue, anxiety, occasionally severe emotional disturbances • Uterine position changes and can lead to prolapse • Uterus decreases 50% in size within 15 years after menopause • Vaginal wall: thinner, less elastic, less lubrication. Increased incidence of vaginal infections • Increased risk of breast, endometrial, cervical, and ovarian cancer VIII. Birth control A. Describe each of the following methods of birth control: 1. Removal of reproductive organs 2. Sterilization - Vasectomy - Tubal ligation 3. Contraception - Hormonal • "Pill" and Norplant • Estrogen and high progesterone • Inhibit FSH, LH and GnRH • Prevents follicular development and ovulation • Also alters cervical mucous and endometrium - IUD - Barriers • Condom • Female condom • Diaphragm - Chemicals - Physiological • Rhythm • Sympto-thermal Laboratory Materials Required: VanPutte/Seeley Text, Chapter 28 pages 1045 – 1065 • Power Point Presentation: Female Reproduction • CD ROM A and P Revealed, Reproduction, Dissection • Breast Female • Pelvis Female, sagittal and superior • Corpus Ablicans, histology • Primary Follicle, histology • Primoidal Follicle, histology • Secondary Follicle, histology • Uterus, histology Performance Objectives: Use the materials listed above to complete the following performance objectives 1. Upon completion of the study of the anatomy of the female reproductive system, be able to identify the following structures on a drawing: a. ovary b. fimbriae c. fallopian tube d. broad ligament e. ovarian ligament u. uterus 1) endometrium f. round ligament g. anterior fornix h. posterior fornix i. urethra j. ureter k. urethral meatus l. urinary bladder m. labia majora n. labia minora o. glans clitoris p. vaginal meatus q. vagina r. vestibule s. mons pubis t. pubic symphysis 2) myometrium 3) fundus 4) body 5) cervix 6) internal os 7) external os 2. Define the term anteflexion in reference to the normal position of the uterus. 3. Upon completion of the study of the homologous reproductive structures, be able to list the male structures homologous to the following female structures: a. labia majora b. labia minora c. glans clitoris d. ovaries e. fallopian tubes 4. Upon completion of the study of the ovarian cycle, be able to identify the following structures on a drawing: a. germinal epithelium b. primordial follicle (nest cells) c. primary follicle d. maturing follicle e. mature (Graffian) follicle f. corpus hemorrhagicum g. oocyte h. developing corpus luteum i. mature corpus luteum j. corpus albicans 5. Upon completion of study of the histology of the female reproductive system, be able to: Refer to Power Point Presentation - Female a. identify the following structures of the ovary slide: 1) egg nests 3) mature follicle 2) immature follicles 4) secondary oocyte b. identify a corpus luteum on the corpus luteum slide c. identify the myometrium and endometrium on the slide of the uterus d. identify the slide of the fallopian tube and relate its structure to the functions it performs 6. Upon completion of study of the anatomy of the mammary gland, be able to identify the following structures on a drawing: a. lobe b. areola c. papilla d. lactiferous sinus e. lactiferous ducts 7. Upon completion of the study of female hormones, be able to: a. relate the models of the menstrual cycle (ovary and uterus) to the days of the menstrual cycle and describe the level of pituitary hormones, estrogen, and progesterone during the days of the cycle b. discuss the feedback mechanism involved in the control of the menstrual cycle c. relate the slide of the uterus to the hormonal controls of estrogen, progesterone, oxytocin, and prostaglandins d. state hormone which stimulates the graffian follicle to develop e. state hormone which is secreted by the maturing follicle f. state the hormones necessary for ovulation g. state the hormone necessary for the development of the corpus luteum h. state the two hormones secreted by the corpus luteum i. state the effect of estrogen on FSH secretion j. state the effect of progesterone on LH secretion 8. Upon completion of the study of the process of oogenesis, be able to: a. explain the process of oogenesis using the following terms: 1) oogonium 4) ovum 2) primary oocyte 5) first polar body 3) secondary oocyte 6) second polar body b. relate the slide of the ovary and the model of the ovarian cycle to the process of oogenesis c. relate the stages of oogenesis including primary oocyte, secondary oocyte, and polar bodies to the menstrual cycle