![Quantification of [ F]diprenorphine kinetics in the human brain with](//s3.studylib.net/store/data/008858163_1-72f2d0d46bf0d160df98a688f97feda5-768x994.png)
www.elsevier.com/locate/ynimg
NeuroImage 22 (2004) 1523 – 1533
Quantification of [18F]diprenorphine kinetics in the human brain with
compartmental and non-compartmental modeling approaches
Mary E. Spilker, a,* Till Sprenger, b Michael Valet, b Gjermund Henriksen, a Klaus Wagner, c
Hans-J. Wester, a Thomas R. Toelle, b and Henning Boecker a
a
Nuklearmedizinische Klinik und Poliklinik, Klinikum rechts der Isar, Technische Universität München, München, Germany
Neurologische Klinik und Poliklinik, Klinikum rechts der Isar, Technische Universität München, München, Germany
c
Klinik für Anästhesiologie, Klinikum rechts der Isar, Technische Universität München, München, Germany
b
Received 31 October 2003; revised 31 March 2004; accepted 6 April 2004
6-O-(2-[18F]fluoroethyl)-6-O-desmethyldiprenorphine ([18F]FDPN) is a
nonselective opiate ligand that binds to postsynaptic M, K and D opiate
receptors. Due to the longer half-life of F-18, compared to C-11,
labeling DPN with F-18 allows for alternative experimental protocols
and potentially the evaluation of endogenous opioid release. The
applicability of this compound to assorted experimental protocols
motivated the evaluation of [18F]FDPN kinetics with compartmental
and non-compartmental models. The results indicate that a two-tissue
compartmental model best characterizes the data obtained following a
bolus injection of [18F]FDPN (120-min scanning protocol). Estimates of
distribution volume (DV) were robust, being highly correlated for the
one-tissue compartmental model as well as the invasive Logan model
and the basis function method. Furthermore, the DV estimates were
also stable under a shortened protocol of 60 min, showing a significant
correlation with the full protocol. The binding potential (BP) values
showed more variability between methods and in some cases were more
sensitive to protocol length. In conclusion, this evaluation of [18F]FDPN
kinetics illustrates that DV values can be estimated robustly using
compartmental modeling, the basis function method or the invasive
Logan modeling approach on a volume of interest level. BP values were
also found to correlate with DV values; however, these results should be
interpreted with the understanding that specific binding in the
reference region (occipital region) may exist.
D 2004 Elsevier Inc. All rights reserved.
Keywords: [18F]diprenorphine; Kinetic models; Ligand; Opiate receptors;
PET
Abbreviations: DV, distribution volume; BP, binding potential; 2T, twotissue compartmental model; 1T, one-tissue compartmental model;
Inv_Logan, invasive Logan model; BFN, basis function method; NonInv_Logan, noninvasive Logan model; SRTM, simplified reference tissue
model; TRM, tissue ratio method.
* Corresponding author. Nuklearmedizinische Klinik und Poliklinik der
Technischen Universität München, Klinikum rechts der Isar, Ismaninger
Strasse 22, 81675 München, Germany. Fax: +49-89-4140-4938.
E-mail address: mspilker@lrz.tu-muenchen.de (M.E. Spilker).
Available online on ScienceDirect (www.sciencedirect.com.)
1053-8119/$ - see front matter D 2004 Elsevier Inc. All rights reserved.
doi:10.1016/j.neuroimage.2004.04.009
Introduction
The radioligand, [11C]diprenorphine ([11C]DPN), is commonly used to assess the opiate receptor system in physiologic
and pathophysiologic conditions (Duncan, 1999; Jones et al.,
1991; Mayberg et al., 1991; Sadzot et al., 1990; Weeks et al.,
1997). However, applicability of this radioligand to long
acquisition protocols can be limited due to the short half-life
of 11C (t1/2, C-11 = 20 min). Thus, efforts were made to
synthesize 6-O-(2-[18F]fluoroethyl)-6-O-desmethyldiprenorphine
([18F]FDPN) (Wester et al., 2000), which has similar pharmacologic properties to [11C]DPN, but a longer half-life (t1/2, F-18
= 109.7 min). [18F]FDPN is now applicable to alternative
experimental designs, including single bolus protocols investigating endogenous ligand release (Alpert et al., 2003; Pappata et al.,
2002; Sprenger et al., 2003), which may serve as alternatives to
the two scan or bolus plus constant infusion approaches. Furthermore, this compound can be used at centers without an on-site
cyclotron, thereby increasing its usage in the assessment of the
opiate receptor system as well as its use in routine clinical
evaluations. Due to the longer half-life, this compound also shows
improved signal intensity compared that of [11C]DPN, which
results in an improved signal to noise ratio (SNR) (Wester et al.,
2000).
The potential application of [18F]FDPN within the scientific
and medical community motivated the characterization of this
compound’s time-varying dynamics in a population of normal
healthy subjects. Therefore, we have undertaken a kinetic study
to compare the performance of various modeling approaches
with the [18F]FDPN tracer. The invasive models assessed here
include the standard one-tissue and two-tissue compartmental
models, the Logan model and the basis function method.
Additionally, three reference tissue models were examined,
including the noninvasive Logan model, the simplified reference
tissue model and the tissue ratio method. The performance of
each model is evaluated and estimates of distribution volume
(DV) and binding potential (BP) are compared. Lastly, the
stability of the DV and BP parameters are also examined for a
shortened protocol.
1524
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
Materials and methods
Data acquisition
Six healthy volunteers (mean age 42 years, range 30 – 59 years;
two females, four males) underwent a [18F]FDPN PET-study as
part of an existing protocol. All subjects gave informed written
consent and the study protocol was approved by the ethics
committee at the Technische Universität München and the radiation protection authorities. Images were acquired over 120 min
with the following frame durations: 6 30 s; 7 1 min; 4 2.5
min; 2 5 min; 3 10 min; 5 2 min; 4 2.5 min; 2 5 min;
3 10 min for a total of 36 frames. The subjects studied here
served as controls in a protocol involving a challenge at 60 min
p.i.; while they did not receive any challenge, the frame lengths
reflect such a paradigm. PET scans were acquired using a
Siemens/CTI ECAT EXACT HR+ scanner (Knoxville, TN,
USA) in 3D mode with septa retracted. A neck-shield (NeuroShield, Scanwell Systems, Lavigne St., Montreal, Canada) was
used to reduce random count rates. Attenuation was corrected
using transmission scanning before the [18F]FDPN studies. The
acquired data were reconstructed using filtered backprojection
with a ramp filter (cut-off 0.3 cycles per projection element) into
63 image planes with a 128 by 128 pixel image matrix and a final
spatial resolution of 2.0594 2.0594 2.425 mm. In addition to
the dynamic PET images, high-resolution T1-weighted anatomical
MR images were also acquired for each subject using an MPRage sequence.
The radioactive tracer was injected as an intravenous bolus with
a mean injected radioactive dose of 3 mCi (specific activity: 1000 –
1500 mCi/Amol). Arterial blood samples were acquired throughout
the scanning period as fast as possible for the first 2 min followed
by samples at increasingly spaced intervals ranging from 20 s to 5
min. The metabolites were measured at time points of 5, 15, 30, 60
and 90 min p.i. to allow for the generation of a metabolite corrected
arterial input function. This is performed by fitting a biexponential
function [A exp(a t) + B exp(b t)] to the fraction of intact
tracer. The total plasma curve is then multiplied by this function to
arrive at the metabolite corrected input function.
Following acquisition, all images were transferred to a standard
PC and then realigned and resliced using SPM99 (Wellcome Dept.
of Cognitive Neurology, London, UK). The MR images were coregistered to the 4D (x, y, z, time) dynamic PET data sets using the
Mutual Information subroutine in SPM99. The MR images were
then used to select individualized volumes of interest (VOIs)
corresponding to the following locations: occipital cortex, cingulate cortex, frontal cortex, putamen/caudate, thalamus and cerebellum. The cingulate cortex, putamen/caudate, thalamus and
cerebellum were selected using free-form VOIs, while 10-mm
spherical VOIs were used for the occipital and frontal regions.
These regions were selected based on a priori knowledge that they
contain a range of opiate receptor densities, from minimal opiate
receptors in the occipital region to high receptor density in the
thalamus and basal ganglia.
mertsma and Hume, 1996), the basis function method (Gunn et
al., 2001, 2002) and the tissue ratio method (Endres et al., 2003;
Frost et al., 1989). The models are described below and their
parameters, along with their relationship to DV and BP are
summarized in Table 1. There are also several detailed reviews
of these models available in the literature (Laruelle et al., 2002;
Meyer and Ichise, 2001). Note that the occipital region was
specified as the reference region for all models and calculations
where necessary.
Unless otherwise stated, all modeling was performed using
the Kinetic tool in the PMOD Medical Imaging Program,
version 2.4 (PMOD Group, Zurich, Switzerland). The PMOD
program uses the Levenburg – Marquardt routine when performing nonlinear least-squares fitting and otherwise solves the
analytical model equation(s) when appropriate. The error model
for the nonlinear fitting was assumed to be Gaussian with mean
zero and standard deviation proportional to the square root
of the total counts within each frame divided by the frame’s
duration.
Invasive kinetic models
A two-tissue compartmental model (2T) with a plasma input
function was applied to the data and adjusted appropriately to
evaluate both reversible and irreversible specific binding. The
differential equations corresponding to the 2T model with reversible kinetics are given below.
dCF þ NS ðtÞ
¼ K1 Cp ðtÞ ðk2 þ k3 ÞCF þ NS ðtÞ þ k4 CS ðtÞ
dt
ð1Þ
dCS ðtÞ
¼ k3 CF þ NS ðtÞ k4 CS ðtÞ
dt
ð2Þ
CVOI ðtÞ ¼ CF þ NS ðtÞ þ CS ðtÞ þ Vp CWP ðtÞ
ð3Þ
where Cp is the metabolite corrected arterial plasma tracer concentration (kBq ml1); CF + NS is the concentration in the free and
nonspecifically bound tracer in the tissue (kBq ml1); CS is the
Table 1
Model parameter summary
Invasive methods
2T
Parameters K1, k2, k3, k4,Vp
k1
k3
DV
1þ
k2
k4
k3
k4
BP
1T
Inv_Logan
K1, k2, Vp
slope, intercept /i,hi
k1
k2
DVVOI
1
DVref
slope
BFN
DV ¼
n
P
/i
i ¼1
DVVOI
1
DVref
hi
DVVOI
1
DVref
Noninvasive methods
SRTM
NonInv_Logan TRM
Kinetic model descriptions and implementation
Parameters R1, k2, BP
DV
–
BP
BP
The kinetic behavior of [18F]FDPN was quantified using
compartmental models (one- and two-tissue models) (Slifstein
and Laruelle, 2000), the Logan model (invasive and noninvasive)
(Logan, 2000), the simplified reference tissue model (Lam-
2T, two-tissue compartment model; 1T, one-tissue compartment model;
Inv_Logan, invasive Logan model; BFN, basis function method; SRTM,
simplified reference tissue model; NonInv_Logan, noninvasive Logan
model; TRM, tissue ratio method; DVR, distribution volume ratio.
DVR, intercept BPratio
DVR
–
DVR 1
BPratio
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
concentration of specifically bound tracer in the tissue (kBq ml1);
CWP is the concentration of tracer in whole plasma without
correction for metabolites. K1 (ml ml1 min1) is the tracer’s rate
of exchange from the vasculature to the tissue, while k2 describes
the efflux of tracer from tissue to plasma. The rate constants, k3 and
k4, quantify the rate of specific binding and release of the ligand.
The rate constants, k2, k3 and k4, are first-order rate constants with
units of min1, while Vp (ml/ml) is the fractional plasma volume
within the VOI.
Although a three-tissue compartmental model (free, nonspecific
and specific compartments) was evaluated, the kinetic parameters
of this model could not be identified with adequate precision and
the model was simplified. If it is assumed that the free and
nonspecific binding compartments exchange at a faster rate than
the free and specific binding compartments, then the former can be
lumped together, reducing the model to the two-tissue compartmental model described here.
A one-tissue compartmental model (1T) was also applied to the
data for each VOI according to Eqs. (4) and (5).
CT ðtÞ ¼ K1 ek2 t Cp ðtÞ
ð4Þ
CVOI ðtÞ ¼ CT ðtÞ þ Vp CWP ðtÞ
ð5Þ
Here, the estimated parameters include K1, k2 and Vp and the
symbol, , represents the convolution function. This model is most
appropriate when the specific binding compartment cannot be
resolved due to rapid binding and release of the ligand.
The basis function (BFN) method is a data-driven modeling
approach where no a priori structure is assumed to characterize
the data. Instead, an impulse response function is generated from
a sum of exponentials that describes the data given the input
function. The DV is then determined from the integral of the
impulse response function. The BFN method evaluated here uses
basis pursuit denoising as implemented in the DEPICT software
(Gunn et al., 2001, 2002) according to Eq. (6) and the DV is
calculated as defined in Eq. (7). This method eliminates the
positive constraint on the coefficients (/i) that was necessary
under the spectral analysis method by including a regularization
term so that the underdetermined system of equations can be
solved.
CT ðtÞ ¼ Vp CWP ðtÞ þ ð1 Vp Þ
n
X
/i eh;t Cp ðtÞ
ð6Þ
i¼1
DV ¼
n
X
/i
i¼1
ð7Þ
hi
The final invasive model applied to the data was the invasive
Logan model (Inv_ Logan), which transforms the data so that a
linear relationship exists between two variables and the slope of
this relationship equals the DV.
Z
Z
t
CVOI ðuÞdu
0
CVOI ðtÞ
¼ DV
t
Cp ðuÞdu
0
CVOI ðtÞ
þ int
ð8Þ
1525
To ensure linearity in the transformed data, frames 60 – 120 min p.i.
were included in the invasive Logan analysis. For the shortened
protocol, a linear fit was performed with the transformed data
corresponding to original frames between 25 and 60 min p.i.
Noninvasive (reference region) models
The noninvasive Logan model (NonInv_ Logan) replaces Cp(t)
in Eq. (8) with CREF(t) and an additional term, CREF(t) / kref
2 , is
added to the equation.
Z
Z
t
CVOI ðuÞdu
0
CVOI ðtÞ
¼ DVR
0
t
CREF ðuÞdu þ CREF ðtÞ=k2ref
CVOI ðtÞ
þ Int
ð9Þ
In this model’s analysis, the linear fit was performed between the
same frames as described for the invasive Logan model. This
model was implemented using a gradient-expansion algorithm for
nonlinear least-squares fitting in IDL 5.6 (Research Systems Inc,
Boulder, CO, USA).
The simplified reference tissue model (SRTM) assumes that the
VOI data can be characterized using a one-tissue compartment
model and that the distribution volume in the tissue of interest and
the reference region are approximately equal, such that K1,VOI /
k2,VOI = K1,REF / k2,REF. With these assumptions, the parameter, R1,
is defined as K1,VOI / K1,REF, and the operational equation can be
defined for a VOI as follows.
CVOI ðtÞ ¼ R1 CREF ðtÞ þ ½k2 þ R1 k2 =ð1 þ BPÞ
CREF ðtÞ
exp½k2 t=ð1 þ BPÞ
ð10Þ
In the above equation, the three parameters that are estimated
include R1, k2 and BP. The full four-parameter reference tissue
model was also examined; however, it performed approximately as
well as the SRTM; therefore, only results from the SRTM are
presented here.
Tissue ratio method
The tissue ratio method (TRM) calculates a binding potential
ratio: BPratio = (TACVOI TACREF)/TACREF, where TACVOI and
TACREF are the time activity curves for the receptor rich and
reference regions, respectively (Endres et al., 2003; Frost et al.,
1989). For this data set, the BPratio was calculated as the average
of the ratio values from time points of 80 – 120 min p.i. using
standard data processing software. The choice to start at 80 min
was made since a plateau in the BPratio began between 70 and 80
min p.i.
Model assessment
Several criteria were used to compare the performance of each
compartmental model. Goodness of fit was assessed both visually
and statistically using the Runs Test of the residuals, which is a
statistical test for the randomness of the residuals. Model parsimony was evaluated using the Akaike Information Criteria (AIC),
where the lowest AIC value is an indication of the better model fit
to the data (Akaike, 1974). Finally, parameter coefficients of
1526
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
variation (CV = standard deviation / mean) were examined to
quantify parameter precision. The performance of the various
models was also compared in terms of the DV and BP values.
For consistency, all measures of bias in DV and BP between the
various methods were compared to the 2T model with reversible
specific binding and reported as percentages according to the
following equation.
%Bias ¼
ðĥ h2T Þ
100%
h2T
ð11Þ
where, ĥ is the model’s estimate of DV or BP and h2T is the
estimate of DV or BP as determined from the 2T model. All
correlation measures are reported as Pearson R2 values. Correlations and statistical tests were performed in GraphPad Prism
version 4.00 for Windows (GraphPad Software, San Diego, CA,
www.graphpad.com).
Results
Compartmental model performance
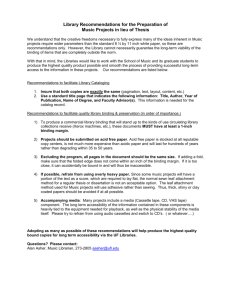
Representative time activity curves from a single subject are
shown in Fig. 1. Fig. 2 presents the model fits from the 2T and 1T
analyses to data from the occipital and thalamus VOIs of this
subject. In general, the 1T model tended to underestimate the
kinetic behavior at early and late time points while overestimating
the concentration in the middle portion of the curve. This was
especially evident in the occipital and cerebellum VOIs, which
were both fit optimally with a 2T model.
The performance criteria for each compartmental model are
summarized in Table 2. The results of this work found that the 2T
model with reversible specific binding best characterized the
majority of the VOIs across all regions and subjects as determined
from the AIC values (67%) and random scatter of the residuals
(89%). While a 2T model with irreversible specific binding (k4 = 0)
performed better than the 1T model with regards to AIC values and
random scatter of the residuals, it did not perform as well as the 2T
model with reversible specific binding (k4 p 0) when considering
all of the model performance criteria. This is appropriate since
[18F]FDPN is an antagonist and not expected to be internalized
after binding.
In general, the parameter CVs were higher for the 2T model
compared to the 1T model, which is expected given the increased
model complexity resulting from the presence of the specific
binding compartment. In 14% of the 2T model fits, at least one
parameter had a CV greater than 100%. Usually, the k3 and k4
parameters showed the highest CVs, with the maximal CV of 158%
observed across all subjects and regions. However, even with
larger CVs on the parameters, the model fits to the data were
clearly improved for the 2T model vs. the 1T model.
While the 2T model produced an optimal fit to the majority of
the VOIs, the k3/k4 ratio did not reflect BP values consistent with
those found in the literature for [11C]DPN (determined from a
pulse-chase experiment) (Jones et al., 1994) and [18F]FDPN
(determined from spectral analysis and reference tissue models)
(Lochmann et al., 2003). Note that Jones et al. (1994) also found
it difficult to attain reliable k3/k4 values from a tracer study for
[11C]DPN. In the current study, BP was determined for the 2T
model in the same manner as with the other methods, namely,
(BP = DVVOI/DVREF) 1, where a 2T model was applied to
both the VOI and reference region.
Distribution volume
The DV values from the compartmental, Inv_Logan and BFN
methods are reported in Table 3. The regional DV values are
consistent with the expected outcome of high receptor density in
the thalamus, decreasing to the lowest in the occipital region. The
BFN method resulted in the highest DV values for all regions
except the occipital region, where the 2T model resulted in
higher DV values. The large standard deviations associated with
each regional mean DV value illustrate the degree of interindividual variability within this population of normal, healthy
subjects.
Fig. 1. Time activity curves for a single subject. Occipital (x); cerebellum (5); frontal cortex (n); putamen/caudate (+); thalamus (E).
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
1527
Fig. 2. Representative 2T and 1T model fits. Occipital (x); thalamus (E); 2T model fit (solid line); 1T model fit (dashed line).
The range of the DV values from minimum to maximum
across all subjects and regions was also examined and found to
be smaller for the Inv_ Logan model (37.01), but quite similar
between the compartmental models (40.84 2T model; 40.39 1T
model). The largest range was observed with the BFN method
(43.93).
DV values determined from the 2T model correlate well with
those from the 1T model, Inv_ Logan model and BFN method
(Fig. 3). The BFN method exhibited the most variability in DV
values compared to the 2T model and thus resulted in the lower
R2 value of 0.917 compared to the other methods, which had R2
values greater than 0.934; however, all correlations were significant (P < 0.0001). The mean bias between the 2T model and
other invasive modeling approaches was less than 15% (Table 4)
when excluding the occipital region, which showed an increased
difference between modeling methods. The DV for the occipital
region was consistently underestimated by the 1T and Inv_ Logan
approaches. The Inv_ Logan model also consistently underestimated the DV values, with the exception of the frontal region,
suggesting a unidirectional bias in the results of this modeling
approach. This is not always the case when considering the 1T
and BFN models, as can be observed from the large standard
deviations compared with the mean values.
Binding potential
In this study, an estimate of the BP independent of the reference
region was not possible; therefore, any biases introduced by the
reference region could not be evaluated. Instead, a comparison of
the BP values between the different models is presented. The mean
BP values across all regions are reported in Table 5. These values
are lower than those observed for [11C]DPN (Jones et al., 1994) and
with the exception of the cerebellum are consistent with those
reported for [18F]FDPN (Lochmann et al., 2003). Discrepancies
between the 2T and other methods are likely influenced by the
occipital DV values, which were consistently higher with the 2T
model compared with the other invasive models. Furthermore,
while the R2 values of the BP regressions with the 2T model derived
BP values were reduced (Table 5) compared to the regressions with
DV values (Fig. 3), all methods still resulted in significant correlations ( P < 0.0001). Additionally, the normalized mean BP values
(Table 6) illustrate a larger range of values across regions for the
invasive methods compared to the noninvasive methods.
A regression analysis was performed between the BP values
determined from all models and the DV values estimated from the
Table 3
DV values across regions
Table 2
Model performance summary
a
Lowest AIC value
Randomly scattered
residualsb
CVs < 100%b
2T (k4 p 0) (%)
2T (k4 = 0) (%)
67
89
25
83
8
39
86
86
100
1T (%)
A total of 36 VOIs were evaluated. 2T( k4 p 0) corresponds to a 2T model
with reversible specific binding; 2T (k4 = 0) corresponds to an 2T model
with irreversible specific binding.
a
Percentage of VOIs meeting the criterion between all three models.
b
Percentage of VOIs meeting criterion for each model.
Refer to Table 1 for label descriptions. Values are reported as mean F SD.
Colored lines report results from the full 120-min protocol, while white
lines report results from the 60-min protocol.
1528
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
Fig. 3. Distribution volume. Lines represent regression with the 2T model. 1T model (5; dotted line); Inv_ Logan model (E; dashed line); BP (x; solid line).
2T model. When all subjects were examined together, the BP
values exhibited more variability and lower R2 values (0.291 –
0.717) but all correlations were still significant (P V 0.0025). In
examining the plots, it was observed that the BP values of two
subjects were significantly higher than the values determined for
the other subjects. This in turn was adding variability to the
correlation plot and thereby reducing the correlation’s R2 value.
When the BP and DV values were compared on a per subject basis,
the minimum R2 value observed was 0.716 for the comparison of
the BP determined with the basis function method vs. the DV value
estimated from the 2T model. These results illustrate the consistency between DV and BP estimates.
Shortened protocol
A shorter protocol with a length of 60 min rather than the full
120 min p.i. was performed to examine the stability of the DV
and BP estimates. The DV values from the short and full protocol
are reported in Table 3. It can be seen that the short protocol
resulted in lower DV values than those determined from the 120min protocol. In some cases, it was more difficult to resolve the
extra compartment with the shorter protocol and it can be
observed that the 2T and 1T model results are becoming
increasingly similar.
Table 4
Percentage of differences in DV values (120-min protocol)
Region
1T
Inv_ Logan
Thalamus
Putamen/caudate
Cingulate
Frontal
Cerebellum
Occipital
7.92
5.29
3.04
2.59
4.04
21.61
F
F
F
F
F
F
13.42 10.67
7.90
10.59
6.05
8.90
5.25
3.26
8.84
3.59
16.93 18.45
F
F
F
F
F
F
8.51
7.44
2.99
3.48
3.28
13.52
The DV values from the shorter protocol were found to
correlate with the DV values estimated from the 2T model applied
to the entire 120-min data set (R2 values: 2T model, 0.854; 1T
model, 0.865; Inv_ Logan, 0.847; BFN, 0.606). The basis function
method showed the most variability in DV values and therefore
resulted in the lower R2 values observed here. Additionally, all
correlations of DV values between the long and short protocols
were found to be significant (P < 0.0001).
The BP values were used to evaluate the performance of the
noninvasive methods under the 60-min protocol and are reported in
Table 5. It can be observed that the SRTM showed minimal
changes in BP values between the long and short protocols. The
majority of regions assessed with the noninvasive methods showed
a decrease in BP under the short protocol when compared to the
long protocol, while the invasive methods showed the opposite
effect. Also, excluding the 1T model, the noninvasive methods
were less variable than the invasive methods when each was
compared separately for differences between long and short protocols (R2 values: noninvasive methods, 0.936 – 0.972; invasive
methods, 0.339 – 0.857; 1T, 0.937). These within method regressions were significant at P < 0.0001, with the exception of the BFN
method (P = 0.0017).
Lastly, it can be observed that the basis function method
resulted in smaller estimates of BP for the cerebellum. This is
propagated into the large differences in the normalized BP
values observed with the basis function method presented in
Table 6.
BFN
14.38
4.89
1.53
12.67
10.30
10.29
F
F
F
F
F
F
21.27
19.86
17.20
11.41
21.68
18.67
Values were compared with the 2T model using Eq. (11) and are reported as
mean F SD. 1T, one-tissue compartmental model; Inv_ Logan, invasive
Logan model; BFN, basis function method.
Discussion
In ligand binding studies, it is desired to determine the receptor
density and the binding/release of a ligand under different physiologic conditions. Thus, in the analysis of PET radioligand
experiments, kinetic models have been formulated that provide
surrogate measures of ligand binding kinetics (e.g. Bmax/Kd)
(Mintun et al., 1984). In this regard, the macro-parameters of
DV and BP have been established as standard outcome measures
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
1529
Table 5
Binding potential values
Refer to Table 1 for label descriptions. Values are reported as mean F SD. Colored lines report results from the full 120-min protocol, while white lines report
results from the 60-min protocol.
a
BP was calculated as (DVVOI/DVREF) 1 rather than k3/k4.
b
Regressions with BP determined from the 2T model for the long protocol (120 min). All were significant at p < 0.0001.
c
Mean BP values taken from literature. [18F]FDPN, BP values determined from spectral analysis (Lochmann et al., 2003); [11C]DPN, BP values determined
from a pulse-chase experiment (Jones et al., 1994).
for ligand binding studies. These parameters are combinations of
the directly estimated model parameters and are often more stable
than the micro-parameters that generate them. To provide some
insight into the appropriate models and outcome measures for
[18F]FDPN, we evaluated this tracer’s kinetics using seven standard models, including both invasive and noninvasive models
under a bolus injection protocol. The macro-parameters, DV and
BP, were then compared between the various modeling approaches.
In this study, invasive compartmental models were applied to
determine the maximal number of identifiable compartments given
the current protocol, noise level and kinetic behavior of the data. It
was observed that a two-tissue compartmental model could successfully characterize the majority of the VOIs evaluated. The
parameter precisions degraded somewhat with increasing model
complexity; however, the DV estimates were comparable for both
the 2T and 1T models.
Table 6
Normalized BP values
Refer to Table 1 for label descriptions. All values are normalized to the
cerebellum. Colored lines present results from the full 120-min protocol,
while white lines present results from the 60-min protocol.
Under the shortened protocol, a 2T model could still be applied;
however, the 2T and 1T model fits were increasingly similar and
the DV estimates from these two model structures appear to be
converging. This suggests that under the shortened protocol, it is
increasingly difficult to quantify k3 and k4 appropriately and that a
simplification to the 1T model may be necessary, which may in
turn lead to an underestimation of absolute DV values.
The other outcome measure of interest, BP, can be defined as
the k3/k4 ratio estimated from the 2T model; however, we were
unable to attain reasonable estimates for this ratio. Jones et al.
(1994) also found it difficult to attain reliable k3/k4 values from a
tracer study for [11C]DPN, yet noted that the DV estimates from the
tracer studies correlated well to the BP values obtained from pulsechase studies. Additionally, the significant correlations between BP
and DV values observed here suggest that DV and BP values are
providing similar relative information about [18F]FDPN binding
kinetics.
While compartmental models provide the most physiologically
detailed description of the data (where compartments and rate
constants often have direct physiologic interpretations), it is unlikely that the SNR of the data at a voxel level is sufficient to allow for
the application of a compartmental model to the formation of
parametric images. There is, however, increasing interest and utility
in generating parametric images. Therefore, two additional invasive
models (Inv_ Logan and BFN) that have previously been used in
parametric image analysis were also evaluated. The BFN method is
a data-driven method that does not make any assumptions on the
connectivity of the compartments as does the compartmental
modeling approach and its counterpart, spectral analysis, has been
1530
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
previously applied in the analysis of [11C]DPN data (Piccini et al.,
1997; Weeks et al., 1997; Willoch et al., 1999, 2004) and
[18F]FDPN (Lochmann et al., 2003). For the data analyzed here,
we observed that the BFN method performed well and the resulting
DV values were significantly correlated with those from the 2T
model (R2: 0.917; P < 0.0001). This method resulted in DV values
that were more variable across subjects and the values were slightly
higher, yet consistent with the other methods. While differences in
the absolute mean DV values were observed (Table 3), the mean
regional DV distributions when normalized to the occipital region
were more similar between the long and short protocols for the BFN
method than the other methods. This may reflect the method’s
ability to characterize the data without imposing a particular
compartmental structure upon the data. This aspect of the method
supports its use in future studies.
The Logan model is a graphical-based method which can be
easily applied on a voxel-by-voxel basis since it is performing a
linear fit to the transformed data. However, this approach can lead
to biased estimates for DV and additionally requires that the data be
evaluated for times when a linear relationship exists between the
transformed variables (Logan, 2000; Slifstein and Laruelle, 2000,
2001). Thus, the invasive Logan model was evaluated against the
compartmental approaches to determine any potential biases in the
model’s DV estimates for [18F]FDPN. A greater mean bias from the
2T model was observed with the Inv_ Logan model compared with
that observed for the 1T model. The Inv_ Logan model also
consistently underestimated DV across all regions with greater
biases observed in regions with higher DV values. This is consistent with the findings in the literature (Logan, 2000; Slifstein and
Laruelle, 2000). Note that the results presented here are based on a
VOI analysis and the performance of the Logan model may be
more variable in a parametric analysis due to the increased amount
of noise on each voxel.
Noninvasive modeling methods, which are also commonly
referred to as reference region methods, could potentially circumvent the need for arterial sampling thereby reducing the risk and
discomfort to the patient and simplifying the experimental and
analysis protocols. While these methods are clearly attractive, the
performance of reference region methods should be carefully
evaluated before routine application. We thus included three such
methods (the noninvasive Logan model, SRTM and tissue ratio
method), which are all applicable to the generation of parametric
images. The occipital region was chosen as the reference region for
the noninvasive models. With regards to the models implemented
here, the SRTM and NonInv_ Logan models resulted in similar BP
values, which were consistent with those estimated from the 2T
model. When comparing the full and shortened protocols, the
NonInv_ Logan showed a greater difference under the shortened
protocol than did the SRTM, which may reflect the fact that the
NonInv_ Logan is affected by the noise in the transformed variables
and possibly the fact that fewer data points were contributing to the
analysis, since the model was applied to data between 25 and 60
min p.i., whereas the SRTM made use of the entire data set up to
60 min.
The TRM’s BPratio values were found to correlate with estimates of BP determined by the 2T model, although they were
higher across all regions under the full protocol. Since the current
analysis follows a bolus injection protocol, we have most likely
reached a transient equilibrium. Here, a constant BP value can be
achieved since a constant ratio exists between the VOI and
reference region, which is due to an equivalent rate of radioactive
clearance between the two regions. However, we must emphasize
that the resulting BP values may not be equivalent to the actual BP
that is achieved at true equilibrium or through kinetic modeling.
Carson et al. (1993) has illustrated that large errors in DV can
result from the application of this method to bolus injection
protocols. These errors are somewhat reduced with ratios of tissues
(BPratio values), as we have calculated here, yet can still be
significant. Additionally, Carson highlights the fact that this
method is sensitive to differences in plasma clearance between
subjects and patient populations. Therefore, while this method is
simpler to implement than kinetic modeling methods, it should
only be applied when a state of true equilibrium can be achieved,
such as with bolus plus constant infusion protocols.
Distribution volume and binding potential
The regional distributions of DV and BP values were consistent
with opioid receptor distributions known from post-mortem and
[11C]DPN studies (Jones et al., 1994; Pfeiffer et al., 1982). The
thalamus and basal ganglia contain high opioid receptor density,
followed by the frontal regions with decreasing receptor densities
in the cerebellum and minimal opioid receptors in the occipital
cortex. While it is assumed that [18F]FDPN and [11C]DPN have
similar kinetic and metabolite behaviors, there are subtle differences between the fate of the two compounds that manifest
themselves in differences in the outcome parameters (DV and
BP). For example, the IRF60 distribution of [18F]DPN has also
been previously shown to correspond to that of [11C]DPN,
although higher nonspecific binding with [18F]FDPN is expected
due to its higher lipophilicity (Wester et al., 2000). The increased
nonspecific binding may also impact the binding potential values
which were found to be lower than those determined from pulsechase experiments for [11C]DPN (Table 5) (Jones et al., 1994).
DV was consistent between the models evaluated here with
fairly low mean bias (<15% in applicable models and all regions
except the occipital) and strong correlations between the models
(R2 > 0.917; P < 0.0001). The occipital region was optimally fit by
a 2T model, while the 1T model and Inv_ Logan model appear to
underestimate the true value of the occipital region, leading to
increased bias in these regions when compared with the 2T model.
A broad range of DV values is important to adequately resolve
subtle differences in regional DV values. The observed range of
DV values was slightly reduced in the Inv_ Logan model compared
with that observed for the compartmental models. While the BFN
method exhibited a somewhat greater range in values compared
with the compartmental models, it was also found to contain the
most variability.
The consistency of DV values determined by the various
modeling approaches supports its use as an outcome measure
reflective of receptor density for [18F]FDPN studies. However, it
should be mentioned that the DV values calculated here will
contain a contribution from the nonspecific binding compartment.
Therefore, variability in the nonspecific compartment will be
reflected in the DV values and may be contributing to some of
the interindividual variability observed in this study.
While the compartmental modeling approach is supported for
VOI data with good SNR, alternative methods such as the Logan
model and basis function methods may be better suited for voxelby-voxel analyses. Data-driven methods, such as the basis function
and spectral analysis methods, have already been established as
valid approaches for [11C]DPN and the work herein supports such
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
an approach with [18F]FDPN as well. These methods may be better
choices than the Logan model since they avoid transforming the
data that propagates errors into the analysis.
With regards to BP, our results indicated that the 2T compartmental and reference region modeling methods were strongly
correlated (R2 values > 0.763; P < 0.0001). The BFN method was
not found to correlate as well with the other methods, which may
be reflective of the increased variability observed in the BFN’s
DV values and thus propagated to the BP values. The higher BP
values observed with the BFN method are most likely influenced
by the method’s lower DV estimates for the occipital region and
higher DV values across other regions. Regardless of the differences in BP values (Table 5), the normalized values (Table 6)
illustrate that all methods were able to generate similar distribution ratios between the various regions under the full 120-min
protocol.
It is encouraging that a strong correlation was observed between
BP estimates and the DV estimates on an individual subject basis,
which indicate that the values we are calculating are reflective of the
underlying binding potential, although their actual magnitude may
be biased due to the use of the occipital reference region. The
interindividual variability and the improved correlations of BP and
DV values on an individual basis also suggest that when evaluating
a study with statistical parametric mapping, it may be more
appropriate to use proportional scaling in the evaluation.
1531
researcher. Therefore, we performed a stability analysis of DV
and BP estimates for a protocol length of 60 min. In general, the
shortened protocol resulted in DV values that were reduced in
absolute value yet significantly correlated with the full protocol’s
results (P < 0.0001). As mentioned earlier, the BFN method
resulted in a consistent distribution of DV values under the long
and short protocol, suggesting its use in a protocol of a shorter
duration. Of the noninvasive methods, the SRTM resulted in very
consistent BP values between the long and short protocols. This
stability analysis showed promising results and we would encourage a future study for optimization of protocol length and other
experimental factors in the quantification of [18F]FDPN.
A secondary motivation for examining the 60-min data is
focused on developing an appropriate protocol for potential displacement studies, where a challenge is delivered at some point
during a single scan. The first requirement of such an analysis is to
accurately quantify the prechallenge binding of the tracer. Our data
suggest that accurate quantification of prechallenge binding is
feasible; however, since this was not the main motivation for this
manuscript, we would again suggest further studies to determine an
efficient and accurate experimental design for displacement studies, including exploring alternative dosing protocols (e.g. twoinjection protocols or bolus plus constant infusion), scan length
and placement of the challenge.
Study improvements
Reference region
There is recent evidence from a naloxone blocking study with
95% occupancy of available opiate receptors that the occipital
region cannot serve as an ideal receptor free reference region for
[11C]DPN (Asselin et al., 2003). Nonetheless, previous studies
have employed the use of a reference region when evaluating
DPN data (Lochmann et al., 2003; Piccini et al., 1997; Willoch et
al., 2004). The occipital region is commonly used as such a
reference region for DPN studies and although it may contain a
small amount of opiate receptors, specific binding in this region
is expected to be minimal. Thus, we also used the occipital
region as the reference region for the noninvasive modeling
methods. While we were unable to evaluate the bias introduced
by using the occipital cortex as a reference region, we presented a
comparison between the modeling methods and evaluated BP
against DV estimates.
The consistency of the normalized BP values between methods
suggests that in a longitudinal study where subjects are evaluated
more than once, the noninvasive methods and the use of BP may
be a viable analysis approach. However, due to the presence of
minimal yet nonnegligible specific binding in the occipital region,
any potential change in specific binding within the occipital region
between conditions should be investigated. If DV values within the
reference region are changing significantly between conditions,
this will influence BP estimates. In such a setting, it would be more
reasonable to use an invasive approach and DV values rather than
BP, assuming that the nonspecific binding remains relatively
constant across regions and subjects.
Shortened protocol
A shortened protocol that accurately quantifies [18F]FDPN
binding kinetics would be beneficial to both the subject and
This study has provided an initial examination of [18F]FDPN
binding kinetics in humans and has also revealed some areas for
potential methodological improvements. For example, the estimation of K1 and Vp may be improved by shortening the initial
imaging frames. Additionally, for practical reasons, the last metabolite sample was acquired at 90 min. It has been pointed out
elsewhere that errors in the metabolite estimation and hence the
metabolite corrected input function will have a direct effect on the
estimate of binding parameters (Lammertsma, 2002). Therefore, an
additional sample at 120 min may improve the accuracy of the final
results, although we have found large errors associated with
metabolite samples at late time points.
As shown in Eqs. (3) and (5), we have been estimating plasma
volume, rather than blood volume. Ideally, the whole blood
measurement should be acquired and used in the modeling process
(Lammertsma, 2002). However, in this study, whole blood measurements were not acquired; therefore, the whole plasma curve
(without metabolite correction) was used to estimate a plasma
volume term. Thus, to improve the full interpretation of future
study results, we would also suggest acquiring whole blood values
for the estimation of blood volume.
Summary
This work shows that DV values estimated from compartmental, basis function and invasive Logan modeling approaches are
robustly determined by each of these methods for [18F]FDPN. The
fact that the invasive Logan and basis function methods are
providing similar results to those of the compartmental analyses
is encouraging for their application to parametric image generation, although the level of noise in the data should be considered
when applying the invasive Logan model parametrically. The
binding potential values correlated well with one another although
more variability was observed in these values compared with the
1532
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
DV values. The BP values were also significantly correlated with
the DV values estimated from the 2T model, illustrating consistency between DV and BP measures of [18F]FDPN binding. The
noninvasive methods resulted in BP values consistent with those
of the invasive methods, and additionally showed less interindividual variability. The results also suggest that a shorter protocol
may be feasible to assess [18F]FDPN kinetics following a bolus
injection, although the appropriate analysis method should be
considered.
In conclusion, all models evaluated in this study were able to
quantify [18F]FDPN kinetics. The distribution volume appears to
be a more consistent parameter for the quantification of receptor
density for [18F]DPN and is not influenced by the choice of
reference region. However, the noninvasive methods and binding
potential values may be of value in clinical research when large
numbers of patients are examined and a manageable study protocol
(without arterial sampling) is necessary.
Acknowledgments
We would like to acknowledge the work of our colleagues
Brigitte Dzewas and Choletta Kruschke for their excellent
technical assistance in data acquisition. This work was supported
by grants from the KKF (8764153), the Deutsche Forschungsgesellschaft (SFB 391, TP C9), the German Network for Neuropathic
Pain by BMBF and the Norwegian Research Council Project
number 151445/432.
References
Akaike, H., 1974. A new look at the statistical model identification. IEEE
Trans. Autom. Control 19, 716 – 723.
Alpert, N.M., Badgaiyan, R.D., Livni, E., Fischman, A.J., 2003. A novel
method for noninvasive detection of neuromodulatory changes in specific neurotransmitter systems. NeuroImage 19 (3), 1049 – 1060 (Jul.).
Asselin, M.C., Hammers, A., Sethi, F.N., Koepp, M.J., Grasby, P.M.,
Cunningham, V.J., 2003. Definition of a reference region for PET/
[11C]diprenorphine studies. J. Cereb. Blood Flow Metab. 23 (S1),
679 (Jun.).
Carson, R.E., Channing, M.A., Blasberg, R.G., Dunn, B.B., Cohen, R.M.,
Rice, K.C., Herscovitch, P., 1993. Comparison of bolus and infusion
methods for receptor quantitation: application to [18F]cyclofoxy and
positron emission tomography. J. Cereb. Blood Flow Metab. 13 (1),
24 – 42 (Jan.).
Duncan, J.S., 1999. Positron emission tomography receptor studies in epilepsy. Rev. Neurol. (Paris) 155 (6 – 7), 482 – 488 (Review, Jul.).
Endres, C.J., Bencherif, B., Hilton, J., Madar, I., Frost, J.J., 2003. Quantification of brain mu-opioid receptors with [11C]carfentanil: referencetissue methods. Nucl. Med. Biol. 30 (2), 177 – 186 (Feb.).
Frost, J.J., Douglass, K.H., Mayberg, H.S., Dannals, R.F., Links, J.M.,
Wilson, A.A., Ravert, H.T., Crozier, W.C., Wagner Jr., H.N., 1989.
Multicompartmental analysis of [11C]-carfentanil binding to opiate
receptors in humans measured by positron emission tomography.
J. Cereb. Blood Flow Metab. 9 (3), 398 – 409 (Jun.).
Gunn, R.N., Gunn, S.R., Cunningham, V.J., 2001. Positron emission tomography compartmental models. J. Cereb. Blood Flow Metab. 21 (6),
635 – 652 (Jun.).
Gunn, R.N., Gunn, S.R., Turkheimer, F.E., Aston, J.A., Cunningham, V.J.,
2002. Positron emission tomography compartmental models: a basis
pursuit strategy for kinetic modeling. J. Cereb. Blood Flow Metab. 22
(12), 1425 – 1439 (Dec.).
Jones, A.K., Liyi, Q., Cunningham, V.V., Brown, D.W., Ha-Kawa, S.,
Fujiwara, T., Friston, K.F., Silva, S., Luthra, S.K., Jones, T., 1991.
Endogenous opiate response to pain in rheumatoid arthritis and cortical and subcortical response to pain in normal volunteers using
positron emission tomography. Int. J. Clin. Pharmacol. Res. 11 (6),
261 – 266.
Jones, A.K., Cunningham, V.J., Ha-Kawa, S.K., Fujiwara, T., Liyii, Q.,
Luthra, S.K., Ashburner, J., Osman, S., Jones, T., 1994. Quantitation
of [11C]diprenorphine cerebral kinetics in man acquired by PET using
presaturation, pulse-chase and tracer-only protocols. J. Neurosci. Methods 51 (2), 123 – 134 (Mar.).
Lammertsma, A.A., 2002. Radioligand studies: imaging and quantitative
analysis. Eur. Neuropsychopharmacol. 12 (6), 513 – 516 (Dec.).
Lammertsma, A.A., Hume, S.P., 1996. Simplified reference tissue model
for PET receptor studies. NeuroImage 4 (3 Pt 1), 153 – 158 (Dec.).
Laruelle, M., Slifstein, M., Huang, Y., 2002. Positron emission tomography: imaging and quantification of neurotransporter availability. Methods 27 (3), 287 – 299 (Jul.).
Lochmann, M., Buchholz, H.G., Siessmeier, T., Schreckenberger, M.,
Roesch, F., Bartenstein, P., 2003. Comparison of different quantification
methods for calculating Binding Potential (BP) of the new unselective
opiate-receptor ligand [18F]Fluor-Ethyl-Diprenorphine. J. Cereb. Blood
Flow Metab. 23 (S1), 669 (Jun.).
Logan, J., 2000. Graphical analysis of PET data applied to reversible and
irreversible tracers. Nucl. Med. Biol. 27 (7), 661 – 670 (Oct.).
Mayberg, H.S., Sadzot, B., Meltzer, C.C., Fisher, R.S., Lesser, R.P., Dannals, R.F., Lever, J.R., Wilson, A.A., Ravert, H.T., Wagner Jr., H.N.,
Bryan, N., Cromwell, C.C., Frost, J.J., 1991. Quantification of mu and
non-mu opiate receptors in temporal lobe epilepsy using positron emission tomography. Ann. Neurol. 30 (1), 3 – 11 (Jul.).
Meyer, J.H., Ichise, M., 2001. Modeling of receptor ligand data in PET and
SPECT imaging: a review of major approaches. J. Neuroimaging 11 (1),
30 – 39 (Jan.).
Mintun, M.A., Raichle, M.E., Kilbourn, M.R., Wooten, G.F., Welch, M.J.,
1984. A quantitative model for the in vivo assessment of drug binding
sites with positron emission tomography. Ann. Neurol. 15 (3), 217 – 227
(Mar.).
Pappata, S., Dehaene, S., Poline, J.B., Gregoire, M.C., Jobert, A., Delforge,
J., Frouin, V., Bottlaender, M., Dolle, F., Di Giamberardino, L., Syrota,
A., 2002. In vivo detection of striatal dopamine release during reward: a
PET study with [(11)C]raclopride and a single dynamic scan approach.
NeuroImage 16 (4), 1015 – 1027 (Aug.).
Pfeiffer, A., Pasi, A., Mehraein, P., Herz, A., 1982. Opiate receptor binding
sites in human brain. Brain Res. 248 (1), 87 – 96 (Sep. 23).
Piccini, P., Weeks, R.A., Brooks, D.J., 1997. Alterations in opioid receptor
binding in Parkinson’s Disease patients with levodopa-induced dyskinesias. Ann. Neurol. 42, 720 – 726.
Sadzot, B., Mayberg, H.S., Frost, J.J., 1990. Imaging opiate receptors in
the human brain with positron emission tomography. Potential applications for drug addiction research. Acta Psychiatr. Belg. 90 (1), 9 – 19
(Jan – Feb.).
Slifstein, M., Laruelle, M., 2000. Effects of statistical noise on graphic analysis of PET neuroreceptor studies. J. Nucl. Med. 41 (12), 2083 – 2088
(Dec.).
Slifstein, M., Laruelle, M., 2001. Models and methods for derivation of in
vivo neuroreceptor parameters with PET and SPECT reversible radiotracers. Nucl. Med. Biol. 28 (5), 595 – 608 (Jul.).
Sprenger, T., Valet, M., Boecker, H., Henriksen, G., Willoch, F., Wester, H.,
Wagner, K., Schwaiger, M., Conrad, B., Tolle, T.R., 2003. Heat Pain
triggers [18F]-diprenorphine displacement in the limbic system. J.
Cereb. Blood Flow Metab. 23 (S1), 719 (Jun.).
Weeks, R.A., Cunningham, V.J., Piccini, P., Waters, S., Harding, A.E.,
Brooks, D.J., 1997. 11C-diprenorphine binding in Huntington’s disease:
a comparison of region of interest analysis with statistical parametric
mapping. J. Cereb. Blood Flow Metab. 17 (9), 943 – 949 (Sep.).
Wester, H.J., Willoch, F., Tolle, T.R., Munz, F., Herz, M., Oye, I., Schadrack, J., Schwaiger, M., Bartenstein, P., 2000. 6-O-(2-[18F]fluo-
M.E. Spilker et al. / NeuroImage 22 (2004) 1523–1533
roethyl)-6-O-desmethyldiprenorphine ([18F]DPN): synthesis, biologic
evaluation, and comparison with [11C]DPN in humans. J. Nucl. Med.
41 (7), 1279 – 1286 (Jul.).
Willoch, F., Tölle, T.R., Wester, H.J., Munz, F., Petzold, A., Schwaiger,
M., Conrad, B., Bartenstein, P., 1999. Central pain after pontine infarction is associated with changes in opioid receptor binding: a PET study
1533
with 11C-diprenorphine. AJNR Am. J. Neuroradiol. 20 (4), 686 – 690
(Apr.).
Willoch, F., Schindler, F., Wester, H.J., Empl, M., Straube, A., Schwaiger,
M., Conrad, B., Tölle, T.R., 2004. Central poststroke pain and reduced
opioid receptor binding within pain processing circuitries: a 11C-diprenorphine PET study. Pain. 108, 213 – 220 (Apr.).
![Quantification of [ F]diprenorphine kinetics in the human brain with](http://s3.studylib.net/store/data/008858163_1-72f2d0d46bf0d160df98a688f97feda5-768x994.png)