Nursing Care Plan Development - Regan Preston Professional
advertisement

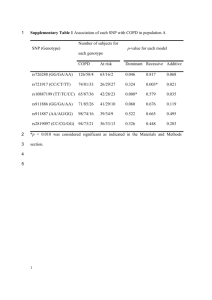
Nursing Care Plan Development Chronic illness - emphysema 9/23/2011 Unit: NURS 8822 Unit co-ordinator: Assistant Professor Olivia Hill Student: Regan Preston Student No: 20825201 Table of Contents Emphysema – a Chronic Obstructive Pulmonary Disease ................................................................. 3 Epidemiology: ........................................................................................................................................ 3 Aetiology: ................................................................................................................................................ 4 Pathophysiology: ................................................................................................................................... 5 Clinical manifestations .......................................................................................................................... 7 Risk Factors ........................................................................................................................................... 8 Diagnosis of emphysema ..................................................................................................................... 9 Problem Identification ............................................................................................................................. 11 Care Planning .......................................................................................................................................... 14 Collaborative care ................................................................................................................................... 23 Conclusion ............................................................................................................................................... 24 References ............................................................................................................................................... 25 2 Emphysema – a Chronic Obstructive Pulmonary Disease Chronic Obstructive Pulmonary Disease (COPD) is a multi-component respiratory disease that is progressive, with no known cure.1-3 COPD is defined by the Global Initiative for Chronic Obstructive Lung Disease (GOLD)4 as a preventable and treatable disease with significant extra pulmonary effects that may contribute to the severity in the individual patient.4, 5 A mixture of small airway disease and parenchymal destruction are characteristic of emphysema, and conditions vary amongst individuals.4 6 COPD has a very variable history and diseased patients do not follow typical symptomatic patterns, and trends. It is a progressive disease and limiting exposure to harmful agents will reduce progression of the disease, however once COPD has developed, only treatment can be given to reduce symptoms and exacerbations, and improve overall quality of patients life.4 Epidemiology: COPD has a huge burden on our society and health care system, and according to the World Health Organization (WHO) World Health Report 2000, respiratory diseases account for 17.4% of all deaths and 13.3% of all Disability Adjusted Life Years (DALYs).2, 7, 8 COPD is projected by 2020 to become the fifth largest in burden of disease, and the third leading cause of death worldwide.2 9, 10 The Burden of Obstructive Lung Disease (BOLD) study showed that the worldwide prevalence of COPD was approxiatemelty10%.11 This figure varied by geographic 3 location and by sex. Prevalence among men was 11.8% and among women was 8.5%.11 The differences in sex can be explained by the prevalence of smoking. Historically incorrect and inaccurate definitions of COPD have made difficult to quantify the factors such as prevalence, morbidity and mortality of COPD and emphysema.4 Under recognition and under diagnosis of COPD are responsible for large variances in underreporting.4 In Australia, COPD is the fourth major cause of deaths in males, and sixth major cause in females. It is reported that over 80% of the COPD sufferers are experienced over the age of 45 years.8 In 2003, the Australian Burden of Disease and Injury Study estimated almost 400,000 people with COPD in Australia, with 20,000 new cases every year.8 In Australia, The Australian Institute of Health and Welfare (AIHW) 2008 reported COPD as the leading cause of death 4%, around 4900 deaths per annum.12 In 2000, COPD had accounted for 4% of all make deaths and 3% of female deaths in Western Australia.12 History has shown that COPD was more prevalent among men. This was attributed to the difference in smoking rates in men and women. However the increase in smoking among women, the difference has declined.12 Furthermore COPD is also associated with socio-economic status, and high rates of COPD exist in aboriginal populations.12 This was due to extremely high rates of smoking within these communities.8 Aetiology: COPD is most often caused by smoking. Most people with COPD are long-term smokers, and evidence shows that smoking cigarettes increases the risk of getting COPD.4, 8 13 Overwhelming evidence that lung destruction resulting in emphysema is largely due to enzymatic action on the pulmonary connective tissues such as elastin. These enzymes are possibly derived from neutrophil polymorphonulear leucocytes and alveolar macrophages.4 Some research has shown release of these enzymes related to cigarette smoking. Emphysema can be seen as very closely related to the fact that individuals smoke, and result of smoking habit. A mixture of small airway disease and parenchymal destruction are characteristic of emphysema, and conditions vary amongst individualls.4 Emphysema damages the structure of the alveoli causing the walls to break down. This means the alveoli are no longer able to hold the bronchioles open, making it hard for the lungs to expel air. Emphysema makes the lungs resemble an old used sponge with large holes that lack elastic recoil.14, 15 4 Pathophysiology: Emphysema is defined as an enlargement and inflammation of air pathways and coupled with destruction of alveolar walls and septa of lung tissue.16, 17 There is parenchymal destruction typical of emphysema and develop from long time smokers and exposure to noxious particles or gas substances.2, 16, 18 This causes limitations and reduction in elastic recoil required in correct lung function.16 This loss of lung natural elasticity results in lung becoming permanently inflated.18 Condition is caused by destruction of the pulmonary connective tissue namely elastin and collagen.14 Gas exchange abnormalities are characteristic and result in hypercarnia and hypoxemia.4 The severity of emphysema relates to the ventilation –perfusion (V/Q) imbalance, and disease worsens as this imbalance gets greater. This imbalance and loss of elastic recoil in alveoli, depicted in figure 1, leads to carbon dioxide retention and hypercapnia state. Figure 1: The major mechanism of airflow limitation is loss of elastic recoil.19 19 5 Figure 2: The pathophysiology of emphysema.20 6 Figure 3: The effects of emphysema on the gas exchange units. A Normal lung with many small alveoli. B Lung tissue affected by emphysema. Notice that the alveoli have merged into larger air spaces, reducing the surface area for gas exchange.21 21 Clinical manifestations The clinical manifestations of emphysema are tabulated in table 1. Typically dyspnoea, productive cough, history of smoking and barrel chest are common clinical manifestations of emphysema. Table 1: Clinical manifestations of emphysema: 15 VARIABLES EMPHYSEMA Age (years) 50-75 Infections Occasional Dyspnoea Severe, early in course Productive cough Late in course with infection Wheezing Common History of smoking Common Prolonged expiration Always present Cyanosis Late in course Chronic hypoventilation Late in course Chest x-ray findings Hyperinflation General appearance “pink puffer” Barrel chest Classic 7 A classical clinical manifestation is the barrel chest of an emphysema sufferer. This is well depicted in Figure 4. 22 22 Figure 4: Lateral CXR of a person with emphysema. Not the barrow chest and flap diaphragm Risk Factors Cigarette smoking is the most common risk factor for COPD and emphysema.4, 23 Identification of risk factors is an important step in determining strategies for prevention and treatment of these chronic respiratory diseases. Risk factors do interact and interlink with each other and with the current overpopulation being experienced around the world, factors like poverty, socioeconomic status, level of nutrition and level of education are all becoming major determinants in COPD.4 Figure 3-1 lists common risk factors associated with emphysema and COPD6. 6 8 Diagnosis of emphysema Key indicator in considering a diagnosis for emphysema would be the presence of dyspnoea, chronic cough, sputum production, and health history of smoking or smoke related risk factors.6 Diagnosis of emphysema is achieved through physical assessment, spirometry tests, arterial blood gas assessment, chest x-ray, electro cardio graphs (ECG) and microbial testing.2, 16 Although physical examination is an important clinical diagnostic tool, in COPD it is used conjunctively with other diagnostic assessments such as spirometry, spirometry being the gold standard in assessment and diagnosis of COPD.4 A physical assessment is made up of an inspection, palpation, percussion, auscultation of respiratory region. Table 3 compares the assessment process and diagnostic difference between and normal and a diseased lung. Physical Assessment Inspection Normal Lung Anteroposterior transverse diameter, RR 10-18, regular, no cyanosis or pallor14 Palpation Symmetric chest expansion. Tactile fremitus present and equally bi laterally, diminishes towards periphery. No masses, lumps, tenderness.14 Resonant. Diaphragmatic excursion 3-5 cm14 Vesicular over peripheral fields. Broncho vesicular parasternally (ant) and between scapula (post) None Percussion Auscultation Adventitious Sounds Emphysema Increased anteroposterior diameter. Barrel chest. Use accessory muscles to breathe. Tripod position. Shortness of breath. Tachypnea.14 Decreased tactile fremitis and chest expansion. Hyper resonant. Decreased diaphragmatic excursion.14 Decreased breath sounds. Prolonged expiration. Muffled heart sounds from over distention of lungs.14 Usually None, occasionally, wheeze. Spirometry is a simple and painless test which measures the capacity of your lungs.24 9 24 Emphysema can be diagnosed by using the gold standard spirometric classification of stages of COPD, and GOLD guidelines.2, 17, 25 The presence of a post bronchodilator FEV1/FVC<0.70 and FEV1 <80% predicted confirms the presence of airflow limitation that is no fully reversible.4 Table 2: Spirometric classifications of COPD26 Arterial blood gas measurement is performed on patients with FEV<50%. Development of respiratory failure is indicated by a PaO2<6.7kPa (60mmHg) with or without PaCO2>6.7 kPa (50mmHg) in arterial blood gas measurements made while breathing air at sea level.4, 23 Low 10 pH, High PaCO2, normal or high normal bicarbonate, are indicators of lung disease like COPD. Chest X-ray can determine densities in lung fields that are produced by fluids, tumors and other pathological conditions and also used in excluding alternative diagnoses and establishing the presence of other co morbidities such as cardiac failure.23 Chest x-rays on CPOD patients show signs of hyperinflation, flattened diaphragm, and increase in the volume of the retrosternal air space. In addition chest CT scans also useful in showing the actual distribution of the emphysema, for patients that may undergo lung volume reduction surgery. Genetic diagnostic screen testing can also be undertaken, checking for Alpha-1 antitrypsin deficiency. A serum concentration of below 15-20% of the normal value is a predictive sign of alpha-1 antitrypsin deficiency and COPD.6 Presence of purulent sputum during exacerbation of symptoms is sufficient indication for starting empirical antibiotic treatment, with common COPD pathogens being namely Streptococcus pneumonia, Hemophilus influenzae and Moraxella catarrahalis.6 Problem Identification COPD is a chronic and disabling respiratory disease, studies cited by Blinderman et al 20099 have shown that the most prevalent symptoms experienced by COPD sufferers were dyspnoea (94%), fatigue (71%), coughing (56%) and anxiety (51%).9 Other symptoms with high prevalence were drowsiness, nervousness and wheezing.9 Studies by Silbeck et al 1998 as cited by Wilson27 showed breathlessness (95%), pain (68%), fatigue (68%), sleeping difficulty (55%) and thirst were common clinical manifestations.27 Edmonds et al 2001 as cited by Wilson, collect evidence to show that breathlessness was experienced more often, and became extremely distress by this excacerbation.27 Evidence shows dyspnoea as the main standout symptom of COPD patients who seek medical attention, and major cause of disability and anxiety associated with the disease.4 Studies conducted by a British team Elkington 2004, as cited by Wilson27, found that breathless was the main symptom experienced by COPD sufferers, and anxiety and depression were common.27 Feelings of anxiety and depression are also common in patients with chronic COPD and emphysema, mainly dyspnoea inducing factor of fear and anxiety.28 The increase in breathlessness will result in the increase in the fear of exercise and this in itself becoming a major reason for avoidance of physical activities.29 Breathlessness could trigger 11 panic attacks, which in turn exacerbate the symptom of dyspnoea. This avoidance is shown to cause further disability through physical deconditioning and hence avoidance in social and physical activities.18 Kunik et al 2005 as cited by Addy29, showed that a very high percentage of COPD suffers would develop negative beliefs about self image as the disease progressed.29 The onset of increased anxiety and depression would develop and become major comorbid symptom. Feelings of anxiety and depression are common place in COPD sufferers due to the impact of the increase in dyspnoea, altered sleep patterns and the feelings of loss and grief associated with disability of COPD.28, 29 The element of fear is aroused when breathlessness is experienced in large majority of sufferers. The psychosocial problems experienced by emphysema patients range from depression, loneliness, helplessness and hopelessness.30, 31 Intense loneliness can be brought about by lack of self worth feelings and overall lack in personal confidence. Loneliness has been associated with depression.30 Psychological states such as depression and anxiety in COPD have important repercussions.32 Physical deterioration, becoming further housebound and reflection on what was once a previously active body, produce negative depressive emotions.1 Patients become withdrawn, lonely, isolated, anxious and in worse cases, lose the ability to show or display any emotion such as anger, or even sadness.18, 32 Without a clinical intervention from mental health specialists, symptoms like fatigue, weight loss and ability to cope and tolerate symptoms of emphysema will not alleviated.1 Attitudes such us wanting to “give up” have also been observed in chronic suffers, due to the fact that not much more could be done with respect to a cure for disease.1, 29 Sleep pattern alterations and difficulties due to COPD symptoms further enhanced feelings of anxiety and depression.18 Sleep anxiety is also prevalent in oxygen therapy patients with fear of one dying in ones sleep.25 Angel et al 2007 as cited by Rabe2 study showed that a serious element of depression in COPD patients was there lack of desire and willingness to participate in rehabilitation programs for the disease. These programs have been proven to increase patients self esteem, decrease fear of dyspnoea and physical activity and overall depression.2 Therefore, from the above evidence reviewed, the following patient problem statements have been prioritized: 12 Patient problem statements: 1. Ineffective airway clearance related to bronchoconstriction, increased mucous production, ineffective cough and sputum expectoration, manifested by acute episodes of dyspnoea and breathlessness. 2. Impaired gas exchange related to the imbalance and loss of elastic recoil in alveoli, secondary to parenchymal lung tissue destruction, manifested by pursed lip breathing and inability to speak. 3. Fatigue and activity intolerance related to imbalance between oxygen supply and demand, manifested by verbalizations of lack of energy, lethargy and increased need for rest. 4. Anxiety related to the fear of episodes of breathlessness, threat of death, and hopelessness to a chronic illness, manifested by lack of self care and depressive mood states. 13