What is a Blood Gas?
advertisement

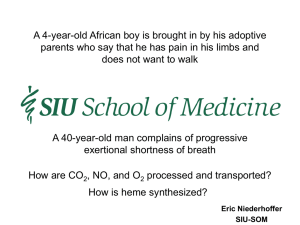
Publication of the Association of Polysomnographic Technologists • Winter 2006 • www.aptweb.org What is a Blood Gas? BY WILLIAM W. ECKHARDT, RPSGT, CRT, A2Zzz MAGAZINE ASSOCIATE EDITOR his article is not about the invasive procedure of obtaining a “blood gas.” Rather, it is about gas molecules and their movement from outside the body to the cells within the body. Arterial blood gases (ABGs), commonly called blood gases, are introduced to the blood via the thoracic pump driving air in and out of the lungs (convection). In the lung, the air (a mixture of gases) exchanges gases with the blood (diffusion). This is done through the alveolar capillary membrane. Whichever side of the alveolar capillary membrane (lung or blood) has the greater concentration of a particular gas, the higher concentration will diffuse to the side with the lesser concentration trying to equilibrate gas pressures on both sides of the alveolar capillary membrane. the other). Eventually the movements from greater to lesser stop as both sides are equal called dynamic equilibrium (we are in a dynamic system where there is always new blood to reach equilibrium, so this process never really stops). When a gas meets a liquid there is also an exchange of molecules as long as the gas is soluble in the liquid such as O2 in blood, the molecules then become dissolved unless they combine chemically with the liquid. The air or earth’s atmosphere is made up of different gas molecules (we like oxygen quite a bit) and they are all important to the big picture. These molecules have mass and are attracted to the earth by its gravitational force. This pressure of course is greatest at the earth’s surface (more molecules pushing down from above). This is atmospheric pressure. Water vapor or humidity is a gas and acts like the other gases in the air and exerts a pressure. Once the air reaches the lungs, it is 100% humidified often exerting a greater partial pressure than in the atmosphere. The partial pressure of oxygen in arterial blood when breathing ambient air for healthy individuals is 80-100 mm Hg, but when supplemental oxygen is given, it can be as high as 600 mm Hg. See Sidebar 1 for calculation of partial pressure of gases ambient and alveolar at standard conditions (BTPS — Barometric pressure the body is exposed to 750 mm Hg or one atmosphere (atm), body temperature at 37° C and water vapor at maximum for 37° C being 47 mmHg). Henry’s Law — The amount of gas that can be dissolved in a liquid is proportional to the partial pressure of the gas to which the liquid is exposed. T Gas Percentage Within Mixture of Gases Partial Pressure Air at Sea Level (760 mm Hg) Oxygen 20.9% 159 Nitrogen 79% 600 Inerts 1% 1 Alveolar Gas at Sea Level (760 mm Hg) Oxygen 13.3% 101 Nitrogen 75.2% 572 Carbon Dioxide 5.3% 40 Water Vapor 6.2 47 760 mm Hg (standard pressure of 1 atm) x .20.9 (percentage of oxygen in the atmosphere expressed as a decimal) = 159 William W. Eckhardt Why do we care about diffusion? O2 and CO2 are dissolved in the blood. O2 comes from the air we breathe and CO2 comes from metabolism within the cells of our bodies (small amounts are of course in the air we breathe). So, these gases are in differing quantities and states e.g. dissolved or combined chemically when in the lungs, in pulmonary circulation or within cells. Within our blood we have red blood cells. Red blood cells contain hemoglobin, lots of hemoglobin (280 million molecules). Each hemoglobin molecule contains 4 atoms of iron and can have a reversible bond with O2. The fact that the bond is reversible helps when transporting O2 from one area to another. So, if this “affinity” of hemoglobin for O2 changes it will gain or lose its hold on the O2. This is good as blood needs to pick up O2 in the lungs (we want the affinity to be high). In the cells the reverse is true, we want the hemoglobin to release the O2 to the cell (we want a lower affinity). There are factors that affect this affinity e.g. temperature, carbon dioxide, and carbon monoxide (CO). Carbon dioxide is also carried in direct chemical combination with hemoglobin called carbamino-CO2. It also is transported in the form of carbonic acid via the bicarbonate ion mechanism. O2 and CO2 also travel dissolved in the plasma, albeit in small amounts. The measurement of blood gases are derived from the partial pressure of the dissolved gases. Bohr Effect Dalton’s Law — In a mixture of gases, the total pressure is equal to the sum of the partial pressures of the separate components. There is a relationship between O2 and CO2. The addition of CO2 to the blood enhances O2 release (decreases the affinity). If we think about this — it is good. When oxygenated blood reaches the cell, the cell has a large amount of CO2 compared to the blood. The blood will pickup the CO2 (higher partial pressure so it wants to diffuse to the side with the lesser partial pressure) the affinity therefore decreases and O2 is released to the cell. Why Do Gases Diffuse? Haldane Effect Diffusion is the movement of gas molecules from high concentration to a lower concentration. This can take place in the atmosphere and across cell membranes. Each gas works independently. If Carbon Dioxide (CO2) and Oxygen (O2) are both moving across the alveolar capillary membrane they will likely move at different rates and amounts due to a difference in their respective gradients (pressure differences from one side to The addition of O2 to the blood enhances CO2 release. This too is good! When blood reaches the lung it will pickup O2 (higher partial pressure of O2 in the lung causes the O2 to diffuse across the alveolar capillary membrane). This addition of O2 to the blood causes enhanced CO2 release at a time conducive to its elimination. Sidebar 1 Gas Laws 14 ª Publication of the Association of Polysomnographic Technologists • Winter 2006 • www.aptweb.org Blood gas measurements are generally done after performing an arterial puncture and using a blood gas analyzer. This analyzer works by measuring the dissolved form of the gases partial pressure. The blood gas measurement is seldom done in the sleep lab for various practical reasons. What we do measure in the sleep lab is the O2 saturation of the blood and sometimes the end tidal CO2 of expired gases. These are noninvasive methods and the values can change over time as the patients status changes, even on a breath by breath basis. The Oxy-hemoglobin dissociation curve gives us a representation of oxygen partial pressure in relation to the oxyhemoglobin (percent hemoglobin saturated with oxygen) at differing partial pressures. At the alveolar capillary membrane the amount of oxygen that can be dissolved in the blood is proportional to the partial pressure of the oxygen to which the blood is exposed (Henry’s Law). Most the oxygen attaches to hemoglobin and once the pressure gradient equilibrates the hemoglobin is maximally saturated for that blood oxygen tension. It is possible to increase the saturation by increasing the oxygen tension (increased inspired oxygen concentration or FiO2). The oxy-hemoglobin dissociation curve is a sigmoid shape between 0 and 100 mm Hg. This shape shows that hemoglobin’s affinity for O2 progressively increases as more and more molecules of O2 combine with the hemoglobin. At the beginning of the curve O2 saturation increases significantly as the partial pressure of O2 increases. At the flatter part of the curve only slight increases in saturation are seen with increases in partial pressure. The curve can shift, right or left, showing the relationship certain factors have on hemoglobin’s affinity for oxygen. A shift to the right presents with a decreased oxygen affinity. For a given partial pressure of oxygen the oxygen content is decreased. Oxygen content being the sum of the oxygen dissolved in the blood and that attached to hemoglobin. A left shift presents with a increased oxygen affinity. For a given partial pressure of oxygen the oxygen content is increased. So, this affects the availability of the oxygen to the tissues. At higher affinity there is less oxygen available for a given partial pressure. Some factors that affect availability or shifts are carbon dioxide tension (Bohr Effect), blood pH, and temperature. An increase in these causes decreased oxygen affinity. Blood needs to pick up O2 in the lungs (we want the affinity to be high) the decreased CO2 (carbon dioxide partial pressure is higher in the blood and diffuses across the alveolar capillary membrane) increases the affinity for oxygen and the oxygen content increases. In the cells the reverse is true, we want the hemoglobin to release the O2 to the cell (we want a lower affinity) and the tissue metabolism produces carbon dioxide resulting in a slight shift to the right. Fig. 1 Oxyhemoglobin Dissociation Curve — A left shift means that smaller increases in the partial pressure of O2 correspond to higher hemoglobin saturations. A right shift would require (reduced affinity) greater increases in partial pressure of O2 to maintain saturation. Left shifts are good for the uptake of O2 (Haldane effect — seen as the blood enters the lungs. The addition of O2 to the blood enhances CO2 release) and right shifts are good for the release of O2 to the tissues (Bohr Effect — the addition of CO2 to the blood enhances O2 release from hemoglobin). So how do we measure the oxygen level? You know the answer, with an oximeter. The oximeter uses Spectrophotometry to determine the amounts of oxyhemoglobin and deoxygenated hemoglobin. This method shines light of two different wavelengths through the sensor site. These are absorbed differently by the hemoglobin depending on its state with the oxygen molecules. The oximeter calculates these into a saturation value which is given as a percentage of saturation. Knowing this value you can look at the curve and determine where on the curve it lays, giving you the partial pressure. The difference between the value of an oximeter and that of a blood gas is the oximeter gives us arterial oxyhemoglobin saturation whereas the blood gas gives us the partial pressure of oxygen in the arterial blood. The blood gas also gives values of other gases/parameters that the Figure 1 oximeter can not but the patient’s oxygenation status can be evaluated with either the blood gas (PaO2) or the saturation (SpO2). There are of course technical and physiological factors that can influence the accuracy of either test. Blood oxygen measurements need to be evaluated relative to the patient status, history, and other clinical tests. Another important aspect of blood gas partial pressure is in the regulation of breathing. The drive to breathe is controlled by The Respiratory Control System that uses the partial pressure of O2 and CO2 for the feedback in which to modify system controls. Sensors or chemoreceptors with in the medulla in the brainstem (central chemoreceptors) and the carotid and aortic bodies (peripheral chemoreceptors) send afferent input back to the controllers (negative feedback). So, the controller takes input and this precipitates an action which affects the “plant” or controlled system (here the lungs) which in turn changes the system output. The feedback is sent to the controller utilizing output from these receptors that react to partial pressures of the gases O2 and CO2. This is a negative feedback system largely run from values of the blood gases. Why Do I Need To Know All This? Because the oxygen saturation of our patient’s blood is one of the most important parameters we measure in the sleep lab. When measuring something you should know where that value comes from. A patient may need support to enhance their oxygenation. This may be done by enhancing ventilation such as with PAP therapy or increasing the patients inspired oxygen concentration (FiO2). Please refer to the APT CORE COMPETENCY: Monitoring Pulse Oximetry in Polysomnographic Technology and APT CORE COMPETENCY: Supplemental Low Flow Oxygen Titration in Polysomnographic Technology. This is an aspect of care in which polysomnographic technologists need to gain competency, in order to provide the best possible patient care. # References Clinical Application of Blood Gases, Barry A. Shapiro, Ronald A. Harrison, John R. Walton, Third Edition, Year Book Medical Publishers Mosby’s Respiratory Care Equipment, J.M. Cairo, Susan P. Pilbeam, Seventh Edition, Mosby Ventilatory Control and the Thoracic Pump, William W. Eckhardt, A2Zzz Magazine, Volume 14 Number 1 About the Author Will Eckhardt, RPSGT, CRT is a member of the APT Board of Directors, and serves the APT Board Liaison for the APT Standards and Guidelines Committee. He is a board member of the New England Polysomnographic Society (NEPS) and is NEPS Education Committee Chair. His full time position is with Sleep HealthCenters where he is the Director of Education. Eckhardt also is a faculty member at Northern Essex Community College where he teaches in the polysomnography program and is a member of the advisory board. He is a member of the A2Zzz Magazine Editorial board and a recipient of the APT Dr. Allen DeVilbiss Literary Award in 2004. He is also a member of the American Academy of Sleep Medicine Committee on Polysomnographic Technologists Issues. 15