Lewis-Manning – Lymphoedema Awareness Day 2015
advertisement
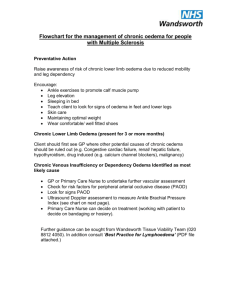
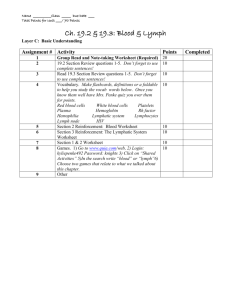
Dawn Heal RN, MLD/CDT MLD Therapist/Lymphoedema Nurse Specialist The Hampshire Lymphoedema Clinic Aims Anatomy & Physiology Signs & Symptoms Preventative Measures Maintenance What is lymphoedema ? Lymphoedema is a chronic swelling/chronic oedema anywhere in the body but usually affecting an arm or leg. It occurs when the lymphatic system is overloaded. It may begin as a feeling of heaviness and aching in the affected limb. Mild swelling will initially reduce overnight and may also be exacerbated by heavy lifting or certain types of exercise. Left untreated the swelling will become worse, firmer and more rigid, the skin hard and thickened. The limb becomes dry, heavy and uncomfortable and at risk of cellulitis Role of Lymphatic System • To gather fluid from tissue spaces and return it to circulation • To gather, transport and absorb protein and lymph fluid (containing: water, hormones, bacteria, enzymes, fats and cell waste products) and return it to the circulatory system • To act as a defence mechanism against bacteria and mutant cells Blood and Lymph Circulatory Systems • The lymphatic system acts as a one way drainage system parallel to the venous system • The main differences between the blood circulatory system and the lymphatic system are: – the lymphatic system only forms a semicircle – has no pump for moving the lymph • The Lymph transport is maintained by several alternate transport mechanisms Normal Flow Initial Lymphatics - Superficial Blind ended tubes Single layer of epithelium No muscle – passive Collapsed when empty Attached to surrounding structures by anchoring filaments Opens and takes in fluid in response to movement of surrounding tissues No flow when limb at rest Lymphatic System Components Superficial vessels – blind end tubes Pre-collector vessels Collector vessels Lymph nodes Right lymphatic duct Left lymphatic duct Cysterna chyli Anchoring Filaments Anchoring filaments Skin Muscle Initial Lymphatics Lymph Nodes • Lymph nodes – where lymphatics drain into – occur in groups or as node chains alongside the blood vessels • Multiple functions – biological filter stations – production of lymphocytes (especially in an immune reaction) – regulates the protein content of the lymph Lymphatic System The Whole Picture • Superficial lymphatics • Deeper lymphatics Understanding the venous system The lower limbs contain both deep veins (femoral, tibial and popliteal) and superficial veins (long and short saphenous) Perforator veins connect them through the fascia and are reliant on a system of non-return valves Therefore when we stand up blood is prevented from flowing downwards back into the superficial veins. Non-return valves can be congenitally absent, weakened as in pregnancy, or traumatized by injury or deep vein thrombosis. Backflow dilates the superficial veins which then become visible Venous vs Lymphatics Starlings Law Revised ! Lymph vessels are responsible for taking ALL the interstitial fluid away Venous congestion causes higher capillary filtration Venous oedema will turn into chronic oedema if left untreated! Lymphoedema Lymphoedema (chronic oedema) is the result of accumulation of fluid in the tissue spaces due to an imbalance between interstitial fluid production and transportation. Lymph fluid is corrosive to skin and causes skin maceration and ulceration (Lymphorrhea) Imbalance Lymphoedema develops when the balance is disturbed between: • Fluid exchange from blood capillaries and the interstitium • Fluid transportation via blood capillaries and the lymphatic system out of the interstitium More fluid is entering the interstitium than the venous capillaries and lymph vessels can absorb Lymphatic Overloading - Flooding Factors Causing Oedema • Trauma and tissue damage: • Malignant disease: • Venous disease: • Obesity • Infection: • Inflammation: • Endocrine: • Immobility / dependency: – – – – – – – surgery, radiotherapy, scarring, burns, chemotherapy metastases, infiltrating tumour, extrinsic pressure, lymphoma ulceration, chronic venous insufficiency, post thrombotic syndrome, IV drug use cellulitis, lymphadenitis, filariasis, TB rheumatoid arthritis, dermatitis, psoriasis hormonal surges (eg: puberty, pregnancy, menopause) paralysis, dependency oedema Influencing Factors in Oedema Low Protein • Low Serum Albumin • Cardiac Insufficiency • Allergic Reactions • Renal Insufficiency • Drugs (NSAID’s, Steroids, Hormonals) Mixed • Vena Caval Obstruction • Venous Insufficiency • Injuries to bones/tissues • Inadequate muscle pump High Protein • Lymphostatic disorders Classification of Lymphoedema Lymphoedema is classified as primary or secondary depending on aetiology Primary Lymphoedema is a congenital abnormality of the lymphatic system, often present from birth Secondary Lymphoedema results from damage to lymphatic vessels or nodes or overload to the system ie. Chronic venous insufficiency or cancer treatments Primary Lymphoedema Congenital Missing or malformed Lymphatics Hyperkeratosis scaly patches caused by overproliferation of the keratin layer Classification of oedema Swelling – mild, moderate or severe Skin condition – thickened, warty, blistered, lymphorrhea, ulcerated Shape change – abnormal or distorted shape Frequency of cellulitis/erysipelas Classification of Severity Mild <20% excess limb volume Moderate 20%-40% excess limb volume Severe >40% excess limb volume Assessment components Medical history Neurovascular assessment Oedema history and treatment Examination of skin, subcutaneous tissues, site, circulation – Stemmer sign Degree and distribution of swelling Functional abilities Psychological response and motivation Social situation ABPI in patients with Chronic Oedema Ankle Brachial Pressure Index in a patient with oedema may not be possible or advisable. Consider using a larger cuff and Doppler probe with lower frequency ie 5mHz rather than 8mHz Pulse oximetry is a useful alternative or toe doppler Refer for Duplex Ultrasound Skin colour and temperature Sensation checks Capillary Refill For those ‘at risk’ and those with Lymphoedema Common Sense General Advice Keep nails short - if help required referral to a podiatrist Use an insect repellent in Summer Treat pets for fleas Treat Athletes foot/fungal nail infections Protect skin at all costs What to Avoid Things that can lead to infection and make swelling worse • Having bloods taken from “at risk” or swollen arm • Having infusions (drips) into “at risk” or swollen arm • Scratches, cuts and grazes • Acupuncture • Blood pressure cuffs to a swollen limb • Insect bites / flea bites • Care whilst cleaning or in the garden • Fungal nail infections What to Avoid Constriction of swollen area Having blood pressure taken on “at risk” or swollen limb Tight clothing, cuffs, socks Tight jewellery, such as rings, bracelets and watches Skin Care Skin Care Essential natural barrier to infection Wash and dry area daily water not too hot Pay attention to awkward areas! Stretched skin can become very dry and cracked port of entry for bacteria Application of emollient gentle, with final stroke in downwards fashion to prevent folliculitis Skin Care - Ointment, Cream or Lotion ? Lotions – are less moisturising than creams as they have a higher water to oil ratio. Creams – are less greasy than ointments but not as beneficial to very dry skin. May also cause skin sensitivities due to preservatives added. Ointments – are greasy and rarely cause skin sensitivities. Will lift dry, scaly patches and intensely moisturize dry skin. Skin Observation • Daily skin care to keep limb supple • Prevent trauma and injury • Reduce risk of infection • Prompt treatment of infection Address • Lymphorrhoea - skin care - MLLB • Prevent and treat fungal infections Lymphorrhoea • Lymphorrhoea is the leakage of lymph through the skin surface • Large beads of fluid appear on the skin and trickle down from affected areas • It is often cold to the touch • Possible source of infection! Papillomatosis Dilation of lymphatic vessels and fibrosis Cellulitis Cellulitis is a severe infection requiring urgent treatment with antibiotics. Cellulitis can cause lymphoedema or worsen existing swelling. Following cellulitis lymphoedema is unlikely to resolve independently, or ever return to normal Cellulitis not completely eradicated will remain chronic and keep returning. Chronic Cellulitis Management of Cellulitis Acute cellulitis – Treat for at least 14 days or until all signs of inflammatory episode has gone. Prophylactic antibiotics if recurrent episodes of infection. Amoxicillin 500mg q8h or Flucloxacillin 500mg q 6hr If allergic to Penicillin – Clindamycin 300mg BLS Consensus Document of the Management of Cellulitis in Lymphoedema – www.lymphoedema.org/lsn Preventing cellulitis Skin Care – frequent bathing and moisturizing of affected limb Treating infections effectively Reducing oedema Compression therapy (bandaging or hosiery) Exercise and Lymphoedema Promotes lymph drainage Improves joint mobility Helps maintain weight Gentle regular exercise – swimming, yoga, Pilates Avoid exercise that puts a heavy strain on the limb such as lifting weights (includes lifting children), digging the garden, prolonged ironing or window cleaning, jogging Exercise & Movement – improves lymph flow Use the limb as normally as possible Avoid strenuous movement Rest is as important Position and support the limb Encourage normal activity walking, swimming, etc. Over-activity can cause increased swelling - Treatment decisions Compression Hosiery Multi layer lymphoedema bandaging (MLLB) Intensive therapy (this includes skin care, exercise and elevation of the limb) Refer to Specialist MLD (manual lymphatic drainage) to decongest the impaired lymphatic pathways MLLB Compression hosiery MLD (manual lymphatic drainage) Aims to reduce swelling by encouraging lymph flow Gently massage technique recognised as key component in DLT Bypasses ineffective or obliterated lymph vessels MLD must be combined with compression to support and maintain its effects MLD – not traditional Massage! Dependant Oedema Pre Treatment 3 weeks later with short stretch bandaging DVT – Post Thrombotic Syndrome Before Treatment (unable to work – leg 100% larger distally) 3 weeks later – leg just 10% larger – now working full time What about Obesity? Morbid obesity can produce lymphoedema in absence of any other compromise to lymph system. When sitting both venous and lymphatic vessels are obstructed. Obese patients should avoid sitting at 90 degrees. Elusive but definite link between fat, lymphatics and immune system’ (Rockson 2004) Metastatic Pelvic Disease Case Study 71 year old female Skin Condition Discharge Photos Total fluid loss in 1st 10 days – 14 litres ! Each litre weighs 2lb Maintenance Compression Hosiery Consider the ‘stiffness factor’ Interface pressure is the pressure produced by the hosiery on the skin’s surface. Materials that are less elastic ie flat knit give sustained pressure levels. In the case of shape distortion elastic circular knit hosiery may cause a tourniquet effect and therefore skin damage. Flat knit hosiery is the safe option. Education and applicators Hosiery in the drawer doesn’t help! What's wrong with this picture? Compression garments What type ? Flat knit or Circular knit Off the self or made to measure Need for a zip ? Applicator device ? Circular knit Prevention of oedema Varicose veins Venous disease Leg of Uniform shape No folds or rebound swelling Flat knit garments • The limb shape is uneven and distorted • The skin is intact and resilient • The oedema is long-standing and at risk of further breakdown • The oedema is prone to “rebound” Flat Knit Circular knit Mtm flat knit garments Time for Questions?