Perinatal Journal
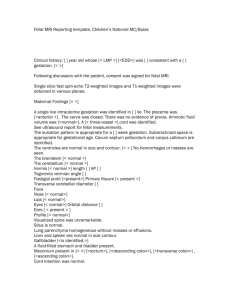
advertisement

ISSN 1300-3124 PERINATAL JOURNAL AT AL JO U R A PE IN N R www.perinataljournal.com L IN N R The Official Publication of Perinatal Medicine Foundation Turkish Perinatology Society Turkish Society of Obstetrics and Gynecology A PE L Volume 23 | Issue 1 | April 2015 AT U AL JO R AL JO U R A PE R AT N IN L L R N A PE IN AT U AL JO R www.perinataljournal.com The Official Publication of Perinatal Medicine Foundation, Turkish Perinatology Society and Turkish Society of Ultrasound in Obstetrics and Gynecology Description Perinatal Journal, the Official Publication of Perinatal Medicine Foundation, Turkish Perinatology Society and Turkish Society of Ultrasound in Obstetrics and Gynecology, is an international online open access peer-reviewed scientific journal (e-ISSN: 1305-3124) published triannually in English. The manuscripts which are accepted for publication in the Perinatal Journal are published as a parallel publication of Turkish version in “Perinatoloji Dergisi” (p-ISSN:13005251, e-ISSN:1305-3132). Translation in to Turkish language is provided by the publisher as free of charge for authors. This is automatically accepted by the authors of manuscripts at the time of submission. The journal mainly includes original clinical and experimental research articles, case reports, reviews, editorial and opinion articles, and a letters column. Perinatal Journal can be read by perinatologists, obstetricians, gynecologists, radiologists, pediatricians, sonographers, midwives, radiographers, and scientific members of other related areas. Aim and Scope Perinatal Journal aims to create an interdisciplinary scientific platform for sharing and discussing topics on perinatal medicine and to share its experience with international scientific community. Copyright Periantal Journal does not officially agree with the ideas of manuscripts published in the journal and does not guarantee for any product or service advertisements in its content. Scientific and legal responsibilities of published articles belong to their authors. Materials such as pictures, figures, tables etc. sent with manuscripts should be original or if they were published before written approval of copyright holder should be sent with manuscript for publishing together. All published materials will become the sole property of, and will be copyrighted by Perinatal Journal. Therefore, "Acknowledgement of Authorship and Transfer of Copyright Agreement" are requested in addition to manuscripts that are to be assessed. Acknowledgement of Authorship and Transfer of Copyright Agreement form is available online at www.perinataljournal.com. No payment is done for manuscripts under the name of copyright or others approved for publishing in the journal and no publication cost is charged. Deomed Publishing Gür Sok., No: 7B Kad›köy 34720 Istanbul, Turkey Telefon: +90 216 414 83 43 (Pbx) Faks: +90 216 414 83 42 e-posta: medya@deomed.com • www.deomed.com To promote the development of global open access to scientific information and research, the journal provides copyrights of all online published papers (except where otherwise noted) for free use of readers, scientists, and institutions (such as link to the content or permission for its download, distribution, printing, copying, and reproduction in any medium, without any changing and except the commercial purpose), under the terms of CC BY-NC-ND 3.0 License (www.creativecommons.org/licenses/by-nc-nd/3.0), provided the original work is cited. To get permission for commercial purpose please contact the publisher. Conflicts of Interest The authors should disclose all issues concerning financial relationship, conflict of interest, and competing interest that may potentially influence the results of the research or scientific judgment. All financial contributions or sponsorship, financial relations, and areas of conflict of interest should be clearly explained in the cover letter to the Editor-in-Chief at the time of submission, with full assurance that any related document will be submitted to the journal when requested. For the details of journal's "Conflicts of Interest Policy" please visit www.perinataljournal.com. Publication Ethics and Malpractice Statement For the details of journal's “Publication Ethics and Malpractice Statement” please visit www.perinataljournal.com. Publication Info Ownership: On behalf of the Perinatal Medicine Foundation, Cihat fien Managing Editor: Murat Yayla Administrative Office: Cumhuriyet Cad. 30/5 Elmada¤, Taksim 34367 ‹stanbul Due the Press Law of Turkish Republic dated as June 26, 2004 and numbered as 5187, this publication is classified as a local periodical. Perinatal Journal is published by Deomed Publishing (Copyright © 2015, Perinatal Medicine Foundation). Publication Coordinator: ‹lknur Demirel English Editor: Fikret Yeflilyurt Graphic Design: Tolga Erbay Page Layout: Nurgül Özcan AL JO U R A PE R AT N IN L L R N A PE IN AT U AL JO R www.perinataljournal.com Volume 23 | Issue 1 | April 2015 Editor-in-Chief Advisory Board Cihat fien, Istanbul, Turkey Abdallah Adra, Beirut, Lebanon Arif Akflit, Eskiflehir, Turkey Aris Antsaklis, Athens, Greece Saadet Arsan, Ankara, Turkey Abdel-Latif Ashmaig, Khartoum, Sudan Alev At›fl-Ayd›n, Istanbul, Turkey Ahmet Baschat, Baltimore, MD, USA Ahmet Baflaran, Konya, Turkey Lous Cabero Roura, Barcelona, Spain Manuel Carrapato, Porto, Portugal Jose M. Carrera, Barcelona, Spain Julene Carvalho, London, UK Rabih Chaoui, Berlin, Germany Frank Chervenak, New York, NY, USA Bülent Çakmak, Tokat, Turkey Filiz Çayan, Mersin, Turkey Ebru Çelik, Malatya, Turkey Vincenzo D’Addario, Bari, Italy Nur Daniflmend, Istanbul, Turkey Cansun Demir, Adana, Turkey Jan Deprest, Leuven, Belgium Ebru Dikensoy, Gaziantep, Turkey Gian Carlo DiRenzo, Perugia, Italy Tony Duan, Shanghai, PRC Joachim Dudenhausen, Berlin, Germany Alaa Ebrashy, Cairo, Egypt Elif Gül Yapar Eyi, Ankara, Turkey Ali Gedikbafl›, Istanbul, Turkey Ulrich Gembruch, Bonn, Germany Anne Greenough, London, UK Gökhan Göynümer, Istanbul, Turkey Arif Güngören, Hatay, Turkey Melih A. Güven, Istanbul, Turkey Joseph Haddad, Paris, France Davor Jurkovic, London, UK Oliver Kagan, Tübingen, Germany Ömer Kandemir, Ankara, Turkey Burçin Kavak, Elaz›¤, Turkey ‹schiro Kawabata, Osaka, Japan Selahattin Kumru, Düzce, Turkey Mertihan Kurdo¤lu, Ankara, Turkey Associate Editors Murat Yayla, Istanbul, Turkey Olufl Api, Istanbul, Turkey As›m Kurjak, Zagreb, Croatia Nilgün Kültürsay, Izmir, Turkey Malcome Levene, Leeds, UK Narendra Malhotra, Agra, India Giampaolo Mandruzzato, Trieste, Italy Alexandra Matias, Porto, Portugal Ratko Matijevic, Zagreb, Croatia Israel Meizner, Tel Aviv, Israel Mohammed Momtaz, Cairo, Egypt Giovanni Monni, Cagliari, Italy Ercüment Müngen, Istanbul, Turkey Kypros Nicolaides, London, UK Lütfü Öndero¤lu, Ankara, Turkey Soner R. Öner, Izmir, Turkey Okan Özkaya, Isparta, Turkey Alexander Papitashvilli, Tbilisi, Georgia ‹brahim Polat, Istanbul, Turkey Ritsuko Pooh, Osaka, Japan Ruben Quintero, Tampa, FL, USA Nebojsa Radunovic, Belgrade, Serbia Guiseppe Rizzo, Rome, Italy Stephen Robson, Newcastle, UK Roberto Romero, Detroid, MI, USA Levent Salt›k, Istanbul, Turkey Haluk Sayman, Istanbul, Turkey Mekin Sezik, Isparta, Turkey Jiri Sonek, Dayton, OH, USA Yunus Söylet, Istanbul, Turkey Milan Stanojevic, Zagreb, Croatia Florin Stomatian, Cluj, Romania Turgay fiener, Eskiflehir, Turkey Alper Tanr›verdi, Ayd›n, Turkey Ebru Tar›m, Adana, Turkey Neslihan Tekin, Eskiflehir, Turkey Ilan Timor-Tritsch, New York, NY, USA Seyfettn Uluda¤, Istanbul, Turkey Liliana Voto, Buenos Aires, Argentina Miroslaw Wielgos, Warsaw, Poland Simcha Yagel, Tel Aviv, Israel Ahmet Yal›nkaya, Diyarbak›r, Turkey Ivica Zalud, Honolulu, HI, USA Names are in alphabetical order. The Official Publication of Perinatal Medicine Foundation, Turkish Perinatology Society and Turkish Society of Ultrasound in Obstetrics and Gynecology Correspondence: Perinatal Journal, Perinatal Medicine Foundation, Cumhuriyet Cad. 30/5 Elmada¤, Taksim 34367 ‹stanbul, Turkey Phone: (0212) 225 52 15 • Fax: (0212) 225 23 22 e-mail: editor@perinataljournal.com www.perinataljournal.com AL JO U R A PE R AT N IN L L R N A PE IN AT U AL JO R Coverage The manuscripts should be prepared for one of the following article categories which are peer-reviewed: • Original Article • Case Report • Technical Note • Letter to the Editor In addition, the journal includes article categories which do not require a peer review process but are prepared by the Editorial Board or consist of invited articles, titled as: • Editorial • Opinion • Review • Abstracts • Announcements • Erratum Manuscript Evaluation All submissions to Perinatal Journal must be original, unpublished, and not under the review of any other publication. This is recorded by the system automatically with the IP number, the date and time of submission. On behalf of all authors the corresponding author should state that all authors are responsible for the manuscripts. The name, date, and place of the relevant meeting should be stated if the submission is a work that was previously presented in a scientific meeting. Following the initial review, manuscripts which have been accepted for consideration are reviewed by at least two reviewers. The Editors of the journal decide to accept or reject the manuscript considering the comments of the reviewers. They are authorized to reject or revise the manuscript, to suggest required corrections and changes upon the comments and suggestions of reviewers, and/or to correct or condense the text by permission of the corresponding author. They have also the right to reject a manuscript after authors’ revision. Author(s) should provide additional relevant data, documents, or information upon the editorial request if necessary. Ethical Issues All manuscripts presenting data obtained from studies involving human subjects must include a statement that the written informed consent of the participants was obtained and that the study was approved by an institutional ethics board or an equivalent body. This institutional approval should be submitted with the manuscript. Authors of case reports must submit the written informed consent of the subject(s) of the report or of the patient’s legal representatives for the publication of the manuscript. All studies should be carried out in accordance with the World Medical Association Declaration of Helsinki, covering the latest revision date. Patient confidentiality must be protected according to the universally accepted guidelines and rules. Manuscripts reporting the results of experimental studies on animals must include a statement that the study protocol was approved by the animal ethics committee of the institution and that the study was conducted in accordance with the internationally accepted guidelines, including the Universal Declaration of Animal Rights, European Convention for the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes, Principles of Laboratory Animal Science, and the Handbook for the Care and Utilization of Laboratory Animals. The authors are strongly requested to send the approval of the ethics committee together with the manuscript. In addition, manuscripts on human and animal studies should describe procedures indicating the steps taken to eliminate pain and suffering. The authors should also disclose all issues concerning financial relationship, conflict of interest, and competing interest that may potentially influence the results of the research or scientific judgment. All financial contributions or sponsorship, financial relations, and areas of conflict of interest should be clearly explained in the cover letter to the Editor-in-Chief at the time of submission, with full assurance that any related document will be submitted to the journal ii Perinatal Journal when requested. For the details of journal's "Conflict of Interest Policy" please read the PDF document which includes "Conflicts of Interest Disclosure Statement". Perinatal Journal is committed to upholding the highest standards of publication ethics and observes the following principles of Publication Ethics and Malpractice Statement which is based on the recommendations and guidelines for journal editors developed by the Committee on Publication Ethics (COPE), Council of Science Editors (CSE), World Association of Medical Editors (WAME) and International Committee of Medical Journal Editors (ICMJE). For the details of journal's "Publication Ethics and Malpractice Statement" please visit www.perinataljournal.com. Manuscript Preparation In addition to the rules listed below, manuscripts to be published in Perinatal Journal should be in compliance with the Uniform Requirements for Manuscripts Submitted to Biomedical Journals published by International Committee of Medical Journal Editors (ICMJE) of which latest version is available at www.icmje.org. Authors are requested to ensure that their manuscript follows the appropriate guidelines such as CONSORT for randomized controlled trials, STROBE for observational studies, STARD for diagnostic accuracy studies, and PRISMA for systematic reviews and meta-analyses, for the study design and reporting if applicable. Authorship and Length of Texts The author(s) must declare that they were involved in at least 3 of the 5 stages of the study stated in the “Acknowledgement of Authorship and Transfer of Copyright Agreement” as “designing the study”, “collecting the data”, “analyzing the data”, “writing the manuscript” and “confirming the accuracy of the data and the analyses”. Those who do not fulfill this prerequisite should not be stated as an author. Original research articles base on clinical or experimental studies. The main text should not exceed 2500 words (max. 16 pages), and a maximum of six authors is advisable. Case reports should illustrate interesting cases including their treatment options. The main text should not exceed 2000 words (max. 8 pages), and a maximum of five authors is advisable. Viewpoint articles: Only by invitation and should be no more than 2000 words long (max. 8 pages). Review articles: Only by invitation and should be no more than 40005000 words long (max. 20 pages). Technical notes aims to present a newly diagnostic or therapeutic method. They should not exceed 2000 words (max. 8 pages) and include a maximum of 10 references. Letters to the Editor should be no more than 500 words long (max. 2 pages) and include a maximum of 10 references. Sections in the Manuscripts Manuscripts should be designed in the following order: title page, abstract, main text, references, and tables, with each typeset on a separate page: Page 1 - Title page Page 2 - Abstract and key words Page 3 and next - Main text Next Page - References Next Page - Table heading and tables (each table should be placed in separate pages) Next Page - Figure legends and figures (each figure should be placed in separate pages) Last Page - Appendices (patient forms, surveys etc.) Title page This page should only include the title of the manuscript, which should be carefully chosen to better reflect the contents of the study. No anusual abbreviations Information for the Authors www.perinataljournal.com should be used in the title of the manuscript. A short title as running heading not exceeding 40 characters should be given which is desired to appear on top part of continuing pages when journal is published. should not be used. Papers published in only electronic journals or in the preprint or online first issues of the electronic versions of conventional periodicals should be absolutely presented with DOI (digital object identifier) numbers. Abstract page Abstracts should not contain any abbreviation and references. They should be prepared under following designs. Journal titles should be abbreviated according to the Index Medicus. All authors if six or fewer should be listed; otherwise, the first six and “et al.” should be written. — Abstracts of research articles should be max. 250 words and structured in four paragraphs using the following subtitles: Objective, Methods, Results, and Conclusion. Following the abstract, each abstract page should include max. 5 key words separated with comma and written in lower cases. Direct use of references is strongly recommended and the authors may be asked to provide the first and last pages of certain references. Publication of the manuscript will be suspended until this request is fulfilled by the author(s). — Abstracts of case reports should be max. 125 words and structured in three paragraphs using the following subtitles: Objective, Case, Conclusion. Following the abstract, each abstract page should include max. 3 key words separated with comma and written in lower cases. — Abstracts of review articles should be max. 300 words and presented not structured in one paragraph. Following the abstract, each abstract page should include max. 5 key words separated with comma and written in lower cases. — Abstracts of technical notes should be max. 125 words and structured in three paragraphs using the following subtitles: Objective, Technique, Conclusion. Following the abstract, each abstract page should include max. 3 key words separated with comma and written in lower cases. — Standard journal article: Hammerman C, Bin-Nun A, Kaplan M. Managing the patent ductus arteriosus in the premature neonate: a new look at what we thought we knew. Semin Perinatol 2012;36:130-8. Main text: The sections in main text are defined according to the manuscript type. — In research articles, main text should consist of sections titled as "Introduction, Methods, Results, Discussion and Conclusion". Each title may have subtitles. The categories of subtitles should be clearly defined. The Introduction section should include a brief summary of the base of the work and clearly states the purpose of the study. The Methods section should contain a detailed description of the material, the study design and clinical and laboratory tests, and statistical methods used. A statement regarding the ethical issues should also be given in this section. The Results section should provide the main findings of the study. Data should be concisely presented, preferably in tables or graphs. The Discussion section should mainly rely on the results derived from the study, with relevant citations from the most recent literature. The Conclusion section should briefly and claearly present the conclusions derived from the results of the study. It should be in compliance with the aim of the work and and point out its application in clinical practice. — In Case Reports, main text should be divided with the titles "Introduction, Case(s), Discussion". Reported case(s) should be introduced clearly including the case story, and the results of laboratory tests should be given in table format as far as possible. — The text of the reviews articles should follow the "Introduction" and be organized under subtitles which should clearly define the text's context categorization. The Reviews are expected to include wide surveying of literature and reflect the author's personal experiences as far as possible. — The text of the technical note type of articles should be divided into "Introduction, Technic, Discussion". The presented technic should be defined briefly under the related title, and include illustrations or figures as soon as possible. — Letters to the Editor should not have titled sections. If there is a citation about a formerly published article within the text, reference(s) should be provided. References References used in the text should be directly related to the topic, as recent as possible and in enough numbers. They should be numbered in square brackets in the order in which they are mentioned in the text including Tables and Figures. Citation order should be checked carefully. Only published articles or articles in press can be used in references. Unpublished data including conference papers or personal communications The style and punctuation should follow the formats outlined below: — Article published in an only electronic journal: Lee J, Romero R, Xu Y, Kim JS, Topping V, Yoo W, et al. A signature of maternal anti-fetal rejection in spontaneous preterm birth: chronic chorioamnionitis, anti-human leukocyte antigen antibodies, and C4d. PLoS ONE 2011;6:e16806. doi:10.1371/ journal.pone.0011846. — Book: Jones KL. Practical perinatology. New York: Springer; 1990. p. 112-9. — Chapter in a book: Sibai BM, Frangieh AY. Eclampsia. In: Gleicher N, editors. Principles and practice of medical therapy in pregnancy. 3rd ed. New York: Appleton&Lange; 1998. p. 1022-7. Figures and tables All illustrations (photographs, graphics, and drawings) accompanying the manuscript should be referred to as “figure”. All figures should be numbered consecutively and mentioned in the text. Figure legends should be added at the end of the text as a separate section. Each figure should be prepared as a separate digital file in “jpeg” format, with a minimum 300 dpi or better resolution. All illustrations should be original. Illustrations published elsewhere should be submitted with the written permission of the original copyright holder. For recognizable photographs of human subjects, written permission signed by the patient or his/her legal representative should be submitted; otherwise, patient names or eyes must be blocked out to prevent identification. Microscopic photographs should include information on staining and magnification. Each table should be prepared on a separate page with table heading on top of the table. Table heading should be added to the main text file on a separate page when a table is submitted as a supplementary file. Submission For a swift peer review, Perinatal Journal operates a web-based submission, peer review and manuscript tracking system. Authors are required to submit their articles online. Details of how to submit online can be found at www.perinataljournal.com. Submission Checklist The following list will be useful during the final check of a manuscript before submission: 1. Manuscript length (max. 4000 words for research articles) 2. Number of authors (max. 6 authors for research articles) 3. Title page (no anusual abbreviations) 4. Abstracts (max. 250 words for research articles) 5. Key words (max. 5 keys for research articles) 6. Main text (subtitles) 7. References (listed according to the rules of ICMJE) 8. Figures and tables (numbering; legends and headings; copyright info/permission) 9. Cover letter 10. Acknowledgement of Authorship and Transfer of Copyright Agreement (undersigned by all authors) 11. Conflicts of Interest Disclosure Statement (if necessary) Volume 23 | Issue 1 | April 2015 iii AL JO U R A PE R AT N IN R IN N A PE L L Contents AT U AL JO Volume 23, Issue 1, April 2015 R www.perinataljournal.com Original Articles Ultrasonographic evaluation of ventriculomegaly cases 1 Hakan Kalayc›, Halis Özdemir, Ça¤r› Gülümser, Ayfle Parlakgümüfl, Tayfun Çok, Ebru Tar›m, Filiz Bilgin Yan›k Perinatal outcomes of patients diagnosed borderline gestational diabetes mellitus 6 Gök Özgül, Rauf Meleko¤lu, Sevda Yeleç, ‹pek Eskiyörük, Fatma Tuncay Özgünen Health practices of pregnant women in Gumushane City Center 13 Handan Özcan, Nezihe K›z›lkaya Beji The evaluation of pregnancies complicated by eclampsia: retrospective analysis of 37 cases in our clinic 20 Aytekin Tokmak, Korkut Da¤lar, Ali ‹rfan Güzel, Bergen Laleli, Salim Erkaya, Dilek Uygur Factors affecting postpartum depression in Diyarbak›r 26 Ali Emre Tahao¤lu, Cihan To¤rul, Mehmet ‹rfan Külahç›o¤lu, Beflire Ayd›n Öztürk, Deniz Balsak, Hanifi Bademk›ran, Erdo¤an Gül, Ümit Görkem, Tayfun Güngör Analysis of maternal serum and urinary lipocalin-2 levels 30 Yeflim Bayo¤lu Tekin, Ülkü Mete Ural, Aynur K›rbafl, fienol fientürk, Figen K›r fiahin Critical pulmonary stenosis with prenatal diagnosis: a case series and review of literature 34 Oya Demirci, Taner Yavuz, Resul Ar›soy, Emre Erdo¤du, P›nar Kumru, Oya Pekin Evaluation of prenatal invasive procedures: analysis of retrospective cases 39 Aybike Tazegül Pekin, Özlem Seçilmifl Kerimo¤lu, Setenay Arzu Y›lmaz, Nadir Koçak, Feyza Nur ‹ncesu, Ayfle Gül Kebapc›lar, Çetin Çelik Investigation of the effects of fetal gender on umbilical artery and middle cerebral artery Doppler findings 45 Burcu Artunç Ülkümen, Halil Gürsoy Pala, Y›ld›z Uyar, Yeflim Baytur, Faik Mümtaz Koyuncu Results of routine first trimester screening tests and following invasive procedures during pregnancy 50 Rahime Nida Ergin, Murat Yayla Case Reports The association of congenital hand reduction defect and uterine anomaly 56 Bülent Kars, Önder Sakin, Yasemin Karageyim Karfl›da¤, Cenk Demir, Esra Esim Büyükbayrak Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case 60 Sevil Eraslan, Rauf Meleko¤lu, Ebru Çelik Goiter in fetus without maternal thyroid disease: a case report 65 Önder Sakin, Bülent Kars, Yasemin Karageyim Karfl›da¤, Cenk Demir, Esra Esim Büyükbayrak Letter to Editor Letter to the Editor regarding “Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case” Baflak Kaya, Ali Gedikbafl› iv Perinatal Journal 70 AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):1–5 R N A PE IN AT U AL JO R Ultrasonographic evaluation of ventriculomegaly cases Hakan Kalayc›, Halis Özdemir, Ça¤r› Gülümser, Ayfle Parlakgümüfl, Tayfun Çok, Ebru Tar›m, Filiz Bilgin Yan›k Department of Gynecology & Obstetrics, Medical School of Baflkent University, Ankara, Turkey Abstract Özet: Ventrikülomegali vakalar›n›n ultrasonografik de¤erlendirilmesi Objective: To evaluate retrospectively the demographic data of the patients diagnosed in or referred with the pre-diagnosis of ventriculomegaly to Perinatology Department of Adana and Ankara Hospitals of Baflkent University. Methods: In this study, 61 pregnant women with fetal ventriculomegaly diagnosed in our clinic or referred by other centers to the Perinatology Department of Ankara and Adana Hospitals of Baflkent University between May 2008 and March 2013 were evaluated in terms of their demographic data, diagnosis weeks, concomitant anomalies and the course of their pregnancies. SPSS v. 16.0 was used for statistical calculations. Results: The analysis of 61 pregnant women between 20 and 41 years old showed that it was the first pregnancy of 45.9% of them. Only 16.4% of them were at or over 35 years old. It was observed that 4.9% of them were conceived by assisted reproduction techniques. The rates of mild (10–12 mm), moderate (12.1–14.9 mm) and severe ventriculomegaly (≥15 mm) were 65.6%, 24.7% and 4.8%, respectively. Toxoplasma, Cytomegalovirus, Rubella or Herpes virus infections were not found in any case. Down syndrome was found in the karyotype analysis of 3 patients (4.9%). The ventriculomegaly was unilateral in 67.2% of the cases. The detection rate between 16 and 24 weeks which were also the weeks for detailed ultrasonography was 52.5%. There was an additional anomaly in 33.3% of the cases. The most frequent concomitant anomalies were found as increased nuchal thickness (13.3%), corpus callosum agenesis (11.1%) and nasal bone hypoplasia (8.9%). In their follow-ups, it was observed that the findings were regressed in 53.8% of the cases, progressed in 19.3% of the cases and remained unchanged in 26.9%. Conclusion: When ventriculomegaly is detected, the presence of additional anomalies should be investigated by detailed ultrasonographic examination during etiological investigation. In the selective cases, the physicians may utilize the method of magnetic resonance imaging to evaluate additional cerebral anomalies. It is also necessary to recommend karyotype analysis and investigating Toxoplasma, Rubella, Cytomegalovirus and Herpes virus infections in the presence of additional anomaly and even in isolated cases regardless of the level of ventriculomegaly. Patients should be followed up regularly. Amaç: Baflkent Üniversitesi Adana ve Ankara Hastaneleri Perinatoloji bilim dal›nda tan› alm›fl veya ventrikülomegali ön tan›s› ile refere edilmifl hastalar›n demografik verilerinin retrospektif olarak de¤erlendirilmesi. Yöntem: Bu çal›flmada May›s 2008 ve Mart 2013 tarihleri aras›nda Baflkent Üniversitesi Ankara ve Adana Hastaneleri Perinatoloji Bilim Dal›na d›flar›dan gönderilen veya klini¤imizde tespit edilen fetal ventrikülomegalisi olan 61 gebe demografik verileri, tan› konulma haftalar›, efllik eden anomaliler ve gebeliklerin seyri aç›s›ndan de¤erlendirildi. ‹statistiksel hesaplamalarda SPSS v. 16.0’dan faydalan›ld›. Bulgular: 20–41 yafl aras› 61 gebenin de¤erlendirmesinde, %45.9’unun ilk gebelikleriydi. %16.4’ü 35 yafl ve üzeriydi. %4.9’unun yard›mc› üreme teknikleri ile gebe kald›¤› izlendi. Hafif (10–12 mm), ›l›ml› (12.1–14.9 mm) ve ciddi ventrikülomegali (≥15 mm) oranlar› s›ras› ile %65.6, %24.7 ve %4.8 idi. Hiçbir vakada toksoplazma, sitomegalovirüs, rubella veya Herpes virüs enfeksiyonu saptanmad›. Karyotip analizinde 3 hastada Down sendromu tespit edildi (%4.9). Ventrikülomegalilerin %67.2’si tek tarafl› idi. Ayr›nt›l› ultrasonografi haftas› olan 16–24 haftalar› aras› tespit oran› %52.5 idi. %33.3 ek anomali mevcuttu. En s›k efllik eden anomaliler s›kl›k s›ras›na göre artm›fl nukal kal›nl›k (%13.3), korpus kallozum agenezisi (%11.1) ve nazal kemik hipoplazisi (%8.9) olarak izlendi. Takiplerde %53.8 vakada bulgular›n geriledi¤i, %19.3’ünde ilerledi¤i ve %26.9’unda de¤iflmeden kald›¤› izlendi. Sonuç: Ventrikülomegali tespit edildi¤inde etyoloji araflt›rmas›nda ayr›nt›l› ultrasonografik muayene ile ek anomalilerin varl›¤› araflt›r›lmal›d›r. Selektif vakalarda ek serebral anomalileri de¤erlendirmek için manyetik rezonans görüntüleme yönteminden faydalan›labilir. Karyotip analizi ve toksoplazma, rubella, sitomegalovirüs ve Herpes virüs enfeksiyonlar›n›n araflt›r›lmas› ek anomali varl›¤›nda ve hatta izole vakalarda ventrikülomegalinin derecesi ne olursa olsun önerilmelidir. Hastalar düzenli takibe al›nmal›d›r. Keywords: Isolated ventriculomegaly, additional anomalies, followup. Anahtar sözcükler: ‹zole ventrikülomegali, ek anomaliler, takip. Correspondence: Hakan Kalayc›, MD. Baflkent Üniversitesi T›p Fakültesi Kad›n Hastal›klar› ve Do¤um Anabilim Dal›, Ankara, Turkey. e-mail: smartdr96@yahoo.com Received: April 15, 2014; Accepted: September 7, 2014 Please cite this article as: Kalayc› H, Özdemir H, Gülümser Ç, Parlakgümüfl A, Çok T, Tar›m E, Bilgin Yan›k F. Ultrasonographic evaluation of ventriculomegaly cases. Perinatal Journal 2015;23(1):1–5. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231001 doi:10.2399/prn.15.0231001 QR (Quick Response) Code: Kalayc› H et al. Introduction The term ventriculomegaly (VM) is used for the cases where anterior horns of ventricle, cavum septum pellucidum and choroid plexus can be seen in the axial plane and lateral ventricle measurement on the plane is 10 mm and above at the glomus level of choroid plexus (Fig. 1).[1,2] There are various definitions according to the width of lateral ventricle. When lateral ventricle measurements are 10–12 mm and 12.1–15 mm, the definitions of mild and moderate VM are used.[3,4] However, some authors deny 10-12 mm as mild VM and define mild VM as 10-15 mm.[5] In measurements which are 15 mm and above, severe VM term is used.[6] While mild VM prevalence is 7.9 out of 10,000 live births, severe VM prevalence is reported as 3.6 out of 10,000 live births.[7] Many factors are assumed in the etiology such as infections; cerebral atrophy induced by white matter injury and/or cases causing absorption of cerebrospinal fluid to decrease; obstructive causes such as DandyWalker malformation or aqueductal stenosis; developmental anomalies such as encephalocele, corpus callosum agenesis (Figs. 2a and 2b); genetic disorders such as trisomy 13, 18 and 21; and cases such as choroid plexus papilloma which may cause excessive cerebrospinal fluid production.[8] This expansion in ventricles may be accompanied by anomalies such as hydrocephaly, gray matter migration anomalies, corpus callosum agenesis, trisomies and microcephaly.[5] The incidence of associated cerebral or extracerebral anomalies varies between 41% and 78%.[2] Many authors a Fig. 2. 2 Fig. 1. Moderate ventriculomegaly. believe that the presence of additional malformations is directly associated with the prognosis. Prognosis is observed better in most of the isolated VM cases.[2,9] Therefore, prenatal diagnosis becomes crucial. In this study, we aimed to analyze the demographic data, diagnosis weeks, concomitant anomalies and the course of pregnancy retrospectively in patients diagnosed with ventriculomegaly during intrauterine period. Methods In this study, 61 pregnant women with fetal ventriculomegaly diagnosed in our clinic or referred by other centers to the Perinatology Department of Ankara and b (a) Corpus callosum agenesis (arrow). (b) Corpus callosum agenesis, colpocephaly, teardrop appearance (arrow). Perinatal Journal Ultrasonographic evaluation of ventriculomegaly cases Adana Hospitals of Baflkent University between May 2008 and March 2013 were evaluated in terms of their demographic data, diagnosis weeks, concomitant anomalies and the course of their pregnancies. All fetuses were evaluated by detailed fetal biometric examination. Statistical data were analyzed by SPSS v. 16.0 (SPSS Inc., Chicago, IL, USA) software. Results The analysis of 61 pregnant women between 20 and 41 years old showed that it was the first pregnancy of 45.9% of them. Only 16.4% of them were at or over 35 years old. It was observed that 4.9% of them were conceived by assisted reproduction techniques. The rates of mild (10–12 mm), moderate (12.1–14.9 mm) and severe ventriculomegaly (≥15 mm) were 65.6%, 24.7% and 4.8%, respectively. No Toxoplasma, Rubella, Cytomegalovirus (CMV) and Herpes virus infection was found in any of the pregnant women. Down syndrome was found in the karyotype analysis of 3 fetuses (4.9%). The ventriculomegaly was unilateral in 67.2% of the cases. The detection rate between 16 and 24 weeks which were also the weeks for detailed ultrasonography was 52.5%. The most frequent concomitant anomalies were observed as increased nuchal thickness (13.3%), corpus callosum agenesis (11.1%), and nasal bone hypoplasia (8.9%). Additionally, obstetric magnetic resonance was applied to 44.3% of the pregnant women. Of pregnant women, 72.5% of them delivered at 37 weeks or later. In their follow-ups, it was observed that the findings were regressed in 53.8% of the cases, progressed in 19.3% of the cases and remained unchanged in 26.9%. Discussion In the detailed ultrasonographic examination performed on 18–22 weeks of gestation, it is routinely recommended to measure the width of lateral cerebral ventricles.[1,10,11] In the lateral ventricle measurements, 10–12 mm is defined as mild VM, 12.1–15 mm as moderate and 15 mm, and above as severe VM.[3,4] Infections may also have a role in the etiology. In the study of Do¤an et al., severe VM was found in 5 of 8 cases with CMV infection, increased periventricular echogenicity, intracranial calcification in 4 cases, thalamic hyperechogenicity in 3 cases, and mega cisterna magna.[12] Tijana et al. found VM, which did not display any finding on previous weeks, in patient with positive toxoplasmosis at 25 weeks of gestation.[13] Dommergues et al. detected CMV positivity in 29% of the cases in their study.[14] In various publications, infection positivity was observed as 10–20% in severe VM cases while it was 1–5% in mild VM cases.[9,15,16] Therefore, it is recommended to evaluate all cases diagnosed with VM in terms of infection.[6,15,17,18] In our study, no infection factor was found; the reason is the rate of severe VM seen in our patients as low as 4.8%. Chromosomal anomaly incidence varies in VM cases between 0% and 14%.[5,6,15] In our study, Down syndrome was found in 4.9% (3) cases. While Nicolaides et al. reported chromosomal anomaly incidence as 3% in isolated VM cases, they showed this rate as 36% in the presence of additional anomaly. Also, aneuploidy was reported at a low rate in isolated severe VM cases compared to isolated mild VM cases.[19] Similarly, Melchiorre et al. reported the rate of chromosomal anomaly in isolated cases as 2.8%.[20] Gaglioti et al. did not find any chromosomal anomaly in severe VM cases while aneuploidy rate was 3.5% in mild and moderate VM cases.[16] Gezer et al. reported chromosomal anomaly incidence (6.8%) in fetuses with severe ventriculomegaly higher than the fetuses with mild ventriculomegaly (4.2%). Chromosomal anomaly incidence (8.6%) in fetuses with isolated ventriculomegaly was also found higher than those with additional anomaly (3.8%).[21] Sezik observed Type 2 triploidy case with VM accompanied by atrioventricular septal defect.[22] Kara described the association of VM and 47 XXY syndrome in a case report.[23] In ventriculomegaly cases, it is possible to observe both cerebral and extracerebral malformations as an additional anomaly. They especially accompany with severe VM. The most frequent concomitant anomalies of severe VM cases are corpus callosum agenesis and bifid spine.[24,25] In mild and moderate VM cases, this rate varies between 10% and 76%.[17,26] Various studies reported additional anomaly incidence at rates reaching up to 50%.[6,11,15] Gaglioti et al. found additional anomaly in 60% of severe VM cases. In 88% of these cases, families preferred to terminate the pregnancy.[16] Tatl› et al. found additional anomaly in 9% of cases with 10-15 mm ventricle width.[27] In our study, the most frequent additional anomalies (33.3%) were increased nuchal thickness (13.3%), corpus callosum agenesis (11.1%) and nasal bone hypoplasia (8.9%). Volume 23 | Issue 1 | April 2015 3 Kalayc› H et al. We observed in our study that the findings were regressed in 53.8% of the cases, progressed in 19.3% of the cases and remained unchanged in 26.9%. Ouahba et al. reported regression in 11% of 167 mild VM cases, and they observed more regression in these cases in terms of neurological development.[9] Melchiorre et al. found a progression at a rate of 15.7%. In those with progression, there was poor prognosis in terms of neurological development and association with chromosomal anomalies.[20] During magnetic resonance imaging, Levine et al. found additional findings at a rate of 13.5% which may change patient management in cases found to have anomaly by ultrasonography.[28] Gezer et al. asserted that ventricle width and brain parenchyma volume rate may be helpful to determine prognosis in magnetic resonance imaging. Parenchyma volumes of those with poor prognosis were found to be low.[29] We applied obstetric magnetic resonance imaging to 44.3% of our cases. We confirmed the diagnosis of corpus callosum agenesis in four fetuses by ultrasonography, cortical atrophy in one case, and encephalomalacia in one case. In line with these findings, magnetic resonance imaging is significant to confirm the suspected diagnoses established by ultrasonography. The use of magnetic resonance imaging is useful for pathologies such as neuronal migration disorders, delayed sulcation, gyrus formation and heterotopias which can be detected at late second and third trimesters and overlooked by ultrasonography.[30,31] After the 11 years of follow-up of 101 children with isolated VM, normal psychomotor development was observed in 89 of them, and neurological disorder in the spectrum reaching out from language delay up to the severe mental retardation.[12] Vergani et al. found neurological development retardation clearly lower in groups with 12 mm and lower widths than the group with 12 mm and above (3% vs. 23%).[6] Devaseelan et al. reported neurological development retardation as 14% in children with progressed VM during intrauterine period.[32] In another study, scores below the normal levels were reported for fine motor skills and language development in children with persisting ventricle width during prenatal period.[33] Conclusion When ventriculomegaly is detected, the presence of additional anomalies should be investigated by detailed 4 Perinatal Journal ultrasonographic examination during etiological investigation. In the selected cases, the physicians may utilize the method of magnetic resonance imaging to evaluate additional cerebral anomalies. In line with the current information we have, we recommend performing karyotype analysis and investigating Toxoplasma, CMV and infections such as Rubella regardless of the level of ventriculomegaly and even in the isolated ventriculomegaly cases without any additional anomaly. Patients should be followed up regularly. The parents should be informed in detail for the neuropsychiatric conditions that may arise during postpartum period. Conflicts of Interest: No conflicts declared. References 1. International Society of Ultrasound in Obstetrics and Gynecology Education Committee. Sonograpic examination of the fetal central nervous system: Guidelines for performing the “basic examination” and the “fetal neurosonogram”. Ultrasound Obstet Gynecol 2007;29:109–16. 2. Cardoza JD, Goldstein RB, Filly RA. Exclusion of fetal ventriculomegaly with a single measurement: the width of the lateral ventricle atrium. Radiology 1988;169:711–4. 3. Signorelli M, Tiberti A, Valseriati D, Molin E, Cerri V, Groli C, et al. Width of fetal lateral ventricular atrium between 10 and 12 mm: a simple variation of the norm? Ultrasound Obstet Gynecol 2004;23:14–18. 4. Wax JR, Bookman L, Cartin A, Pinette MG, Blackstone J. Mild fetal cerebral ventriculomegaly: diagnosis, clinical associations, and outcomes. Obstet Gynecol Surv 2003;58:407– 14. 5. Bromley B, Frigoletto FD Jr, Benacerraf BR. Mild fetal lateral cerebral ventriculomegaly: clinical course and outcome. Am J Obstet Gynecol 1991;164:863–7. 6. Vergani P, Locatelli A, Strobelt N, Cavallone M, Ceruti P, Paterlini G, et al. Clinical outcome of mild fetal ventriculomegaly. Am J Obstet Gynecol 1998;178:218–22. 7. Sethna F, Tennant PWG, Rankin J, C Robson S. Prevalence, natural history, and clinical outcome of mild to moderate ventriculomegaly. Obstet Gynecol 2011;117:867– 76. 8. McKechnie L, Vasudevan C, Levene M. Neonatal outcome of congenital ventriculomegaly. Semin Fetal Neonatal Med 2012;17;301–7. 9. Ouahba J, Luton D, Vuillard E, Garel C, Gressens P, Blanc N, et al. Prenatal isolated mild ventriculomegaly: outcome in 167 cases. BJOG 2006;113:1072–9. 10. American College of Obstetricians and Gynecologists (ACOG). Ultrasonography in Pregnancy: ACOG Technical Bulletin 187. Washington, DC: ACOG; 1993. Ultrasonographic evaluation of ventriculomegaly cases 11. American Institute of Ultrasound in Medicine. AIUM Practice Guideline for the performance of an antepartum obstetric ultrasound examination. J Ultrasound Med 2003; 22:1116–25. 12. Dogan Y, Yuksel A, Kalelioglu IH, Has R, Tatl› B, Yildirim A. Intracranial ultrasound abnormalities and fetal cytomegalovirus ›nfection: report of 8 cases and review of the literature. Fetal Diagn Ther 2011;30:141–9. 13. Zivkoviç T, Ivoviç V, Vujaniç M, Klun I, Bobiç B, Nikoliç A, et al. Adverse fetal outcome in the absence of timely prenatal diagnosis of congenital toxoplasmosis. Wien Klin Wochenschr 2011;123;43–6. 14. Dommergues M, Mahieu-Caputo D, Fallet-Bianco C, Mirlesse V, Aubry MC, Delezoide AL, et al. Fetal serum interferon-alpha suggests viral infection as the aetiology of unexplained lateral cerebral ventriculomegaly. Prenat Diagn 1996;16:883–92. 15. Pilu G, Falco P, Gabrielli S, Perolo A, Sandri F, Bovicelli L. The clinical significance of fetal isolated cerebral borderline ventriculomegaly: report of 31 cases and review of the literature. Ultrasound Obstet Gynecol 1999;14:320–6. 16. Gaglioti P, Danelon D, Bontempo S, Mombrò M, Cardaropoli S, Todros T, et al. Fetal cerebral ventriculomegaly: outcome in 176 cases. Ultrasound Obstet Gynecol 2005;25:372–7. 17. den Hollander NS, Vinkesteijn A, Schmitz-van Splunder P, Catsman-Berrevoets CE, Wladimiroff JW. Prenatally diagnosed fetal ventriculomegaly: prognosis and outcome. Prenat Diagn 1998;18:557–66. 18. Pilu G, Hobbins JC. Sonography of fetal cerebrospinal anomalies. Prenat Diagn 2002;22:321–30. 19. Nicolaides KH, Berry S, Snijders RJM, Thorpe-Beeston JG, Gosden C. Fetal lateral cerebral ventriculomegaly: associated malformations and chromosomal defects. Fetal Diagn Ther 1990;5:5–14. 20. Melchiorre K, Bhide A, Gika AD, Pilu G, Papageorghiou AT. Counseling in isolated mild fetal ventriculomegaly. Ultrasound Obstet Gynecol 2009;34:212–24. 21. Gezer C, Ekin A, Özeren M, Taner CE, Özer Ö, Koç A, et al. Fetal serebral ventikülomegalide kromozomal anomali s›kl›¤›. Perinatoloji Dergisi 2013;21 Suppl 1:S32. 22. Sezik M. Ventrikülomegali ve atriyoventriküler septal defekt: Tip 2 triploidi. Perinatoloji Dergisi 2013;21 Suppl 1:S39. 23. Kara M. Prenatal 47 XXY sendromu ve ventrikülomegali birlikteli¤i: Vaka sunumu. Bozok T›p Dergisi 2012;1:53–6. 24. Breeze ACG, Alexander PMA, Murdoch EM, MissfelderLobos HH, Hackett GA, Lees CC. Obstetric and neonatal outcome in severe ventriculomegaly. Prenat Diagn 2007;27: 124–9. 25. Morris JE, Rickard S, Paley MNJ, Griffiths PD, Rigby A, Whitby EH. The value of in-utero magnetic resonance imaging in ultrasound diagnosed foetal isolated cerebral venticulomegaly. Clin Radiol 2007;62:140–4. 26. Romero R, Pilu G, Jeanty P, Ghidini A, Hobbins JC. The central nervous system. Prenatal Diagnosis of Congenital Anomalies. East Norwalk, CT: Appleton & Lange; 1988. p. 1–79. 27. Tatl› B, Özer I, Ekici B, Kalelio¤lu I, Has R, Eraslan E, et al. Neurodevelopmental outcome of 31 patients with borderline fetal ventriculomegaly. Clinical Neurol Neurosurg 2012; 114;969–71. 28. Levine D, Barnes PD, Robertson RR, Wong G, Mehta T. Fast MR imaging of fetal central nervous system abnormalities. Radiology 2003;229:51–61. 29. Gezer NS, Güleryüz H, Gezer C, Koçyi¤it A, Yeflil›rmak CD, Güçlü S, et al. Fetal manyetik rezonans görüntüleme ile yap›lan beyin hacim ölçümlerinin ventrikülomegali ile iliflkisi. Perinatoloji Dergisi 2013;21 Suppl 1:S35. 30. Benaceraf BR, Shipp TD, Bromley B, Levine D. What does magnetic resonance imaging add to the prenatal sonographic diagnosis of ventriculomegaly? J Ultrasound Med 2007;26: 1513–22. 31. Manganaro L, Savelli S, Francioso A, Di Maurizio M, Coratella F, Vilella G, et al. Role of fetal MRI in the diagnosis of cerebral ventriculomegaly assessed by ultrasonography. Radiol Med 2009;114:1013–23. 32. Devaseelan P, Cardwell C, Bell B, Ong S. Prognosis of isolated mild to moderate fetal cerebral ventriculomegaly: a systematic review. J Perinat Med 2010;38:401–9. 33. Lyall AE, Woolson S, Wolfe HM, Goldman BD, Reznick JS, Hamer RM, et al. Prenatal isolated mild ventriculomegaly is associated with persistent ventricle enlargement at ages 1 and 2. Early Hum Dev 2012;88;691–8. Volume 23 | Issue 1 | April 2015 5 AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):6–12 R N A PE IN AT U AL JO R Perinatal outcomes of patients diagnosed borderline gestational diabetes mellitus Gök Özgül1, Rauf Meleko¤lu2, Sevda Yeleç1, ‹pek Eskiyörük1, Fatma Tuncay Özgünen1 1 Department of Gynecology & Obstetrics, Faculty of Medicine, Çukurova University, Adana, Turkey 2 Department of Gynecology & Obstetrics, Faculty of Medicine, Inönü University, Malatya, Turkey Abstract Özet: Borderline gestasyonel diabetes mellitus saptanan gebelerin perinatal sonuçlar› Objective: Although the effects of gestational diabetes mellitus to maternal and fetal health are well known, we have few data about maternal and fetal condition of borderline gestational diabetic pregnants who have gestational hyperglycemia not meeting gestational diabetes criteria. Considering this, we aimed to investigate perinatal and neonatal outcomes of patients who have borderline gestational diabetes mellitus in our hospital. Methods: In this study, we retrospectively examined maternal characteristics, obstetric and perinatal outcomes of pregnants whose antenatal follow-up and birth occurred in Department of Obstetrics and Gynecology in Faculty of Medicine in Çukurova University between January 2009 and January 2013 and who have normal 50g oral glucose tolerance test (OGTT) but abnormal 100-g OGTT and have normal 50-g OGCT test results. SPSS v. 19.0 statistics software was used for data analysis. For the statistical significance level between results, p value was taken as <0.05. Results: A total of 239 pregnant women were included in the study. The study group consisted of 105 pregnant women whose 50-g OGTT results were abnormal but 100-g OGTT results were within normal limits and the control group consisted of 134 pregnant women whose 50-g OGTT results were within normal limits. Compared to healthy pregnant women, mean age of the women in the study group was found to be significantly higher (p=0.000). The duration of hospitalization in the study group was found to be statistically significantly higher compared to the control group (p=0.001). Mode of delivery, preterm labor, premature rupture of membranes, gestational hypertension, preeclampsia, the presence of fetal distress and postpartum hemorrhage were analyzed in both groups. Only postpartum hemorrhage was found to be statistically significantly higher in the study group compared to the control group (p=0.049). There was statistically no significant difference in neonates between two groups for LGA, SGA, hypoglycemia, hyperbilirubinemia, neonatal admissions to the intensive care unit and neonatal death. Conclusion: In our study, perinatal and neonatal outcomes of patients who have borderline gestational diabetes mellitus and normoglisemic condition are same except postpartum hemorrhage and hospitalization period. To acquire perinatal and neonatal outcomes of women with borderline gestational diabetes mellitus, we need further well-designed randomized studies with larger populations. Amaç: Çal›flman›n amac› gestasyonel diyabetin fetal ve maternal sa¤l›¤a etkileri oldukça iyi bilinmesine ra¤men, gestasyonel diyabet kriterlerini karfl›lamayan gebelik hiperglisemisine sahip borderline gestasyonel diyabeti olan gebelerin maternal ve fetal durumunu ortaya koyan az say›da çal›flma olmas›n› göz önünde bulundurarak, hastanemizdeki borderline gestasyonel diyabeti olan hastalar›n perinatal ve neonatal sonuçlar›n› irdelemektir. Yöntem: Bu çal›flmada Ocak 2009 ve Ocak 2013 tarihleri aras›nda Çukurova Üniversitesi T›p Fakültesi Kad›n Hastal›klar› ve Do¤um Anabilim Dal› Gebe Poliklini¤inde antenatal izlemleri yap›lan ve do¤umlar› klini¤imizde gerçekleflen gebeler aras›ndan 50 g OGTT sonuçlar› yüksek ancak 100 g OGTT sonuçlar› normal olan hastalar ile 50 g OGTT sonuçlar› normal olan hastalar tespit edilerek, maternal özellikleri, obstetrik ve perinatal sonuçlar› retrospektif olarak incelendi. Verilerin analizi için SPSS v 19.0 paket program› kullan›ld›. Sonuçlar aras›nda istatistiksel anlaml›l›k düzeyi için p de¤eri <0.05 olarak al›nd›. Bulgular: Çal›flmaya toplamda 239 gebe dahil edildi. 50 g OGTT sonuçlar› yüksek ancak 100 g OGTT sonuçlar› normal s›n›rlarda olan 105 gebe çal›flma grubunu, 50 g OGTT sonuçlar› normal olan 134 gebe ise kontrol grubunu oluflturdu. Çal›flma grubundaki gebelerin yafl ortalamalar›n›n sa¤l›kl› gebelere oranla istatistiksel olarak anlaml› derecede yüksek oldu¤u saptand› (p=0.000). Çal›flma grubundaki gebelerin hastanede yat›fl sürelerinin kontrol grubundakilere oranla istatistiksel olarak anlaml› oranda daha fazla oldu¤u saptand› (p=0.001). Her iki grubun do¤um flekli, erken do¤um, erken membran rüptürü, gestasyonel hipertansiyon, preeklampsi varl›¤›, fetal distres varl›¤› ve postpartum kanama aç›s›ndan obstetrik sonuçlar› incelendi. Sadece postpartum kanaman›n kontrol grubuna göre çal›flma grubunda istatistiksel olarak anlaml› derecede fazla oldu¤u saptand› (p=0.049). Yenido¤an bebeklerde LGA, SGA, hipoglisemi, hiperbilirubinemi, yenido¤an yo¤un bak›m ünitesine yat›fl ve neonatal ölüm görülme oranlar› aras›nda da her iki grup aras›nda istatistiksel olarak anlaml› fark saptanmad›. Sonuç: Çal›flmam›zda borderline gestasyonel diyabeti olan hastalar›n postpartum kanama s›kl›¤› ve hastanede yat›fl süreleri d›fl›nda perinatal ve neonatal sonuçlar› normoglisemik gebeler ile benzer saptanm›flt›r. Keywords: Gestational diabetes, glucose tolerance test, pregnancy outcomes. Anahtar sözcükler: Gestasyonel diyabet, glukoz tolerans testi, gebelik sonuçlar›. Correspondence: Rauf Meleko¤lu, MD. ‹nönü Üniversitesi T›p Fakültesi Kad›n Hastal›klar› ve Do¤um Anabilim Dal›, Malatya, Turkey. e-mail: rmelekoglu@gmail.com Received: November 17, 2014; Accepted: November 30, 2014 Please cite this article as: Özgül G, Meleko¤lu R, Yeleç S, Eskiyörük ‹, Tuncay Özgünen F. Perinatal outcomes of patients diagnosed borderline gestational diabetes mellitus. Perinatal Journal 2015;23(1):6–12. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231002 doi:10.2399/prn.15.0231002 QR (Quick Response) Code: Perinatal outcomes of patients diagnosed borderline gestational diabetes Introduction Gestational diabetes mellitus (GDM) is defined as the “carbohydrate intolerance occurring or found for the first time during pregnancy”.[1] Pregnancy is characterized by insulin resistance and hyperinsulinemia. This may be predisposing for pregnant women to develop diabetes. This resistance is caused by the influence of some diabetogenic placental secretion hormones (growth hormone, corticotropin releasing hormone, placental lactogenic hormone, progesterone etc). Decreased exercise, increased caloric intake and increased adiposis tissue amount are also among the reasons of insulin resistance. Gestational diabetes is seen in women who have insufficient pancreatic functions and do not have insulin release sufficient enough to tolerate diabetogenic hormone change.[2] It is recommended to all pregnant women to have 50-g oral glucose tolerance test (OGTT) for gestational diabetic screening between 24 and 28 weeks of gestation.[3] If the result is above 140 mg/dl, patient is referred to 100-g OGTT. For GDM diagnosis, at least two threshold values of 100-g OGTT should be met or exceeded. However, there is also a major patient group who has positive result for 50-g OGTT but normal result for 100-g OGTT. Although the effects of gestational diabetes mellitus to maternal and fetal health are well known, maternal and fetal conditions of borderline gestational diabetic women who are between normal glucose values and gestational diabetic levels. Some studies in the literature point out that the pregnant women with normal 100-g OGTT results despite high 50-g OGTT results may have different maternal characteristics compared to normal pregnant women and may have more risks in terms of adverse obstetric outcomes.[4] This group is called as “borderline GDM”. In our study, we aimed to analyze retrospectively the pregnant women with normal 100-g OGTT results despite high 50-g OGTT results and the pregnant women with normal 50-g OGTT results among the cases who were followed up and delivered at the Department of Gynecology & Obstetrics, Faculty of Medicine, Çukurova University between January 2009 and January 2013, and to investigate and compare their maternal characteristics and obstetric and perinatal outcomes. Methods This study includes 239 pregnant women who had their antenatal follow-ups and deliveries at the Department of Gynecology & Obstetrics, Faculty of Medicine, Çukurova University between January 2009 and January 2013 in accordance with the follow-up and delivery protocols prepared in compliance with the Prenatal Care Management Guide and Delivery and Cesarean Labor Management Guide of the Health Ministry, and their babies. The approval of the Ethics Committee of Faculty of Medicine, Çukurova University was obtained before the study. Also, in compliance with the Helsinki Declaration Principles, all women included in the study were informed in written and verbally about the study and their informed consents were received. The study group consisted of 105 pregnant women who were at 24-28 weeks of gestation, undergone GDM screening and had normal results for 100-g OGTT despite the high results for 50-g OGTT (those having all values below the threshold value of 100-g OGTT and those with single high value), and the control group consisted of 134 pregnant women who delivered at the same period and had normal results for 50-g glucose screening test performed at 24-28 weeks of gestation. Pregnant women below 18-year-old and above 35year-old, multipara pregnant women, those with multiple pregnancies, presence of major fetal anomaly in fetus and of maternal chronic diseases (such as chronic hypertension, diabetes mellitus, chronic renal failure asthma, pulmonary or cardiac diseases etc.), patients with maternal thrombophilia history and pregnant women who undergone labor induction were excluded from the study. In our clinic, we perform 50-g OGTT to pregnant women, who admit to follow-up clinics between 24 and 28 weeks of gestation, by orally administering 50 g glucose dissolved in 200 ml water. One hour after patient receives glucose solution, venous blood sample is collected from patient and plasma glucose levels are measured spectrophotometrically via oxidase method by using Roche diagnostic kits on Roche/Hitachi (Roche Diagnostics Corp., Indianapolis, IN, USA) device in biochemistry laboratory. Those with blood glucose levels: • Below 140 mg/dl are considered as normal • Above 200 mg/dL are considered as directly GDM • For those with a value between >140 mg and <200 mg, OGTT is carried out with 100 g glucose after 8-14 of fasting. During this test, venous blood samVolume 23 | Issue 1 | April 2015 7 Özgül G et al. ple is collected from patient for fasting blood glucose first and after 100 g glucose dissolved in 200 ml is administered to patient, venous blood samples are collected first, second, and third hours, and the samples are analyzed in biochemistry laboratory. GDM diagnosis is established when at least two threshold values used by National Diabetes Data Group are met or exceeded (fasting: 105, first hour: 190, second hour: 165, third hour: 145). The patients who were included in the study were retrospectively recorded and compared in terms of demographical data such as age, weight, body mass index, smoking habit, gestational age, blood pressure data during the referral for delivery; perinatal data such as preterm labor as a perinatal outcome (delivery before 37+0 weeks of gestation), pregnancy induced hypertension (hypertension developed without proteinuria after 20 weeks of gestation), presence of preeclampsia (hypertension developed with proteinuria after 20 weeks of gestation), delivery type (vaginal delivery/cesarean), presence of cesarean, shoulder dystocia and postpartum hemorrhage due to fetal distress (≥500 ml blood loss through genital tract after delivery), hospitalization period; and neonatal data such as APGAR score, head circumference, gender, LGA rates according to gestational age [birth weight being ≥90 p according to gestational age], SGA rates according to gestational age [birth weight being ≤10 p according to gestational age], neonatal hypoglycemia (blood glucose below 40 mg/dl regardless of birth weight and gestational week), nenonatal hyperbilirubinemia (blood bilirubin levels being at pathological levels according to gestational age, weight and gender), newborn intense care need and neonatal mortality rates of babies born in both groups. SPSS ver. 19.0 software was used for the statistical analysis of the data. Categorical measurements were summarized as figures and percentages while constant measurements were indicated as mean and standard deviation. The distributions were checked in the comparison of constant measurements among groups; t-test for two independent samples was used for variables displaying parametric distribution while Mann-Whitney U test was used for variables not displaying parametric distribution. Either chi-square test or Fisher’s test statistics was used for the comparison of categorical variables such as smoking habit and gender. In all tests, p<0.05 was considered statistically significant. 8 Perinatal Journal Results A total of 239 pregnant women were included in the study. While mean age of the pregnant women in the study group was 31.5±5.1, it was 28.9±4.4 in the control group (p=0.000). It was found that the mean age of pregnant women in the study group was statistically and significantly higher than the mean age of healthy pregnant women. There was statistically no significant difference between the groups in terms of gravida, parity, gestational week, weight, blood pressure, presence of poor obstetric history and smoking habit. When the groups were evaluated in terms of postnatal hospitalization period, it was seen that hospitalization period of the pregnant women in the study group was 1.7±0.6 days while it was 1.5±0.5 days in the control group (p=0.001). The hospitalization period of the pregnant women in the study group was statistically and significantly higher than those in the control group. The distribution of the patients in study and control groups by demographic characteristics is shown in the Table 1. While 54.3% of the pregnant women in the study group had delivered by cesarean, 45.7% of them delivered vaginally. While cesarean rate in the control group was 44%, the rate of vaginal delivery was 56%. There was statistically no significant difference between the groups in terms of delivery types (p=0.116). Preterm labor, premature rupture of membranes, gestational hypertension, presence of preeclampsia and fetal distress, and obstetric outcomes in terms of postpartum Table 1. Distribution of demographic characteristics according to the groups. Study group (Mean±SD) Control group (Mean±SD) p 0.000 Age 31.5±5.1 28.9±4.4 Weight 79.6±11.5 77.6±10.9 0.180 Gravida 2.7±1.2 2.7±1.4 0.913 0.534 Parity 1.3±0.6 1.2±0.8 Systolic blood pressure 114.3±13.6 112.1±12.2 0.188 Diastolic blood pressure 71.9±9.5 70.2±9.6 0.181 Week of gestation 38.4±1.7 38.3±1.5 0.556 Hospitalization 1.7±0.6 1.5±0.5 0.003 n (%) n (%) p Smoking habit 4 (3.8) 1 (0.7) 0.101 Poor obstetric history 4 (3.8) 10 (7.5) 0.234 Perinatal outcomes of patients diagnosed borderline gestational diabetes hemorrhage were evaluated. It was found that only postpartum bleeding was statistically and significantly higher in the study group compared to the control group (p=0.049). The distribution of obstetric outcomes in both groups is shown in the Table 2. Newborn follow-up forms of 234 pregnant women included in the study were analyzed and neonatal data were collected. The newborns in both groups were compared in terms of birth weights, head circumference measurements and gender distributions, and statistically no significant difference was found (p=0.188, p=0.670, p=0.958, respectively). While the 1-minute APGAR score of 14.2% of the newborns in the study group was below 7, it was 12.6% in the control group. The percentage of those with 5minute APGAR score below 7 was 2% in the study group while it was 2.9% in the control group. No statistically significant difference was found between two groups in terms of APGAR scores (p=0.815, p=0.599, respectively). No statistically significant difference was seen between the newborns of two groups in terms of LGA, SGA, hypoglycemia, hyperbilirubinemia, hospitalization at newborn intense care unit and neonatal mortality rates. The distribution of neonatal outcomes in both groups is shown in the Table 3. Table 2. Distribution of the obstetric outcomes according to the groups. Preterm labor Premature rupture of membranes Study group n (%) Control group n (%) p 4 (3.8) 9 (6.7) 0.327 13 (12.4) 8 (6) 0.083 Gestational HT 5 (4.8) 4 (3) 0.476 Preeclampsia 2 (1.9) 5 (3.7) 0.408 Fetal distress 4 (3.8) 2 (1.5) 0.258 Postpartum hemorrhage 3 (2.9) 0 (0) 0.049 Cesarean 57 (54.3) 59 (44) 0.116 Normal delivery 48 (45.7) 75 (56) 0.116 Delivery type According to the results of few studies, many obstetricians define cases, who have positive results for 50-g OGTT but normal results for 100-g OGTT, as glucose intolerant or borderline gestational diabetics and recommend more frequent follow-up.[9] Yee et al. reported advanced maternal age, multiparity and being of Asian or Latin American ethnicity as the risk factors for having abnormal results of glucose tolerance test in the absence of GDM.[10] In our study, we compared the cases in the study group who had high results in 50-g OGTT but normal results in 100-g OGTT with the cases in the control group and found that the age was Discussion GDM prevalence increases in the world and it affects 1-14% of the pregnancies. Estimated GDM prevalence is 1.4-2.8% in a low-risk population, 3.3-6.1% in a riskier population, and it may be more than 10% in high-risk population.[5] There are less data about the gestational hyperglycemia prevalence not meeting the criteria of gestational diabetes mellitus. The data received from the Australian studies showed that 7% of all pregnant women have hyperglycemia not meeting GDM criteria while 5.5-8.8% of them already have GDM every year.[6,7] There is no sufficient study in terms of blood glucose follow-ups of this group, how to follow up them and perinatal outcomes. Stamilio et al. confirms that the positivity of 50-g OGTT is an independent risk factor in terms of perinatal complications and indicates that these cases may more frequently benefit from fetal monitorization, nutritional consultation or diabetic diet.[8] Table 3. Distribution of the neonatal outcomes according to the groups . Study group Control group (Mean±SD) (Mean±SD) Birth weight of neonatal p 3224.7±446.0 3142.7±498.7 0.188 Head circumference of neonatal 34.4±1.5 34.3±1.9 0.670 n (%) n (%) p 1-minute APGAR score <7 15 (14.2) 17 (12.6) 0.815 5-minute APGAR score >7 3 (2) 4 (2.9) 0.599 Male 56 (53.3) 71 (53) 0.958 Female 49 (46.7) 63 (47) 0.958 SGA 2 (1.9) 7 (5.2) 0.182 LGA 2 (1.9) 5 (3.7) 0.408 Neonatal hypoglycemia 3 (2.9) 1 (0.7) 0.208 Hyperbilirubinemia 2 (1.9) 1 (0.7) 0.427 Hospitalization at newborn intense care unit 9 (8.6) 16 (11.9) 0.400 1 (1) 1 (0.7) 0.259 Gender Neonatal death Volume 23 | Issue 1 | April 2015 9 Özgül G et al. statistically and significantly high in the study group compared to the control group.[9,11–13] Gestational hyperglycemia not meeting the criteria of gestational diabetes mellitus is associated with a series of known health risks. It is known that the insulin resistance which is characteristics for the occurrence of GDM is also associated with the development of preeclampsia.[14] In their multi-central multi-ethnical cohort study (HAPO study), Metzger et al. evaluated 25,505 women in terms of effects of maternal hyperglycemia on gestational outcomes and reported that there was a linear association between preeclampsia prevalence and the results of glucose tolerance test.[6] In our study, we found statistically no significant difference between the study group and the control group in terms of the gestational hypertension and preeclampsia incidence. Preterm labor is defined as the deliveries occurring before 37 weeks of gestation are completed. GDM and especially pregestational DM are known risk factors for preterm labor. Beigelman et al. found preterm labor rate as 10% in the study conducted on 3841 pregnant women with GDM.[15] In our study, although preterm labor rate was found at a lower rate in the study group than the control group, there was no statistically significant difference between the groups. Maternal diabetes is a risk factor for cesarean delivery. Cesarean delivery rate varies from 25% up to 80% in diabetic women. Many factors such as diabetic complications including prematurity, macrosomia and nephropathy are associated with high cesarean rates.[16] In their studies, Stamilio et al. observed statistically higher cesarean rate in cases with high results for 5 g glucose tolerance test but normal results for 100-g OGTT compared to the cases with normal results for 50-g OGTT.[8] Dudhbhai et al. found no significant difference between borderline diabetic pregnant women and the control group in terms of the cesarean rates.[13] Hong et al. investigated demographical characteristics and obstetric and neonatal outcomes of patients with borderline gestational diabetes, and found that the cesarean rate due to fetal distress was higher in this group than the normoglycemic pregnant women.[17] In our study, although we found cesarean rates higher in the study group, there was no statistically significant difference between two groups. We also did not see any statistically significant difference between two groups in terms of the cesarean delivery carried out due to fetal distress. The conditions such as episiotomy extension during vaginal delivery, vaginal laceration and postpartum 10 Perinatal Journal atonia are observed more frequently in those who deliver large baby. Jastrow et al. reported that the risks for cephalopelvic disproportion, uterine rupture, shoulder dystocia, perineal laceration and postpartum hemorrhage due to LGA or macrosomic baby risk are higher in mothers with maternal hyperglycemia.[18] In our study, the postpartum hemorrhage rate was statistically and significantly higher in the study group than the control group. We found that the most frequent reasons for postpartum hemorrhage seen in the study group were uterine atony followed by delivery tract lacerations and rest placenta induced hemorrhage. When we compared the groups in terms of maternal hospitalization periods, we found that the mothers in the study group had statistically and significantly longer hospitalization periods than the mothers in the control group. In their study, Hong et al. reported statistically no significant difference between control group and the study group with patients having borderline DM.[17] Long hospitalization periods of the patients in our study group may be due to the high cesarean rates and postpartum hemorrhage rates. Figueroa et al. indicated in their studies that LGA and macrosomia rates of the patients with borderline gestational diabetes increased 2 and 1.6 times, respectively.[19] In the study of Bonomo et al., the authors suggested that even the slight changes in glucose intolerance may cause overgrowth in babies.[20] From 20% up to 40% of diabetic mothers are over 90th percentile in birth weight according to the gestation. In our study, we found statistically no significant difference between the groups despite the high rates of birth weight in the study group compared to the control group. Birth traumas, increased preterm labor rates, obstetric conditions such as preeclampsia, and various metabolic disorders depending on the maternal diabetes cause low APGAR scores and high level of intense care needs in babies of diabetic mothers.[21] Although Hong et al. found statistically no significant difference between 1-minute and 5-minute APGAR scores in patients with high results for 50-g OGTT but normal results for 100-g OGTT, they reported statistically and significantly higher rates for newborn intense care and hospitalization periods in newborns in this group.[17] We, on the other hand, found statistically no significant difference between the groups in terms of 1-minute and 5-minute APGAR scores, newborns’ intense care needs and neonatal mortality rates. Perinatal outcomes of patients diagnosed borderline gestational diabetes Dodd et al. carried out a study by using the data of 16,975 women who delivered in tertiary healthcare organizations in Australia between 1993 and 2003, and they found that the patients with borderline GDM had risks for preeclampsia and cesarean and when compared to the babies of mothers with normal results for glucose tolerance test, they indicated that the babies of these patients had increased risks for hypoglycemia and hyperbilirubinemia.[7] We did not observe statistically any significant difference between two groups in terms of neonatal hypoglycemia, hyperbilirubinemia, and SGA and LGA baby rates. We believe that the reason is low numbers of patients in the study and control group, and non-availability of detailed neonatal information in the patient files analyzed retrospectively. Conclusion Gestational hyperglycemia not meeting the criteria of gestational diabetes mellitus affects a great number of pregnant women. Hyperglycemia seen during pregnancy is associated with a series of negative gestational outcomes including preeclampsia, delivery trauma and type II DM development in mother, and future obesity, type I and type II DM development in baby. While we do not have certain threshold values to be categorized for establishing GDM diagnosis, the values for upper limit to initiate the treatment in order to keep blood glucose within normal limits in case of gestational hyperglycemia are also unclear. In our study, except postpartum hemorrhage rate and hospitalization periods of the patients with gestational diabetes, the perinatal and neonatal outcomes were similar with the outcomes of normoglycemic pregnant women. While there are researchers recommending to refer patients with gestational hyperglycemia not meeting GDM and type II DM diagnosis criteria to dieticians and to carry out blood glucose monitorization and follow-ups more frequently, there are also researchers who assert that such approaches would increase labor induction and cesarean rates, would raise healthcare costs due to frequent examinations and investigations but not create any significant difference in maternal and neonatal outcomes. Our knowledge on this issue is based on limited number of randomized studies. In order to make precise recommendations for the management of such patients, we need further welldesigned randomized studies with larger population. Conflicts of Interest: No conflicts declared. References 1. Committee opinion no. 504: Screening and diagnosis of gestational diabetes mellitus. Obstet Gynecol 2011;118:751–3. 2. Gabbe SG, Niebyl JR, Galan HL, Jauniaux ERM, Landon MB, Simpson JL, Driscoll DA. Diabetes Mellitus Complicating Pregnancy. Obstetrics: Normal and Problem Pregnancies. 6th ed. Philadelphia: Saunders; 2012. p: 902–4. 3. Practice Bulletin No. 137. Gestational diabetes mellitus. Obstet Gynecol 2013;122(2 Pt 1):406–16. 4. Han S, Crowther CA, Middleton P. Interventions for pregnant women with hyperglycaemia not meeting gestational diabetes and type 2 diabetes diagnostic criteria. Cochrane Database Syst Rev 2012;1:CD009037. 5. Mulla WR, Henry TQ, Homko CJ. Gestational diabetes screening after HAPO: has anything changed? Curr Diab Rep 2010;10:224–8. 6. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 2008;358:1991–2002. 7. Dodd JM, Crowther CA, Antoniou G, Baghurst P, Robinson JS. Screening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomes. Aust N Z J Obstet Gynaecol 2007;47:307–12. 8. Stamilio DM, Olsen T, Ratcliffe S, Sehdev HM, Macones GA. False-positive 1-hour glucose challenge test and adverse perinatal outcomes. Obstet Gynecol 2004;103:148–56. 9. Edelman D, Olsen MK. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010;33(Suppl 1):S62–S9. 10. Yee LM, Cheng YW, Liddell J, Block-Kurbisch IB, Caughey AB. 50-Gram glucose challenge test: is it indicative of outcomes in women without gestational diabetes mellitus? J Matern Fetal Neonatal Med 2011;24:1102–6. 11. Gumus II, Turhan NO. Are patients with positive screening but negative diagnostic test for gestational diabetes under risk for adverse pregnancy outcome? J Obstet Gynaecol Res 2008;34:359–63. 12. Gezer A, Esen F, Mutlu H, Oztürk E, Ocak V. Prognosis of patients with positive screening but negative diagnostic test for gestational diabetes. Arch Gynecol Obstet 2002;266: 201–4. 13. Dudhbhai M, Lim L, Bombard A, Jullard K, Meenakshi B, Trachelenberg Y, et al. Characteristics of patients with abnormal glucose challenge test and normal oral glucose tolerance test results: comparison with normal and gestational diabetic patients. Am J Obstet Gynecol 2006;194:e42–5. 14. Wolf M, Sandler L, Munoz K, Hsu K, Ecker JL, Thadhani R. First trimester insulin resistance and subsequent preeclampsia: a prospective study. J Clin Endocrinol Metab 2002;87:1563–8. 15. Beigelman A, Wiznitzer A, Shoham-Vardi I, Vardi H, Holtcberg G, Mazor M. Premature delivery in diabetes: etiology and risk factors. Harefuah 2000;138:919–23. Volume 23 | Issue 1 | April 2015 11 Özgül G et al. 16. James DK, Steer P, Weiner C, Gonik B, Crowther C, Robson S, et al. Pregnancy and laboratory studies: a reference table of clinicians. Obstet Gynecol 2010;115:868. 17. Ju H, Rumbold AR, Willson KJ, Crowther CA. Borderline gestational diabetes mellitus and pregnancy outcomes. BMC Pregnancy Childbirth 2008;8:31. 18. Jastrow N, Roberge S, Gauthier RJ, Laroche L, Duperron L, Brassard N, et al. Effect of birth weight on adverse obstetric outcomes in vaginal birth after cesarean delivery. Obstet Gynecol 2010;115(2 Pt 1):338–43. 19. Figueroa D, London MB, Mele L, Spong CY, Ramin SM, Casey B, et al. Relationship between 1-hour glucose chal- 12 Perinatal Journal lenge test results and perinatal outcomes. Obstet Gynecol 2013;121:1241–7. 20. Bonomo M, Cetin I, Pisoni MP, Faden D, Mion E, Taricco E, et al. Flexible treatment of gestational diabetes modulated on ultrasound evaluation of intrauterine growth: a controlled randomized clinical trial. Diabetes Metab 2004;30:237–44. 21. Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS; Kaiser Permanente of Colorado GDM Screening Program. Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care 2005;28:579–84. AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):13–19 R N A PE IN AT U AL JO R Health practices of pregnant women in Gumushane City Center Handan Özcan1, Nezihe K›z›lkaya Beji2 1 Vocational Health High School, Gumushane University, Gumushane, Turkey Department of Women Health and Diseases Nursing, Florence Nightingale Faculty of Nursing, Istanbul University, Istanbul, Turkey 2 Abstract Özet: Gümüflhane il merkezindeki gebelerin sa¤l›k uygulamalar› Objective: The study aimed to investigate the health practices of pregnant women living in Gumushane city center, and to increase awareness among pregnant women. Amaç: Çal›flma, Gümüflhane il merkezinde yaflayan gebelerin sa¤l›k uygulamalar›n› araflt›rmak ve gebelerin fark›ndal›klar›n› artt›rmak amac›yla planlanm›flt›r. Methods: The research is of definitive characteristics. It was conducted with a total of 189 pregnant women between October 1st and December 10th, 2012. The data was provided as figure, percentage, arithmetic mean and standard deviation. After normality analyses were applied to the data, Mann-Whitney U test, one-way analysis of variance (ANOVA) test and post hoc analyses to determine the source of difference were carried out. Yöntem: Araflt›rma tan›mlay›c› niteliktedir. 1 Ekim – 10 Aral›k 2012 tarihleri aras›nda toplam 189 gebeyle gerçeklefltirilmifltir. Veriler; say›, yüzde, aritmetik ortalama ve standart sapma ile verilmifltir. Verilere normallilik analizleri uygulamas› sonras› MannWhitney U testi, tek yönlü varyans analizi (ANOVA) testi, farkl›l›klar›n kayna¤›n› belirlemek amac›yla post hoc analizler yap›lm›flt›r. Results: The ages of pregnant women are between 19- and 48-yearold, and the mean age is 29.09±5.5. Of the participants, 65.1% of them stated that their expenses were equal to their incomes, 8.58% of them had no social security, 24.6% of them had a job, and 51.3% of them were living in the city center. Statistically significant difference was found in the ANOVA test analysis carried out among the score averages of the “Health Practices Questionnaire” according to the educational background of the spouses of the pregnant women. Difference was found between primary school and university graduates. Score average of the “Health Practices Questionnaire” for those living in metropolises was higher than those living in villages; it was found that the score average of the questionnaire decreased as the age increased. Bulgular: Gebelerin yafllar› 19–48 yafl aral›¤›nda olup, ortalama 29.09±5.5’dir. Kat›l›mc›lar›n %65.1’i gelirlerinin giderlerine eflit oldu¤unu, %8.58’inin sosyal güvencesi olmad›¤›n›, %24.6’s› çal›flt›¤›n›, %51.3’ü il merkezinde yaflad›¤›n› söyledikleri tespit edilmifltir. Gebelerin efllerinin e¤itim düzeylerine göre ‘Gebelikte Sa¤l›k Uygulamalar› Ölçek’ puan ortalamalar› aras›nda yap›lan ANOVA testi analizinde istatistiksel aç›dan anlaml› fark elde edilmifltir. ‹lkokul ve üniversite mezunlar› aras›nda farkl›l›k oldu¤u saptanm›flt›r. Büyük flehirlerde yaflayanlar›n ‘Gebelikte Sa¤l›k Uygumalar› Ölçek’ puan ortalamas›, köylerde yaflayanlardan daha yüksek bulunmufl ve yafl›n artmas› ile ölçek puan ortalamas› da düflmektedir. Conclusion: For the health practices during pregnancy, the ages of pregnant women and their spouses and living in whether in urban or rural areas caused differences. It is required to extend “prenatal and postnatal training programs” among pregnant women and their families, to enable the spouses of pregnant women to join such programs by informing them, to carry out detailed interviews in order to evaluate and modify the practices of pregnant women in advanced age group, and to increase awareness on this subject matter. Keywords: Pregnancy, health behavior, education. Sonuç: Gebelikte sa¤l›k uygulamalar›nda; gebenin kendisinin ve eflinin yafllar›n›n, yaflad›¤› alan›n kentsel ya da k›rsal olmas›n›n farkl›l›klara sebep oldu¤u görülmüfltür. Gebelere ve ailelerine yönelik “prenatal ve postnatal e¤itim programlar›n›n” yayg›nlaflt›r›lmas›, gebelerin efllerinin de bilgilendirilerek bu programlara kat›l›m›n›n sa¤lanmas›, ileri yafl grubundaki gebelerin uygulamalar›n›n de¤erlendirilmesi ve düzeltilmesi ad›na ayr›nt›l› görüflmelerin yap›lmas› ve bu konuda fark›ndal›klar›n›n artt›r›lmas› gerekmektedir. Anahtar sözcükler: Gebelik, sa¤l›k davran›fl›, e¤itim. Correspondence: Handan Özcan, MD. Gümüflhane Üniversitesi Sa¤l›k Hizmetleri Meslek Yüksekokulu, Gümüflhane, Turkey. e-mail: hndnozcn@hotmail.com Received: April 7, 2014; Accepted: December 1, 2014 Please cite this article as: Özcan H, K›z›lkaya Beji N. Health practices of pregnant women in Gumushane City Center. Perinatal Journal 2015;23(1):13–19. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231003 doi:10.2399/prn.15.0231003 QR (Quick Response) Code: Özcan H, K›z›lkaya Beji N Introduction According to the data of TNSA-2008, a woman who reaches at the end of her fertility age in Turkey gives 2.16 births on average. Total fertility rate today is 50% lower than the rate in 1970s. In Turkey, fertility piles up in the age group 20–29. An average woman has her first child at 25-year-old, and two children at 30-year-old. Fertility period diminishes swiftly after 30-year-old, and reaches a negligible level at 40s.[1] Health practices of women during pregnancy affect both maternal and neonatal health both during pregnancy and postpartum period. Health practices during pregnancy can be defined as the activities including the health of pregnant woman, fetus and newborn and affecting the gestational outcome. Health practices which are significant for gestational outcomes should be identified and earned during prenatal care. These practices should include various topics such as dental care, not smoking, not using alcohol or illegal substances, balanced nutrition and gaining appropriate amount of weight, regular exercising, having training about pregnancy and labor, and avoiding risky sexual acts or exposure to other infection factors.[2] As well as going for regular health checks, proper nutrition and resting habits, factors such as knowing regular course of pregnancy and possible gestational complications, and choosing right information source also directly affect the quality of gestational period.[3] Dental care and checks during pregnancy are very important in terms of fetal health. The studies show that more than one third of women have dental problems.[4] Risky conditions such as preterm labor, baby with low birth weight and preeclampsia are seen in those who have periodontal problems during pregnancy. Mothers should be encouraged for dental checks.[5] Smoking during and after pregnancy causes significant health issues for fetus, newborn and child. Active smoking is one of the major reasons for various health risks such as preterm labor, miscarriage, postpartum hemorrhage, ectopic pregnancy, fetus with low birth weight and placenta praevia.[6] Smoking during the first trimester is one of the major factors increasing the risks for spontaneous abortion and ectopic pregnancy.[7] It was reported that the risk for ectopic pregnancy is 1.5 – 2.5 higher in smoking women.[8] Physical activity is important for a healthy life. The importance of exercising during pregnancy is empha- 14 Perinatal Journal sized in the literature.[9] It is reported that exercising is useful for pregnant women who have no obstetric and medical complication, and physical activity is recommended minimum 30 minutes weekly in order not to have any gestational complication.[10] Direct heavy physical activities, competitive sports increasing cardiac rhythm and prolonged activities on supine position are not recommended.[11] The recent studies in particular have highlighted that physical activities have a significant role for a healthy pregnancy.[12,13] Problems such as fatigue particularly, physical discomfort, being unable to use time efficiently and incompetency in child care are seen more in pregnant women who do not engage in physical activities.[14-16] High quality care and balanced nutrition during pregnancy is very important for the maternal health.[17] As the education, health and nutrition condition, socioeconomic life standards and provided healthcare services of mother improve, the chance to have a successful pregnancy also increases. A successful pregnancy and delivery ensure babies to born into a healthy life.[18] Maintaining pregnancy healthy for both mother and baby requires medical checks from the beginning up to the end of pregnancy. In normal pregnant women, prenatal checks are estimated to be once a month until the 28 weeks of gestation, once every 15 days between 28 and 36 weeks of gestation and once a week from the 36 weeks of gestation up until delivery. According to the Ministry of Health, it is aimed to follow up each pregnant woman at least for 6 times by identifying as of the beginning of pregnancy. Making visits regularly ensures to decrease fetal and neonatal problems.[19] Vaccination programs have a significant role especially to decrease infant deaths. According to the World Health Organization (WHO), 1/5 of the infant deaths in developing countries are caused by the preventable diseases. Thanks to the “Expanded Program on Immunization” initiated by WHO in 1974, considerable decreases have been observed in the incidence, mortality and morbidity rates of preventable diseases by vaccination.[20] Main purposes of vaccination are to protect fetus during pregnancy against infections such as varicella and rubella causing congenital malformation, growth retardation, stillbirth and neurological sequels, to protect mother against diseases such as influenza, hepatitis B which progress more severely during pregnancy, and to decrease infant morbidity, mortality and infectious dis- Health practices of pregnant women in Gumushane City Center ease risk of newborn in the first 6 months.[21] There are significant differences in vaccination rates according to the region, residential area and educational background of mother. The percentage of fully vaccination children is significantly low in the Eastern Anatolia Region (64%). It is followed by Northern and Southern Regions (84% and 82%, respectively).[1] Postpartum care is very important both for mother and baby. Considerably majority of them are being physicians, 82% of women had postpartum care. Four out of five women had their first postnatal check within two days after the delivery. Postpartum care and its timing vary according to the regions. The rate of having care within first 41 days is the highest among the women in Aegean Region (92%), and the rate of women in MidEastern Anatolia is only 55%.[1] The care to be provided to mother and baby is very significant for facilitating the adaptation of mother to postpartum period, early start of and sustaining lactation, providing mother-baby interaction, accelerating healing process, preventing complications, and for the postnatal comfort.[22] The study aimed to investigate the health practices of pregnant women living in Gumushane city center, and to increase awareness among pregnant women. ‘Rarely (b)’ as 2 points, ‘Sometimes (c)’ as 3 points, ‘Frequently (d)’ as 4 points and ‘Always (e)’ as 5 points; each question from 18 to 34 has 5 appropriate options which are scaled from 1 to 5 points. Some questions have reverse scaling. These are the questions 6, 7, 8, 22, 23, 24, 25, 26, 27, 33 and 34. The points of these questions are scaled from 5 to 1, in a reverse way. A general point is obtained from the total of the all questions. Getting high score represents high quality health behavior which has a significant benefit on pregnancy. In the study of Lindgreen, the lowest possible score in the scale is 34 while the highest possible score is 170.[2] The method of face-to-face interview was applied in the data collection. After the questionnaire, health practice trainings were provided to pregnant women. SPSS software was used for the analysis of the data. The data obtained in the study was provided as figure, percentage, arithmetic mean and standard deviation. After normality analyses were applied to the data, Mann-Whitney U test, one-way analysis of variance (ANOVA) test and post hoc analyses to determine the source of difference were carried out. p<0.05 was considered as significant. Results Methods The research is of definitive characteristics. A total of 233 pregnant women visiting the maternity clinic for pregnancy control between October 1st and December 10th 2012 were accessed and only 189 of them accepted to participate in the study. During the period when the investigation was planned and it was started to collect the data, written permission was received from Gumushane Provincial Directorate of Health. All participants were informed and read the purposes and methods of the investigation. The data collection tool used in the investigation has two parts. The first part of the form, which is intended for personal information, performs a literature review and it includes 25 questions such as age, educational background, employment status, health insurance, residential area, family type, pregnancy follow-up, and child number. The second part of the form is “Health Practices Questionnaire” (HPQ). HPQ-II is a questionnaire with 34 questions. Questions from 1 to 17 include five-point likert scale varying between “Always” and “Never”. The answer ‘Never (a)’ is calculated as 1 point, Mean age of the pregnant women is 29.09±5.5 (min: 19, max: 48). Of the participants, 65.1% of them stated that their expenses were equal to their incomes, 8.58% of them had no social security, 24.6% of them had a job, and 51.3% of them were living in the city center (Table 1). While 66.7% of the pregnant women preferred to visit an obstetrician at state hospital, 6.8% of them visited obstetricians both at private hospital and state hospital. Of the pregnant women, 60.6% said that they had pregnancy follow-up for 5 times or more, 75.4% of them became pregnant voluntarily, 72.3% of them had health practice training before pregnancy (from internet, those with pregnancy experience, TV, family physician, nurse), and 89.3% of them said that they would like to be informed about health practices. Only 1.7% of the participants had the history of sexually transmitted disease (Table 2). Of the spouses, 10.1% were primary school graduate, 14.9% were secondary school graduate, 51.1% were high school graduate, and 23.9% were university graduate. While 2.6% of them were unemployed, Volume 23 | Issue 1 | April 2015 15 Özcan H, K›z›lkaya Beji N Table 1. Distribution of pregnant women according to definitive characteristics (n=189). Table 2. Pregnancy history of participants. Pregnancy history Definitive characteristics Number Number % Planning the pregnancy (n=183) I got pregnant accidentally I got pregnant on purpose I got pregnant accidentally but I want to deliver 37 138 37 20.2 75.4 4.4 Health checks during pregnancy (n=188) Once Twice Three times Four times Five times or more 13 17 22 22 114 6.9 9.0 11.7 11.7 60.6 Number of pregnancy First pregnancy Second pregnancy Third pregnancy Fourth pregnancy Fifth pregnancy or more 55 61 43 17 6 30.2 33.5 23.6 9.3 3.3 Having training on health practices during pregnancy (n=188) Yes No 136 51 72.3 27.1 % Age (n=189) 15–24 25–34 35 and above 43 112 34 22.8 59.3 18.0 Educational background (n=188) Primary school Secondary school High school University 48 51 62 27 25.5 27.1 32.9 14.4 Residential area (n=189) Metropolis City center County Village 9 97 56 27 4.8 51.3 29.6 14.3 Profession (n=187) Housewife Civil service Worker Self-employed Other 141 31 6 5 4 75.4 16.6 3.2 2.7 2.1 Income level (n=186) Income less than expenses Income equals to expenses Income higher than expenses 27 121 38 14.5 65.1 20.4 Performer of the follow-ups during pregnancy (n=168) Family physician 4 Private obstetrician 41 Obstetrician at state hospital 112 Other 1 ence was caused by the mean values of first group (age range of 15-24) and third group (35-year-old and above), and that the score average of the questionnaire decreased as the age increased (Table 3). 39.7% of them were civil service employees, 32.8% of them were worker, 18.5% of them were self-employed and 6.3% of them were engaged in other fields. The mean score of the participants for health practice questionnaire (HPQ) was 111.76±18.53. Statistically no significant difference was observed in the analysis of ANOVA test carried out in the HPQ scores according to the educational background of pregnant women (p>0.05) (Table 4). In the analysis of ANOVA test performed between age groups of pregnant women and mean HPQ scores, statistically a significant difference was found. According to the post-hoc analysis to determine the source for the difference, it was found that the differ- The average HPQ scores were also analyzed according to the employment status of pregnant Table 3. Distribution of mean HPQ scores according to age groups of pregnant women.* Mean HPQ Score Age group N X SS 15–24 43 117.4884 12.56862 25–34 112 110.6786 20.69174 35 and above 33 107.9697 15.88924 Total 188 111.7606 18.53660 *ANOVA test was used. 16 Perinatal Journal 2.3 24.4 66.7 1.7 F P 2.996 0.052 Health practices of pregnant women in Gumushane City Center Table 4. Distribution of mean HPQ scores according to educational background of pregnant women.* Mean HPQ Score Educational background N X SS Primary school 47 109.8298 15.94190 Secondary school 51 111.6667 21.24116 High school 63 112.6190 17.50615 University 27 113.2963 20.30312 Total 188 111.7606 18.53660 F P 0.274 0.844 *ANOVA test was used. women. There was no significant difference in the Mann-Whitney U analysis performed between the employment statuses and mean HPQ scores of pregnant women (Table 5). graduate. According to TNSA 2008 data, about 52% of women were only primary school graduates. In the study, 73% of women were secondary school or higher level graduates. In the analysis of ANOVA test performed on mean HPQ scores according to the educational background of the spouses of pregnant women, statistically a significant difference was found. In the post-hoc analysis carried out for determining the source of difference, it was seen that there was difference between primary school graduates and university graduates. In Turkey, the lowest employment rate among women was in Central and Eastern Regions.[1] Our study, we observed that the rates of unemployed women in Gumushane, which is a province in the Black Sea Region, were high similar to the women living in Central and Eastern Regions. Discussion While 51.3% of the women participated in the study were living in the large city, 29.6% of them were living in counties, 14.3% of them in villages, and 4.8% of them in the city. The most of the pregnant women being living in the city and the metropolis is important in terms of having follow-up, care and training during pregnancy. In our study, we found statistically a significant difference in the analysis of ANOVA test performed on mean HPQ scores according to the most frequent residential area of pregnant women. The mean scores of those living in the city were higher than those living in the villages. While 82.1% of the participants were in the 15–34 age range, 47.6% of them were high school and university It is known that carrying out the delivery in healthy conditions and getting postpartum follow-ups regular- In the analysis of ANOVA test performed on mean HPQ scores according to the most frequent residential areas of pregnant women, statistically a significant difference was found. A post-hoc analysis was performed for the difference, and the p value was found as <0.05 for the difference between the average values of those living in urban and rural areas. The mean HPQ scores of pregnant women living in the city center were found to be higher than those living in villages. Table 5. Distribution of mean HPQ scores according to employment statuses of pregnant women.* Mean HPQ Score Employment status N X 140 83.24 Employed 31 98.47 Total 171 Unemployed SS U P 18.536 1783.50 0.121 *Mann-Whitney U test was used. Volume 23 | Issue 1 | April 2015 17 Özcan H, K›z›lkaya Beji N ly decrease maternal and perinatal newborn deaths.[23] Total visits before the delivery is a significant indication for evaluating the sufficiency of prenatal care. While pregnant women need to have follow-ups for 6 times during the pregnancy, insufficient number of visits shows that this service is not carried out actively.[24] Although the mean HPQ scores in the study are low, the rate of participants to visit a health institution during pregnancy for five or more times is 60.6%. their families, to enable the spouses of pregnant women to join such programs by informing them, to carry out detailed interviews in order to determine the mistakes and to modify the practices of pregnant women in advanced age group, and to increase awareness on this subject matter. In the analysis of ANOVA test performed on mean HPQ scores according to the educational background of the spouses of pregnant women, statistically a significant difference was found. As the educational background increases, HPQ score also increases. Similarly, as in the study of Çakmakç› and Eser, there was statistically a significant difference between the pregnant women whose spouses were university/college graduate and those whose spouses were high school or lower level graduates.[25] References In the analysis of ANOVA test performed on the mean HPQ scores according to the age groups of pregnant women, statistically a significant difference was found. Mean HPQ score of young pregnant women was 117.48 while it was 107.96 for pregnant women with advanced ages. The reason for difference based on age may be that young group tries to learn by searching studies as a source of information, and that the advanced age group utilizes their experience. The results of our study are similar to the studies performed to analyze the effects of age and educational background of women on gestational health. The major factors increasing the possibility to carry out a delivery in a healthcare institution are the young ages of women, early in the rank of birth order, mother having high number of prenatal care and high level of education. It has been reported that the possibility to deliver a baby in a healthcare institution in an urban area is 1.2 times higher than rural areas, and the rate of home birth is higher in Eastern Regions than Central Anatolian Regions (27%).[1,19] Conclusion For the health practices during pregnancy, the ages of pregnant women and their spouses and living in whether in urban or rural areas caused differences. Therefore, it is required to extend “prenatal and postnatal training programs” among pregnant women and 18 Perinatal Journal Conflicts of Interest: No conflicts declared. 1. Türkiye Nüfus ve Sa¤l›k Araflt›rmas› TNSA. Ankara: Hacettepe Üniversitesi Nüfüs Etütleri Enstitüsü; 2008. 2. Lindgreen K. Testing the health practices in pregnancy questionnaire- II. JOGNN 2005;34:465–72. 3. Sözeri C, Cevahir R, fiahin S, Semiz O. Gebelerin gebelik süreci ile ilgili bilgi ve davran›fllar›. F›rat Sa¤l›k Hizmetleri Dergisi 2006;1:93–104. 4. Ovenbacher S, Boggess KA, Murtha AP, Jared HL, Lieff S, McKaig RG, et al. Progressive periodontal disease and risk of very preterm delivery. Obstet Gynecol 2006;107:29– 36. 5. Hullah E, Turok Y, Nauta M, Yoong W. Self-reported oral hygiene habits, dental attendance and attitudes to dentistry during pregnancy in a sample of immigrant women in north london. Arch Gynecol Obstet 2008;277:405–9. 6. Marako¤lu K, Erdem D. Türkiye’de, Orta Anadolu’daki bir evde gebe kad›nlarda sigara kullan›m›n›n de¤erlendirilmesi. Turkiye Klinikleri J Med Sci 2011;31:928–34. 7. Getahun D, Amre D, Rhoads G, Demissie K. Maternal and obstetric risk factors for sudden infant death syndrome in the United States. Obstet Gynecol 2004;103:646–52. 8. Goel P, Radotra A, Singh I, Aggarwal A, Dua D. Effects of passsive smoking on outcome in pregnancy. J Postgrad Med 2003;154:316–24. 9. Gharaibeh M, Al-Ma’atiah R, Al Jada N. Lifestyle practices of Jordanian pregnant women. Int Nurs Rev 2005;52:92– 100. 10. Ezmerli NM. Exercise in pregnancy. Prim Care Update Ob Gyns 2000;7:260–5. 11. Committee on Obstetric Practice. ACOG committee opinion. Exercise during pregnancy and the postpartum period. Number 267, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet 2002; 77:79–81. 12. American College of Sports Medicine. Impact of physical activity during pregnancy and postpartum on chronic disease risk. Med Sci Sports Exerc 2006;38:989–1006. 13. Hedegaard M, Damm P, Ottesen B, Petersson K, Henriksen TB. Leisure time physical activity is associated with a reduced risk of preterm delivery. Am J Obstet Gynecol 2008;198:180.e1–5. Health practices of pregnant women in Gumushane City Center 14. Evenson KR, Moos MK, Carrier K, Siega-Riz AM. Perceived barriers to physical activity among pregnant women. matern. Child Health J 2009;13:364–75. 19. Turan T, Ceylan S, Teyikçi S. Annelerin düzenli prenetal bak›m alma durumlar› ve etkileyen faktörler. F›rat Sa¤l›k Hizmetleri Dergisi 2008;3:157–73. 15. Pereira MA, Rifas-Shiman SL, Kleinman KP, Rich-Edwards JW, Peterson KE, Gillman MW. Predictors of change in physical activity during and after pregnancy: Project Viva. Am J Prev Med 2007;32:312–9. 20. Kurçer M, fiimflek Z, Solmaz A, Dedeo¤lu Y, Gülel R. fianl›urfa Harrankap› Sa¤l›k Oca¤› bölgesinde 0–2 yafl çocuk ve gebelerde afl›lanma oranlar› ve afl›lamada sorunlar. Harran Üniversitesi T›p Fakültesi Dergisi 2005;2:10–5. 16. Mudd L, Nechuta S, Pivarnik J, Paneth N; N; Michigan Alliance for National Children's Study. Factors associated with women’s perceptions of physical activity safety during pregnancy. Prev Med 2009;49:194–9. 21. Yenicesu C, Demirel Y. Gebelerde afl›lar. Turkiye Klinikleri Journal of Family Medicine - Special Topics 2011;2:75–81. 17. Lundberg P, Trieu TN. Vietnamese women’s cultural beliefs and practices related to the postpartum period. Midwifery 2011;27:731–6. 18. Duran Ö, Ceyhan O. Tokat Karfl›yaka Do¤um ve Çocuk Bak›mevinde do¤an bebeklerin gebelik haftas›, do¤um flekli, do¤um a¤›rl›¤›, boy uzunlu¤u ve anomali durumu ile anne ve babaya ait özellikler aras›ndaki iliflki. Erciyes Üniversitesi Sa¤l›k Bilimleri Dergisi (E. Ü. Journal of Health Sciences) 2004;13:26–34. 22. P›nar G, Do¤an L, Alg›er N, Kaya N, Çakmak F. Annelerin do¤um sonu konforunu etkileyen faktörler. Dicle T›p Dergisi 2009;36:184–90. 23. Ergin F, Baflar P, Karahasano¤lu B, Befler E. Güvenli olmayan do¤umlar ve do¤um sonras› evde bak›m hizmetlerinin de¤erlendirilmesi. Türk Silahl› Kuvvetleri Koruyucu Hekimlik Bülteni 2005;4:78–92. 24. Taflk›n L. Kad›n Sa¤l›¤› ve Hastal›klar› Hemflireli¤i. XI. bask›. Ankara: Sistem Ofset Matbaac›l›k; 2012. p: 67–80. 25. Çakmakç› A, Eser E. Gebelikte olumlu davran›fl envanteri: bir metodolojik çal›flma. Hemflirelik Forumu 2003;6:8–18. Volume 23 | Issue 1 | April 2015 19 AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):20–25 R N A PE IN AT U AL JO R The evaluation of pregnancies complicated by eclampsia: retrospective analysis of 37 cases in our clinic Aytekin Tokmak, Korkut Da¤lar, Ali ‹rfan Güzel, Bergen Laleli, Salim Erkaya, Dilek Uygur Gynecology & Obstetrics Clinic, Zekai Tahir Burak Maternal Health Training and Research Hospital, Ankara, Turkey Abstract Özet: Eklampsi ile komplike olan gebeliklerin de¤erlendirilmesi: Klini¤imizdeki 37 olgunun retrospektif analizi Objective: We aimed to evaluate the clinical characteristics and maternal and perinatal outcomes of pregnancies complicated by eclampsia. Amaç: Eklampsi ile komplike olan gebeliklerin klinik özelliklerinin ve maternal ve perinatal sonuçlar›n›n de¤erlendirilmesi. Methods: A total of 37 patients were identified who were diagnosed and treated in Zekai Tahir Burak Maternal Health Training and Research Hospital between January 2009 and December 2013. These patients found in and reviewed by their hospital records were evaluated retrospectively in terms of their clinical characteristics, laboratory parameters, and maternal and perinatal outcomes. Results: It was found that a total of 89,908 deliveries were performed in our hospital during the study. Eclampsia incidence was calculated as 0.4/1000 deliveries. Mean age of the cases in our study was 27.2±6.6 years and mean gestational age was 33.2±4.5 weeks. The rate of the cases who were nullipara was 78.4%. It was understood that the most of the eclamptic seizures occurred during the antenatal period (59.6%) after 28 weeks of gestation (89.2%). Neonatal morbidity rate was 61.1% and perinatal mortality rate was 12.5%. While major morbidity rate was 43.2%, the leading cause of the morbidity was HELLP syndrome (37.8%). It was found that a thirty-year-old woman who was multipara (G2P1) died on the postpartum 10th day due to intracranial hemorrhage. Conclusion: Eclampsia is one of the most significant reasons of maternal and perinatal morbidity and mortality. Even though it is not always possible to prevent it, the best approach can be provided by ensuring patients with highest risk for eclampsia to have regular antenatal care, preventing convulsions through hospitalization in tertiary healthcare centers with proper conditions, bringing blood pressure under control and carrying out delivery at the most convenient time. Keywords: Eclampsia, clinical characteristics, maternal and perinatal outcomes. Yöntem: Zekai Tahir Burak Kad›n Sa¤l›¤› E¤itim ve Araflt›rma Hastanesinde Ocak 2009 ve Aral›k 2013 tarihleri aras›nda eklampsi tan›s› konulan ve tedavi edilen toplam 37 hasta tan›mland›. Hastane kay›tlar›ndan saptanan ve dosyalar› incelenen bu hastalar klinik özellikleri, laboratuvar parametreleri ve maternal ve perinatal sonuçlar›na göre retrospektif olarak de¤erlendirildi. Bulgular: Çal›flma süresince hastanemizde toplam 89.908 do¤umun gerçekleflti¤i saptand›. Eklampsi insidans› 0.4/1000 do¤um olarak hesapland›. Çal›flmam›zda yer alan olgular›n yafl ortalamas› 27.2±6.6 y›l ve ortalama gebelik yafl› 33.2±4.5 haftayd›. Olgular›n %78.4’ü nullipar idi. Eklamptik nöbetlerin ço¤unlu¤unun antenatal dönemde (%59.6) ve 28. gebelik haftas›ndan sonra (%89.2) gerçekleflti¤i anlafl›ld›. Neonatal morbidite oran› %61.1 ve perinatal mortalite oran› %12.5 olarak bulundu. Majör morbidite oran› %43.2 ve morbiditeye neden olan önde gelen sebep HELLP sendromuydu (%37.8). Otuz yafl›nda multipar (G2P1) bir kad›n›n, do¤umdan sonra 10. günde intrakranial kanama nedeniyle kaybedildi¤i saptand›. Sonuç: Eklampsi, maternal ve perinatal morbidite ve mortalitenin en önemli nedenlerinden biridir. Her zaman önlenemese de, eklampsi geliflme riski yüksek olan hastalar›n düzenli antenatal bak›m almalar›n›n sa¤lanmas›, uygun koflullara sahip üçüncü basamak merkezlerde hospitalize edilerek, konvülziyonlar›n önlenmesi, kan bas›nc›n›n kontrol alt›na al›nmas› ve uygun zamanda do¤umun gerçeklefltirilmesi ile en iyi yaklafl›m sa¤lanabilir. Anahtar sözcükler: Eklampsi, klinik özellikler, maternal ve perinatal sonuçlar. Correspondence: Aytekin Tokmak, MD. ZTB Kad›n Sa¤l›¤› E¤itim ve Arafl. Hast. Kad›n Hastal›klar› ve Do¤um Klini¤i, Ankara, Turkey. e-mail: aytekintokmak@gmail.com Received: November 2, 2014; Accepted: January 5, 2015 Please cite this article as: Tokmak A, Da¤lar K, Güzel, A‹, Laleli B, Erkaya S, Uygur D. The evaluation of pregnancies complicated by eclampsia: retrospective analysis of 37 cases in our clinic. Perinatal Journal 2015;23(1):20–25. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231005 doi:10.2399/prn.15.0231005 QR (Quick Response) Code: The evaluation of pregnancies complicated by eclampsia Introduction Methods Hypertensive disorders are the most frequent medical complication of pregnancy, and it has been reported that they affect 5-10% of pregnancies in the USA.[1] Despite its higher incidence and wider incidence range in developing countries, its incidence rate (0.16– 1/1000 delivery) is stable in developed countries.[2] Eclampsia is a specific neurological complication of pregnancy, it is characterized by hypertension and tonic clonic convulsions, and its pathophysiology is still unclear. It has been found that the cerebral anomalies developing in eclampsia are similar to the changes in hypertensive encephalopathy.[3] Early marriage, nulliparity, insufficient prenatal care, low socio-economical condition and malnutrition are the risk factors for eclampsia as in preeclampsia. While eclamptic seizure may develop after severe preeclampsia, it also may develop unexpectedly without hypertension and proteinuria.[4] A mild hypertension can be seen only in 3060% of the women developing eclampsia.[3] Headache, blurring of vision, photophobia and mental changes may be early diagnoses of an approaching eclampsia; however, the eclampsia may develop even without these findings. Thirty-seven cases who were established eclampsia diagnosis and treated in high-risk pregnancy and delivery room departments of Zekai Tahir Burak Maternal Health Training and Research Hospital between January 2009 and December 2013 were evaluated retrospectively. Patient data were obtained from patient files. Demographic characteristics, laboratory findings and obstetric outcomes were recorded. For each women, age, gravida, parity, abortion, gestational body mass index (BMI), blood pressure measurements, week of gestation at diagnosis, additional disease, smoking habit, initial symptoms, educational level, the phase that delivery occurs, laboratory findings, hospitalization period, magnesium application, delivery type, birth weight, Apgar score, and finally maternal - fetal morbidity and mortality were investigated. It was seen that the weeks of gestation were calculated according to last menstrual periods, and that the gestational age was noted according to ultrasound screenings carried out on the first trimester in those who did not know their last menstrual period. Full urinalysis, full blood counts, liver and kidney function tests and LDH values of all cases were recorded. It was found that fetal biometry and Doppler examination by ultrasonography and continuous external fetal monitorization by cardiotocography were carried out for each patient. With 12-hour dosing interval, 12 mg betamethasone was administered to all pregnant women at or below 34 weeks of gestation for fetal lung maturation. Eclampsia is a life-threatening complication of pregnancy. Its most frequently reported reason is HELLP syndrome.[3] Maternal mortality rate of eclampsia was reported was as high as 15%.[5] Intracranial hemorrhage, pulmonary edema, renal, hepatic and respiratory failures are the leading mortality reasons. Increased perinatal mortality is a result of eclampsia, and perinatal mortality rate was reported as 10% in a multicentric study carried out in Brazil.[6] Chronic placental insufficiency, preterm labor and ablatio placentae are among perinatal mortality reasons.[7] It is easy to establish eclampsia diagnosis; however, it should be remembered that conditions such as epilepsy, encephalitis, meningitis, brain tumors, cysticercosis and ruptured brain aneurysm may trigger eclampsia during advanced weeks of gestation and puerperium. All pregnants having convulsion should be considered as eclamptic until all other reasons are ruled out.[8] Eclampsia requires immediate treatment in order to minimize maternal and fetal morbidity and mortality. In this study, we aimed to analyze eclampsia cases in our hospital which is a tertiary healthcare center in Central Anatolia. Eclampsia was identified according to the presence of following criteria: the presence of at least two among hypertension, proteinuria, thrombocytopenia, and increased serum AST level within 24 hours after convulsions developed during pregnancy or within 10 days during following delivery. The diagnosis of HELLP syndrome was established according to hemolysis (LDH >600 U/L), thrombocytopenia (<100×103/μL) and increased liver enzyme (AST>70U/L). It was found that 10-minute intravenous loading dose of 4.5 g magnesium sulphate (MgSO4) was administered to all women having eclamptic seizure and then convulsion prophylaxis was initiated so as to progress as 2 g/h intravenous infusion, and nifedipine and alpha-methyldopa were used in the anti-hypertensive treatment in order to keep diastolic blood pressure between 90 and 100 mmHg and severe hypertension under control. Volume 23 | Issue 1 | April 2015 21 Tokmak A et al. Statistical Package for the Social Sciences (SPSS) version 15.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Definitive data and frequencies were calculated by the computer. Conformity of the data to normal distribution was evaluated by Kolmogorov-Smirnov test. The data with constant and normal distribution were provided as mean±standard deviation, and the data without constant and normal distribution were provided as median (minimum-maximum). Categorical variables were given as figure (percentage). Results During the 5-year period of the study, a total of 89,908 deliveries occurred in our hospital. It was found that 37 of these pregnancies were complicated with eclampsia. Eclampsia incidence was calculated as 0.4/1000 deliveries. Eclampsia was more common in nullipara cases (78.4% vs. 21.6%). Mean age and weeks of gestation of the patients were 27.2±6.6 (range: 16 to 42) years and 33.2±4.5 (range: 25 to 39) weeks, respectively. While mean systolic blood pressure value was 155.7±26.9 mmHg, it was 101.6±17.5 mmHg for diastolic blood pressure. The clinical and laboratory findings of the patients are shown in the Table 1. Eclamptic seizure occurred during antepartum period in 22 patients, during postpartum period in 10 patients and during intrapartum period in 5 patients. Eclamptic seizure developed without hypertension in 5 patients, and headache was the most frequent initial symptom (Table 2). The rates of cesarean and vaginal delivery were 89.2% and 10.8%, respectively. Two out of 4 patients who had vaginal delivery developed postpartum eclampsia, one patient had intrauterine fetal death and one multipara patient developed intrapartum eclampsia on the second phase of the delivery. The educational level of more than half of the patients was primary school or below. One patient had gestational diabetes while one patient had smoking history. Multiple pregnancy was found in two patients (one twin, and one triplet). It was seen in two patients that eclampsia developed without proteinuria. While maternal morbidity developed in 16 patients, the diagnosis of HELLP syndrome was established in 14 of them, disseminated intravascular coagulation (DIC) in one patient, sudden temporary loss of vision in one patient and renal failure following detachment in one patient. It was found that one 22 Perinatal Journal Table 1. Clinical and laboratory characteristics of cases. Variable Result Age (year)* 27.2±6.6 Nullipara† 29 (78.4) Gravida‡ 2 (1–6) Parity‡ 0 (0–3) Abortion‡ BMI (kg/m2)* Smoking† 1 (0–6) 29.8±4.8 1 (2.7) Educational level† Illiterate 2 (5.4) Primary school 17 (45.9) Secondary school 8 (21.6) High school 10 (27) SBP (mmHg)* 155.7±26.9 DBP (mmHg)* 101.6±17.5 Hospitalization period (day)* 8.6±3.3 AST (U/L)* 236.2±458.9 ALT (U/L)* 176.8±305.1 Creatinine (mg/dL)* 0.7±0.2 Platelet (x103/μL)* 179.4±108.6 LDH (U/L)* 1008.4±705.9 Proteinuria in spot urine (mg/dL)† 0 0< and ≤30 >30 and ≤300 >300 2 (5.4) 3 (8.1) 22 (59.5) 10 (27) BMI: Body mass index; DBP: Diastolic blood pressure; SBP: Systolic blood pressure. Data *: 9±SD; †: n(%); ‡: median (minimum–maximum). patient was referred to the Intense Care Unit of Anesthesiology and Reanimation Department of Ankara Training and Research Hospital due to intracranial hemorrhage, but died on the way. Maternal mortality was found as 2.7% due to this case. Prematurity and intrauterine growth retardation (IUGR) were the most frequent reasons for perinatal morbidity (Table 3). Perinatal mortality rate was found as 12.5% (5/40). Table 2. Initial symptom. Symptom n (%) Headache 10 (27) Blurring of vision 8 (21.6) Epigastric pain 2 (5.4) Recurring seizure 5 (13.5) The evaluation of pregnancies complicated by eclampsia Discussion Eclampsia is a life-threatening gestational complication developing acutely. It has a high risk of morbidity and mortality for mother and fetus. When eclampsia usually occurs following severe preeclampsia, it may appear without any preeclamptic symptoms. Munro[9] reported that 38% of eclamptic seizures occurred without any symptom and finding previously. Its incidence reported in developed countries is 1/2000–1/3000; however, this rate is much more in developing countries.[4] The eclampsia rates reported in Turkey vary. In their study, Y›ld›r›m et al.[10] investigated 113 eclampsia cases and found eclampsia rate as 1.2/1000 delivery, which was reported as 1.7/1000 in another study carried in the western region of Turkey.[11] The study performed in Southeastern Anatolia found the incidence rate as 19/1000[12] while it was reported as 1.2/1000 in Northeastern Anatolia.[13] In our study, we found a lower rate which was 0.4/1000 (1/2430). The reason may be that especially the eclampsia cases developing during the postpartum period referred to other multidisciplinary hospitals in the region. Liu et al.[14] found that eclampsia incidence gradually decreased and nulliparity, anemia and the presence of cardiac disease in singleton deliveries increased the risk of eclampsia for 2.3–4.8 times. In another study, it was argued that being younger than 20-year-old and older than 35-year-old, long intervals between deliveries, low socio-economic level, gestational diabetes, gestational obesity and gaining weight during pregnancy less or more than recommended were found to be the risk factors associated with eclampsia, and that multiparity and smoking decreased the eclampsia.[15] Y›ld›r›m et al. showed in their studies that 63.7% of eclamptic seizures developed in nullipara cases.[10] Similarly, we found in our study that nulliparity was more common among eclamptic cases (78.4%). Lopez-Llera[16] categorized eclampsia according to the onset time of the seizure and defined as antepartum if it develops before delivery, as intrapartum if it occurs during delivery and as postpartum if it develops within 7 days after delivery. It was reported that 38–53% of the eclamptic seizures developed during antepartum period while 11–44% of them developed during postpartum period.[3] However, it can be difficult to distinguish them since antepartum and intrapartum periods intertwine. Also, in higher than 90% of the eclamptic Table 3. Obstetric and maternal-perinatal outcomes. Variable Result Week of gestation* 33.2±4.5 ≤28 week of gestation† 4 (10.8) Birth weight* 1988.9±973.6 Apgar score‡ 6 (0–9) Multiple pregnancy† Twin 1 (2.7) Triple 1 (2.7) Perinatal morbidity† Prematurity 22 (61.1) IUGR 12 (32.4) Perinatal mortality† 5 (12.5) Maternal complication† 16 (43.2) HELLP 14 (37.5) Maternal mortality† Delivery 1 (2.7) type† Vaginal delivery 4 (10.8) Cesarean section 33 (89.2) Period that seizure occurred† Antepartum Postpartum Intrapartum 22 (59.5) 10 (27) 5 (13.5) IUGR: Intrauterine growth retardation. Data *: 9±SD; ‡: n(%); ‡: median (minimum–maximum). cases, it develops after 28 weeks of gestation.[4] In line with the literature, we observed eclamptic seizure in most of our cases during antepartum period (59.4%) and after 28 weeks of gestation (89.2%). The first step of eclampsia management is to prevent maternal injuries and to provide cardiopulmonary support. Afterwards, it is to prevent the recurrence of convulsions and to decrease blood pressure to the safe levels. There are strong evidences for using routine magnesium sulphate (MgSO4) for the prophylaxis of seizures in the literature, and a full consensus has been reached.[17,18] The recommendation for patient with eclamptic seizure is to administer 1–2 g/h maintenance dose for at least 24 hours after 4–6 g intravenous loading dose.[1] However, in 9.4% of the cases, it was reported that eclamptic seizures may recur despite MgSO4 prophylaxis.[17] We initiate MgSO4 prophylaxis for all our severe preeclamptic and eclamptic patients. We monitor our patients by their urination, respiratory rate, patellar reflex and intermittent serum magnesium levels. In our study, similar to the literature, the seizure recurred under MgSO4 proVolume 23 | Issue 1 | April 2015 23 Tokmak A et al. phylaxis in 5 (13.5%) patients, and we kept the seizure under control in all these patients by single dose diazepam (10 mg). In women developing eclampsia, detachment, DIC, HELLP, cerebral hemorrhage and maternal mortality risk increased.[4] The risk of HELLP syndrome is reported about 10–15% in eclamptic cases.[3] However, in recent publications in our country, the rate of eclamptic patients developing HELLP syndrome reached up to 40% and the eclampsia was grouped in two categories as developing HELLP and not developing HELLP.[10,11,19] In line with the literature, HELLP syndrome was the most common complication in our patients while one patient had DIC, one patient had renal failure following detachment and one patient had sudden temporary loss of vision. Also, our patient developing HELLP died after intracranial hemorrhage on postpartum 10th day in the intense care unit of a multidisciplinary hospital. In the study investigating maternal death of 174 cases, Akar et al. found maternal mortality rate as 40/100,000 and preeclampsia- and eclampsia-induced complications as the most common direct maternal death.[20] It is reported in the world that eclampsiainduced maternal mortality rates has increased up to 15%.[5] Eclamptic cases are more common in developing countries and it is explained by the multiple numbers of convulsions occurring out of hospital and nonpresence of antenatal follow-ups of these cases. In our country, maternal mortality rate in eclamptic cases is reported between 0 and 14.6%.[21] In our study, we found eclampsia-induced maternal mortality rate as 2.7% (1 case). Perinatal morbidity and mortality rates are high in the babies of eclamptic mothers. Preeclampsia and eclampsia are responsible for 2.7% of perinatal mortality independent from prematurity and IUGR, preeclampsia rate is 12% in newborns with IUGR and 19% in preterm newborns.[22] In a multinational study supported by WHO and involved 29 countries, perinatal mortality rates were found as 2.6%, 9.2% and 22.6% in non-preeclamptic/non-eclamptic, preeclamptic and eclamptic pregnant women, respectively.[23] These complications are most likely prematurity-induced RDS, apnea, jaundice, kernicterus, malnutrition, hypoglycemia, seizure, periventricular leukomalacia and prolonged hospitalization periods.[24,25] While most of our 24 Perinatal Journal cases (61.1%) were born as premature, 12 (32.4%) cases had IUGR. One case died during perinatal period and 4 cases during neonatal period. We found perinatal mortality rate as 12.5%. Conclusion In conclusion, severe preeclampsia and eclampsia are significant reasons for maternal and perinatal morbidity and mortality in the world. Understanding the pathophysiology better, close antenatal follow-ups and appropriate treatment by hospitalizing risky cases in tertiary healthcare centers with proper conditions may decrease eclampsia incidence and associated secondary maternal and perinatal morbidity and mortality rates. Conflicts of Interest: No conflicts declared. References 1. Moussa HN, Arian SE, Sibai BM. Management of hypertensive disorders in pregnancy. Women’s Health 2014;10: 385–404. 2. Norwitz ER. Eclampsia; incidence and epidemiology. In: Lockwood CJ (ed) UpTodate. Last updated in Jul 14, 2014. Retrieved from http://www.uptodate.com/contents/eclampsia. 3. Sibai BM. Diagnosis, prevention, and management of eclampsia. Obstet Gynecol 2005;105:402–10. 4. Mattar F, Sibai BM. Eclampsia. VIII. Risk factors for maternal morbidity. Am J Obstet Gynecol 1999;182:307–12. 5. Ghulmiyyah L, Sibai B. Maternal mortality from preeclampsia/eclampsia. Semin Perinatol 2012;36:56–9. 6. Giordano JC, Parpinelli MA, Cecatti JG, Haddad SM, Costa ML, Surita FG, et al. The burden of eclampsia: results from a multicenter study on surveillance of severe maternal morbidity in Brazil. PLoS One 2014;9:e97401.e1–10. 7. Sibai BM. Eclampsia. VI. Maternal-perinatal outcome in 254 consecutive cases. Am J Obstet Gynecol 1990;163:1049–54. 8. Cunningham FG, Leveno KJ,Bloom SL, Hauth JC, Gilstrap LC, Wenstrom KD. Hypertensive Disorders in Pregnancy. Williams Obstetrics. 22nd ed. Columbus, OH: McGraw-Hill Companies; 2005; p: 787. 9. Munro PT. Management of eclampsia in the accident and emergency department. J Accid Emerg Med 2000;17:7–11. 10. Y›ld›r›m G, Aslan H, Gül A, Aktafl FN, Çakmak D, Güngördük K, et al. Eklampside maternal ve perinatal sonuçlar: 113 olgunun de¤erlendirilmesi. Perinatoloji Dergisi 2007;15:61–7. 11. As›c›oglu O, Güngördük K, Yildirim G, Aslan H, Günay T. Maternal and perinatal outcomes of eclampsia with and without HELLP syndrome in a teaching hospital in western Turkey. J Obstet Gynaecol 2014;34:326–31. The evaluation of pregnancies complicated by eclampsia 12. Sumnulu I, ‹ldeniz M, Özel N. The incidence of pregnancy induced hypertension in southeast Turkey. Int J Gynaecol Obstet 1989;28:211–5. 13. ‹ngec M, Kumtepe Y, Borekci B, Bebek Z, Kadanal› S. 2001–2003 y›llar›ndaki 81 eklampsi olgusunun maternal ve perinatal sonuclar›. Jinekoloji ve Obstetik Dergisi 2005;19: 135–41. 14. Liu S, Joseph KS, Liston RM, Bartholomew S, Walker M, León JA, et al.; Maternal Health Study Group of Canadian Perinatal Surveillance System (Public Health Agency of Canada). Incidence, risk factors, and associated complications of eclampsia. Obstet Gynecol 2011;118:987–94. 15. Coghill AE, Hansen S, Littman AJ. Risk factors for eclampsia: a population-based study in Washington State, 19872007. Am J Obstet Gynecol 2011;205:553.e1–7. 16. Lopez-Llera M. Main clinical subtypes of eclampsia. Am J Obstet Gynecol 1992;166:4–9. 17. Witlin AG, Sibai BM. Magnesium sulfate therapy in preeclampsia and eclampsia. Obstet Gyencol 1998;92:883–9. 18. Hall DR, Odendaal HJ, Smith M. Is the prophylactic administration of magnesium sulphate in women with pre-eclampsia indicated prior to labor? BJOG 2000;107:903–8. 19. Kumtepe Y, Dündar O, Cetinkaya K, Ingeç M. Preeclampsia and eclampsia incidence in the eastern anatolia region of Turkey: the effects of high altitude. J Turk Ger Gynecol Assoc 2011;12:26–30. 20. Akar ME, Eyi EG, Yilmaz ES, Yuksel B, Yilmaz Z. Maternal deaths and their causes in Ankara, Turkey, 1982–2001. J Health Popul Nutr 2004;22:420–8. 21. Erden AC, Yayla M. Preeklampsi ve eklampside maternal ve fetal morbidite-mortalite. Perinatoloji Dergisi 1993;1:24–30. 22. Dodd JM, O’Brien C, Grivell RM. Preventing pre-eclampsia – are dietary factors the key? BMC Med 2014;12:176. 23. Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel JP, et al.; WHO Multicountry Survey on Maternal and Newborn Health Research Network. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG 2014;121 Suppl 1:14–24. 24. Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet 2008;371:75–84. 25. Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008;371:261–9. Volume 23 | Issue 1 | April 2015 25 AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):26–29 R N A PE IN AT U AL JO R Factors affecting postpartum depression in Diyarbak›r Ali Emre Tahao¤lu1, Cihan To¤rul1, Mehmet ‹rfan Külahç›o¤lu1, Beflire Ayd›n Öztürk1, Deniz Balsak1, Hanifi Bademk›ran1, Erdo¤an Gül1, Ümit Görkem2, Tayfun Güngör2 1 Gynecology & Obstetrics Clinic, Diyarbak›r Maternity and Pediatrics Hospital, Diyarbak›r, Turkey 2 Department of Gynecology & Obstetrics, Hitit University, Çorum, Turkey Abstract Özet: Diyarbak›r'da postpartum depresyonu etkileyen faktörler Objective: The aim of this study is to investigate the factors affecting postpartum depression (PPD) according to age groups in Diyarbak›r city located on the southeastern part of Turkey. Amaç: Bu çal›flman›n amac› Türkiye’nin güneydo¤usunda yer alan Diyarbak›r ilinde postpartum depresyonu (PPD) etkileyen faktörleri yafl gruplar›na göre incelemektir. Methods: The questions of Edinburgh postpartum depression scale (EPDS) were asked to 495 women who referred to our clinic at their postpartum periods. A separate statistical analysis was carried out for 51 adolescent women (below 18-year-old) and 72 puerperant women over 35-year-old. Score 13 according to EPDS score result was determined as cut-off value. Yöntem: Klini¤imize baflvuran 495 postpartum dönemdeki kad›na Edinburgh postpartum depresyon skoru (EPDS) anket sorular› soruldu. Elli bir adölesan (18 yafl alt›) ve 35 yafl üstü olan 72 lohusa için ayr› istatistiksel inceleme yap›ld›. EPDS skor sonucuna göre 13 puan cut-off de¤er olarak belirlendi. Results: In 101 out of 495 (20.4%) patients, EPDS score was 13 and above. This rate was 27.4% in adolescent puerperant women, and 19.4% in puerperant women over 35-year-old. It was found that depression history was a significant variable affecting postpartum depression (p<0.005). Conclusion: Postpartum depression is a significant disease possible to overlook which affects the health of mother and baby. This is risky especially during adolescent period. Depression history is an important variable in the etiology of postpartum depression. This period can be screened for postpartum depression. The greatest factor limiting postpartum depression in Southeastern Anatolia Region which has the highest reproduction rate in Turkey can be the support provided to the puerperant women by relatives and friends during puerperal period. Keywords: Postpartum period, postpartum depression. Introduction Gestation is a period when a woman has her physiological, psychological and social changes. Prenatal and post- Bulgular: Toplam 495 hastan›n 101’inde (%20.4) EPDS skoru 13 ve üzerinde idi. Adölesan lohusalarda bu oran %27.4, 35 yafl üstü lohusalarda ise %19.4 idi. Geçirilmifl depresyon öyküsünün postpartum depresyonu etkileyen anlaml› bir de¤iflken oldu¤u bulundu (p<0.005). Sonuç: Postpartum depresyon anne ve çocuk sa¤l›¤›n› etkileyen önemli ve gözden kaç›r›lmas› olas› bir hastal›kt›r. Bu durum özellikle adölesan ça¤da risklidir. Geçirilmifl depresyon hikayesi postpartum depresyon etyolojisinde en önemli de¤iflkendir. Postpartum depresyon için bu dönemde tarama yap›labilir. Türkiye’nin en yüksek üreme h›z›na sahip olan Güneydo¤u Anadolu bölgesinde postpartum depresyonu s›n›rlayan en büyük etken akraba ve arkadafl çevresinin puerperal dönemde lohusalara verdi¤i destek olabilir. Anahtar sözcükler: Postpartum dönem, postpartum depresyon. natal changes, newborn care, breast feeding problems, new environment, and changes in social status may cause the health of pregnant woman to deteriorate. A peak in Correspondence: Ali Emre Tahao¤lu, MD. Diyarbak›r Kad›n Do¤um ve Çocuk Hastal›klar› Hastanesi Kad›n Hast. ve Do¤um Klini¤i, Diyarbak›r, Turkey. e-mail: alyemre@yahoo.com Received: April 23, 2014; Accepted: January 5, 2015 Please cite this article as: Tahao¤lu AE, To¤rul C, Külahç›o¤lu M‹, Ayd›n Öztürk B, Balsak D, Bademk›ran H, Gül E, Görkem Ü, Güngör T. Factors affecting postpartum depression in Diyarbak›r. Perinatal Journal 2015;23(1):26–29. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231006 doi:10.2399/prn.15.0231006 QR (Quick Response) Code: Factors affecting postpartum depression in Diyarbak›r the depression rate was reported at postpartum fourth and eighth weeks.[1] In a meta-analysis, it was reported that postpartum depression rate in the first three postpartum months was 14.5%, and major depression criteria were satisfactorily met in 6.5% of postpartum women, and this was at higher levels especially in nullipara population.[1] Changes during pregnancy may bring along many problems and cause stress.[2] The period after pregnancy is 3–4 times more risky in terms of mental illnesses than gestational period.[3] Therefore, possible postpartum depression may constitute a significant health problem. According to Diagnostic and Statistical Manual of Mental Disorders (DSM), having 5 or more of the criteria for at least two weeks is defined as postpartum depression (PPD). These are insomnia-hypersomnia, psychomotor agitation or retardation, fatigue, unhappiness or sense of guilt, decreased concentration, changes in appetite and suicide ideation. These episodes begin within postpartum four weeks and ends within 1 year. According to DSM, PPD is described as non-psychotic major depression.[4] Identifying and preventing postpartum depression in advance is significant in terms of the health of baby and mother. Edinburgh Postpartum Depression Scale (EPDS) can be used to investigate postpartum depression.[5] Although this scale is not diagnostic, sensitivity of PPD is 61.5% and specificity of PPD is 77.4% for those scoring 13 and above.[6] where each option is scored between 0 and 3 and maximum total score is 30.[6] The study was separated into 3 groups according to the age groups which are adolescents, puerperant women who are over 35-year-old and all puerperant women. Statistical analysis was performed by SPSS 15.0 (SPSS Inc., Chicago, IL, USA) and definitive statistics and chi-square test were used. Results The factors affecting postpartum depression were investigated by categorizing 495 puerperant women in the study according to their age groups, which were adolescent puerperant women and puerperant women over 35year-old. As risk factors, their ages, number of their living children, financial status, educational status, delivery type, if they had any emesis problem, gender of baby, depression history and if the pregnancy was intended were asked. Among all the age groups, it was found that only depression history affected PPD (p<0.001). In 101 out of 495 (20.4%) patients, EPDS score was 13 and above. In the factors investigated, it was found that only the depression history was a significant factor affecting postpartum depression in puerperant women (Table 1). Table 1. Statistical analysis of 495 patients. No depression Depression exists (n=394) (n=101) Methods Our study was carried out on 495 puerperant women who referred to Diyarbak›r Maternity and Pediatrics Hospital between September 2012 and May 2013. The approval of the Ethics Committee of Okmeydan› Training and Research Hospital was obtained. Patient consent forms were received from all participants. Women who delivered term babies (at 37 weeks and above) were included in the study. The exclusion criteria included multiple pregnancy, pregnancy by assisted reproductive techniques, history of mental disease diagnosis, antenatal fetal anomaly and mother or baby being in the intense care unit. All puerperant women included in the study on postpartum 8 weeks were asked EPDS questions and factors that may affect postpartum depression. EPDS is a questionnaire with 10 items, each having 4 options p value Age Mean: 26.7±6.6 (14–52) 26.7±6.5 26.5±7.1 0.7540 Number of living children 2.2 (0–10) 3.8 (0–11) 0.115 Financial status 600 TL and below 600–1500 TL 1500–5000 TL 78.4 19.3 2.3 72.3 22.8 5 0.162 Educational level Illiterate Literate Primary school Secondary school High school University 36.3 23.4 23.9 7.1 6.6 2.8 35.6 23.8 19.8 9.9 5.9 5 0.718 Delivery type (C/S) 207 54 0.602 Emesis (present) 64 17 0.887 Depression history (exists) 6 16 <0.001 Gender of baby (male) 198 55 0.452 Planned pregnancy (exists) 41 14 0.325 Volume 23 | Issue 1 | April 2015 27 Tahao¤lu AE et al. It was seen in 495 patients who were analyzed that age, number of living children, educational status, financial status, delivery type, emesis problem, if the pregnancy was intended or not and gender of baby were not significant factors in terms of postpartum depression. Postpartum depression was identified in 51 patients, of which 14 cases (27.4%) were adolescent puerperant women below 18-year-old (Table 2). None of the factors analyzed had a significant effect on postpartum depression. Postpartum depression was identified in 14 (19.4%) out of 72 patients who were puerperant women above 35-year-old (Table 3). None of the factors had any effect on postpartum depression. Discussion Even though the pregnancy and delivery are physiological, they may affect the health of mother and baby in a negative way. While most of the women can adapted to physiological, psychological and social changes occurring during pregnancy and delivery, some women may suffer mental illnesses at different levels.[7] It has been shown that PPD constitutes a risk in motherinfant relationship, and affects cognitive and emotional development of baby.[8] Verbal and visual communication problems of baby and disorders in emotional, cognitive, verbal and social abilities are the negative effects of PPD.[9] In our study, we found that number of living children, financial status, educational level, delivery type, presence of emesis during pregnancy, whether pregnancy being intended or not and gender of baby did not affect postpartum depression. It was observed that only depression history affected postpartum depression. It has been already shown in many studies that depression history is a significant factor affecting postpartum depression.[10,11] In our study, we found that the rate of postpartum depression at postpartum 8 weeks in Diyarbak›r city and nearby regions was 20.4% (according to EPDS, cut-off was 13 and above). The study carried out in Trabzon found PPD rate as 28.1%.[12] However, other studies performed in Turkey found PPD rate as 14.0%, 16.8% and 14.0%, respectively.[11,13,14] We found PPD rate during adolescent period as 27.4% which was the highest result among the age groups. There are 28 Perinatal Journal Table 2. Statistical analysis of puerperant women below 18-year-old. No depression Depression exists (n=37) (n=14) Number of living children p value 1 1 0.079 Financial status 600 TL and below 600–1500 TL 1500–5000 TL 64.9 35.1 - 50 50 - 0.337 Educational level Illiterate Literate Primary school Secondary school High school University 35.1 16.2 16.2 16.2 13.5 2.2 28.6 28.6 14.3 21.4 7.1 - 0.871 Delivery type (C/S) 26 7 0.176 Emesis (present) 5 1 1.000 Depression history (exists) 1 0 1.000 Gender of baby (male) 20 8 0.843 Planned pregnancy (exists) 1 2 0.179 contradictory results among age groups for PPD. Some studies found that being below 25-year-old is a significant factor for PPD.[15,16] Some other studies showed that postpartum depression presented no difference among age groups.[17] The prevalence of postpartum depression during the test period may differ according to population size, Table 3. Statistical analysis of puerperant women above 35-year-old. No depression Depression exists (n=58) (n=14) Number of living children p value 5 (0–10) 5 (0–11) 0.835 Financial status 600 TL and below 600–1500 TL 1500–5000 TL 77.6 17.2 5.2 78.6 14.3 7.1 0.969 Educational level Illiterate Literate Primary school Secondary school High school University 44.8 10.3 20.7 12.1 5.2 6.9 50 14.3 28.6 7.1 0.460 Delivery type (C/S) 20 3 0.525 Emesis (present) 7 4 0.207 Depression history (exists) 2 2 0.168 Gender of baby (male) 34 11 0.166 Planned pregnancy (exists) 3 0 1.000 Factors affecting postpartum depression in Diyarbak›r study design, test type and cut-off value. Mostly, the negative results of this situation which cannot be detected by healthcare professionals on health of mother and baby should be known and it should be on the alert against this mood disorder in puerperant women especially with depression history. Routine screening is performed for postpartum depression diagnosis in some countries such as Australia and the USA.[18] Such screening procedures may also be helpful in Turkey to detect such a complicated condition for baby and mother. The depression rate is correlated with other regions in Anatolia region which has the highest fertility rate in Turkey, and in Diyarbak›r which on the 10th rank for fertility rate.[19] The reason for this situation can be explained with the support from relatives and friends during postpartum period. Conclusion Although postpartum depression is usually overlooked, it is a significant mood disorder, which should be diagnosed and treated, and it affects maternal health and development of baby. Conflicts of Interest: No conflicts declared. References 6. Aydin N, Inandi T, Yigit A, Hodoglugil NN. Validation of the Turkish version of the Edinburgh Postnatal Depression Scale among women within their first postpartum year. Soc Psychiatry Psychiatr Epidemiol 2004;39:483–6. 7. Gülseren L. Do¤um sonras› depresyon: Bir gözden geçirme. Turk Psikiyatri Derg 1999;10:58–67. 8. Murray L, Cooper PJ. Effects of postnatal depression on infant development. Arch Dis Child 1997;77:99–101. 9. Brand SR, Brennan PA. Impact of antenatal and postpartum maternal mental illness: how are the children? Clin Obstet Gynecol 2009;52:441–55. 10. Gonidakis F, Rabavilas AD, Varsou E, Kreatsas G, Christodoulou GN. A 6-month study of postpartum depression and related factors in Athens Greece. Compr Psychiatry 2008;49:275–82. 11. Kirpinar I, Gözüm S, Pasinlio¤lu T. Prospective study of postpartum depression in eastern Turkey prevalence, sociodemographic and obstetric correlates, prenatal anxiety and early awareness. J Clin Nurs 2010;19:422–31. 12. Ayvaz S, Hocao¤lu C, Tiryaki A, Ak I. Incidence of postpartum depression in Trabzon province and risk factors at gestation. [Article in Turkish] Turk Psikiyatri Derg 2006;17: 243–51. 13. Danaci EA, Dinç G, Deveci A, Sen FS, Içelli I. Postnatal depression in Turkey: epidemiological and cultural aspects. Soc Psychiatry Psychiatr Epidemiol 2002;37:125–9. 14. Gulseren L, Erol A, Gulseren S, Kuey L, Kilic B, Ergor G. From antepartum to postpartum: a prospective study on the prevalence of peripartum depression in a semiurban Turkish community. J Reprod Med 2006;51:955–60. 1. Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol 2005; 106:1071–83. 15. Lanes A, Kuk JL, Tamim H. Prevalence and characteristics of postpartum depression symptomatology among Canadian women: a cross-sectional study. BMC Public Health 2011;11:302. 2. Okanl› A, Tortumo¤lu G, K›rp›nar ‹. Gebe kad›nlar›n ailelerinden alg›lad›klar› sosyal destek ile problem çözme becerileri aras›ndaki iliflki. Anadolu Psikiyatri Dergisi 2003; 4:98–105. 16. Inandi T, Elci OC, Ozturk A, Egri M, Polat A, Sahin TK. Risk factors for depression in postnatal first year, in eastern Turkey. Inter J Epidemiol 2002;31:1201–7. 3. Deveci, A. Postpartum psikiyatrik bozukluklar. Birinci Basamak için Psikiyatri 2003;2:42–6. 17. Goker A, Yan›kkerem E, Demet MM, Dikayak S, Yildirim Y, Koyuncu FM. Postpartum depression: is mode of delivery a risk factor? ISRN Obstet Gynecol 2012;2012:616759. 4. American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-IV-tr. 4th ed. Washington DC: American Psychiatric Association; 2000. 5. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782–6. 18. Hübner-Liebermann B, Hausner H, Wittmann M. Recognizing and treating peripartum depression. Dtsch Arztebl Int 2012;109:419–24. 19. Türkiye ‹statistik Kurumu (TÜ‹K). Do¤um ‹statistikleri, 2012. Ankara: TÜ‹K; 2013; Nr. 13618. Volume 23 | Issue 1 | April 2015 29 AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):30–33 R N A PE IN AT U AL JO R Analysis of maternal serum and urinary lipocalin-2 levels Yeflim Bayo¤lu Tekin1, Ülkü Mete Ural1, Aynur K›rbafl2, fienol fientürk1, Figen K›r fiahin1 1 Department of Obstetrics & Gyneceology, Faculty of Medicine, Recep Tayyip Erdo¤an University, Rize, Turkey 2 Department of Biochemistry, Faculty of Medicine, Recep Tayyip Erdo¤an University, Rize, Turkey Abstract Özet: Maternal serum ve üriner lipokalin-2 düzeylerinin de¤erlendirilmesi Objective: Lipocalin-2 is a glicoprotein secreted by leukocytes. It is known that lipocalin-2 levels are affected in maternal blood and urine depending on the endothelial damage induced by preeclampsia, and hyperglycemia created by gestational diabetes. However, there are not sufficient studies investigating the levels in healthy pregnants. In our study, we aimed to determine the changes in lipocalin-2 levels of healthy pregnant women. Amaç: Lipokalin-2 lökositlerden salg›lanan bir glikoproteindir. Preeklampsinin indükledi¤i endotel hasar›na ve gestasyonel diyabetin oluflturdu¤u hiperglisemiye ba¤l› olarak maternal kanda ve idrarda lipokalin-2 düzeylerinin etkilendi¤i bilinmektedir. Ancak sa¤l›kl› gebelerdeki düzeylerini araflt›ran yeterli say›da çal›flma bulunmamaktad›r. Bu çal›flmada sa¤l›kl› gebelerde lipokalin-2 düzeylerindeki de¤iflikliklerin belirlenmesi amaçlanm›flt›r. Methods: This study was carried out as cross-sectional and casecontrolled. Lipocalin-2 levels were determined in blood and urine at first and third trimesters in the same patient group and they were compared. Also, full blood parameters, biochemical and urinary data of the cases were also evaluated. Yöntem: Bu çal›flma kesitsel ve vaka kontrollü olarak yürütülmüfltür. Ayn› hasta grubundan ilk ve üçüncü trimesterde kan ve idrarda lipokalin-2 düzeyleri belirlenerek karfl›laflt›r›lm›flt›r. Ayr›ca olgular›n tam kan parametreleri, biyokimyasal ve üriner verileri de de¤erlendirilmifltir. Results: Lipocalin-2 levels decrease at a statistically significant level in both maternal blood and urine at the third trimester (p<0.05). However, no significant change was found in other hematologic, biochemical and urinary parameters (p>0.05). Bulgular: Lipokalin-2 düzeyleri hem maternal kanda hem de idrarda üçüncü trimesterde istatistiksel olarak anlaml› düzeyde düflmektedir (p<0.05). Ancak di¤er hematolojik, biyokimyasal ve üriner parametrelerde anlaml› de¤ifliklik saptanmam›flt›r (p>0.05). Conclusion: Lipocalin-2 is a new marker used in the early diagnosis of gestational complications such as preeclampsia and gestational diabetes. It is seen that lipocalin-2 levels in healthy pregnant women decrease to lower levels in third trimester compared to first trimester. However, further studies are required with more populations where maternal serum and urine levels are determined longitudinally. Sonuç: Lipokalin-2 preeklampsi ve gestasyonel diyabet gibi gebelik komplikasyonlar›n›n erken tan›s›nda kullan›lan yeni bir markerdir. Sa¤l›kl› gebeliklerde lipokalin-2 seviyelerinin ilk trimestere göre 3. trimesterde daha düflük seviyelere indi¤i görülmektedir. Ancak daha genifl olgu serileri ile longitudinal olarak maternal serum ve idrar düzeylerinin belirlendi¤i çal›flmalara ihtiyaç vard›r. Keywords: Pregnancy, lipocalin-2, biochemical marker. Anahtar sözcükler: Gebelik, lipokalin-2, biyokimyasal marker. Introduction Lipocalin-2 is a glycoprotein weighing 25 kDa from lipocalin family. It was first defined as a matrix protein in granules within human neutronphiles.[1] In different cell types, it has a role as a growth and differentiation factor. Its expression was found in many organs such as liver, kidney and adipose tissue. It was shown that it is also secreted at higher rates in also inflammatory reactions.[2] It has been determined that lipocalin-2 is an inflammatory marker closely associated with insulin resistance and hyperglycemia, and has a role to create insulin resist- Correspondence: Yeflim Bayo¤lu Tekin, MD. Recep Tayyip Erdo¤an Üniversitesi T›p Fakültesi, Kad›n Hastal›klar› ve Do¤um Anabilim Dal›, Rize, Turkey. e-mail: yesimbay@yahoo.com Received: October 4, 2014; Accepted: January 12, 2015 Please cite this article as: Bayo¤lu Tekin Y, Mete Ural Ü, K›rbafl A, fientürk fi, K›r fiahin F. Analysis of maternal serum and urinary lipocalin-2 levels. Perinatal Journal 2015;23(1):30–33. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231007 doi:10.2399/prn.15.0231007 QR (Quick Response) Code: Analysis of maternal serum and urinary lipocalin-2 levels ance for gestational diabetes.[3] It was shown that it is secreted from mature renal epithelium, and it is useful to identify renal damage at early period. Also, it was found that maternal lipocalin-2 levels increased at the early period depending on the preeclampsia.[4] Although lipocalin-2 levels were found to be high in gestational complications such as preeclampsia and gestational diabetes in the literature, there are no sufficient studies evaluating lipocalin-2 levels in normal pregnancies and changes during pregnancy. Our aim in this study is to evaluate lipocalin-2 levels in healthy pregnant women and to determine changes during pregnancy. In this way, it would be more significant to understand if the changes found in gestational complications are physiological responses or the results of the disease pathogenesis. In our study, we aimed to determine and compare lipocalin-2 values at first and third trimesters in healthy pregnant women not complicated by any pregnancy-induced diseases, and to identify the changes in lipocalin-2 levels during pregnancy. Methods This is a cross-sectional case-controlled study. The study was carried out for a year in antenatal polyclinic of a university hospital. The study was approved by the local ethics committee of the university, and the consents of the participants were received by informing them about the study. Pregnant women between 18- and 35-year-old referred to the hospital for their first antenatal visit were included in the study. Patients with chronic hypertension, preeclampsia, pregestational diabetes history or those diagnosed with gestational diabetes in their previous pregnancies were excluded from the study. Also the patients with the history of renal, cardiovascular, autoimmune and hepatobiliary system diseases were excluded from the study. First venous blood and urine samples were collected from the patients who referred within their first trimester during their 9–12 weeks of gestation and found to have single alive fetus. Second blood and urine samples were collected at the visit carried out between 34 and 36 weeks of gestation. Blood and urine samples were first centrifuged and then separated as supernatant, and kept at -20°C. Full blood parameters and routine biochemical and urinary analyses of the participants were done concurrently in order to determine possible additional pathologies and hematologic, biochemical and urinary anomalies which may be induced by pregnancy. Lipocalin-2 serum and urine levels were studied by ELISA method and according to the recommendations of Biovender (Research and Diagnostic Products, Heidelberg, Germany). Intra-assay and inter-assay coefficients of variation (CV) were found as 7.5% and 9.7%. Sensitivity was calculated as 0.02 ng/ml. Statistical analysis was carried out by SPPS statistical software (SPSS Inc., Chicago, IL, USA) version 17.0. Normal distribution of the data was tested by Kolmogorov-Smirnov test and Lilliefor’s correction test. The data displaying normal distribution were provided as mean±standard deviation. Paired-sample test was used to compare first and second blood and urine samples. The value p<0.05 was considered statistically significant. Results Forty healthy pregnant women who referred in their first trimester were included in the study. Five of the cases did not come for their visits. Two cases were excluded from the study due to gestational diabetes and one case due to preeclampsia. The study was completed with a total of 32 cases. Mean age of the participants was 28.9±5.6 and the gravida was 2.0±1.1. Maternal hematologic, biochemical and urinary parameters of first and third trimesters were compared. In both visits, no significant difference was found in hemoglobin, hematocrit and platelet values from full blood parameters and in glucose, BUN, creatinine, ALT, AST and urinary pH and density values from biochemical parameters (Table 1). It was seen that both Table 1. Comparison of maternal serum and urinary parameters according to the trimesters. s-lipocalin-2 (ng/ml) u-lipocalin-2 (ng/ml) Glucose (mg/dL) Creatinine (mg/dL) BUN (mg/dL) ALT (U/L) AST (U/L) WBC (K/uL) Hb (g/dL) Hct (%) PLT (K/uL) u-pH Density First trimester Last trimester P value 78.79±20.4 76.84±62.50 90.84±13.29 0.57±0.07 14.36±4.02 11.45±4.86 14.62±3.15 10.93±1.68 11.3±1.08 33.20±2.48 236.91±61.74 6.37±0.76 1.012±0.004 60.48±20.69 36.34±29.79 92.15±13.07 0.57±0.06 14.8±3.4 11.33±3.96 14.70±2.86 9.94±1.48 11.58±1.33 33.96±2.43 233.47±60.25 6.14±0.56 1013±0.005 0.001 0.022 0.837 0.705 0.530 0.893 0.711 0.053 0.083 0.172 0.431 0.217 0.507 ALT: alanine transaminase; AST: aspartate transaminase; BUN: blood urea nitrogen; Hb: hemoglobin; Hct: hematocrit; PLT: platelet; s-: serum; u-: urinary; WBC: white blood cell. Volume 23 | Issue 1 | April 2015 31 Bayo¤lu Tekin Y et al. urinary and serum lipocalin-2 levels were significantly low in the third trimester compared to the first trimester (Table 1). Discussion In our study, we evaluated maternal serum and urinary lipocalin-2 levels in the first and third trimesters of non-complicated pregnant women, and we found that lipocalin levels of both in urine and serum were significantly lower in the third trimester. In their study, Edelstam et al. evaluated lipocalin-2 levels on healthy pregnant women during the third trimester at 33, 36 and 39 weeks of gestation and postpartum period. They reported that lipocalin-2 levels increased depending on the week of gestation; however, these levels reached their highest values at postpartum period.[5] They stated that increasing lipocalin-2 levels may be associated with postpartum infection. Lipocalin-2 levels are usually the discussion topic of the studies carried out on complicated pregnancies. As being a marker to determine endothelial damage, they are used in studies on preeclampsia.[6] The lipocalin-2 values in pregnant women complicated with preeclampsia were reported at higher levels. It was even shown that this increase induced by endothelial damage began in the second trimester and continued to increase on the third trimester. In these studies where healthy pregnant women were included as control group, it was stated that lipocalin-2 levels were stable in healthy cases.[6] Similarly, Karampas et al. found in their longitudinal studies where healthy pregnant women were compared with pregnant women complicated with preeclampsia and growth retardation that lipocalin-2 levels were similar to normal pregnant women in all three trimesters.[7] Ödum et al. reported that lipocalin-2 in the urine were at high levels in normal pregnant women unlike preeclampsia.[8] However, we observed in our study that lipocalin-2 levels were not stable in normal pregnant women, and they were significantly low both in urine and serum in the third trimester compared to the first trimester. In a study performed on 130 healthy individuals where lipocalin-2 was used to determine renal function and glomerular filtration, serum lipocalin-2 levels of non-pregnant women were compared with the values at all three trimesters of gestation. However, this was not a case-controlled study, and the values at the second trimester were high significantly.[9] 32 Perinatal Journal The strength of our study is to be a case-controlled study. Analysis of lipocalin-2 levels of the same patient group in urine and serum at both first and third trimesters, and significantly low results obtained in both analyses show the reliability of the study. However, small number of population, cases being preconceptional, and non-availability of second trimester and postpartum values are among the limitations of the study. Conclusion Lipocalin-2 is a promising marker as the early identifier of endothelial damage, and for the early diagnosis of preeclampsia as well as glucose intolerance and hyperglycemia. However, in the light of existing studies, it raises concern that lipocalin-2 levels in healthy pregnant women do not have clear standard ranges, and there are contradictory results about the progress of blood and urine levels during pregnancy. The results of our study contribute to the determination of the normal progress of lipocalin-2 in healthy pregnant women as a candidate marker to predict severe gestational complications. On the other hand, further studies with wider populations where reference ranges are determined well according to the trimesters in healthy pregnant women will help to enhance the diagnostic capabilities of lipocalin-2. Conflicts of Interest: No conflicts declared. References 1. Kjeldsen L, Bainton DF, Sengelov H, Borregaard N. Identification of neutrophil gelatinase-associated lipocalin as a novel matrix protein of specific granules in human neutrophils. Blood 1994;83:799–807. 2. Cowland JB, Sorensen OE, Sehested M, Borregaard N. Neutrophil gelatinase-associated lipocalin is up-regulated in human epithelial cells by IL-1 beta, but not by TNF-alpha. J Immunol 2003;171:6630–9. 3. Lou Y, Wu C, Wu M, Xie C, Ren L. The changes of neutrophil gelatinase-associated lipocalin in plasma and its expression in adipose tissue in pregnant women with gestational diabetes. Diabetes Res Clin Pract 2014;104:136– 42. 4. D’Anna R, Baviera G, Giordano D, Todarello G, Corrado F, Buemi M. Second trimester neutrophil gelatinase-associated lipocalin as a potential prediagnostic marker of preeclampsia. Acta Obstet Gynecol Scand 2008;87:1370–3. Analysis of maternal serum and urinary lipocalin-2 levels 5. Edelstam G, Löwbeer C, Kral G, Gustafsson SA, Venge P. New reference values for routine blood samples and human neutrophilic lipocalin during third-trimester pregnancy. Scand J Clin Lab Invest 2001;61:583–92. metalloproteinase-9 (MMP-9) and their complex MMP9/NGAL in pregnancies with preeclampsia and those with a small for gestational age neonate: a longitudinal study. Prenat Diagn 2014;34:726–33. 6. D’Anna R, Baviera G, Giordano D, Todarello G, Russo S, Recupero S, et al. Neutrophil gelatinase-associated lipocalin serum evaluation through normal pregnancy and in pregnancies complicated by preeclampsia. Acta Obstet Gynecol Scand 2010;89:275–8. 8. Ødum L, Andersen AS, Hviid TV. Urinary neutrophil gelatinase-associated lipocalin (NGAL) excretion increases in normal pregnancy but not in preeclampsia. Clin Chem Lab Med 2014;52:221–5. 7. Karampas G, Eleftheriades M, Panoulis K, Rizou M, Haliassos A, Hassiakos D, et al. Maternal serum levels of neutrophil gelatinase-associated lipocalin (NGAL), matrix 9. Ma∏yszko JS, Rams L, Drozdowska-Rams L, Ma∏yszko J. Serum neutrophil gelatinase-associated lipocalin as a marker of kidney function in pregnancy – useful or doubtful? Arch Med Sci 2010;6:744–7. Volume 23 | Issue 1 | April 2015 33 AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):34–38 R N A PE IN AT U AL JO R Critical pulmonary stenosis with prenatal diagnosis: a case series and review of literature Oya Demirci1, Taner Yavuz2, Resul Ar›soy1, Emre Erdo¤du1, P›nar Kumru1, Oya Pekin1 1 Perinatology Clinic, Zeynep Kamil Maternity and Pediatrics Training and Research Hospital, Istanbul, Turkey Pediatric Cardiology Unit, Zeynep Kamil Maternity and Pediatrics Training and Research Hospital, Istanbul, Turkey 2 Abstract Özet: Prenatal tan›l› kritik pulmoner stenoz: Olgu serisi ve literatür derlemesi Objective: The aim of the study is to investigate the morphology of right ventricular cavity, the tricuspid valve size and the treatments applied at postnatal period in cases with critical pulmonary stenosis (PS) having intact ventricular septum. Amaç: Ventriküler septumu intakt olan kritik pulmoner stenozlu (PS) olgularda sa¤ ventrikül kavitesinin morfolojisi, triküspit kapak boyutu ve postnatal uygulanan tedavilerin de¤erlendirilmesi amaçlanm›flt›r. Methods: Seven cases included in the study who were considered to have critical PS in fetal echocardiography at second and third trimesters. The fetuses found to have antegrade jet stream at pulmonary valve level and reverse flow at ductus arteriosus as well as hyperthrophy and hypoplasia on the right ventricle were determined as critical PS. The cases were categorized as bipartite or tripartite according to the morphology of right ventricular cavity. Z-score of tricuspid valve was calculated according to the week of gestation. Yöntem: Çal›flmaya ikinci ve üçüncü trimestrede fetal ekokardiyografide kritik PS düflünülen 7 olgu al›nd›. Sa¤ ventrikülde hipertrofi ve hipoplazinin yan› s›ra pulmoner kapak seviyesinde ileri yönde jet ak›m ve duktus arteriozusta ters ak›m saptanan fetüsler kritik PS olarak de¤erlendirildi. Sa¤ ventrikül kavitesinin morfolojisine göre olgular bipartit veya tripartit olarak ayr›ld›. Gestasyon haftas›na göre triküspit kapak Z-skoru hesapland›. Results: Bipartite right ventricle cavity was found in cases diagnosed at second trimester, and tripartite right ventricle cavity in cases diagnosed at third trimester. Tricuspid valve Z-score of the cases with bipartite right ventricle morphology was less than those with tripartite. Two out of seven cases were monochorionic diamniotic twin pregnancies. Balloon valvuloplasty was performed on postnatal second day despite the prostaglandin E1 (PGE1) infusion in 3 cases with bipartite, and 3 cases required Blalock-Taussing shunt. In four tripartite cases, cyanosis control was better by PGE1 infusion, and balloon valvuloplasty was performed on postnatal second day in 3 cases and on postnatal 55th day in 4 cases. No Blalock-Taussing shunt was required. Conclusion: In critical PS cases, the treatment methods to be applied during postnatal period may vary according to the right ventricle being of two or three parts and the stenosis level of tricuspid valve. Keywords: Critical pulmonary stenosis, tricuspid stenosis, tricuspid deficiency, postnatal treatment. Bulgular: ‹kinci trimesterde tan› konulan olgularda bipartit, üçüncü trimesterde tan› konulan olgularda tripartit sa¤ ventrikül kavitesi belirlendi. Bipartit sa¤ ventrikül morfolojili olgular›n triküspit kapak Z-skoru, tripartit olanlardan daha düflük olarak hesapland›. Yedi olgunun ikisi monokoryonik diamniyotik ikiz gebelikti. Bipartit olan 3 olguda prostaglandin E1 (PGE1) infüzyonuna ra¤men postnatal 2. günde balon valvüloplasti yap›ld› ve 3 olguda da Blalock-Taussing flant gereksinimi oldu. Tripartit dört olguda ise PGE1 infüzyonu ile siyanoz kontrolü daha iyi sa¤lanm›fl, üç olguda postnatal 2. haftada, dördüncü olguda ise postnatal 55. günde balon valvüloplasti uyguland›. Blalock-Taussing flant gereksinimi olmad›. Sonuç: Kritik PS olgular›nda sa¤ ventrikülün iki ya da üç parçal› olma durumuna, triküspit kapa¤›n darl›k derecesine ba¤l› olarak postnatal dönemdeki uygulanacak tedavi yöntemleri de¤iflebilmektedir. Anahtar sözcükler: Kritik pulmoner stenoz, triküspit darl›k, triküspit yetmezlik, postnatal tedavi. Correspondence: Oya Demirci, MD. Zeynep Kamil Kad›n ve Çocuk Hastal›klar› E¤itim ve Araflt›rma Hastanesi, Perinatoloji Klini¤i, ‹stanbul, Turkey. e-mail: demircioya@gmail.com Received: October 27, 2014; Accepted: January 24, 2015 Please cite this article as: Demirci O, Yavuz T, Ar›soy R, Erdo¤du E, Kumru P, Pekin O. Critical pulmonary stenosis with prenatal diagnosis: a case series and review of literature. Perinatal Journal 2015;23(1):34–38. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231008 doi:10.2399/prn.15.0231008 QR (Quick Response) Code: Critical pulmonary stenosis with prenatal diagnosis Introduction Critical pulmonary stenosis (PS) causes reverse flow in the ductus arteriosus of fetus and severe right ventricular hypertrophy. Secondary to hypertrophy, the right ventricular cavity gets narrow especially at apex. During neonatal period, it causes shunt and cyanosis at interatrial level from right to left. Critical PS can also be evaluated within pulmonary atresia with intact ventricular septum (PAIVS) due to the fact that it may progress to pulmonary atresia (PA) as week of gestation advances.[1] The most distinguishing characteristic of the fetus with critical pulmonary stenosis from mild and medium PS is the reverse flow of ductus arteriosus seen in ultrasonographic examination.[1,2] There is no concomitant genetic disease or extra cardiac anomaly in most of the PAIVS and critical PS cases.[1] The abnormal appearance in quadrilocular during cardiac examination between 18 and 22 weeks of gestation at second trimester is usually the most striking characteristics and it initiates the process toward the diagnosis. However, although some cases have PS at critical levels, the sizes of right ventricle may seem normal and it may cause late diagnosis. In some other cases, PAIVS and critical PS diagnosis may be established even at the first trimester.[1] Right ventricular cavity morphologically consists of three parts which are inlet, apex and outlet. Ventricular hyperthropy occurs at various levels depending on the size of narrowing of the right ventricular outlet and the week of gestation that pulmonary atresia occurs, stenosis on tricuspid valve and the level of failure.[1] As a result of the overgrowth of intracavity muscular layer, apex of right ventricle (bipartite) or both apex and outlet (unipartite) may not develop. In critical PS, right ventricle usually has all three parts (tripartite). Sometimes, apical region may not develop well and may have bipartite morphology as in PAIVS.[1,2] Z-score is used when evaluating tricuspid valve size.[1–3] In cases which developed right ventricular hypoplasia with bipartite and unipartite morphology, severe tricuspid valve stenosis (low Z-score) is also observed.[1,2] For newborns with critical pulmonary stenosis, various treatment options are offered according to right ventricular morphology usually at postnatal early period such as balloon valvuloplasty, ductal stent, BlalockTaussing (BT) shunt operation, biventricular repair at advanced periods, and Glenn or Fontan procedures. In our study, we aimed to investigate the morphology of right ventricular cavity, tricuspid valve Z-scores and treatments applied in cases with critical pulmonary stenosis (PS) having intact ventricular septum. Methods Seven cases considered having critical PS in fetal echocardiography at second and third trimesters at the Perinatology Clinic of Zeynep Kamil Maternity and Pediatrics Training and Research Hospital between 2013 and 2014 were included in the study. The fetuses found to have antegrade jet stream at pulmonary valve level and reverse flow at ductus arteriosus as well as hyperthrophy and hypoplasia on the right ventricle were suspected to be critical PS. The cases with postnatal clinical progress and echocardiography findings compatible with critical PS were included in the study. The cases were categorized as bipartite or tripartite according to the morphology of right ventricular cavity. Zscore of tricuspid valve was calculated according to the week of gestation.[3] Tricuspid valve insufficiency was categorized as mild, medium and severe.[4,5] Ultrasonographic examinations were performed with the use of Voluson 730 Pro (GE Healthcare, Milwaukee, WI, USA). Transthoracic echocardiography was carried out on the first day after the delivery. Prenatal and postnatal echocardiography measurements were evaluated by pediatric cardiology and perinatology departments. Statistical analysis was done by SPSS v. 11.5 (SPSS, Inc., Chicago, IL, USA). Constant data were provided as median. Results Median week of gestation for the cases was 32 (range: 24 to 34) weeks when prenatal diagnosis was established. In the fetal ultrasonography during second trimester for the cases which were diagnosed at third trimester, the size of right ventricle was normal, and no abnormality was observed at the right ventricle outlet. Bipartite right ventricle cavity was found in cases diagnosed at second trimester, and tripartite right ventricle cavity in cases diagnosed at third trimester. No case developed pulmonary atresia. Median delivery week was 37 (range: 37 to 39 weeks) and median birth weight was 2950 (2570–3060) g. Two of the seven cases were monochorionic diamniotic twin pregnancy, and twinto-twin transfusion syndrome was not developed in either case. One of the twin pregnancies delivered at 37 Volume 23 | Issue 1 | April 2015 35 Demirci O et al. weeks of gestation while the other one at 34 weeks of gestation. Development of fetuses was normal in the twin pregnancy which delivered at 37 weeks of gestation; however, selective intrauterine growth retardation (IUGR) developed in the other twin pregnancy delivered at 34 weeks of gestation. While critical PS was observed in the elder fetus, there was perimembranous ventricular septal defect in the donor fetus. Chromosome examinations of all cases were normal; one case had anal atresia. Tricuspid valve Z-score of the cases with bipartite right ventricle morphology was less than those with tripartite. Also, in 5 cases with negative tricuspid valve Z-score, medium tricuspid failure was detected. Prostaglandin E1 (PGE1) infusion was initiated in all cases as soon as they were born. In 3 bipartite cases, cyanosis developed at early period despite the PGE1 infusion, and all had balloon valvuloplasty on postnatal second day. In one case, BT shunt was performed since cyanosis continued on 5th day after balloon valvuloplasty, no problem observed during 3month follow-up. Another case had operation due to anal atresia after valvuloplasty; when cyanosis increased after the operation, the case was referred for BT shunt but passed away when 15-day-old before shunt was applied. The other 37-week-old twin with bipartite morphology was applied BT shunt at the same day since sufficient clinical response was not received after balloon valvuloplasty. Clinical findings were stable during 3-month clinic follow-up. In four tripartite cases, cyanosis was kept under control better with PGE1 infu- sion; balloon valvuloplasty was applied in 3 cases on postnatal 2nd week (9th, 11th and 12th day, respectively); also ductal stent was placed to one case (case nr. 6). Fourth case was monitored in the newborn intense care unit for 54 days by PGE1 treatment on receptor baby developing selective IUGR; and balloon valvuloplasty was applied on 55th day (Table 1). Discussion Critical PS is a cardiac anomaly which is present at postnatal early period together with right ventricular hypoplasia and where pulmonary circulation depends on ductus. It requires postnatal emergency medical and invasive/surgical treatment. Therefore, diagnosing at prenatal period and delivering at a tertiary center are very significant in terms of applying prostoglandin E1 treatment at postnatal period without any delay and to make preparations for required procedures afterwards. In our study, we aimed to discuss treatment methods applied at postnatal period according to the right ventricular morphologies of 7 cases which were diagnosed as critical PS during prenatal period. In cases where right ventricular outlet of fetal is congested or closed, it is the tricuspid valve size which determines the development level of right ventricle.[1] The postnatal treatment planning of critical PS and PAIVS cases is determined according to tricuspid valve Z-scores.[6] In compliance with the literature, we found that tricuspid valve Zscores of those with bipartite right ventricular morphol- Table 1. Summary of the prenatal and postnatal data of 7 cases with critical pulmonary stenosis. Case Week of Chromosomal/ gestation- extra-cardiac diagnosis anomaly Week of gestation and weight (percentile) Cardiac Right insufficiency, ventricle/ hydrops component Tricuspid insufficiency– stenosis/Z-score Postnatal treatment 1 25 n/a 39-2950 g (10–50p) n/a Two Exists–medium /-2.02 Balloon valvuloplasty on 2nd day BT shunt on 5th day - ALIVE 2 24 Anal atresia 37-2650 g (10–50p) n/a Two Exists–medium /-2.05 Balloon valvuloplasty on 2nd day Exitus on 15th day before BT shunt 3 22 MCDA twin n/a 37-2570 g (10–50p) n/a Two Exists – medium/-2.65 Balloon valvuloplasty on 2nd day BT shunt on 2nd day - ALIVE 4 36 n/a 37-3000 g (10–50p) n/a Three n/a/0.17 Balloon valvuloplasty on 9th day – ALIVE 5 34 n/a 39-3060 g (10–50p) n/a Three n/a/0.14 Balloon valvuloplasty on 11th day – ALIVE 6 32 n/a 38-2450 g (10–50p) n/a Three Exists–mild /-0.49 Balloon valvuloplasty on 12th day+ ductal stent – ALIVE 7 34 MCDA twin n/a 34-3150 g (50–95p) n/a Three Exists–mild /-0.65 Balloon valvuloplasty on 55th day – ALIVE 36 Perinatal Journal Critical pulmonary stenosis with prenatal diagnosis ogy were less than those with tripartite.[2,7-9] Given the treatments applied during postnatal period, those with bipartite were required to have balloon valvuloplasty despite the prostaglandin treatment and also BT shunt was required since there was no sufficient recovery. Similar to our study, Cho et al. reported that BT shunt requirement was higher in those with bipartite right ventricular cavity among critical PS and PAIVS cases.[10] Many studies highlighted that prenatal tricuspid valve sizes are significant to predict prognosis during postnatal period.[2,7-9] The narrowing of tricuspid valve affects right ventricular development negatively while tricuspid valve deficiency affects right ventricular development positively. Therefore, in cases with high level of narrowing on tricuspid valve, the tricuspid valve deficiency is significant for the development of right ventricle.[1] In our study, we found distinctive tricuspid valve deficiency in our 3 bipartite cases which had distinctive narrowing of tricuspid valve (Z-score <-2). It is considered that the tricuspid valve deficiency increases the volume load on right ventricle and supports the development of right ventricle.[1] In cases having only narrowing on the tricuspid valve without any deficiency, it is possible to observe muscular pulmonary atresia as a result of the overgrowth of muscle layer on infundibular area.[11] Similarly, Lowenthal et al. reported that postnatal prognosis was better in PAIVS and critical PS cases with mid- and severe deficiency on tricuspid valve.[7] trimester since hyperthrophy on right ventricle increases gradually.[15,16] In monochorionic twin pregnancies, especially in twin-to-twin transfusion syndrome, the narrowing or atresia on the right ventricular outlet of the receptor fetus was higher than the normal population.[12–14] In our two cases with monochorionic twin pregnancies, twin-to-twin transfusion syndrome did not develop. On the other hand, one case had selective IUGR and critical pulmonary stenosis was found in elder fetus. Similarly, Gardiner et al. reported in their series of 21 cases that there were 2 cases with monochorionic twin pregnancy which did not develop twin-to-twin transfusion syndrome.[2] While we diagnosed one of our twin pregnancy cases at second trimester, we diagnosed other one at third trimester, and we did not found any cardiac pathology in second trimester ultrasonography. In the ultrasonographic screening at 18-22 weeks, right ventricle can be seen at relatively normal size, and therefore it can be overlooked. At the same time, the narrowing on right ventricular outlets displays progression and we are able to detect such patients at third References In cases with critical PS, chromosomal anomaly and extra cardiac anomaly are quite rare. Similarly, we found in our study no chromosomal anomaly, but anal atresia as extra cardiac anomaly only in one case. Generally, cardiac failure and intrauterine growth retardation are not observed during intrauterine period in cases with PAIVS and critical pulmonary stenosis.[1] Correlatively, our cases did not develop any cardiac failure finding. Except the twin pregnancy with selective intrauterine growth retardation, we did not find intrauterine growth retardation in any of our cases. Conclusion Consequently, in critical PS cases, the treatment methods to be applied during postnatal period may vary according to the right ventricle being of two or three parts and the stenosis level of tricuspid valve. Therefore, diagnosing at prenatal period and categorizing cases will facilitate to maintain postnatal hemodynamic stability and to plan required invasive and/or surgical treatment options by initiating prostaglandin treatment. Conflicts of Interest: No conflicts declared. 1. Yagel S, Silverman NH, Gembruch U. Fetal Cardiology: Embryology, Genetics, Physiology, Echocardiographic Evaluation, Diagnosis and Perinatal Management of Cardiac Diseases (Series in Maternal Fetal Medicine). 2nd ed. London: Informa Helatcare; 2008; p: 267–80. 2. Gardiner HM, Belmar C, Tulzer G, Barlow A, Pasquini L, Carvalho JS, et al. Morphologic and functional predictors of eventual circulation in the fetus with pulmonary atresia or critical pulmonary stenosis with intact septum. J Am Coll Cardiol 2008;51:1299–308. 3. Schneider C, McCrindle BW, Carvalho JS, Hornberger LK, McCarthy KP, Daubeney PE. Development of Z-scores for fetal cardiac dimensions from echocardiography. Ultrasound Obstet Gynecol 2005;26:599–605. 4. Bolger AF, Eigler NL, Maurer G. Quantifying valvular regurgitation. Limitations and inherent assumptions of Doppler techniques. Circulation 1988;78:1316–8. 5. Rivera JM, Vandervoort PM, Vazquez de Prada JA, Mele D, Karson TH, Morehead A, et al. Which physical factors determine tricuspid regurgitation jet area in the clinical setting? Am J Cardiol 1993;72:1305–9. Volume 23 | Issue 1 | April 2015 37 Demirci O et al. 6. Hanley FL, Sade RM, Blackstone EH, Kirklin JW, Freedom RM, Nanda NC. Outcomes in neonatal pulmonary atresia with intact ventricular septum. A multiinstitutional study. J Thorac Cardiovasc Surg 1993;105:406–23. 11. Davignon AL, Greenwold WE, Dushane JW, Edwards JE. Congenital pulmonary atresia with intact ventricular septum. Clinicopathologic correlation of two anatomic types. Am Heart J 1961;62:591–602. 7. Lowenthal A, Lemley B, Kipps AK, Brook MM, MoonGrady AJ. Prenatal tricuspid valve size as a predictor of postnatal outcome in patients with severe pulmonary stenosis or pulmonary atresia with intact ventricular septum. Fetal Diagn Ther 2014;35:101–7. 12. Zosmer N, Bajoria R, Weiner E, Rigby M, Vaughan J, Fisk NM. Clinical and echographic features of in utero cardiac dysfunction in the recipient twin in twin-twin transfusion syndrome. Br Heart J 1994;72:74–9. 8. Peterson RE, Levi DS, Williams RJ, Lai WW, Sklansky MS, Drant S. Echocardiographic predictors of outcome in fetuses with pulmonary atresia with intact ventricular septum. J Am Soc Echocardiogr 2006;19:1393–400. 9. Salvin JW1, McElhinney DB, Colan SD, Gauvreau K, del Nido PJ, Jenkins KJ, et al. Fetal tricuspid valve size and growth as predictors of outcome in pulmonary atresia with intact ventricular septum. Pediatrics 2006;118:e415–20. 10. Cho MJ, Ban KH, Kim MJ, Park JA, Lee HD. Catheterbased treatment in patients with critical pulmonary stenosis or pulmonary atresia with intact ventricular septum: a single institute experience with comparison between patients with and without additional procedure for pulmonary flow. Congenit Heart Dis 2013;8:440–9. 38 Perinatal Journal 13. Lougheed J, Sinclair BG, Fung Kee Fung K, Bigras JL, Ryan G, Smallhorn JF, et al. Acquired right ventricular outflow tract obstruction in the recipient twin in twin-twin transfusion syndrome. J Am Coll Cardiol 2001;38:1533–8. 14. Herberg U, Gross W, Bartmann P, Banek CS, Hecher K, Breuer J. Long term cardiac follow up of severe twin to twin transfusion syndrome after intrauterine laser coagulation. Heart 2006;92:95–100. 15. Todros T, Paladini D, Chiappa E, Russo MG, Gaglioti P, Pacileo G, et al. Pulmonary stenosis and atresia with intact ventricular septum during prenatal life. Ultrasound Obstet Gynecol 2003;21:228–33. 16. Paladini D, Volpe P. Ultrasound of Congenital Fetal Anomalies: Differential Diagnosis and Prognostic ‹ndicators. 2nd ed. Boca Raton, FL: CRC Press; 2014; p: 184–6. AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):39–44 R N A PE IN AT U AL JO R Evaluation of prenatal invasive procedures: analysis of retrospective cases Aybike Tazegül Pekin1, Özlem Seçilmifl Kerimo¤lu1, Setenay Arzu Y›lmaz1, Nadir Koçak2, Feyza Nur ‹ncesu1, Ayfle Gül Kebapc›lar1, Çetin Çelik1 1 Department of Gynecology & Obstetrics, Faculty of Medicine, Selçuk University, Konya, Turkey 2 Department of Medical Genetics, Faculty of Medicine, Selçuk University, Konya, Turkey Abstract Özet: Prenatal invaziv giriflimlerin de¤erlendirilmesi: Retrospektif olgular›n analizi Objective: In this study, we aimed to present the results of prenatal invasive procedures carried out in our clinic. Amaç: Bu çal›flmam›zda amaç, klini¤imizde uygulanan prenatal invaziv giriflimlerin sonuçlar›n› sunmakt›r. Methods: The records of the prenatal invasive procedures carried out between April 2011 and 2014 were analyzed retrospectively, and the indications, complications and karyotype results of invasive procedures were evaluated. Yöntem: Nisan 2011–2014 tarihleri aras›nda uygulanan prenatal invaziv giriflimlerin kay›tlar› retrospektif olarak tarand›, invaziv giriflimlerin endikasyonlar›, komplikasyonlar› ve karyotip sonuçlar› de¤erlendirildi. Results: Prenatal invasive procedure was applied to 72 (23.4%) pregnant women who had only minor and/or major anomalies according to ultrasonography, 226 (73.3%) patients who referred for increased risk at screening tests, 5 (1.6%) patients with family history and 5 (1.6%) patients with advanced maternal age. Amniocentesis was carried out for 81.8% (n=252) of these patients, chorionic villus sampling for 11.7% (n=36) of them, and cordocentesis due to advanced week of gestation for 6.5% (n=20) of them. Karyotype analysis results were normal in 278 (90.2%) patients but no cytogenetic result was obtained in 11 (3.5%) patient, and aneuploidy was reported in 19 (6.2%) patients (trisomy in 2.9% and other genetic anomalies / variations in 3.3%). Two patients with karyotype results as 46XX+22p and 46XY,9qh were followed up. The results of the patients whose ultrasonography examination did not show any minor marker or major anomaly were considered as normal variants. Such pregnancies resulted in healthy live births. Karyotype anomalies also having ultrasonography findings were terminated. Bulgular: Ultrasonografide tespit edilen sadece minör ve/veya majör anomalisi olan 72 (%23.4) gebeye, tarama testlerinde artm›fl risk nedeniyle baflvuran 226 (%73.3) hastaya, aile öyküsü olan 5 (%1.6) hastaya ve ileri anne yafl› nedeniyle 5 (%1.6) hastaya prenatal invaziv giriflim uyguland›. Bu hastalar›n %81.8’ine (n=252) amniyosentez, %11.7’sine (n=36) koryon villus biyopsisi, %6.5’ine (n=20) ileri gebelik haftas› nedeniyle kordosentez uyguland›. Karyotip analizi sonuçlar› 278 (%90.2) hastada normal, 11 (%3.5) hastada sitogenetik sonuç al›namad› ve 19 (%6.2) hastada anöploidi, (%2.9 trizomi ve %3.3 di¤er genetik anormallikler/ varyasyonlar) olarak bildirildi. Karyotip sonucu, 46XX+22p ve 46XY,9qh olan 2 hasta takip edildi. Ultrasonografi de¤erlendirmesinde minör belirteç veya majör anomali saptanmayan hastalar›n sonuçlar› normal varyant olarak kabul edildi. Bu gebelikler sa¤l›kl› canl› do¤um ile sonuçland›. Ultrasonografi bulgular› da olan karyotip anomalileri termine edildi. Conclusion: Prenatal screening tests are still the major indications for prenatal invasive procedures. However, minor and/or major anomalies can be displayed in most of the aneuploidic fetuses; therefore, fetuses established with prenatal diagnosis indication should be evaluated carefully. Keywords: Prenatal diagnosis, amniocentesis, chorionic villus sampling. Sonuç: Prenatal tarama testleri halen prenatal invaziv giriflimlerin ilk s›radaki endikasyonlar›n› oluflturmaktad›r. Ancak minör ve/veya majör anomaliler anöploidik fetüslerin büyük k›sm›nda görüntülenebilmektedir, bu nedenle prenatal tan› endikasyonu konulan fetüsler dikkatle de¤erlendirilmelidir. Anahtar sözcükler: Prenatal tan›, amniyosentez, koryon villus biyopsisi. Correspondence: Aybike Tazegül Pekin, MD. Selçuk Üniversitesi T›p Fakültesi Kad›n Hastal›klar› ve Do¤um Anabilim Dal›, Konya, Turkey. e-mail: aybiketzgl@hotmail.com Received: October 18, 2014; Accepted: February 1, 2015 Please cite this article as: Tazegül Pekin A, Seçilmifl Kerimo¤lu Ö, Y›lmaz SA, Koçak N, ‹ncesu FN, Kebapc›lar AG, Çelik Ç. Evaluation of prenatal invasive procedures: analysis of retrospective cases. Perinatal Journal 2015;23(1):39–44. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231009 doi:10.2399/prn.15.0231009 QR (Quick Response) Code: Tazegül Pekin A et al. Introduction Methods In pregnancies with the risk of fetal chromosomal anomaly, chorionic villus sampling (CVS) at the first trimester, amniocentesis at the second trimester and invasive prenatal diagnosis methods such as cordocentesis at further weeks may be carried out for diagnostic purposes. While all these prenatal invasive methods can be done mainly for fetal karyotype analysis, they also can be carried out to identify single gene diseases such as sickle cell anaemia or thalassemia major, and to investigate fetal infections, fetal blood type, hematocrit value, enzymes associated with metabolic diseases and lung maturation.[1] Fetal blood transfusion, amnioreduction, amnioinfusion, fetal shunt and laser practices can be can be listed as the other invasive procedures for fetal treatment purposes.[1] During a few decades, invasive procedure indications have become based on nuchal translucency and maternal serum biochemistry parameters rather than being based on advanced maternal age.[2,3] In this way, with the use of first trimester screening tests, CVS practices have become prevalent and they have enabled earlier diagnosis. Also, using maternal serum markers has increased the detection rates and decreased false positivity rates, thus decreased invasive procedure rates. With the tests analyzing cell-free fetal DNA (cfDNA) becoming popular recently, the decrease of false positivity and invasive procedure rates is expected.[4,5] Karyotype analysis can be done in case of advanced maternal age, trisomy in previous pregnancy or history of fetus with sex chromosome anomaly, presence of translocation, inversion or chromosomal anomaly in spouses, markers indicating aneuploidy or presence of major anomaly in the ultrasonography, positive prenatal test results, increased nuchal translucency and maternal anxiety.[6,1] Amniocentesis is considered to be the easiest method with the least risk for maternal and fetal morbidity among prenatal invasive diagnosis methods.[7] American College of Obstetricians and Gynaecologists (ACOG) reports the risk of pregnancy loss associated with the procedure during amniocentesis performed after 15 weeks of gestation as 1/300–500.[6] Also, it is reported in experienced centers that the risk of pregnancy loss with CVS is similar with amniocentesis.[6] Fetal loss risk after cordocentesis is shown as 1.4%.[8] In our study, we aimed to present the results of prenatal invasive procedures that we carried out with various indications in our clinic. A total of 308 pregnant women were included in the study who were applied prenatal invasive procedures for the purpose of karyotype analysis between 2011 and 2014 in our clinic. The approval of Ethics Committee of the Selçuk University Hospital was obtained for the study. The consent forms were received from the patients in our clinic by informing them that their ultrasound images and genetic results can be used in the study before the examination and the procedure. The cases were evaluated retrospectively in terms of invasive procedure indications, cell culture success, genetic results and fetal prognosis. The pregnant women with risk rate over 1/250 according to the first trimester combined test result, the pregnant women with risk rate over 1/300 according to second trimester screening tests, pregnant women having major anomaly or ultrasonographic markers which may be associated with fetal karyotype anomaly, pregnant women who are above 40-year-old but did not have any prenatal screening test and pregnant women with karyotype anomaly risk in their obstetric history were recommended invasive procedures appropriate for their weeks of gestation. The patients and their spouses were informed about the indication related with the procedure, the technique to be applied, complications and the rates to accomplish result and their written consents were received. Before the procedure, blood type and HIV and hepatitis B serology of pregnant women were evaluated. CVS was carried out transabdominally between 11 and 14 weeks of gestation under sterile conditions with 18-Gauge (G) needle. Classical amniocentesis procedure at appropriate week of gestation was preferred in cases with retroverted uterus or posterior located placenta which were technically not suitable for transabdominal CVS procedure. Amniocentesis procedure was carried out between 15 and 20 weeks of gestation with 21-G needle under sterile conditions by entering through a distant zone from placenta and aspiring 1–2 ml fluid for each week of gestation. First 2 ml amniotic fluid was not examined in order to avoid maternal contamination. Cordocentesis procedure was carried out by using 22-G needle in pregnancies older than 21 weeks. By entering through the placental insertion zone or free floating area of umbilical cord, 2–3 ml fetal blood was collected from umbilical vein with an injector washed with heparin. Voluson 730 Expert (General Electric Healthcare, Milwaukee, WI, USA) and 3.5 MHz convex probe were used during the procedures. The procedure was carried out after fetus 40 Perinatal Journal Evaluation of prenatal invasive procedures and placenta were examined systematically. After the procedure, a single dose of 300 microgram anti-D immunoglobulin was administered intramuscularly to the pregnant women with Rh alloimmunization risk. Routine antibiotic prophylaxis was not applied. The patients were discharged in the same day. Fetal loss within three weeks following the procedure was considered as the complication of the procedure. The samples collected for genetic analysis were cultured for 1 week for CVS, for 3 days for cordocentesis and for approximately 15–20 days for amniocentesis through the methods suitable for the samples, and culture extractions were done. Metaphase preparations obtained after the culture were stained by using Trypsin Giemsa banding method (GTG). In all cases, 25 metaphase plates were evaluated for structural irregularities and 50 metaphase plates were evaluated for numerical irregularities. Computerized analysis system was used in karyotyping analysis. Chromosomal anomalies were defined according to International System for Human Cytogenetic Nomenclature (ISCN) 2009.[9] The statistical analysis of data was done by using SPSS software, version 16.0 (SPSS, Inc., Chicago, IL, USA). The data in parametric tests were provided as mean±standard deviation. Percentage values were used in groups. Results Of 308 pregnant women who undergone invasive procedures, mean age was 31.3±6.4 (range: 16 to 46) years, gravida was 2.4±1.1 (range: 1 to 7) and parity was 1.2±1.0 (range: 0 to 6). Prenatal invasive test was applied to 72 (23.4%) pregnant women who had only minor and/or major anomalies according to ultrasonography, 226 (73.3%) patients who referred for increased risk at screening tests, 5 (1.6%) patients with family history and 5 (1.6%) patients with advanced maternal age. The most frequent invasive procedure indications were increased risk at triple test (46%), major and/or minor anomalies (23.4%), increased risk at first trimester combined test (17%) and increased risk at quad test (10.3%) (Fig. 1). Increased nuchal thickness (2.9%) and increased nuchal translucency (2.3%) where the most frequent ultrasonographic findings among karyotype analysis indications (Table 1). Amniocentesis was carried out for 81.8% (252) of these patients, CVS for 11.7% (36) of them, and cordocentesis due to advanced week of gestation for 6.5% (20) of them. Karyotype analysis results were nor- Fig. 1. The rates of invasive procedure indications. mal in 278 (90.2%) patients but no cytogenetic result was obtained in 11 (3.5%) patient, and aneuploidy was reported in 19 (6.2%) patients (trisomy in 2.9% and other genetic anomalies/variations in 3.3%) (Table 2). Cordocentesis was applied to one (0.3%) of the cases without cytogenetic result, CVS was applied to two (0.6%) of them and amniocentesis was applied to eight (2.5%) of them. There was ultrasonographic marker in 16 (84.2) of 19 fetuses found to have aneuploidy. The results of two patients, whose karyotype results were 46XX+22p and 46XY,9qh but there was no ultrasonographic finding, were considered as normal variant and followed up. Such pregnancies resulted in healthy live births. The follow-ups of two patients whose chromosomal analysis results were found as 46XX/47XX+ mar (live healthy delivery) and 46XY,inv(9) (intrauterine fetal death at 33 weeks) were discontinued. Gestational prognoses of these patients were learnt by contacting the patients. There was major anomaly (omphalocele) in the fetus whose chromosome structure was reported as 46XY,inv(9). Fifteen pregnancies which were found to have karyotype anomalies with ultrasonographic findings were terminated upon the requests of patients and families. Four of the terminated fetuses had minor markers and 11 fetuses had major anomalies. In this way, the results of three patients were considered as variation and the aneuploidy rate was calculated as 5.2% (16/308). The pregnancy of a patient, who undergone cordocentesis due to the diagnosis of non-immune hydrops fetalis at 20 weeks, was terminated due to the onset of the pains. Also, another pregnancy undergone CVS due to increased nuchal translucency at 11 weeks of gestation Volume 23 | Issue 1 | April 2015 41 Tazegül Pekin A et al. Table 1. Invasive procedure indications according to ultrasonographic findings. Ultrasonographic findings Normal Bilateral cleft palate/lip Hypoplastic left heart + hydrops fetalis AVSD Hydrops fetalis Cystic hygroma Cystic hygroma + omphalocele Omphalocele Choroid plexus cyst >10 mm + SUA Fallot’s tetralogy Dandy-Walker syndrome Echogenic intestine grade 3 + ECF Echogenic intestine grade3 + pyelectasis + increased nuchal thickness Echogenic intestine grade 3 + pyelectasis + hypoplasic nasal bone Holoprosencephaly + corpus callosum agenesis ECF + pyelectasis Ventriculomegaly/hydrocephaly Ventriculomegaly + cleft palate-lip + hydrocephaly VSD+ARSA Ventriculomegaly + SUA Absence/hypoplasia of nasal bone Increased nuchal thickness Increased nuchal translucency Corpus callosum agenesis + ventriculomegaly + Fallot’s tetralogy n=308 % 236 1 1 3 6 5 3 2 2 2 2 2 1 1 2 8 8 1 1 1 3 9 7 1 76.6 0.3 0.3 1 1.9 1.6 1 0.6 0.6 0.6 0.6 0.6 0.3 0.3 0.6 2.6 2.6 0.3 0.3 0.3 1 2.9 2.3 0.3 AVSD: atrioventricular septal defect; ARSA: aberrant right sub-clavian artery; ECF: echogenic cardiac focus; SUA: single umbilical artery; VSD: ventricular septal defect. was terminated at 13 weeks of gestation. The karyotype analysis of this fetus was 46,XY,inv(Y)(p11;q11). Procedure-related fetal loss rate was 0.6%. Discussion In our study, we found the most frequent invasive procedure indications as increased risk at triple test (46%) and major and/or minor anomalies detected by ultrasonography (23.4%) while various amniocentesis series published in Turkey reported advanced maternal age as the most frequent invasive procedure indication.[10,11] We found the invasive procedure rate due to advanced maternal age as 1.6%, and invasive procedures were recommended due to the advanced maternal age risk only to the patients who were over 40-year-old and did not undergo prenatal screening tests. Tongsong et al. reported advanced maternal age as the most frequent amniocentesis indication (86.3%), and found invasive procedure rate associated with anomalies found by ultrasonographically as 0.6%.[12] Tabor et al. also reported advanced maternal age as the most frequent indication 42 Perinatal Journal and they reported invasive procedure rate with ultrasonography indication as 9%.[13] While previously the literature was reporting advanced maternal age as the 50–60% of amniocentesis indications,[13–15] it is not considered as an amniocentesis indication by itself today. In Table 2. Karyotype analysis results. Cytogenetic results N=308 % Normal 278 90.2 No cytogenetic result 11 3.5 46XY,t(16;22)(p13;q13) 1 0.32 46XY,inv(Y)(p11,q11) 1 0.32 Trisomy 13 1 0.32 46XY+15p 1 0.32 Trisomy 21 6 1.94 Trisomy 18 2 0.64 Triploidy 69 XXX 1 0.32 46XX/47XX+mar 1 0.32 46XX+22p 2 0.64 46XY,inv(9) 1 0.32 46XY,9qh 2 0.64 Evaluation of prenatal invasive procedures recent years, invasive procedure rates have decreased recommended due to only advanced maternal age risk[16] by the prevalent use of prenatal screening tests and extracellular DNA determination in maternal blood. By our study, we believe that the reason of the high rates of invasive procedure rates associated with major and/or minor anomalies detected by ultrasonography results from the high number of pregnant women with fetal anomalies and minor markers referred to our clinic since our clinic is a reference hospital. In our study, increased nuchal thickness (2.9%), increased nuchal translucency (2.3%) were among the ultrasonographic findings of invasive procedure indications and there were ultrasonographic markers in 16 (84.2%) of 19 fetuses who had aneuploidy. Nyber and Souter analyzed 7 studies in their meta-analysis where genetic sonograms were evaluated, and they reported that nuchal thickness increase was the most frequent marker followed by choroid plexus cyst, echogenic cardiac focus, pyelectasis and humerus shortness.[17] On the other hand, choroid plexus cysts are not considered as a marker for trisomy 21 today. It has been shown that many ultrasonographic markers do not clearly increase previous trisomy 21 risk of pregnant women; however, it increases 3–4 times in the presence of ventriculomegaly, nuchal thickness increase and aberrant right sub-clavian artery, and 6–7 times in case of hypoplasia of nasal bone.[18] In our study, we found the rate of detecting chromosomal anomaly in invasive procedures as 5.2%. Due to the non-existence of concomitant ultrasonographic findings in three patients, presence of similar chromosomal structure in paternal/maternal chromosomal analysis, completion of pregnancies with healthy live births and non-existence of anomaly in postnatal evaluations, cytogenetic changes were considered as variant. Our rate to detect chromosomal anomaly was higher than the rates reported in other regions of Turkey[19,20] and the rate of chromosomal anomalies found as 2.4% in risky group.[21] We believe that the reason results from the association of our invasive procedures with the indications and the wide use of screening tests. First trimester combined test is applied to all pregnant women in our clinic, and integrated test is carried out on patients if they have mid-level risk accordingly; however, we recommend second trimester quad screening test if the patient is considered not to be at appropriate week. Also, ultrasonography is performed for all pregnant women in order to evaluate fetal anomaly between 18 and 23 weeks of gestation. In 11 (3.5%) of our cases which undergone amniocentesis, there was no reproduction in the culture. We attributed the reason to the laboratory errors associated with the period when the genetic laboratory of our hospital was established. In 7 of the patients without reproduction in the culture, analyses were run for 13, 18, 21 and X,Y chromosomes with fluorescence in situ hybridisation (FISH) method. The results evaluated as normal were confirmed by quantitative fluorescence polymerase chain reaction (QF-PCR). Four patients recommended cordocentesis refused the procedure. The literature reports the rate not obtaining reproduction in the culture after amniocentesis between 15 and 20 weeks as 0.6–1%.[22] However, these rates are reported higher in the studies performed in Turkey.[19,23] In our study, we found procedure-related fetal loss rate as 0.6%. The pregnancy of a patient who undergone cordocentesis with the diagnosis of non-immune hydrops fetalis was lost at 21 weeks of gestation, and another pregnancy which undergone CVS due to increased nuchal translucency at 11 weeks was terminated at 13 weeks of gestation. The karyotype analysis of this fetus was 46,XY,inv(Y)(p11;q11). Also, we found that another fetus, which was found to have omphalocele with chromosome structure as 46XY,inv(9), was in utero ex at 33 weeks of gestation. However, this pregnancy was not deemed as procedure-related loss. In a study where pregnancy loss rates were compared in patients who undergone amniocentesis but no invasive procedure, it was reported that pregnancy loss risk increased 1% (95% CI, 0.3–1.5%) by amniocentesis.[7] Although differences were found among studies in a meta-analysis systematically evaluating complications associated with amniocentesis and CVS procedures, pregnancy loss rate before 24 weeks of gestation was reported as 0.9% after amniocentesis and as 1.3% after CVS.[24] Second trimester amniocentesis is considered as a safer method than early amniocentesis and transcervical CVS; however, transabdominal CVS for prenatal diagnosis purpose before 15 weeks of gestation is recommended as the first option.[25] In our study, we observed amniotic fluid leakage in 1 patient after amniocentesis at 16 weeks of gestation. The pregnancy of the patient whose fluid leakage stopped within 48 hours by strict bed rest resulted with healthy live birth at term. Amniotic fluid leakage is seen in 1–2% of the patients after amniocentesis and stops usually by itself; however, infection, oligohydramnios and fetal loss rate increase in case of persistent fluid leakage.[26] Volume 23 | Issue 1 | April 2015 43 Tazegül Pekin A et al. Conclusion Amniocentesis is the most easy-to-use invasive prenatal diagnosis method with the lowest complication rate, and also the procedure used most frequently in our study for prenatal diagnostic purposes. However, when first trimester combined test is preferred most frequently in screenings, the rate of CVS procedure with similar complication rates will increase and this method will offer earlier diagnosis opportunity. Also, together with the nuchal translucency measured according to the standards, wide use of first trimester combined tests which has lower false positivity rates will decrease unnecessary invasive procedure rates. Today, the indication of “advanced maternal age” which comes first in prenatal invasive procedures has been superseded by the indication of “increased risk at prenatal screening tests.” Besides, together with the active use of ultrasonography devices with higher resolution beginning from the early weeks of gestation, viewable minor and/or major anomalies also become indications for invasive procedures more frequently. Despite all these practices, the rates of invasive procedures for fetal karyotyping purposes will decrease significantly as the tests evaluating extracellular free fetal DNA in maternal blood are used widely. Conflicts of Interest: No conflicts declared. References 1. Beksaç MS. Fetal T›p; Prenetal Tan›. Ankara: Medical Network; 1996; p: 29–38. 2. Kagan KO, Etchegaray A, Zhou Y, Wright D, Nicolaides KH. Prospective validation of first-trimester combined screening for trisomy 21. Ultrasound Obstet Gynecol 2009; 34:14–8. 3. Nicolaides KH. Screening for fetal aneuploidies at 11 to 13 weeks. Prenat Diagn 2011;31:7–15. 4. Chiu RW, Akolekar R, Zheng YW, Leung TY, Sun H, Chan KC, et al. Noninvasive prenatal assessment of trisomy 21 by multiplexed maternal plasma DNA sequencing: large scale validity study. BMJ 2011;342:c7401. 5. Gil MM, Akolekar R, Quezada MS, Bregant B, Nicolaides KH. Analysis of cell-free DNA in maternal blood in screening for aneuploidies: meta-analysis. Fetal Diagn Ther 2014; 35:156–73. 6. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 88, December 2007. Invasive prenatal testing for aneuploidy. Obstet Gynecol 2007;110: 1459–67. 7. Tabor A, Philip J, Madsen M, Bang J, Obel EB, NorgaardPetersen B. Randomized controlled trial of genetic amniocentesis in 4606 low-risk women. Lancet 1986;1(8493): 1287–93. 44 Perinatal Journal 8. AU Ghidini A, Sepulveda W, Lockwood CJ, Romero R. Complications of fetal blood sampling. Am J Obstet Gynecol 1993;5:1339–44. 9. Shaffer LG, Slovak ML, Campbell LJ, editors. ISCN 2009: An international system for human cytogenetic nomenclature (2009) Basel: S. Karger; 2009. 10. Saatçi Ç, Özkul Y, Tafldemir fi, Kiraz A, Müderris ‹, Taflc›o¤lu N ve ark. Retrospective analysis of 2295 cases with ›nvasive prenatal diagnosis. Perinatal Journal 2007;15:120–6. 11. Kaplan Ö, Güney M, Yüksel M. 2. Trimester genetik tarama amniyosentez: 1586 olgunun de¤erlendirilmesi. Süleyman Demirel Üniversitesi T›p Fakültesi Dergisi 2012;19:144–7. 12. Tongsong T, Wanapirak C, Sirivatanapa P, Piyamongkol W, Sirichotiyakul S, Yampochai A. Amniocentesis-related fetal loss: a cohort study. Obstet Gynecol 1998;92:64–7. 13. Tabor A, Vestergaard CHF, Lidegaard Ø. Fetal loss rate after chorionic villus sampling and amniocentesis: an 11-year national registry study. Ultrasound Obstet Gynecol 2009;34: 19–24. 14. Sjögren B, Uddenberg N. Decision making during the prenatal diagnostic procedure. A questionnaire and interview study of 211 women participating in prenatal diagnosis. Prenat Diagn 1989;9:263–73. 15. Lindemann CH, Theile U. Prenatal karyotyping in second trimester pregnancies. Prenat Diagn 1989;9:594–8. 16. American College of Obstetricians and Gynecologists Committee on Genetics, Committee opinion no. 545: noninvasive prenatal testing for fetal aneuploidy. Obstet Gynecol 2012;120:1532–4. 17. Nyberg DA, Souter VL. Use of genetic sonography for adjusting the risk of fetal Down syndrome. Semin Perinatol 2003;27:130–44. 18. Agathokleous M, Chaveeva P, Poon LCY, Kosinski P, Nicolaides KH. Meta-analysis of second trimester markers for trisomy 21. Ultrasound Obstet Gynecol 2013;41:247–61 19. Erdemo¤lu M, Kale A. Genetik amaçl› amniyosentez uygulanan 183 olgunun prospektif analizi. Dicle T›p Dergisi, 2007; 34:170–5. 20. Yayla M, Bayhan G, Yal›nkaya A, Alp N. Yüksek riskli gebeliklerde 2. trimester genetik amniyosentez: 165 olgunun klinik de¤erlendirilmesi Perinatoloji Dergisi 1999;7:40–6. 21. Evans MI, O’Brien JE, Dvorin E, Johnson MP. Biochemical screening. Curr Opin Obstet Gynecol 1994;6:453–8. 22. Golbus MS, Loughman WD, Epstein CJ, Halbasch G, Stephens JD, Hall BD. Prenatal genetic diagnosis in 3000 amniocentesis. N Engl J Med 1979;300:157–63. 23. Pala HG, Artunç Ülkümen B, Eskicio¤lu F, Uluçay S, Çam S, Bülbül Baytur Y, et al. Amniocentesis results of Manisa tertiary care in 2012. Perinatal Journal 2014;22:23–7 24. Mujezinovic F, Alfirevic Z. Procedure-related complications of amniocentesis and chorionic villus sampling. A systematic review. Obstet Gynecol 2007;110:687–94. 25. Alfirevic Z, Sundberg K, Brigham S. Amniocentesis and chorionic villus sampling for prenatal diagnosis. Cochrane Database Syst Rev 2003;(3):CD003252. 26. Crane JP, Rohland BM. Clinical significance of persistant amniotic fluid leakage after genetic amniocentesis. Prenat Diagn 1986;6:6–25. AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):45–49 R N A PE IN AT U AL JO R Investigation of the effects of fetal gender on umbilical artery and middle cerebral artery Doppler findings Burcu Artunç Ülkümen, Halil Gürsoy Pala, Y›ld›z Uyar, Yeflim Baytur, Faik Mümtaz Koyuncu 1 Department of Gynecology & Obstetrics, Faculty of Medicine, Celal Bayar University, Manisa, Turkey Abstract Özet: Fetal cinsiyetin umbilikal arter ve orta serebral arter Doppler bulgular›na etkisinin araflt›r›lmas› Objective: In this study, we aimed to investigate the effects of fetal gender on umbilical artery and middle cerebral artery Doppler measurements. Amaç: Bu çal›flmada fetal cinsiyetin, umbilikal arter ve orta serebral arter Doppler ölçümlerine etkisini araflt›rmay› amaçlad›k. Methods: Umbilical artery (UA) and middle cerebral artery (MCA) Doppler ultrasonographic measurements were screened retrospectively from image and file records of 60 healthy singleton pregnant women who were on their third trimesters and referred to the Perinatology Clinic of Celal Bayar University between 2013 and 2014. Umbilical artery and MCA Doppler indexes were calculated by obtaining at least 3 consecutive waveforms. The pregnancies were evaluated in two different groups according to fetal gender (31 female fetuses and 29 male fetuses) and compared. The difference between two groups was analyzed by SPSS v.20. Results: Female fetuses were identified in 31 (51.67%) out of 60 pregnancies and male fetuses were identified in 29 (48.33%) cases included in the study. Mean maternal ages of female and male fetuses were 29.14±6.21 and 31.88±5.16 (p=0.162), and mean gestational weeks were 31.71±3.77 and 33.88±4.41 (p=0.111), respectively. Umbilical artery PI in female and male fetuses was found as 1.00±0.24 and 1.03±0.21, respectively (p=0.761). Middle artery PI in female and male fetuses was found as 2.16±0.67 and 1.84±0.85, respectively (p=0.197). Cerebral-umbilical rate was calculated as MCA PI/UA PI. Although cerebral-placental rate was not statistically significant, it was higher in female fetuses; while it was 1.86±0.92 in male fetuses, it was 2.23±0.78 in female fetuses (p=0.172). Conclusion: Today, the new approach is not to ignore the gender of baby during intrauterine period. The decrease in MCA resistance of male fetuses should be evaluated in greater studies. Keywords: Fetal gender, Doppler, middle cerebral artery (MCA), umbilical artery (UA). Yöntem: 2013-2014 y›llar›nda Celal Bayar Üniversitesi Perinatoloji Poliklini¤ine baflvuran üçüncü trimesterde olan 60 sa¤l›kl› tekil gebelikte yap›lm›fl olan umbilikal arter (UA) ve orta serebral arter (MCA) Doppler ultrasonografik ölçümleri retrospektif olarak görüntü ve dosya kay›tlar›ndan tarand›. Umbilikal arter ve MCA Doppler endeksleri en az ard›fl›k 3 dalga formu elde edilerek hesapland›. Gebelikler fetal cinsiyete göre iki ayr› grupta de¤erlendirildi (k›z fetüsler 31 ve erkek fetüsler 29 olgu) ve karfl›laflt›r›ld›. Her iki grup aras›ndaki fark SPSS v.20 ile de¤erlendirildi. Bulgular: Çal›flmaya dahil edilen 60 gebeli¤in 31 tanesinde k›z fetüs (%51.67) ve 29 tanesinde erkek fetüs (%48.33) tespit edildi. K›z ve erkek fetüslerde s›ras› ile ortalama maternal yafl 29.14±6.21 ve 31.88±5.16 (p=0.162), ortalama gestasyonel hafta 31.71±3.77 ve 33.88±4.41 (p=0.111) olarak tespit edildi. Umbilikal arter PI k›z ve erkek fetüslerde s›ras› ile 1.00±0.24 ve 1.03±0.21 olarak tespit edildi (p=0.761). Orta serebral arter PI k›z ve erkek fetüslerde s›ras› ile 2.16±0.67 ve 1.84±0.85 olarak tespit edildi (p=0.197). Serebro-umbilikal oran MCA PI/UA PI olarak hesapland›. Serebro-plasental oran, istatistiksel olarak anlaml› olmamakla birlikte k›z fetuslarda daha yüksek olarak bulundu; erkek fetüslerde ortalama 1.86±0.92 iken k›z fetüslerde ortalama 2.23±0.78 idi (p=0.172). Sonuç: Günümüzdeki yeni yaklafl›m intrauterin dönemde bebe¤in cinsiyetinin göz ard› edilmemesi yönündedir. Erkek fetüslerde MCA rezistans›nda azalma daha büyük çal›flmalarda de¤erlendirilmelidir. Anahtar sözcükler: Fetal cinsiyet, Doppler, orta serebral arter (MCA), umbilikal arter (UA). Correspondence: Halil Gürsoy Pala, MD. Celal Bayar Üniversitesi T›p Fakültesi Kad›n Hastal›klar› ve Do¤um Anabilim Dal›, Manisa, Turkey. e-mail: gursoypala@yahoo.com Received: July 10, 2014; Accepted: February 6, 2015 Please cite this article as: Artunç Ülkümen B, Pala HG, Uyar Y, Baytur Y, Koyuncu FM. Investigation of the effects of fetal gender on umbilical artery and middle cerebral artery Doppler findings. Perinatal Journal 2015;23(1):45–49. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231010 doi:10.2399/prn.15.0231010 QR (Quick Response) Code: Artunç Ülkümen B et al. Introduction Ultrasonographic examination is one of the most important tools of modern obstetric practice. In particular, Doppler ultrasonography provides valuable data about fetal circulation and fetal hemodynamic condition.[1] The vessels most frequently used for the evaluation of the fetal well-being are umbilical artery (UA), middle cerebral artery (MCA), and ductus venosus (DV).[2] In case of placental failure and associated fetal stress, the increases in umbilical artery resistance indexes are the leading hemodynamic changes in fetus.[3] Following these changes, MCA resistance indexes decrease as a result of cerebral redistribution, which helps to maintain blood flow towards fetal brain by this adaptation mechanism.[4] In the studies of Askling et al. and James, the increases of placental dysfunction in male fetuses and of associated gestational complications such as preeclampsia and ablatio placentae were shown.[5,6] Also, an increase in preterm labor and postterm pregnancy frequency was found in male fetuses.[7-10] Intrapartum fetal distress and increased cesarean rates are also observed more frequently in male fetuses.[11] Besides, hyperemesis gravidarum and placental invasion anomalies are more frequent in female fetuses.[6] Based on fetal gender being effective on placentation, we considered that fetal gender might cause a change in Doppler indexes that we use for placental perfusion evaluation, and we aimed in this study to investigate the effect of fetal gender on umbilical artery and fetal middle cerebral artery flow measurements. Methods Sixty healthy singleton pregnant women who were on their third trimesters between 28 and 36 weeks of gestation and had their Doppler ultrasound examination in the perinatology clinic of our hospital between January 2013 and June 2014 were included in the study. The study group was separated into two groups by pairing according to week of gestation and maternal age, and fetuses being male and female. While 29 cases were identified as male fetuses, 31 cases were female fetuses. Approval of Local Ethics Committee was obtained for the study planned retrospectively. Week of gestation was calculated according to the last menstrual period (LMP) and it was confirmed by 46 Perinatal Journal first trimester ultrasound findings. Multiple pregnancies, pregnant women with chronic systemic diseases (such as diabetes, liver and kidney diseases, connective tissue disease etc.) and pregnancies with preeclampsia and intrauterine growth retardation were excluded from the study. Also, the pregnancies found to have fetal chromosomal or structural anomalies were excluded from the study. Ultrasound measurements were done by using Voluson 730, RAB 3.5-MHz probe (GE Medical Systems, Milwaukee, WI, USA). All measurements were done by a single operator (H.G.P.). Umbilical artery Doppler measurements were done through free region.[12,13] MCA Doppler measurement was done on the axial section where thalamic nuclei are seen on the display. Willis polygon was distinguished by color flow. The measurements were done through the proximal 1/3 part close to the internal carotid artery with origin. Doppler indexes were calculated by obtaining 3 consecutive waveforms. Amniotic fluid index (AFI) was considered as the total of amniotic fluid depths measured on 4 quadrants. The statistical analysis was done by SPSS v.20 (SPSS Inc., Chicago, IL, USA). The results were provided as mean±standard deviation (SD). The p value less than 0.05 was considered as statistically significant. The difference between the groups was calculated by using t-test. Results Female fetuses were identified in 31 (51.67%) out of 60 pregnancies and male fetuses were identified in 29 (48.33%) cases included in the study. Mean maternal ages of female and male fetuses were 29.14±6.21 and 31.88±5.16 (p=0.162), and mean gestational weeks were 31.71±3.77 and 33.88±4.41 (p=0.111), respectively. Umbilical artery PI in female and male fetuses was found as 1.00±0.24 and 1.03±0.21, respectively (p=0.761) (Fig. 1). Middle umbilical artery PI in female and male fetuses was found as 2.16±0.67 and 1.84±0.85, respectively (p=0.197) (Fig. 2). Cerebral-placental rate was calculated as MCA PI/UA PI. Although cerebral-placental rate was not statistically significant, it was higher in female fetuses; while it was 1.86±0.92 in male fetuses, it was 2.23±0.78 in female fetuses (p=0.172). The clinical data about the study group are shown in the Table 1. No sig- Investigation of the effects of fetal gender on umbilical artery and middle cerebral artery Doppler findings Fig. 1. UA PI values in female and male fetuses. Fig. 2. MCA PI values in female and male fetuses. nificant relation was found between UA PI & MCA PI and maternal age & parity (Table 2). AFI was found as 14.86±4.28 in male fetuses and 13.99±5.42 in female fetuses (p=0.594). There was no significant relationship between AFI and estimated fetal weight (r=0.131; p= 0.368) and the week of gestation (r=0.008; p=0.958). ing placental perfusion has been analyzed only in one study so far.[14] A total of 388 term pregnant women were included in this study carried out by Prior et al., and 212 (54.6%) male and 176 (45.4%) female fetuses were identified in these pregnancies. In this study, no difference was observed between fetal genders in terms of UA PI. MCA PI was higher among female fetuses (mean female fetus value: 1.42; mean male fetus value: 1.34) (p=0.004). MCA PSV (peak systolic velocity) was higher in female fetuses (p<0.001). Mean cerebral-umbilical rate was 1.74 in male fetuses and 1.81 in female fetuses (p=0.10). Umbilical venous velocity was higher in female fetuses (p=0.009). Discussion In our study, although we did not observe any statistically significant level in male fetuses, we identified decreased MCA resistance and slightly increased umbilical artery resistance. Although different placentation processes and implantation and angiogenesis pathways are defined depending on the fetal gender, Doppler difference associated with fetal gender in terms of evaluat- It was shown in previous studies that male fetuses are more associated with placental insufficiency and therefore the gestational complications related with placenta- Table 1. Clinical characteristics of the pregnant women included in the study. Pregnancies with male fetuses n=29 Pregnancies with female fetuses n=31 p Maternal age (mean±SD 31.88±5.16 29.14±6.21 0.162 Parity (mean±SD) 1.06±1.03 0.71±1.10 0.330 Week of gestation (mean±SD) 33.88±4.41 31.71±3.77 0.111 Birth weight (g) (mean±SD) 3160.0±709.67 3021.43±972.09 0.613 UA PI (mean±SD) 1.03±0.21 1.00±0.24 0.761 MCA PI (mean±SD) 1.84±0.85 2.16±0.67 0.197 Cerebral-umbilical rate (mean±SD) 1.86±0.92 2.23±0.78 0.172 AFI (cm) (mean±SD) 14.86±4.28 13.99±5.42 0.594 Volume 23 | Issue 1 | April 2015 47 Artunç Ülkümen B et al. Table 2. Relationship between UA & MCA PI and maternal age and parity*. Maternal age Parity UA PI r p 0.014 0.922 -0.261 0.089 MCA PI r p 0.101 0.489 0.041 0.779 *Spearman’s correlation analysis; r=Spearman’s correlation coefficient tion failure (such as miscarriage, intrauterine loss, preeclampsia, IUGR etc.) are observed more frequently in male fetuses.[5,6] In a study evaluating pregnancies with loss of end diastolic flow, it was shown that 63.2% of the cases were male fetuses, and 83% of the pregnancies with reverse end diastolic flow were male fetuses.[15] Prior et al. reported that decreased resistance in MCA flow even in the male fetuses considered to have uterine artery flow and umbilical artery flow within normal ranges and to have fetal growth compatible with the week of gestation and normal placental functions compared to female fetuses depends on a physiological adaptation to the various levels of placentation in male fetuses.[14] Also, Ghidini and Salafia, and Clifton showed in their studies that the progress of angiogenesis is weaker in male fetuses and it is more difficult for male fetuses to adapt poor maternal environmental conditions.[16,17] By the change of maternal conditions during intrauterine period, the responses of male and female fetuses towards these poor conditions and the steroidogenesis pathways in this process and protein and gene expressions vary.[17] Male fetuses may adapt better to the poor intrauterine microenvironment molecularly and metabolically.[17] So, male fetus differ molecularly even in the implantation and placentation phases of pregnancy. Presence of decreased resistance in MCA flow even in male fetuses displaying normal clinical development may show that male fetuses have a physiological adaptation to the differences in placentation. Cerebral-umbilical rate is the most reliable measurement showing brain sparing effect in babies with IUGR.[18] In our study, we did not find any difference between female and male fetuses in terms of cerebralumbilical rate. However, we also did not expect a significant difference in terms of cerebral redistribution since our study group consisted of healthy pregnant women at their third trimesters. In the study of Yücel et al. where 48 Perinatal Journal Doppler findings of term pregnancies were compared according to fetus genders, there was no significant difference between female and male fetuses in terms of UA and MCA pulsatility indexes.[19] In our study, we did not observe any significant difference in female and male fetuses in terms of AFI. In their study, Perni et al. reported a positive correlation between AFI and fetal weight in female fetuses before 38 weeks of gestation.[20] In our study, there was no association between AFI and estimated fetal weight and the week of gestation. The weakest aspect of our study was the population size. Our study was limited with 60 patients since we planned the study retrospectively and excluded the babies with chronic disease, placental insufficiency findings or fetal anomaly from the study. By this size, the power of the study was 0.6 (α-error= 0.05; d=0.5). The advantage of our study was that it was paired by the maternal age, parity and the week of gestation when the cases were separated as female and male fetuses. Also, measuring values by a single operator minimized the inter-observer difference. Conclusion Consequently, placentation perfusion may vary depending on the fetal gender. Our preliminary results we provided here should be confirmed by further comprehensive studies. Conflicts of Interest: No conflicts declared. References 1. Alfirevic Z, Stampalija T, Gyte GML. Fetal and umbilical Doppler ultrasound in high-risk pregnancies. Cochrane Database Syst Rev 2010;(1):CD007529. 2. Mari G, Abuhamad A, Cosmi E, Segata M, Altaye M, Akiyama M. Middle cerebral artery peak systolic velocity: technique and variability. J Ultrasound Med 2005;24: 425–30. 3. Piazze J, Padula F, Cerekja A, Cosmi EV, Anceschi MM. Prognostic value of umbilical-middle cerebral artery pulsatility index ratio in fetuses with growth restriction. Int J Gynaecol Obstet 2005;91:233–7. 4. Vyas S, Nicolaides KH, Bower S, Campbell S. Middle cerebral artery flow velocity waveforms in fetal hypoxaemia. Br J Obstet Gynaecol 1990;97:797–803. 5. Askling J, Erlandsson G, Kaijser M, Akre O, Ekbom A. Sickness in pregnancy and sex of child. Lancet 1999;354: 2053. Investigation of the effects of fetal gender on umbilical artery and middle cerebral artery Doppler findings 6. James WH. Sex ratios of offspring and the causes of placental pathology. Hum Reprod 1995;10:1403–6. 7. James WH. Why are boys more likely to be preterm than girls? Plus other related conundrums in human reproduction. Hum Reprod 2000;15:2108–11. 8. McGregor JA, Leff M, Orleans M, Baron A. Fetal gender differences in preterm birth: findings in a North American cohort. Am J Perinatol 1992;9:43–8. 14. Prior T, Wild M, Mullins E, Bennett P, Kumar S. Sex specific differences in fetal mid cerebral artery and umbilical venous doppler. PLoS One 2013;8(2):e56933. 15. Edwards A, Megens A, Peek M, Wallace EM. Sexual origins of placental dysfunction. Lancet 2000; 355:203–4. 16. Ghidini A, Salafia CM. Gender differences of placental dysfunction in severe prematurity. BJOG 2005;112:140–4. 9. Cooperstock M, Campbell J. Excess males in preterm birth: interactions with gestational age, race and multiple birth. Obstet Gynecol 1996;88:189–93. 17. Clifton VL. Review: Sex and the human placenta: mediating differential strategies of fetal growth and survival. Placenta 2010;31 Suppl:S33–9. 10. Divon MY, Ferber A, Nisell H, Westgren M. Male gender predisposes to prolongation of pregnancy. Am J Obstet Gynecol 2002;187:1081–3. 18. Gramellini D, Folli MC, Raboni S, Vadora E, Merialdi A. Cerebral-umbilical Doppler ratio as a predictor of adverse perinatal outcome. Obstet Gynecol 1992;79:416–20. 11. Bekedam DJ, Engelsbel S, Mol BWJ, Buitendijk SE, van der Pal-de Bruin KM. Male predominance in fetal distress during labor. Am J Obstet Gynecol 2002;187:1605–7. 19. Yücel A, Y›lmazer M, Acar M, De¤irmenci B, Köse S, Haktan›r A, Fenkçi V, Cevrioglu S. Termde normal gebelerde, Doppler indeksleri ve non-stres test de¤erlerinin fetus cinsiyetine göre karfl›laflt›r›lmas›. Kocatepe T›p Dergisi 2005;6: 19–24. 12. Burrel SJ, Kingdom JC. The use of umbilical artery Doppler ultrasonography in modern obstetrics. Curr Opin Obstet Gynecol 1997;9:370–4. 13. ISUOG Practice Guidelines. Use of Doppler ultrasonography in obstetrics. Ultrasound Obstet Gynecol 2013;41: 233–9. 20. Perni SC, Predanic M, Cho JE, Kalish RB, Chasen ST. Association of amniotic fluid ›ndex with estimated fetal weight. J Ultrasound Med 2004;23:1449–52. Volume 23 | Issue 1 | April 2015 49 AL JO U R AL PE R AT N IN Original Article L Perinatal Journal 2015;23(1):50–55 R N A PE IN AT U AL JO R Results of routine first trimester screening tests and following invasive procedures during pregnancy Rahime Nida Ergin1, Murat Yayla2 1 Department of Obstetrics & Gyneceology, Faculty of Medicine, Bahçeflehir University, Istanbul, Turkey 2 Obstetrics & Gyneceology Clinic, International Hospital, Istanbul, Turkey Abstract Özet: Gebelikte rutin ilk üç ay taramas›n›n sonuçlar› ve sonras›nda yap›lan tan›sal giriflimler Objective: The purpose of this study is to show distribution of risk in pregnancies which underwent first trimester combined tests, and investigate general demographic and clinical characteristics of patients, underwent invasive diagnostic tests after screening tests. Amaç: Bu çal›flmada gebeli¤in ilk üç ay›nda kombine test yap›lan gebelerde risk da¤›l›m›n›n gösterilmesi, tarama sonras› yap›lan di¤er ifllem ve giriflimler ile tan›sal test uygulanan hastalar›n genel demografik ve klinik özelliklerinin incelenmesi amaçlanm›flt›r. Methods: Combined test data of first trimester screening in 20082011 were evaluated retrospectively and cross-sectional. After the measurement of nuchal translucency (NT), double test was applied to complete combined test within the same day. Invasive diagnostic procedures were compared in terms of rate, indications, karyotype and postnatal outcomes. Results: A total of 1109 pregnant women were included. Their mean age was 31.07±3.73 years. Free-βhCG was 1.26±0.94 MoM and PAPPA was 1.16±0.65 MoM. Mean NT value was 1.60±0.67 mm. With threshold of 1/250, screening test was positive in 3.1% of the cases. Additional 22 cases due to first trimester screening and 19 cases due to second trimester screening had invasive procedures (6.4% in total). Invasive procedures revealed karyotype anomaly in 11.3%. Karyotype anomalies were more frequent in group (20%) with positive combined test compared to ones performed for other reasons like maternal anxiety. Yöntem: 2008–2011 y›llar› aras›nda ilk üç ay gebelik taramas›na ait kombine test verileri retrospektif-kesitsel olarak de¤erlendirildi. Ense kal›nl›¤› (NT) ölçümü sonras›nda ayn› gün içinde kombine testi tamamlamak için ikili test uyguland›. Taramalar›n sonras›nda uygulanan tan›sal giriflimler oran, endikasyonlar›, karyotip ve postnatal sonuçlar aç›s›ndan karfl›laflt›r›ld›. Bulgular: Toplam 1109 gebe de¤erlendirmeye al›nd›. Takipteki gebelerin ortalama yafl› 31.07±3.73 y›ld›. Serbest βhCG ölçümü 1.26±0.94 MoM ve PAPP-A ölçümü 1.16±0.65 MoM saptand›. Birinci üç ayda ortalama NT de¤eri 1.60±0.67 mm bulundu. Eflik de¤eri 1/250 al›nd›¤›nda olgular›n %3,1’inde tarama testi pozitif saptand›. ‹lk üç ay taramas› sonunda 22 olguya ve ikinci üç ay taramalar› sonras›nda 19 olguya daha tan›sal giriflim yap›ld›¤› gözlendi (toplamda %6.4). Giriflim yap›lan hastalar›n %11.3’ünde karyotip anomalisi saptand›. Kombine test sonucu pozitif olan grupta anne yafl›na ba¤l› anksiyete gibi di¤er nedenlerle giriflim yap›lanlara göre karyotip anomalisi daha fazla (%20) gözlendi. Conclusion: Although false positive rate is 3.1% in first trimester combined test, rate of total invasive procedures is more than double (6.4%). Number of invasive diagnostic procedures increased due to maternal anxiety of age and physicians evaluating only NT or double tests. With diagnostic procedures, chromosome anomalies reaches 11% and termination need reaches 10%. Invasive procedures performed due to anxiety of mother or physician revealed no chromosomal anomaly requiring termination. Sonuç: Çal›flmam›zdaki gebelik takiplerinde ilk üç ay taramas›nda kombine testte yanl›fl pozitiflik oran› %3.1 olmas›na ra¤men toplam giriflim oran› iki kat›ndan fazlad›r (%6.4). Tan›sal ifllem say›s› yafl s›n›r›ndan kaynaklanan anne anksiyetesine ve hekimlerin sadece NT veya ikili test sonucunu dikkate almalar› nedeni ile artmaktad›r. Tan›sal giriflimlerde %11’lere ulaflan kromozom anomalisi ile %10’lara ulaflan sonland›rma gereksinimi ile karfl›lafl›lm›flt›r. Anne veya hekim anksiyetesine ba¤l› uygulanan giriflimlerin hiçbirinde sonland›rma gerektiren bir kromozom anomalisine rastlanmam›flt›r. Keywords: Combined test, chorionic villus sampling, amniocentesis, anxiety. Anahtar sözcükler: Kombine test, koryon villüs biyopsisi, amniyosentez, anksiyete. Correspondence: Rahime Nida Ergin, MD. Bahçeflehir Üniversitesi T›p Fakültesi Kad›n Hastal›klar› ve Do¤um Ana Bilim Dal›, ‹stanbul, Turkey. e-mail: drnidaergin@gmail.com Received: January 12, 2014; Accepted: February 17, 2015 Please cite this article as: Ergin RN, Yayla M. Results of routine first trimester screening tests and following invasive procedures during pregnancy. Perinatal Journal 2015;23(1):50–55. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231012 doi:10.2399/prn.15.0231012 QR (Quick Response) Code: Results of routine first trimester screening tests and following invasive procedures during pregnancy Introduction By the development of ultrasonographic fetal biometry measurements and early and effective screening programs based on biochemical methods in the early diagnosis of chromosomal anomalies, maternal preferences have increased actively.[1-3] Combined test, as one of the efficient screening programs, includes fetal nuchal screening and double screening test from maternal blood consecutively between 11 and 14 weeks of gestation, and chromosome anomaly is used for the risk determination of trisomy 21 in particular. In this study, we aimed to show the distribution of combined test results in pregnant women who underwent combined screening test between 11 and 14 weeks of gestation and to investigate general demographic, laboratory and clinical characteristics of patients who underwent invasive procedures and diagnostic tests according to the results of screening tests. Methods The data of patients for first trimester screenings between 2008 and 2011 were evaluated retrospectively and as cross-sectional. Before the screening tests, all pregnant women were informed and their consents were obtained for the efficiency of ultrasonography and biochemical procedure to be carried out. First, the week and day of gestation were determined. In fetuses which had 45–84 mm ultrasonographic crown-rump length (CRL), nuchal translucency (NT) was measured according to current rules.[1] In addition to this measurement, fetal anatomy was evaluated. Then, in the same day, 4–6 ml peripheral venous blood was collected for double test (free beta human chorionic gonadotropin [f-βhCG] and pregnancy-associated plasma protein A [PAPP-A]) calculation, and it was studied in the same laboratory with same method in 24 hours. The risk distribution of f-βhCG and PAPP-A MoM values reached during screening program and combined test results were obtained. The patients whose combined test risk scores were 1/250 and above were considered as positive and they were informed about other screening methods and diagnostic methods again. For karyotype analysis, chorionic villus sampling (CVS) at 12–14 weeks of gestation or amniocentesis at 16–20 weeks of gestation was carried out. Chromosome analyses were performed in the genetic laboratory of the same institution. In the risk groups which had and did not have invasive procedures, gestational follow-ups were continued to determine gestational prognosis. The distribution of the numbers and reasons of CVS and amniocentesis carried out after screening tests and karyotype results, and perinatal prognosis of the group which had invasive procedure were re-investigated after the delivery, and amniocentesis and CVS groups were compared. T-test and Mann-Whitney U tests were performed for statistical data, and the value p<0.05 was considered statistically significant. Results In a period of four years, 1109 pregnant women were included in the study in total. Mean age of the cases was 31.07±3.73 years. Mean f-βhCG value was 1.26±0.94 MoM and PAPP-A value was 1.16±0.65 MoM in the first trimester. Mean NT value in the first trimester was 1.60±0.67 mm. When threshold value of the combined test result was considered as 1/250, screening test result was positive in 3.15% (35/1109) of the cases. It was observed that 30 (85.7%) of these 35 cases accepted diagnostic procedure. After first trimester briefing and screening, additional 22 cases also requested diagnostic procedures and had invasive procedures. Given the additional screenings during the second trimester, additional 19 cases also had diagnostic procedures. Among pregnant women found to be positive in the first trimester screening test, 5 (14%) out of 35 cases did not accept invasive diagnostic method recommended and preferred to decrease their risks by consecutive screenings, and no chromosomal anomaly finding was found neither during follow-up nor postnatal period. Chromosome anomaly was found in 20% (6/30) of those who underwent CVS or amniocentesis after positive screening finding, and pregnancy was terminated in all cases. Although combined test result was within low risk range, both physicians and pregnant women considering maternal age as too advanced, and separate interpretation of increased nuchal translucency and biochemical risk level in consecutive screening tests caused anxiety and uncertainty in some cases. This anxiety caused pregnant women to prefer CVS or amniocentesis directly or to have second trimester screening tests. Non-directing consultancy was provided again by Volume 23 | Issue 1 | April 2015 51 Ergin RN, Yayla M the physicians who carried out the screening in this group which had negative screening test results and requested procedures, and therefore invasive procedures were carried out since they did not change their minds. No karyotype anomaly was observed in these 22 pregnant women within low risk range. In the last group consisting of 19 cases, which were examined during second trimester and found to have positive results for biochemical test or genetic marker, had 4 structural fetal anomalies and all underwent invasive procedures. Among them, there were 2 karyotype anomalies not requiring termination and 2 structural anomalies which were required to terminate. In terms of the reasons of the procedures (n=71), combined test was effective in 30 cases, advanced maternal age in 15 cases, positive genetic sonography in 13 cases, maternal anxiety in 7 cases, and positive result for second trimester screening test in 6 cases. The reasons of diagnostic procedures were observed in the first trimester screening tests in 52/71 cases and in the second trimester screening tests in 19/71 cases. In total, 6.4% of the screened cases (CVS in 1% and amniocentesis in 5.4%) underwent diagnostic procedures. In 11.27% of the patients which underwent the invasive procedure had karyotype anomaly (three fetuses had trisomy 21, two fetuses had trisomy 18, two fetuses had mosaic XXY and one fetus had triploidy). It was determined that karyotype anomalies were more frequent in the group (6/30: 20%) with positive result for combined, and less frequent in the group (1/19: 5.3%) with negative result for combined test but positive result for second trimester biochemistry or genetic ultrasonography screening test and in the group (1/22: 4.5%) with anxi- Table 1. Results of combined test risk and the distribution of diagnostic procedures. Risk rate Number of screened pregnant women Number pregnant women underwent diagnostic procedure Number of karyotype anomaly detected 6 >1/250 35 30 1/251-1/1000 70 12 - 1/1001-1/10,000 444 22 1 1/10,001-1/100,000 560 7 1 Total 1109 71 8 ety. In the last two groups, the karyotype anomaly detected was 47, XXY. The distribution of screened pregnant women according to combined test risk results and the distribution of diagnostic procedures performed are shown in Table 1; karyotype anomalies found are shown in Table 2, and the comparison of the groups which had and did not have procedures is shown in Table 3. As expected, mean maternal age and mean fetal NT were statistically significant in the group which underwent procedures. When cases which underwent amniocentesis or CVS were compared, it was seen that mean age was low but mean fetal NT and risk score were higher in those underwent CVS (Table 4). Among the cases which had no karyotype anomaly after procedure and followed up until delivery delivered, 87.3% of them delivered at term, 9.5% of them delivered preterm or IUGR but healthy babies, and 3.2% of them had fetal loss at prenatal period. Also, in 3.2% of this group, there was minor anomaly. In none Table 2. Laboratory and clinical characteristics of karyotype anomalies. Case Maternal age Week of gestation 1 40 12 9 2 27 12 2.9 3 40 13 3.2 4 35 12 5 30 12 6 36 7 29 8 31 CVS: Chorionic villus sampling 52 Perinatal Journal NT (mm) βhCG f-β (MoM) PAPP-A (MoM) Combined test risk Diagnostic procedure Karyotype - - 1/6 CVS Trisomy 21 1.5 0.5 1/2 CVS Trisomy 21 2.1 1.0 1/6 Amniocentesis Trisomy 21 4.5 0.4 0.1 1/2 CVS Trisomy 18 1.5 0.3 0.4 1/21,836 CVS Trisomy 18 13 1.7 0.7 0.6 1/3850 Amniocentesis Mozaic XXY 13 1.2 0.9 0.8 1/50,000 Amniocentesis Mozaic XXY 13 3.0 0.1 0.06 1/2 CVS Triploidy Results of routine first trimester screening tests and following invasive procedures during pregnancy of the procedures applied due to the anxiety of mother or physician, no chromosomal anomaly requiring termination was observed. False negative major chromosome anomaly was not observed in any of the cases followed-up, and no such findings were reported to us in the following 3 years. Table 3. The mean and standard deviation distribution of age, NT and biochemical markers in cases. Procedure In the studies carried out in Turkey,[5,6] mean fβhCG values were reported between 0.82 and 1.07 MoM and mean PAPP-A values were reported between 1.06 and 1.61 MoM. In our study group, we found these values as 1.25 and 1.16 MoM, respectively. f-βhCG value in our study was slightly higher than the values in other studies. We believe that the difference may result from various laboratory methods. In the same studies, NT values were found between 1.16 and 1.58 mm. Mean NT value of normal cases we found in our study was 1.53 mm and it is similar to the results of other studies. Including combined test into clinical practice caused conflicts to determine fetal chromosome anomaly risk in the use of second trimester tests, increase in false positivity rates and unnecessary invasive procedures.[7] Applying these tests of two different periods in clinical practice with various combinations has been improved by SURUSS (Serum, Urine and Ultrasound Screening Study) study and it was reported that “Integrated Test” practice (NT death + PAPP-A in 11 weeks of gestation and carrying out quad test – αFP, uE3, hCG and inhib- NT* βhCG MoM PAPP-A MoM Yok Mean Standard deviation 30.84 3.473 1.53 0.34 1.25 0.93 1.16 0.64 CVS / AS Mean Standard deviation 34.43 5.38 2.60 2.14 1.30 1.08 1.04 0.75 Total Mean Standard deviation 31.07 3.73 1.60 0.67 1.25 0.94 1.15 0.65 Discussion Using biochemical parameters as trisomy 21 screening test efficiently has increased the rates of maternal preferences in gestational follow-up practices.[2] However, in the perinatology, one of the cornerstones (or even of the milestones) in screening and determined karyotype anomalies is to add ultrasonographic nuchal translucency measurement into biochemical analyses as trisomy 21 screening test during relatively early period of pregnancy such as first trimester.[3] Ultrasonographic nuchal translucency measurement together with maternal age and f-βhCG and PAPP-A measurements from maternal serum between 11 and 14 weeks of gestation are defined as “combined test”. Also, in pregnant women recommended first trimester combined screening test by adding combined test into the clinical use, it is seen that the rate of pregnant women accepting procedure increases significantly.[4] Age* *: Statistically significant; p<0.05. AS: Amniocentesis, CVS: Chorionic villus sampling in A – in the early second trimester) was effective.[7,8] In this prospective study carried out in multiple center where over 47,000 pregnancies were followed up, it was stated that it is the best method with 85% early detection rate and 0.9% false positivity rate.[7,8] In our study, we found false positivity rate as 4.3% for combined test.[7,8] However, in following modeling and clinical studies, “Contingent sequential” (recommending invasive diagnostic procedures for those evaluated to have high risk in first trimester test and carrying out quad test at second trimester in pregnancies with threshold risk values) method was shown as the effective method with the high early detection rate of anomaly and high rate of false positivity rate which are 1, 3, and 5%.[9,10] Although it is stated in some publications that contingent sequential screening method has a complex structure and low detection rate in the comparison of sequential and contingent prenatal Down syndrome screening test,[11] it was reported in FASTER (First and Second Trimester Table 4. The mean and standard deviation distribution of age, NT and biochemical markers in procedures. Procedure Age* NT* βhCG MoM PAPP-A MoM CVS Mean N Standard deviation 30.64 11 10.38 4.92 11 2.89 1.16 10 0.79 0.66 10 0.0 AS Mean N Standard deviation 35.11 60 3.64 2.14 56 1.64 1.33 56 1.13 1.11 56 0.77 Total Mean N Standard deviation 34.43 71 5.38 2.60 67 2.14 1.30 66 1.08 1.04 66 0.75 *: Significant difference with Mann-Whitney U test; p<0.05. AS: Amniocentesis, CVS: Chorionic villus sampling Volume 23 | Issue 1 | April 2015 53 Ergin RN, Yayla M Evaluation of Risk) study that the results of first trimester combined screening test at 11 weeks of gestation are better than the results of quad test at second trimester and similar to the results at 13 weeks of gestation.[12] It was shown that both sequential consecutive screening test and full-integrated screening test have low false positivity rates and high detection rates for Down syndrome.[12] However, considering the costs and time loss to be brought by carrying out these tests routinely and consecutively in general screening procedures, the efficiency and practicality of a well-combined test should not be overlooked. The results of our study having 4-year clinical experience show that high anomaly detection rate and low false positivity rates are similar to the rates reported in the literature.[12-14] Ultrasonographic nasal bone measurement, ductus venosus, hepatic artery and tricuspid valve flows and many other parameters have been offered to increase the detection rates of these tests until recently.[15] In fact, it was reported that maternal serum sampling before or simultaneously with NT measurement increased test performance.[16] By including combined test into clinical practice in England, the number of positive Down syndrome screening test in 2003–2004 decreased in 2008-2009.[17] This also provided a 72% decrease in the requests to cytogenetics laboratory and the total screening positivity rate from 9% to 3.1% in 9 years.[17] In our study, false positivity rate was 3.1% in first trimester screening combined test in the gestational follow-ups, and it is consistent with the results of that study. However, total procedure rate was more than double (6.4%) compared to test positivity in our study. The reason is the high rate of invasive procedures due to the anxiety of mother and/or physician. However, there was no chromosome anomaly in such cases. Today, parallel to the technical developments of molecular biology, detection rates were 98% for trisomy 21, 96% for trisomy 18 and 13, and invasive test rate was 0.7% by including extracellular free fetal DNA in maternal blood into the combined test.[18,19] Perhaps, by including molecular tests into routine practices after their efficiencies are proven by wide series, anxiety indications of mothers and/or physicians, which are the major reason for high rate of invasive procedures, may be decreased substantially. It has been shown that the most significant preference criteria of mothers among invasive test versus non-invasive follow- 54 Perinatal Journal up methods is to diagnose Down syndrome with at least 95% accuracy with related test.[20] Therefore, investigating extracellular free DNA in maternal blood and combined tests have high potential for patient admission. Conclusion Although false positivity rate is 3.1% in first trimester combined test during pregnancy follow-ups in our study, the rate of total invasive procedures is more than double (6.4%). In some pregnant women, the request for invasive procedure due to anxiety caused by “age limit”, which is especially an old habit, increases the number of diagnostic procedures. In addition, physicians taking only nuchal translucency or double test result into consideration also increase the number of procedures as well as general anxiety. As a result of the both first and consecutive second trimester screening tests, 15.5% of the diagnostic procedures are CVS and 84.5% are amniocentesis. While 73% of these procedures are caused by first trimester screening tests and briefing, and 27% of them are caused by second trimester screening tests. At the end of diagnostic procedures, chromosome anomalies reach up to 11% and termination need reaches up to 10%. No anomaly requiring termination has been found in any of the procedures caused by the anxiety of mother or physician. Proper screening and briefing during pregnancy may decrease the number of procedures associated with false positivity, and therefore financial losses and possible fetal losses. The basic rule to prevent anxiety is to issue reports which do not include age and double test results or to interpret such reports accordingly. Considering the costs and efficiency of trisomy 21 screening tests, “combined test” examination to be carried out by proper individuals and laboratories seems to continue until other screening tests to be done on maternal blood become cheaper and are widely used. Conflicts of Interest: No conflicts declared. References 1. Nicolaides KH. Screening for chromosomal defects. Ultrasound Obstet Gynecol 2003;21:313–21. 2. Salonen R, Turpeinen U, Kurki L, Lappalainen M, Ammälä P, Hiilesmaa V, et al. Maternal serum screening for Down’s syndrome on population basis. Acta Obstet Gynecol Scand 1997;76:817–21. Results of routine first trimester screening tests and following invasive procedures during pregnancy 3. Wald NJ, Hackshaw AK. Combining ultrasound and biochemistry in first-trimester screening for Down’s syndrome. Prenat Diagn 1997;17:821–9. 4. Tringham GM, Nawaz TS, Holding S, Mcfarlane J, Lindow SW. Introduction of first trimester combined test increases uptake of Down’s syndrome screening. Eur J Obstet Gynecol Reprod Biol 2011;159:95–8. 5. fianl› DB, Kartkaya K. Determination of the median levels of first trimester screening test parameters in our region. [Article in Turkish] Perinatal Journal 2012;20:6–11. 6. Özer Ö, Say›n CN, Varol FG. The assessment of nuchal translucency and serum markers for down syndrome screening with ductus venosus Doppler measurements in the first trimester. J Turk Ger Gynecol Assoc 2010;11:194–8. trimester or second-trimester screening, or both, for Down’s syndrome. N Engl J Med 2005;353:2001–11. 13. Kagan KO, Wright D, Baker A, Sahota D, Nicolaides KH. Screening for trisomy 21 by maternal age, fetal nuchal translucency thickness, free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A. Ultrasound Obstet Gynecol 2008;31:618–24. 14. Borrell A, Casals E, Fortuny A, Farre MT, Gonce A, Sanchez A, et al. First-trimester screening for trisomy 21 combining biochemistry and ultrasound at individually optimal gestational ages. An interventional study. Prenat Diagn 2004;24:541–5. 15. Nicolaides KH. Screening for fetal aneuploidies at 11 to 13 weeks. Prenat Diagn 2011;31:7–15. 7. Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM. First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS). J Med Screen 2003;10:56–104. 16. Ekelund C, Wright D, Ball S, Kirkegaard I, Nørgaard P, Sørensen S, et al. Prospective study evaluating performance of first-trimester combined screening for trisomy 21 using repeat sampling of maternal serum markers PAPP-A and free β-hCG. Ultrasound Obstet Gynecol 2012;40:276–81. 8. Wald NJ, Rodeck C, Hackshaw AK, Rudnicka A. SURUSS in perspective. BJOG 2004;111:521–31. 17. Morgan S, Delbarre A, Ward P. Impact of introducing a national policy for prenatal Down syndrome screening on the diagnostic invasive procedure rate in England. Ultrasound Obstet Gynecol 2013;41:526–9. 9. Wright D, Bradbury I, Benn P, Cuckle H, Ritchie K. Contingent screening for Down syndrome is an efficient alternative to non-disclosure sequential screening. Prenat Diagn 2004;24:762–6. 10. Cuckle H, Benn P, Wright D. Down syndrome screening in the first and/or second trimester: model predicted performance using meta-analysis parameters. Semin Perinatol 2005;29:252–7. 11. Wald NJ, Rudnicka AR, Bestwick JP. Sequential and contingent prenatal screening for Down syndrome. Prenat Diagn 2006;26:769–77. 12. Malone FD, Canick JA, Ball RH, Nyberg DA, Comstock CH, Bukowski R, et al; First- and Second-Trimester Evaluation of Risk (FASTER) Research Consortium. First- 18. Nicolaides KH, Syngelaki A, Poon LC, Gil MM, Wright D. First-trimester contingent screening for trisomies 21, 18 and 13 by biomarkers and maternal blood cell-free DNA testing. Fetal Diagn Ther 2014;35:185–92. 19. Fairbrother G, Johnson S, Musci TJ, Song K. Clinical experience of noninvasive prenatal testing with cell-free DNA for fetal trisomies 21, 18, and 13, in a general screening population. Prenat Diagn 2013;33:580–3. 20. Chan YM, Leung TY, Chan OK, Cheng YK, Sahota DS. Patient’s choice between a non-invasive prenatal test and invasive prenatal diagnosis based on test accuracy. Fetal Diagn Ther 2014;35:193–8. Volume 23 | Issue 1 | April 2015 55 AL JO U R AL PE R AT N IN Case Report L Perinatal Journal 2015;23(1):56–59 R N A PE IN AT U AL JO R The association of congenital hand reduction defect and uterine anomaly Bülent Kars1, Önder Sakin2, Yasemin Karageyim Karfl›da¤3, Cenk Demir1, Esra Esim Büyükbayrak2 1 Department of Gynecology & Obstetrics, Private Dragos Gülen Medical Center, Istanbul, Turkey Department of Gynecology & Obstetrics, Dr. Lütfi K›rdar Kartal Training and Research Hospital, Istanbul, Turkey 3 Health High School, K›rklareli University, K›rklareli, Turkey 2 Abstract Özet: Konjenital el redüksiyon defekti ile uterus anomalisinin birlikteli¤i Objective: Fetal hand anomalies can be overlooked in ultrasonographic examinations. In our report, we aim to present the case of hand reduction defect in a patient with uterine anomaly that we diagnosed during antenatal follow-up with the use of 2D and 3D ultrasound examinations. Amaç: Fetal el anomalileri prenatal ultrasonografik incelemelerde gözden kaçabilmektedir. Bu yaz›m›zda uterus anomalisi olan bir olguda; 2 boyutlu ve 3 boyutlu ultrason ile antenatal takipte tan›s›n› koydu¤umuz bir el redüksiyon defekti olgusunu sunmay› amaçlad›k. Case: Genetic consultation was provided to a patient who had absence of hand in one extremity during the ultrasound control performed for triple test while nothing was detected in the ultrasound for double test screening. After the amniocentesis, the karyotype of fetus was found as normal (46 --). No other anomaly was observed in perinatology consultation, anomaly screening and fetal echocardiography. Remaining gestational period of the patient was free of problem and a single 3300 g fetus was delivered by cesarean section through breech presentation and the pictures of the hand were taken with the permission of the family. Olgu: ‹kili test taramas›nda ultrasonda fark edilmeyen ancak üçlü test amac›yla yap›lan ultrason kontrolünde bir ekstremitesinde el yoklu¤u tespit edilen hastaya genetik dan›flmanl›k verildi. Hastaya amniosentez yap›ld›ktan sonra fetüsün karyotipi normal (46 --) olarak geldi. Perinatoloji konsültasyonu, anomali taramas› ve fetal ekokardiyografide efllik eden baflka bir anomali tespit edilmedi. Hastan›n geri kalan gebelik süreci sorunsuz geçti ve 3300 g, tekiz canl› makat ile prezante olan fetüs sezaryen operasyonu ile do¤urtuldu ve ailenin izni ile elin foto¤raflar› çekildi. Conclusion: Congenital hand reduction defects may occur together with uterine anomalies. Such anomalies can be diagnosed easily during ultrasonographic examinations in early weeks of gestation, and therefore they should be a part of early anomaly screening procedures. Sonuç: Konjenital el redüksiyon defektleri uterus anomalileri ile birliktelik gösterebilen durumlard›r. Bu anomalilerin tan›s› erken gebelik haftalar›nda yap›lan ultrason incelemesinde rahatl›kla konabilir ve bu nedenle erken anomali taramalar›n›n bir parças› olmal›d›r. Keywords: Congenital diagnosis, congenital hand deformities. Anahtar sözcükler: Konjenital tan›, do¤umsal el deformiteleri. Introduction Congenital hand reduction defect is the stump end or full or partial absence of an extremity at the distal of a point. Transverse forming defect is also known as transverse reduction defect, transverse melia or transverse arrest.[1] Congenital anomaly is seen about 1% of newborns, and 10% of such cases are upper extremity anomalies. Congenital hand reduction defect is seen one in every 20,000 births. In 50% of these cases, there is simple transverse reduction defect on forearm or hand, and no other concomitant anomaly. In other 50% of the cases, Correspondence: Bülent Kars, MD. Özel Dragos Gülen T›p Merkezi Kad›n Hastal›klar› ve Do¤um Klini¤i, ‹stanbul, Turkey. e-mail: ‹stanbulent1972kars@yahoo.com Received: November 27, 2014; Accepted: February 16, 2015 Please cite this article as: Kars B, Sakin Ö, Karageyim Karfl›da¤ Y, Demir C, Esim Büyükbayrak E. The association of congenital hand reduction defect and uterine anomaly. Perinatal Journal 2015;23(1):56–59. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231011 doi:10.2399/prn.15.0231011 QR (Quick Response) Code: The association of congenital hand reduction defect and uterine anomaly there is more than one reduction and 25% of such cases also have anomalies in other organs or in craniofacial structures.[2] Congenital hand reduction defect of upper extremity is usually an isolated anomaly. Congenital hand anomalies may occur together with uterine anomalies. In our case, we aimed to discuss hand reduction defect that we diagnosed during antenatal follow-up with the use of 2D and 3D ultrasound examinations. Case Report In the obstetric examination of a 27-year-old patient who referred to our clinic for the complaint of delayed menstruation, gestation was observed through fetal cardiac activity which was intrauterine but located on cornual region close to right uterine. The patient who was pregnant for the first time had no kin marriage and specific finding in her family history. The patient was prescribed folic acid support and called for follow-up two weeks later in terms of cornual pregnancy. In her follow-ups, the localization of gestational sac was normal. Double screening test of the patient between 11 and 14 weeks of gestation were within normal ranges. The patient who started to take iron support visited the clinic for AFP screening at 17 weeks of gestation. In the USG examination, absence of hand in the extremity was found and genetic consultation was provided to the patient (Figs. 1 and 2). After the genetic amniocentesis, the karyotype of fetus was found as normal (46 --). No other anomaly was observed in perinatology con- sultation, anomaly screening and fetal echocardiography. Remaining gestational period of the patient was free of problem and a single 3300 g fetus was delivered by cesarean section through breech presentation and the pictures of the hand were taken with the permission of the family (Fig. 3). It was found during the operation that uterus was unicornuate, and the presence of non-communicating horn was detected on the left. Both tubes and ovaries were normal. Fig. 2. 3D USG image for the absence of hand. Fig. 3. Postnatal image for the absence of hand. Fig. 1. 2D USG image for the absence of hand. Discussion The best time to evaluate fetal hands with ultrasound is between the end of first trimester and mid-period of sec- Volume 23 | Issue 1 | April 2015 57 Kars B et al. ond trimester. During this period, fetus moves frequently and hands are on open position more frequently than next periods. 3D USG is not necessary; however, it may be useful to define the morphology better.[3] We detected our case who referred for AFP test at 17 weeks of gestation when we observed the absence of the hand in the extremity. We applied 3D USG to the patient at the same session and confirmed the diagnosis. Hand anomalies may be isolated and also may accompany to other skeletal and organ anomalies, aneuploidies, syndromes and bone dysplasias.[4,5] Therefore, if a hand anomaly is detected, the patient should be referred to a center where all fetal and cardiac anomalies can be investigated. We therefore carried out genetic screening by amniocentesis, and investigated other anomalies at further weeks by perinatology consultation and anomaly screening. We found no additional concomitant pathology. Congenital transverse arrest, amniotic band syndrome and Adams-Oliver syndrome (an autosomal dominant inherited syndrome with aplasia cutis and asymmetric transverse extremity defects) are among the distinctive diagnosis of congenital distal hand reduction defect which is also a complication of early period chorion villus sampling. Amniotic band syndrome is usually sporadic and generally causes asymmetric anomaly.[6] Amniotic band, which develops after embryologic development is completed, may cause many hand defects from hand reduction up to syndactyly. Congenital transverse arrest is seen rarely although there are great differences among societies and countries in terms of its incidence rate. Genetics, environmental factors and teratogenic agents are shown as the reason in the etiology; however, actual reasons have not been clearly identified. Ninety-eight percent of congenital transverse arrest is unilateral.[7] It was reported that transverse arrest may be seen together with some congenital anomalies; and transverse arrest was found together with congenital band syndrome in one case.[1] Unicornuate uterine anomaly was found in the patient. However, before identifying this uterine anomaly, it was seen in the ultrasound during the first referral of the patient that gestational sac was located in a region close to cornual area. Uterine anomaly was confirmed by the cesarean section carried out due to breech presentation in the case. In the literature, it has 58 Perinatal Journal been stated that there is a relationship between uterine anomalies and extremity defects. It has been reported that it may cause reduction defects and problems in extremity development associated with compression in uterine anomalies.[8] Extremity processes can be seen with ultrasound at 8 weeks of gestation at the earliest. Femur and humerus can be seen as of 9 weeks of gestation, tibia/fibula and radius/ulna as of 10 weeks of gestation, fingers and toes as of 11 weeks of gestation, and all long bones can be seen fully as of 11 weeks of gestation.[9,10] The aim in early anomaly screening is to diagnose minor or major anomalies before it is too late and to be able to get early management chance. Therefore, carefully checking the extremities of fetuses in the ultrasound examination to be performed for double test will help to identify this anomaly at early weeks. Conclusion Congenital hand reduction defects may occur together with uterine anomalies. Such anomalies can be diagnosed easily by carrying out ultrasonographic examinations in early weeks of gestation, and therefore they should be a part of early anomaly screening procedures. Conflicts of Interest: No conflicts declared. References 1. Jain S, Lakhtakia PK. Profile of congenital transverse deficiencies among cases of congenital orthopaedic anomalies. J Orthop Surg (Hong Kong) 2002;10:45–52. 2. Pilu G, Nicolaides KH. Fetal Anomalilerin Prenatal Tan›s› / 18–23 Gebelik Haftas› Ultrasonu. Çeviri: Hayri Ermifl. Nashville, TN: Panthenon 2000; p: 94. 3. Reiss RE, Foy PM, Mendiratte V, Kelly M, Gabbe SG. Ease and accuracy of evaluation of fetal hands during obstetrical ulrasonography: a prospective study. J Ultrasound Med 1995; 14:813–20. 4. Budorick NE. The fetal musculoskeletal system. In: Callen PW, ed. Ultrasonography in Obstetrics and Gynecology. 4th ed. Philadelphia: Saunders; 2000; p: 331–77. 5. Ploeckinger-Ulm B, Ulm MR, Lee A, Kratochwil A, Bernaschek G. Antenatal depiction of fetal digits with three dimentional ultrasonography. Am J Obstet Gynecol 1996; 175:571–4. 6. Rypens F, Ziereisen F, Avni F. Perinatal diagnosis of musculoskeletal anomalies. In: Avni FE, ed. Perinatal Imaging: The association of congenital hand reduction defect and uterine anomaly From Ultrasound to MR Imaging. New York: Springer; 2002; p: 197-226. 7. Ogino T, Saitou Y. Congenital constriction band syndrome and transverse deficiency. J Hand Surg Br 1987;12:343–8. 8. Graham JM, Miller ME, Stephan MJ, Smith DW. Limb reduction anomalies and early in utero limb compression. J Pediatr 1980;96:1052–6. 9. Van Zalen-Sprock RM, Brons JT, van Vugt JM, van der Harten HJ, van Geijn HP. Ultrasonographic and radiologic visualization of the developing embryonic skeleton. Ultrasound Obstet Gynecol 1997;9:392–7. 10. Timor-Tritsch IE, Farine D, Rosen MG. A close look at early embryonic development with the high-frequency transvaginal transducer. Am J Obstet Gynecol 1988;159: 676–81. Volume 23 | Issue 1 | April 2015 59 AL JO U R AL PE R AT N IN Case Report L Perinatal Journal 2015;23(1):60–64 R N A PE IN AT U AL JO R Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case Sevil Eraslan, Rauf Meleko¤lu, Ebru Çelik Department of Gynecology & Obstetrics, Faculty of Medicine, Inönü University, Malatya, Turkey Abstract Özet: Tek tarafl› ileri derecede fetal hidrotoraks olgusunda ekstrauterin intrapartum tedavi prosedürü Objective: Congenital hydrothorax is a rare anomaly seen in one per 10,000–15,000 pregnancies. Progress of the prenatal diagnosis has enabled the practice of extrauterine intrapartum treatment (EXIT) procedure in the fetal hydrothorax management. In this report, we presented a unilateral advanced fetal hydrothorax case found on ultrasonography at third trimester and underwent EXIT procedure during delivery. Amaç: Konjenital hidrotoraks, 10.000–15.000 gebelikte bir görülen nadir bir anomalidir. Prenatal tan›n›n ilerlemesi, fetal hidrotoraks yönetiminde ekstrauterin intrapartum tedavi (EXIT) prosedürünün uygulanmas›na olanak sa¤lam›flt›r. Bu makalede 3. trimesterde ultrasonografide saptanm›fl, do¤umda EXIT iflleminin uyguland›¤›, tek tarafl› ileri derecede fetal hidrotoraks olgusu sunulmufltur. Case: No additional anomaly was observed except unilateral pleural effusion and polyhydramnios on the right in the obstetric ultrasonography of the thirty-five-year-old primigravida patient with no specific finding in medical and obstetric histories who was referred to our clinic when pleural effusion and polyhydramnios were found in fetus at 36 weeks of gestation for the first time during routine obstetric follow-up. EXIT procedure was carried out in the case where perinatologists, neonatologist and pediatric surgeon were present in a sterile way during the cesarean operation. Olgu: Otuz befl yafl›nda primigravid, t›bbi ve obstetrik öyküsünde herhangi bir özellik saptanmayan, rutin obstetrik takibi s›ras›nda ilk kez gebeli¤in 36. haftas›nda fetüste plevral efüzyon ve polihidramniyos saptanmas› üzerine klini¤imize yönlendirilen hastada yap›lan obstetrik ultrasonografide sa¤da tek tarafl› plevral efüzyon ve polihidramniyos d›fl›nda ek anomali izlenmedi. Sezaryen s›ras›nda perinatolog, neonatalog ve çocuk cerrah›n›n steril bir flekilde haz›r olarak bulundu¤u vakada EXIT prosedürü uyguland›. Conclusion: EXIT procedure is a safe treatment option in fetal hydrothorax cases since it allows placentofetal circulation during large amount of pleural effusion discharge from newborn at birth. Sonuç: EXIT prosedürü, fetal hidrotoraks olgular›nda, do¤umda yenido¤andan büyük miktarda plevral efüzyonun boflalt›mas› s›ras›nda plasentofetal sirkülasyona izin verdi¤i için güvenli bir tedavi seçene¤idir. Keywords: EXIT procedure, hydrothorax, obstetric surgical procedures. Anahtar sözcükler: EXIT prosedürü, hidrotoraks, obstetrik cerrahi giriflimler. Introduction Congenital hydrothorax is the fluid accumulation in pleural cavity seen in one per 10,000–15,000 pregnancies and it has many reasons such Noonan syndrome, chromosomal anomalies, immune system disease, car- diac failure etc.[1,2] Primary congenital pleural effusion may be unilateral or bilateral; it is usually on the right side and in cheilosis form.[3] While it may regress spontaneously, it has a variable prognosis reaching up to fetal or neonatal death.[4,5] Particularly, some of the bilateral severe congenital hydrothorax cases may Correspondence: Rauf Meleko¤lu, MD. ‹nönü Üniversitesi T›p Fakültesi Kad›n Hastal›klar› ve Do¤um Anabilim Dal›, Malatya, Turkey. e-mail: rmelekoglu@gmail.com Received: November 12, 2014; Accepted: February 24, 2015 Please cite this article as: Eraslan S, Meleko¤lu R, Çelik E. Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case. Perinatal Journal 2015;23(1):60–64. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231013 doi:10.2399/prn.15.0231013 QR (Quick Response) Code: Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case progress rapidly and may result in intrauterine death due to pulmonary hypoplasia developing as a result of long-term pressure. Antepartum treatment options have been developed depending on the increase of ultrasonography use in prenatal diagnosis. Prenatal treatment varies depending on the pleural effusion amount and the diagnosis week of gestation.[6] If isolated pleural effusion is detected before 32 weeks of gestation, it usually has a poor prognosis and it is fatal in 55% of the cases. Mortality rate is 30% in pleural effusion cases diagnosed after 32 weeks of gestation.[7] If hydrops fetalis accompanies pleural effusion cases, mortality rate is almost 100%.[6] When prenatal diagnosis is accurate and other fatal anomalies are ruled out, prenatal invasive procedure is useful, even life-saving in some bilateral cases with poor prognosis. In the presence of pleural effusion especially diagnosed at first and second trimesters, thoracic needling is not curative and thoracoamniotic shunt is preferred in such cases since recurrence rate is high.[8] Thoracoamniotic shunt placed by using intrauterine thoracentesis or double pigtail catheter in fetal hydrothorax management is not always efficient since it depends on fetal and placental position. If drainage and ventilation are insufficient for rapid lung expansion and alveolar gas exchange when thoracentesis is carried out after postnatal emergency intubation in pleural effusion management, permanent hypoxemic cerebral damage may occur. In this report, we presented an unilateral advanced fetal hydrothorax case found on ultrasonography at third trimester and underwent EXIT procedure. Case Report Thirty-five-year-old primigravida patient with no specific finding in medical and obstetric histories was referred to our clinic when pleural effusion and polyhydramnios were found in fetus at 36 weeks of gestation for the first time during routine obstetric follow-up. In the obstetric ultrasonography of the patient whose pregnancy developed spontaneously, it was found that fetal biometric measurements were consistent with the week of gestation, there was no additional anomaly except unilateral pleural effusion and polyhydramnios on the right (Fig. 1). In the examinations to understand the reasons of fetal pleural effusion of patient whose blood type was 0 Rh (+), maternal TORCH panel was negative and fetal echocardiography (ECO) result was normal. Biochemical examinations, gram staining, culture and karyotype analyses were done on thoracentesis fluid collected during intrauterine fetal thoracentesis. There was no reproduction in the culture analysis made on pleural fluid found to be in chylothorax characteristics according to biochemical parameter. The result of karyotype analysis was normal. The patient was provided newborn, pediatric surgery and anesthesia consultations by Perinatology Department, and cesarean operation Progress of the prenatal diagnosis has enabled the practice of extrauterine intrapartum treatment (EXIT) procedure in the fetal hydrothorax management.[9] EXIT is the procedure representing the operations carried out on newborn before cord flow is cut when fetal-placental unit is functional during the delivery. It is applied first in congenital diaphragmatic hernia.[10] While the most frequent indication is external and internal airway obstructions, there are also other indications. These indications are the removal of obstructive apparatus (gripper, balloon) in the temporary tracheal obstruction, great neck masses (cervical teratoma, lymphangioma), congenital high airway obstruction syndrome (CHAOS), extracorporeal membrane oxygenization (ECMO).[11] EXIT procedure helps to gain time for safe adaptation of newborn.[12] Fig. 1. The image of pleural effusion on the right side of fetus found at the 36 week of gestation via gray-scale ultrasonography. Volume 23 | Issue 1 | April 2015 61 Eraslan S, Meleko¤lu R, Çelik E under elective conditions at 38 weeks of gestation and EXIT procedure were planned. Spinal anesthesia was applied in the case where intraoperative perinatologist, neonatologist and pediatric surgeon were present in a sterile way. No drug was administered for the relaxation of uterine. By performing hysterectomy through lower segment transverse incision, 2840 g male baby was delivered. The newborn was placed on a sterile and flat surface on the legs of mother as maintaining uteroplacental and placentofetal circulation, not stretching the cord and on the placenta level without clamping. While obstetrician was providing maternal hemostasis, the pulse of the umbilical cord was checked during the procedure. Underwater drainage was performed by inserting tube thoracostomy into right pleural cavity via 16G intravenous catheter through 4th intercostal space (Fig. 2). Newborn evaluated by neonatologist during tube thoracostomy and drainage did not require intubation. During this period, about 400 cc pleural fluid in cheilosis form was discharged. The baby, whose cord was clamped on the fourth minute of labor and who was stabilized after tube thoracostomy, was transferred to newborn intense care unit for examination, treatment and follow-up. In the direct chest radiography during the followups in newborn intense care unit, pneumothorax was observed in the left lung and therefore thorax tube was also placed on the left side. No pathological finding was found in the examinations carried out for pleural effusion etiology. Newborn received respiratory support by nasal continuous positive airway pressure (nCPAP), and bilateral thorax tubes were removed when pleural effusion on the right and pneumothorax on the left regressed on the third day in newborn intense care unit. On the 14th day in newborn intense care unit, the baby was discharged in a healthy condition with completely regressed pleural effusion by recommending newborn clinical follow-up. increase depending on the increase of early diagnosis together with the wide use of antenatal ultrasonography. Pleural effusion case was first found by Carrol in a pregnant woman at 27 weeks of gestation.[14] Generally, 75% of the cases are diagnosed at third trimester. In the literature, the earliest diagnosis of pleural effusion case was reported in the 13 week of gestation.[15] Pleural effusion is usually detected by ultrasonography at third trimester and it frequently accompanies to polyhydramnios developing secondarily as a result of the external pressure of advanced pleural effusion to esophagus.[16] The prognosis of pleural varies. Perinatal mortality rate associated with pleural effusion is about 50%. Considering the clinical progress of such patients, it is seen that 22% of them regress spontaneously, 43% of them recover by treatment, and 35% of them result in fetal or neonatal death. In the absence of polyhydramnios, unilateral pleural effusion cases generally regress a b Discussion Fetal hydrothorax may occur due to idiopathic and secondary reasons. Among the secondary reasons, there are cardiac, pulmonary and gastrointestinal malformations, infectious, hematologic and chromosomal diseases and immune hydrops.[13] Fetal hydrothorax is a rare anomaly and its pathogenesis is not known clearly although its incidence rates 62 Perinatal Journal Fig. 2. EXIT procedure (a). Underwater drainage procedure by inserting thorax tube into the right pleural cavity (b). Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case spontaneously. In pleural effusion cases caused by hydrops, the prognosis is poor independent from the gestational age and the presence of bilateral effusion.[15] tion and cooperation both when deciding to apply EXIT procedure and planning the procedure, and we prepared plans for interventions against possible complications. The initial treatment of fetal pleural effusion is the drainage with aspiration needle in company with ultrasonography. In the meantime, amniocentesis can be performed or the etiology can be investigated by collecting fetal blood sample. Reasons such as anemia and cardiac arrhythmia, which are among the causes of pleural effusion but can be treated, should be investigated. In case of the re-accumulation of pleural fluid in the follow-ups after drainage, pleuro-amniotic shunt can be considered.[15] There are two significant complications which may affect EXIT procedure. First, intraoperative uterine hemorrhage may require delivering placenta swiftly; and secondly, since uterine contractions may disorder uteroplacental circulation right after the delivery, halothane administration may be required to prevent such disorder and to help the relaxation of uterine. We ensured intraoperative uterine hemostasis rapidly in our case of which we planned perinatal management and we did not need any medication reducing uterine contractions.[20] It was reported in the literature that EXIT procedure was first used when removing tracheal clip placed to prevent tracheal obstruction caused by severe congenital diaphragmatic hernia.[17] EXIT is a procedure generally used in the management of extrinsic (teratomas, lymphangiomas) or intrinsic (laryngeal atresia, congenital upper airway obstruction syndrome) obstructive malformations of upper airways diagnosed during prenatal period.[18] The widest series in the literature was reported by Bouchard et al. in 2002. Thirty-one cases applied EXIT were detailed. In their series, they did not report any case applied for pleural effusion, but they stated that they applied EXIT procedure due to mass in the neck in 13 cases and that they lost only one case during the EXIT procedure.[19] First application of EXIT procedure in the severe advanced fetal bilateral pleural effusion case detected during prenatal period was reported by Prontera et al. in the literature.[20] In the case reported by Prontera et al., which had pregestational diabetes and normal follow-up results until 32 weeks of gestation, severe isolated bilateral pleural effusion was found at 38 weeks of gestation, the case was applied EXIT supported bilateral thoracentesis procedure; the newborn was extubated on the 5th day of its life, and was discharged on 25th day in a healthy condition. They emphasized that the close and efficient cooperation among anesthetist, obstetrician, neonatologist and pediatric surgeon to maintain fetoplacental circulation during EXIT procedure, and pointed out the necessity to plan the procedure in detail.[20] In our case, we worked with the teams of anesthesia, newborn and pediatric surgery in our clinic with continuous communica- Conclusion Although intrapartum thoracentesis is a preferred method in fetuses with severe pleural effusion in the last period of gestation, thoracentesis together with ultrasound may cause fetal lung injury and fetal distress induced by excessive amount of pleural fluid collection, and this procedure cannot be applied in some cases due to inappropriate fetal position. EXIT is a procedure appropriate to use in cases where intrauterine drainage is technically difficult or impossible and postpartum drainage may cause deep and extended hypoxia until pleural fluid drainage is done sufficient enough to allow lung expansion in the newborn. It is a safe treatment options as it allows placentofetal circulation during the discharge of pleural effusion in large amounts. More experience and further studies are required in order to reveal maternal and neonatal effects of applying EXIT procedure in fetal hydrothorax cases, and this procedure should be limited with viable newborns appearing only at late gestational periods today. Conflicts of Interest: No conflicts declared. References 1. John E. Pleural effusion in the newborn. Med J Aust 1974;1: 102–3. 2. Longaker MT, Laberge JM, Dansereau J, Langer JC, Crombleholme TM, Callen PW et al. Primary fetal hydrothorax: natural history and management. J Pediatr Surg 1989;24: 573–6. 3. Agrawal R, Aggarwal R, Kriplani A, Bhatla N. Primary Fetal Hydrothorax. Indian Pediatr 2002;39:92–5. 4. Eddleman KA, Levine AB, Chitkara U, Berkowitz RL. Reliability of pleural fluid lymphocyte counts in the antena- Volume 23 | Issue 1 | April 2015 63 Eraslan S, Meleko¤lu R, Çelik E tal diagnosis of congenital chylothorax. Obstet Gynecol 1991;78(3 Pt 2):530–2. 13. Lange IR, Manning FA. Antenatal diagnosis of congenital pleural effusions. Am J Obstet Gynecol 1981;140:839–40. 5. Aubard Y, Derouineau I, Aubard V, Chalifour V, Preux PM. Primary fetal hydrothorax: a literature review and proposed antenatal clinical strategy. Fetal Diagn Ther 1998;13:325– 33. 14. Carrol B. Pulmonary hypoplasia and pleural effusions associated with fetal death in utero: ultrasonic findings. AJR Am J Roentgenol 1977;129:749–50. 6. Pijpers L, Reuss A, Stewart PA, Wladimiroff JW. Noninvasive management of isolated bilateral fetal hydrothorax. Am J Obstet Gynecol 1989;161:330–2. 7. Hagay Z, Reece A, Roberts A, Hobbins JC. Isolated fetal pleural effusion: a prenatal management dilemma. Obstet Gynecol 1993;81:147–52 8. Gonen R, Degani S, Shapiro I, Samberg I, Sharf M. The effect of drainage of fetal chylothorax on cardiac and blood vessel hemodynamics. J Clin Ultrasound 1993;21:265–8. 9. Kern C, Ange M, Morales, Peiry B, Pfister RE. Ex utero intrapartum treatment (EXIT), a resuscitation option for intrathoracic foetal pathologies. Swiss Med Wkly 2007;137:279– 85. 10. Mychaliska GB, Bealer JF, Graf JL, Rosen MA, Adzick NS, Harrison MR. Operating on placental support: the ex utero intrapartum treatment procedure. J Pediatr Surg 1997;32: 230–1. 11. MacKenzie TC, Crombleholme TM, Flake AW. The exutero intrapartum treatment. Curr Opin Pediatr 2002;14: 453–8. 12. Henry PY, Aravindan CS, Sivakumar K, Krishna HR. Extrauterine ›ntrapartum treatment (EXIT) in bilateral primary fetal hydrothorax. Indian J Pediatr 2009;76:99–101. 64 Perinatal Journal 15. National Institute for Health and Clinical Excellence. Insertion of pleuro-amniotic shunt to drain fetal pleural effusion (Interventional Procedure Consultation Document) [Internet]. 2006 [cited 2014 Sept 2]. Available from: www.nice.org.uk/ip333 overview 16. Mandelbrot L, Dommergues M, Aubry MC, Mussat P, Dumez Y. Reversal of fetal distress by emergency in utero decompression of hydrothorax. Am J Obstet Gynecol 1992; 167:1278–83. 17. Mychaliska GB, Bealer JF, Graf JL, Rosen MA, Adzick NS, Harrison MR. Operating on placental support: the ex utero intrapartum treatment procedure. J Pediatr Surg 1997;32: 227–31. 18. Hirose S, Farmer DL, Lee H, Nobuhara KK, Harrison MR. The ex utero intrapartum treatment procedure: looking back at the EXIT. J Pediatr Surg 2004;39:375–80 19. Bouchard S, Johnson MP, Flake AW, Howell LJ, Myers LB, Adzick NS, et al. The EXIT procedure: experience and outcome in 31 cases. J Pediatr Surg 2002;37:418–26. 20. Prontera W, Jaeggi ET, Pfizenmaier M, Tassaux D, Pfister RE. Ex utero intrapartum treatment (EXIT) of severe fetal hydrothorax. Arch Dis Child Fetal Neonatal Ed 2002;86: F58–60. AL JO U R AL PE R AT N IN Case Report L Perinatal Journal 2015;23(1):65–69 R N A PE IN AT U AL JO R Goiter in fetus without maternal thyroid disease: a case report Önder Sakin1, Bülent Kars2, Yasemin Karageyim Karfl›da¤3, Cenk Demir2, Esra Esim Büyükbayrak1 1 Department of Gynecology & Obstetrics, Dr. Lütfi K›rdar Kartal Training and Research Hospital, Istanbul, Turkey 2 Private Dragos Gülen Medical Center, Istanbul, Turkey 3 Health High School, K›rklareli University, K›rklareli, Turkey Abstract Özet: Maternal tiroid hastal›¤› olmayan fetüste guatr: Olgu sunumu Objective: The aim is to discuss fetal hypothyroidism which we consider that its prenatal diagnosis and treatment is significant since it may cause physical and mental growth retardation in affected fetuses. Amaç: Amaç, etkilenen fetüslerde fiziksel ve zihinsel geliflme geriliklerine yol açabildi¤i için prenatal tan› ve tedavisinin önemli oldu¤unu düflündü¤ümüz fetal hipotiroidizmi güncel bilgiler ›fl›¤›nda tart›flmakt›r. Case: A fetal goiter case was presented which was found during routine ultrasonographic examination at 30 weeks of gestation. The pregnant women had no thyroid history and all thyroid function tests were normal including thyroid auto-antibodies in laboratory tests. In the Doppler ultrasonography, a thyroid gland grown diffusely with increased bloodshot was observed in the fetus. By these findings, it was considered that fetal goiter would be caused by fetal hypothyroidism. Amniocentesis or cordocentesis was recommended as final diagnosis, but the patient refused invasive procedures. Olgu: Otuz haftal›k gebe iken rutin ultrasonografi incelemesinde tespit edilmifl bir fetal guatr olgusu sunuldu. Gebenin özgeçmiflinde tiroid hastal›¤› öyküsü mevcut de¤ildi ve laboratuvar testlerinde tiroid otoantikorlar› da dahil tüm tiroid fonksiyon testleri normaldi. Doppler ultrasonografide fetüste diffüz olarak büyümüfl ve kanlanmas› artm›fl tiroid bezi izlendi. Bu bulgularla fetal guatr›n fetal hipotiroidizme ba¤l› olabilece¤i düflünüldü. Kesin tan› için amniyosentez veya kordosentez önerilen hasta invazif giriflimleri kabul etmedi. Conclusion: Doppler and ultrasonographic findings are important for fetal goiter diagnosis and follow-up. Sonuç: Fetal guatr tan› ve izleminde ultrasonografi ve Doppler bulgular› önemlidir. Keywords: Fetal goiter, ultrasonography, prenatal diagnosis. Anahtar sözcükler: Fetal guatr, ultrasonografi, prenatal tan›. Introduction Thyroid disorders are the common endocrine disorders seen during perinatal period. While maternal thyroid anomalies can be diagnosed easily by maternal serum tests, it is considerably difficult to determine and diagnose fetal goiter.[1] Different biochemical disorders in the thyroid hormone synthesis or maternal autoimmune thyroid diseases may cause fetal goiter.[2] Goiter may be related with fetal hypothyroidism or hyperthyroidism. Many authors believe the necessity to determine fetal thyroid function in order to initiate early treatment process for this condition.[3] Weiner et al. reported in 1980 for the first time that they diagnosed fetal goiter by prenatal sonography method.[4] Presence of a large thyroid gland on fetal neck region may cause a difficult delivery due to polyhydramnios by Correspondence: Önder Sakin, MD. ‹stanbul Dr. Lütfi K›rdar Kartal E¤it. ve Arafl. Hast., Kad›n Hastal›klar› ve Do¤um Klini¤i, ‹stanbul, Turkey. e-mail: sakin-onder@hotmail.com Received: October 29, 2014; Accepted: December 20, 2014 Please cite this article as: Sakin Ö, Kars B, Karageyim Karfl›da¤ Y, Demir C, Esim Büyükbayrak E. Goiter in fetus without maternal thyroid disease: a case report. Perinatal Journal 2015;23(1):65–69. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231004 doi:10.2399/prn.15.0231004 QR (Quick Response) Code: Sakin Ö et al. esophageal and tracheal pressure and also hyperextension on neck by mass effect.[5] Fetal hypothyroidism generally depends on antithyroid treatments or endemic iodine deficiency. Their incidence rate is very low without maternal disease.[6] iodine or thyroid drug history. In the maternal examination, no examination finding related with thyroid disease was found. There was also no anomaly in routine gestational analyses. The 28-year-old patient having her first pregnancy admitted to our hospital for examination on her 30 weeks of gestation. A great homogeneous mass was detected on the anterior side of fetal neck during ultrasonographic examination. The mother was married to her second cousin. There was no thyroid disease in the history or family history of the mother. She had no In the ultrasonographic examination, a wide, symmetric and bilobulated mass pressuring trachea on the anterior side of the fetal neck (47.4x32.2x26.6 mm) (Fig. 1) and mild polyhydramnios were found. Due to its pressure on esophagus and trachea, angle changes made by growing thyroid tissue on the background, deterioration in normal traces and concomitant polyhydramnios, we suspected of the presence of goiter. The mass was in very vascularized appearance in the Doppler examination (Fig. 2). Fetal heart rate was 220 bpm. It was seen as a tachycardia in sinusoidal type. No other anomaly was observed in the fetus. Fetal growth and movements were normal. Maternal serum thyroid function tests and thyroid ultrasound results were normal. The mother was euthyroid, free T3 was 3.34 pg/ml, free T4 was 2.30 ng/dl and TSH was 3.86 IU /ml. Anti-thyroid antibodies were negative. The family was informed about fetal condition and prognosis. The family refused to have any invasive procedure such as amniocentesis, cordocentesis and/or intraamniotic thyroxine treatment. Fetal condition, cardiac activity, fetal development, thyroid dimensions and fetal thyroid bleeding were followed up by color Doppler. No pathology was seen to explain fetal tachycardia. In the follow-ups during further weeks, fetal heart rate was observed within normal ranges. Since newborn cardiac evaluation was not characterized, Fig. 1. Fig. 2. As in the world, hypothyroidism screening is carried out successfully during newborn period in Turkey and successful treatments are performed as of the early period. However, hypothyroidism developing in fetal period is very significant for the life. The possibility of congenital hypothyroidism which causes mental retardation but mostly possible to treat is 1 out of each 4000 live birth.[7] Fetal goiter hypothyroidism forming only 10–15% of all congenital hypothyroidism cases is rarely seen (one out of 4000).[8] Thanks to the development in ultrasonography technology, even though it is a rare case, the number of reports prepared for fetal goiter investigations increases day by day.[9] Case Report 66 2D ultrasound image of fetal goiter. Perinatal Journal Doppler ultrasound image of fetal goiter. Goiter in fetus without maternal thyroid disease no further evaluation and diagnosis method was required. it may cause obstruction due to trachea, and the mechanic problems during delivery may cause morbidity.[12] The patient delivered a male baby (2600 g) by cesarean since the delivery began on 36 weeks of gestation and due to pelvic contraction. One-minute APGAR score was 6, and five-minute score was 7. There was bilobulated goiter; however, it caused no obstruction in the airway of newborn and resuscitation was not required. The baby had no problem with postnatal respiratory adaptation. Postnatal color Doppler examination confirmed enlarged thyroid gland. One of the prenatal examinations is Doppler ultrasound. It can be seen in the Doppler ultrasound that neck vessels spread around soft tissue mass. If it is hypervascular, the increase in the diameters of carotid and jugular veins can be seen. In case of hyperthyroidism, the diffuse increased flow in the gland can be seen. In case of hypothyroidism, peripheral flow around the gland can be observed.[6] Iodothyronines in cord blood and TSH measurements confirmed the diagnosis of hypothyroidism. As of the first neonatal day, oral 50 mcg/day thyroxine hormone treatment was initiated. Fetal tachycardia was not observed after the delivery. Weight, height and psychomotor developments of child were normal in the first 6 months, and the follow-ups have been maintained. Discussion A great goiter may cause fetal neck hyperextension resulting with malpresentation and complicated delivery process. The trachea may be obstructed after birth due to goiter, and this may cause asphyxia and death. During the delivery, pediatric anesthesia and pediatric ENT experts should be present in the delivery room with their intubation and bronchoscopy devices. Neonatal screening programs are successfully used in the diagnosis of congenital hypothyroidism just after the delivery and normal development is remedied significantly by early postnatal treatment. On the other hand, some babies exposed to congenital hypothyroidism have difficulties and delays in neuromotor, perception and language abilities despite the postnatal early treatment. Therefore, it is important to place emphasis on prenatal treatment of congenital hypothyroidism.[10] The enlargement of thyroid gland can be seen by ultrasonography on the anterior side of the fetal neck as homogenous straight masses with high echogenicity and distinct edges. The mass can be bilobulated and its size can enlarge up to 30–35 mm.[11] There are also nomograms for thyroid dimensions appropriate to related fetal weeks of gestation. It can be considered that the treatment of fetal hypothyroidism during intrauterine period is controversial; however, it has been reported that the treatment of fetuses with large goiter is indicated. The reason is that However, in another source, it was reported that the detection of the increase in blood flow towards fetal thyroid is an unreliable finding of hyperthyroid, and even surprisingly, that increased blood flow was found by using power Doppler for hypothyroidism.[13] Consequently, it is not possible to make clear interpretation about thyroid functions just based on Doppler findings. Amniotic fluid concentrations of TSH reflect fetal serum levels properly. However, Bruner and Dellinger asserted that fetal cord blood measurements are more reliable, and the evaluation made by amniocentesis is suspicious.[14] Fetal thyroid functions can be evaluated properly by fetal blood sampling method; however, this method is more risky since it has a 1% risk of fetal death.[15] However, the publications stating that the determination of thyroid hormone levels found through amniotic fluid is not reliable for the diagnosis are predominant.[16] The association of fetal goiter with chromosomal anomalies was analyzed, and it was found that it has no association with aneuploidy. However, in the Pendred syndrome, hearing loss in sensorineural type and goiter can be seen. It is an autosomal recessive condition and thyroid hormone synthesis is insufficient.[6] Different approaches may be applied in fetal treatment. If fetal goiter is detected in pregnant women receiving treatment for maternal hyperthyroidism, decreasing the drug dose by considering the placental transition of drugs and following up fetal thyroid gland measurements have been recommended. If fetal goiter sizes decrease as a result of this treatment, it is recommended to perform no procedure. However, if goiter continues to enlarge or no respond is received, the fetus may have hyperthyroid and it is suggested to analyze direct fetal thyroid hormones by doing cordocentesis. If fetal hyperthyroidism is found as a result, maternal treatment dose is increased until a fetal Volume 23 | Issue 1 | April 2015 67 Sakin Ö et al. respond is received. Propylthiouracil is recommended as the drug.[6] Intra-amniotic levothyroxine injection as the least invasive approach in fetal treatment referred by Abuhamad et al. is a treatment method accepted widely so far.[17] In this sense, Medeiros-Neto et al. found increased TSH and decreased sT4 in the cordocentesis analysis of the fetus with 29×34 mm fetal goiter at 23 weeks of gestation, and they performed intrauterine levothyroxine treatment. As a result of 400 mcg levothyroxine single-dose injection, the size of thyroid was found as 4.8×12.5 cm at the end of 4 weeks and the treatment was considered as sufficient.[18] The treatment dose estimation recommended by Abuhamad et al. is to do intraamniotic levothyroxine injection with the dose of 10 mcg/kg according to the birth weight.[17] However, as a result of different treatments and case reports later, Ribault et al. evaluated the treatments of 18 compiled cases. For 1–4 weeks, they made 1–7 injections and found that there was 70–800 mcg dose difference in each application and 3–23 mc/kg difference in each protocol. Also, fetal hormonal analysis was performed through amniotic fluid in some cases while it was done through cord blood in some other cases. In the conclusion section of that study, the authors reported that there has been no certain consensus on the treatment of fetal hypothyroidism.[16] In their recent case report, Khamisi et al. found maternal hormones within normal ranges and fetal TSH as >100 mU/l in pregnant women with fetal goiter at 18 weeks of gestation, and they administered intraamniotic thyroxine for 9 times at intervals of 7–10 days between 24 and 33 weeks of gestation. They administered 10 mcg/kg in the first 6 applications, and 5 mcg/kg in the last 3 applications. Fetal development was normal; however, the delivery was made by cesarean at 34 weeks of gestation due to the suspicion of chorioamnionitis. Since TSH was higher than 596 mU/L (reference values: 8.0±5.12) in the cord blood during delivery, thyroxine treatment was initiated just after the delivery. In the conclusion section of the investigation, it was indicated that new investigations are required for intraamniotic thyroxine treatment.[2] Conclusion As a conclusion, ultrasound and Doppler examinations, diagnosing and following up fetal goiter are of vital 68 Perinatal Journal importance. Fetal hypothyroidism is a negative pathology for the development of central nervous system and physical and mental development. Fetal goiter which is not present in the ultrasound during the early periods but becomes evident in the advanced weeks of gestation should not be overlooked. Mental retardation and other development disorders can be prevented by early diagnosis and treatment. Therefore, we believe that it will be useful to remember fetal goiter in the ultrasonographic screenings even during advanced weeks of gestation. Conflicts of Interest: No conflicts declared. References 1. Singh PK, Parwin CA, Gronowski AM. Establishment of reference intervals for markers of fetal thyroid status in amniotic fluid. J Clin Endocrinol Metab 2003;88:4175–9. 2. Khamisi S, Lindgren P, Karlssson FA. A rare case of dyshormonogenetic fetal goiter responding to intra-amniotic thyroxine injections. Eur Thyroid J 2014;3:51–6. 3. Perrotin F, Sembely-Taveau C, Haddad G, Lyonnais C, Lansac J, Body G. Prenatal diagnosis and early in utero management of fetal dyshormonogenetic goiter. Eur J Obstet Gynecol Reprod Biol 2001;94:309–14. 4. Weiner S, Scharf JI, Bolognese RJ, Librizzi RJ. Antenatal diagnosis and treatment of a fetal goiter. J Reprod Med 1980; 24:39–42. 5. Davidson KM, Richards DS, Schatz DA, Fisher DA. Successful in utero treatment of fetal goiter and hypothyroidism. N Engl J Med 1991;324:543–6. 6. Paula JW, Anne K, Roya S, Janice LB, Karen YO, Michael DP. Face and neck anomalies – Goiter. Diagnostic imaging obstetrics. 2nd edition. Utah Amirsys 2013. p: 4/54–5. 7. Delange F. Neonatal screening for congenital hypothyroidism: results and perspectives. Horm Res 1997;48:51–61. 8. Fisher DA. Fetal thyroid function: diagnosis and management of fetal thyroid disorders. Clin Obstet Gynecol 1997; 40:16–31. 9. Meideros-Neto GA, Stanbury JB. Inherited Disorders of the Thyroid System. Boca Raton: CRC Pres; 1994; p: 1–218. 10. Morine M, Takeda T, Minekawa R, Sugiyama T, Wasada K, Mizutani T, et al. Antenatal diagnosis and treatment of a case of fetal goitrous hypothyroidism associated with high-output cardiac failure. Ultrasound Obstet Gynecol 2002;19:506–9. 11. Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. Tiroid ve di¤er endokrin bozukluklar. Williams Obstetrik. 23. bask›. Istanbul: Nobel T›p Kitapevi; 2010. p. 1128–35. 12. Mestman JR. Tyroid and parathyroid diseases in pregnancy. In: Gabbe SG, Niebly JR, Simpson JL, editors. Obstetrics: normal and problem pregnancies. 5th edition. London: Churchill Livingstone; 2007. p.1023–9. 13. Merz E. Obstetrik ve jinekolojide ultrason. Çeviri: Özden S. 2. bask›. Cilt 1. ‹stanbul: Do¤an T›p Kitapevi; 2002. p. 247–52. Goiter in fetus without maternal thyroid disease 14. Bruner JP, Dellinger EH. Antenatal diagnosis and treatment of fetal hypothyroidism. A report of two cases. Fetal Diagn Ther 1997;12:200–4. 15. Simsek M, Mendilcioglu I, Mihci E, Karagüzel G, Taskin O. Prenatal diagnosis and early treatment of fetal goitrous hypothyroidism and treatment results with two-year followup. J Matern Fetal Neonatal Med 2007;20:263–5. 16. Ribault V, Castanet M, Bertrand AM, Guibourdenche J, Vuillard E, Luton D, et al.; French Fetal Goiter Study Group. Experience with intraamniotic thyroxine treatment in nonimmune fetal goitrous hypothyroidism in 12 cases. J Clin Endocrinol Metab 2009;94:3731–9. 17. Abuhamad AZ, Fisher DA, Warsof SL, Slotnick RN, Pyle PG, Wu SY, et al. Antenatal diagnosis and treatment of fetal goitrous hypothyroidism: case report and review of the literature. Ultrasound Obstet Gynecol 1995;6:368–71. 18. Medeiros-Neto G, Bunduki V, Tomimori E, Gomes S, Knobel M, Martin RT, et al. Prenatal diagnosis and treatment of dyshormonogenetic fetal goiter due to defective thyroglobulin synthesis. J Clin Endocrinol Metab 1997;82:4239–42. Volume 23 | Issue 1 | April 2015 69 AL JO U R AL PE R AT N IN Letter to the Editor L Perinatal Journal 2015;23(1):70–71 R N A PE IN AT U AL JO R Letter to the Editor regarding “Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case” Baflak Kaya, Ali Gedikbafl› Perinatology Unit, Gynecology & Obstetrics Clinic, Kanuni Sultan Süleyman Training and Research Hospital, Istanbul, Turkey This letter has been written for the aspects to criticize for the EXIT procedure in the case report of unilateral advanced fetal hydrothorax case published in Perinatal Journal.[1] Although various treatment and management recommendations and studies have been provided for fetal hydrothorax in the literature, better results are obtained by using improved fetal treatment methods. If hydrothorax develops before 27 weeks of gestation, pulmonary development is affected and cardiac failure and intrauterine loss may occur associated with cardiac and central vein pressure.[2] Besides, isolated fetal hydrothorax developing at late second trimester and third trimester may not cause hypoplasia.[3] Poor prognostic factors are bilateral effusion development, nonregression of effusion spontaneously, hydrops and prematurity.[4] The type of treatment during prenatal period is determined primarily according yo the severity of effusion and diagnosis week of gestation. Conservative management may be preferred since spontaneous regression may develop in the presence of mild-mid unilateral pleural effusion not causing mediastinal shift and hydrops and not accompanied by polyhydramnios.[5,6] If rapid increase in effusion, hydrops or polyhydramnios development is observed during the follow-up, invasive fetal treatment should be performed by using thoracoamniotic shunt. When thoracoamniotic shunt procedure is significant especially before 36 weeks of gestation, thoracentesis or thoracoamniotic shunt can be preferred in further weeks of gestation. Thoracoamniotic shunt should be preferred primarily in the presence of severe pleural effusion where mediastinal shift is accompanied by hydrops or polyhydramnios.[5,7,8] Direct shunt application should also be considered in hydropic fetuses with bilateral effusion.[9] Nicolaides and Azar reached 50% survival rate in hydrothorax cases with non-immune hydrops by applying thoracoamniotic shunt.[10] Decompression of effusion fluid by thoracentesis allows normal pulmonary development to continue, also may fix hydrops and polyhydramnios.[11] It also helps to diagnose for the etiology of hyrops and pleural effusion.[6,12] However, since fluid is accumulated rapidly in 24–48 hours in the most of the cases, thoracoamniotic shunt should be preferred especially in the cases detected in the early second trimester.[8,13] On the other hand, while some authors prefer thoracentesis in the initial treatment, they apply thoracoamniotic shunt in case of reaccumulation of pleural effusion.[13] It may not be always possible to apply thoracoamniotic shunt due to the inappropriate fetal position and increased fetal skin edema. Transplacental application during the procedure is not preferred for thoracoamniotic shunt.[6] In such cases where thoracoamniotic shunt cannot be applied, multiple thoracentesis, conservative follow-up of hydropic fetus or early labor of fetus are other possible treatment options.[13] Since prematurity is a poor prognostic factor affecting survival, it is recommended to carry out the delivery Correspondence: Ali Gedikbafl›, MD. Kanuni Sultan Süleyman E¤itim ve Araflt›rma Hast., Kad›n Hastal›klar› ve Do¤um Klini¤i, ‹stanbul, Turkey. e-mail: ali.gedikbasi@kssh.gov.tr Received: February 24, 2015; Accepted: February 24, 2015 Please cite this article as: Kaya B, Gedikbafl› A. Letter to the Editor regarding “Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case”. Perinatal Journal 2015;23(1):70–71. ©2015 Perinatal Medicine Foundation Available online at: www.perinataljournal.com/20150231014 doi:10.2399/prn.15.0231014 QR (Quick Response) Code: Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case in tertiary centers at 37-38 weeks of gestation.[5] It is reported that draining mid-severe pleural effusion just before the delivery helps neonatal resuscitation and ventilation support.[5,6] However, Klam et al. found no difference between those applied thoracentesis just before the delivery and postpartum practices in terms of Apgar score, entubation and ventilation requirements and survival rates.[8] References In the case presented, it is seen that thoracentesis was applied to investigate the etiology of pleural effusion at 36 weeks of gestation and to treat the case. In this case, in the presence of appropriate fetal position, thoracoamniotic shunt treatment could be planned if transplacental transition was not required technically. 3. Gül A, Aslan H, Cebeci A, Polat ‹, Agral› G, Ceylan Y. Primary fetal hydrothorax: successful perinatal outcomes with single thoracentesis just prior to delivery. J Turk Ger Gynecol Assoc 2004;5:143–6. Extrauterine intrapartum treatment (EXIT) can be useful in cases which are near term or at term with severe pleural effusion where intrauterine drainage failed. Prontera et al. who defined EXIT procedure for the first time due to fetal hydrothorax carried out this procedure in a case which had bilateral severe pleural effusion, increased central venous pressure findings, cardiac diastolic function disorder and with lungs completely collapsed and echogenic. Fetal thoracentesis could not be applied due to polyhydramnios and fetal position, and postnatal drainage was not preferred due to the presence of bilateral and severe pleural effusion and the concern of postnatal long and severe hypoxia. Therefore, thoracentesis and EXIT procedure were preferred as the least complicated methods.[2] When patients who were applied EXIT procedure and other cases delivered by cesarean section were compared in terms of maternal complications, wound site complications and estimated blood loss were more in cases who were applied EXIT procedure.[14] As congenital fetal hydrothorax is a rare clinical condition with limited number of case reports in the literature, there are disputes about the treatment options and most suitable delivery time. First of all, it is required to refer such cases to tertiary centers and to plan treatment and delivery in such centers. The treatment should be planned according to the characteristics and clinical condition of current case, the experience of the team which will carry out invasive procedure, and the suitability of technical conditions. Conflicts of Interest: No conflicts declared. 1. Eraslan S, Meleko¤lu R, Çelik E. Tek tarafl› ileri derecede fetal hidrotoraks olgusunda ekstrauterin intrapartum tedavi prosedürü. Perinatoloji Dergisi 2015;23:60–4. 2. Prontera W, Jaeggi ET, Pfizenmaier M, Tassaux D, Pfister RE. Ex utero intrapartum treatment (EXIT) of severe fetal hydrothorax. Arch Dis Child Fetal Neonatal Ed 2002;86: F58–60. 4. Aubard Y, Derouineau I, Aubard V, Chalifour V, Preux PM. Primary fetal hydrothorax: a literature review and proposed antenatal clinical strategy. Fetal Diagn Ther 1998;13: 325–33. 5. Yinon Y, Kelly E, Ryan G. Fetal pleural effusions. Best Pract Res Clin Obstet Gynaecol 2008;22:77–96. 6. Petersen S, Kaur R, Thomas JT, Cincotta R, Gardener G. The outcome of isolated primary fetal hydrothorax: a 10year review from a tertiary center. Fetal Diagn Ther 2013;34:69–76. 7. Pellegrinelli JM, Kohler A, Kohler M, Weingertner AS, Favre R. Prenatal management and thoracoamniotic shunting in primary fetal pleural effusions: a single centre experience. Prenat Diagn 2012;32:467–71. 8. Klam S, Bigras JL, Hudon L. Predicting outcome in primary fetal hydrothorax. Fetal Diagn Ther 2005;20:366–70. 9. Derderian SC, Trivedi S, Farrrell J, Keller RL, Rand L, Goldstein R, et al. Outcomes of fetal intervention for primary hydrothorax. J Pediatr Surg 2014;49:900–3. 10. Nicolaides KH, Azar GB. Thoraco-amniotic shunting. Fetal Diagn Ther 1990;5:153–64. 11. Cardwell MS. Aspiration of fetal pleural effusions or ascites may improve neonatal resuscitation. South Med J 1996;89: 177–8. 12. Smith RP, Illanes S, Denbow ML, Soothill PW. Outcome of fetal pleural effusions treated by thoracoamniotic shunting. Ultrasound Obstet Gynecol 2005;26:63–6. 13. Deurloo KL, Devlieger R, Lopriore E, Klumper FJ, Oepkes D. Isolated fetal hydrothorax with hydrops: a systematic review of prenatal treatment options. Prenat Diagn 2007;27: 893–9. 14. Noah MM, Norton ME, Sandberg P, Esakoff T, Farrell J, Albanese CT. Short-term maternal outcomes that are associated with the EXIT procedure, as compared with cesarean delivery. Am J Obstet Gynecol 2002;186:773–7. Volume 23 | Issue 1 | April 2015 71 AL JO U R A PE R AT N IN L L R N A PE IN AT U AL JO R www.perinataljournal.com The Official Publication of Perinatal Medicine Foundation, Turkish Perinatology Society and Turkish Society of Ultrasound in Obstetrics and Gynecology Publication Ethics and Malpractice Statement Perinatal Journal is committed to upholding the highest standards of publication ethics and observes the following principles of Publication Ethics and Malpractice Statement which is based on the recommendations and guidelines for journal editors developed by the Committee on Publication Ethics (COPE), Council of Science Editors (CSE), World Association of Medical Editors (WAME) and International Committee of Medical Journal Editors (ICMJE). All submissions must be original, unpublished (including as full text in conference proceedings), and not under the review of any other publication synchronously. Each manuscript is reviewed by one of the editors and at least two referees under double-blind peer review process. We reserve the right to use plagiarism detecting software to screen submitted papers at all times. We check for plagiary and fraudulent data; falsification (fabrication or manipulation of research data, tables, or images) and improper use of humans or animals in research. All manuscripts not in accordance with these standards will be removed from the publication. This also contains any possible malpractice discovered after the publication. In accordance with the code of conduct we will report any cases of suspected plagiarism or duplicate publishing. We follow the COPE Ethics Flowcharts for dealing with cases of possible scientific misconduct and breach of publication ethics. Author Responsibilities Authors should ensure that submitted work is original. They must certify that the manuscript has not previously been published elsewhere or is not currently being considered for publication elsewhere, in any language. Applicable copyright laws and conventions should be followed. Copyright material (e.g. tables, figures or extensive quotations) should be reproduced only with appropriate permission and acknowledgement. Any work or words of other authors, contributors, or sources should be appropriately credited and referenced. The author(s) of the original research articles (including short communications) must declare that they were involved in at least 3 of the 5 stages of the study as "designing the study", "collecting the data", "analyzing the data", "writing the manuscript" and "confirming the accuracy of the data and the analyses". All authors should disclose all issues concerning financial relationship, conflict of interest, and competing interest that may potentially influence the results of the research or scientific judgment. All financial contributions, supports or sponsorship of projects should be clearly explained. When an author discovers a significant error or inaccuracy in his/her own published paper, it is the author's obligation to promptly cooperate with the Editor-in-Chief to provide retractions or corrections of mistakes. Responsibility for the Reviewers Reviewers evaluate manuscripts based on content without regard to ethnic origin, gender, sexual orientation, citizenship, religious belief or political philosophy of the authors. They should have no conflict of interest with respect to the research, the authors and/or the research funders. Their judgments should be objective. Reviewers should identify relevant published work that has not been cited by the authors. They must ensure that all the information related to submitted manuscripts is kept as confidential and must report to the Editor-in-Chief if they are aware of copyright infringement and plagiarism on the author's side. A reviewer who feels unqualified to review the topic of a manuscript or knows that its prompt review will be impossible should notify the Editor-in-Chief and excuse himself from the review process. Editorial Responsibilities Editors evaluate manuscripts for their scientific content without regard to ethnic origin, gender, sexual orientation, citizenship, religious belief or political philosophy of the authors. They provide a fair double-blind peer review of the submitted articles for publication. They ensure that all the information related to submitted manuscripts is kept as confidential before publishing. Editors are responsible for the contents and overall quality of the publication. They should publish errata pages or make corrections when needed. Editor-in-Chief does not allow any conflicts of interest between the authors, editors and reviewers. Only he has the full authority to assign a reviewer and is responsible for final decision for publication of the manuscripts in Perinatal Journal. PERINATAL JOURNAL Volume 23 | Issue 1 | April 2015 C o n te n ts Original Article Case Reports Letter to Editor Ultrasonographic evaluation of ventriculomegaly cases Hakan Kalayc›, Halis Özdemir, Ça¤r› Gülümser, Ayfle Parlakgümüfl, Tayfun Çok, Ebru Tar›m, Filiz Bilgin Yan›k 1 Perinatal outcomes of patients diagnosed borderline gestational diabetes mellitus Gök Özgül, Rauf Meleko¤lu, Sevda Yeleç, ‹pek Eskiyörük, Fatma Tuncay Özgünen 6 Health practices of pregnant women in Gumushane City Center Handan Özcan, Nezihe K›z›lkaya Beji 13 The evaluation of pregnancies complicated by eclampsia: retrospective analysis of 37 cases in our clinic Aytekin Tokmak, Korkut Da¤lar, Ali ‹rfan Güzel, Bergen Laleli, Salim Erkaya, Dilek Uygur 20 Factors affecting postpartum depression in Diyarbak›r Ali Emre Tahao¤lu, Cihan To¤rul, Mehmet ‹rfan Külahç›o¤lu, Beflire Ayd›n Öztürk, Deniz Balsak, Hanifi Bademk›ran, Erdo¤an Gül, Ümit Görkem, Tayfun Güngör 26 Analysis of maternal serum and urinary lipocalin-2 levels Yeflim Bayo¤lu Tekin, Ülkü Mete Ural, Aynur K›rbafl, fienol fientürk, Figen K›r fiahin 30 Critical pulmonary stenosis with prenatal diagnosis: a case series and review of literature Oya Demirci, Taner Yavuz, Resul Ar›soy, Emre Erdo¤du, P›nar Kumru, Oya Pekin 34 Evaluation of prenatal invasive procedures: analysis of retrospective cases Aybike Tazegül Pekin, Özlem Seçilmifl Kerimo¤lu, Setenay Arzu Y›lmaz, Nadir Koçak, Feyza Nur ‹ncesu, Ayfle Gül Kebapc›lar, Çetin Çelik 39 Investigation of the effects of fetal gender on umbilical artery and middle cerebral artery Doppler findings Burcu Artunç Ülkümen, Halil Gürsoy Pala, Y›ld›z Uyar, Yeflim Baytur, Faik Mümtaz Koyuncu 45 Results of routine first trimester screening tests and following invasive procedures during pregnancy Rahime Nida Ergin, Murat Yayla 50 The association of congenital hand reduction defect and uterine anomaly Bülent Kars, Önder Sakin, Yasemin Karageyim Karfl›da¤, Cenk Demir, Esra Esim Büyükbayrak 56 Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case Sevil Eraslan, Rauf Meleko¤lu, Ebru Çelik 60 Goiter in fetus without maternal thyroid disease: a case report Önder Sakin, Bülent Kars, Yasemin Karageyim Karfl›da¤, Cenk Demir, Esra Esim Büyükbayrak 65 Letter to the Editor regarding “Extrauterine intrapartum treatment procedure in the unilateral advanced fetal hydrothorax case” Baflak Kaya, Ali Gedikbafl› 70