Residential Provider Expansion into Home and Community
advertisement

Residential Provider Expansion into Home and Community-Based Services TABLE OF CONTENTS Executive Summary 2 Introduction5 Nursing Homes Alterszentrum Viktoria, Switzerland 13 Feros Care, Australia 19 Isabella Geriatric Care, United States 31 Tabitha Health Care, United States 42 Continuing Care Retirement Communities BallyCara, Australia 51 First Choice, United States 60 Shepherd’s Care Foundation, Canada 67 Well-Spring Continuing Care Retirement Community, United States 77 Continuing Care at Home Programs Cadbury Senior Living, United States 87 Conclusion96 EXECUTIVE SUMMARY A growing number of not-for-profit, residential providers of aging services are developing new business lines in the area of home and community-based services (HCBS). These services include home health care, non-medical home care and adult day care. Few studies have examined the HCBS expansion process to identify successful business models and marketing strategies, or common challenges and lessons learned. With so many residential providers entering the field of home and communitybased services, an elucidation of common themes, important lessons and promising practices would greatly benefit the sector. The Study The International Association of Homes and Services for the Ageing sought to fill this evidence gap by conducting a qualitative study of not-for-profit residential service providers that expanded to provide home and community-based services. Researchers used the case study method, combined with an analysis of emergent themes, to conduct this study. They sought to include a diverse set of providers in the study in an effort to identify emerging themes that transcended the differences among providers of aging services. This method helped researchers identify useful guidance that would apply to the array of organizations in the sector. The research team conducted structured phone interviews with two representatives of each organization, usually the chief executive officer and the vice president or director of the home and community-based services program. The purpose of the interviews was to understand the: Program Relevant policy context Financial implications Workforce Organizational culture 2 | Residential Provider Expansion into Home and Community-Based Services Program outcomes Perceived challenges Perceived benefits Lessons learned The research team also conducted two-day site visits with two organizations. One organization had a longstanding and welldeveloped home and community-based services program and the other was in the early stages of expanding into HCBS. The site visits featured focus groups or telephone interviews with: Home health and home care aides Other frontline staff Supervisors of frontline staff Additional executives Marketing, human resources and quality-assurance staff The site visits allowed the research team to enrich the perspectives developed during the phone interviews and to focus more deeply on certain areas, including successful strategies for staffing the new business lines and the financial implications of the expansion. Researchers wrote case studies describing each participating provider. They also identified common themes that emerged across these diverse organizations. An evaluation of the themes led to the identification of guidelines that might be useful to providers that are considering an expansion into home and community-based services, or are in the early stages of such an expansion. Each case study, as well as a discussion of the emerging themes and lessons, is included in this report. The Organizations The research team completed case studies of five U.S. providers, one Canadian provider, two Australian providers and one European provider. EXECUTIVE SUMMARY Nursing Homes Four organizations included in the study began as nursing homes: Alterszentrum Viktoria (Bern, Switzerland): Beginning as a nursing home in 1995, Alterszentrum Viktoria began providing home health care and limited non-medical home care to members of the external community in 2011. The organization’s small program currently serves 23 clients. Its predominant source of reimbursement is mandated insurance. Feros Care (Queensland, Australia): Established as an operator of two nursing homes in the early 1990s, Feros Care expanded into home and community-based services in 20022003 and now delivers home health care, home care, telehealth, companionship, and other services to approximately 5,000 clients per year. The Australian government’s Home Care Packages Program comprises its main source of reimbursement for home health and home care. Isabella Geriatric Center (New York, USA): Founded as a nursing home in 1875, the non-sectarian Isabella Geriatric began expanding into home and community-based services in 1989. The organization now provides more than one million service hours per year of home health care, home care, adult day and other services. Isabella serves mainly low-income clients. Its primary payer source for home health care is Medicaid. Tabitha Health Care (Nebraska, USA): Established as an orphanage in 1886 and a nursing home in 1890, faith-based Tabitha began providing home health care in 1966 and home care in 1974. Each month, the organization delivers more than 10,000 service hours of home care and serves an average of 254 home health clients. Tabitha’s main source of reimbursement for home health care is Medicare. Most of its home care services are private pay. Continuing Care Retirement Communities Four organizations included in the study began as continuing care retirement communities (CCRCs) or a CCRC-like entity, and developed traditional home and community-based services programs. They include: BallyCara Village of Friends (Queensland, Australia): BallyCara began in 1983 as a residential provider offering successively higher levels of care, from independent living to a nursing home. The organization expanded to home and community-based services in 2013 and now provides an average of 458 service hours to 200 external clients per month. BallyCara’s funding sources are a mix of government-funded and private pay. First Choice (Virginia, USA): Founded by two faith-based CCRCs in 2007, with a third partner joining the partnership in 2015, First Choice now provides more than 4,000 service hours of home care per month and serves 65-70 home health clients per day. First Choice was established through a partnership among three providers that acquired an existing agency with a client base. The agency’s primary funding sources are Medicare, private insurance and private pay. Shepherd’s Care Foundation (Alberta, Canada): Beginning as a CCRC 45 years ago, faith-based Shepherd’s Care began providing companionship, transportation services and other home care services in September 2014. Older adults living in the organization’s residential communities make up the majority of home care clients. Shepherd’s Care structured its home and community-based service lines within a separate, for-profit corporate entity that now provides more than 1,500 service hours per month to approximately 40 clients. Its main sources of reimbursement are currently private pay and government contracts. Sodexo • IAHSA • LeadingAge | 3 EXECUTIVE SUMMARY Well-Spring (North Carolina, USA): In addition to operating a CCRC, Well-Spring provides home care and adult day services to the external community. Each month, the organization delivers more than 10,000 hours of home care, approximately 1,000 of which are delivered outside the CCRC. Well-Spring’s adult day program serves approximately 200 clients each month. The organization’s primary source of reimbursement for home care is private pay. The adult day program has multiple funding sources. Continuing Care at Home One organization included in the study began as a CCRC and provides home and community-based services through a “continuing care without walls” or “continuing care at home” program. Cadbury at Home (New Jersey, USA): Founded as a CCRC, Cadbury established a continuing care at home program in 1998. The program provides a full range of services to its 200 members. Those services include home health care and non-medical home care. The organization’s primary source of reimbursement is private pay. The expansion timeline for organizations in this study ranges from more than 25 years (Tabitha Health Care and Isabella Geriatric Center) to under one year (Shepherd’s Care Foundation). This range of experience with home and community-based services allowed researchers to glean insights from individuals whose programs had a long track record of success, and from individuals whose programs are currently in the planning and early-implementation stages. Common Themes: Highlights An analysis of interview transcripts, notes and case studies revealed several common themes among the organizations regarding their experiences with the expansion process. Some highlights of these themes are described below. Reasons for expanding: When asked why they expanded into home and community-based services, most organizations cited a desire to fulfill their mission by serving more community members, as well as a desire to grow their roster of services in order to provide a continuum of care. Some providers said they hoped to become a “one-stop shop” that community-dwelling older adults and their adult children would turn to for all of their aging services needs. Additionally, some organizations said they were seeking additional revenue streams to support their residential businesses. Staffing: All organizations in the sample primarily hired new frontline staff for their home and community-based service lines, rather than redeploying frontline residential staff. Organizations took this approach because the type of worker who thrives in the home care environment tends to differ from the type of worker who thrives in a residential setting. The organizations often shared back-end support systems with the residential services division. 4 | Residential Provider Expansion into Home and Community-Based Services Funding: Several organizations said they were seeking the best balance between government and private funding. Home and community-based service lines drew on private-pay clients and had the potential to provide surplus revenue. Challenges: Most providers said they faced tough competition and found it difficult, at least at first, to distinguish themselves from their competitors. Some organizations also cited the difficulty of maintaining communication with the workforce during the expansion process, especially regarding the organization’s brand and high standards. Benefits: Several providers noted that their home and community-based service lines provided their organizations with referrals to on-campus services. Most providers said they derived pleasure from fulfilling their organization’s mission. Organizations also reaped financial benefits from the expansion into home and community-based services. Lessons Learned and Promising Practices: Highlights Many of the lessons providers said they learned during the expansion process concerned marketing. Several providers emphasized the need to conduct in-depth market analysis before expanding into home and community-based services. Providers emphasized the importance of understanding the needs and desires of the target community before designing the HCBS business model. Providers should consider how to distinguish their service lines from the competition, according to study participants. Several providers also noted that marketing strategies that are successful for home and community-based services differ from successful marketing practices for residential services. HCBS marketing tends to be referral-based while residential care marketing tends to depend on word-of-mouth. It is important to understand these differences in advance. Prior to launching a home and community-based service program, it is important to develop a network that fosters relationships with referral sources. Providers also should develop a business strategy that aligns with the realities of the market. Several providers noted the importance of educating staff members, residents, boards of directors and consumers about the value of HCBS programs. Finding the “right” workers for the home setting is critical to the success of HCBS programs. Providers emphasized the importance of developing and supporting staff. Workers should be empowered to identify client needs and provide services to meet those needs. Study participants discussed their strategies for expanding to new services lines and geographical areas. Providers might consider using contract staff and then hiring their own staff, they suggest. Virtual offices can also enable organizations to operate multiple satellite offices with minimal infrastructure. INTRODUCTION The International Association of Homes and Services for the Ageing (IAHSA) and LeadingAge collaborated on a project to examine why and how aging service providers transition from a residential setting model into a home and community-based services (HCBS) model, and to examine the operations of the programs. Sodexo Institute for Quality of Daily Life, a research partner of IAHSA, funded the project. The research team performed a qualitative study of notfor-profit residential providers. As part of this effort, the team conducted 90- to 120-minute telephone interviews with nine provider organizations in the United States, Canada, Switzerland and Australia. The interviews typically were conducted with the organization’s president/chief executive officer and the vice president or director of the HCBS program. These interviews covered the following topics: Reason for expanding into home and community-based services History and description of the current program Relevant policy context Financial implications of the HCBS program Workforce Organizational culture Program outcomes Perceived challenges Perceived benefits Lessons learned through the experience The research team also conducted two-day site visits to two organizations: one organization in the United States had a longstanding and well-developed HCBS program, and one organization in Canada was in the early stages of expanding into home and community-based services. During each site visit, the research team held focus groups with agency aides who directly provided care, other frontline staff,1 and supervisors of frontline staff. The site visits also included structured interviews with additional executives, including the chief operating officer at one site and the chief financial officer at the other; and the directors of marketing, human resources and quality assurance. Researchers sought to gain an in-depth understanding of the programs’ implementation, operations and impact. Researchers wrote case studies describing each participating provider, and then analyzed all transcripts and notes to identify common themes that emerged across these diverse organizations. An evaluation of these themes led to the identification of guidelines that might be useful to providers that are considering an expansion into home and communitybased services, or are in the early stages of such an expansion. Each case study, as well as a discussion of the emerging themes and lessons, is included in this report. Any errors in the study report are the responsibility of the authors. Background Aging services providers are reinventing themselves by offering home and community-based services to on-campus residents and older adults living in the external community. These organizations offer programs and services that reach beyond the traditional, residential setting to meet consumer demands and the economic realities of people who are aging in their own homes. Demand for services like in-home care and adult day is booming in many countries. Providers’ reasons for expansion are varied and numerous, including meeting consumer demands to age in place, reaching a greater percentage of the older adult population, seeking new revenue streams in the face of low occupancy rates, diversifying payer services, and enhancing the organization’s brand. Home and community-based services can be delivered to a consumer at home or in a campus-based supportive living or independent living setting. Operators have a variety of options Sodexo • IAHSA • LeadingAge | 5 as they design an HCBS program. These programs can include, but are not limited to: Private duty (non-medical) home care: This service provides assistance with activities of daily living or instrumental activities of daily living, companionship services, or specialized care. A non-licensed caregiver usually provides the care. In some cases, a certified aide provides care. Home health care: This type of intermittent skilled care requires more expertise than private duty care and more regulatory oversight. Continuing Care at Home: This package of long-term services and supports is provided to adults who want the security that a retirement community offers but want to remain at home. This HCBS program differs from the traditional home and community-based programs that CCRCs deliver in the community. A continuing care at home program takes the concept of the life care contract and a bundle of services into the home. Continuing care at home is not just a menu of services that consumers purchase on an as-needed basis. Rather, it is a comprehensive approach to providing a health and wellness lifestyle to older adults in their homes. Aging service providers follow different models when designing the structure of their HCBS program. That program can be a department within the retirement community, a separate agency, or an affiliate of the retirement community. The organization might also choose to provide home and community-based services through multiple partners. Government or private-pay reimbursement for different services varies widely by region and by case. Participating Providers The research team completed case studies of four U.S. providers, one Canadian provider, two Australian providers and one Swiss provider. A fifth U.S. provider also participated in the study, even though the organization does not offer a 6 | Residential Provider Expansion into Home and Community-Based Services traditional HCBS program. The provider delivers continuing care at home, an emerging model that is described on page 87. A brief description of each provider is presented below. More detailed descriptions can be found in the individual case studies. The organizations participating in this study differed in a number of ways, including: Nature of initial residential services Design of the current HCBS line Size of the workforce Number of clients served Number of years since the initial expansion Location Primary payer sources Policy contexts and regulatory challenges encountered Nursing Homes Four organizations included in the study began as nursing homes. Alterszentrum Viktoria in Berne, Switzerland was established as a nursing home in 1995. It expanded to offer home and community-based services to external clients in 2011. Viktoria provides primarily home health (medical) care and limited non-medical care to 23 clients in the community. Its predominant source of reimbursement is government-mandated insurance. The organization started a new program that is housed within the parent organization. Feros Care in Queensland, Australia is a standalone organization that provides assisted or supportive living care and nursing home care. Feros Care expanded into home and community-based services in 2002-2003 and now delivers personal care, home care, social care, allied health care, wellness services and an extensive range of telehealth services to 5,000 clients each year. Its main source of reimbursement for home health and home care is the Australian government’s Home Care Packages Program. The HCBS program delivers services through a combination of new programs and strategic partnerships. The program is housed within the parent organization and has 245 service partners. INTRODUCTION Isabella Geriatric Care in New York, United States is a nonsectarian organization that has provided care for older adults since 1875. Founded as a traditional nursing home, Isabella now provides a continuum of services, including nursing home care, moderately priced senior housing, adult day health care, child day care, home care, certified home health care, licensed home health care, short- and long-term rehabilitation, Naturally Occurring Retirement Community (NORC) services,2 community-based care coordination, and other community programs designed to help older adults remain healthy and independent at home. Isabella began offering home and community-based services in 1989. It delivers more than one million service hours per year. Its primary payer sources are Medicaid and managed care. Isabella started its own programs, which are now part of overall organization. Tabitha Health Care in Nebraska, United States started as a nursing home in 1890. It has since expanded to offer older adults a comprehensive line of services, including three nursing homes for rehabilitation and long-term care, assisted living, affordable senior housing, and a variety of home and community-based services. These services include home health care, nonmedical home care, adult day services, Meals on Wheels, and personalized services. Each month, Tabitha provides more than 10,000 home care service hours and serves an average of 254 home health clients. Its main source of reimbursement for home health care is Medicare. Its main source of reimbursement for private duty is private pay. Tabitha started a new program, which is now part of the parent organization. Continuing Care Retirement Communities Four organizations included in the study began as continuing care retirement communities (CCRCs)3 or a CCRC-like entity, and developed traditional home and community-based service programs. BallyCara Village of Friends in Queensland, Australia is a residential provider offering progressively higher levels of care, including independent living, assisted living and nursing home care. BallyCara established its first home and communitybased services program in October 2013. The organization provides external clients with private duty care that includes domestic assistance, home maintenance, transportation and social support. BallyCara Community Care serves approximately 200 clients across all its home care service lines and averages 428 service hours each month. Its main funding sources are government funding for home care, private pay and government-allocated Home Care Packages, which it currently delivers in partnership with other providers that have been allocated funding by the Australian government. The HCBS programs, which feature a combination of new programs and strategic partnerships, are housed within the parent organization. First Choice in Virginia, United States is a home health and home care agency jointly owned by three retirement communities: Virginia Mennonite Retirement Community (VMRC), Bridgewater Retirement Community and Sunnyside Communities. VMRC and Bridgewater jointly purchased First Choice in 2007. Sunnyside Communities joined the partnership in 2015. First Choice provides home health and home care services to people living on retirement community campuses and in their own homes. The agency serves 65 to 70 home health clients each day and provides 4,000 hours of home care services each month. Its primary funding sources are Medicare, private insurance and private pay. Shepherd’s Care Foundation in Alberta, Canada was founded in 1970 and is a faith-based retirement community offering independent living, supportive living and nursing home care on its campus. The organization serves more than 1,600 older adults who have low to moderate incomes. Shepherd’s Care Foundation extended its service lines into home care in October 2014 and offers transportation and companionship services. The agency delivers 1,500 service hours each month. Shepherd’s Care at Home, a for-profit agency, is independent and separate from Shepherd’s Care Foundation. Its main sources of reimbursement are private pay and government contracts. Well-Spring Retirement Community in North Carolina, United States was established in 1993 by a coalition of nine local churches. Well-Spring offers several different types of home and community-based programs: the Program of All Inclusive Care for the Elderly4, adult day care, and home care. The organization acquired an existing adult day provider and started a new home care program. The adult day and home care services have since combined and are under the umbrella of Well-Spring. Well-Spring delivers more than 10,000 hours of home care per month, of which 1,000 are supplied outside the Well-Spring CCRC. The adult day program serves approximately 200 clients each month. The primary source of reimbursement for home care is private pay. The adult day program relies on a variety of funding sources. Continuing Care at Home One organization included in the study began as a CCRC and provides home and community-based services through a continuing care at home program. Cadbury Senior Living in New Jersey and Delaware, United States launched its Continuing Care at Home program in 1998. Cadbury at Home, one of the first continuing care at home programs in the United States, combines home care, assisted living and nursing home care into a comprehensive program that provides members with long-term services and supports in the home and the opportunity to move onto the CCRC campus as their health care needs change. The program’s primary source of reimbursement is private pay. The at-home program was created by Cadbury and is affiliated with the parent organization. Sodexo • IAHSA • LeadingAge | 7 INTRODUCTION Overview of Providers5 The timeline for expansion into home and community-based services varied considerably for the eight providers with traditional HCBS programs: Over 25 years (Tabitha Home Health and Isabella Geriatric Center) Eight to 10 years (First Choice and Feros Care) Three years or less (Viktoria, Well-Spring and Shepherd’s Care). Cadbury’s continuing care at home program has been in existence almost 20 years. Size of Program Agencies reported the size of their program in different ways: hours per month and number of clients per month or year. Some agencies chose to report the number of service hours instead of number of clients because of clients’ wide range of service needs. For example, some clients only require a few hours of service each month while others require more than 16 hours each day. The agencies felt the service hours provided a more accurate portrayal of their size than the number of clients served. This was particularly true for the private duty care. All four providers who offered both home health and home care had a substantial client base. Their service hours ranged from 4,000 to 10,000 hours each month to one million service hours each year. Two out of the three providers delivering home care only had a smaller client base. One agency averaged 428 service hours each month while another delivered 1,500 service hours per month. One agency delivered 10,000 service hours per month to on-campus residents primarily. That agency delivered approximately 1,000 hours per month to off-campus clients. The remaining home health care agency served approximately 23 clients. Type of Partnership Organizations considered many factors when deciding whether to house the home care/home health agency within the parent corporation or establish it as a separate organization. The factors—including financial, legal, expertise-related, and branding-related issues—will be described more fully later in this Introduction. The majority of the providers have kept the home care/ home health agency as part of the parent organization. One retirement community bought an existing agency to deliver adult day services. This business will reside on the main campus and house all of the organization’s HCBS programs, including home care. While the parent company and the adult day provider have separate boards of directors, they are legally connected with each other. Two home care providers function independently from the parent organization. One home health/home care agency is 8 | Residential Provider Expansion into Home and Community-Based Services The eight agencies with traditional HCBS programs offered a mix of service types: 50 % provided both private duty care and home health care 38 % provided private duty or home care only 1 provided home health care only operated through a joint venture of three provider organizations that purchased the agency. The other provider structured the agency so it would be separate and independent from the parent organization. Reasons for Expansion Residential providers diversified their service lines as a way to fulfill the organization’s mission, reach a larger percentage of the target population, create marketing opportunities and referrals for a retirement community, develop a potential revenue stream, and transform the organization into a “onestop shop.” Several providers cited more than one of these reasons for expanding. Mission: Skilled nursing home providers and aging-in-place providers that offer a tiered approach to the aging process by combining independent living, assisted living and skilled nursing home care may not be able to reach all individuals. In addition, some aging-in-place providers attract wealthier clients and their care is not affordable to low- or modestincome groups. By diversifying service lines, the organization can potentially serve less-affluent clients and reach the most vulnerable individuals in the community. Expanded reach: As more people choose to remain at home, organizations that provide only residential options will be unable to reach a significant portion of the older adult population, including older adults who are unlikely to use oncampus services. Providing services in the community is an opportunity to serve these individuals. Retirement community feeder: When community-dwelling older adults, or their family members, require higher levels of care, they may consider moving to a residential care setting. A home and community-based service line can serve as a feeder into an organization’s other business lines by creating brand awareness and connecting with consumers. When those connections are made early in the aging process, INTRODUCTION individuals and their family/support networks will think of the organization when they need more services. Potential revenue stream: A home and community-based service line can supplement or support revenues from the residential side of a business. The expansion into other services lines also can attract different payer sources. One-stop shop: A provider of aging services can be a “onestop shop” for individuals by providing a full continuum of care, starting with services in a person’s home. The provider can ensure that it helps people no matter where they live or what level of care they need. In addition, campus residents can receive high-quality home and community-based services from a home care/home health agency that is affiliated with or a department within the parent organization. Workforce Organizational environment: A strong workforce is a critical component of any HCBS program. Staff members, particularly the aides who provide direct care, are much more autonomous and work with less supervision than their counterparts in the residential setting. Aides in the home care setting also perform a greater variety of tasks, have more responsibility to make accurate and timely observations, and require flexibility. Aides rarely report to the agency. Instead, they go directly to the client’s home to provide care. It can be challenging for home health and home care agencies to create camaraderie among their employees. These workers have few opportunities to engage and connect with each other. Special events, trainings and meetings can give staff the opportunity to share information and build connections with each other. A few providers occasionally use these events to give staff from the HCBS and residential programs the opportunity to interact with each other. Hiring and orienting staff: Most providers did not staff the HCBS program by redeploying staff from the organization’s residential settings. Instead, they hired new staff with experience in the home setting, including a vice president or director of home and community-based with extensive experience in the type of service lines included in the HCBS program. A few providers held some type of orientation for new staff. This generally included an introduction to the organization. Supervisors in some organizations accompanied new staff members on their first home visit and introduced the aide to the client. One provider recommended using a “buddy system” to allow a new aide to shadow an experienced aide a few times before going out alone. Training sessions: Almost all of the providers who offered additional staff trainings held separate training sessions for residential and home care aides. This decision was based on the fact that home care and residential staff work in very different work environments. Two providers conducted some form of combined trainings. One provider held a joint orientation for aides from both environments and separate in-service trainings. Training sessions often included a mix of mandated education for certified aides as well as additional trainings that exceeded government requirements. Providers typically seek input from aides when deciding on topics for trainings sessions, which often address specific diseases or issues aides encounter while caring for the organization’s clients. Staff resources: Two providers with separate home care/ home health agencies did not share resources or staff with the residential provider. Other providers often called on the organization’s management team to run the daily operations of the HCBS program. The residential and home care businesses frequently shared back-end support functions, including executive management, financial management, human resources, billing, and information technology. This arrangement helped to spread administrative costs over several business lines. Some providers relied on a single marketing team to promote their home-based and residential businesses. Other providers had separate marketing teams because marketing strategies for home-based and residential care are so different. Quality assurance and supervision: The quality of the HCBS programs are monitored in a variety of ways, depending, in part, on the source of funding. Home health care programs were generally required to submit data on specified quality indicators to the government. Some home health and home care providers used their quality improvement committees to review that data and make action plans to improve or change operations based on the findings. Approximately half of the providers elicited feedback from clients and family members to determine their satisfaction with the services. Providers also supervised the aides, although the level of supervision varied and aides and supervisors typically had little interaction. Most providers had a process in place to address clients’ complaints, although some systems were more formal and sophisticated than other systems. Outcomes Few providers conducted formal evaluations of their programs to determine their impact on consumers. Most of the providers that measured outcomes conducted client and family member surveys or solicited feedback to assess satisfaction with provided services. Some providers have established committees or other groups to review satisfaction data and develop action plans to address areas of concern. Organizations that offer home health care through government funding have formal assessments and are measured on select quality indicators. A few providers have initiated efforts to track key measures through dashboards or scorecards. Challenges Providers experienced challenges in launching, operationalizing and sustaining their HCBS programs. The key difficulties reported by providers included: Market competition: Organizations encounter competition from other home care or home health providers serving the same demographic group and geographic area. This can limit the growth potential for agencies. In some regions, providers who rely on government-funded services have found that select entities have a large share of the market because they Sodexo • IAHSA • LeadingAge | 9 INTRODUCTION Organizations encounter competition from other home care or home health providers serving the same demographic group and geographic area. This can limit the growth potential for agencies. are an official government provider or have a longstanding relationship with the government. Providers emphasized the importance of defining a niche for a program and identifying features that distinguish the program from its competitors. Financial: Most HCBS programs operated at a loss, at least during their first year. Growth can be slow due to difficulties associated with growing the program’s client base. Additionally, providers struggled to establish the best balance between private-pay and government-funded services. Clients: Remaining solvent often involves balancing the case mix of clients and their utilization of services. Home health and home care aides reported challenges working with clients who were noncompliant with the services listed on their care plans, were combative or aggressive, or whose family members expected that aides would provide services to them in addition to the client. Regulations: Providers experienced challenges with regulations. A common regulation required organizations to have a certificate of need to enter the market. The certificate of need process requires approval from the state health planning agency before an organization can begin any major capital project, such as expansion into home health. As a result, the government can limit the number licenses/certifications it issues to service providers. Additional challenges included: Inconsistency in the funding that a government issues to different service providers Strict regulations to create or fund HCBS programs Staffing: Hiring and retaining the “right staff” for the home care environment was challenging for several providers. The home setting is different from the residential setting and certain characteristics make individuals better suited for the more autonomous setting. In addition, providers experienced staffing shortages because they could not find staff with adequate qualifications, or lacked sufficient staff when there was increased demand for services. Benefits Continuum of care: Providing a multitude of services allows the provider to support the individual through the continuum of care. Clients can age as they wish and the organization can adapt to client needs and the desire of consumers to stay at home. The organization can provide care across service lines and across the aging process. Expanding market and mission: The addition of home and community-based services is an opportunity to expand the number of older adults an organization can serve and to reach a 10 | Residential Provider Expansion into Home and Community-Based Services greater percentage of the target population. An HCBS program targets a different market composed of individuals who choose not to live on a campus and prefer to age in the home. A provider that serves a more affluent resident population can use an HCBS program to serve individuals with more modest incomes. The HCBS provider also can help consumers navigate the system of long-term services and supports, and can reach a variety of individuals through different service lines. Relationships and marketing opportunities: Serving people at home creates a relationship between the provider and consumers early in the aging process. The retirement community can build awareness of its on-campus options and market its services. The client and family members can build trust with the provider and can be comforted by the fact that they can turn to the same organization over time. Clients, or the members of their family/support networks, may become oncampus residents when their care needs change and they require higher levels of care. Serving people at home creates a relationship between the provider and consumers early in the aging process. Financial: HCBS programs have generated revenues and positive financial gains for some providers. These revenues are particularly beneficial when interest in retirement community living is down. The additional service lines also have diversified the revenue stream in some organizations. An organization’s residential setting may be supported primarily by publicly funded services. The HCBS program, which may rely more on private funding, can augment and subsidize the public funding. Lessons Learned Providers offer several suggestions for residential service providers that are considering or already expanding into home and community-based services. These suggestions are based on their experience launching and operating HCBS programs. Prior to Launch Market research: It is important to know the needs of the community, and understand the competition, before launching a program. Conduct extensive market research to understand what services the community wants and how to most effectively market to the target group. Identify organizations that already INTRODUCTION provide the services you want to offer and learn about their successes and challenges. Understanding the market can lead to greater program success. For example, one provider noted that its superficial market analyses identified the services consumers wanted, but not the services for which they were willing to pay. This resulted in lower-than-expected rates of participation in a transportation program. Networks and partnerships: Establish a network prior to launching the program. The network should include potential referral sources and partners that will help you build the client base. Build relationships with key referral sources, including hospital discharge planners, physician practices or insurance companies. Evaluate whether it is more beneficial to compete with other providers in the community, or collaborate with them to fill specific service gaps. Carefully review a prospective partner’s business plan, philosophy, organizational cultures and “business chemistry” to ensure compatibility. Business strategy: Have a defined strategy in place before starting your program. Test the business idea. Develop a solid business plan and vision of how to operationalize the program. The business plan should align with the realities of the market. Education: Educate staff and residents about home care/ home health care and how it can benefit the organization, workforce and community. Consider educating the board of directors about the reasons and benefits for diversifying service lines. Think about conducting informational sessions or workshops to educate community members. Staffing: Staff the home care/home health business with people who have the right personalities and backgrounds to launch and operate the program. These individuals should have an understanding of home and community-based services, particularly the service lines at your organization. They should also be familiar with the different payment models. Ensure that you care for your aides to engender loyalty among current aides and attract the best aides through word-of-mouth recommendations. Program Operations Expanding service lines and geography: When expanding into new geographic areas, consider using contract staff that will establish your brand by providing excellent service. Then hire your own staff to ease management and communication demands while further building your reputation. Establish virtual offices to minimize the infrastructure needed to expand. These strategies can help providers open multiple satellite office and gain clientele. Leadership patience: It takes time and energy to move outside your core business and start a new service line, even when partnering with an existing agency. The leadership team will have to understand, grow and expand the new model of care. Start with relatively few services and clients and gradually build up your capabilities. Learn from your experiences and growing pains. Staff and systems development: Engage in a continual process of staff and systems development. Recruit potential hires well, offer them good initial training, and train them throughout their tenure with the organization. Consider creating career pathways to retain staff. Understand the needs of consumers: Listen carefully to clients and members of their family/support networks to ensure that you understand their priorities. Learn what consumers value most and be sure to provide it. Marketing strategy: Employ a comprehensive strategy to promote your services. Recognize that marketing the HCBS program will require different strategies than marketing your residential services. Consider reinforcing your brand identity and distinguishing your services from the competition. In many regions, it is critical to engage referral sources for your program. You can accomplish this by meeting with referring agencies, attending networking events, accepting speaking engagements, and sponsoring celebrations and other organizational events. One particularly successful organization stressed that organizations need to distinguish their service lines and direct their marketing to different groups of potential clients, while maintaining the primacy and quality of the organization’s brand. It is important to know the needs of the community, and understand the competition, before launching a program. Conduct extensive market research to understand what services the community wants and how to most effectively market to the target group. Sodexo • IAHSA • LeadingAge | 11 NURSING HOMES Case Study ALTERSZENTRUM VIKTORIA BERN, SWITZERLAND | January 2015 Introduction Alterszentrum Viktoria was established in 1995 as a nursing home. It offers residential care to protected group homes for dementia patients, community nursing services, and medical care. Alterszentrum Viktoria also has independent housing with access to various services, as required. The organization began providing primarily medical and limited non-medical care to external clients in 2011 after making a strategic decision to expand its services and its client base. This study of Alterszentrum Viktoria’s expansion into home and community-based services was conducted through interviews with the organization’s director and a member of its board of directors. Policy Context Switzerland is a confederation of 26 independent cantons (federal states) that are distributed among the country’s four regions. Alterszentrum Viktoria is located in the Canton of Bern. Governance of Switzerland’s system of long-term services and supports is highly decentralized and involves federal, cantonal and communal governments. Primarily, cantonal governments develop policies affecting older people and long-term care services. Each canton has its own government and set of rules for each sector of the health care system. However, cantons may coordinate their actions at the regional or national level. Swiss government policy has favored home care, over care in nursing homes, for several years. The government is working to ensure that individuals who require nursing home care can stay in their own homes or apartments until the end of life and will not be required to move to a special care unit. There are two reasons why home care is preferred: Delivering care services within the older person’s social environment allows relatives, friends and neighbors to continue providing informal care. Home care reduces the pressure on nursing home beds and leads to a more rational and economical use of those beds. When nursing home beds are not available, older people who cannot remain at home often are sent to the hospital, even though they do not have a medical need to be there. Insurance providers, not the government, pay almost all the expenses associated with physician-approved, home-based medical care. Care recipients pay a small percentage (10%) of these expenses out of their own pockets. Reimbursement rates for home-based medical care are consistent and do not fluctuate. However, the tendency for insurance providers to reduce their fees each year has resulted in lower prices for consumers, but lower reimbursements for organizations that provide services to those consumers. Swiss providers considering an expansion into medical home health care services must obtain a license after demonstrating that they meet criteria established by the canton. License holders must have the professional staff necessary to deliver medical care. If a provider meets this requirement, it will be approved, receive a license, and be free to open a home health care agency. The government continues to monitor the agency to ensure that it provides quality services. Each canton has one government-sponsored home health care agency. The government-sponsored home health care provider in Bern is strong and has been operating for many years. Private providers, including Alterszentrum Viktoria home health care, compete with the government agency. This makes it challenging, from a business point of view, to enter the home health care market and obtain new clients. Sodexo • IAHSA • LeadingAge | 13 ALTERSZENTRUM VIKTORIA Process for Launching the Program When the Alterszentrum Viktoria board of directors approved home and community-based services as a new service line, it was making a strategic decision to grow the organization. The government approved Alterszentrum Viktoria’s request to provide home health care and provided the documentation that the organization needed to deliver these services. Alterszentrum Viktoria decided to focus primarily on offering medical home care due to the great need—and high demand— for these services in the community. State-mandated insurance covers medical care services if a physician prescribes them. Competition in the Marketplace Alterszentrum Viktoria provides limited non-medical home care and, at this time, is not interested in expanding its nonmedical care. Providing non-medical home care is much more challenging than providing medical home care because statemandated insurance does not cover non-medical services and providers do not need a license to enter the market. Several factors increase competition among providers of nonmedical care services: On the regulatory side, however, the Canton of Bern has few regulations for the home health care service sector. It is relatively easy for providers to enter the market once they have hired professional staff. If an agency has a license and maintains standards of quality, it faces few problems from the canton. An agency that wishes to provide non-medical care is not required to obtain a license or to meet any government requirements. This regulatory environment made it fairly easy for Alterszentrum Viktoria to diversify its services. Expansion into Home and CommunityBased Services Alterszentrum Viktoria was established in 1995 as a nursing home. The organization began offering primarily medical and limited non-medical care to external clients in 2011. Alterszentrum Viktoria’s diversification into home care was driven primarily by government policies that provide stronger support to home care services than to nursing home services. Alterszentrum Viktoria’s management and board of directors made the decision to provide services to the general public so the organization could diversify its services and reach a larger percentage of the older population. Management and board were also seeking an opportunity to market the organization’s other services to home care clients who might require higher levels of care and services over time. It is not uncommon for nursing home providers in Switzerland to launch external home care services. Most (90%) Swiss adults who require assistance live in their own homes. Only a small percentage of these adults reside in nursing homes. In this market environment, the survival of nursing homes depends on their ability to offer services to external clients. However, competition for these external clients is fierce. 14 | Residential Provider Expansion into Home and Community-Based Services Many agencies offer non-medical care services. Consumers must pay for non-medical services out of their own pockets. Clients often do not want to pay for the assistance they receive. Intense market competition also characterizes the medical home health care market. Specifically: Home health care providers face competition from many private and government-owned agencies. As a result, growing a client base is a slow process for most providers. The market is open to any provider that obtains a license. There are no mandated restrictions on the number of home health care agencies that can deliver services in a specific geographic area. Description of the Program Partnerships Alterszentrum Viktoria provides its home health care services in-house and does not partner with outside agencies, although it does belong to an association representing notfor-profit providers. The organization considered establishing a partnership to lower its investment in software and staff education. However, stiff competition made it difficult to collaborate with outside agencies. In addition, partnerships with outside entities are not common in Switzerland. Most organizations believe that they can “do it better” on their own. Having an in-house agency allows Alterszentrum Viktoria to deliver home health care services to individuals in the community and to bring these services to independent residents who live on its campus. Alterszentrum Viktoria’s board of directors is considering the possibility of converting the nursing Timeline 1868 ALTERSZENTRUM VIKTORIA Guesthouse called Viktoria built. 1870 Viktoria is a sanatorium. 1897 Expansion of Viktoria sanatorium into Viktoria hospital. 1991–95 Viktoria Hospital converted to a nursing home. 2008 Opening of day center. 2011 Founding of home health care agency. Sodexo • IAHSA • LeadingAge | 15 home portion of its campus to independent apartments. The organization would then bring at-home services to the apartments. This option could help the organization reach more clients and strengthen its home health care service agency. Admission Criteria Before an individual can receive medical home health care, a physician must determine that he or she meets the criteria for this care. Non-medical care does not require a doctor’s approval and individuals do not have to meet eligibility requirements before they can receive these services. Services Alterszentrum Viktoria offers a range of medical care services to support older adults so they can stay in their own homes for as long as possible. As a supplement to medical care, the organization’s staff also provides limited non-medical services, including meals, cleaning, transportation and shopping. Alterszentrum Viktoria clients who require extensive nonmedical services must receive those services from a different provider. The organization maintains a list of providers in Bern that can deliver this type of care. Staff will make recommendations to clients who need more services than Alterszentrum Viktoria can provide. Alterszentrum Viktoria staff members provide home health care services for a minimum of 15 minutes. The organization offers services from 7 a.m. to 11 p.m., on weekdays and weekends. The agency does not provide overnight care, mostly because it is too small to offer this type of coverage. Clients Alterszentrum Viktoria has been providing home and community-based services for the past four years. It has been difficult to expand the program’s client base due to competition from other providers. As a result, the organization currently serves only 23 individuals. Most clients (95%) receive medical care. On average, Viktoria adds five to eight new clients each year. Alterszentrum Viktoria was not able to provide demographic information about its home health care clients. While the organization collects data about residents living on its campus, it does not currently gather information about clients living in the community. The organization estimates that only about half of its clients live alone and do not have family caregivers. Quality Assurance The Canton of Bern monitors the quality of Alterszentrum Viktoria’s home health care services. Bern, like other cantons, strictly supervises home health care providers and specifies guidelines for provider quality and staff professionalism. At a minimum, the canton conducts an annual, unannounced site visit to assess the agency. During this annual assessment, the home health care provider uses special instruments to measure the quality of its services. Alterszentrum Viktoria does not track quality measures outside of the government oversight process. The government uses its funds as leverage when providers do not fulfill regulatory requirements. If an agency does not meet 16 | Residential Provider Expansion into Home and Community-Based Services ALTERSZENTRUM VIKTORIA the canton’s standards, the canton will discontinue payment for services and close down the provider. When a client has a complaint about a home health care agency, its staff or services, the complaint is first addressed by the organization. If the organization is not successful in resolving the issue, the complaint is then forwarded to a canton office that is charged with handling complaints about home health care services. Since non-medical care services are private pay, the cantons do not conduct oversight to ensure the quality of those services. Instead, the private market controls quality and outcomes. It is assumed that clients will select a different provider if an agency does not meet a client’s quality standards. Alterszentrum Viktoria’s home health care staff consists only of nurses. There are no aides on staff. After the government issues a license, it supervises home health care nurses in the same way that it supervises nursing home nurses. Workforce Alterszentrum Viktoria’s home health care agency has two codirectors and nine full-time nurses. The organization’s clientbase is not large enough to warrant additional staff. Home health care nurses care for the same clients each week, when possible, and work in the home environment, either on-campus or off-campus. The home health care staff receives the same benefits as residential care staff. Alterszentrum Viktoria’s nursing home and home health care agency have the same director and structure. However, the residential and non-residential settings do not share nurses. All home health care staff members are new hires. The organization does not redeploy staff from elsewhere in the organization to work in the home health care agency. Other staff in the home health care agency, including human resources, marketing, billing and information technology (IT) staff, are shared with Alterszentrum Viktoria’s corporate offices. This sharing has created challenges for the billing staff, which needed additional training about the specialized billing practices associated with home health care services. The deployment of a new billing software for home health care services will require additional support from the IT department. All nurses at Alterszentrum Viktoria receive in-service training and attend workshops directed by the head of the nursing department. Nurses from residential care and home health care are cross-trained. It can be taxing to bring these two staff groups together for training due to the nurses’ attitudes toward the sector in which they do not work and are not likely to work. Alterszentrum Viktoria is aware of the differences between these two staff groups, and addresses those differences during training workshop discussions. Organizational Culture The nursing home and home health care agency at Alterszentrum Viktoria are not separate entities and the organizational culture for home health care and residential care staff is the same, since the newer home health care agency adopted Alterszentrum Viktoria’s culture when the agency was created. Workers from residential care and non-residential care have opportunities to interact with each other and exchange ideas. This can occur during formal meetings and the training/ workshops mentioned above. In addition, home health care and nursing home staff members can meet and engage with each other in a shared dining room. This sharing of organizational culture is not typical in Switzerland. In most organizations, home health care agencies are separate from their parent organizations and have vastly different cultures. These culture differences are due, in part, to the political debate over home health care that is currently taking place in Switzerland as the government increases its support for home health care services while decreasing its support for nursing home care. The debate extends to the relative merits of the different models of care. Alterszentrum Viktoria did not face any pushback from its staff when it expanded its services. Many nursing homes in Switzerland diversify into different service models, and home health care is a common service model. Staff members had no trouble accepting the expansion. Financial Implications Alterszentrum Viktoria’s home health care agency is based on the organization’s campus, but it has its own building. The diversification of the organization’s services involved an initial investment in office space, equipment and staff. The home health care agency has not yet broken even and may find it difficult to generate adequate revenues until the agency can expand its small client pool. This will be a challenge, given the competition for home health care clients. For the time being, other Alterszentrum Viktoria service lines can make up for the losses incurred by the home health care business line. Alterszentrum Viktoria’s management and board of directors have considered discontinuing the home health care agency because of slow growth and competition. However, they decided to continue the agency’s operation because of its potential to bring future customers to the organization’s residential care services. For this reason, the continuation of home health care is believed to be an advantage for the organization. Perceived Challenges Alterszentrum Viktoria’s home health care agency faces a variety of perceived challenges: Market competition with other providers makes it difficult to grow and expand the home health care service business. Competition from the official government-sponsored home health care service provider is fierce. Private providers must prove to clients that they are better, faster and have higher quality than the government-sponsored home health care agency. A Swiss nursing shortage makes it difficult to find and hire qualified personnel to provide medical care to people in their homes. Non-professional staff members, including aides, are easier to recruit and hire. Sodexo • IAHSA • LeadingAge | 17 ALTERSZENTRUM VIKTORIA A Swiss nursing shortage makes it difficult to find and hire qualified personnel to provide medical care to people in their homes. Alterszentrum Viktoria has found it difficult to make a profit from its home health care business. The organization’s management is unsure how long it will take for this business to break even, if ever. Lack of growth is the greatest barrier to the sustainability of Alterszentrum Viktoria’s home health care program. The organization has addressed this challenge by adopting a comprehensive strategy to market its entire organization, not just its home health care services. Alterszentrum Viktoria advertises its other services—including concerts, a day care center and a campus restaurant—in hopes that these opportunities will help the organization connect with prospective clients and create public awareness of its home health care operation. Perceived Benefits Alterszentrum Viktoria executives believe that the benefits of providing home health care services outweigh the challenges associated with the expansion. Those benefits include the following: The ultimate benefit associated with home health care services is the opportunities they create for Alterszentrum Viktoria to gain future customers. Alterszentrum Viktoria can now offer services along the entire continuum of aging services, including independent living, home health care, and special nursing services for people with dementia. Alterszentrum Viktoria has positioned home health care as one of many points of entry into the organization and a link to its nursing home. As the home health care staff builds relationships with the public, the individuals they encounter become potential customers who may eventually move to the Alterszentrum Viktoria campus, either as independent, assisted living or nursing home residents. The ultimate benefit associated with home health care services is the opportunities they create for Alterszentrum Viktoria to gain future customers. 18 | Residential Provider Expansion into Home and Community-Based Services Outcomes Alterszentrum Viktoria has not evaluated the impact of its home health care service program. The board of directors is discussing plans to conduct such an evaluation at a future date. Lessons Learned Providers considering diversifying their services face risks, but the benefits can be substantial. Offering a variety of services, and knowing the external environment, can help an organization determine which services will lead to greater success. Alterszentrum Viktoria learned the hard way just how important it is to understand the market before launching a new business line. Viktoria did not research the market and just “jumped into” the home health care business without knowing its competitors. That experience convinced Alterszentrum Viktoria that organizations should consider pre-development market research before launching a new home health care program. Such research would help an organization gain a better understanding of its market and the expertise needed for each new business line. Case Study FEROS CARE COOLANGATTA, QUEENSLAND, AUSTRALIA | March 2015 Introduction Feros Care is a not-for-profit, non-sectarian, standalone organization based in Coolangatta, Queensland, in the Commonwealth of Australia. The organization provides a wide range of aging-related services to older adults along Australia’s eastern coast. Feros Care provides services through three types of programs: Two low-care nursing homes6 One high-care nursing home7 Home and community-based service lines The organization’s home and community-based service lines include: Nursing services Personal care Home care Social care Wellness services An extensive range of telehealth services Overnight and weekend respite care Allied health care featuring community-based chronic disease management and other services subsidized by Australia’s Medicare program. Policy Context Australia is currently implementing a major reform of its aged care systems. There are currently five major government-funded home care programs. Feros Care has worked closely with all of these programs to expand its home and community-based service programs. The Commonwealth Home Support Program (CHSP) provides entry-level care for older adults who need governmentfunded support to remain at home. These services operate on a wellness model and may include a range of low-intensity services like domestic assistance, personal and social care, transportation and meals. CHSP is the largest governmentfunded program in Australia. The Home Care Packages Program serves individuals with complex chronic conditions who are eligible for residential aged care8 but are striving to age in the community. The program allocates home health and community aged care “packages” to older adults based on their level of need, as assessed by the government’s Aged Care Assessment Team. Eligible older adults receive one of four packages, which range from a relatively modest level of support (Level 1) to a very high level of support (Level 4). The packages cover a combination of clinical, personal and social care that may include nursing care, personal care, allied health, and domestic and social services. All levels of support include an option for dementia care. Feros Care currently receives the majority of its funding from the Home Care Packages Program. The Veterans’ Community Nursing Program aids individuals who have served in the armed forces. These beneficiaries receive home health care, including nursing and personal care. The program also covers the cost of care for veterans’ spouses, widows and widowers. The Veterans’ Home Care Program serves veterans, their spouses, widows or widowers. Beneficiaries receive non-medical home supportive care that is similar to the services provided through CHSP. The Allied Health Services Program provides a range of health services in hospitals, community health centers, homes, rehabilitation units and the community. Australia’s Medicare and private reimbursement fund the program. Services include: Sodexo • IAHSA • LeadingAge | 19 FEROS CARE Physiotherapy Podiatry Dentistry Audiology Occupational therapy Social, mobility, pain management, fall-prevention and disease management programs designed to support healthy aging Organizations like Feros Care face two primary complications as they provide services and supports to older Australians: consumer-directed care and government regulation. Consumer-directed care: Australia began promoting consumer-directed care in 2012 as part of its Living Longer Living Better aged care reform legislation. Consumerdirected care allows clients to choose their preferred provider, thus giving older Australians more control over their care and who provides it. The consumer-directed care policy places additional administrative and cost burdens on providers of aged care. For example, Feros Care and other providers sometimes must enter into new partnerships with local providers in order to honor clients’ choices. Government regulation: Organizations providing government-funded services are highly regulated and must comply with strict funding agreements, guidelines, external audits and external complaint mechanisms. In contrast, there are almost no regulations governing the provision of private-pay services. Most of the care that Feros Care provides is at least partly government-funded. Expansion into Home and CommunityBased Services Feros Care was established in 1990 as a small, low-care nursing home in Byron Shire, New South Wales. The organization has followed a steady path of expansion since then, as the following timeline illustrates. 1997: Feros Care added a high-care nursing home. 1999: Feros Care won funding to establish a small homecare service providing 25 older adults in Bryon Shire with community aged care packages. Providers of these packages receive a certain amount of funding per day to provide a range of services that support an older adult aging at home. Such packages might include the following services: One nurse visit per week for chronic disease management Weekly shopping services Transportation to therapy appointments three times each week Assistance with cooking and light housework for two hours a day 20 | Residential Provider Expansion into Home and Community-Based Services 2002-2003: The organization developed a plan to expand its home and community-based services and began carrying out the plan. Although the expansion proceeded slowly for the first two years, the organization has grown by more than 20% per year since 2005. 2005: The organization began offering home health care and home care in the private-pay market. 2012: Feros Care purchased another community-owned company operating a large nursing home. 2015: Feros Care currently provides a range of home and community-based services through various government programs and for private-paying clients. These services are available in a 3,000-kilometer area along Australia’s East Coast. The service area spans four states: New South Wales, Queensland, Tasmania and Victoria. Reasons for Expansion and Growth Feros Care’s decision to expand its home and community-based services was primarily market-driven. Although Feros Care was operating at a surplus in the early 2000s, its leaders knew that the organization would be vulnerable to competition due to its small size and the fact that the Byron Shire area did not have a large aging population. Feros Care realized it would soon struggle to compete for funding against providers in neighboring areas that had larger populations and greater proportions of older adults. The organization decided to expand its services and geographical reach for the following reasons: Expanding Feros Care’s home and communitybased services seemed less risky than expanding the organization’s assisted living and nursing home operations. Home and community-based services held two advantages in comparison with residential care: a lack of adverse media coverage and a much-reduced set of regulations. An expansion into home and community-based services would not be as capital-intensive as an expansion of residential care. Feros Care would not need to build new buildings or invest in new infrastructure. The expansion would provide Feros Care with a much larger potential market. Most (80%) of older adults in Australia were receiving government-funded support services in 2003, and the vast majority of those older adults were still living in their homes. Feros Care’s senior managers and board of directors made the decision to expand into home and community-based services as part of the organization’s strategic planning deliberations. The expansion received little-to-no resistance from staff members, who expressed excitement about Feros Care’s vision for the future. Timeline FEROS CARE 1990 Began as low-care nursing home in Byron Shire, New South Wales. 1997 Added high-care nursing home. 1999 Received government funding to provide home care to 25 older adults. 2002 Began competing for home care and home health care government funding on wider scale. 2005 Began offering privatepay home care and home health care. 2015 Provides a range of government-funded and privately paid home health, home care and other HCBS to older adults along the 3,000-km eastern coast of Australia. 2012 Purchased a company operating a large nursing home. Sodexo • IAHSA • LeadingAge | 21 FEROS CARE Dependence on Government Programs Initially, Feros Care provided only government-subsidized home care. The availability of government packages has greatly influenced organizational discussions regarding possible expansion into the private-pay home care market. In 2005, for example, the organization performed a market analysis to gauge opportunities within the private-pay market. At the time, long waiting lists for government-funded aged care threatened to curtail the organization’s growth potential. Feros Care viewed a private-pay expansion as a way to grow outside its current market and region, and to become more competitive with larger home care providers. The organization began offering a few private-pay services in 2005. However, an extensive expansion into private-pay services was put on hold when the government increased its funding for aged care that same year. Essentially, the government’s decision to increase its funding of aged care allowed Feros Care to grow by winning more government packages. Feros Care is once again considering an expansion of its private-pay services. This latest discussion stems from a government move in July 2014 to develop more stringent means testing for the receipt of home care packages. The new rules could make it cost-efficient for some consumers to purchase Feros Care’s private services. As a result, the organization expects the private-pay home care business to grow over the next several years. Ironically, the few private services Feros Care began offering in 2005 allowed the organization to compete more effectively for government packages. As Feros Care began offering services in other regions, it learned that those services were often superior to services offered by other providers. Feros Care’s responsiveness, flexibility, staff values and philosophy of care helped it build a strong reputation in these regions. As a result, the organization became even more successful at acquiring government contracts. This success spurred a positive feedback cycle that helped Feros Care further improve and expand its services, succeed during subsequent funding rounds, and then improve and expand its services even more. Description of the Program Services Provided Most of the home and community-based services that Feros Care provides are delivered to older adults who receive assistance through the Home Care Packages Program. To a lesser extent, the organization provides services to older adults covered by the Veterans’ Community Nursing, Veterans’ Home Care, Commonwealth Home Support, and Allied Health Services programs. Feros Care provides non-medical and medical services through these government programs and for its private-paying clients. Non-medical services include: Light housework Cooking Lawn care Pet care Assistive and smart technologies Moving services Table 1. Services Provided by Feros Care DOMESTIC CARE PERSONAL CARE & NURSING WELLNESS AND LIFESTYLE Cleaning & Light Housework Personal Self Care (showering, Companionship & Social Support Personal Laundry dressing, grooming, toileting) Accompanied Community Outings Unaccompanied Shopping Continence Management Counseling & Chaplaincy Services Errands & Bill Paying Clinical Care Maintaining Independence Program Accompanied Transport Palliative Care Mobility Exercise Programs (Strong Home-Cooked Meals Dietary Planning & Education Foundations & Forever Young) Home Maintenance Mobility Assistance & Equipment Respite (in-home, day, residential) Lawn Mowing & Gardening Communication Aides Day Trips & Social Groups Pantry/Cupboard & Spring Cleaning Accompanied Medical Appointments Volunteer Activities Moving Services Foot Care & Nail Care Falls Prevention & Re-ablement Pet Care Life Link Personal Alarms Reminiscence, Hobbies, Crafts Internet Training & Support (banking, Lifelink Smart Home Monitoring (auto Telehealth Vital Signs Monitoring shopping) night lighting, bed/chair/door sensors, Internet training & Support (virtual Technology (Robo-vac cleaners) environmental alerts) visiting & social connections) Hairdressing: Visiting Services Beautician: Visiting Services 22 | Residential Provider Expansion into Home and Community-Based Services FEROS CARE Internet training and support Personal care Companionship Accompaniment to appointments Counseling and chaplaincy services Exercise programs Respite care Efforts to help older adults participate in community outings and wellness programs organizations that work under contract to provide frontline staff to its service lines. These agreements clearly spell out specific service delivery expectations and requirements. Feros Care also closely monitors client feedback and reported incidents associated with contract providers. The organization does not hesitate to discontinue partnerships due to differences in corporate philosophies or inadequate care provision. Medical home care services include, but are not limited to: Continence management Palliative care Nutritional planning and education Mobility assistance and home retrofitting Foot and nail care Medical monitoring services offered through telehealth programs Feros Care provides around-the-clock care when needed, and its Contact and Referral Center is staffed at all hours. While the organization does not offer live-in staff placements, it does provide nighttime and weekend care when clients are discharged from the hospital and for other needs. Feros Care regularly provides some services, such as personal care and help with medications, to clients during evening hours and on weekends. See Table 1 for more details about Feros Care’s home health, home care and community services. Partnerships Feros Care delivers services using a combination of its own staff and service partners from the surrounding community. When Feros Care expands into new regions, the organization strategically engages service partners in those areas to deliver direct care until it has a sufficient number of clients and services. At that point, Feros Care begins recruiting its own direct-care staff while maintaining its relationships with local service partners. Feros Care calls on those partners for assistance during times of high care volume. In contrast, Feros Care does not contract for any care coordination or case management services. Because care coordinators play a major role in monitoring direct-care provision and upholding its quality, Feros Care always fills these positions with its own staff members. This is one way that the organization works to ensure that its client assessment and care planning activities meet the highest standards, and that its service philosophy and the quality of its care are maintained. Feros Care employs other strategies to ensure that it maintains high standards of care. For example, Feros Care signs formal service/brokerage agreements with all Feros Care has 245 service partners across all of its service lines. The organization selects partners based on a number of factors, including reputation, price, capabilities and flexibility. Feros Care contracts with several franchisees associated with larger home care organizations like Just Better Care and Home Instead. The executives of these franchises tend to be smallbusiness owners who care deeply about maintaining good relationships with other providers. These business owners help Feros Care maintain its reliability, which is a source of pride for the organization. Australia’s implementation of consumer-directed care adds to the complexity of contracting for services. Empowered to choose the provider they want, consumers can select a local cleaner to do their housework instead of the service provider with which Feros Care has an agreement. In cases like this, the consumer-directed care program requires that Feros Care perform the necessary inquiries and develop a service partnership with the provider preferred by the client. Sources of Reimbursement Feros Care receives Commonwealth reimbursement from the Department of Social Services and the Department of Veterans Affairs for the services it provides through the Home Care Packages, Veterans’ Community Nursing, and Veterans’ Home Care programs. Medicare, private insurance,9 and privatepay clients pay for services provided under the Allied Health Services program. Sodexo • IAHSA • LeadingAge | 23 FEROS CARE Feros Care also receives some state funding for post-acute care that is managed by state health departments. These programs include Transitional Care; ComPacks, which provides immediate access to short-term community services; and programs for sub-acute care. State funding is generally for short-term interventions designed to reduce the likelihood of readmission. Consumer Eligibility In order to be eligible for government-funded programs, Australians are required to participate in an independent assessment, conducted either by telephone or in-person, or both. Independent assessors include the Aged Care Assessment Team for home care packages and the new Regional Assessment Service Team for the Commonwealth Home Support Program.10 The approvals process for each major government program is as follows: Home Care Packages Program: Traditionally, a local Aged Care Assessment Team determined an individual’s eligibility for a home care package after conducting an in-person assessment. This system changed on July 1, 2015. Now, clients access the Aged Care Assessment Team through Australia’s new My Aged Care Gateway, which makes an initial phone assessment and then refers eligible individuals to the Aged Care Assessment Team. Commonwealth Home Support Program: Beginning July 1, 2015, the client calls the Commonwealth’s My Aged Care Gateway for an initial phone assessment. Eligible individuals are then referred to the Regional Assessment Service for an inhome, face-to-face assessment. The assessors complete a goaloriented support plan and make the necessary service referrals to the client’s preferred home support service providers. Veterans’ Community Nursing Program: Clients must receive a referral for an approved service from a doctor or nurse. The amount of funding is based on the individual’s level of need. Veterans’ Home Care Program: A regional Veterans Home Care Assessment Team determines the individual’s needs and the level of support they may receive. Allied Health Services Program: A doctor must approve the client’s participation in this Medicare-funded system for chronic disease management and other allied health services. Private health providers have predetermined eligibility criteria. Clients must access approved providers, including Feros Care. Individuals can access all of these services regardless of their financial means. However, retirees who are not receiving a full pension may be required to make substantial co-payments. There are no requirements for receipt of privately paid services, other than ability to pay. Provider Eligibility Providers must apply for the right to provide services through government-funded programs. There are no upper limits on the number of clients a provider organization may accept through the Commonwealth’s veterans’ programs. 24 | Residential Provider Expansion into Home and Community-Based Services In contrast, providers participating in the Home Care Packages Program are awarded a license for a certain number of packages. For example, they may be allocated packages for 50 clients at a given time. Providers in the Commonwealth Home Support Program are given a certain amount of money to provide a given number of services. For example, providers may be allocated $100,000 in a given year to provide 1,000 medical transport trips. Feros Care Clientele Feros Care provided this snapshot of its home and communitybased services clients: The average age of clients is 82 years, and 59% are at least 80 years old. Two-thirds of clients are female. Most clients have at least one chronic condition. One-quarter of clients are nursing home certifiable but are living at home with assistance. Three-quarters of clients are receiving lower level care to help them maintain their independence. Most clients have financial needs, and 85% are full pensioners. Less than half (44%) of clients live alone without a full-time family caregiver. Quality Assurance Feros Care is committed to ensuring that it maintains high quality standards, through its own efforts and the efforts of its service partners. Quality is assured through four strategies. 1. The Commonwealth’s Aged Care Quality Agency regularly conducts on-site audits of government-funded community care programs, and compares providers’ quality assurance systems against a set of common standards. 2. Feros Care contracts with a standards-compliance company called SAI Global for comprehensive quality management of all its programs. Feros Care and SAI Global track many measures, including the following: Daily incident and hazard reporting Systems of improvement Workflow management Customer feedback programs Internal audit programs Business excellence parameters Response times Adherence to policies and procedures 3. Feros Care employs a chief resolution officer who oversees the resolution of all complaints to the organization’s Customer Feedback Program. 4. Feros Care uses its care coordinators to oversee the work performed by direct-care aides and to ensure that high quality is maintained. Care coordinators integrate the feedback they receive from clients with data collected Feros Care provided this snapshot of its home and community-based services clients: Feros Care Clientele A snapshot of Feros Care’s home and community-based services clients 82 Average age of clients 59 % at least 80 years old 2/3 1 1/4 are female clients number of chronic conditions for most clients (at least) clients who are nursing home certifiable, but live at home with assistance 75 85 % of clients receiving lower level care to help maintain indepencence % of clients who are full pensioners (most have financial needs) 44 % of clients who live alone without a full-time family caregiver Sodexo • IAHSA • LeadingAge | 25 FEROS CARE through tracking of quality indicators. The coordinators discuss issues with aides as they arise, and pass information to supervisors. This information is included in daily communication updates on services and clients, monthly staff meetings, and performance reviews. Marketing Feros Care uses many venues to spread the word about its home and community-based services. The organization employs a comprehensive branding and marketing strategy that includes Feros Care magazine, newspaper advertisements, local media coverage, social media outreach, and participation in such community events as expos, festivals and public celebrations. The organization also employs a comprehensive strategy to engage referral sources. These strategies include scheduled visits with referring agencies; participation in networking events, speaking engagements, celebrations and other events; and maintenance of an extensive customer relations database. Figure 1. Feros Care: Annual Growth Since Expanding to Home and Community-Based Services 2002-03 2003-04 2004-05 2005-06 2006-07 2007-08 2008-09 2009-10 2010-11 2011-12 2012-13 2013-14 2014-15 0% 5% 10% 15% 20% 25% 30% 35% 26 | Residential Provider Expansion into Home and Community-Based Services Feros Care uses its care coordinators to oversee the work performed by direct-care aides and to ensure that high quality is maintained. Care coordinators integrate the feedback they receive from clients with data collected through tracking of quality indicators. Financial Implications In 2005, Feros Care served 50 clients per year. In 2014, the organization served approximately 4,000 clients, and it expects to serve at least 6,000 clients in 2015, due to the advent of new government-funded transportation and allied health services. Client numbers could expand even further to 30,000 clients per year due to the organization’s recent approval to operate the Regional Assessment Service for the Commonwealth Home Support Program (CHSP). However, services to some CHSP clients may be provided only on a short-term basis. Figure 1 presents Feros Care’s annual growth, beginning in 2002-2003 when the organization began its expansion into home and community-based services. Feros Care has experienced double-digit growth during most years since home and community-based services became its largest service line. The first two years of Feros Care’s expansion into home and community-based services (2003-2005) proved difficult, as the organization struggled to find its niche in a field crowded with many competitors. However, Feros Care’s growth has exceeded 20% per year for almost every year from 2006 until the present. In 2003, the organization funded its community care services with only $250,000. In contrast, current funding levels for community care is $35 million. The new Regional Assessment Service is likely to bring this growth level to $45 million in 2016. The initial growth period did not require a large expansion of the Feros Care staff. Prior to 2005, Feros Care hired a part-time marketing assistant and a part-time writer who was responsible for submitting applications for government packages. The organization’s chief executive officer also spent considerable time on marketing and budgeting efforts. Once the organization began to obtain a significant number of government contracts, however, these positions began paying for themselves. The organization’s home and community-based service program broke even in 2007. FEROS CARE The bulk of Feros Care’s current revenues stem from the services it provides to a quarter of its clients. That’s because Feros Care receives most of its funding from the Home Care Packages Program, despite the fact that the Commonwealth Home Support Program (CHSP) is larger and serves more of Australia’s older adults. Generally, the monetary value of individual home care packages is much greater than the value of packages provided through CHSP. For example, a typical CHSP client might only be approved to receive $2,000 per year in services, whereas typical home care packages range from $7,500 to $45,000 per year. Workforce Feros Care employed approximately 350 people in 2014. More than 280 of these employees were care aides, and a majority of these care aides worked in the organization’s home care division. Nurses comprised just over 5% of Feros Care staff in 2014 when Feros Care also used staff members to develop staff rosters (6%) and coordinate services (8%). Allied health professionals, who work in a Feros Care service line that is growing rapidly, are expected to comprise 5% of the organization’s employees by the end of 2015. Feros Care expects its workforce profile to change over the next year, although home care workers will continue to comprise the majority of its staff. The organization expects to see staff growth in three areas: Allied health: The allied health line will soon be expanding due to the increased use of specialists like physiotherapists and occupational therapists in Feros Care’s restorative care programs. These specialists operate a range of mobility, strengthening, fall-prevention and wellness programs designed to increase the independence of clients. Telehealth: The number of telehealth nurses performing chronic disease management is expected to increase as Feros Care’s telehealth services continue their rapid growth. Information technology (IT): Feros Care will also be expanding its IT staff to meet the growing needs for health technology in clients’ homes. Staff Benefits Because Feros Care is a not-for-profit provider, its employees can receive some of their income tax free. Feros Care also offers employees: Wellness programs11 Free gym memberships In-house leadership programs External education An employee assistance program Discounted mobile technologies Feros Care employees do not receive health insurance through their jobs because Australia has a public insurance program. Staff Recruitment and Training Working in home care differs greatly from working in a residential setting for aides at Feros Care and other organizations. Home care aides work alone primarily and perform a greater variety of tasks for clients than aides in residential settings. Home care aides have more responsibility to make accurate and timely observations and to prudently make care decisions on their own. They also have to be more flexible and versatile than residential employees, since they are called on to provide cleaning, cooking, social care and, in some cases, therapy support in addition to traditional care tasks. For these reasons, Feros Care generally does not redeploy residential aides to home care unless those aides are very open to working on their own and undertaking all the activities required to support clients. Residential care aides may never have performed activities like cooking and cleaning as part of their prior professional responsibilities. In addition to taking direct job inquiries, Feros Care partners with jobs networks and registered training organizations to identify the most qualified candidates. Once potential hires have been identified, Feros Care conducts structured interviews and tests applicants’ skills in such areas as technology and observation, before making hiring decisions. Feros Care has found that it is important to hire staff members who are independent, are known to the organization, have experience, and understand the expectations of the job. Independence: Feros Care looks for staff members who are self-starters and are comfortable working alone most of the time. These staff members also need to be comfortable using technology to stay connected with the organization and with clients. Known quantities: Feros Care places great importance on hiring aides it knows and trusts. That’s why the organization reduces its reliance on contracted services after it has settled in a new region. And that is why Feros Care grooms its best home care staff for management and supervisory positions, rather than hiring staff from outside the organization or from its residential services division. Feros Care also shares executive and billing staff across its home and residential care divisions, rather than hiring additional staff from outside the organization. Feros Care places great importance on hiring aides it knows and trusts. That’s why the organization reduces its reliance on contracted services after it has settled in a new region. Sodexo • IAHSA • LeadingAge | 27 FEROS CARE The hiring process for care coordinators is an exception to this practice. When expanding into new geographical areas, Feros Care hires local residents to serve as care coordinators because these individuals are familiar with local communitybased services. Feros Care carries out an extensive training program for these new hires so they will be well versed in the organization’s philosophy and procedures and well prepared to uphold the quality and reputation of the Feros Care brand. Experience: Feros Care works hard to recruit aides and other personnel who are already experienced at providing care in the community. Applicants’ values, service philosophy and love of working with older adults play a large role in the selection process. In its search for employees with these soft skills, the organization may hire workers with less-than-developed clinical and care skills, and then provide mentors and training to help these staff members develop any missing skills. Clear expectations: Detailed position statements ensure that job candidates understand Feros Care’s expectations for them. Feros Care has mechanisms in place to ensure that staff members understand unwritten ground rules and the organization’s underlying philosophy. In addition, a staff competency registry contains information about mandatory and additional qualifications for each major role. Feros Care takes steps to ensure that new staff members know how management views their performance. It also provides opportunities for staff members to give feedback during regular performance reviews. Staff Training and Orientation Feros Care uses various training processes to maintain the competence of new hires and existing staff. Training begins at the time of hiring and continues throughout employees’ tenure with the organization. New hires undergo a staged orientation program that reviews the organization’s comprehensive staff handbook and the mandatory competencies for their positions. New staff members are on probation during the first six months of their employment and receive a number of supports to ensure their success: Feros Care pairs new staff with a current staff member in a similar role. New staff members are closely monitored and supported through the organization’s Staff Candidate Care Program. To foster tight coordination, Feros Care provides smartphones to all new direct care staff, case managers, nurses and allied health professionals. Beyond required training, Feros Care employees have numerous opportunities to develop themselves professionally. These opportunities include enrolling in certificate courses and workshops, and participating in educational competitions. Feros Care runs an ongoing education competition that encourages employees to earn points on “Passport to Learning” 28 | Residential Provider Expansion into Home and Community-Based Services Training begins at the time of hiring and continues throughout employees’ tenure with the organization. continuing education cards. Employees who complete various learning and development activities receive awards like gift cards and entry into drawings for substantial prizes. Feros Care also provides access to internal and external professional networking websites and gives employees opportunities to develop their leadership abilities. The organization offers the Seven Star Staff Development Program, a three-year leadership course culminating in the attainment of a nationally recognized management certificate. Perceived Challenges Feros Care has faced challenges throughout the organization’s growth process, including challenges associated with meeting the needs of clients around the clock, communicating with remote staff, and navigating a highly competitive home care market. Meeting the Needs of Clients Around the Clock Clients with substantial care needs experience a greater level of risk living in the community than they would in a residential setting. In order to provide care for these clients around the clock, Feros Care staff members must learn about additional services available in clients’ communities and the capabilities and availability of family members and close friends to ensure that clients’ needs are met when Feros Care aides are not with them. FEROS CARE Feros Care has learned that it needs a substantial number of part-time staff working flexible hours to meet clients’ needs on a 24/7 basis. The growing use of telehealth technologies has helped the organization monitor clients at all times. However, training staff to use and maintain these technology solutions has required substantial effort. Communicating with Remote Staff Communicating effectively with remote staff, ensuring that they have adequate support, and helping them to feel valued, has also been challenging. To accomplish these goals, aides and care coordinators depend heavily on technology, including an advanced videoconferencing infrastructure. In addition, the organization provides regular opportunities for face-to-face socializing through organization-sponsored and individual celebrations. Feros Care’s many care-related awards have presented opportunities for celebrating the organization’s successes and fostering a sense of pride and teamwork. Fierce Competition The competition among Australian providers of home care services is fierce and has required Feros Care to define its niche sharply, rapidly and innovatively. As part of that effort, the organization seeks to provide care in regions with a demographic makeup that will support home care services. Feros Care resolved to meet new care needs without opening numerous new offices. Technology has helped the organization maintain a central organizational structure while creating virtual offices that rely on electronic records and other technologies. This high-tech approach has allowed Feros Care to move quickly as it launches high-quality community programs in distant geographic areas. At the same time, Feros Care uses remote-monitoring technology to provide care at all hours when it is needed. Feros Care’s technological expertise and its commitment to preserving high-quality services have allowed the organization to distinguish itself from competitors. The organization advertises these differences to consumers and showcases them in funding applications. Strengthening the organization’s virtual infrastructure will help it offer even more telehealth services so it can compete even more successfully in distant areas. The advent of consumer-directed care in 2014 made it even more important for Feros Care to raise its brand profile so potential clients would choose its services rather than the services of a local competitor. The fierce competition for home care packages has presented a more general challenge. Applicants to the Home Care Packages Program are requesting many more packages than are available. In 2014, for example, 1,821 home care companies sought 108,281 packages, yet the Commonwealth allocated only 6,598 packages to only 137 of the applying companies. That year, providers requested a total of $577 million worth of packages, but the government allocated only $53 million. The allocated packages have been distributed disproportionately. The top-10 organizations applying for home care packages received 30% of the total number of packages. The top-20 applying organizations received 50% of the packages allocated to the 137 successful companies. Given this intense competition, Feros Care is continually exploring new strategies, models and innovations. Perceived Benefits Feros Care’s executives and staff have found the provision of home care to be extremely rewarding, despite the challenges associated with that care provision. The organization’s leaders report that they have greatly enjoyed the challenge of leveraging a limited capital outlay to expand services and supports to more older adults in the community. They have also derived great satisfaction from pioneering new models and growing their organization’s competencies in a market that is growing, thriving and constantly evolving. These leaders take enormous pride in their service lines’ growth and their company’s reputation. They are relieved that expansion into home and community-based services does not require the physical or capital outlays associated with expanding residential aged care. Outcomes Feros Care has not conducted any formal evaluations of its programs, beyond analyzing income growth, geographic expansion and the organization’s profile within the industry. Home and community-based services have grown into the organization’s largest and most successful business line. These new services have greatly augmented the organization’s profile and its leadership within the industry. As a result, Feros Care has won national and international awards and its leaders are asked to speak at national and international conferences. The success of this business line has allowed Feros Care to help many more older adults and their family/support networks. It has also provided the organization with a healthy cash flow that, in turn, has benefited all its service lines. Home and community-based services have grown into the organization’s largest and most successful business line. These new services have greatly augmented the organization’s profile and its leadership within the industry. Sodexo • IAHSA • LeadingAge | 29 FEROS CARE Lessons Learned Feros Care offers the following suggestions for residential service providers that are considering or already expanding into home and community-based services: Start with relatively few services and clients and gradually build up your capabilities. Identify organizations that already provide the services you want to offer. Visit those organizations to learn about their successes and challenges. Invest in hiring staff members who have experience providing care in the community. Invest in technology, like telehealth, to enhance service provision. Engage in a continual process of staff and systems development. Recruit potential hires well, offer them good initial training, and continually train them throughout their tenure with the organization. Provide frequent feedback and review. Document the models that work for you. Involve members of a care recipient’s family/support network in the care planning process. Treat these individuals as partners. Listen carefully to clients and members of their family/ support networks to ensure that you understand their priorities. Don’t impose your expectations. Learn what consumers value most and be sure to provide it. Make sure that informal caregivers are adequately supported. 30 | Residential Provider Expansion into Home and Community-Based Services Know the communities in which clients live. Link clients to additional services as needed. Employ a comprehensive strategy to promote your services. Market your brand extensively, and engage referral sources by meetings with referring agencies, attending networking events, accepting speaking engagements, and sponsoring celebrations and other organizational events. Use these events to promote your brand. Demonstrate success and quality in related fields—like mental health, care for people with disabilities, postacute care, and private home care—when competing for government funding for home and community-based services. Engage in a continual process of staff and systems development. Recruit potential hires well, offer them good initial training, and continually train them throughout their tenure with the organization. Case Study ISABELLA GERIATRIC CENTER NEW YORK, NEW YORK | May 2015 Introduction Isabella Geriatric Center is a not-for-profit, non-sectarian organization in New York City that has pioneered the care of older adults since 1875. Isabella grew from a traditional nursing home into a leading health care organization that provides a continuum of services on its own campus, in the Washington Heights and Inwood neighborhoods of Manhattan, and throughout New York City’s five boroughs and surrounding suburbs. In addition to a 705-resident nursing home, Isabella offers moderately priced senior housing, adult day health services, child day care, certified home health care, licensed home care services, short and long-term rehabilitation, a service program for Naturally Occurring Retirement Communities (NORC),12 community-based care coordination, and other community programs designed to help older adults remain healthy and independent at home. This case study of Isabella’s expansion into home and community-based services was conducted through interviews with executives at Isabella Geriatric Center and a two-day site visit at Isabella Geriatric Center. Sodexo • IAHSA • LeadingAge | 31 ISABELLA GERIATRIC CENTER Policy Context Isabella began offering home care after New York State instituted the Nursing Home without Walls (Lombardi) program in 1977 to help Medicaid-eligible older adults with chronic illnesses and disabilities remain in the community. The program offered eligible Medicaid beneficiaries an alternative to institutionalization by providing medical, nursing and rehabilitative care at home. Lombardi participants also had access to home health care aides, social day services, homedelivered meals and transportation to and from medical appointments. Isabella supplemented the program’s Medicaid reimbursement with grant funding. New York Governor Andrew Cuomo recently disbanded the Lombardi program and began implementing an array of cost-cutting initiatives for Medicaid beneficiaries, including a requirement that all New York Medicaid recipients enroll in a managed care plan. This new mandate has made it necessary for Isabella to alter its approach to recruiting and billing clients. Prior to the managed care mandate, Isabella recruited adult day health services clients from the community. Now, Isabella’s adult day health program depends on care settings like doctors’ offices to refer clients to the program. New York State has joined the Delivery System Reform Incentive Payment Program (DSRIP) to further reduce Medicaid costs. Nine states, including New York, have adopted DSRIP to date. DSRIP fundamentally restructures the way care for Medicaid recipients and the uninsured is delivered and billed. Hospitals, physician practices and other health care providers work together through the program to meet specific measures that are designed to reduce costs while improving or maintaining health outcomes. One of DSRIP’s major goals is to reduce hospital admissions and readmissions by 25% in five years. New York State providers that succeed in meeting DSRIP measures will receive a portion of $6.4 billion in shared savings from the federal government’s Medicaid reform initiatives. Successful providers may also draw on over $1 billion in federal savings for capital outlays that will make care more efficient. Hospitals participating in the DSRIP program determine which DSRIP measure they will address, and how they will distribute savings, if any, to participating partners. Isabella’s partnerships with four DSRIP participants could bring the organization a share of newly available funds that will reward teams meeting specific program objectives. The program is nascent and rapidly evolving, and Isabella does not yet know how beneficial its participation will be. Expansion into Home and CommunityBased Services History of the Expansion Isabella established its nursing home in 1875, and began offering senior housing at Isabella House in 1964. Both of these residential options are delivered in two buildings: a 17-story building and a 13-story building in the Washington Heights neighborhood on Manhattan’s Upper West Side. 32 | Residential Provider Expansion into Home and Community-Based Services Providing services to the greater community was a natural move for Isabella because it is well established and well known in New York. The organization began offering home-based services in 1989, seeking Lombardi program funds to care for community-dwelling Medicaid clients who were seriously ill or had disabilities. In 1991, Isabella began providing child day care onsite at its nursing facility. In 2000, Isabella added adult day health services to the community-based service lines it provided from its Washington Heights campus. More recently, Isabella began providing a diverse array of community-based health, wellness and care management services for older adults. Those services, described fully in the next section of this case study, include a supportive service program for NORC residents; service-specific case management services provided by a consortium of eight community services providers; an information and referral clearinghouse for older adults and their caregivers; education, counseling, and wellness programs provided by Isabella’s Institute for Older Adults; certified home health care; and licensed home care services. Reasons for Expansion and Growth Isabella’s expansion into home and community-based services, while facilitated by the availability of Lombardi program funds, was mission-driven. Isabella realized that few members of its community were likely to move to the organization’s nursing home or senior housing property. Given its long-standing ties to families in northern Manhattan, Isabella wanted to serve that community in other ways by developing a continuum of services that would support older New Yorkers who wanted to remain in their homes. The expansion into home and community-based services also supported Isabella’s longstanding mission to provide services and supports to poor, underserved, and non-English-speaking older adults. Isabella executives believe that an enduring commitment to the community distinguishes not-for-profit providers from their for-profit counterparts. Not-for-profit providers, they believe, are less inclined than for-profit providers to abandon that commitment for financial reasons. Description of the Program Services Provided Adult Day Health Care: Since 2000, the Isabella Adult Day Health Care Program has provided health care to approximately 40 older adults per day. The program operates Monday through Saturday from 9 a.m., to 3 p.m., at nearly a full daily census. It provides participating adults with health care, social activities, recreation and meals. A substantial portion of clients has serious psychological or neurological issues, including depression and intellectual disabilities. The program staff includes social workers, two registered nurses (RN), certified nursing assistants (CNA), a recreation therapist and bus monitors. Members of the program staff work with each client to develop a care plan that outlines goals in such areas as nutrition, exercise and medication adherence. The plans’ goals are reviewed and updated every six months. Timeline 1875 ISABELLA GERIATRIC CENTER Opens as a nursing home. 1964 Opens Isabella House providing senior housing. 1989 Begins providing home health and home care through the Lombardi Program. 1991 Begins offering child day care onsite at its nursing home. 2000 Begins offering adult day health care onsite at its nursing home. 2009 2014 Establishes Isabella Care at Home, Inc., a certified home health agency. Establishes Isabella Visiting Care, Inc., a licensed home care agency. Sodexo • IAHSA • LeadingAge | 33 ISABELLA GERIATRIC CENTER Naturally Occurring Retirement Communities: Isabella has been serving older adults in two Naturally Occurring Retirement Communities since 2006. The El Corazon Neighborhood Naturally Occurring Retirement Community (NNORC) consists of 40 contiguous low-rise buildings within six square blocks. The Fort George VISTAS Naturally Occurring Retirement Community (NORC) is located in three high-rise buildings at the Mitchell-Lama Co-Op. Each NORC houses approximately 400 residents, 275 of whom make use of services that Isabella delivers in each building. The design of both programs is based on a standard model for NORC services developed by New York City’s Department for the Aging. The programs’ core service areas are social work assistance and case management, health care assistance and health care coordination. Staff members and community partners provide NORC residents with comprehensive services that include the following: Social work services Individualized health care assistance and management provided by a nurse Health promotion and screenings Education Recreation Support groups Volunteer opportunities The El Corazon NNORC, currently funded by the New York State Office for the Aging and New York City Council discretionary funding, provides additional services to New York’s low-income immigrant communities. Full-time social workers and part-time nurses provide these services five days a week on site at the NNORC, at a centralized storefront, and during home visits. In addition, staff offers a menu of preventive care and health-related activities. NNORC provides these much-needed additional services without the help of a distinct housing partner. Isabella Visiting Care, Inc.: Launched six years ago, Isabella Visiting Care Inc., (IVCI) is a licensed home care services agency currently providing more than one million hours of home care services each year to more than 500 New Yorkers over the age of 18. Services are available in Manhattan, the Bronx, Brooklyn, Queens and Westchester County. IVCI offers paraprofessional and escort services, with oversight by a registered nurse, that include: Cooking Cleaning Personal care Medication reminders 34 | Residential Provider Expansion into Home and Community-Based Services Companionship Care management for individual with complex chronic conditions Agency services are delivered by hourly and live-in home health aides. A nurse is on-call at all times. IVCI hires its own home health aides and trains them, in its own program, to meet New York State certification requirements. The agency uses Home Health Aide Exchange to match home health aides with clients based on availability, proximity, relationships, and preferred language. Language is an important placement criterion since half of Isabella’s clients are Hispanic and a growing number are Chinese or Russian. IVCI currently employs 650 home health aides, most of whom live in and feel a connection with the community. Many aides work with one or just a few clients each week. This helps aides feel “like family.” Clients may invite aides to birthday and other parties, or refuse to receive medical treatment unless their home health aide is present. Isabella Care at Home, Inc.: Launched one year ago, Isabella Care at Home, Inc., is a certified home health agency providing post-acute, part-time or intermittent skilled health care and support services to individuals over the age of 18 who reside in Manhattan, Bronx, Brooklyn, Queens and lower Westchester and whose needs may be relatively short-term. Services are provided directly or through contracts with other providers. They include: ISABELLA GERIATRIC CENTER Management of transitions between a hospital or nursing facility and home Comprehensive health assessment Skilled nursing Physical, occupational and speech therapy Social work services Nutrition counseling Supplemental assistance with home care and personal care Ninety-one clients had been admitted to the program as of the first quarter of 2015. Clients typically stay in the program for four to six weeks. Home Health Program: Isabella’s health home program provides care management services to over 130 Medicaid beneficiaries with complex chronic conditions who are enrolled in two New York State Department of Health-designated Lead Health Home Programs. The program is designed to manage clients’ health conditions and prevent hospital admissions and the overuse of Emergency Room (ER) services. The home health program began in 2012 as a Medicaidfunded operation. Today, five care coordinators serve 132 clients. In addition to providing care coordination services, the home health program links clients to doctors and other providers in the community. The care coordinators develop, review and update a care plan for each client every six months. Care Management Services: Isabella’s Care Management Services program provides services to more than 650 members of managed long-term care programs. The following care management services are provided by a team of health care professionals led by an RN or social worker, as appropriate: Pre-enrollment assessments Coordination of services Authorizations for changes/additions to care Communication with physicians, medical professionals and family members, as needed Assurance of continuity of care throughout the health care system. Upper Manhattan Partnership for Senior Independence: Isabella is a founder and leading partner of the Upper Manhattan Partnership for Senior Independence (UMPSI), a consortium of eight community service providers in Northern Manhattan. Social workers in the UMPSI Program provide free, service-specific case management to older adults living in Washington Heights, Inwood and Central or West Harlem. UMPSI connects older adults with meal, transportation, social work, wellness, benefits enrollment, and other services. Isabella Senior Resource Center: Founded in 2004, the Isabella Senior Resource Center provides information about health care services and insurance, and assistance with benefits enrollment, to older adults and their caregivers. The Institute for Older Adults: Established in conjunction with the 1995 White House Conference on Aging,13 the Institute for Older Adults provides free education, counseling, health, wellness and exercise programs to approximately 4,000 New Yorkers over the age of 50. The institute offers a 50+ Club and a Walking Works Wonders program that provides free exercise classes to more than 500 community residents. Partnerships Isabella has a long history of working with community partners to meet the needs of older adults. It is a member of the Washington Heights and Inwood Council on Aging (WHICOA), a partnership organization through which more than 40 community organizations advocate and provide resources and services for more than 28,000 older adults and their informal caregivers each year. Isabella’s Senior Resource Center, UMPSI and case management programs often refer clients to the services of other WHICOA members. Isabella has also become a generous benefactor to neighboring not-for-profit organizations in Northern Manhattan. For example, the organization offers not-for-profit organizations and local public schools free use of its meeting space so they can carry out education initiatives. Overall, Isabella has an outstanding relationship with its community. However, the recent expansion process has strained some of those ties. For example, Isabella Adult Day Health Care initially sought to recruit clients from local senior centers that provide social activities and recreation but not health care. Fearing that they would lose clients to Isabella’s new program, the senior centers restricted the organization’s access to senior center clients. As a result, Isabella initially had trouble building its daily census for the adult day program. Despite early struggles, the adult day health center has become an important and wellrespected program among Isabella’s WHICOA partners, which include several senior centers. Isabella has also recently partnered with other providers through the DSRIP program. These partners include: Mt. Sinai Health System New York Presbyterian Health & Hospitals Corporation Advocacy Community Partners, a consortium of area physicians Isabella may consider forming additional partnerships as it seeks to remain financially independent and to define and pursue its community-oriented mission. Marketing Marketing efforts for most of Isabella’s service lines are centrally coordinated. These efforts once were focused on recruiting older adults from the community by: Conducting direct mail campaigns Talking with older adults at health fairs, senior centers, doctor’s offices and clinics Sodexo • IAHSA • LeadingAge | 35 ISABELLA GERIATRIC CENTER Purchasing print and radio advertising in English and Spanish Seeking media coverage from local televisions stations The Spanish radio advertisements and direct mail campaigns were particularly effective at engaging a local immigrant client base. Television and radio continue to be important vehicles for Isabella’s marketing. However, most of the marketing team’s efforts currently focus on social media and Isabella’s website. The marketing team places ads on Facebook and Google+ and maintains an active Twitter account. It also monitors these outlets multiple times a day to ensure that they are enhancing Isabella’s reputation. The marketing team responds promptly and courteously to any concerns posted on social media. The team also demonstrates publicly that Isabella is investigating any complaints. In cases where complaints are unfounded, the team contacts the social media outlet where the complaint was aired and urges that outlet to remove the inaccurate material. The marketing team is still determining the best strategies for harnessing the power of social media marketing. Members of Isabella’s marketing staff have learned to make use of the buzzwords that community members prefer to hear during discussions of aged care services. For example, “mental health” services tend to carry a stigma among Latino clients, but these clients will use “wellness” services that incorporate the same approaches. Over time, Isabella has developed a language with which the community is very comfortable. The re-emergence of managed care plans as dominant payers for home and community-based services has necessitated changes in Isabella’s marketing strategy. For example, the management of Isabella’s adult day health program taps into the managed care market by raising its profile with physicians, eldercare attorneys, geriatric care managers and other stakeholders who refer older adults to its services. These strategies partially overlap with efforts to market the organization’s residential services, which depend on the same referral sources. Members of Isabella’s marketing staff make use of the buzzwords that community members prefer to hear during discussions of aged care services. In the process of developing the NORC programs, Isabella surveyed building residents, conducted a community needs assessment, and carried out grassroots marketing, such as door-to-door advertising and blood pressure screenings. Specifically, staff members used a number of strategies to recruit participants: 36 | Residential Provider Expansion into Home and Community-Based Services They placed flyers under residents’ doors in 40 apartment buildings. The flyers advertised a day when eligible residents could visit the Isabella Senior Resource Center, complete a survey and receive a free Red Cross emergency kit. They developed a database, which is continually updated and contains information about residents who want to take part in NORC activities and services. They began sending residents a calendar of NORC activities. This calendar has evolved into a monthly newsletter. The NORCs now provide residents with an expanded array of services in core program areas. An initial key to success was staff’s ability to attract prospective clients with healthful and delicious ethnic food that appealed to residents of the increasingly diverse Washington Heights and Inwood neighborhoods. Program staff serves healthful lunches at celebratory events, and snacks during all education and recreation programming events. The Institute for Older Adults distributes a quarterly newsletter containing advice about healthy aging and information about Isabella’s programs. Every two months, 4,000 members of the institute receive postcards with information about upcoming educational seminars, wellness and exercise programs and trips to local cultural sites. Sources of Reimbursement Each of Isabella’s major services accepts the following forms of reimbursement. Isabella Adult Day Health Care: Medicaid managed care plans and private pay Isabella Visiting Care, Inc.: Private pay and most longterm care insurance plans Isabella Care at Home, Inc.: Medicaid, Medicare and most insurance plans NORC Services: Funded by New York City and New York State grants Isabella Home Health: Medicaid Quality Assurance Isabella’s adult day health care program measures quality by regularly asking families to complete annual satisfaction surveys and by tracking how several quality indicators are associated with specific agency initiatives. For example, the adult day health program monitors hospital admissions, readmissions and ER use among specific client groups, including clients who receive mental health care. The organization discovered that its psychological services appear to reduce preventable hospitalizations and ER visits. Isabella completes and monitors all assessments required by the Centers for Medicare & Medicaid Services (CMS)14 for its home health and home care agencies. These measures, which are incorporated into the Home Health Compare website, include assessments of client pain, depressive symptoms, falls, pressure ulcers and wound management. In addition, CMS ISABELLA GERIATRIC CENTER Table 1. Demographic Composition of Isabella’s Community-Based Programs ADULT DAY CARE HEALTH CARE PROGRAM 93.4% Hispanic 6.6% African American EL CORAZON NEIGHBORHOOD NORC PROGRAM 90.8% Hispanic 4.7% Asian 3.5% Caucasian 1% African American FORT GEORGE VISTAS NORC 38% Hispanic 35% Caucasian 23% African American 4% Asian ISABELLA CARE AT HOME 40% Hispanic 29% Caucasian 22% African American 2% Asian 7% Unknown ISABELLA HEALTH HOME PROGRAM 72% Hispanic 21% African American 5% Caucasian 2% Asian required OASIS reports track clients’ progress as they receive care. Isabella also tracks the quality of its processes, including the accuracy and timeliness of initial assessments. Data is submitted to CMS on a quarterly basis. Clients receive a statement of their rights at the outset of care. Those rights include a requirement that Isabella will thoroughly investigate any complaints. Home health clients also have the option to call the U.S. Department of Health and Human Services with their complaints. Home health and personal care aides, if implicated, provide their version of events to the Isabella administration before there is a final adjudication. Isabella may reassign, discipline or terminate an aide if it is found that poor performance led to the complaint. Isabella follows up on all incidents and keeps clients’ physicians informed of the investigation’s progress. Financial Implications Isabella has experienced a decline in fee-for-service Medicaid reimbursements at the same time that it has gained revenue from Medicaid Managed Care and Medicare. In 2013, the organization generated just under $127 million in revenues, and had a $2 million surplus after making all payouts. This compares favorably to 2012, when the organization operated at a deficit. Because Isabella Care at Home, Inc. started in mid-2014, it has not yet generated a revenue gain as the program is still in a start-up phase. Isabella Visiting Care, Inc., has improved its contribution to the bottom line each year and is partly responsible for the organization’s favorable financial outcomes in 2013. Workforce Isabella employs approximately 1,200 people, 900 of whom are members of SEIU 1199, the health care workers’ union in New York. Union membership includes a variety of direct-care workers: aides, dieticians, cooks, housekeeping staff, social workers, therapists and others. Initially, Isabella contracted with 10-15 home care agencies to provide its home health and home care services. This arrangement made it difficult to ensure quality and maintain communication with partner agencies. To address these difficulties, Isabella soon began hiring non-unionized employees to staff its home care agencies. As the number of aides grew, the 1199 SEIU union became interested in Isabella. The organization’s aides became unionized in 2011. Isabella’s nursing home and community-based staffs are largely separate as a result of their relatively small number of interactions. CNAs seldom cross from residential to home care settings, although they may perform private-duty work on the side, if desired. However, Isabella’s use of a shared support staff across nursing home and home care groups increases cohesion between these two groups of workers. Additionally, nearly all employees across Isabella’s service lines attend the organization’s holiday parties, summer barbeques and other staff events. Sodexo • IAHSA • LeadingAge | 37 ISABELLA GERIATRIC CENTER Staff Benefits Pay rates are determined through negotiations with the union. Table 2 shows the current hourly pay rate for home health aides versus CNAs, not accounting for overtime or holiday pay. Isabella Visiting Care licensed home care agency 650 home health aides Administrative staff Supervisors and managers Table 2. Hourly Pay Rates for Home Health Aides and CNAs HOME HEALTH AIDES CERTIFIED NURSING ASSISTANTS $10.00/hr $16.50/hr $11.10/hr on weekends N/A Isabella Care at Home certified home health agency 5 supervisors 1 physical therapist per visit 1 occupational therapist per visit 1 speech therapist per visit 4 full-time field RNs 4 RNs per visit Isabella Care Management Program 3 supervisors 3 support staff 7 care coordinators 4 RN Assessors Most benefits provided to union members are determined through negotiations with the union, paid by Isabella to the union, and distributed to workers by the union. Isabella compensates non-unionized workers with the same pay and benefits as unionized workers. This helps to level the playing field for workers of both groups. Table 3 presents the benefits that Isabella’s home health aides currently receive. Staff Roles and Numbers by Service Line Isabella Adult Day Health Care 2 nurses 1 social worker 2 CNAs 1 manager 1 program assistant 3 bus monitors Psychiatric nursing or other student interns NORC Services (Latino staff members from the local community) 1 director 11 staff members 60 volunteers Isabella Health Home 1 manager 4 care coordinators UMPSI Program 1 manager/director 3 supervisors 14 case managers 1 administrative/intake worker Table 3. Current Benefits for Home Health Aides PAID TIME OFF 1 hour for every 17 hours worked HOLIDAY PAY $15-$20/hour TRANSPORTATION SUBSIDIES None, unless accompanying a client to an appointment HEALTH INSURANCE Isabella pays into a union-managed fund LIFE INSURANCE Isabella pays into a union-managed fund PENSION $2.54/aide/hour, through the union TUITION REIMBURSEMENT $2/aide/hour, through the union SUPPLIES Uniforms and protective gear 38 | Residential Provider Expansion into Home and Community-Based Services ISABELLA GERIATRIC CENTER Staff Recruitment The human resources (HR) department at Isabella’s nursing home hires all nursing home staff and supervisory and management team members. Isabella Visiting Care Inc., (IVCI) hires home health aides separately. The HR department at IVCI also hires home health aides to meet the organization’s contractual obligations with its partners, including hospice programs. The IVCI HR staff members recruit home health workers through a variety of means: Job fairs: HR staff members participate heavily in job fairs with community-based organizations, the New York State Department of Labor and other training organizations they respect. Newspaper ads: The HR department places advertisements in newspapers as needed. Training programs: Some aides are recruited after they attend Isabella training programs. The HR department selects the students who excel in the program and exhibit an ability to work independently and responsibly. Word of mouth: The largest percentage of aides is recruited through word-of-mouth recommendations stemming from Isabella’s strong reputation in the community. Even though Isabella does not pay substantially more than similar employers in its area, the organization does provide competitive pay and comprehensive health benefits. It also supports employees by writing letters of reference for apartments and providing educational, personal development and other opportunities for advancement. IVCI recruiters prefer to hire home health aides who have prior experience. They seek aides who feel a calling to the work, will perform well in the home setting, can handle challenging clients, and will maintain their professionalism in adverse situations or perhaps even when wrongly accused. During job interviews, recruiters ask experienced candidates to describe a difficult situation they faced with a client, how they managed it, and what they learned from the experience. Prospective aides with no prior experience are presented with a difficult situation and asked to role-play their response. The nursing home’s HR department uses similar interviewing techniques when recruiting candidates to fill other home care staff positions at Isabella, including paraprofessional coordinators. Recruiters do not require that coordinators have prior experience in their role. Nonetheless, recruiters have found that experience as a front-line staff member in multiple settings often helps individuals perform well in a coordinator role. Required Qualifications for Aides Nursing home-based CNAs and home health aides must meet different requirements in order to qualify for employment at Isabella. In addition to meeting training and certification requirements, nursing home aides must be able to read, write and speak English fluently, and to have a high school diploma or a GED certificate. In contrast, home health aides are not required to be fluent in English or to have a high school diploma or equivalent. Training for aides New home health aides must attend a one-day orientation that educates them about Isabella’s mission, history and general operating procedures. In order to continue working at the agency, aides are also required by New York State to undergo 12 hours of in-service training each year and to score at least 75% on annual competency exams and skills assessments administered by Isabella Visiting Care, Inc. Isabella offers free in-house training programs for home health aides and CNAs. Home health aides receive 90 hours of instruction during these training programs. This represents 15 hours more than the New York State requirement. Isabella has come to rely on the training programs as a vehicle for recruiting aides. Retention of Aides The annual turnover rate for Isabella’s CNAs is 10%. The turnover rate for home health aides is only slightly higher, approximately 12% per year. These rates tend to fluctuate with economic cycles and industry trends. Staff Satisfaction Overall, Isabella’s home health aides find their jobs rewarding and enjoy the independence that comes with their positions. This satisfaction might be linked to several factors: Isabella’s paraprofessional coordinators match home health aides and clients based on personal traits and geographical location, and frequently match aides to one or two clients to whom they provide care all week every week. This practice fosters the development of close relationships between home health aides and their clients. It also ensures the client’s conformity with the care plan. Home health aides can choose whether to continue working with clients with whom they have been matched. Aides seldom lack work. Due to demand for Isabella’s services, the paraprofessional coordinators quickly match aides to new clients when former clients no longer need their services. Home health aides acknowledge several challenges associated with their work. These include: Developing new relationships: When working with a new client, aides must strive to establish a unique bond with the client that will lead to a close relationship. Aides expressed a desire for courses that would teach them how to nurture trusting relationships with clients. Sodexo • IAHSA • LeadingAge | 39 ISABELLA GERIATRIC CENTER When working with a new client, aides must strive to establish a unique bond with the client that will lead to a close relationship. Resistance to the care plan: Some clients may demonstrate their resistance to following the care plan in a variety of ways, such as not taking their medication as prescribed. While aides are held responsible for the client’s welfare, they lack the authority to administer medications or provide skilled care. Trust issues: Clients sometimes have trust issues with aides, falsely accusing them of actions such as stealing. Aides must learn not to take such incidents personally. Family relations: Home health aides sometimes find it challenging to interact with clients’ families, as many families insist that Isabella aides provide care for them as well as the client. As a result, some aides prefer to work with clients who live alone. in accordance with those plans. As part of their oversight role, nurses are required to call clients every one to two months and to make an in-home visit every six months. Nurses are also required to make an in-person visit when aides report that clients are not following their care plans. Safety concerns: Supervisors cited safety as a major issue in their community. To ensure the safety of employees working in violent neighborhoods, supervisors send aides out in pairs and provide each aide with a telephone. They also track aides’ locations using web-based software. All care delivered by the home health aides is supervised by a nurse. These supervisors acknowledged several challenges. Turnover: The home care industry generally undergoes considerable churn. Staff members jump from agency to agency as they seek job placements that best fit their needs. This creates considerable stress for supervisors. Staff assignments: Isabella does not reimburse home health aides for their travel expenses or travel time. As a result, aides do not want to work outside the community in which they live. This can make it difficult to provide care for clients living outside the Washington Heights-Inwood neighborhoods. It also interferes with efforts to expand services to new geographic locations. Live-in requests: Supervisors find it difficult to meet the requests of some clients for live-in aides. Home health aides are not paid for time they spend sleeping in clients’ homes, and these aides often do not want to be away from home overnight. Difficulty supervising a large workforce: Nurses supervise many aides, and sometimes they do not take the time to determine that the clients’ needs are being met and that difficult clients are accepting their care plans and behaving 40 | Residential Provider Expansion into Home and Community-Based Services Perceived Challenges Executives and managers at Isabella highlighted three major challenges that they have faced during the expansion process. Effective communication: Staff members have worked hard to maintain effective communication throughout the organization. With over 1,200 employees in a variety of service lines, it has sometimes been difficult to make sure that front-line workers are adequately supervised and supported, that nurses have followed up with clients as needed, and that clients are being served in a manner true to Isabella’s mission. A related challenge has been ensuring that all staff members are adequately educated about pertinent special topics like best practices for communitybased mental health care. Isabella has addressed this challenge with in-service training sessions presented by instructors who are deeply immersed in the topic area. Managed care: Participating in managed care plans has complicated the task of providing the best care possible for clients. Every six months, for example, nursing and social workers in Isabella’s adult day health care program must administer an evaluation that takes a minimum of 45 minutes per enrollee to complete. Moreover, a client experiencing a new issue triggers the requirement to complete another 45-minute, issue-specific questionnaire to determine whether a doctor or nurse should reevaluate the client. It can be time-consuming and challenging ISABELLA GERIATRIC CENTER to complete all forms that are required so that clients with multiple health problems can be evaluated by the appropriate clinicians. Staying true to mission while adapting to changes in the health care landscape: Isabella’s mission calls the organization to provide members of the greater community with the services and supports they need to age as they wish. This usually entails remaining healthy at home for as long as possible. In cases where skilled nursing care is required, Isabella remains committed to providing the highest quality of care within its nursing home setting. The organization will be challenged as it strives to meet the needs of the community while navigating a changing operational landscape characterized by new funding sources, technological advancements and increased consumer expectations. Perceived Benefits Isabella staff members derive satisfaction from helping the community’s older adults age as they wish while, at the same time, overcoming issues that they say make their work difficult. For example, home health aides report that they derive the greatest satisfaction from developing close ties with their clients and helping them feel better physically and mentally. Yet, they also report that many clients are non-compliant with their care plans and difficult in other ways. Similarly, adult day health program employees said they enjoy helping clients improve their health and seeing corresponding declines in measures such as ER use and hospital admissions. Managers of the NORC and case management programs derived great satisfaction from learning about and working with community partners to help the older adults they serve, and making use of policy levers available to advance their causes. Isabella executives cited the pleasure they take in weathering the rapidly changing health care landscape, and being able to continue to fulfill the organization’s mission. Lessons Learned Isabella executives and managers offered the following suggestions for residential organizations that are currently expanding or considering expanding their home and community-based services: Home health aides report that they derive the greatest satisfaction from developing close ties with their clients and helping them feel better physically and mentally. Hire your own aides. To facilitate effective communication across your organization, consider hiring your own home health aides to provide this care, and consider offering training to ensure you have an ample supply of home health aides you trust. When Isabella evaluated the quality of care it was providing while contracting out services through more than 15 home health agencies, the organization concluded that it could provide better care with in-house staff. This has been confirmed in subsequent evaluations. Care for your home health aides. Provide aides with needed services, such as promptly written letters of recommendation if they request them. This will help you engender loyalty among current aides and recruit additional aides through word-of-mouth recommendations. Strive to attract and hire home health aides with prior experience. Community-dwelling older adults are older, sicker and frailer than ever before. You and your clients will want to have dependable home health aides on staff. Conduct practical job interviews. Present real-life scenarios and monitor how prospective home health aides respond. Pay attention to who “gets it” and who does not during training sessions and orientations. Trust your instincts in selecting the most qualified aides. Consider creating new career paths for your workers. Lack of growth opportunities can result in higher turnover. Isabella created positions for a Senior CNA and a Rehabilitation Coordinator in its nursing home. CNAs and other aides aspire to fill these positions. Don’t become complacent, even if your programs are running well. The health care landscape will continue evolving and communication breakdowns will occur. One executive recommended that every staff member walk onto the job each day “as if it is your first day there.” In a related point, supervisors and executives urged their counterparts at other organizations to “stay hands-on and involved.” Recognize the power of food. Provide tasty food at community events for prospective clients. They will appreciate the extra effort you made and they will return for future events. Monitor social media. Social media outlets are great marketing tools but they must be continually monitored for complaints and negative posts. If someone posts something negative on your site, determine whether there is any basis for the negativity. If there is, follow it up aggressively with an investigation and proper resolution. If there is no basis for the comment, ask the site to clear the comment. Additionally, home health aides at Isabella recommended the following: Reimburse home health aides for transportation to and from clients’ homes. This practice will encourage aides to accept distant assignments and to begin serving new locations. Sodexo • IAHSA • LeadingAge | 41 Case Study TABITHA HEALTH CARE LINCOLN, NEBRASKA | March 2015 Introduction Tabitha Health Care is a not-for-profit, Lutheran organization that delivers a comprehensive line of services to older adults living in Southeast Nebraska. Headquartered in Lincoln, Tabitha offers rehabilitation services, long-term care, assisted living, affordable senior housing, and a variety of homeand community-based services. Its three nursing homes offer palliative care, memory care, Green House living and outpatient therapy services. Its home and community-based services include: Home health care, including palliative care Non-medical home care Meals on Wheels Adult day services EngAGE Program, a full-service health care coordination program Established as an orphanage in 1886, Tabitha evolved into a nursing home in 1890, and has since expanded to provide older Nebraskans with a continuum of long-term services and supports. This study of Tabitha’s expansion into home and communitybased services was conducted through interviews with executives at the organization. Policy Context Nebraska has a multitude of very specific, sometimes conflicting and often outdated regulations governing the delivery of long-term services and supports. These regulations are generally written with the view that various care sectors within the field of long-term services and supports represent 42 | Residential Provider Expansion into Home and Community-Based Services separate industries that require their own regulations. These regulations do not adequately address the rapidly evolving field of long-term services and supports, or the need of providers in that field to offer services that span the continuum of care. The state’s complex regulatory framework has complicated Tabitha’s efforts to provide seamless care to older Nebraskans. Nevertheless, Tabitha has worked hard to transcend these limitations so it can provide a full range of innovative services. The organization has been assisted by the advocacy efforts of LeadingAge Nebraska, a state association of not-for-profit aging service providers. Expansion into Home and CommunityBased Services In 1966, Tabitha began offering home health care in the Lincoln metropolitan area. Tabitha expanded its home health services to other Nebraska counties in 1974, and now serves 28 counties. The organization began offering non-medical home care in 1982 and hospice care later in the 1980s. Tabitha’s expansion into home and community-based services was primarily mission-driven. The organization wanted to provide a continuum of compassionately delivered care to more older adults, and realized that it could reach only a small percentage of prospective clients through its residential services. The advent of Medicare in the mid-1960s helped to advance Tabitha’s mission by allowing the organization to reach a much greater number of older adults living in their homes. Tabitha launched its home health agency in 1966 to take advantage of new Medicare reimbursements. Those reimbursements, in turn, allowed Tabitha to meet the needs of a much larger clientele. The organization moved into home care delivery when it saw that many clients needed services that Medicare did not reimburse. TABITHA HEALTH CARE Many private-pay clients currently make use of both services. Despite its early reliance on Medicare reimbursements, Tabitha also has a long history of providing unreimbursed, mission-based care. This tradition continues today through a variety of service lines, including home and communitybased services. When Tabitha needs money to launch new projects or expand existing projects, it seeks help from its own foundation, other local foundations and private donors. Tabitha’s expansion into home and community-based services has not been entirely smooth, due to market competition, the challenges of rural service delivery, and lack of cooperation from other care sectors. The organization has responded to these circumstances by reorganizing its service delivery scheme to make it more efficient. For example, Tabitha initially provided home and community-based services in northern Kansas, but pulled out of the state once local providers began offering similar services. Similarly, Tabitha cut back on service delivery in northern Nebraska when Medicaid reimbursements became insufficient to support those services. Hospitals have also played a role in restricting Tabitha’s expansion. For example, physicians did not strongly support the use of hospice and home health care in David City, a city of 3,000 residents in eastern Nebraska. Tabatha’s client base in David City became too small to justify maintaining an office there. Tabitha continues to provide services in the area, however. Tabitha originally maintained three regional offices in Nebraska, but has cut back to two regional offices in recent years. Five satellite offices have helped the organization serve a large geographic area more efficiently. These satellite offices do not have full-time staff but serve as “drop sites” where the organization’s registered nurses (RN), therapists, certified nursing assistants (CNA) and personal care aides (PCA) can download client data to their laptops, pick up or return supplies, and attend regional meetings and training sessions. Description of the Program Tabitha provides regulated medical home health care through an agency called Tabitha Home Care, which was expanded in 2009 when Tabitha acquired another home health agency. The organization delivers non-medical home care through a licensed agency called Home Care Specialties of Tabitha. Partnerships Members of the Tabitha staff deliver most of the organization’s home and community-based services. However, the organization has formed partnerships with other agencies to fill geographic gaps in its service delivery. For example, Tabitha contracts out some therapy services in the northern part of the state, and in areas that are distant from Lincoln. In addition, the organization partners with other agencies, as needed, to fill service delivery needs of particular clients. Tabitha’s strongest partnership is with Bryan Health, which operates a network of hospitals in the Lincoln metropolitan area. Tabitha first partnered with Bryan in 1987 to provide skilled home health care to heart transplant patients through a program called Tabitha Bryan Special Care. Tabitha continued to support Bryan Health after that organization established its own home health agency and merged with a county hospital. When Bryan Health decided to close its home health agency in 2009, Bryan and Tabitha merged their home health care businesses, further expanding Tabitha Home Health. Most recently, Tabitha partnered with the Bryan Heart Institute to ensure that patients with congestive heart failure can safely transition from hospital to home. The goal of the partnership is to reduce preventable rehospitalizations. Sources of Reimbursement Approximately half of Tabitha’s reimbursements for skilled nursing, assisted living, and home and community-based services come from Medicaid. The other half comes from Medicare, the U.S. Department of Veterans Affairs (VA), commercial insurance, private pay and charity care. Private insurance and Medicare are the most significant payers for home health care. Tabitha has seen large increases in the number of clients using commercial insurance and in the number of reimbursements it receives from Medicare Advantage plans. Sodexo • IAHSA • LeadingAge | 43 Timeline 1886 1890 TABITHA HEALTH CARE Expanded to provide shelter to the indigent elderly. Founded as an orphanage. 1909 Expanded to provide nursing care and tuberculosis hospital services. 1960 Role as orphanage ends. 1966 Expanded to provide certified home health care. 1974 Expanded to provide home care. 1979 1982 Beginning of Tabitha Hospice. Hospice becomes Medicare-certified. 1990 Hospice expands to neighboring counties. 1997 Tabitha home care services expand geographically. 2001 Intergenerational service, providing child care, begins. 44 | Residential Provider Expansion into Home and Community-Based Services TABITHA HEALTH CARE Approximate reimbursement figures for Tabitha’s various agencies in 2014 include the following: Non-medical home and personal care: Medicaid (25%) and private pay (75%) Home health care: Medicare traditional or HMO plans (81%); Medicaid traditional or HMO plans (10%), and VA, commercial insurance or private pay (9%) Hospice: Medicare (88%), Medicaid (2%), commercial insurance (7%), and VA, private pay and other sources (less than 3%) Adult day services: Private pay (62%), Medicaid (13%) and other payer sources (less than 25%) Nutrition and lifestyle counseling Disease management education Hands-on personal care, companionship and supervision Tabitha also offers non-medical home care, including personal care, housekeeping, errands and companionship. The organization is currently licensed to deliver adult day services for up to 36 individuals per day. Tabitha hopes to expand that number to 46 clients. Currently, about 20 older adults use the organization’s adult day services on a given day. Tabitha offers the following services under its private-pay model: Admission Criteria Tabitha’s medical models of home health care follow Medicare admission guidelines. Before a client can receive services, a physician must certify that the client is “homebound,” meaning that the client finds it taxing to leave home. The requirements for non-medical home care depend on the payer source. Medicare does not pay for non-medical care and private-pay clients must meet very few requirements. Tabitha executives note that a growing number of individuals are purchasing long-term care insurance packages. These policyholders, who represent approximately 15% of Tabitha’s non-medical home care clientele, face few restrictions in accessing home care, although their plans often require them to pay a substantial portion of care costs. Long-term care insurance frequently covers only 10%-15% of the costs of nonmedical home care services. Medicaid and VA clients are subject to the greatest number of restrictions as they try to access non-medical home care services. For example: Services Each year, Tabitha provides more than 1 million service hours to clients. Its home health offerings include the following services: Skilled visiting nurses Physical therapy Occupational therapy Speech therapy Social work/case management, not including behavioral health Home health aide services Nutrition counseling Licensed practical nurse (LPN) visits to check blood pressure, set up medication boxes, etc. Registered nurse (RN) visits Certified home health aide visits Personal care attendant visits Figure 1. Payer Sources for Home Health Care Medicaid Waiver clients living in Lancaster County must be certified as needing nursing home services. This means they must have difficulties performing more than three activities of daily living (ADL) or have substantial cognitive impairment. Difficulty performing instrumental activities Figure 2. Payer Sources for Home Care 81% Medicare Medicare Medicaid Other 75% Other 9% 20 25% Medicaid 10% 0 0% 40 60 80 100 0 20 40 60 80 100 Sodexo • IAHSA • LeadingAge | 45 TABITHA HEALTH CARE Figure 3. Payer Sources for Hospice Figure 4. Payer Sources for Adult Day Medicare/ Other 88% Medicare Medicaid Medicaid 2% 13% Other 20 62% Private Pay 10% 0 25% 40 60 80 100 of daily living (IADL) can be cited as a contributing factor to the need for a nursing home level of care. VA clients must meet the same requirements that apply to Medicaid Waiver clients. In addition, these clients are eligible to receive non-medical services if they require home care while receiving hospice services, or if they have two ADL dependencies along with more than two other conditions, such as more than three IADL impairments, clinical depression, or a solitary living arrangement. Service Hours Tabitha clients living in the Lincoln metropolitan area pay a minimum charge for one hour of private-duty care. The minimum charge for private-duty care is two hours elsewhere in the state. Intense competition for highly qualified staff in the Lincoln area has made it challenging for Tabitha to provide around-the-clock services when clients need them. The city’s unemployment rate is currently only 2.4%, and competition for workers affects all industries. Maintaining sufficient staff, especially as the baby boomers age, will continue to be a challenge. Approximately 60%-70% of Tabitha’s home health and home care clients have family caregivers, but these caregivers are usually unable to stay with the care recipient around the clock. Many caregivers are adult children who live out of town. Tabitha offers respite care as a service through its private-duty, hospice and adult day services programs. Tabitha executives believe that respite services are underutilized due to cultural reasons: Nebraska’s citizens believe they are “tough” and “can take care of themselves.” Client Demographics Tabitha provided the following demographic descriptions of the older adults using its varied service lines during 2014. 46 | Residential Provider Expansion into Home and Community-Based Services 0 10 20 30 40 50 60 70 80 Home health care: About 85% of home health care clients were age 65 years or older, and more than 60% of clients were age 75 years or older. Hospice: Approximately 85% of hospice clients were age 65 years or older, and nearly 60% were age 75 years or older. Just over 55% of hospice clients were female. About 97% of hospice clients were non-white Hispanic while 3% were African American and white Hispanic. Home care: Tabitha was unsure about the demographic makeup of its home care client populations. Adult day health care: As of March 2015, 75% of adult day clients were age 70 years or older, and 33% were age 80 years or older. Almost half (48%) of adult day clients were female. Almost all (99%) were white, with African Americans making up only 1% of the client population. Almost three-quarters (70%) had mild, moderate or severe dementia. In addition: 39% paid for services privately. 11% paid privately or with long-term care insurance. 29% were covered by the VA. 14% were covered by a Medicaid waiver program. 7% were covered by a Medicaid block grant program. Non-medical home care clients: Tabitha did not have readily available descriptive statistics for its non-medical home care client population. Financial Implications Tabitha Home Health Care serves a 28-county area and averages 10 referrals per day or about 300 referrals per month. Tabitha’s Continuum Navigation division receives referrals and incorporates them into the organization’s service lines. The average daily census for home health is 254 clients. Maintaining that client level requires approximately 280 referrals per month. TABITHA HEALTH CARE Finding the right mix of clients, payers and services is a challenging endeavor for Tabitha. For example, a veteran might be referred to Tabitha for occupational therapy, which is reimbursed at $90 a visit. However, the time it takes to acquire the referral might cost $400. Tabitha must consider these factors when calculating potential revenue. Revenues from Tabitha’s hospice services are lower than hospice-related revenues that providers in other regions of the country report. Tabitha executives attribute lower revenues to a lack of comfort with hospice among Nebraska physicians. As a result, Tabitha’s average hospice stay is a very short 14-21 days. Tabitha executives believe that the quality of care at the end of life could be improved if Nebraska doctors would initiate endof-life conversations with their dying patients earlier in their illness. Quality Oversight There are two layers of quality assurance at Tabitha. External: Tabitha engages in federally required quality assurance programs that are managed by the Centers for Medicare & Medicaid Services14 (CMS). Internal quality boards evaluate the CMS-mandated data to track the organization’s accountability and progress toward achieving goals. Internal: For the last three years, Tabitha’s corporate office has evaluated quality across all of the organization’s service lines to provide a broad view of how Tabitha is performing and how it might improve. An internal Continuum Quality Group meets quarterly to determine how the organization’s different service lines impact its overall quality and to identify advantages and disadvantages of different services for clients receiving different levels of care. The group also evaluates the results of analyses and surveys conducted by outside firms. For example, SHP Consulting conducts data analytics and benchmarking for the hospice and home health care service lines. My InnerView conducts satisfaction surveys with adult day health clients. Tabitha evaluates its own private-duty home care service line. An internal Continuum Quality Group meets quarterly to determine how the organization’s different service lines impact its overall quality and to identify advantages and disadvantages of different services for clients receiving different levels of care. Workforce Nurses and therapists provide many of Tabitha’s home health services. In addition, Tabitha staffs its home health and home care agencies with CNAs and PCAs. A strong CNA pool of 60-70 full-time aides and approximately 100 part-time aides delivers private-duty care. The organization tries to hire home care aides from the communities they will be serving. Frontline staff members delivering Tabitha’s home and community-based services provide clients with private-duty care and extended-hour care ranging from one to 24 hours. Figure 5 shows Tabitha’s 2014 full-time and part-time staffing levels by role. All full-time CNAs, PCAs, therapists and nurses receive full benefits, including paid time off, health insurance, life insurance (if desired) and dental and vision benefits (if desired). Tabitha has found that aides, therapists and nurses prefer working in either a residential setting or in clients’ homes, but not usually both. For this reason, the organization maintains separate direct-care workforces for its nursing home and assisted living settings, and its home and community-based services. In contrast, these business lines share corporate, marketing, information technology and case management staff. Certification and Training Home health aides currently undergo the standard Medicare certification process, which includes a 75-hour course plus 12 additional hours of training. PCAs receive initial competency training provided by the corporate office. Staff members also receive ongoing, in-service training. In 2014, Tabitha began the practice of sending two PCAs to clients’ homes. The buddy system is designed to familiarize new aides with their clients, ensure quality, and facilitate continuity of care in the event that one aide is not available. Organizational Culture When Tabitha began offering home health care, reimbursements for the new services were plentiful and the nascent home and community-based services line was growing quickly. The organization’s nursing home served long-stay clients almost exclusively, and clients seldom transitioned from the nursing home to home care. These factors helped to create a disconnect between Tabitha’s nursing home and home health care staff. Members of the home care staff considered themselves to be “at the top of the heap” and regarded the nursing home’s staff with some disdain. Tabitha executives knew that these attitudes would make it more difficult to create a seamless experience for clients across the continuum, particularly as the nursing home began serving more short-stay clients. Nurses and aides from the different settings would need to work together to coordinate care transitions as clients moved from short-stay nursing to their homes with the support of Tabitha’s home health care services. The service lines still have a tendency to compete with one another. For instance, members of home health care staff may Sodexo • IAHSA • LeadingAge | 47 TABITHA HEALTH CARE Figure 5. Full-Time and Part-Time Staffing by Role 57% CNA 61% 3% PCA Clinical Manager 11% 14% 0% 12% 10% Therapist 46% RN 24% LPN Therapy Aides 3% 7% 3% 0% want to keep a client in need of hospice care on their roster and continue trying to meet the client’s needs at home. Tabitha’s management works to mitigate employees’ competitive urges by continually reinforcing the principle that clients’ needs come first. This effort has helped Tabitha’s management and staff work together more effectively. Although the frontline staff in Tabitha’s different service lines remains largely separate, the organization asks some nurses and aides to be available to provide 24/7 emergency services when other staff members are not available. This request, which most often affects skilled nurses who are needed for home health care, is not easy for staff members who prefer to work in their own settings. Tabitha executives acknowledge that these coverage issues could be resolved if the organization maintained a float pool of staff that could serve in any capacity. However, creating this pool would require different hiring procedures, different management styles and a more unified organizational culture. Perceived Challenges Tabitha has faced several major challenges, in addition to the workforce challenges described above. These challenges include: Rural service delivery: Nebraska’s rural nature has forced Tabitha to rethink some of its expansion plans for areas that are distant from Lincoln. The organization still finds it challenging to maintain good financial returns on rural care when its staff must spend hours driving long distances to serve clients. In addition, many rural clients want to 48 | Residential Provider Expansion into Home and Community-Based Services Full-time Part-time receive care from local, familiar home health and home care aides who they might see in church and at the grocery store. Tabitha has made an effort to hire local home care staff so its services remain competitive. Market competition for clients: While providing services in Kansas, Tabitha was crowded out of the market by a new group of local providers. Market competition for staff: The proliferation of providers has made it challenging for Tabitha to fill top staff positions across the organization. If this trend continues, outstanding staff members will be spread thinly across many organizations and there may eventually be no excellent providers in the market. Regulatory challenges: Tabitha has been affected by the multitude of seemingly unnecessary state regulations that have proliferated over the past two years. For instance, while building a new hospice center located only 900 feet from its already-certified and licensed skilled nursing home, Tabitha was required by a newly changed state statute to obtain separate certification and licensing. Fluctuating client base and revenues: Maintaining the right case mix with a constantly fluctuating client base has been challenging for Tabitha. Fluctuating revenue levels have also challenged the organization as it works with different payers and experiences unpredictable reimbursement delays. Required documentation: A physician is required to authorize all home health services. This requirement TABITHA HEALTH CARE creates so much paperwork that Tabitha employs a fulltime assistant to ensure that the organization has the documentation it needs to receive payment for physicianordered services. Tabitha also conducts regular educational sessions with physicians to ensure that every referral to home health care is accompanied by the signed document. Perceived Benefits Tabitha executives report that home and community-based services have enhanced the organization’s ability to fulfill its mission by providing high quality care across clients’ continuum of needs. Executives say they feel extremely gratified to have developed a loyal client base that turns to Tabitha for all its care needs. An adult child might seek progressively higher levels of care for a parent and then turn to Tabitha decades later to care for a spouse. Providing home and community-based services has been especially satisfying because it allows Tabitha to develop relationships with clients earlier in the aging process. Tabitha pioneered the use of case managers, now called Continuum Navigators, in its region in the 1990s. These employees quickly became central to the organization’s mission to provide care across service lines and throughout the aging process. Families appreciate knowing they can turn to the same organization, and the same continuum navigators, over a span of years. Over time, this appreciation has grown into a strong trust in Tabitha and the services it provides. Outcomes Tabitha regularly evaluates its service lines and maintains dashboards and scorecards that track key measures, such as rehospitalizations. On average, Tabitha’s clients are discharged home more frequently, and rehospitalized less often, than their peers at the city, county or state levels. Lessons Learned Throughout its expansion into home and community-based services, Tabitha has learned several lessons, including the following: Put the client first. Think of each client initially as a “blank page” whose needs and wishes you will identify and then meet. Do not make assumptions at the outset about what would be best for a given client. Maintain a diverse menu of services. Design these services to fill the variety of care needs that emerge from early in the aging process to the end of life. Partner with organizations that can fill specific gaps in your services. Pick partners who align with your business and philosophy. Make sure your partners provide the services you need and that your “business chemistry” is compatible. Operate above margin. Make sure that at least one of your service lines is operating well above its margin. This will allow you to rebalance your other services, as needed, in the face of continually changing services, regulations and reimbursements. Home and communitybased services have enhanced the organization’s ability to fulfill its mission by providing high quality care across clients’ continuum of needs. Sodexo • IAHSA • LeadingAge | 49 CONTINUING CARE RETIREMENT COMMUNITIES 50 | Residential Provider Expansion into Home and Community-Based Services Case Study BALLYCARA VILLAGE OF FRIENDS SCARBOROUGH, QUEENSLAND | March 2015 Introduction BallyCara Village of Friends (BallyCara) is a not-for-profit provider of aged care located on the eastern coast of Australia, about 44 kilometers from Brisbane. The organization is owned and operated by the Queensland Hibernian Friendly Society, a “public benevolent institution that serves the community and disadvantaged people.” Since 1983, BallyCara has been providing independent living, assisted living and nursing home care to older adults living on its Scarborough campus. Older adults living in their own homes could not access BallyCara’s services until 2011, when the organization’s senior management team decided to enhance its mission by providing services to consumers living in the community. This case study describes BallyCara’s expansion into home and community-based services through one private-pay and two government-subsidized service programs. The study was conducted through interviews with staff from the BallyCara Village of Friends. Policy Context Australia is currently reforming its aged care systems in an effort to create a better and more sustainable system and to provide older adults with more choice and better access to services. More than half of Australians who receive aged care services receive that support at home.15 As part of its reform effort, the government created the Home and Community Care (HACC) program, which is designed for older people who are able to live on their own, and do not require higher levels of care at home. Another government initiative called the Home Care Packages Program, serves individuals with complex chronic conditions who are eligible for residential aged care but want to age in the community. Home Care Packages In 2013, the Australian government replaced three separate programs that previously provided government-funded aged care services with the Home Care Packages Program. The new program offers coordinated packages of services that are tailored to meet the specific needs of individuals. The government allocates home health and community aged care packages to older adults based on their level of need, as determined through assessments conducted by the government’s Aged Care Assessment Team. The government funds the Home Care Packages Program and approves the providers who will deliver packaged services. The program has required a hefty investment of government funds: $1.2 billion (AUD) in 2013-2014 and $1.3 billion (AUD) in 2014-2015. Aged care organizations are approved to provide services through the Home Care Packages Program and they must participate in an annual bidding process called the Aged Care Allocation Rounds. The bidding process enables prospective and existing approved providers of aged care to apply for Australian Government funded age home care packages, and/or financial assistance in the form of a capital grant. The program is designed to control the supply of packages by allocating a fixed number of packages to various regions throughout the country. The Home Care Package bidding process is extremely competitive. There is no guarantee that an approved Sodexo • IAHSA • LeadingAge | 51 BALLYCARA VILLAGE OF FRIENDS organization will actually receive an allocation of packaged services that it can provide directly to consumers. If an approved provider does not receive an allocation, it can only deliver packaged services in partnership with an approved provider that received a package allocation. The Home Care Packages Program will change significantly in July 2015 when all packages must be delivered in accordance with a Consumer Directed Care (CDC) framework. The Australian Government is making this change because it believes that consumer-directed care represents a more sustainable and affordable model. The CDC framework is designed to empower consumers by allowing them to decide what types of care and services they will access, and how, when and by whom those services will be delivered. In addition, the CDC model gives consumers a personalized budget containing information about available funding and how the money is being spent. Providers can help consumers develop their care plans and individualized budgets. All Home Care Package providers will have to convert existing packages to the new CDC framework by July 2015, if their services are not already consumer-directed. This will involve changing long-standing delivery systems and staffing patterns. BallyCara will have less trouble than most providers in adapting to the new requirements because the organization designed its service model for the Home Care Packages Program knowing that the CDC framework for service delivery would be required. Reimbursement Rates Government reimbursement rates for home care are fairly consistent. However, the number of Home Care Package allocations can fluctuate. Until now, providers that have longstanding relationships with government agencies have had the advantage when the packages are allocated. It remains to be seen how pending legislative changes to the aged care system will impact this arrangement. Expansion to Home and CommunityBased Services In 2011, BallyCara’s senior management team began exploring the possibility of enhancing the organization’s mission by providing services to consumers living in the community. Community care services became part of BallyCara’s strategic plan after the organization’s management team spent several years discussing possible service models. BallyCara’s expansion into home and community-based services was spurred, in part, by the government’s new emphasis on home care, and its willingness to fund that care through new and expanded programs, including governmentsubsidized Home Care Packages. BallyCara’s leaders felt that the organization could leverage increased government support to fulfill its mission to reach more clients in the community and become a “one-stop shop” for consumers. 52 | Residential Provider Expansion into Home and Community-Based Services The BallyCara management team had little hesitation about diversifying the organization’s service lines, given the potential benefits they anticipated. However, some BallyCara board members expressed concern about how the community-based service line would impact the organization’s residential options. These board members worried that older adults would not use BallyCara’s residential care options if they could access services and supports while staying in their own homes. Board members had several other questions about the proposed community services program: How would BallyCara implement the expansion program? What level of investment would be required to build the service line’s infrastructure and workforce? How would the new program impact BallyCara’s existing residential services business model? How would the new service line affect BallyCara’s brand identity? The decision to diversify BallyCara’s service line was made jointly by the board of directors and management, with the ultimate decision coming from the board of directors. The management team—including the chief executive officer, director of aged care, and quality manager—focused on integrating BallyCara’s new home care model with the organization’s other services so an expansion into home and community-based services would not compromise existing services. This integration process involved the development of new operating systems and new staffing models for the at-home programs. BallyCara launched its home and community-based services program, called BallyCara Community Care, in October 2013. The rollout had several steps: During the first phase of the expansion, BallyCara Community Care offered social and personal care services to on-campus residents, but not to individuals living in the external community. All the on-campus services were private-pay. Next, the program offered short-term housing and support to disadvantaged people living in the external community. These services were provided through outside funding or other charitable organizations. BallyCara then applied for and received permission from the Australian government’s Department of Social Services to launch the Home and Community Care (HACC) program. HACC provides at-home services to older people who are able to live on their own, and do not require higher levels of care at home. BallyCara launched HACC in 2014. BallyCara received approval to participate in the Home Care Packages Program, which serves individuals with complex chronic conditions who are eligible for residential aged care but want to age in the community. The organization is now waiting to receive allocations from the government so it can begin directly delivering Home Care Packages to older adults living in its community without working with a partner provider. Timeline BALLYCARA VILLAGE OF FRIENDS 1983 Began as a retirement community in Queensland, Australia. 2011 Decision by management team to provide services in the community. 2013 Added home care: Social and personal care services to clients residing on the campus. 2014 Received government approval for the Home and Community Care program, but still awaits allocation from the government to administer the program independently. Sodexo • IAHSA • LeadingAge | 53 BALLYCARA VILLAGE OF FRIENDS BallyCara Community Care faced some initial challenges as it rolled out its community services program. Key challenges were associated with the need to: Invest in the community services program before the program generated revenues Hire qualified staff members who had experience in the home environment and understood the relationship between the residential and home care models Brand the organization as both a community care provider and a residential care provider Description of the Program The BallyCara board of directors approved a strategic plan that included the development of three community care services for BallyCara: A private-pay Personal Services program The Home and Community Care (HACC) program The Home Care Packages Program Services are generally provided Monday through Friday. BallyCara offers limited evening and weekend services. The organization provides around-the-clock coverage to residents on its campus through an emergency call system. On-site staff members respond to the calls and provide medical attention as required. Personal Services BallyCara’s fee-for-service Personal Services Program is customized to the individual consumer and offers more control, choice and flexibility than government-subsidized programs. BallyCara offers a range of home and communitybased services through this program: 54 | Residential Provider Expansion into Home and Community-Based Services Personal care, including assistance with showering, dressing and medication monitoring Domestic assistance, including house cleaning and laundry assistance Home maintenance, including minor general repair and care of the house or yard Home modifications like alarms, ramps and support rails Transportation to attend appointments, shop and engage in social activities Center-based adult day programs offering social activities in a community setting Social support, such as offering companionship or taking people shopping or to appointments Home and Community Care (HACC) Providers in the government-subsidized HACC program assess consumers to ensure they are eligible for the program’s specific set of approved services. The non-clinical (non-medical) services offered through HACC include: Domestic assistance, including help with routine household tasks like gardening or maintenance Social supports, including transportation to social activities and shopping, which help older people maintain their independence, health and well-being Center-based adult day programs, including small group activities that take place either every day or several times a week BallyCara may be able to provide additional services to HACC clients, as needed. Those services would be paid for with HACC funds for a short period of time or through the privatepay Personal Services program. BALLYCARA VILLAGE OF FRIENDS Home Care Packages The government-subsidized Home Care Packages Program offers support services and case management services to support a full range of care needs, from basic to high-level. The coordinated package of services includes: Personal care, including help with showering or bathing, dressing and mobility Support services, such as washing and ironing; house cleaning, gardening, basic home maintenance, home modifications related to the care needs; and transportation for shopping, medical appointments and social activities Allied health supports, including physiotherapy, occupational therapy, physical therapy, services of a dietitian, and hearing and vision services Four levels of Home Care Packages meet different ranges of care needs: Level 1: Basic care needs Level 2: Low-level care needs Level 3: Intermediate care needs Level 4: High-level care needs Older adults receiving care under a Home Care Package sign a Home Care Agreement with their home care provider. The agreement identifies the care and services the consumer will receive. The government makes payments directly to the home care provider. The provider spends these funds on the service package described in the Home Care Agreement. Funding Challenges: BallyCara had an opportunity to obtain funding for the Home Care Packages Program in 2013 when the Australian government opened up the bidding process in an effort to expand the availability of home care services throughout the country. In prior years, it was difficult for new providers to enter the program. The Australian government’s Department of Social Services has recognized BallyCara as an approved provider of Home Care Packages since 2014. However, BallyCara cannot deliver Home Care Package services directly to older consumers because it has been unsuccessful in obtaining Home Care Package allocations during the annual Aged Care Allocation Rounds. The organization plans to apply for an allocation during the next bidding round. In the meantime, BallyCara Community Care provides home care and case management services through formal agreements with other approved Home Care Package providers that have received the government allocations in its region. BallyCara may have a new opportunity to deliver Home Care Package services in 2017 if the government approves a legislative proposal allowing approved providers to deliver Home Care Package services without the need for an allocation. There is no certainty that the provision will be approved. If it is, it could open new opportunities for BallyCara. Clinical Care BallyCara focuses exclusively on providing non-clinical care in the community. If BallyCara receives an allocation of Home Care Packages, it may begin providing the clinical care component of the Home Care Packages Program. The move into home health care would bring with it more government oversight of service provision and staff training, and would require BallyCara to extend its service hours to include evenings and weekends. These requirements would add to the cost of providing clinical care services. Partnerships The Personal Services and HACC programs are operated as service lines under the umbrella of BallyCara’s parent organization and use in-house staff. BallyCara also works as a subcontractor for a local Home Care Package provider that has received a government allocation. BallyCara also has an arrangement with a community organization that serves homeless older adults. BallyCara helps the organization’s clients transition to different levels of housing, depending on their needs. For example, the organization might help some clients move to a nursing home or receive palliative care. In addition to these “formal agreements” with external agencies, BallyCara has less formal arrangements with referral groups and health networks. These collaborations create important connections that will eventually give BallyCara the opportunity to deliver services in different regions, to serve clients of other residential care providers, and to identify educators who can train BallyCara staff to provide direct care to clients. Sodexo • IAHSA • LeadingAge | 55 BALLYCARA VILLAGE OF FRIENDS Sources of Reimbursement BallyCara’s Personal Services program is entirely private pay. The organization receives federal reimbursements from the Department of Social Services (Aged Care) for services delivered through the HACC and Home Care Packages Program. Even though the Australian government subsidizes the HACC and Home Care Packages Program, these programs still require that care recipients pay something for the services they receive. Most clients in the HACC program pay a small fee for each service they receive. The fee amount, agreed upon by the individual and the service provider, depends on the individual’s income and the type and number of services requested. This fee helps cover staffing and equipment costs. Recipients of Home Care Package services also pay a basic fee. The fee might be calculated as a percentage (17.5%) of the basic Age Pension for an individual. Low-income clients may pay an income-tested care fee featuring annual and lifetime caps. Once consumers reach this cap, they cannot be asked to pay any more income-tested care fees. Eligibility Personal Services: The Personal Services program does not have any eligibility requirements. HAAC: The HACC program requires an assessment by the service provider. In addition, eligible consumers must: Be age 65 or older (50 years and over for Aboriginals and Torres Strait Islanders) Live in the community Have difficulty performing activities of daily living (showering, house cleaning, meal preparation, shopping, etc.) due to functional limitation Demonstrate that their capacity to live independently in the community is at risk Not have access to a Home Care Package Not live permanently in a residential care setting Home Care Packages: Access to the Home Care Packages Program requires an assessment by a member of the Aged Care Assessment Team to determine if the individual is eligible to receive government-subsidized aged care services. The assessment for an approved individual will identify the types of services the individual can receive. The assessment also will determine which level of package the individual will receive. Clientele BallyCara Community Care serves approximately 200 clients across all service lines and averages 428 service hours each month. The number of clients has increased significantly over the past year, mostly because of BallyCara’s participation in the HACC program. BallyCara added 100 clients in 2014 and expects similar gains over the next 12 months. Half (55%) to three-quarters (70%) of BallyCara Community Care clients come through the HACC program while only about 10% of clients come through the Home 56 | Residential Provider Expansion into Home and Community-Based Services Care Packages Program. The remainder of BallyCara’s clients (20%) receives services through the Personal Services program. Client demographics are varied. The average age of all clients receiving some type of home and community-based services is 83. Seventy percent of these clients are women. Clients in the Personal Services program have the financial capacity to pay for services. In contrast, HACC clients represent a lower socio-economic group and have greater demographic diversity. BallyCara staff members were not sure what percentage of clients has access to family caregivers. The majority of clients either does not have a caregiver or has a family member accessing services on behalf of the individual. Quality Assurance BallyCara Community Care has a robust quality assurance system to ensure that its community services programs meet the highest standards. As BallyCara expands into other regions, the organization will need to enhance its systems to ensure quality in the wider geographical area. The organization’s quality improvement initiatives drive continuous improvements of its programs. Those initiatives include the following: The organization’s technology infrastructure allows staff members to obtain and update information about clients. This improves communication about the individual among staff members. A committee of the organization’s leaders reviews data from client and family feedback surveys and manages the process for acting on the findings. Support advisors coordinate and assist aides who work in clients’ homes. These advisors also interact with clients to ensure they are satisfied with their services. Management supervisors, who oversee the support advisors, seek feedback from clients to ensure their satisfaction with services and staff performance. Advertising/Promoting Services in the Community BallyCara has stepped up the promotion of its services in the past year. The organization works with private health networks to gain referrals and to drive collaboration and innovation that will improve health and wellness outcomes in the community. BallyCara faces ongoing challenges as it tries to engage with and educate consumers. For example, educating consumers about the Consumer Directed Care (CDC) framework is critical to enhancing consumer understanding of the Home Care Packages Program. The Australian Government has relied on its website to communicate with consumers about CDC. However, many consumers still do not understand the new framework. BallyCara holds information sessions for consumers and has initiated oneon-one discussions to educate consumers about this new feature of the Home Care Packages Program. The organization’s goal is to inform consumers about the services available to them and help consumers gain access to those services. BALLYCARA VILLAGE OF FRIENDS BallyCara relies primarily on its own staff and rarely uses contract staff. Contract staff, when needed, are hired on a shortterm basis to fill a staff shortage related to an aide’s absence or an unexpected growth in the number of clients. Aides receive personal and professional development opportunities as their primary benefit. The supervisory team includes a full-time manager and two part-time support advisors. The organization is in the process of establishing a supervisory role for advisors. The advisors may provide onsite monitoring of aides twice a year while introducing mechanisms for clients to contact the support advisor and manager with questions or concerns. The team is exploring the pros and cons of placing an advisor in a client’s home for the sole purpose of monitoring the aide and assuring quality staff performance. Team members are looking at ways to support quality through other avenues, such as training sessions and regular team meetings. BallyCara Community Care strives to provide a single point of contact for clients as a way to establish trusting relationships between aides and clients and allow aides to understand the needs and preferences of clients. Financial Implications Initially, BallyCara did not receive government funding for services it provided and was required to make an investment of about $200,000 (AUD) in its community care service line. Government funding offset a similar investment by the organization in the second year of the program. During the last few years, BallyCara’s investment has increased to $400,000 (AUD). Funding from the Australian Government offset those costs. BallyCara’s community care services were operating at a surplus within a year after their launch. The organization’s leaders are satisfied with how the programs are tracking in terms of revenue generation. They anticipate the private-pay Personal Services Program will continue to grow. Workforce BallyCara Community Care employs eight permanent, part-time aides and three supervisors. Some employees are unionized, but the majority are non-union workers. The unions have little impact on the organization. Staffing Across Service Lines Aides and supervisors serve both on-campus residents and off-campus clients who require at-home services. BallyCara Community Care strives to provide a single point of contact for clients as a way to establish trusting relationships between aides and clients and allow aides to understand the needs and preferences of clients. Aides work either in the residential setting or the home care setting and do not move across settings. Most of the community services staff have been new hires and were not redeployed from BallyCara’s residential setting. However, two staff members who were hired from the residential care setting have been reliable and strong performers. BallyCara’s community services and residential care business lines each have their own management teams, but share corporate staff, including staff working in quality management, financial management, billing, human resources, and information technology. Staff Training BallyCara seeks to maintain the competence of staff through in-house trainings. The organization holds regular meetings with senior staff and regular training for aides. New legislative requirements to incorporate a Consumer-Directed Care (CDC) framework into the Home Care Packages Program will require intense training so staff members can conform to the CDC requirements, manage client agreements and understand how to deliver consumer-directed care. BallyCara’s residential staff and home care staff have numerous opportunities to interact and engage with each other. Interviewees report that interactions between managers of both business lines are more effective than interactions among direct-care staff. Managers from both service lines connect with one another during senior staff and organization-wide meetings. Aides from home care and residential care interact during an initial orientation session, mandatory annual training sessions, and all-staff meetings. BallyCara continues to develop opportunities for staff members to engage and share information. Sodexo • IAHSA • LeadingAge | 57 BALLYCARA VILLAGE OF FRIENDS Workforce Challenges BallyCara Community Care’s key workforce challenge has been recruiting the “right” people and providing enough work hours to attract and retain new staff. Home care aides must be comfortable working independently in a person’s home and with less supervision. Similarly, supervisors must be able to trust aides who work most of their hours without direct oversight. Other workforce challenges include the following: Need for a variety of skills: The work of aides is primarily domestic in nature. BallyCara is able to find prospective workers who have the qualifications for this domestic work. However, as BallyCara Community Care begins delivering higher levels of care to people in the community, it will need staff members who can provide clinical and personal care, perform domestic household chores and provide clients with social interaction. Offering challenging work: Most aides would prefer to carry out work tasks that are more challenging than the domestic work they currently perform. These staff members would like to perform clinical care. However, this is not currently allowed. Scheduling: It is important to provide staff with enough hours to entice them to remain with the organization. This can be challenging in the home care environment, where schedules are often unpredictable. For example, BallyCara Community Care may need to reduce an aide’s work hours when a client no longer requires services or is hospitalized. BallyCara invests significant time in the screening and interviewing process it uses to recruit and select aides and ensure they are a good fit for their role. The Human Resources officer conducts the initial screening for prospective employees. The Director of Community Services and the Community Service Manager then conduct in-person interviews and reference checks. Once an aide is hired, BallyCara provides supervision and a support network for the new recruits. Organizational Culture Even though BallyCara’s community services program initially blended with the parent corporation’s organizational culture, the management team still struggled to ensure that the home care workforce was engaged with the rest of the organization. Team members recognized that the community care workforce needed its own identity. The nature of home care work, which involves less teamwork and less supervision, was different than the nature of work for BallyCara’s residential care staff. BallyCara decided to provide the community services team with its own building adjacent to the main site. Home care aides also have their own uniforms and receive recognition for their accomplishments from BallyCara. However, BallyCara still works to engage the home care team in the larger organization. The differences between the home care environment and residential care environment will continue to be a challenge as BallyCara expands its community services program to other regions. 58 | Residential Provider Expansion into Home and Community-Based Services For many years, BallyCara’s mission statement was based on residential care policies and language. The BallyCara management team rewrote the mission statement when the organization began delivering at-home services. The new statement references home care, and reflects the organization’s growing range of services. The home care management team communicates with staff across service lines and updates them about the organization’s work in the community and its range of services. BallyCara uses its website and other communication tools to keep employees informed of each service line’s activities. The website also provides a forum where staff members can exchange information. Perceived Challenges Market competition, for both private-pay and governmentfunded services, is the greatest challenge facing BallyCara as it tries to operate and sustain its community services program. This competition affects BallyCara on several levels: Diversification is common: It is not uncommon for Australian residential service providers—both not-forprofit and for-profit—to diversify their service lines by expanding into community care services. This competition makes it difficult to grow the BallyCara client base. Expansion in other geographic areas: Competition will also be a factor if BallyCara rolls out its community services in other regions. In order to accomplish this goal, the organization’s executives will have to enhance internal structures and communication platforms and identify gaps. It will also have to find ways to establish a brand identity in a larger geographic area. Allocation of Home Packages: Even though it is an approved provider in the Home Care Packages Program, BallyCara has not been able to obtain any of the Home Care Packages allocated by the government. As a result, it can only participate in the program through partnerships with other providers. Balancing reimbursements: BallyCara strives to balance its privately funded services with its government-funded services. The organization is considering whether it should focus on expanding its private-pay Personal Services program. The Australian Government controls the supply of providers in its subsidized programs and is slow to approve eligibility for its shrinking service packages. This suggests that consumers will need to pay out-of-pocket for a growing number of services. In addition, clients may receive certain types of at-home services more conveniently from the private market than through the government assessment and approval process. BallyCara wants to be positioned to take advantage of private-market opportunities that will supplement its government-funded services. BALLYCARA VILLAGE OF FRIENDS By providing a range of services, BallyCara is a “one-stop shop” for consumers seeking to meet aging-related needs. Perceived Benefits Despite the challenges described above, BallyCara executives have found it beneficial and rewarding to provide community services. These services help the organization support more older adults and form relationships with more clients throughout the continuum of care. By providing a range of services, BallyCara is a “one-stop shop” for consumers seeking to meet aging-related needs. Staff members are familiar with the individual’s values and service preferences. This enables BallyCara to tailor its services to the needs of the individual. Outcomes BallyCara has not conducted any formal evaluations of its programs. Its community care programs continue to grow. These services lines allow the organization to help many more older adults and their loved ones. As BallyCara expands into the private market with its community services program, it has the potential to earn revenues to support the program. BallyCara is looking to design a system to evaluate its community services program. The organization plans to involve different community groups, such as families of prospective clients and stakeholders, in this process. Lessons Learned BallyCara executives offer the following suggestions for residential service providers that are considering expanding into home and community-based services, or are beginning the expansion process: Establish a network. Before you put any services in place, establish referral and partnership networks that will help you develop and implement your plans. Networks and referral channels are essential to building a client base. In Australia, home care providers collaborate more than residential providers do. Residential providers are reluctant to work together and exchange information. Maintain your brand identity. BallyCara executives spent considerable time thinking about how the organization’s dual role as a community care and residential care provider should be presented to consumers. They decided to reinforce the parent corporation’s brand by clearly identifying the different service lines that now come under the organization’s umbrella. The management team continues to review this strategy, particularly as the organization expands the geographic reach of the community care program. Keep staff informed. Educate and communicate with staff early in the expansion process. Staff members should be informed about what home care is and how an expansion into home and community-based services will benefit the organization, its workforce and community. Educate consumers. Host well-run informational sessions for consumers and back up oral presentations with written materials. Web-based advertising is less useful with older adults. BallyCara executives spent considerable time thinking about how the organization’s dual role as a community care and residential care provider should be presented to consumers. They decided to reinforce the parent corporation’s brand by clearly identifying the different service lines that now come under the organization’s umbrella. Sodexo • IAHSA • LeadingAge | 59 Case Study FIRST CHOICE Virginia Mennonite Retirement Community Bridgewater Retirement Community Sunnyside Retirement Communities HARRISONBURG, VIRGINIA | April 2015 Introduction Three independently operated aging services organizations in central Virginia have expanded their home and communitybased services by jointly purchasing an existing home health and home care agency called First Choice. The not-for-profit, faith-based partners include: Virginia Mennonite Retirement Community (VMRC) is a continuing care retirement community (CCRC) offering independent living, assisted living, memory support and dementia care, and a “complete living care” option that delivers long-term care services in a “home-style community-within-the-community.” Established in 1954, the Harrisonburg-based VMRC also provides health services, including a wellness center, community health center, outpatient therapy and transitional rehabilitation care. Bridgewater Retirement Community (Bridgewater) is affiliated with the Church of the Brethren and offers independent living, assisted living, memory care and skilled nursing care to adults 55 and older. The CCRC, based in Bridgewater, was founded in 1965. Sunnyside Communities (Sunnyside) owns and operates not-for-profit CCRCs in Harrisonburg, Martinsville and Summit Square. Founded in 1912, the organization offers independent living, assisted living, memory care, health care and therapy services. It is affiliated with the Presbyterian Church. 60 | Residential Provider Expansion into Home and Community-Based Services VMRC and Bridgewater purchased First Choice in 2007. Sunnyside joined the partnership in 2015. Senior Options, a limited liability corporation associated with Westminster-Canterbury on Chesapeake Bay in Virginia Beach, provides technical assistance and consulting services to First Choice. Westminster-Canterbury also operates its own home health and hospice service in Hampton Roads, VA. This case study describes the home and community-based services program operated through the VMRC-BridgewaterSunnyside partnership. This study was conducted through interviews with executives at the three CCRCs, Senior Options and First Choice. Policy Context The Commonwealth of Virginia administers a certificate of need program designed to regulate the number of beds in hospitals and nursing homes and create a balance between the level of need in a region and the number of providers who are allowed to enter the market. Home health care in Virginia is not regulated by the commonwealth’s certificate of need program. This lack of limits on the number of home health providers might be expected to facilitate the process that home health providers must follow to enter the market. However, the licensing system still experiences delays, making it difficult for an organization to launch a home health or home care business. Timeline 1912 FIRST CHOICE Sunnyside Communities begins operations. 1954 Virginia Mennonite Retirement Community is established. 1965 Bridgewater Retirement Community is founded. 1977 First Choice home care and home health agency begins operations. Mid-2000s 2007 VMRC and Bridgewater jointly decide to expand into home and communitybased services and work with Senior Options to assess the best approach to entering the market. VMRC and Bridgewater jointly purchase First Choice. 2015 Sunnyside joins the VMRCBridgewater joint venture. Sodexo • IAHSA • LeadingAge | 61 FIRST CHOICE Expansion into Home and CommunityBased Services About a decade ago, Bridgewater and VMRC were each considering options that would allow their organizations to expand service delivery beyond their campuses. Even though they were competitors, the presidents of both organizations decided to work together to diversify their business lines. They reasoned that a joint venture made sense for the organizations, which had similar missions and cultures, as well as a shared desire to provide a continuum of services and supports to oncampus and off-campus residents through one entity. Bridgewater and VMRC engaged Senior Options, a third-party consulting firm, to assess the feasibility of each organization establishing its own home health agency. The assessment identified several barriers to such an endeavor, including: Potential financial losses Fierce competition in a crowded market As an alternative, VMRC and Bridgewater decided to purchase an existing agency that already had a market share and a reputation for delivering home health care. When the First Choice home health agency came up for sale in 2007, Bridgewater and VMRC formed a joint venture and purchased the agency. The Harrisonburg-based First Choice, established in 1977, was a Medicare certified agency16 that provided skilled home health care to a large private-pay clientele. Purchasing the agency meant that VMRC and Bridgewater could start providing services immediately. Sunnyside joined the joint venture in 2015. Reasons for Expansion and Growth VMRC and Bridgewater had similar reasons for wanting to expand into home health and home care services. Both organizations wanted to: 62 | Residential Provider Expansion into Home and Community-Based Services Extend their reach to individuals who would never move to their campuses but needed support to age in the place they called home Provide services, as part of a continuum of care, both oncampus and off-campus Diversify their business models and create additional revenue streams Establish relationships with community-dwelling consumers who might consider moving to the retirement communities when they required higher levels of care Sunnyside’s leadership also wanted to take advantage of the market demand for at-home services to add to its revenue streams. The organization initially weighed three options: establishing its own agency, buying an existing agency, or affiliating with an organization that was already operating an agency. The Sunnyside leadership team decided that partnering with VMRC and Bridgewater was its best option for two reasons: Sunnyside expected that the process to start its own certified home health agency would be expensive and could take up to a year. Sunnyside’s leadership wasn’t sure there were enough potential clients in the external community to justify an investment in its own agency. Description of the Program Services Provided Today, First Choice is a for-profit limited liability corporation with its own offices. It offers a broad range of in-home services that are paid for by Medicare,17 commercial insurance and individual consumers. The agency is Medicare-certified to serve individuals in four counties in central Virginia. It provides: Skilled home health care covered primarily by Medicare and some commercial insurance Non-clinical home care that is exclusively private pay FIRST CHOICE Non-medical services include: Bathing and dressing assistance Walking and exercise activities Eating assistance Meal preparation Medication reminders Transportation for errands, medical appointments and social outings Respite care House cleaning Laundry Linen service Dry cleaning drop-off and pickup Grocery shopping Assistance with entertainment Consumers who do not require hands-on personal care can also receive services that provide companionship and assistance with chores, in addition to the non-medical services listed above. Medical home care services include, but are not limited to: Skilled nursing Physical therapy Occupational therapy Speech therapy Medical social work Home health aide First Choice provides around-the-clock home care and home health care services. Home health care clients are not required to receive a minimum number of service hours per visit. However, consumers using home care services must receive at least two hours of services per visit. The agency provides 24hour coverage in shifts. Partnerships The VMRC-Bridgewater-Sunnyside collaboration represents the primary partnership associated with First Choice. First Choice was licensed to provide Medicare-certified home health when it was purchased by VMRC and Bridgewater. However, the agency provided little skilled care because it did not want to compete with local hospitals that were providing these services. The First Choice purchase offered VMRC, Bridgewater and Sunnyside the opportunity to offer home The residential and community-based service lines in each organization must meet the same expectations for quality and follow the same approach to providing consumer-centered care. skilled care with a business partner that had experience providing the service and had the required license. The partnership faced initial challenges associated with the effectiveness of First Choice’s leadership and operations. To address these issues, the partners engaged Senior Options to provide technical assistance to the agency. Since 2014, Senior Options has offered billing, clinical, financial, marketing, regulatory and operational support to help strengthen First Choice and make it successful. VMRC, Bridgewater and Sunnyside work well together, primarily because their cultures are so well aligned. First Choice has become embedded into the culture of its three partners. Leaders of all three organizations report that their expansion into home health did not require any changes to their corporate cultures. The residential and community-based service lines in each organization must meet the same expectations for quality and follow the same approach to providing consumer-centered care. The only difference is that each organization’s care philosophy has been extended to consumers in the community and is no longer limited to on-campus residents. Consumer Eligibility Consumers can receive Medicare home health care from First Choice if that care meets these eligibility guidelines: A physician must order care. The individual must be homebound, which means he or she leaves the home infrequently and with great effort. Care is provided on an intermittent basis. A skilled health care professional, such as a nurse or therapist, provides care. There are no eligibility requirements for home care, apart from the ability to pay for the services. First Choice conducts an in-home assessment to determine the individual’s need for specific home care services and to customize the care plan. First Choice Clientele First Choice provides home health and home care services to clients on CCRC campuses and to clients living in the external community. A majority of community-based clients has a family caregiver, although that person may not be the best provider of care. Less than 15% of community-based clients live alone and do not have a family member or friend who acts as a caregiver. Home care clients: First Choice provides approximately 4,000 hours of home care service each month. This number has dropped recently due to client deaths or moves to nursing homes. The majority of private-care clients live on the CCRC campuses. First Choice accepts one or two new clients per month, although that number varies. The agency serves a broad range of short-term and long-term clients. Many clients have received home care services for many years. Most clients can afford to pay for services. Sodexo • IAHSA • LeadingAge | 63 FIRST CHOICE Home health care clients: First Choice’s average daily census includes 65 to 70 home health care clients. The agency averages 375 new home health care clients each year. Two-thirds of home health care clients reside in the external community and onethird live on a CCRC campus. The number of on-campus clients may change with the addition of Sunnyside to the partnership. Most home health care clients are white and reside in a rural area. More than a third (35%-40%) are middle income or above. Quality Assurance First Choice is committed to ensuring that it maintains high quality standards and reliable services. The agency uses the following strategies to ensure quality. Patient satisfaction surveys: A third-party organization conducts satisfaction surveys when home health care clients are discharged from the program. First Choice started conducting patient satisfaction surveys for home care clients in March 2015. The surveys are reviewed on a monthly basis. The agency plans to conduct follow-up phone calls with clients to identify issues that should be addressed. Key indicators: The First Choice administrator and her team have developed key indicators to measure quality in home care. Indicators include missed visits, late visits, hours that the agency cannot provide home care, and complaints. The administrator reviews the data and develops plans to address any issues. Data tracking: The Centers for Medicare & Medicaid Services14 requires Medicare-certified home health agencies to collect and transmit data for all adult patients whose care is reimbursed by Medicare or Medicaid. The data include two types of measures that are used to guide quality and performance-improvement measures. Processof-care measures assess how often First Choice provides the recommended care and the rate at which the agency uses specific evidence-based processes of care. Outcomesof-care measures assess how well the home health agency helps clients regain or maintain their ability to function. First Choice tracks these measures on a monthly basis as part of its overall quality-improvement process. When numbers are unfavorable in specific areas, the leadership team develops an action plan to improve the score. Typically, this is achieved through staff training. The agency also uses outcomes data in its marketing campaigns. Supervision of aides: Supervisors speak with clients and their family members about the care they receive from staff. Complaints about home care go to the agency’s scheduling coordinator and, if not resolved, are sent to the administrator for assessment and resolution. Complaints about home health care go directly to the administrator. Record review of client’s charts: Nurses and therapists at First Choice conduct a quarterly review of the client charts maintained by other staff members. If nurses and therapists have trouble finding documentation, the leadership team develops an action plan to improve quality. Marketing First Choice employs many strategies to spread the word about its home health and home care services. The agency has an outreach coordinator who works to establish relationships with community members and promote First Choice services. The outreach coordinator uses the following avenues to promote the agency: Meeting with on-campus residents during weekly transition meetings at each CCRC Attending community events like health fairs and visiting nursing homes to raise awareness of the program Networking to gain referrals from hospitals, doctor’s offices, assisted living communities and other organizations not affiliated with the CCRCs Maintaining an up-to-date website and using social media to disseminate information about the program and gain referrals VMRC, Bridgewater and Sunnyside have integrated home health care services into their marketing efforts and discharge processes. When a client is discharged from one of the CCRC’s nursing homes and requires home health care, the organizations are able to connect them to First Choice. The CCRCs also provide residents with a list of other agencies in the area, but promote the fact that they own First Choice. Financial Implications The initial investment to purchase First Choice was $500,000. Workforce First Choice employs approximately 50 staff members, most of whom are part-time. The agency contracts with its CCRC partners when it needs the services of a therapist. First Choice staff members include: Administrator Scheduling coordinator 40 home health and home care aides Health information coordinator Outreach coordinator Approximately five registered nurses (RN) Office manager First Choice consistently assigns two to three aides to care for each client. This ensures that the client will become comfortable working with several caregivers, rather than relying on only one aide. 64 | Residential Provider Expansion into Home and Community-Based Services FIRST CHOICE First Choice consistently assigns two to three aides to care for each client. This ensures that the client will become comfortable working with several caregivers, rather than relying on only one aide. This arrangement helps prevent client anxiety when an aide is unable to provide care. RNs supervise the home care aides by accompanying them on visits to clients’ homes and observing the delivery of care. The aides are supervised in this way at least every 60 days. RNs or therapists supervise the home health aides. Medicare requires that aides be supervised every 14 days or less. Staff Benefits All full-time aides receive health, dental and vision insurance coverage and retirement benefits. Staff Recruitment and Training Aides who work in home care have a vastly different experience than aides working in residential settings. An aide who prefers working independently will be attracted to the home care setting, while an aide who prefers working with others will be drawn to residential care. For this reason, First Choice home health aides work separately from the aides who work in residential settings at the CCRCs. Movement across settings is rare. Home health aides must be certified nurse aides and are required to participate in 12 hours of in-service training per year. Aides who provide skilled care receive more training than aides who provide home care services. Home care aides can be certified nursing assistants (CNA), but it is not a requirement. Ideally, the candidate will have prior home care experience. The agency will provide training for home care aides who do not have experience in the home setting. Home health aides and home care aides receive monthly inservice trainings that are scheduled during work hours. Annual training on some topics is required. First Choice used to train certified and non-certified home health aides together. Now, the agency conducts separate training for home health and home care aides. While the home health workforce is stable, the home care workforce has a high turnover rate. Home care aides lack the commitment of home health aides, possibly because home health aides tend to fill full-time positions and receive higher pay. The turnover rate among home care aides could make it difficult for First Choice to meet the demand for home care services. Offering benefits to full-time aides has helped raise their commitment level. These aides now feel part of the team. Perceived Challenges Market competition has been the greatest challenge facing First Choice. Prior to the partnership with the CCRC communities, a local hospital’s home health and hospice program competed with First Choice and made it difficult for First Choice to grow its client base. The hospital’s restructuring created a market The nurses and administrator provide the training and hold the aides accountable for the assistance they provide in a person’s home. opportunity for the agency. First Choice hired the hospital agency’s nurses and executive director. These staff members had many years’ experience in home care and their names were recognized in the community. These factors helped strengthen First Choice, particularly on the home health side. The First Choice partners report that the home care side of the business is more challenging to manage than the home health care side because the home care staff is more transient than the home health care staff. In addition, problems on the home care side of the business can impact the home health business. First Choice has addressed these challenges by holding in-service training sessions for home care aides. The nurses and administrator provide the training and hold the aides accountable for the assistance they provide in a person’s home. First Choice managers are also making an effort to help the aides feel part of the organization. Offering benefits to full-time home care aides was a major component of that effort. Perceived Benefits The executives of VMRC, Bridgewater and Sunnyside report that the provision of home health care and home care has been beneficial for each organization. VMRC appreciates the fact that the joint venture has allowed it to offer assistance to individuals who want to stay in their own homes. Bridgewater’s leadership believes the partnership has helped it “close the loop” on the continuum of care by offering additional services to on-campus residents and consumers living in the community. The organization’s diversification has raised Bridgewater’s community profile and offered it the opportunity to market its residential services to clients who are now receiving care in their homes. Sunnyside, which has only been part of the joint venture for a few months, already has seen positive financial returns from First Choice. Sunnyside residents, particularly those who had been interested in receiving home care services, welcomed the expansion. Outcomes First Choice has not conducted any formal evaluations of its programs, beyond analyzing client satisfaction surveys and outcomes data for its home health care services. The agency receives positive feedback from clients, especially residents at CCRCs who appreciate receiving home care services. Sodexo • IAHSA • LeadingAge | 65 FIRST CHOICE Lessons Learned First Choice and executives from its CCRC partners offer the following suggestions for residential service providers that are considering expanding into home and community-based services or have already begun the expansion process: Be patient. Expanding into home and community-based services can be a slow process. The timeline will depend on whether a provider starts its own agency or purchases an existing agency. Be prepared to put time and energy into the new service line. Although VMRC, Bridgewater and Sunnyside purchased an existing agency, it took a great deal of work to integrate that agency into their businesses. The consulting services and expertise provided by Senior Options have been beneficial. It would have been difficult for any of the partners to support a home health care business on its own. Advocate and educate. It’s important to ensure that staff members accept your new community-based business line. Advocate for home health with your staff and educate those employees about the benefits of your diversified service line. Make sure aides have a good understanding of home care. It is not always “glamorous” to work in someone else’s home and can be disappointing. Before hiring a new home care aide, First Choice conducts a “ride along” to help the person get a better sense of home care. Protect your reputation. It’s important to understand that the reputation of your home health and/or home care agency will affect the reputation of your entire organization. 66 | Residential Provider Expansion into Home and Community-Based Services Case Study SHEPHERD’S CARE AT HOME EDMONTON, ALBERTA, CANADA | June 2015 Introduction Shepherd’s Care Foundation (foundation) was established in 1970 and provides a campus-based continuum of care that includes independent living, supportive living,18 and nursing home care. The foundation is a not-for-profit organization that has five locations in Edmonton and Barrhead, and manages a number of additional care sites. It serves more than 1,600 older adults who have low or moderate incomes. The organization’s vision is to provide “agingin-place services with excellence.” Service options include: Home care Supportive living, which blends a homelike environment with 24-hour nursing care Supportive living with dementia Long-term care services provided by a registered nurse (RN) around the clock The design of the foundation’s service program is based on its person-centered care philosophy, which emphasizes an individual’s autonomy, choice and flexibility. Staff members are viewed as “flexible solutions masters” who listen to residents and find creative ways to meet their requests. In 2008, Shepherd’s Care Foundation became the first organization in Canada to receive accreditation as an aging services network through CARF International, an independent, not-for-profit accreditor of health and human services in several service areas, including aging services. The organization was reaccredited in 2011. Shepherd’s Care Foundation established Shepherd’s Care at Home (agency), its home care agency, in 2014. This study was conducted through interviews with staff at Shepherd’s Care Foundation and Shepherd’s Care at Home and a site visit at Shepherd’s Care at Home. Policy Context Provincial governments are primarily responsible for senior care in Canada. Each province has different rules and regulations for long-term services and supports. The Province of Alberta, where Shepherd’s Care Foundation is located, has strict regulations for publicly funded home care and home health care. Alberta Health Services (AHS), Canada’s first province-wide, fully integrated health system, has proprietary control over the delivery of services for most providers. AHS uses funding and regulations to influence how providers deliver services within the province. AHS also restricts the number of publicly funded agencies providing services. There are no comparable restrictions for the private agencies. Alberta’s political leadership changed significantly in May 2015 when voters ended the 44-year dominance of the Progressive Conservative Party and brought the New Democratic Party into leadership. How these political changes will affect the provision of health care, particularly home health care, is uncertain. Most (90%) long-term services and supports delivered in Alberta, including home care, are publicly funded. The government does not require care recipients to undergo asset testing in order to qualify for services. On the contrary, most Albertans expect the government to cover the majority of their costs for long-term services and supports. Consumers do not expect to pay for services out of their own pockets. The increasingly complex care needs of older Albertans could challenge the sustainability of the government-funded system of long-term services and supports. The fact that home care costs are rising faster than the savings these services bring to the health care system is putting political pressure on the government to balance the budget. In an emerging trend, many consumers in Alberta will receive a mix of publicly funded and Sodexo • IAHSA • LeadingAge | 67 SHEPHERD’S CARE AT HOME private-pay home care services because publicly funded health care will not meet all consumer wants or needs. AHS recently introduced a new government-funded service called “Added Care.” Administered through the government’s Supportive Living program, “Added Care” provides extra hours of supportive care to individuals who are on the waitlist for higher levels of residential care. The initiative is part of Alberta’s new strategy to offer older adults and adults with disabilities greater choice and the ability to remain in their own homes and communities. Through the AHS Coordinated Access process, consumers in need of services are assessed to determine which program and level of care would meet their needs most effectively. These consumers receive information about the range of available services and options—including the availability of affordable accommodations—to meet their assessed needs. Expansion into Home and CommunityBased Services Shepherd’s Care Foundation began offering home and community-based services in October 2014. The decision to expand the organization’s service lines was driven by the foundation’s need to diversify its portfolio and increase the percentage of the revenues it receives from private-pay clients. Sixty percent of the foundation’s revenue came from the government in 2012. The foundation’s leadership team does not believe that dependence on government funding is a sustainable model, given the growing challenges associated with the government’s policy to provide free health care to all citizens. The agency’s leadership team is also aware of the growing tendency for not-for-profit providers in the United States to expand their operations to include home health and home care programs. Shepherd’s Care Foundation initially conducted limited market research to determine service needs on its campus and in the external community. Findings from focus groups showed a gap in the availability of companionship and transportation services. The focus groups did not gather information about consumers’ willingness to pay for these services, despite the fact that consumer hesitation to pay for services could limit a home care agency’s growth potential. After reviewing the market research and perceived trends in Alberta, the foundation’s leadership team decided to establish a home care agency called Shepherd’s Care at Home. The new agency would be a for-profit entity that would be independent and separate from Shepherd’s Care Foundation. Board members felt that establishing a separate corporate entity made sense for the following reasons: Concerns about unions: Shepherd’s Care Foundation has collective labor agreements with the largest union in Alberta. Because the annual compensation rates included in the agreements increase at twice the rate of inflation, the cost of providing services exceeds the government reimbursement rate for those services. Foundation leaders 68 | Residential Provider Expansion into Home and Community-Based Services reasoned that establishing the home care agency as a separate entity would keep the union from applying the foundation’s collective agreement to the new home care agency. Unique identity: Foundation leaders also wanted the new home care agency to have its own identity as a service provider. For this reason, it decided that the new agency would have its own management team and board of directors. A different type of business: The board recognized that the business models for home care and residential care were so different that these business lines should be housed in separate organizations and not merged into one organization. Shepherd’s Care Foundation has been challenged by the fact that it launched Shepherd’s Care at Home at a time of political upheaval in Alberta. That upheaval could bring about policy changes that might impact the new home care agency. On the other hand, Shepherd’s Care at Home also has an opportunity to provide and supplement government-funded home care at a time when consumers are looking for more services than the government can provide. Description of the Program Services Provided Shepherd’s Care at Home only provides non-medical care or home care. The agency delivers most of its services (80%) to the foundation’s on-campus residents, while a smaller portion of its services (20%) are used by external clients living in their own homes in the community or on other residential care campuses. This distribution of clients is a direct result of the agency’s two-pronged strategy to build its client base on the foundation’s campus first and then expand service delivery to the wider community. This strategy allowed Shepherd’s Care at Home to begin delivering services in October 2014, before a legal structure for the new agency was in place. Many foundation residents receive services through the government’s “Added Care” program, which provides additional supports to help older adults remain at home. 20% 80% On-campus residents External clients Timeline SHEPHERD’S CARE AT HOME 1970 Established Shepherd’s Care Foundation. 2008 + 2011 Shepherd’s Care Foundation awarded CARF Accreditation as an Aging Services Network. 2014 Launched Shepherd’s Care at Home in Edmonton, Alberta. Sodexo • IAHSA • LeadingAge | 69 SHEPHERD’S CARE AT HOME “Added Care” could potentially offer Shepherd’s Care at Home a solid client base. However, because “Added Care” services are based on client needs, the amount of service hours delivered through the program can fluctuate on a monthly and annual basis. Shepherd’s Care at Home’s participation in the “Added Care” program allows the foundation to provide additional services to its residents without putting added pressure on its own staff. Residents receive regular care from their permanent foundation aide and “Added Care” services from the Shepherd’s Care at Home aide. The agency’s campus-based business model has encountered some challenges due to the fact that many foundation residents cannot afford to pay privately for services. These challenges underscore the need for the agency to build a private-pay client base in the external community. Eventually, the Shepherd’s Care at Home executive director hopes to reverse the agency’s client mix so most clients come from the external community. These external clients may be better equipped to pay for services. Shepherd’s Care at Home provides person-centered care and recognizes each client is different and unique. It strives to meet the wishes of the individual and promote his or her choice and independence. Aides also take time to know clients and immediately respond to their requests. The agency’s philosophy of care is based on three Cs:19 Compassion: Staff members provide honest, respectful and compassionate care. Communication: The agency team listens to the needs of the client and presents the best options for care. Team members ensure that the consumer and family know what is happening each step of the way. 70 | Residential Provider Expansion into Home and Community-Based Services Consistency: The team provides consistent and reliable services to each client. Each team member is matched carefully with a client. Care and services remain consistent. Shepherd’s Care at Home primarily provides transportation and companionship services. The agency plans to grow these two programs before branching out to other service areas. Shepherd’s Care at Home plans to add personal care to its service options in the future. AHS’s limits on coverage for skilled home health services are increasing the need for privatepay services. Shepherd’s Care at Home believes it may have a role to play in supplementing publicly funded skilled services with private-pay services. The agency is in the process of hiring a licensed practical nurse (LPN) as clinical director to oversee the development of its personal care services. Following is a list of Shepherd’s Care at Home’s current and future services: Transportation services currently include door-to-door transportation for: Appointments Personal errands Shopping trips Assistance and companionship services currently include, but are not limited to: Accompaniment on a walk Accompaniment to medical appointments Assistance with grocery shopping Light housekeeping and laundry service Meal preparation Medication reminders SHEPHERD’S CARE AT HOME Mental stimulation Overnight services Pet care Playing cards and games Reading a book or watching a movie Respite care Safety monitoring Social visiting Sharing a hobby Personal care services will include, but will not be limited to: Assistance with dressing or putting on shoes Assistance with feeding Assistance with bathing and personal cleanliness, including dental hygiene and shaving Incontinence care and toileting Managing care for people with Alzheimer’s disease and other dementias, including managing behaviors, encouraging engagement, and assisting with activities of daily living Medication management Mobility assistance, including helping individuals get in and out of the bed Shepherd’s Care at Home learned from market research that its competitors are charging between $27 and $35 per hour for a minimum of three to four hours of service. Based on this information, the agency decided to charge an hourly rate of $30 for its services and to require a minimum of two service hours per visit. So far, most prospective clients seem willing to pay these fees. Partnerships Shepherd’s Care Foundation and Shepherd’s Care at Home operate as separate businesses. Shepherd’s Care at Home will have its own board of directors and management team when it becomes “official and legal” later this year. Consumer Eligibility Consumers do not need to meet any eligibility requirements, other than ability to pay, in order to receive private-pay services from Shepherd’s Care at Home. The agency’s executive director conducts an assessment to determine each client’s service needs, and works with family members to develop a care plan. Clients receiving publicly funded home care services on the campus are assessed by a team at Shepherd’s Care Foundation to determine their eligibility for services. Shepherd’s Care at Home Clientele Shepherd’s Care at Home was providing an average of 263 hours of service per month after its “soft” launch in October 2014. The agency has increased those hours significantly. Since February 2015, the number of non-skilled service hours has held steady at 1,500 per month for approximately 35 to 40 clients. The agency’s clients differ in their service needs and the amount of services they receive each week. Some clients require an hour or two of weekly services while others need 20 hours of service delivery during the same time period. Given the range of clients’ need for service hours, Shepherd’s Care at Home feels that the number of service hours it provides each month is a better indicator of its service volume than the number of individuals served. The agency anticipates that service hours will increase exponentially over the next few months once its ownership framework is established and it can market its services more actively. The executive director would like service hours to grow to 2,000 hours per month over the next few months. One strategy for accomplishing this goal involves targeting the agency’s marketing efforts to older adults living on other residential campuses. Shepherd’s Care at Home does not have demographic data about its clients. Approximately 70% of clients do not have family or friend caregivers. Most clients have a low to modest income. Quality Assurance Shepherd’s Care Foundation has received accreditation from CARF International over the last three years. CARF International’s standards, which are designed to “promote quality, value and optimal outcomes of services,” have guided the development of the Shepherd’s Care at Home agency. Shepherd’s Care at Home does not have a formal quality assurance process. While Shepherd’s Care Foundation has a quality committee, agency staff members have not been part of that committee. It is not clear whether Shepherd’s Care at Home will establish its own quality care committee or be integrated into the foundation’s quality committee. Most of the agency’s quality assurance efforts currently take place through communication with aides, clients and family members. The agency does not conduct client satisfaction surveys, but is considering implementing a survey process to track satisfaction with companion, transportation and personal care services. The agency also may administer staff satisfaction surveys. Shepherd’s Care at Home aides who provide “Added Care” services to foundation residents follow an informal quality assurance system, but it is a “work in progress.” The manager of the foundation’s Supportive Living unit, where “Added Care” services are delivered, works with the agency’s executive director to resolve any quality-related problems. When a client complains about services, the executive director of Shepherd’s Care at Home will talk with the client and the aide to understand their different perspectives. The executive director will also assure family members that the situation will be addressed. As Shepherd’s Care at Home becomes more established, the agency may implement a more formal system to assess and address clients’ complaints. Agency aides working in the foundation’s Supportive Living unit follow the foundation’s procedures for documenting clients’ Sodexo • IAHSA • LeadingAge | 71 SHEPHERD’S CARE AT HOME complaints and concerns. During this process, the unit’s manager: build relationships with consumers and providers in various sectors, including: Provides the client with a timeline for addressing the concern Gathers information to understand the perspectives of clients and aides Meets with the executive director of Shepherd’s Care at Home to develop solutions to the problem Marketing The Shepherd’s Care Foundation and Shepherd’s Care at Home market their programs separately. Marketing for residential care takes place primarily through fundraising efforts. With a two-year waiting list, the foundation does not have to actively promote its services. On the other hand, Shepherd’s Care at Home needs to create awareness of its program and distinguish its services from the competition. The agency believes that its person-centered approach to care and its policy regarding service hour minimums puts it at an advantage when marketing its companionship and transportation services. The agency anticipates that its marketing strategy will change when it begins offering personal care services. The agency believes that its personcentered approach to care and its policy regarding service hour minimums puts it at an advantage when marketing its companionship and transportation services. Despite their separate marketing efforts, the foundation and the agency do work together to market their services. For example, the foundation refers clients to the agency when those clients are on the waiting list to receive campus-based accommodations. Shepherd’s Care at Home has “softly” promoted its services for several months. The agency will formalize its promotional efforts after it becomes a distinct legal entity. In the meantime, the agency has connected with most of its clients through referrals from the foundation. Because the foundation serves a low- to modest-income population with limited resources and ability to pay for services, growth of the agency’s home care business has been limited. Shepherd’s Care at Home will soon need to expand its clientele to include older adults who are willing and able to pay for the services. In a few months, Shepherd’s Care at Home plans to launch an active marketing campaign that will create community awareness about the program, brand the agency’s services and 72 | Residential Provider Expansion into Home and Community-Based Services Independent senior living communities where managers tend to be more open to private-pay home care services Churches Senior centers, where agency staff can distribute flyers and make presentations to older adults and recreation coordinators Community events that attract older adults Grocery stores where agency staff can distribute flyers Shepherd’s Care at Home has already held informational seminars to help community members navigate Edmonton’s system of long-term services and supports. These seminars have been well attended and have yielded positive feedback from families and individuals. As a result, more relatives of foundation residents are requesting companionship services for family members with Alzheimer’s disease and other forms of dementia. Families recognize that agency services can help these older adults stay in their current residence rather than relocating to a more secure unit on the foundation’s campus. The agency’s marketing team has experienced challenges as it attempts to build relationships with providers and inform them about its services. These challenges include: Difficulty marketing to hospitals: Hospital staff members often do not think about home care services as an option for their patients and may not be willing to learn about these services. In addition, there is often not one hospital staff member who serves as a contact person for agencies like Shepherd’s Care at Home. The agency could address this challenge by trying to build a rapport with the hospital staff when residential clients are hospitalized. Resistance from consumers: Consumers do not always believe they need the services that Shepherd’s Care at Home provides. To address this challenge, staff members often market the agency’s services indirectly. For example, staff members may offer to help a client by providing informal help with a few tasks. The appreciative client may then request formal services from the agency. Providers’ lack of receptiveness to agency services: Some providers of aging services may already have established relationships with other home care agencies and may not be interested in making Shepherd’s Care at Home their provider of choice. The agency could overcome this challenge by targeting its marketing efforts to consumers who live in their own homes and not on a campus. These consumers could purchase a small number of services at first and continue to use the agency as their service needs increase. Shepherd’s Care at Home also is considering targeting its marketing efforts to family members, in addition to older adults. The agency’s outreach coordinator could educate family members who are responsible for making decisions about whether a relative needs services and what services are most appropriate. SHEPHERD’S CARE AT HOME As the official launch of Shepherd’s Care at Home approaches, the agency has an opportunity to review its business model, client projections and operational strategies and then identify two or three tangible strategies for carving out the agency’s market niche. Strategy development would be enhanced by market research that assesses: The potential size of the service market How Shepherd’s Care at Home compares with its competitors Emerging trends in the field of aging services New opportunities to fill service gaps and convince clients to pay for services The agency’s pricing structure Financial Implications Shepherd’s Care Foundation made an initial investment of approximately $250,000 (CAD) when it expanded into home and community-based services. The investment covered the following costs: Purchase of a van Salary and wages, which represented most of the costs Marketing and advertising Office space rental A consultant to develop a business plan Shepherd’s Care at Home is not generating a profit at this time, but anticipates doing so within a year after the program officially opens later this year. When the agency does begin generating profits, its revenues will be used to supplement the government-funded reimbursements that the foundation now receives. The foundation’s reimbursement rates are lower than the cost of care. To date, the foundation has reduced its expenditures in areas that don’t impact resident care. Profits from Shepherd’s Care at Home will help strengthen the foundation’s bottom line and ensure that it can continue serving older adults who cannot afford to pay the full cost of care. The foundation’s board of directors will be watching carefully to see if Shepherd’s Care at Home can expand its client base beyond foundation residents. Some believe that if agency financials do not improve substantially over the next year, members of the board of directors may question whether it makes sense to continue the agency’s operations. Workforce Shepherd’s Care at Home employs 45 workers, including: Executive director Outreach coordinator Approximately 40 to 45 home health aides Four drivers An office assistant The agency employs certified home health aides or aides who are working toward their certification. These aides are well positioned to provide more clinical care when the agency begins offering personal care services. The agency’s home care aides are all casual workers and do not receive benefits. This arrangement gives Shepherd’s Care at Home the flexibility it needs to accommodate the changing needs of its clientele. As the client base grows, the agency will be able to increase the hours that current staff members work rather than hiring additional staff. Executive Director: Shepherd’s Care at Home plans to involve its executive director in all aspects of its work and give her many hats to wear. The executive director currently supervises all of the agency’s aides and goes on visits to clients’ homes to monitor quality. In addition, the executive director is responsible for hiring and training staff and shares responsibility for overseeing the agency’s billing system. The executive director accompanies aides on their first visit to the client’s home and updates the aide about the client. The executive director occasionally visits the clients and stays in touch with the family members to make sure they are satisfied with their services and don’t have any concerns. Aides reported that the executive director is very responsive when they are seeking advice about a particular situation. Aides: Although Shepherd’s Care at Home provides primarily non-medical care, the agency employs certified home health aides or aides who are working toward their certification. These aides are well positioned to provide more clinical care when the agency begins offering personal care services. Some current aides have worked in both residential and home care while others only have experience in the home care setting. All aides were new hires. No aides were redeployed from the Shepherd’s Care Foundation’s residential setting. Sodexo • IAHSA • LeadingAge | 73 SHEPHERD’S CARE AT HOME Aides account for their time by using a timesheet that is signed by the client. When an assigned aide is unavailable, the executive director appoints another aide to provide a client’s care temporarily. When no substitutes are available, the executive director covers a shift. Approximately 40 Shepherd’s Care at Home aides care for 45 clients. Many of the aides are assigned to one client. The agency practices consistent assignment, which allows aides to build relationships with their clients and become familiar with their wants and needs. Clients who require 16 or more hours of care each day have three or four aides assigned to them. The executive director takes personalities into account when matching clients and aides. Supervision: Shepherd’s Care at Home plans to hire an LPN and an RN consultant to oversee the personal care side of the agency. The LPN will conduct orientation for aides and introduce them to their new clients. He or she also will supervise the aides during visits to the home and make reports about the quality of those visits to the agency’s executive director. The LPN will also communicate with family members, conduct training and education, and hire new staff. The agency will determine the frequency of supervision for aides. Aides interact with the supervisor and the agency’s executive director primarily through text messages and emails. They rarely see or interact with their supervisor. When aides provide care to residents of Shepherd’s Care Foundation, the LPNs on the unit are available to answer any questions. The aides also submit a written report documenting any personal care services they provide to clients. No report is required for companion services. Some workforce challenges include: Unreliable schedules for aides: Since aides typically work with only one client, an aide may not have work when the client no longer requires services. A high number of referrals makes it possible for the agency’s executive director to reassign aides to new clients in a timely manner. Aggressive or combative clients: An aggressive or combative client can cause injury to an aide. The aides at Shepherd’s Care at Home have developed strategies to address these behaviors. After getting to know their clients, aides can devise innovative strategies for calming clients who become combative. If these strategies are unsuccessful, the aide will notify the LPN at the foundation or call the agency’s executive director for advice on how to handle the situation. Caring for clients with dementia: Aides appreciate the opportunity to form relationships with clients and to feel that they are making a difference. Clients often view their aides as family and friends. However, it can be difficult for aides to form relationships with individuals with dementia. Clients with dementia may not remember the aide from one visit to the next. Aides must reestablish their connection with the client at each visit. Dealing with clients who resist care: Some clients refuse an aide’s assistance with tasks that are outlined in the care plan. Aides must create a balance between respecting the wishes 74 | Residential Provider Expansion into Home and Community-Based Services of clients and providing services necessary to maintain the individual’s health and quality of life. On-the-job training: Shepherd’s Care at Home doesn’t hold orientation sessions for new aides and those aides do not shadow experienced aides. Aides who are new to the field could benefit from a buddy system that helps them understand the home environment, observe how an experienced aide interacts with clients, and review care basics. Consistent assignment: Shepherd’s Care at Home strives to ensure that each client has an aide who can continue to provide higher levels of care when they are needed. Staff Benefits All aides at Shepherd’s Care at Home are casual workers who are not entitled to benefits. The aides are reimbursed for travel expenses when they escort a client to an appointment. However, aides are not reimbursed for mileage when they visit clients. In addition, aides receive a four-percent premium when they work holidays. Aides on the day shift are paid the same hourly wage as aides who work the evening shift. Staff Recruitment and Training Shepherd’s Care at Home has no difficulty recruiting staff. The agency receives resumes from prospective employees on a regular basis. The recruitment process emphasizes the importance of hiring the right people and ensuring the agency and its culture represent a good fit for the individual. If the executive director does not believe this to be the case, she will suggest other employment options for the individual. Shepherd’s Care at Home uses a thorough process to hire the right staff members. The executive director conducts a national criminal background check on all aides. In addition, she interviews potential aides to assess: General experience caring for older adults and younger adults with disabilities in any setting Personality and attitude, including the ability to work on a team, serve customers, respect others, deliver personcentered care, maintain a positive attitude, solve problems and be dependable How the individual interacts with others and addresses issues Shepherd’s Care at Home currently has a low turnover rate. Only one staff person has left the agency since October 2014. This is consistent with, and could be related to, the low turnover rate at Shepherd’s Care Foundation, which is known for having a positive work environment and supportive management. Agency staff members have around-the-clock access to the executive director. The new LPN is expected to contribute to the positive work environment because she will have the time and clinical expertise to support aides. The agency plans to provide quarterly trainings once the LPN is hired. These trainings will focus on specific diseases SHEPHERD’S CARE AT HOME and other issues that affect the agency’s clientele. The LPN will select the training topics with input from aides. The aides from Shepherd’s Care at Home and Shepherd’s Care Foundation will have separate trainings. Shepherd’s Care at Home and Shepherd’s Care Foundation have similar organizational cultures. Because Shepherd’s Care at Home is relatively new, there have been limited opportunities for interaction between agency and foundation staff. It can be challenging to create an environment where the aides who work independently and do not report daily to the agency can engage with one another, share information and develop relationships. The only time aides see each other is when there is a hand-off in a client’s home. The executive director hosted a holiday party for staff and plans to host other special events throughout the year. Aides may also have opportunities to meet during the quarterly trainings and staff meetings. Perceived Challenges Shepherd’s Care at Home faces significant competition from other home care service providers. As the government scales back on the type and number of services it will cover, more private home care agencies are being launched. The agency also encounters competition from larger private home care agencies. On-campus residents are not required to use Shepherd’s Care at Home as their home care service provider. As a result, residents are not always aware of the agency’s transportation and companionship services. A more robust marketing effort could encourage residents to consider Shepherd’s Care at Home when they require assistance. Other challenges include: Launch delays: Shepherd’s Care at Home was delayed in launching its program while it created a separate legal entity, developed a business plan and put a business structure into place. This process required more time and effort than anticipated. Increases in client base: Keeping up with a significant increase in the number of home care clients has been challenging for Shepherd’s Care at Home. When the number of clients nearly doubled from 800 to 1,500 in February 2015, the agency had some difficulty hiring and training staff to meet the demand. Cost of labor: Unions have a powerful voice and control the supply of labor in the home care sector. If Shepherd’s Care at Home makes a collective agreement with the unions that is similar to the union’s collective agreement with Shepherd’s Care Foundation, the costs of care could increase by 30%. If these costs are passed on to clients, the agency’s hourly rates will be significantly higher. Logistics: Providing transportation services across a large region presents logistical challenges. Changing consumer mindsets: Alberta Health Services covers the fees for most long-term services and supports. As a result, older Albertans don’t expect to privately pay for their care. This mindset has affected the transportation services that Shepherd’s Care at Home provides. This service hasn’t done as well as expected and is operating at a loss. An informal survey found that 80% of foundation residents use family and friends for transportation, which can place a burden on families who may be juggling family and work issues. For this reason, Shepherd’s Care at Home plans to target its private-pay transportation services to family members. Low demand: The economic circumstances of many foundation residents suggest that they are not an ideal audience for private-pay services. Competitors with volume and pricing advantage: Agencies competing with Shepherd’s Care at Home can offer lower prices because they have a larger client base. False sense of optimism: Shepherd’s Care Foundation assumed that private-pay home care services would be an “easy sell” for consumers seeking to supplement government-funded services. This has not been the case. Administrative practices: The business model for home care is different than the business model for residential care. It’s important to understand that residential care administrative practices are not effective for home care agencies. Communication rift: The leadership teams from Shepherd’s Care Foundation and Shepherd’s Care at Home have not collaborated enough as they strive to understand the market and establish a niche for their services. Funding: Agencies that provide publicly funded services lack a profit margin. While reimbursement rates are currently stable, the government keeps changing the services that it will cover. As long as Shepherd’s Care at Home provides private-pay services exclusively, this dynamic will not impact its operations. However, fluctuating coverage could become an issue once the agency moves more into the publicly funded market. Providing in-home services helps to improve quality of life for Shepherd’s Care at Home clients. These services can enhance an older person’s health and ability to function. Sodexo • IAHSA • LeadingAge | 75 SHEPHERD’S CARE AT HOME Perceived Benefits Despite the challenges outlined above, the leadership teams at Shepherd’s Care Foundation and Shepherd’s Care at Home identified numerous benefits associated with providing home care services, including: Aging in place: Consumers who receive services from Shepherd’s Care at Home can stay at home longer. Financial rewards: The agency may be able to earn greater revenues by providing private-pay services than it can by providing publicly supported services. Those revenues can help subsidize shrinking government reimbursement for care. Rural outreach: Shepherd’s Care at Home currently serves an urban population, but a large percentage of Albertans lives in rural areas. The agency’s leadership team would like to provide home care services to individuals residing in rural areas in the next five to 10 years. Support for foundation aides: Aides from Shepherd’s Care at Home are helping to support foundation residents through the government-funded “Added Care” program. Asking the agency to provide this care has helped the foundation meet the needs of its residents while easing the pressure on its permanent aides. Improving quality of life: Providing in-home services helps to improve quality of life for Shepherd’s Care at Home clients. These services can enhance an older person’s health and ability to function. For this reason, agency staff members believe they are making a difference in people’s lives. Outcomes Given the novelty of Shepherd’s Care at Home, the agency has not conducted any formal evaluations of its services. Shepherd’s Care at Home plans to conduct client and referral source surveys to determine whether and how it has assisted clients and helped community organizations. Lessons Learned Shepherd’s Care at Home and Shepherd’s Care Foundation offer the following suggestions for residential service providers that are considering or already expanding into home and community-based services: Build relationships. Developing good relationships with community organizations, providers, clients and family members can help an agency create awareness about its program and develop strong referral sources. When building relationships with consumers and family members, be sure to create a personal connection with the individual. Follow-up with clients when they return from the hospital to determine their preferences and needs. Test the business idea before launching the program. Make sure you have a solid business plan and a vision for how to operationalize your program. Identify, through market research, where the business can grow and understand the competition. It is essential to know what 76 | Residential Provider Expansion into Home and Community-Based Services is occurring in the market, whether there is a need for services, and whether consumers are willing to pay for those services. Wait to hire new staff until consumer needs justify a workforce expansion. Understand how for-profit and not-for-profit business models differ. This understanding is important in situations where the residential care provider is a not-forprofit organization and the home care agency is a forprofit organization. Growing a for-profit entity requires a distinctive mindset and business plan. Establish a brand identity. A home care agency may not have the same bond with off-campus consumers as it does with the on-campus residents. The agency must establish itself within the external community and can’t rely on the residential care provider’s brand identity. Identify shared goals. This is important if the home care agency is affiliated with, but independent from, a larger organization. Leadership teams from both groups must have the same goals for the home care agency. Conduct extensive market research to understand the target group. This research should identify service needs and gaps as well as consumer willingness to pay for services. While market research conducted by Shepherd’s Care at Home demonstrated a need for transportation, the study did not take into account whether people would be willing to pay for these services. Consumer unwillingness to pay for services has made it difficult to grow the agency’s transportation component. One possible alternative might involve expanding the target market for transportation services to include other populations like younger people with disabilities. Recruit the right executive director. The executive director must understand how to provide both private-pay and government-subsidized services. Understand the pros and cons of offering personal care services. Personal care services entail higher administrative costs due to the policies and practices required to obtain a license and provide licensed services. Get comfortable with growing pains. Growing pains are always associated with a new service line that forces an organization to step outside its core business. The management team must learn from this experience and put processes in place to improve the system. Conduct staff meetings. These meetings allow staff members to develop relationships with and learn from each other. They also provide a good opportunity for staff members to discuss their clients and share information that will help them address potential issues. Develop a strategy. Ask the leadership team to develop a strategy for the home care program. Seek different perspectives and get input from all team members. Measure progress against a formal business plan at regular intervals so you can make quick changes to the plan, add new resources as needed, and adjust forecasts for future results. Share what you learn with the board and other stakeholders. Case Study WELL-SPRING RETIREMENT COMMUNITY GREENSBORO, NORTH CAROLINA | January 2015 Introduction Well-Spring Retirement Community (Well-Spring) is a not-forprofit continuing care retirement community (CCRC) located in Greensboro, NC. Well-Spring was established in 1993 by a coalition of nine local churches. Well-Spring provides accommodations at every level of care, including independent living, assisted living, and skilled care. The organization received the North Care New Organizational Vision Award, which is a special licensure designation for nursing homes, adult care homes and home care agencies that voluntarily meet higher standards for workplace culture. To accommodate its expansion into home and communitybased services, Well-Spring created an umbrella organization called Well-Spring Services, Inc. This parent organization includes four distinct service lines: Well-Spring Retirement Community Well-Spring Home Care, which provides non-medical home care services The Adult Center for Enrichment (ACE), a provider of adult day care, caregiver education and respite day services Two Programs of All-Inclusive Care for the Elderly20 (PACE): PACE of the Triad in Greensboro and PACE of the Southern Piedmont in Charlotte, NC This study was conducted during interviews with staff from Well-Spring Services, Inc., and the Adult Center for Enrichment. Policy Context The North Carolina Department of Health and Human Services requires that organizations obtain a certificate of need and a license before they can provide medical services through a certified home health agency. Many state governments in the United States use certificate of need laws to regulate the number of beds in hospitals and nursing homes and to create a balance between the level of need in a region and the number of providers who are allowed to enter the market. Providing non-medical care through a home care agency does not require a certificate of need in North Carolina. However, applicants must: Acquire a license to operate a home care agency Meet specific standards regarding administration, staff competencies, supervision of patient care, and records Have written policies and procedures that comply with rules established by the North Carolina Department of Health and Human Services Run criminal background checks on all employees Agencies may be denied a license if they do not understand or comply with all requirements. For many years, North Carolina issued a specified number of licenses for home care agencies. But in 2009, the North Carolina Department of Health and Human Services instituted a brief moratorium on its practice of restricting the number of home care licenses it would issue. The state soon reinstated the practice of limiting new home care licenses, making it difficult Sodexo • IAHSA • LeadingAge | 77 WELL-SPRING RETIREMENT COMMUNITY for an organization to enter the market unless it partners with or purchases a license from an existing provider. Barriers to the development of adult day programs focus on reimbursement rather than regulation. Only about half the counties in North Carolina have adult day centers due to adult day’s numerous funding sources. It can be time-consuming and complicated to navigate these multiple funding layers. Expansion to Home and CommunityBased Services Process for Launching Program Well-Spring launched its home and community-based services program between 2009 and 2012. The decision to diversify services, as described in Well-Spring’s 2008 strategic plan, reflected the organization’s desire to expand its services. Oncampus residents requiring home care services were using outside entities and Well-Spring watched potential revenue going to other providers. The organization believed that it could provide quality home care services to on-campus residents and compete for external clients when its brand awareness grew. The following staff members were involved in the development of the home care program: Chief executive officer/president Chief financial officer Controller Human resources director Health care administrator Marketing staff The CCRC’s management and members of the board of directors had ongoing discussions before agreeing to the expansion of service lines. They continue to discuss the value of expanding into home and community-based services. While board members agreed to the diversification, they actively track the venture’s profit margins, quality measures and service volume. The decision to add new service lines was driven by the need to: Create a continuum of care for CCRC residents and external clients: Well-Spring wanted to be a “one-stop shop” that would allow consumers to access and obtain a variety of needed services from one agency. Bring continuity to a fragmented market: The aging services market did not include a not-for-profit home care agency dedicated to providing quality services. This gap represented an opportunity for Well-Spring. Serve the underserved: Well-Spring’s strategic discussions took place during the 2008 economic downturn, when the Well-Spring Retirement Community was attracting only a fraction of local older adults over the age of 75. Well-Spring’s management and leadership teams believed that home and community-based services offered the organization an opportunity to reach more members of this age group, especially those who were not interested in moving to a CCRC. 78 | Residential Provider Expansion into Home and Community-Based Services Fulfill Well-Spring’s not-for-profit mission: Well-Spring strives to serve all older adults, not just a small percentage of the older population. The organization’s board of directors felt an obligation to do more than provide CCRCbased services. Support individuals in their own home: Well-Spring’s decision was rooted in the desire of older adults to remain in their own homes, and the interest of government programs to support aging in place. Organization leaders knew from experience that government resources were insufficient to meet the growing need for long-term services and supports. They viewed home and community-based services as an affordable way for older people to fulfill their preference to remain at home. Build an awareness of long-term services and supports: That awareness might spur community-dwelling older adults to seek on-campus services, and possibly move to Well-Spring’s CCRC, in the future. Well-Spring provides non-medical home care to residents of its retirement community and to clients who live in the external community. The organization decided not to provide home health care because of government restrictions that make it difficult to enter the market. When Well-Spring was considering its expansion into home and community-based services, North Carolina was not issuing certificates of need for home health care. When Well-Spring clients require home health care services, the organization refers them to Advanced Home Care, a preferred home health provider and a partner in Well-Spring’s PACE programs. The regulatory environment actually enabled Well-Spring to establish a non-medical home care agency. In 2009, when the Department of Health and Human Services instituted a brief moratorium on its practice of restricting the number of home care licenses, Well-Spring took advantage of the opportunity to establish a home care agency. Well-Spring experienced some initial challenges while implementing its home and community-based services program. Key challenges include the following: Understanding the funding sources for adult day: While CCRCs provide private-pay services, adult day services rely on multiple funding sources. Well-Spring staff members ventured into new territory as they learned to work with a variety of adult day funders. Finding staff for home and community-based programs: Well-Spring found it difficult to recruit, screen and train qualified staff when its home care program was growing at a fast rate. Securing office space: Initially, Well-Spring Home Care and the Adult Center for Enrichment (ACE) were located in separate off-campus locations, and home care staff used unoccupied residential space on the CCRC campus until a new resident moved into the space. Well-Spring has since leased space close to the CCRC for the ACE leadership, the home care team and staff of Well-Spring Services, Inc. Timeline WELL-SPRING RETIREMENT COMMUNITY 1993 Began as a continuing care retirement community. 2008 2011 + 2012 Started home care program. Acquired Adult Center for Enrichment (ACE), an adult day program, and integrated into Well-Spring Services parent corporation. 2016 Home care will move under ACE’s legal structure and ACE will be the hub for HCBS division. Sodexo • IAHSA • LeadingAge | 79 Description of the Program Well-Spring Home Care delivers 90% of its services to residents living on the Well-Spring CCRC campus and less than 10% to external clients. The organization is in the process of growing the external component of the home care program with the goal of achieving an equal percentage of on-campus and external clients. The adult day program is the largest segment of the organization’s community-based services. Well-Spring’s management viewed adult day as a prime opportunity to participate in health care reform initiatives and the work of Accountable Care Organizations (ACO).21 The organization believes that adult day programs can be important ACO partners because they can help ACOs reduce or prevent hospital readmissions and ease transitions from hospital to home. Partnerships Each of Well-Spring’s home and community-based service lines is a subsidiary of Well-Spring Services, Inc. Well-Spring decided to structure the organization in this way for three key reasons: Economies of scale: All corporate functions—including human resources, finance, and technology—are carried out through the umbrella organization. Limited liability: With an umbrella organization in place, the liabilities of the home and community-based services would not affect Well-Spring’s CCRC and vice-versa. Existing contracts: Having an umbrella organization allowed the Well-Spring CCRC to maintain its existing vendor contracts. Well-Spring works with ACE to provide adult day center programs, caregiver education and respite day services. The two organizations reviewed their cultures, core values, and visions, and consulted with attorneys, before ACE was incorporated into the Well-Spring Services organization. The partnership benefitted both organizations. 80 | Residential Provider Expansion into Home and Community-Based Services 10% 90% On-campus residents External clients Well-Spring recognized that ACE had expertise and a successful track record in adult day services. ACE had contracts and relationships with funders and interested donors. It also employed organizational leaders who could add “bench strength” to the overall Well-Spring management team. A partnership with ACE would allow Well-Spring to move ahead quickly in the adult day services sector. The partnership also provided ACE with the opportunity to move forward and expand. The ACE leadership viewed a partnership with another organization as a critical step in ensuring its own ability to navigate North Carolina’s regulatory environment and federal health care laws. In addition, ACE was growing at a fast pace and research suggested that the pace of growth would continue for several years. The center did not have the capacity to meet anticipated demand. Well-Spring Home Care will move under ACE’s legal corporate structure on January 1, 2016. The new structure will help Well-Spring manage risk and will allow ACE to serve as the hub for the home and community-based services division. The home care program will continue to be branded as Well-Spring WELL-SPRING RETIREMENT COMMUNITY Home Care. ACE will operate the adult day center program, caregiver education, respite day services and home care. Admission Criteria Each program under the Well-Spring Services umbrella has different eligibility requirements. Well-Spring Home Care clients must meet these eligibility requirements: Be at least 62 years of age Receive an assessment that includes an appraisal of needs and an in-home inspection to ensure a safe and adequate physical environment for care Live in the geographical area that Well-Spring serves Clients of the Well-Spring Adult Day Center must meet these basic eligibility requirements: Be at least 18 years of age Be comfortable in a group environment Receive an individualized assessment to ensure their needs can be safely met at the adult day center Eligibility requirements for the adult day center can change, depending on the rules and regulations of the funding source. PACE clients must meet these eligibility requirements: Be at least 55 years of age Meet requirements for a nursing home level of care, as determined by the North Carolina Division of Medical Assistance Have the ability to live safely in the community at the time of enrollment Sources of Reimbursement Adult day service has diverse funding streams, including: Private pay, which accounts for 25% of funding Medicaid Community Alternatives Program (CAP) for Disabled Adults Department of Veterans Affairs Home and Community Care Block Grant State adult day care funds Long-term care insurance The Well-Spring Home Care program is exclusively private pay. Well-Spring chose not to seek Medicaid funds for its home care services because of the low reimbursement rates ($13 per hour) in North Carolina. Adult Day Services ACE provides adult day services, group respite programs and caregiver education. The adult day program operates Monday through Friday from 7:30 a.m. to 5:30 p.m. The adult day program served more than 200 clients in 2014 and offered respite services to more than 200 caregivers. The program is certified to serve 108 individuals each day and averages about 90 people per day. The program is looking to expand so it can serve more people. Adult day services include: Breakfast, lunch and afternoon snacks Exercise programs and recreational activities Bathing and ancillary services, such as podiatry On-site nursing services, such as medication administration, provide by a Registered Nurse (RN) or a Licensed Practical Nurse (LPN) Access to computers Speech, occupational and physical therapy provided by contractors Transportation to and from the adult day center Educational and cultural programs Instruction and assistance with personal and health care needs Group respite allows individuals who are caring for family members to have a break from caregiving responsibilities. The individual requiring care can participate in activities, exercise, music, lunch and interaction with peers in a safe and secure setting and with close supervision. Education programs offer short-term and ongoing opportunities for caregivers to receive the information they need to support themselves and help their loved ones. These opportunities include educational sessions, caregiver support groups and annual caregiver retreats. In addition, ACE offers caregiver educational programs to local congregations and organizations. Well-Spring Home Care Services Well-Spring Home Care offers non-medical services that include: Assistance with activities of daily living, such as bathing, dressing and grooming Laundry and light housekeeping Respite care Transportation to and from appointments and meetings Weekly medication monitoring and reminders by an RN Meal preparation and feeding Toileting and incontinence care Transferring in and out of chair Assistance getting in and out of bed Activities to stimulate mental awareness Hobbies and games Outings and trips Assistance with correspondence Help with reading Companionship and conversation Sodexo • IAHSA • LeadingAge | 81 WELL-SPRING RETIREMENT COMMUNITY Well-Spring Home Care requires a minimum of one hour of service for external clients, but prefers four hours. The agency will provide less than one hour of services to residents of the Well-Spring CCRC as long as the shorter visit is compatible with the agency’s schedule. It also provides services on weekends and offers around-the-clock coverage. Well-Spring Home Care provides 10,000 billed service hours per month, primarily to clients on the CCRC campus. The agency plans to increase the average number of billed hours it provides to external clients each month from approximately 1,000 to 8,000 hours. It anticipates reaching that goal in two to three years, assuming it does not acquire other home care agencies in the area. Well-Spring initially depended on a network of existing partners, including the Area Agency on Aging, Department of Social Services and other social service organizations, to refer external clients to its home care services. Well-Spring Home Care has since implemented a formal referral process. There is significant competition in the market. Well-Spring Home Care remains focused on providing the highest quality of service, not the cheapest services. Demographics Home care: The majority of home care clients are women who are 55 years old or older, white, and have an annual income over $65,000. Transportation and housekeeping are the most popular services. CCRC residents tend to have more extensive needs for home care services than external clients. Less than one percent of the home care clients do not have a family caregiver. Adult day program: The majority of the adult day center clients are women over the age of 60 who belong to a minority group and have Alzheimer’s disease or a related dementia (See Figure 1). A very small percentage of adult day clients (3%) do not have a family caregiver. Quality Oversight Well-Spring Home Care clients use a formal system to report their complaints about services. Clients also have access to managers who will address any conflicts that arise. Figure 1. Demographics of Adult Day Center Clients 80% 60+ Female Minority Alzheimer’s disease or related dementia 50% 53% 66% 82 | Residential Provider Expansion into Home and Community-Based Services The adult day program conducts feedback surveys and uses the results to improve its services. In addition, the program has a Clients Rights Committee that handles unresolved complaints. Future Services Well-Spring’s management has considered offering a continuing care at home (CCaH) program, which provides a full package of CCRC services to older people living in their own homes. However, the organization is not sure its local market could support a traditional CCaH program at this time. Well-Spring Home Care does plan to offer home modification services and home-delivered meals within the next two years. The organization intends to collaborate with outside organizations to deliver these services, either through a joint venture or by incorporating an appropriate agency into the Well-Spring Services organization. Workforce Well-Spring’s adult day program and home care agency have separate workforces. The adult day program currently employs 40 people and the home care agency has a staff of 100 people. The vice president of home and community-based services oversees staff members in both programs. The workforce is expected to grow as the home care side expands its client base. Well-Spring Home Care Well-Spring initially hired several CCRC employees, including one employee who became the home care manager. However, the majority of new hires have come from outside the organization. Well-Spring did not have the capacity to staff the home care agency using CCRC employees. The director of clinical services is responsible for the daily operations of the home care agency. Her leadership team includes RN supervisors, a department coordinator, and office associates that oversee, train and supervise aides. The home care agency’s staff includes a manager and 92 home care aides, of which 36 are full-time employees. The aides serve on-campus clients and off-campus clients. Well-Spring Home Care does not currently have any contract staff. Most of the home care agency’s new hires had prior experience in home care and did not require specific training about the home care environment. Staff members from both Well-Spring’s residential setting and home care agency receive orientation together. The orientation sessions for the home care staff introduce new hires to the organization and provide information about working in the home care environment. Staff also can take in-service education that is tailored to their department. Staff at the home care agency receive transportation subsidies and are offered health insurance. Unlike staff in the residential setting and the ACE staff, home care staff does not receive paid time off. Adult Day Program ACE used existing employees to staff the adult day program because the organization existed before its partnership with Well-Spring. Staff positions for the adult day program include: WELL-SPRING RETIREMENT COMMUNITY Executive director Assistant executive director Activities director Family support specialist Assistant program director Director of caregiver education Respite directors Financial/administrative assistant Program director Assistant program director Health coordinator Director of business and development The adult day center’s program director, assistant program director, RNs and other leadership staff provide ongoing support and direction to the frontline staff. The program director is responsible for the daily operations of the adult day center. ACE contracts with some ancillary service providers for therapy and podiatry services. Well-Spring used a transition committee and sub-committee to help staff understand the adult day model and to address issues that surfaced while ACE was being integrated into the Well-Spring Services organization. For example: Well-Spring integrated ACE’s billing staff into its corporate office. The ACE billing staff was familiar with the billing operations for adult day services and helped educate WellSpring’s chief financial officer and controller about these operations, including the program’s many payer sources. The human resources staff had to become familiar with the regulations for adult day programs and how those regulations differed from skilled nursing regulations. They received help in this regard from the ACE administrative staff. This sharing of information was one benefit of collaborating with an existing provider of adult day services. Well-Spring and ACE held social gatherings and joint trainings of the administrative teams at both organizations. This helped to create camaraderie between the two groups. Shared Functions The Well-Spring subsidiaries share back-end office functions such as payroll, human resources, accounting, compliance and training. Members of Well-Spring’s corporate staff, particularly human resources and billing staff, were challenged by their expanding responsibility to serve the organization’s CCRC, adult day program and home care agency. Well-Spring outsources the billing for its PACE program due to the complexity of the payment model. However, as the PACE census increases, the organization is exploring the possibility of handling PACE billing internally. Organizational Culture Well-Spring’s adult day program, home care agency and CCRC are all subsidiaries of the Well-Spring Services corporate Well-Spring strives to recruit, train and retain the best staff possible across its entire family of services so that all services can provide quality care. organization. The CCRC and home care agency currently share organizational cultures, mainly because they operate on the same campus. The organization’s leaders believe that the home care agency will develop its own culture when it moves from the CCRC campus. There are basic differences between the organizational cultures of the residential business model and the home care agency, due to the fact that home care staff work far more autonomously than residential care staff. Despite these differences, Well-Spring strives to recruit, train and retain the best staff possible across its entire family of services so that all services can provide quality care. The organization also makes an effort to create a shared culture of excellence with new employees across the organization through joint orientations, shared training and employee events. Residential and home care staff members interact well together. Some conflicts exist between these groups because CCRC aides receive paid time off, while home care aides do not. Financial Implications Well-Spring’s investment in home care was minimum and consisted primarily of staff labor costs and an initial investment of less than $15,000 in computers and the licensing process. Well-Spring has recouped this investment. Home care is a lucrative service line for the corporation and has provided net margins every year since 2009. Sodexo • IAHSA • LeadingAge | 83 WELL-SPRING RETIREMENT COMMUNITY Well-Spring’s investment in ACE was more substantial. The organization spent $1.8 million to renovate the ACE building, and incurred additional expenses while consolidating and integrating the two agencies. Given the debt service on the adult day program, Well-Spring anticipates breaking even over the next two to three years. Since joining Well-Spring two years ago, ACE has increased its net assets by 150%, due, in large part, to a major capital campaign that allowed the organization to purchase and renovate its newest adult day center. Well-Spring board members have been satisfied with the financial performance of the PACE program and the home care agency. Board members also are satisfied with ACE’s new building and with its efforts to obtain contributions for the project. Board members would like to see ACE improve its financial performance by attracting more private-pay adult day clients. Perceived Challenges Market competition, particularly in the external community, is the greatest challenge facing the Well-Spring Home Care program. Well-Spring Home Care is the top provider of home care on the CCRC campus and is now trying to expand its reach off-campus. Greensboro has many home care providers and potential clients have several options when they need care. The organization’s leaders believe that quality services and continuous improvement will help distinguish Well-Spring Home Care from the competition. The agency conducts strategic marketing in the community to ensure its continued growth and to garner a greater percentage of external clients. Other challenges for the home care program include the following: Maintaining adequate staff: It can be challenging to recruit and retain enough qualified aides to meet the needs of a growing client base. Well-Spring Home Care leads the way with competitive pay rates for its staff. Regulations: Burdensome regulations can create barriers to growth. Well-Spring works with LeadingAge and other associations to educate policymakers about home care services. Sharing resources and staff talents with other strong, not-for-profit organizations has helped the organization address regulatory challenges. Reliance on philanthropy: Well-Spring relies on capital campaigns to support its CCRC, but the organization’s home and community-based services rely on philanthropy for support. Each year, Well-Spring holds fund-raising events and applies for foundation grants to fund its adult day program. Many reimbursements: The adult day program is challenged by its reliance on an increasingly complex mix of private-pay and publicly funded reimbursements. The program must follow rules and regulations for each funding source. Program leaders see the need to educate consumers and policymakers about the importance of adult 84 | Residential Provider Expansion into Home and Community-Based Services day in the continuum of care. They would like to see adult day eventually become a covered Medicaid benefit, if and when the Medicaid program is reformed. Perceived Benefits Well-Spring Services, Inc., has benefitted tremendously from efforts to promote its brand as a regional provider of aging services. The organization offers a variety of services to a broad spectrum of aging adults. Several clients who received care at home transferred to the CCRC campus when their care needs changed and they required higher levels of care. Well-Spring has enjoyed several other benefits including the following: Strengthened governing boards: Well-Spring has three boards that represent the CCRC and home care; PACE; and adult day services. Each board includes talented individuals with expertise in their fields. Cross-pollinating the talent in all of Well-Spring boards has benefitted the entire organization. However, it can be challenging to keep all board members informed of the organization’s varied activities. Expanded opportunities for staff: Well-Spring has strengthened the quality of its management team through the addition of individuals with expertise in the field of home and community-based services. By offering a diverse collection of services, Well-Spring has created additional job opportunities and career ladders for all staff and given managers the opportunity to expand their career horizons. Mission achievements: Well-Spring’s mission is to provide a continuum of services for older adults and improve their lives. New service lines have allowed the organization to serve older adults with a range of incomes and care needs. Consumers can receive a variety of services, and help navigating the care system, from one organization. New service lines have allowed the organization to serve older adults with a range of incomes and care needs. Financial sustainability: The Well-Spring management and board of directors did not anticipate that the organization would earn high net margins from its home and community-based services. However, Well-Spring has the advantage of offering an array of services to a larger number of older adults, while receiving reimbursement from multiple payers. A larger market: Well-Spring initially served only the small portion of older adults who wanted to live on a CCRC campus. Now, the organization can serve many more older adults with a variety of services. The home care model has given the organization a revenue stream and an expanding client base at a time when consumers are less interested in moving to a CCRC. Consumers who want to live in their own homes now have more care options. WELL-SPRING RETIREMENT COMMUNITY New partnerships: Providing home and communitybased services has improved Well-Spring’s standing in the community and expanded the number of organizations, including accountable care organizations, that now think of Well-Spring as a potential partner. In addition, adult day services could become a strong PACE partner if changing regulations introduce more flexibility into the PACE model. Lessons Learned Throughout its expansion process, Well-Spring has learned several lessons it would like to share with other providers who are considering expanding, including the following: Outcomes Well-Spring Home Care has not yet conducted a formal survey to evaluate its program. The program plans to administer client and employee satisfaction surveys in the next year or two. The adult day center conducts surveys of caregivers and participants. Key survey findings indicate that the program has improved the quality of life and health for caregivers and participants. In 2013-2014 majorities of caregivers reported: Reduced stress Increased knowledge of community services Ability to continue working, if needed Improved job performance, if working The perception that the service prevented a relative’s move to a long-term care setting The conviction that the value of service was worth the cost Caregivers reported that family members participating in the adult day program: Maintained or improved their chronic disease condition and felt better Maintained or improved sleep patterns (19% improved) Maintained or expanded conversation or communication (25% improved) Maintained or improved mobility and flexibility (34% improved). Maintained or increased personal hygiene (25% improved) Maintained or improved medical condition (25% improved) Decreased emergency care episodes Survey participants noted their appreciation for the friendships formed and the feeling of self-importance that clients experience at the adult day center. During interviews conducted in 2013-2014, a majority of adult day participants (88% or higher) reported: Feeling better coming to the program Experiencing less pain (if they normally have pain) Enjoying activities Receiving help as needed Being treated with dignity and respect The perception that coming to the program makes their life better Satisfaction with coming to the program Helping to lead activities Educate board members. Management should constantly and consistently explain the reasons why the organization should diversify its services and begin offering home and community-based services. The education process should continue even after the decision is made. Develop a mix of in-house and partnership programs. When collaborating with outside organizations, consider the organizational culture of the agency and make sure the organizations are compatible. Educate staff. Make sure staff members are familiar with home care trends and understand why it is beneficial for the organization to expand into the home care market. Resources that explore the future of aging services are often helpful in educating staff. Be patient. It takes time to understand and implement a new model of care. Build your referral network. Develop relationships with other organizations that can become referral sources for your services. Partner with competitors. It’s important to weigh whether you want to be a competitor or partner with other providers in your community. There are times when the partnership route brings the best return. Market community-based services differently. Marketing home and community-based services is different than marketing CCRC services. CCRC marketing tends to be based on word-of-mouth and resident satisfaction. Home care marketing is referral-based. In addition, prospective residents take their time when deciding to move to a CCRC. Home care clients make their decision quickly, often when they have an urgent need for services. Being available when the consumer needs help is critical. WellSpring makes itself available by building relationships with hospitals through the discharge process. Ask a partner to help you expand. Regulations governing home and community-based services are becoming more complex, whether they apply to care delivery, accounting or human resources. Partner with an established organization that has experience with the service you want to establish. That partner can help you understand how to operate within the regulatory environment. Sodexo • IAHSA • LeadingAge | 85 CONTINUING CARE AT HOME PROGRAMS 86 | Residential Provider Expansion into Home and Community-Based Services Case Study CADBURY SENIOR LIFESTYLES CHERRY HILL, NEW JERSEY | LEWES, DELAWARE | December 2014 Introduction Cadbury Senior Lifestyles operates two traditional, campusbased continuing care retirement communities (CCRC): Cadbury at Cherry Hill in New Jersey and Cadbury at Lewes in Delaware. Each of Cadbury’s CCRCs also offers the Cadbury at Home program, which brings traditional CCRC services into the private homes of program members. Cadbury was one of the first pioneers to offer this hybrid CCRC model, which has become known in the United States as Continuing Care at Home (CCaH). A CCaH member pays an entrance fee and a monthly fee in return for a comprehensive package of services that are provided for the remainder of the member’s life, unless the individual opts to cancel his or her membership. The service package typically includes access to a variety of home and community-based services, including home health care, home care, delivered meals, adult day programs, home-based technologies, home inspections and transportation. CCaH packages also provide access to assisted living and nursing care if and when that care is needed. Some CCaH membership plans offer an all-inclusive service package for no additional cost, over and above member’s entrance and monthly fees. Other plans require co-payments by the individual or through the individual’s long-term care insurance policy. A CCaH program strives to design and deliver a package of home and community-based services that will help CCaH members postpone or prevent the need for assisted living or nursing home care. Unlike traditional CCRCs, CCaH programs do not require their members to take up residence on a CCRC campus. As such, programs appeal to older consumers who are not interested in leaving their homes and who would probably never move to a CCRC campus. This study of Cadbury at Home was conducted during interviews with staff from the Cadbury Continuing Care at Home program and Cadbury Senior Lifestyles. Policy Context The majority of states in the United States have some type of regulation governing CCRCs. However, state CCRC regulations vary widely and can range from strict rules requiring fullfledged licensing or significant regulatory oversight, to moderate rules requiring minimal financial controls and consumer disclosures, or certificate of need oversight. Several states have minimal or no regulatory oversight of CCRCs. States regulators also take differing approaches to defining the type of CCRC services that can be delivered through an off-campus CCaH program. Some states take the view that CCRC existing regulations already cover the CCaH concept and do not need to be expanded to address this new model. In other states, however, the statutory or regulatory definition of a CCRC, or other regulations, have barred the development of CCaH programs by restricting CCRCs and CCRC contracts to the campus setting. In states that do not regulate CCRCs, there has been no need to consider any regulatory action regarding CCaH programs. Cadbury Senior Lifestyles operates the Cadbury at Home program in New Jersey and Delaware. The Department of Community Affairs (DCA) strictly regulates CCRCs in New Jersey. After Cadbury Senior Lifestyles educated DCA about CCaH programs, the department determined that the state’s existing CCRC regulations applied to these at-home programs and that the new model would not require a separate set of regulations. Sodexo • IAHSA • LeadingAge | 87 CADBURY SENIOR LIFESTYLES The Department of State regulates CCRCs in Delaware, which has fewer CCRC regulations than New Jersey. Cadbury was able to use the same disclosure statement it filed in New Jersey to open and run its CCaH program in Delaware. Expansion to Continuing Care at Home Cadbury Senior Lifestyles (formerly Cadbury Senior Services) has been a service provider since 1977, when it opened its first CCRC—Cadbury at Cherry Hill—to provide independent living, assisted living and nursing home care on one New Jersey campus. The organization also operates Cadbury at Lewes, a CCRC in Delaware; the Cadbury at Home CCaH program; Cadbury Consulting, a professional consulting firm; and Cadbury Foundation, the fundraising entity for Cadbury Senior Services and all its affiliates and services. In the mid-1990s, Cadbury Senior Services decided to expand the number of older adults it could serve. However, expansion through the CCRC model was not possible due to lack of land on which to build a bricks-and-mortar CCRC. The Cadbury at Home program was incorporated in 1998 as a way to reach and provide services to older adults who wanted to stay in their own homes and live independently. In 1995, Cadbury received a three-year grant from the Robert Wood Johnson Foundation to conduct a market study that would help it understand community needs and determine local interest in a CCaH program. Cadbury also used grant funds to educate the New Jersey Department of Community Affairs about the CCaH concept and work with the department to establish a regulatory structure for the new model. Cadbury’s research yielded the following findings: There was a market for a CCaH program, given the high percentage of older adults who wanted to stay in their own homes. Other existing programs targeted older adults living in their own homes. However, these programs were not tied to a CCRC. Many of the other at-home programs were not owned by a single organization. Rather, they operated as networks of providers from whom consumers could purchase individual services. With these findings in hand, the management and board of Cadbury Senior Services implemented a comprehensive process to determine whether to expand the organization’s services into the external community. The CCaH concept was new at the time and there were no other providers offering the program in New Jersey. Launching the program would be risky for Cadbury Senior Services and there were no guarantees that it would succeed. It took several years of board meetings and discussions to reach an agreement to expand Cadbury’s services beyond the CCRC campus. The board chair had initial concerns about diversifying the organization’s services and preferred, instead, to continue building on the organization’s existing services 88 | Residential Provider Expansion into Home and Community-Based Services and strengths. The board chair stood aside from the decision because he saw that the remaining board members wanted to move forward. Members of Cadbury’s marketing staff also raised concerns about establishing a CCaH program. They feared that Cadbury’s campus-based CCRCs would be competing with the CCaH program for the same type of customer. These fears proved to be unfounded. Cadbury’s experience has shown that CCRC and CCaH programs do not compete with each other. Different types of consumers are interested in each program. The two programs continue to work closely together. Process for Launching the Cadbury at Home Program Cadbury created a separate corporate entity for what would eventually become known as “Cadbury at Home.” This allowed the organization to reduce any risks that the program might pose for the corporate organization. The CCaH concept was relatively new at the time and management did not want any financial losses associated with the Cadbury at Home program to impact its established CCRC. Creating a separate CCaH entity made it easier to launch Cadbury at Home as an additional program under the CCRC’s existing license and certification. Program staff at Cadbury at Home worked with actuaries to price the CCaH program appropriately for individual members. This was a challenging task because a similar model did not exist. The Cadbury at Home program continues working with actuaries to assess and study its membership fees. Cadbury at Home also needed to balance the need for steady membership growth with the need to select the right participants for the program. Applicants are accepted into the Cadbury at Home based on their financial and medical eligibility. The medical underwriting process is more stringent for individuals seeking to join the program than for individuals seeking to qualify for the CCRC. Description of Cadbury at Home Cadbury at Home combines several long-term services and supports—including home care, assisted living, nursing home and the financial protection of long-term care insurance—into one comprehensive program. Individuals pay a membership fee and a monthly maintenance fee. In return, they receive appropriate long-term services and supports as their health changes. Individuals are interested in the Cadbury at Home program for a variety of reasons, including the difficulties associated with activating a long-term care insurance policy. For example, many long-term care policies cannot be activated until a person needs assistance with at least two activities of daily living (ADL). In addition, many policies have an “elimination period,” which can range from 30 to 180 days. The elimination period represents the time it takes for the long-term care insurance policy to be activated once a person demonstrates a need for a service. During this period, policyholders must pay all care expenses out of pocket. The Cadbury at Home program is working with actuaries to blend program membership with long-term care Timeline CADBURY SENIOR LIFESTYLES 1977 Began as a continuing care retirement community in Cherry Hill, NJ. 1995–1998 1998 Conducted market research study to determine interest for the “at home” program, funded by the Robert Wood Johnson Foundation. Incorporated Cadbury at Home program in Cherry Hill, NJ. 2007 Opened continuing care retirement community in Lewes, DE. 2015 Began operating Cadbury at Home program in Lewes, DE. Sodexo • IAHSA • LeadingAge | 89 CADBURY SENIOR LIFESTYLES insurance to reduce gaps in coverage. The blended coverage abolishes the elimination period and pays for services not covered by long-term care insurance. The Cadbury at Home program has advantages over longterm care insurance for the following reasons: It is easier for Cadbury at Home members to activate services. Members can receive services after they demonstrate the need for assistance with only one ADL. The Cadbury at Home program provides lifetime coverage and is much more comprehensive and personalized than many long-term care insurance policies. For example, the program’s personal care coordinators work with members and their family members to make sure members receive the assistance they need. Admission Criteria Individuals must be at least 60 years old to qualify for Cadbury at Home. The program also considers the financial situation and medical needs of the person seeking membership. Applicants are required to submit five years of medical notes from their physicians and other health care providers. Persons with managed chronic conditions may meet the criteria for membership. However, persons with an existing diagnosis of neurological issues or any type of dementia will not be considered. The program’s personal care coordinator administers a Mini-Mental State Examination and other tests to determine an applicant’s cognitive health. A Review and Admissions Committee works with the program’s medical director to determine whether an applicant qualifies for Cadbury at Home. The committee consists of the program’s executive director, care coordinator and members of the sales and marketing team. Each person on the review committee interacts with the prospective member to determine whether the applicant is appropriate for the program. The care coordinator conducts an extensive assessment of the prospective member and develops a relationship with the individual and his or her family. Assessments and screenings include the following: Cognitive tests Functional assessments Geriatric screenings A home screening The home screening is designed to make sure the prospective member’s home is appropriate for aging in place. If the home has a staircase, for example, the care coordinator might inquire about the family/individual’s willingness to install a stair glide. The care coordinator might also determine whether the family/ individual is willing and able to place a hospital bed or another type of bed on the home’s first floor if the prospective member’s bedroom is located on an upper floor. Marketing and sales representatives inform and educate potential members about the program. This interaction provides an opportunity for staff to gauge whether the prospective member is appropriate for the program. The sales team is trained to recognize circumstances or situations that would make a prospective member ineligible. Based on their interaction with the prospective member, team members offer their input to the Review and Admissions Committee. Couples applying to the Cadbury at Home program could find that one spouse is eligible for the program while the other does not meet the program’s criteria. The person who does not qualify can participate in a Consultative Care Program, which features a fee-for-service contract with no up-front or ongoing monthly service fees. Another program, called the Consultative Care PLUS program, requires an upfront payment of $7,000 and a $350 monthly fee covering 12 hours of services and two hours of care coordination per month. Participants pay for additional services on a fee-for-service basis. Services The following services are offered to Cadbury at Home members: Home care companion/homemaker Home health care provided by a home health aide A live-in companion, when needed Delivered meals, if their need is due to a medically necessary or temporary situation, and if they are provided by a home health aide Adult day services Access to an emergency response system Transportation for medically necessary outpatient surgery, short procedures or planned hospitalizations, as long as they are recommended by a physician A safety and functional inspection of the home, conducted by a licensed occupational therapist during the first year of membership and thereafter, as needed Access to assisted living and nursing care, when needed In addition, the Cadbury at Home program provides a number of other services that do not involve direct care delivery. These services include: Marketing and sales representatives inform and educate potential members about the program. This interaction provides an opportunity for staff to gauge whether the prospective member is appropriate for the program. 90 | Residential Provider Expansion into Home and Community-Based Services CADBURY SENIOR LIFESTYLES Table 1. Membership Options PAYMENT PLANS Type of Service Platinum* Gold GoldPlus** Silver Bronze HEALTH SUPPORT SERVICES Home health aide 100% 100% 100% 85% 100% Companion/homemaker 100% 100% 100% 85% 100% Live-in companion 100% 100% 100% 85% 65% Delivered meals 100% 100% 100% 85% 100% Adult day program 100% 100% 100% 85% 100% Emergency response 100% 100% 100% 100% 100% Home inspection 100% 100% 100% 100% 100% Transportation 100% 100% 100% 10% 100% 100% 100% 100% 70% 0% 100% 100% 100% 70% 0% ASSISTED LIVING CARE NURSING HOME CARE *Cadbury at Home will refund 90% of the membership fee to a Platinum member’s estate. ** A GoldPlus member must maintain a long-term care insurance policy that meets Cadbury at Home’s criteria. Social and member events: The program hosts three or four luncheons per year and monthly gatherings where members can get acquainted and create a network. It also sponsors book clubs, day excursion trips, exercise classes, arts and craft classes, wellness seminars, speakers and other events. These events are offered for free or a nominal fee. Service referrals: The program offers referrals for various types of home-related services, including handyman services, housekeeping, medical equipment, bathroom conversion, lawn service and transportation. Members are responsible for covering the cost of these services. Some providers offer a 10% discount to Cadbury at Home members. Some Cadbury at Home service providers also deliver services to residents on the CCRC campus. This arrangement is based on the quality of the providers’ services, not on any prearranged agreement between the program and the service providers. Cadbury at Home members can move to the CCRC’s campus if they require greater assistance or simply prefer campus living. The cost for assisted living or nursing home care for Cadbury at Home members can be significantly reduced, depending on the membership plan. For example, when members transition from their homes to a Cadbury nursing home, they will continue paying the Cadbury at Home monthly fee for their plan type, rather than the $12,000/month nursing home rate. In a case where a Cadbury at Home member and a CCRC campus resident are vying for the same spot in the nursing home, the campus resident has priority. Sources of Reimbursement Cadbury at Home is a private-pay program. Some services, such as at-home care after a hospitalization, are eligible for Medicare coverage. The CCaH team encourages members to maintain their Medicare and supplemental insurance. Members sign an addendum to the membership contract stating that Cadbury is not responsible for any co-payments or medical expenses. Membership Plans and Fee Structure Cadbury at Home offers five different lifetime membership options: Platinum Gold Gold Plus Silver Bronze Sodexo • IAHSA • LeadingAge | 91 CADBURY SENIOR LIFESTYLES Table 2. Average Fee Structure PLAN INITIAL FEE MONTHLY FEE Gold $58,000 $466/month Silver $49,601 $455/month Bronze $26,534 $368/month Services available to members do not vary by plan. However, membership costs and possible co-payments do differ by plan. The Gold and Platinum membership plans offer 100% coverage for services and carry a stable monthly fee. The other plans require some type of co-pay for services. Members who choose the all-inclusive Gold Plan receive all services without paying any additional fees. This is the most expensive plan available to members. The majority (63%) of Cadbury at Home members have Gold, Platinum or GoldPlus memberships. GoldPlus integrates an individual’s existing long-term care insurance coverage into the plan. Individuals have various reasons for choosing a specific plan, including their financial situation and their level of comfort with taking risks. Individuals who choose Gold or Platinum plans tend to be risk-averse and anticipate needing services in the future. Cadbury at Home fees depend on the age of the applicant and the type of membership plan he or she chooses. Each member pays an initial membership fee and a monthly fee. Table 2 provides an example of the average fees associated with each plan for a 75-year old member. Membership As of 2014, the Cadbury at Home program had over 200 members. The number of new members continues to grow. Typically, the program enrolls 30 new members each year. Four hundred members have joined the program since it began. The flexible CCaH model does not limit the number of people who can enroll in the program. Each care coordinator is responsible for approximately 75 members. When membership expands, additional care coordinators are added as needed. Program demographics indicate that Cadbury at Home members have these characteristics: Overall, members are “healthy and active,” although their health problems have increased over the years. Members’ average age has consistently been 76.6 years throughout the history of the program. Prospects in the organization’s Delaware program are younger than New Jersey prospects. Many new members in Delaware are in their early or mid-60s. More than half (53%) of the members are couples. Among 92 | Residential Provider Expansion into Home and Community-Based Services single members, there is a 2:1 ratio of women to men. Almost half of members who joined the program in the past three years have long-term care insurance. While Cadbury at Home participants can cancel their membership at any time, only two members have left the program during the past few years. In general, members who leave the program lose 2% of their entrance fee for each month they belong to the program. Cadbury at Home has revised its membership guidelines to allow members to move from one location to another as long as the program receives sufficient notice and is able to contract for services in the person’s new locale. If costs at the new location are higher than the previously quoted rate, the member pays the difference. In the past, Cadbury at Home membership was not portable. Members who moved were dropped from the program. Partnerships Cadbury at Home contracts with partner agencies that provide the program’s at-home services. The CCaH team follows a comprehensive process when selecting partner agencies. The team: Meets with key staff at the prospective partner agency Interviews agency staff members about the agency’s history, services provided, organizational challenges and staffing issues Requires each agency to complete an application requesting information about licensing, insurance certifications, and other business-related documentation The Cadbury at Home team uses a consensus process to decide whether to accept a service provider agency as a partner. The team will stop using the services of a contracted agency if that agency does not meet the program’s standards of care. Workforce The Cadbury at Home program has a small, but strong workforce that is separate from the Cadbury CCRC staff. Cadbury made this decision because it wanted clearly defined, separate teams to focus on the needs of each program. The CCRC and CCaH programs do share human resources and finance staff with the parent organization. Key positions within the Cadbury at Home program include: Care coordinators Office manager Program director Executive director Director of marketing Retirement counselor Program demographics indicate that Cadbury at Home members have these characteristics: The Cadbury at Home team recommends the following staffing positions for a new program: Program Director Sales representative One care coordinator for every 60-70 members Part-time administrative assistant The Cadbury at Home program team has faced few, if any, challenges in the area of workforce. The CCaH model posed the most challenges for the sales team, which had to learn how to build relationships with prospective members, identify medical conditions that would prohibit people from enrolling in the program, and help members function independently in their own home. Program Director The Cadbury at Home team recommends that the program director have a social work or marketing background, as well as experience with long-term services and supports. Care Coordinator The care coordinator, who typically is a licensed Master of Social Work, is the backbone of the Cadbury at Home program and sets the program apart from other long-term care options. The care coordinator is proactive and works as an extension of the member’s family to keep the member independent, healthy and living at home. The care coordinator carries out the following roles: Links members with needed resources Connects by telephone with members at least once every three months Conducts in-person visits once each year, at a minimum, to assess the individual and his or her needs. Visits members who are in the hospital Assists members and helps them understand how to use their Medicare and long-term care insurance benefits The average care coordinator carries a caseload of approximately 75 members. This caseload is manageable because most Cadbury at Home members are healthy and independent. Only a few members require services or use the care coordinator extensively. The number of service coordinators employed by a CCaH program will depend on the size of the program. The New Jersey Cadbury at Home program employs three care coordinators. In Delaware, the program director also serves as the care coordinator due to the program’s small size. Overall, members are “healthy and active,” although their health problems have increased over the years. 76.6 Average age throughout history of the program. Delaware is the exception, with many new members in their mid-60s. 53 2:1 % members who are couples. ratio of single women to men 50 % of members who joined the program in the past three years who have long-term care insurance. Sodexo • IAHSA • LeadingAge | 93 CADBURY SENIOR LIFESTYLES The care coordinator is the backbone of the Cadbury at Home program and sets the program apart from other long-term care options. The care coordinator is proactive and works as an extension of the member’s family to keep the member independent, healthy and living at home. Organizational Culture The organizational culture of the Cadbury at Home program is similar to Cadbury’s CCRC and parent organization. The CCRC and CCaH programs do not compete with each other because they cater to different types of individuals. The Cadbury at Home program is mission driven. It was established as a way for Cadbury to provide another option for individuals to access needed long-term services and supports. The Cadbury at Home program and Cadbury’s CCRCs work together to support individuals in their decisionmaking process. For example, during the initial assessment of prospective members, a staff person may determine that the CCRC is a better option than the CCaH program or vice-versa. Older adults from a variety of cultures take advantage of the Cadbury at Home program rather than moving to one of Cadbury’s CCRC campuses. For example: Members of the Lesbian, Gay, Bisexual and Transgender population in Delaware prefer to stay in their own homes and not move to a CCRC campus. This group has been a key audience for the Cadbury at Home program. The Cadbury at Home program is making headway with the Indian community because adult children, who would have cared for their parents in the past, are not always available to provide services and supports to relatives. Despite its appeal to a variety of populations, the Cadbury at Home program has not faced significant challenges related to cultural diversity. The program works with outside organizations to train and educate its staff in this area. Financial Implications Cadbury at Home’s initial start-up expense was approximately $500,000. A CCRC board member provided a line of credit to launch the program and was repaid within three years. It is estimated that the start-up costs for implementing a similar program today would be higher, probably in the area of 94 | Residential Provider Expansion into Home and Community-Based Services $800,000 to $1,000,000. CCaH programs do not require the development of bricksand-mortar buildings and can continue to serve an increasing number of older adults. On average, a provider can expect losses for four or five years, followed by positive cash returns. The program generally requires 125 to 150 members to break even. The Cadbury at Home program broke even around Year 3. A similar program will likely have a slower growth rate today than the growth rate Cadbury experienced in the late 1990s because prospective members have less disposable income due to the recession. The economic climate was the primary reason the Cadbury at Home program was established as a separate entity from Cadbury’s CCRC. Because the CCaH model was new, Cadbury did not want to put the CCRC at risk if the new program ran into trouble. One disadvantage of this approach is that CCaH revenues must also be kept separate and cannot be used to support the CCRC. Perceived Challenges A CCRC considering implementing a CCaH program may face some operating barriers and challenges. The Cadbury at Home program’s greatest challenges are: The economy: The economy can impact the financial strength of a CCaH program. Since the Cadbury at Home program relies on disposable income, interest in the program declines when the economy is down. Consumer needs: Understanding the needs of people who sign up for a CCaH program can be challenging. Program developers need to balance several goals, including keeping the program affordable, aligning it with long-term care insurance products, and ensuring that program fees are actuarially sound. Managing utilization of program services: A CCaH program will experience losses if the utilization of services is too high. Program flexibility has allowed the Cadbury at Home program to enjoy a growing membership. But early members have aged over the program’s 15-year history and now have greater health care needs. Care coordinators help keep service utilization in balance by using services creatively and anticipating and addressing health-related issues early before they become expensive health crises. The Cadbury at Home program is mission driven. It was established as a way for Cadbury to provide another option for individuals to access needed long-term services and supports. CADBURY SENIOR LIFESTYLES Marketing the program: Educating older consumers so they understand the CCaH concept is one of the greatest challenges in marketing the Cadbury at Home program. Many consumers do not understand that they will continue to live in their own home and that bundled services are brought to them. Education is a very important strategy to distinguish the program from the traditional CCRC. Perceived Benefits A CCaH program can provide several benefits for the organization and the consumer: Adapts to the needs and desires of the consumers: Cadbury at Home fulfills a consumer’s desire to receive services at home. More people, especially members of the next generation of older adults, want to age in their own homes. Fewer people want to move onto a CCRC campus. Protects the assets of the consumers: The cost of long-term care insurance is “astronomical” and continues to grow, according to Cadbury at Home staff. Many consumers are unaware of the gaps and costs associated with long-term care insurance. Creates consumer awareness of CCRC options: This awareness will be important when the individual or family member requires assisted living or nursing home care or decides to move to a campus setting. Expands the organization’s reach: CCRCs with CCaH programs can serve more older adults. Creates a sense of community: The Cadbury At Home program offers older adults living outside the CCRC campus an opportunity to connect with their peers in the community and use services and amenities on the CCRC campus. The Cadbury at Home program is considering the development of a CCaH program for low-income individuals. According to current plans, the program would be governmentsubsidized and would follow the basic format of the current Cadbury at Home program. The current political climate makes it difficult to seek the investment required to carry out this plan. However, the Cadbury at Home team believes the program could save federal and state government funds by reducing hospitalizations and use of nursing homes among older adults. Outcomes The Cadbury at Home team has conducted evaluations of the program through member satisfaction surveys. The survey results show that current members feel they are: The Cadbury at Home team also believes that its bundled services have helped members stay at home. Since its inception, the program has not had more than two people require nursing home care at any one time. Only one of the program’s 200 members was receiving services and supports in a long-term care setting at the time of this study. Lessons Learned Cadbury at Home was one of the first programs to provide bundled at-home services to residents in the community. Several CCRCs have modeled their program after Cadbury’s model and worked with Cadbury’s consulting firm to research, develop and implement the program. Cadbury provides training for organizations and programs seeking to implement a similar program. Cadbury Consulting trains organizations in four areas: Admission process Role of the care coordinator Role of the sales and marketing teams Effective strategies for operating the program The Cadbury at Home program has learned many lessons that can assist other CCRCs considering a CCaH program. Recruit and enroll the right members. Complete a prudent evaluation to ensure that prospects qualify, both medically and financially. Find the right staff. Staff members should have the right personality and background to launch and operate a CCaH program. Successful staff members will be entrepreneurs at heart. Offer different payment options. A CCaH program will capture more people who want to age in place than a “traditional” CCRC can. The financial opportunity is great because the program is not limited to high-income individuals. Offering different payment options makes program membership feasible for more individuals. Do not create a separate entity for the CCaH program. Making the program part of the overall organization will allow it and the CCRC to benefit from each other. Do not market the CCaH program in the same way you market the CCRC. Primarily, the Cadbury at Home program uses direct mail with testimonials. The team also relies on referrals and informational sessions with financial experts and elder care attorneys. Large seminars are conducted throughout the year and are successful. However, the Cadbury at Home team has learned that smaller group seminars of six to 10 people can also be very effective. Satisfied Meeting their desire to stay at home to receive services Protecting their assets and not burdening their families Content they have a plan in place to allow them to age in their own home Sodexo • IAHSA • LeadingAge | 95 CONCLUSION Eight nursing homes, continuing care retirement communities (CCRC) or CCRC-like entities in the United States, Australia, Canada and Switzerland expanded their business lines to include the delivery of home and community-based services (HCBS). In addition, one CCRC in the United States created an innovative way to deliver a comprehensive package of CCRC services to older adults living in their own homes. The organizations participating in this study differed in a number of ways, including: Design of the current HCBS line Number of years since the initial expansion Size of the workforce Number of clients served Primary payer sources Regulatory challenges encountered while operationalizing the program Despite these differences, organizations shared many of the same aspirations, faced common challenges, enjoyed similar benefits, and learned a variety of lessons during the expansion process. Organizations diversified their service lines for a combination of reasons. All wanted to fulfill their organization’s mission and reach a greater percentage of the vulnerable, older adult population. HCBS programs allowed providers to offer a continuum of care, including care in the home, through one organization. Additionally, home and community-based services were viewed as a feeder program for an organization’s retirement community and a source of additional revenue for the organization. The home environment and the residential setting attract different types of workers. Home care workers tend to desire more independence and handle a multitude of tasks in their daily work. While most organizations used separate groups of aides in their residential and home-based settings, both service lines typically shared support functions like billing and human resources. Providers faced several challenges while establishing and operating their HCBS programs. Among the greatest challenges 96 | Residential Provider Expansion into Home and Community-Based Services were market competition and the ability to distinguish a program from the competition. HCBS programs often operated at a loss for the first year, before breaking even. Regulatory limitations or moratoriums on new providers presented barriers for some organizations seeking to provide specific home and communitybased services, such as home health care. Some providers faced difficulties finding qualified staff and ensuring that new hires represented a “good fit” for the home setting. Despite these challenges, providers identified several benefits associated with an expansion into home and community-based services. For example, the expansion process helped organizations fulfill their mission and provide services to a greater number of older adults, including individuals who want to age in their own homes. Several HCBS programs generated profits that helped support the larger organization. Finally, the provision of home and communitybased services helped providers develop relationships with people in the community and secure referrals to on-campus services. The organizations learned many lessons through the expansion process. Most providers emphasized the importance of conducting market research to understand the competition, identify business models that are thriving in the local market, ascertain gaps in local services, and create a niche for the organization’s services. The providers learned that referral-based marketing strategies work better for home and community-based services and differ from the word-of-mouth marketing strategies that work best for residential services. This lesson underscored the importance of establishing a network and relationships with potential referral sources in the community. Organizations looking to expand into home and communitybased services have a number of options as they operationalize their plans. These organizations can start a new program, make selective acquisitions of existing programs, or develop strategic partnerships that can share the risks and responsibilities associated with expansion. Organizations should take adequate time during the planning process to determine which option is best for them. Footnotes 1 One agency: Interview with the one supervisor for all staff. 2 NORC staff members provide residents with social work, nursing, health education and benefits enrollment. 3 A CCRC is a retirement community that offers several levels of health care on one campus: 1) Independent Living for residents who do not need assistance; 2) Assisted or Supportive Living for those who require little supportive help with activities of daily living; and 3) Skilled nursing or rehabilitation care (short-term and long-term care). 4 Program of All-Inclusive Care for the Elderly or PACE is a program that coordinates the care for each person enrolled in the program based on their needs through comprehensive services and supports. 5 One aging service provider offered a different model of the home and community-based services. This program is not included in the overview of the providers. 6 Formerly known in Australia as “hostel care,” low-care nursing homes allow people to live in independent units while providing all meals and assisting clients with chores and some activities of daily living and instrumental activities of daily living. This service seems to be similar to the assisted living concept in the United States and Canada. 7 High-care settings provide care that resembles nursing home care in the United States. 8 According to the Australian Institute of Health and Welfare, permanent residential aged care is offered to people who can no longer be supported living in the community. A residential aged care facility assesses the care needs of residents requiring permanent care. Depending on a person’s assessed needs, permanent care is currently offered at two levels: low care and high care. Permanent residents receiving low care require accommodation and personal care. Residents receiving high care require 24-hour nursing care in addition to their low-care needs. 9 Private insurance does not fund most home-based care. 10 Feros Care was recently chosen as one of 13 organizations in Australia to operate a Regional Assessment Service. 12 A naturally occurring retirement community is a community that was not originally designed for seniors, but that has a large proportion of residents who are older adults (at least 60 years old). These communities are not created to meet the needs of seniors living independently in their homes, but rather evolve naturally, as adult residents age in place. 13 The White House Conference on Aging is a oncea-decade conference sponsored by the Executive Office of the President of the United States which makes policy recommendations to the president and Congress regarding the aged. 14 The Centers for Medicare & Medicaid Services (CMS) is a U.S. federal agency that administers Medicare (federal health insurance for older adults), Medicaid (federal health insurance for low-income individuals), and the State Children’s Health Insurance Program (federal health insurance for low-income children). 15 Australian Government: Department of Social Services website 16 A Medicare certified home health agency is approved by Medicare and meets certain health and safety requirements. 17 Medicare is the federal health insurance program for persons 65 and older, certain younger people with disabilities, and people with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD). 18 Older adults live in a home-like setting where they can remain as independent as possible while accessing accommodations and services that meet their changing needs. 19 Shepherd’s Care at Home website: http:// shepherdscareathome.com/ 20 PACE is a home and community-based services program that provides comprehensive and coordinated services and supports to older adults based on their individual needs. The program is designed to help individuals with a nursing home level of need to continue living in the community, rather than moving to a nursing home or other care setting. 21 Accountable care organizations are groups of doctors, hospitals, and other health care providers who come together voluntarily to deliver coordinated high quality care to their Medicare patients. 11 These programs include FerosFitnesForever, which offers nutritional, exercise and stressreduction counseling and other activities. Sodexo • IAHSA • LeadingAge | 97 98 | Residential Provider Expansion into Home and Community-Based Services


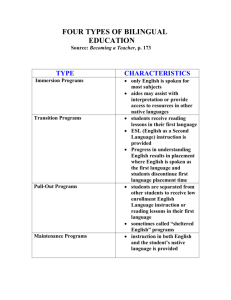
![See our handout on Classroom Access Personnel [doc]](http://s3.studylib.net/store/data/007033314_1-354ad15753436b5c05a8b4105c194a96-300x300.png)