Reliability of Radiographic Parameters in Neuromuscular Scoliosis
advertisement

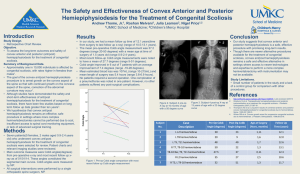
SPINE Volume 32, Number 6, pp 691– 695 ©2007, Lippincott Williams & Wilkins, Inc. Reliability of Radiographic Parameters in Neuromuscular Scoliosis Munish C. Gupta, MD,* Shirvinda Wijesekera, MD,储 Allen Sossan, DO,† Linda Martin, MD,† Lawrence C. Vogel, MD,§ Jennette L. Boakes, MD,‡ Joel A. Lerman, MD,‡ Craig M. McDonald, MD,‡ and Randall R. Betz, MD† Study Design. Retrospective review of radiographic data. Objectives. This study sought to define interoberserver and intraobserver variability to further delineate reliable means by which radiographs of patients with neuromuscular scoliosis can be examined. Summary of Background Data. Previous studies analyzed the use of Cobb angles in the measurement of idiopathic and congenital scoliosis, but no study until now describes a critical analysis of measurement in evaluating neuromuscular scoliosis. Methods. Forty-eight patients with neuromuscular scoliosis radiographs were reviewed. These were evaluated for Cobb angle, end vertebrae selection, Ferguson angle, apex of the curve, C7 balance, pelvic obliquity, Risser sign, status of the triradiate cartilage, kyphosis Cobb angle, endplate selection for kyphosis, and kyphotic index. Interclass and intraclass variability was examined with statistical analysis. Results. Cobb angle had an intraobserver variability was 5.7° and the interobserver variability was 14.8°. The intraobserver and interobserver variability for Ferguson angle was 6.8° and 20.6°, respectively. The kyphotic Cobb angle intraobserver variability was found to be 17.4°, and the interobserver variability was 24.01°. Conclusions. Neuromuscular scoliosis radiographs can be reliably analyzed with the use of Cobb angle. Other forms of analysis, such as Ferguson angle, are not as reliable. Pelvic obliquity should be measured from the horizontal, as other methods are not as reliable. Kyphosis is best evaluated with the use of the kyphotic Cobb angle. Finally, it is felt that a separate anteroposterior pelvis radiograph should be used to assess skeletal maturity, as scoliosis films often truncate the vital anatomy necessary to determine skeletal maturity. Key words: neuromuscular scoliosis, Cobb measurements, pelvic obliquity, kyphosis, sagittal balance, coronal balance. Spine 2007;32:691– 695 From the *University of California, Davis, Department of Orthopaedic Surgery, Sacramento, CA; †Shriners Hospital for Children, Philadelphia, PA; ‡Shriners Hospital for Children, Northern California, Sacramento, CA; §Shriners Hospital for Children, Chicago, IL; and 储Orthopaedic Group, New Haven, CT. Acknowledgment date: June 30, 2005. First revision date: December 14, 2005. Second revision date: July 24, 2006. Acceptance date: July 26, 2006. The manuscript submitted does not contain information about medical device(s)/drug(s). No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. Address correspondence and reprint requests to Munish C. Gupta, MD, University of California, Davis Medical Center, 4860 Y Street, Suite 3800, Sacramento, CA 95817; E-mail: munish.gupta@ucdmc. ucdavis.edu Neuromuscular scoliosis represents a well-known form of scoliosis, with numerous etiologies. Many measurements are used in the analysis of this form of scoliosis. Previous studies have analyzed the use of Cobb angles in the measurement of idiopathic and congenital scoliosis, but no study until now describes a critical analysis of measurement in evaluating neuromuscular scoliosis.1–7 The study represents the first study analyzing the reliability of radiographic measures in neuromuscular scoliosis. This study was undertaken to define interobserver and intraobserver variability to further delineate reliable means by which radiographs of patients with neuromuscular scoliosis can be examined. Materials and Methods Forty-eight patients with neuromuscular scoliosis were selected for evaluation. The posterior-anterior and lateral radiographs on 14 inch ⫻ 36 inch film of 48 patients with neuromuscular scoliosis were obtained. These radiographs were obtained with all of the patients in a seated position. The examiners were 2 attending spine surgeons, 2 attending pediatric orthopaedists, one pediatrician with 20 years of experience in spinal cord injury, one spine fellow, and one resident. The radiographs were copied for each investigator without any markings. Ten sets of films were duplicated and redistributed to the physicians for measurement, for the purpose of evaluating intraclass measurement error. The radiographs were evaluated for Cobb angle, end vertebrae selection, Ferguson angle, apex of the curve, C7 balance, pelvic obliquity, Risser sign, status of the triradiate cartilage, kyphosis Cobb angle, endplate selection for kyphosis, and kyphotic index. The Cobb angle was measured in manner consistent with clinical practice, as we felt that this best represented most appropriate comparison to a clinical setting. End vertebrae were selected by each examiner and recorded. Measurements were conducted with protractors and radiograph pencils available to each examiner. No predetermined levels were given to examiners or were marked on the radiographs. Curve locations were identified and recorded. Thoracic curves were identified with an apex between T5 and T11–T12 disc. Thoracolumbar curves were those with an apex between T12 and L1. Lumbar curves were those with an apex at the L1–L2 disc or below. The C7 balance was measured numerically. The value of line A was found by measuring a line drawn perpendicular from the vertical edge of the left side of the film to the center of S1. The value of line B was found by measuring a line drawn perpendicular from the vertical edge of the left side of the film to the center of C7. Thus, the C7 balance was calculated by the length of line B subtracted from the length of line A, as shown in Figure 1A. 691 692 Spine • Volume 32 • Number 6 • 2007 Figure 1. A, C7 balance ⫽ distance from edge of film to center of S1 ⫺ distance from edge to center of C7. B, Ferguson angle ⫽ angle subtended between lines drawn through the center of the vertebral bodies intersecting at the apex of the curve. C, Kyphotic index ⫽ straight line distance between endplate vertebrae divided by the perpendicular distance from the apex of curve to line A. The Ferguson angle was measurement by measuring a line drawn through the center of the vertebral bodies intersecting at the apex of the curve, as in Figure 1B. Then possible Risser sign was measured from the posteroanterior radiograph and recorded. Whether the triradiate cartilage was open or closed was also measured from the posteroanterior radiograph and recorded, when possible. The kyphotic Cobb angle was measured by selecting the end vertebrae and then calculating a Cobb angle between the 2 levels. The kyphotic index was measured by dividing the measurement of a line A by the measurement of a line B, as in Figure 1C. Line A was defined as the straight line distance between the end vertebrae endplates. Line B was defined as the perpendicular distance from the apex of the curve to line A. Pelvic obliquity was calculated according to 3 methods, as seen in Figure 2. The first method (Figure 2A) entailed drawing a line through the spinous processes of L4 and L5. Then a line was drawn perpendicular to a line drawn across the top of the iliac crests. The angle subtended between the spinous process line and the iliac crest line was the pelvic obliquity. A second method was also used. This pelvic obliquity angle measurement was angle subtended by a line drawn across the top of the iliac crests and the perpendicular line to the T1 to S1 line (Figure 2B). The third method of calculating pelvic obliquity was an angle subtended by a line drawn along caudal level of major Cobb curve and a line drawn along the top of the iliac crests (Figure 2C). A statistical analysis was then conducted. A Pearson correlation was used to evaluate the variables for interclass and intraclass correlation. Cohen’s kappa measurement for dichotomous measures was used to analyze non-numerical data, such as the status of the triradiate cartilage. Results Cobb angles were found to have a range of interclass correlation of 0.82 to 0.982. The interclass correlation coefficient was 0.991 for Cobb angles. The intraclass correla- Figure 2. A, Pelvic obliquity by Mubarak method ⫽ angle subtended between lines drawn from the perpendicular to a line across the iliac crests and a line drawn through the spinous process of L4 and L5. B, Horizontal pelvic obliquity ⫽ angle subtended by a line drawn across the top of the iliac crests and the perpendicular line to the T1 to S1 line. C, Endplate obliquity ⫽ angle subtended by a line drawn along caudal level of major Cobb curve and a line drawn along the top of the iliac crests. Radiographic Parameters in Neuromuscular Scoliosis • Gupta et al 693 tions had a range of 0.785 to 0.988. The intraobserver variability was 5.7° and the interobserver variability was 14.8°. The Ferguson angle had an interclass correlation range of 0.74 to 0.970, with a correlation coefficient of 0.983. The intraobserver variability for Ferguson angle was 6.8°. The interobserver variability for Ferguson angle was 20.6°. Thus, Cobb angles were found to have better inter and intraobserver reliability compared with Ferguson angle. Kyphotic Cobb angle was found to have a range of interclass correlation of 0.775 to 0.943, with a correlation coefficient of 0.991. The intraclass correlation for kyphotic Cobb angle had a range of 0.882 to 0.999. The intraobserver variability was found to be 17.4°, and the interobserver variability was 24.01°. The kyphotic index had an interclass correlation range of ⫺0.041 to 0.942; the correlation coefficient was 0.898. The kyphotic index had an intraclass correlation range of ⫺0.542 to 0.993. Thus, kyphotic Cobb angle was noted to have a superior intraobserver and interobserver variability. The broad range of results for kyphotic index indicates a wide array of data points, thus making this measurement parameter difficult to use in a clinical setting. The results of the 3 methods of measuring pelvic obliquity produced an interclass correlation coefficient of 0.889 for lumbosacral obliquity, 0.950 for the Mubarak method, and 0.972 for the obliquity to the horizontal. This had an interclass correlation range of 0.102 to 0.931, 0.470 to 0.897, and 0.564 to 0.931, respectively. The intraclass correlation range was 0.462 to 0.967 for lumbosacral obliquity, 0.154 to 0.967 for the Mubarak method, and 0.323 to 0.936 for obliquity to the horizontal. On review of these measurements, the obliquity to the horizontal was thought to have the best overall interclass and intraclass correlations. The coronal C7 balance was found to have an interclass correlation range of ⫺0.326 to 0.819, with a correlation coefficient of 0.527. The intraclass correlation range for the coronal C7 balance was ⫺0.419 to 0.990. This demonstrated a wide variation in the coronal C7 balance between both interobserver and interobserver measurements. The interclass correlation for Risser sign had a range of 0.519 to 0.991, with a correlation coefficient of 0.970. The Risser sign was missing in 26.3% of the sample. The intraclass correlation range was 0.740 to 1.0. Triradiate cartilage status was examined with Cohen’s kappa measurements for dichotomous measures. This found a Cohen’s kappa coefficient of 0.894. The triradiate cartilage status was missing in 58.9% of the sample. On review of these 2 measures of maturity, it was thought that they were inadequate. Often the radiographs did not adequately visualize the pelvis. This accounts for the high percentage of missing values in the samples. This is an important point, as this replicates clinical practice; the triradiate cartilage is located more caudally and is even more frequently missing than the iliac crests. In clinical practice, we often find that the pelvis is inadequately Table 1. Interclass Correlations for (Interval-Level) Radiographic Measures Interclass Correlation Coefficient Range of Correlations Between Investigators %Values Missing (n ⫽ 384) 0.991 0.983 0.527 0.889 0.950 0.972 0.970 0.991 0.898 0.820 to 0.982 0.740 to 0.970 ⫺0.326 to 0.819 0.102 to 0.931 0.470 to 0.897 0.564 to 0.931 0.519 to 0.997 0.775 to 0.943 ⫺0.041 to 0.942 5.5 10.7 8.9 12.8 22.9 9.6 26.3 13.8 22.1 Cobb angle Ferguson angle Balance C7 Pelvic obliquity Pelvic obliquity (Mubarak) Pelvic obliquity to horizontal Risser Kyphotic Cobb angle Kyphotic index imaged to evaluate the Risser sign or the status of the triradiate cartilage. Tables 1 and 2 summarize the findings for interclass and intraclass correlation, respectively. Table 3 summarizes the findings for the dichotomous measures of lowest instrumented vertebrae and triradiate cartilage. Finally, Table 4 summarizes the interclass and intraclass variability for angular measurements. Discussion Many authors have studied the accuracy of radiographic measures. Variations between the studies have provided the literature with an array of methods to study this aspect of scoliosis.1–12 Previous studies have examined adolescent idiopathic scoliosis as well as congenital scoliosis.3,5,6,7,11,12 Morrissy et al examined Cobb angle measurement in adolescent idiopathic scoliosis.7 They sought to determine the interobserver and intraobserver variability for the use of Cobb angle and attempted to identify sources of error. The found an error of 6.3° when controlling for the selection of end vertebrae and using standardized measurement tools. Loder et al also evaluated the variability of Cobb angles in children with congenital scoliosis.6 They found that at least 23° of change was necessary to obtain 95% confidence intervals. That margin could be reduced to 19° if the same observer performed the measurements. These studies documented that variability exists when radiographic measures are used in the evaluation of scoliosis. Similar studies to date have not been conducted on patients with neuromuscular scoliosis. This form of Table 2. Cohen’s Kappa for LIV and Triradiate (Dichotomous Measures) Triradiate (open vs. closed vs. missing) Triradiate (open and closed vs. missing) Cohen’s Kappa Cohen’s Kappa With Missing Values Coded % Values Missing (n ⫽ 384) 0.894 0.632 58.9 — 0.615 58.9 694 Spine • Volume 32 • Number 6 • 2007 Table 3. Intraclass Correlations for Radiographic Measures Range of Correlations Within Investigators Average No. of Paired Measures (maximum ⫽ 10) No. of Times Within n Identical (maximum ⫽ 8) 0.785 to 0.988 0.667 to 0.960 ⫺0.419 to 0.990 0.462 to 0.967 0.154 to 0.967 0.323 to 0.936 0.740 to 1.000 0.882 to 0.999 ⫺0.548 to 0.993 8.5 8.0 8.6 8.6 7.5 9.3 6.8 8.3 7.4 3 2 4 5 1 6 1 3 3 Cobb angle Ferguson angle Balance C7 Pelvic obliquity Pelvic obliquity (Mubarak) Pelvic obliquity to horizontal Risser Kyphotic Cobb angle Kyphotic index study represents a key element that is missing from the literature. This study sought to identify reliable methods of radiographic examination. In examining a number of radiographic parameters commonly used in the evaluation of scoliosis, we found that Cobb angle proved to have the best reliability. The intraobserver and interobserver variability was 5.7° and 14.8°, respectively. Loder et al found that interobserver variability in congenital scoliosis was 23°, while intraobserver variability was 19°.6 In comparison to this landmark study, we also found better intraobserver variability in comparison with interobserver variability. Morrissy et al found the interobserver variability to be 7.2° in adolescent idiopathic scoliosis.7 This number improved to 6.3° when the end vertebral level was preselected. Morrissy et al7 did not examine intraobserver variability. As might be expected, we found a larger variability in neuromuscular scoliosis when compared with the adolescent idiopathic curves in Morrissey’s study. These data provide a standard by which errors in measurement can be judged, which is useful in evaluating the progression of neuromuscular curves over time. In addition, the Ferguson angle and kyphotic Cobb angle were examined. The Ferguson angle was thought to be less accurate than the Cobb angle, and this fact was highlighted through our results. The Ferguson angle boasts a higher intraobserver and interobserver variability than the Cobb angle. In light of these findings, we think that Ferguson angle measurements are of little value in neuromuscular scoliosis. The analysis of kyphotic Cobb angle also demonstrated higher intraobserver and interobserver variability, thus making this a less reliable measure. This increased error can be attributed to the fact that endplates or not consistently well visualized on lateral radiographs. The statistical analysis was conducted in a method consistent with the analysis done by Loder et al.6 In their landmark study, Loder et al Table 4. Intraobserver and Interobserver Variability Cobb angle Ferguson angle Kyphotic Cobb angle Intraobserver Variability Interobserver Variability 5.7 6.8 17.4 14.8 20.6 24.01 preselected the end vertebrae.6 In this study, the authors chose not to predetermine the end vertebrae levels. It was thought that this would best replicate clinical practice. The selecting of end vertebrae represents a critical portion of radiographic analysis. When evaluating this measurement tool, it was thought that it ought to be analyzed in a fashion comparable to its clinical use. Despite the lack of control of the end vertebrae, the interobserver and intraobserver variability was better than the historical literature. This provides a foundation allowing our data to be compared with the literatures results regarding other forms of scoliosis. Neuromuscular scoliosis frequently has long curves that extend to and may include the pelvis, thus causing pelvic obliquity. Pelvic obliquity can be associated with difficulty sitting, pressure sores, and difficulty using wheelchairs. In light of these significant issues, it is important to identify a method to measure this deformity. Three commonly used methods were evaluated and compared. In the evaluation of pelvic obliquity, this study found that obliquity measured to the horizontal was the most reliable. These results support this measurement tool as the standard method by which pelvic obliquity can be defined. Evaluation of the skeletal maturity in these patients is an important variable. As in adolescent idiopathic scoliosis, neuromuscular scoliosis can be expected to increase during rapid growth. Thus, it is important to identify a means by which skeletal maturity can be determined. Commonly used methods include the evaluation of Risser sign and the status of the triradiate cartilage. This study examined these 2 commonly used methods. Often it was difficult to visualize the pelvis adequately to conduct these evaluations. This is often the case in clinical practice. In light of the unreliable appearance of the anatomic structures on scoliosis radiographs, we think that a separate anteroposterior pelvic radiograph be obtained. This separate film would reliably provide the radiographic anatomy necessary to use these commonly accepted methods of determining skeletal maturity. Conclusion Several recommendations can be made regarding radiographic measures in neuromuscular scoliosis. Neuromuscular scoliosis radiographs can be reliable analyzed Radiographic Parameters in Neuromuscular Scoliosis • Gupta et al 695 with the use of Cobb angle. Other forms of radiographic analysis, such as Ferguson angle, are not as reliable. Pelvic obliquity should be measured from the horizontal, as other commonly used methods are not as reliable. In addition, kyphosis is best evaluated with the use of the kyphotic Cobb angle. Finally, it is thought that a separate anteroposterior pelvis radiograph should be used to assess skeletal maturity, as scoliosis films often truncate the vital anatomy necessary to determine skeletal maturity. This paper documents the interobserver and intraobserver variability for neuromuscular scoliosis, a piece of the literature previously neglected. Key Points ● Neuromuscular scoliosis radiographs can be reliably analyzed with the using a Cobb angle. ● Other forms of radiographic analysis, such as Ferguson angle, are not as reliable. ● Pelvic obliquity should be measured from the horizontal, as other commonly used methods are not as reliable. ● Kyphosis is best evaluated with the use of the kyphotic Cobb angle. ● A separate anteroposterior pelvis radiograph should be used to assess skeletal maturity, as scoliosis films often truncate the vital anatomy necessary to determine skeletal maturity. ● This paper documents the interobserver and intraobserver variability for neuromuscular scoliosis, a piece of the literature previously neglected. References 1. Beekman CE, Hall V. Variability of scoliosis measurement from spinal roentgenograms. Phys Ther 1979;59:764 –5. 2. Cobb JR. Outline of the study of scoliosis. Instr Course Lect 1948;5:261–75. 3. Dawson EG, Smith RK, McNiece GM. Radiographic evaluation of scoliosis: a reassessment and introduction of the scoliosis Chariot. Clin Orthop 1978; 131:151–5. 4. DeSmet AA, Goin JE, Asher MA, et al. A clinical study of the differences between the scoliotic angles measured on posteroanterior and anteroposterior radiographs. J Bone Joint Surg Am 1982;64:489 –93. 5. Goldberg MS, Poitras B, Mayo NE, et al. Observer variation in assessing spinal curvature and skeletal development in adolescent idiopathic scoliosis. Spine 1988;13:1371–7. 6. Loder RT, Urquhart A, Steen H, et al. Variability in Cobb angle measurements in children with congenital scoliosis. J Bone Joint Surg Br 1995;77:768 –70. 7. Morrissy RT, Goldsmith GS, Hall EC, et al. Measurement of the Cobb angle on radiographs of patients who have scoliosis: evaluation of intrinsic error. J Bone Joint Surg Am 1990;72:320 –7. 8. Brooks HL, Azen SP, Gerberg E, et al. Scoliosis: a prospective epidemiological study. J Bone Joint Surg Am 1975;57:968 –72. 9. Brown JC, Axelgaard J, Howson DC. Multicenter trial of a noinvasive stimulation method for idiopathic scoliosis: a summary of early treatment results. Spine 1984;9:382–7. 10. Jackson RP, Peterson MD, McManus AC, et al. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine 1998;23:1750 – 67. 11. Locke MD. Infrapelvic obliquity and scoliosis in myelomeningocele. In: Sarawark JF, Lubicky JP, eds. Caring for the Child With Spina Bifida. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2001. 12. Mubarak SJ, Morin WD, Leach J. Spinal fusion in Duchenne muscular dystrophy-fixation and fusion to the sacropelvis. J Pediatr Orthop 1993;13:752–7.