Haematology & Blood Transfusion Laboratory Handbook
advertisement

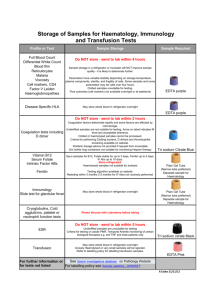
Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Title: Haematology & Blood Transfusion Laboratory Handbook Code: Haematology/Blood Transfusion/Clinical Chemistry 11133 Authors: Chris Brammer and Marie Hughes Version: 5.0 Document Category: Haematology & Transfusion Authorised By: Sheila Kowalczyk Authorised On: 30-Jun-2014 Review On: 30-Jun-2016 Location Of Copy: Intranet Section: All Haematology, Chemistry & Transfusion Locations Date Time Of Last Update: 30-Jun-2014 12:53 Date Time Printed: 30-Jun-2014 12:53 Document Status: Authorised Ou Name: Department of Haematology, Blood Transfusion & Clinical Chemistry Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Department of Haematology and Blood Transfusion Laboratory Handbook Section 1 2 3 4 5 6 7 8 8.1 9 9.1 9.2 9.3 9.4 10 11 12 13 14 15 16 Contents Introduction, Location & Telephone Numbers General Comments and Clinical Guidelines Laboratory Opening Hours and Emergency Service Request Forms Specimen Tubes Blood Transfusion Obstetric Haematology Thrombophilia investigation and testing Anticoagulation and warfarin induction Table of Haematology Tests, Turnaround Times and Reference Ranges Sample Type and Container Guide Guide to notes in Table of Tests Turnaround Times Reference Ranges for Full Blood Count and White Cell Differential Reference Lab Addresses Haematology Tests Special Precautions Haematology Tests Time Limit for adding Additional Request Screening for Malaria and other blood borne parasites Requesting and interpreting Haematinics tests (B12, Folate, Iron studies) Screening for Thalassaemia and Haemoglobinopathies Investigation of Hereditary Spherocytosis Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 1 of 41 1. INTRODUCTION, LOCATION AND TELEPHONE NUMBERS We provide a service to all hospitals and General Practitioners in the area and Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 receive about 2000 specimens each day. The laboratory is located on the second floor as shown on the following floor plan: Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 2 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 CONSULTANTS Dr. C. Brammer ext. 66771 (external 01324 566771) Dr. R.F. Neilson ext. 66772 (external 01324 566772) Dr. M. Hughes ext. 66770 (external 01324 566770) Dr R. Boulton-Jones ext. 66768 (external 01324 566768) Secretary ext. 67084 (external 01324 567084) For urgent clinical queries Consultant Haematologist can be contacted on 01324 567675 Mon-Fri 9am – 5pm. The on-call Haematologist can be contacted via hospital switchboard out with these hours. Non-urgent clinical or laboratory queries should be directed to the departmental mailbox which will be reviewed daily Monday to Friday. Email address: FV-UHB.haematology@nhs.net SENIOR LABORATORY STAFF Mrs Sheila Kowalczyk BMS 4 ext. 66767 (external 01324 566767) Mrs Mandy Dawson BMS 3 ext. 66777 (external 01324 566777) Mrs Gillian Lowe BMS 3 ext. 66775 (external 01324 566775) Mr Mark Gilmour Quality Manager ext. 66773 (external 01786 566773) Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 3 of 41 LABORATORY NUMBERS Laboratory Emergency Pager out of hours 1777 (to page dial 68100 and follow instructions, from outside FVRH phone Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 switchboard and ask to page) Specimen Reception Routine Enquiries ext. 66695 (external 01324 566695) Specimen Reception Emergency Requests ext. 66693 (external 01324 566693) Haematology Laboratory ext. 66755 (external 01324 566755) Transfusion Laboratory ext. 66779 (external 01324 566779) Transfusion Practitioner ext. 66762 (external 01324 566762) FORTH VALLEY ROYAL SWITCHBOARD: 01786 566000 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 4 of 41 2. GENERAL COMMENTS AND CLINCIAL GUIDELINES CHI Number Please ensure that specimens and request forms are both adequately labelled so Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 that they can be matched up without error and the result sent to the appropriate destination. If you do not use the CHI number, we may not be able to link earlier results to the same patient and the result may not match to the patient when the result processes into SCI Store. If you have access to laboratory results electronically they may not be available to you. Clinical Details Relevant clinical details help us to be more helpful to you. It is rarely possible, for example, to interpret blood film morphology without some knowledge of the clinical situation. A comment such as “routine” is not any help. The Consultant Haematologists are always willing to discuss problems and to give advice. Clinical Guidelines Relevant Clinical Guidelines are available on the Forth Valley Intranet at the following link by selecting “Haematology” and “Transfusion Service”. The handbooks for all laboratory departments are found by selecting “Laboratories” through the Clinical Guidelines page or by using the “Departments A-Z” option from the Intranet home page. http://www.qifv.scot.nhs.uk/CE_ClinicalGuidelines.asp Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 5 of 41 3. LABORATORY OPENING HOURS AND EMERGENCY SERVICE LABORATORY OPENING HOURS –HAEMATOLOGY AND BLOOD TRANSFUSION Monday to Friday 08:40 – 17:00 (Normal Service) Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Monday to Friday 17:00 -08:40 (Reduced 24 hour service) Saturday and Sunday all day – (Reduced 24 hour service) Public Holidays – Reduced service (details issued via staff comms) SPECIMEN RECEPTION OPENING HOURS Monday to Friday 08:45-20:00 Saturday and Sunday and 09:00-17:00 Out of hours: The department operates a shift system for Haematology and Blood Transfusion, and the duty BMS should be contacted through the switchboard or internal page number 1777. EMERGENCY SERVICE When sending urgent samples please notify the Laboratory in advance on the numbers below: Monday to Friday 08:45-20:00 and Saturday and Sunday and 09:00-17:00: Phone specimen reception on 66693 (01324 566693) or the laboratory number as in section 1. At all other times contact the duty BMS by paging 1777 or phone the laboratory number. From outside the hospital phone switchboard on 01324 566000 and ask for page 1777. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 6 of 41 4. REQUEST FORMS 1. Haematology: The front sheet (Red on White) of the multi-layer request form is for Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Haematology but not Blood Transfusion. If your request is for other departments also you MUST write firmly with a ballpoint pen and if address labels are used, attach them to all relevant pages. If you do take labels from the patient’s notes check that they refer to the right patient. Haematology request form requirements are: • Surname and forename, date of birth and / or CHI number must be provided – use the CHI number whenever possible as this assists matching results to previous result for the patient • Name and address of requestor is required in order that reports can be directed appropriately or can be found on SCI store using the search facility (consultants name should be clearly identified in full). • Date and time of specimen and person who bled the patient should be recorded • Useful clinical details should be provided • Note that bar-coded addressograph labels should be used on request forms whenever possible 2. Blood Transfusion: (Blue on White): All requests for blood or blood products including “group and save” procedures and Anti-D requests. Please refer to the NHS Forth Valley Blood Transfusion Protocol for request form and sample labelling requirements (use Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 linkAuthorised in section 6). Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 on: 30-Jun-2014. Author(s): Chris Brammer, Marie Hughes Page 7 of 41 3. Direct Order Comms: The DartOCM system is being implemented across Forth Valley in 2014. The system will not be used for Blood Transfusion. Training will be provided to requestors before moving on to the system. Any requests that can’t be Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 generated through DartOCM must comply with 4.1 above. 5. SPECIMEN TUBES Specimens are taken by the Becton Dickinson system. Under or overfilling may lead to invalid results. All anti-coagulated specimens should be mixed gently by repeated inversion, not shaken. Becton Dickinson distributes charts with information on which bottles to use for which test, order of draw and mixing requirements. Charts are available through the practice development team. DO NOT pre-label bottles as this can lead to misidentification errors. Sample bottles should be labelled at the bedside by the person taking blood and initialled by them. A list of tests performed and the type of specimen tube required is in section 9. Please ensure that separate bottles are sent for haematology and clinical chemistry tests. Addressograph labels are acceptable on Haematology sample bottles but under no circumstances will they be accepted for blood transfusion work or ante-natal grouping. This practice has been shown to increase the likelihood of misidentification. For blood transfusion or ante-natal blood group samples: Bar-coded addressograph labels are not accepted on samples for transfusion Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 testingAuthorised or ante natal grouping. The minimum identification requirements are on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes detailed in the Blood Transfusion protocol which is found at the link in section 6. Page 8 of 41 For Haematology samples the following information is required: • Minimum identification required on the sample is: Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 o Surname o Forename o Date of birth and / or CHI number • In addition there should be the name of requestor and requesting location, the date and time the sample is taken and the signature of the person who bled the patient. • The details on the sample and request form must match. Failure to provide the correct details may result in the sample being rejected and a repeat required. • A bar-coded addressograph label is preferred. Place the label on the bottle so that the level of blood in the bottle can still be seen. • When emergency tests are required for unidentified patients a casualty number should be used and as much other information e.g. unknown male / unknown female. • The laboratory cannot process specimens that are not clearly identified. • Note that for requests generated via direct order comms DartOCM barcoded sample labels are printed for each bottle required. Training will be provided for requestors before moving on to the system during 2014. Any requests that can’t be generated through DartOCM must be comply with the above. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 9 of 41 Precautions for High Risk Specimens: • All samples and request forms which are known to be or suspected may be high risk e.g. hepatitis, HIV or other group 3 or 4 agent such as Dengue Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 fever must be labelled with a high risk sticker. • The laboratory must be informed in advance if a sample is suspected of containing any high risk agent other than hepatitis or HIV e.g. Dengue fever. • See section 11 for further information on special precautions required for high risk samples. 6. BLOOD TRANSFUSION The NHS Forth Valley “Blood Transfusion Protocol” details the procedures adopted by this organisation to maximise transfusion safety and is based on national guidelines. Please use the link below to the Forth Valley Intranet Clinical Guidelines page and search for “Transfusion Service” guidelines. http://www.qifv.scot.nhs.uk/CE_ClinicalGuidelines.asp Alternatively from the intranet home page under main menu select “Departments A-Z”, select “Laboratories” and click on the link to “Blood Transfusion”. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 10 of 41 7. OBSTETRIC HAEMATOLOGY ANTI-D IMMUNOGLOBULIN Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Indications for Administration: 1. All Rhesus negative women as soon as possible after, or at least within 72 hours of, delivery of a Rhesus D positive infant, when the post delivery maternal venous blood specimen contains no detectable anti-Rhesus D antibody. Advice should be sought if other antibodies are present. 2. All pregnant Rhesus negative women with no Rhesus D antibody on record, to be given as soon as possible after, or at least within 72 hours of, the following potential sensitising episodes: • Miscarriage; complete, incomplete or threatened at > 12/40; • Persistent PV bleeding at any stage of pregnancy • Termination of pregnancy • Amniocentesis, chorionic villus biopsy and cordocentesis • Anti-partum Haemorrhage • External cephalic Version • Abdominal trauma (sharp/blunt, open/closed) at >12/40 • Ectopic pregnancy • Evacuation of molar pregnancy • Intrauterine death and stillbirth • In-utero therapeutic interventions (transfusion, surgery, insertion of shunts, laser) • Delivery – normal, instrumental or Caesarean section Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 11 of 41 Dosage and Administration: 250 units (50 µg) intramuscularly up to 20 weeks gestation. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 500 units (100 µg) intramuscularly after 20 weeks gestation. Timing of administration of anti-D To be given preferably within 24 hours of the potential sensitising incident, and in no case later than 72 hours. However, in the case of accidental omission, Anti-D should still be given up to 7 days after the incident. The preferred site of injection is the deltoid muscle. Injections should be given every 6 weeks if there is continued ante partum bleeding. NB In the case of Intrauterine death, it should be noted that the diagnosis of IUD is the sensitising event rather than delivery and hence anti-D Ig should be issued for administration within 72 h of diagnosis. Prophylactic anti-D programme A programme for administration during pregnancy of prophylactic Anti-D to suitable Rh(D) Negative women is now in place. Women are offered a dose of 1500 IU Prophylactic Anti-D at 30 weeks. To request Prophylactic Anti-D on this programme send the request to the transfusion laboratory with the 28 weeks grouping sample, stating on the Transfusion Request Form when and where the Anti-D is required, the dose required and that it is to be administered as part of the programme. If a sensitising episode occurs at any stage of pregnancy to a patient who is on the Anti-D Prophylactic Programme, they must be tested in the same way as patients who are not on the programme as above. Anti-D will be issued if appropriate and a Kleihauer test will be performed if the event is after 20 weeks Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 12 of 41 Kleihauer Tests This measures the quantity of feto-maternal transplacental haemorrhage (FMH) for calculation of any additional dose of Anti-D that may be necessary in non- Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 sensitised Rh(D) Negative patients. A specimen of maternal blood in 4 ml EDTA (FBC Tube) for a Kleihauer test in addition to the 6 ml EDTA grouping sample is required in the following circumstances: • Instrumentation at any gestation • Within 2hrs after delivery • Any potentially sensitising event after 20 weeks gestation (as above) • Following a large transplacental bleed (as below) For any FMH > 4 ml an appropriate supplementary dose of anti-D immunoglobulin must be given immediately. A repeat estimation of the FMH should be carried out 48 h following the initial anti D injection. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 13 of 41 Further Points to Remember 1. THE COMMONEST CAUSE OF SENSITISATION TO THE RHESUS D ANTIGEN IS FAILURE TO ADMINISTER ANTI-D IN APPROPRIATE Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 CASES. 2. Particular vigilance is necessary in cases of abortion, whether therapeutic or spontaneous; threatened, complete or incomplete, where stay in hospital is brief. Results must be telephoned as a matter of urgency and staff trained to act properly on them. There must be close liaison between the laboratory, the clinical units and the primary care teams. 3. Where threatened or complete abortion occurs at home, the General Practitioner must ascertain whether anti-D is necessary. 4. Anti-D given to the mother antenatally is not harmful to the baby. 5. Passively administered anti-D may be detected up to 6 weeks after administration, and occasionally up to 6 months. 6. If antibody is not detectable at delivery, further administration of immunoglobulin is necessary whether or not the mother was given a prophylactic dose antenatally. 7. If there is any doubt about whether to give anti-D, advice may be obtained from the Blood Transfusion Laboratory or from Consultant Haematologist. 8. Seek advice when any other antibody is present. 9. Additional doses of anti-D immunoglobulin, when recommended should be administered in multiple muscular sites to avoid local reactions. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 14 of 41 8. THROMBOPHILIA INVESTIGATION AND TESTING Information on thrombophilia testing is available as a Haematology Clinical Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Guideline on the Forth Valley intranet. http://www.qifv.scot.nhs.uk/CE_Guidance.asp?topic=Haematology The Clinical Guideline provides advice on testing in the following conditions: • Acute VTE (DVT+/- PE) • Venous thrombosis of Upper Limb/Eye/Venous Sinus of Brain/Intra-abdominal Veins • Coronary, cerebral and peripheral arterial thrombosis • Woman being considered for HRT/COCP • Prevention of VTE in hospitalised patient • Relatives of patients with a history of VTE • Children Tests Available and Sample Requirements: The following tests comprise the thrombophilia screen: • Antithrombin Assay • Protein C assay • Protein S assay (Total & Free) • Lupus anticoagulant and anticardiolipin assays • Modified activated protein C sensitivity • Prothrombin G20210A mutation • APC:SR ratio as marker for Factor V Leiden Genetic analysis for Factor V Leiden will only be undertaken if the APC:SR is abnormal. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 15 of 41 Samples required for a thrombophilia screen are: 4 x citrate samples (blue topped tubes) Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Requests for thrombophilia testing MUST include full patient and family history details and drug therapy, especially oral contraceptive use or HRT, where appropriate. All requests will be vetted by a Haematology Consultant. Incomplete or clinically inappropriate requests will be rejected and the requesting clinician informed. In all cases, if there is a doubt about who and when to test please contact a consultant haematologist to discuss prior to sending the samples. 8.1 ANTICOAGULATION AND WARFARIN INDUCTION For information on anticoagulation and warfarin induction refer to the Haematology Clinical Guidelines on the FV intranet. http://www.qifv.scot.nhs.uk/CE_Guidance.asp?topic=Haematology Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 16 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 9. TABLE OF HAEMATOLOGY TESTS, TURNAROUND TIMES AND REFERENCE RANGES 9.1 Table of tests analysed Test Refer to sections 9.2 and 9.3 for guides to notes and bottle / container type Notes Anti-nuclear antibodies Bone marrow * Bottle / Container type Vol. (ml) Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results SST 7 Less than 1/64 Tested locally 2 weeks Tested locally 72 hours Tested locally 12 hours Tested locally 12 hours Tested locally 12 hours - PT +APPT controls reported Coagulation Screen (PT, APTT and fibrinogen) 1 Citrate 4 with results fibrinogen 1.5-4.0 g/l D-Dimer for coagulopathy (not for detecting 3 Citrate 4 EDTA 4 <0.5mg/l thrombosis) Direct anti-globulin test (Coombs test) Transfusion EDTA and request form required (pink positive in up to 5% of normal controls top bottle with hand written details) Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 17 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Erythrocyte sedimentation rate (ESR) Notes Bottle / Container type Vol. (ml) 1 EDTA 4 EDTA 4 SST 7 Full Blood Count (FBC) Reference range where applicable (adult unless otherwise stated) Men 0-5mm in 1 hour Women 0-7mm in 1hour see later tables for reference ranges Reference laboratory Expected turnaround time for results Tested locally 12 hours Tested locally 8 hours Haematinics: Serum B12 2, 5 180-900ng/l Tested locally 72 hours Tested locally 72 hours Tested locally 72 hours Age 18-45 male 36-225 ug/l Serum ferritin 5 SST 7 female 10-65 ug/l Age 45+ male 42-262 ug/l female 24-155 ug/l Serum folate 5 SST 7 2.1-14.0 ug/l Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 18 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Notes Bottle / Container type Vol. (ml) 5 EDTA 4 5 EDTA 4 5 EDTA 4 Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results Tested locally 1 week 1.8-3.2% Tested locally 3 working days 0-0.9% Tested locally 3 working days Tested locally 48 hours Tested locally 1 week Tested locally 4 weeks Tested locally 48 hours Tested locally 2 weeks Haemoglobin electrophoresis (See section 12) Hb A2 (HPLC) Hb F (HPLC) Target range for good HbA1c (HPLC) 5 EDTA 4 diabetic control is 48–59 mmol/mol (IFCC units) Haemosiderin 6 Universal 20 SST 7 Infectious Mononucleosis SST or 7 or test EDTA 4 SST 7 Haptoglobin Intrinsic factor antibody 7 0.2-2.0 g/l Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 19 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Notes Bottle / Container type Vol. (ml) Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results Tested locally 12 hours Tested locally 48 hours Target INR range is dependent on reason for INR 1 Citrate 4 anticoagulation. Refer to Haematology clinical guidelines on intranet. Kleihauer EDTA 4 See section 7 Malarial screen antigen test (and other blood borne 12 hours parasites EDTA 4 See section 10 Tested locally (thick and thin film and films plasmodium antigen test) 24 hours Reticulocytes Rheumatoid factor Sickle test 9 EDTA 4 SST EDTA 10-150 x109/l Tested locally 4 hours 7 Tested locally 72 hours 4 Tested locally 24 hours Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 20 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 REFERRED TESTS - see section 10 for list of reference laboratories Test Acetyl choline receptor antibodies Adrenal Antibodies Notes Bottle / Container type Vol. (ml) Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results ** SST 7 <0.1nmol/l xiv 4 weeks ** SST 7 vii 4 weeks ** SST 7 vii 6 weeks ** SST 7 xv 4 weeks ** SST 7 vii 4 weeks ** SST 7 vii 4 weeks ** SST 7 xiv 4 weeks ** SST 7 xv 4 weeks Allergy testing (RAST) allergens must be specified Alpha-NMDA receptor antibodies Anti-Mitochondrial antibodies Anti-Neutrophil cytoplasmic antibodies Anti-neural antibodies (e.g. anti-Hu, Yo) Aquaporin-4-antibodies Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 21 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Notes Bottle / Container type Vol. (ml) Anti-neutrophil antibodies ** EDTA, 20, SST 10 10, ** SST ** Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results i 4 weeks 7 vii 4 weeks SST 1 xv 4 weeks ** EDTA 4 ii 2 weeks ** EDTA 4 iii 2 weeks ** Citrate 4 iv 1 week Auto-antibodies (DNA binding, ENA, AMA, SMA, Ro, La, TTG, Gastric parietal cell, skin, smooth muscle, glomerular basement membrane, cardiac, MPO, Scl70/Jo1,) Anti-musk Bcr-abl pcr Cell marker analysis Coagulation factor assay Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 22 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Notes Bottle / Container type Vol. (ml) Complement ** SST 7 Reference range where applicable (adult unless otherwise stated) C3 0.877-1.82 iu C4 0.185-0.452 iu Factor B C1esterase Reference laboratory Expected turnaround time for results vii 4 weeks ix 4 weeks v 4 weeks 0.137-0.348 iu inhibitor 0.178-0.351 iu CH50 Cytogenetics ** Erythropoietin ** Glutamic acid decarboxylase antibodies Ganglioside antibodies G-6-PD Genetics Genetic SST, EDTA 5 7,4 5-25 mU/ml ** SST 5 xiii 4 weeks ** SST 2 xiv 4 weeks ** EDTA 4 xvii 2 weeks ** EDTA 4 ix 4 weeks 4.3-10.5 iu/gHb at 37oC Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 23 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Haemoglobin DNA screening Hereditary Spherocytosis H.I.T. screen (anti-PF4) HLA-DR, HLA B27 Insulin antibodies Islet cell antibodies JAK 2 PCR Lupus anticoagulant Lymphocyte phenotyping/subsets Notes Bottle / Container type Vol. (ml) ** EDTA ** Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results 4 xii 4 weeks EDTA 4 iii 4 weeks ** SST 2 vi 4 weeks ** EDTA 10 viii 4 weeks ** SST 7 xviii 4 weeks ** SST 1 xiii 4 weeks ** EDTA 4 ii 4 weeks 8, ** Citrate 16 iv 2 weeks ** EDTA 4 vii 4 weeks Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 24 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Mast cell tryptase Notes Bottle / Container type Vol. (ml) Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results ** EDTA 5 2-14 ug/l vii 4 weeks vii 4 weeks iv 2 weeks xvi 4 weeks xvi 4 weeks EDTA from Neutrophil function ** patient and a 4 healthy control See section 11 Thrombophilia screen ** 4 x Citrate 16 Requests screened by Haematology Consultant Thyroid Peroxidase antibodies Thyrotropin receptor antibody ** SST 7 ** SST 3 - Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 25 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Test Tissue transglutaminase Tissue typing Plasma Viscosity Voltage gated Ca+ channel antibodies Warfarin assay Notes Bottle / Container type Vol. (ml) ** SST 7 ** EDTA 20 ** EDTA 4 ** SST 1 4, ** SST 2 Reference range where applicable (adult unless otherwise stated) Reference laboratory Expected turnaround time for results vii 4 weeks viii 4 weeks xix 48 hours - xx 6 weeks - x 2 weeks - 1.50 – 1.72 The list above is not exhaustive so if the test required is not listed phone the laboratory for advice. Requests for New Tests: If a new test not previously provided is required a “New Test Request Form” must be completed, signed off by a General Manager and submitted to the Laboratory Service Manager for approval. The form is available from laboratory senior staff (contact details in section 1). Approval must be obtained in advance of sending a sample for a new test or testing will not be carried out. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 26 of 41 9.1 Sample type and container guide Note that the bottle cap colour of paediatric bottles may not match that of the adult bottle Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Bottle / Container Description Colour of bottle cap Code SST serum separation tube Citrate citrate for coagulation yellow (gold) red (paediatric) light blue (adult) green (paediatric) purple (Haematology) EDTA Potassium EDTA pink (Transfusion) pink/lilac (Paediatric) Heparin Universal Genetic Heparin green urine – use plain universal container white Marrow transport media kept at 2-8oC contact department Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 27 of 41 9.2 Guide to Notes from test table above Notes Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 * ** 1 2 Description By arrangement with lab Referred elsewhere. Must be in laboratory before Thursday 12 midday Specimen tube must not be under or overfilled Do not test following B12 injection D-dimers may be raised in presence of thrombosis, disseminated intravascular coagulation, inflammation, infection, underlying malignancy or 3 recent surgery. The sensitivity of the laboratory test currently only allows for assessment of coagulopathy. Testing for underlying thrombosis requires a lithium heparin sample and is not performed by the laboratory but is available as a point of care test in other hospital departments. 4 5 6 7 8 9 10 Sample should be taken pre-dose Must be requested PRE-TRANSFUSION Early morning sterile urine sample Must be sent before starting cobalamin treatment as test disrupted by high levels of serum B12 Samples should arrive in laboratory no later than 2pm A positive test must be followed by haemoglobin electrophoresis to distinguish between heterozygote and homozygote Please specify which are of clinical interest Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 28 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 9.3 Turnaround Times: • For urgent tests contact the laboratory as in section 3 • Urgent Full Blood Count and Coagulation: results within 2 hours from receipt of sample • If other tests are required urgently contact laboratory staff • See table of tests for routine turnaround times • Results are available in SCI Store between 15 – 45 minutes after completion in the laboratory. 9.4 Reference ranges NORMAL RANGES FULL BLOOD COUNT ADULTS MEN WOMEN White Cell Count (x109/l) 3.9 - 10.6 3.5 - 11.0 Red Cell Count(x1012/l) 4.4 - 5.9 3.8 - 5.2 Haemoglobin (g/l) 133 - 177 117 - 157 Packed Cell Volume .40 - .52 .35 - .47 Mean Cell Volume (fl) 81 - 100 81 - 100 Mean Cell Haemoglobin (pg) 26.6 - 33.8 26.4 - 34.0 MCH Concentration (g/dl) 31.5 - 36.3 31.4 - 35.8 Platelet Count (x109/l) 150 - 440 150 - 440 CHILDREN BIRTH 1 YEAR 6 10 WBC (x109.l) 9.30 6.0 - 17.5 5.0 -14.5 4.5 - 13.5 Hb (g/l) 9.0 - 14.6 10.6 - 15.5 10.7 - 15.5 14.6 - 23.4 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 29 of 41 DIFFERENTIAL WHITE CELL COUNT (as absolute counts, x 109/l) 1 year 6 10 Adult 1.5 - 8.5 1.5 - 8.0 1.5 - 8.0 1.8 - 7.7 Lymphocytes 4.0 - 10.5 1.5 - 7.0 1.5 - 6.5 1.0 - 4.8 Monocytes 0.05- 1.1 0 - 0.65 0 - 0.8 0 - 0.8 Eosinophils 0 – 0.65 0 - 0.65 0 - 0.60 0 - 0.45 Basophils 0 - 0.20 0 - 0.20 0 - 0.20 0 - 0.20 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Neutrophils (Data extracted from “Haematology”, W J Williams et al., 3rd edition, 1983, McGraw Hill) • Reference ranges for other tests are shown in the table of tests. • Reference ranges are provided on reports from referral laboratories. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 30 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 10. REFERENCE LABORATORY ADDRESSES i. NHSBT Filton (Bristol) 500 North Bristol Park Northway Filton Bristol BS34 7QH 0117 9217372 ii. Department of Molecular Haematology Southern General Hospital Govan Road Glasgow 0141 354 9408/9409 iii. Department of Haematology Gartnavel General Hospital 2nd Floor Laboratory Building 21 Shelly Road Glasgow G12 0XL Tel 0141 3017707 iv. Department of Haematology Glasgow Royal Infirmary 82 Castle Street Glasgow G4 OSF 0141 211 4000 v. SAS Erythropoietin Laboratory Department of Clinical Biochemistry King’s College hospital Denmark Hill London SE5 9RS 020 3299 3856 vi. Scottish National Blood Transfusion Service Shelley Road Gartnavel General Hospital Great Western Road Glasgow Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 0141 357 7700 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 31 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 vii. Immunology laboratory 1st floor Laboratory medicine and facilities management building Southern General Hospital Govan Road Glasgow G51 4TF Tel 0141 301 7752 viii. Histocompatibility and immunogenetics Tissue typing service Gartnavel hospital Glasgow 0141 301 7755 ix. West of Scotland genetic services Level 2b, Laboratory medicine and facilities Management Building. Southern General Hospital Glasgow G51 4TF Tel 0141 301 7752 x. Department of Clinical Chemistry Queens Medical Centre Nottingham NG7 2UH 0115 9249924 Ex. 63411 xi. Deleted xii National Haemoglobinopathy reference laboratory Molecular Haematology Level 4 John Radcliffe Hospital Oxford OX3 9DU Telephone-01865572769 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 32 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 xiii Protein reference unit Department of Immunology Northern General Hospital Herries Road PO BOX 894 Sheffield S5 7YT Tel 0114 271 5552 xiv Department of Neuro-Immunology Southern General Hospital 1345 Govan Road Glasgow G51 4TF 141 2491 xv Immunology laboratory John Radcliffe Hospital Headley Way, Headington Oxford, Oxfordshire OX3 9DU 1865 66 xvi Department of Biochemistry Glasgow Royal Infirmary Alexandra Parade Glasgow 0141 211 4000 xvii Department of Haematology Edinburgh Royal infirmary 51 Little France Crescent Edinburgh, EH16 4SA 0131 536 1000 xviii SAS peptide hormone section Clinical laboratory Royal Surrey County Hospital Egerton Road Guildford Surrey GU2 7XX Tel 01483 571122 ext 4696 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 33 of 41 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 xix xx Haematology Department South Laboratory Victoria Hospital Kirkcaldy Fife KY2 5AH Tel 01592 643355 ext 29471 Immunology Department Churchill Hospital Headington Oxford OX3 7LJ Tel 01865 225992 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 34 of 41 11. SPECIAL PRECAUTIONS: The Haematology and Blood Transfusion laboratories are containment level 2 facilities. This means that there is a limited capacity to test samples containing Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 biological agents categorised as group 3 by the “Advisory Committee on Dangerous Pathogens”. The Advisory Committee prepare the “Approved List of Biological Agents” for the Health & Safety Executive. A Biological Agent is categorised by: • The likelihood it will cause disease or toxicity in humans • How likely it is that the infection would spread to the community • The availability of any prophylaxis or treatment (includes vaccines) Hepatitis and HIV, although group 3 agents, are officially approved to be tested in a level 2 facility provided the necessary containment and safety precautions are taken. It is therefore extremely important to identify high risk samples or potentially high risk samples to all staff involved by applying high risk stickers to sample and request form. Group 3 Biological Agents a. All known high risk samples must be clearly labelled as such on the sample and form. b. All samples suspected of containing group 3 biological agents other than hepatitis and HIV must be notified to the laboratory in advance. Only limited testing on other group 3 pathogens may be available e.g. malaria antigen test. Further advice can be sought from the Consultant Microbiologist. Group 4 Biological Agents a) Do not send samples suspected of containing group 4 biological agents to the laboratory other than after a risk assessment has been carried out by the clinician in charge of the patient and after consultation with the Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Consultant Microbiologist. Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 35 of 41 Other Special Precautions a) There are no other special precautions required other than the requirements Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 noted in the table of tests. 12 TIME LIMIT FOR REQUESTING ADDITIONAL REQUESTS: Coagulation: 2 hours from venesection Full Blood Count: 4 hours from venesection Clotted samples, e.g. haematinics: 24 hours Transfusion: Contact the transfusion laboratory for advice Referred tests: Contact the referral laboratory for advice Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 36 of 41 13. SCREENING FOR MALARIA AND OTHER BLOOD BORNE PARASITES If a diagnosis of malaria is suspected, the gold standard diagnostic test is a thick blood film for detection of parasites, accompanied by a thin film for species identification and Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 estimation of parasitaemia. Thick and/or thin films may also detect other blood borne parasites, such as microfilaria or trypanosomes. For specific diagnostic and clinical advice, please contact a consultant haematologist and/or infectious disease specialist. If malaria is suspected: a) Send 4ml blood in EDTA (FBC sample) urgently to the haematology laboratory – samples should ideally arrive in the laboratory within 2 hours of venepuncture (lengthy exposure to anticoagulant may significantly diminish the likelihood of detecting parasites). b) The request form must clearly state that malaria is suspected, and include travel history – which should be as specific as possible. This is likely to significantly aid species identification. c) A thick film and a thin film will be prepared and examined. d) In addition, a rapid malarial antigen detection test (for Plasmodium spp.) will be performed to complement microscopy. Outside of normal working hours, this may be reported before a blood film has been examined. Please note that a negative antigen test must be confirmed by microscopy, and, if clinical suspicion is high, a negative antigen test alone must not be relied upon to fully exclude malaria. e) If the initial thick film proves negative, yet clinical suspicion remains high, send two further consecutive daily samples for malaria screening. Three negative thick films make a diagnosis of malaria unlikely. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 37 of 41 14. REQUESTING AND INTERPRETING HAEMATINIC TESTS (B12, FOLATE, IRON STUDIES) Serum B12 and Folate assay Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 a) Tests for serum vitamin B12, serum folate levels and serum ferritin are frequently requested for the initial investigation of anaemia, or microcytosis / macrocytosis in the absence of anaemia. In addition, a serum B12 assay is included in the list of screening tests in a number of neurological and psychiatric conditions, and ferritin is used as a marker of whole body iron levels in patients with (suspected and confirmed) haemochromatosis. Interpretation of results can be problematic. b) For information on B12 and folate requesting and interpretation refer to the Haematology clinical guideline “B12 and Folate: Practical Guide” which can be found on the Forth Valley Intranet at the following link: http://www.qifv.scot.nhs.uk/CE_Guidance.asp?topic=Haematology Iron studies a) Serum Ferritin is the usual test for iron deficiency. b) The normal range is different for women of childbearing age compared to men and postmenopausal women, but it is debatable whether this is a real physiological difference or simply reflects a high incidence of iron deficiency in the population of women from whom the normal range is derived. c) In general, a serum ferritin <12µg/L is diagnostic of iron deficiency, and if <30µg/L is highly suggestive. Interpretation should be in the context of the FBC (MCH, MCV and blood film features). d) Ferritin is an acute phase reactant, so may be normal even in the presence of iron deficiency if there is intercurrent infection, inflammation or neoplasia. A rough guide might be to interpret a ferritin of <100µg/L with caution in the presence of intercurrent illness, as iron deficiency cannot be excluded. Again, haematological parameters are likely to help. e) A high serum Ferritin (>300µ/l) may indicate iron overload, but such a finding is Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 common in hospitalised patients and others with intercurrent illness. Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 38 of 41 f) A better guide to iron overload is the Transferrin Saturation (calculated from serum iron x100 divided by TIBC – see Chemistry handbook), which, if over 55% (men) or 50% (women) warrants further investigation. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 g) Serum iron and TIBC are generally unreliable tests for diagnosing iron deficiency. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 39 of 41 15. SCREENING FOR THALASSAEMIA AND HAEMOGLOBINOPATHIES Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Indications for screening for thalassaemia and/or haemoglobinopathies include: • Investigation of a hypochromic blood picture in the absence of iron deficiency • Investigation of anaemia in a patient of non-Northern European ancestry • Screening in an individual with a family history of thalassaemia or haemoglobinopathy • Antenatal screening Identification of Sickle haemoglobin prior to surgery in patients from ethnic • Groups with a high incidence of Sickle Cell Disease. When requesting thalassaemia and/or haemoglobinopathy screening please include the following clinical information: a. Ethnic origin of the patient (as precisely as possible). b. Whether or not there is a family history of thalassaemia/haemoglobinopathy, with details of diagnosis if available. c. Please state clearly if the test is for antenatal screening purposes (pregnant woman or partner). d. Reason for request. This information will help direct laboratory tests, which in general will include: a. FBC and blood film examination b. Serum ferritin if MCH is subnormal. c. High Pressure Liquid Chromatography (HPLC) for HbA2, HbF and variant haemoglobins. d. Further analysis by gel electropheresis or DNA testing dependent on HPLC. Further samples may be requested from the patient. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 40 of 41 16. INVESTIGATION OF HEREDITARY SPHEROCYTOSIS Based on BCSH Guidelines 2011 Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 http://www.bcshguidelines.com/documents/HS_BCSH_Sept_2011_final.pdf a) Although the diagnosis of HS is often made in childhood and young adult life, it may be diagnosed at any time of life including old age. Diagnostic testing a) Newly diagnosed patients with a family history of HS, typical clinical features and laboratory investigations (spherocytes on blood film, raised MCHC, increase in reticulocytes, negative DCT) do not require any additional tests. b) If there is no family history AIHA should be excluded. c) If the diagnosis is equivocal the EMA (Eosin-5-maleimide) binding test has a high predictive value for HS. d) This is a flow cytometry test performed at Gartnavel Hospital using an EDTA sample. Testing should be discussed with a haematology consultant and the correct request form obtained. e) Gel electrophoresis analysis of erythrocyte membranes is the method of choice for diagnosis of atypical cases. Haematology & Blood Transfusion Laboratory Handbook - Version: 5.0. Index: Haematology/Blood Transfusion/Clinical Chemistry 11133. Printed: 30-Jun-2014 12:53 Authorised on: 30-Jun-2014. Authorised by: Sheila Kowalczyk. SOP Unique Reference: 112-40460436. Due for review on: 30-Jun-2016 Author(s): Chris Brammer, Marie Hughes Page 41 of 41