Management of Pharyngocutaneous Fistulization in Transoral
advertisement

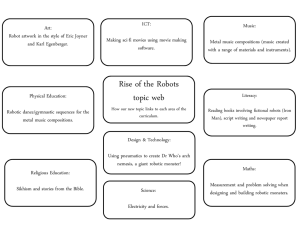
Management of Pharyngocutaneous Fistulization in Transoral Robotic Surgery Eliot J. Martin, PA-C; Eric J. Moore, MD; Kerry D. Olsen, MD. Department of Otorhinolaryngology, Mayo Clinic, Rochester, MN. Abstract Objectives: 1. To determine the incidence of pharyngocutaneous fistula associated with transoral robotic oropharyngectomy with concurrent neck dissection. 2. To discuss the prevention and treatment of pharnyngocutaneous fistulization as a consequence of transoral oropharyngeal surgery with simultaneous neck dissection. Methods: A retrospective, single institution chart review of sixty-six consecutive patients who underwent transoral robotic surgery with synchronous neck dissection for oropharyngeal neoplasia between April 2007 and February 2009. Results: Nineteen out of 66, or 28.8% of patients were identified as having an orocervical communication intraoperatively. All were managed with some combination of primary closure, local tissue advancement, fibrin glue saturation, and cervical drain placement. Of these patients only 3, or 4.5%, went on to develop a persistent salivary leak requiring post operative management via controlled incision and drainage with daily packing placement. All of these patients had aesthetic and functional results comparable to those patients that did not have/develop an orocervical communication. No patients experienced a delay from their operative treatment that prevented them from initiating recommended adjuvant therapy on schedule. Conclusion: Transoral robotic surgery is emerging as a primary treatment modality for oropharyngeal malignancies. Postoperative pharyngocutaneous fistula is an uncommon, preventable, but potentially problematic complication resulting from this operative technique when combined with concurrent neck dissection. Prompt recognition and intervention are of paramount importance in preventing both acute and long term functional impairment. Introduction Transoral resection of oropharyngeal malignancies provides exceptional local/regional disease control and survival benefit while optimizing function, minimizing complications and limiting treatment to that which is essential to maximize results1. Previous approaches to oropharyngeal tumors via the transoral route, however, have been technically challenging and fraught with a limited operative field of view. With the emergence of reports advocating the ease, safety and efficacy of transoral robotic surgery (TORS), it seems probable that a paradigm shift to primary surgery in reference to oropharyngeal carcinoma will ensue2-9. The majority of these reports advocate robotic oropharyngectomy, followed by surgical addressment of the neck in a delayed fashion. The proposed rationale for secondary neck dissection in lieu of TORS with synchronous neck dissection is in effort to avoid pharyngeal entry, as well as to avoid additional laryngopharyngeal swelling that may result in the need for tracheostomy2. The obvious downside to this algorithm is prolonged treatment with multi operational therapy, a delay in recommended adjuvant therapy when clinically necessary, and increased overall medical costs associated with the staggered operative course. We in turn have chosen to manage the neck and the primary tumor during the same operative setting. With these statements/presumptions in mind we wanted to evaluate our institutions data regarding robotic assisted oropharyngectomy with simultaneous neck dissection to see if orocervical fistulization would be a deterrent for single setting operative therapy. Patients and Methods Patient Inclusion After obtaining approval from the Mayo Clinic Institutional Review Board, we used the Mayo Clinic tumor registry to identify patients who underwent daVinci assisted oropharyngectomy with synchronous neck dissection from April 2007 to February 2009 at Mayo Clinic, Rochester, Minnesota. We retrospectively reviewed the electronic medical records of sixty-six consecutive patients that underwent TORS with simultaneous neck dissection within the aforementioned timeframe in effort to identify the actual incidence of intra and postoperative pharyngocervical communications. Patient data was retrieved from operative dictations, final pathology reports, hospital progress notes, and all subsequent visit documentation via the head and neck multidisciplinary team. All reviewed medical records had appropriate documentation regarding the presence, absence or development of a pharyngocervical connection. Operative Procedure All included tumors were located within the confines of the oropharynx and were exposed with the aid of the FeyhKastenbauer (FK) retractor (Gyrus ACMI, Southborough, MA). Utilization of the da Vinci surgical robot (Intuitive Surgical Inc., Sunnyvale, CA) aided in oropharyngeal tumor extirpation via techniques described previously by Weinstein et al.2, Holsinger et al10, and Moore et al.4 When oncologically feasible the buccopharyngeal fascia was not disrupted. Negative margins were confirmed in all patients via frozen section analysis, and no attempts at transoral robotic resection were aborted in favor of alternative approaches. The robotic resected tonsillar primary tumors and unilateral tongue base tumors were coupled with ipsilateral level I – IV neck dissections. Base of tongue malignancies extending across the midline were paired with bilateral level I – IV neck dissections. Patients were pathologically staged according to the American Join Committee on Cancer Criteria11, and standard descriptive statistics are used to summarize the data. Results Sixty-six consecutive patients with oropharyngeal carcinoma who underwent TORS with concomitant neck dissection by the contributing authors comprised the subjects of this review. Nineteen (28.8%) of the subjects were identified intraoperatively as having an iatrogenic orocervical communication. All defects were detected via direct visualization, and or intraoral irrigation flooding that revealed a pharyngeal breach. Of the 19 patients identified as having an operative fistula, 15 had tumor removal from the tonsillar fossa, and 4 had resection of tongue base primaries. The pathology confirmed TNM staging of the 19 patients is as follows: 8 stage T1 tumors, 9 stage T2 tumors, 1 stage T3 tumor, and 1 stage T4a tumor. Despite the fact that 17 of the 19 were low T stage malignancies, all 19 collectively suffered from advanced stage disease: 4 stage III, 14 stage IVa, and 1 stage IVb. The pharyngocervical defects ranged from 5mm in diameter, up to 4cm in diameter. All defects less than 1 cm in diameter were managed via transoral or transcervical primary closure of the pharyngeal constrictors, followed by transcervical application of 4ml of Tisseel (Baxter Bioscience, Deerfield, IL) fibrin sealant and suction drain placement. This patient subset resumed clear liquid oral intake on post operative day 1, and retained their cervical drains until the output dropped to 10ml in a continuous 24 hour time period. Defects greater than one centimeter underwent suction drain placement, were closed primarily when feasible, reenforced with muscular coverage and bathed with Tisseel. In all cases of muscular introduction, the digastric and mylohyoid muscles were utilized. In 3 cases a sternocleidomastoid myofascial flap was employed. The patients with defects greater than 1 cm underwent nasogastric feeding tube placement intraoperatively, and were made NPO for 24 – 48 hours. Cervical drains were managed mirroring those of the first group. On post operative day 2 a clear liquid diet was employed if there was no clinical suspicion for fistula formation. Regardless of defect diameter, intravenous antimicrobial coverage was initiated with either Cefazolin/Metronidazole or Clindamycin. Of the 19 patients identified as having a communication, 3 went on to develop a delayed pharyngocutaneous fistula after hospital dismissal. Two of the patients had T2 tumors (1 tonsil and 1 tongue base), and the third subject had a T1 tonsillar primary. They all varied in their nodal staging: N1, N2a, and N2b, and their intraoperative fistula size ranged anywhere from 5mm to 2cm in greatest dimension. Time until clinical presentation ranged from post operative day 7 to POD 12. Interestingly these patients had not been treated with prior operative or non operative therapy for their carcinoma. Patients with pharyngocutaneous fistulae were treated with non operative, aggressive clinical therapy. All underwent controlled incision and drainage via way of their neck dissection surgical site in an outpatient setting. Rigorous debridement of necrotic tissue was followed by wound packing with half inch Iodoform gauze. Initial local wound care was followed by application of a Barton pressure dressing. These patients were restarted on antibiotics, made NPO and underwent indirect placement of a nasogastric feeding tube for alimentary support. Patient/caregiver education was provided in regards to wound care and enteral nutrition in an outpatient setting, and none of the patients required hospital readmission. . Fistula closure was documented within two weeks in all three cases via clinical inspection and dynamic video swallowing evaluation. None of the patients required reoperation with local or free tissue reconstruction. Once fistula resolution was ascertained, the feeding tubes were removed and an oral diet was resumed. All three patients were able to implement adjuvant therapy four weeks post operatively. None of the 47 patients who lacked an orocervical communication intraoperatively developed delayed fistulization. Further, none of the sixty-six subjects comprising this entire review required reintubation or unplanned tracheostomy. Discussion Squamous cell carcinoma of the oropharynx will affect 9,000 new patients in the United States in 2009, and will be responsible for upwards of 70,000 deaths worldwide during the same calendar year1213. A retrospective analysis of the National Cancer data base has indicated that upfront surgical ablation of oropharyngeal neoplasia followed by radiation therapy affords a survival benefit compared to chemoradiation or radiation alone 14. Several reported series from multiple institutions have shown superior local control and five year survival rates employing this aforementioned treatment algorithm15-16. Though the benefit of initial surgical resection is recognized, traditional operative approaches to the oropharynx have left patients with significant functional and cosmetic impairments, resulting in a trend towards nonoperative therapy3. The recent evolution of transoral laser microsurgery (TLM) has revived enthusiasm for surgical therapy as a primary treatment modality for oropharyngeal carcinoma. This technique, however, has a steep learning curve, a laryngoscope limited view of the disease involved field, and challenges with both tissue manipulation and vascular control. In pursuit of a universal user friendly transoral approach to oropharyngeal neoplasia several authors have recently reported on the operative advantages associated with transoral robotic surgery (TORS)2-4,6-9. The daVinci robotic system allows for an up close, three dimensional view of the tumor field, wristed 6 degree motion, tremor filtration, and it affords users a shorter learning curve when compared to TLM2,3,8,17. Weinstein et al.2 demonstrated acceptable oropharyngeal competency with TORS for squamous cell carcinoma of the tonsil, but with staged neck dissection 1-3 weeks later. . Advocates for delayed neck dissection site a primary worry of fistulization, increased laryngopharyngeal edema resulting in acute functional impairment, and the ability to pursue additional tissue resection should permanent pathology reveal tumor involved margins. Though these arguments are defendable, delayed treatment of the neck is likely associated with increased cost (multi operation therapy, multi hospitalization), longer convalescence, a delay in recommended adjuvant therapy after primary tumor resection, and one could theoretically question patient compliance/acceptance due to drawn out treatment course. The literature is scarce regarding TORS with simultaneous neck dissection. Genden et al.6 were the first to report on 15 patients treated for squamous cell carcinoma with TORS and concomitant neck dissection. They documented one intraoperative orocervical fistula that responded to local musculomucosal flap coverage. None of their patients required tracheostomy. Boudreaux et al. reported nine cases of robotic assisted oropharyngectomy with synchronous neck dissection, with no subjects sustaining intra/postoperative orocervical communications. Our results showed that intraoperative pharyngocervical defects were not uncommon (28.8% of patients), but that when identified and meticulously managed, seldomly (15.8%) resulted in delayed pharyngocutaneous fistulization. When pharyngocervical breakdowns ensued, aggressive non operative management was associated with rapid healing, resulted in no hospital readmissions/reoperation, precluded a delay in postoperative therapy, and was not associated with prolonged oropharyngeal dysfunction. Although communications ensued regardless of tumor T staging, all defects were associated with advanced stage disease. This correlation should alert the surgical oncologist to an increased probability of an orocervical communication when treating stage III and IV oropharyngeal disease. Based on our clinical experience we feel that TORS with simultaneous neck dissection is a safe effective primary treatment modality for select patients with oropharyngeal malignancies. TORS with synchronous neck dissection Intra operative orocervical communication No communication -Neck drain (output <10ml in 24 hrs.) -NO dressing -NO feeding tube -Clear liquid diet, advance as tolerated < 1cm -Primary closure -Tisseel -Neck drain (output <10ml in 24 hrs.) -Clear liquid diet POD1 >1 cm -Primary closure if feasible -Muscle coverage (mylohyoid, digastric, SCM) -Tisseel -Neck drain (output <10ml in 24 hrs.) -Feeding tube -NPO 24-48hrs. If no leak start clear liquid diet (ADAT) Pharyngocutaneous fistula -Controlled incision and drainage, necrotic tissue debridement -Iodoform packing (changed bid) +/- barton dressing, NPO with feeding tube placement References 1. Moore EJ, Henstrom, Olsen KD, Kasperbauer JL. Transoral resection of tonsillar squamous cell carcinoma. Laryngoscope 2009;119:508-515. 2. Weinstein GS, O’Malley BW, Snyder W, Sherman E, Quon H. Transoral robotic surgery radical tonsillectomy. Arch Otolaryngol Head Neck Surg 2007;133:1220-1226. 3. O’Malley BW, Weinstein GS, Snyder W, Hockstein NG. Transoral robotic surgery (TORS) for base of tongue neoplasms. Laryngoscope 2006;116:1465-1472. 4. Moore EJ, Olsen KD, Kasperbauer JL Transoral robotic surgery for oropharyngeal squamous cell carcinoma: a prospective study of feasibility and functional outcomes. Laryngoscope 2009. 5. Lobe TE, Wright SK, Irish MS. Novel uses of surgical robotics in head and neck surgery. Journal of Laparoendoscopic and Advanced Surgical Techniques 2005;15:647-652. 6. Genden EM, Desai S, Sung CK. Transoral robotic surgery for the management of head and neck cancer: a preliminary experience. Head and Neck 2009;10.1002:283-289. 7. Boudreaux BA, Rosenthal EL, Magnuson JS, Newman JR, Desmond RA, Clemons L, Carroll WR. Robot-assisted surgery for upper aerodigestive tract neoplasms. Arch Otolaryngol Head Neck Surg 2009;135:397-401. 8. Solares CA, Strome M. Transoral robot assisted CO2 laser supraglottic laryngectomy: experimental clinical data. Laryngoscope 2007;117:817-820. 9. Weinstein GS, O’Malley BW, Snyder W, Hockstein NG. Transoral robotic surgery: supraglottic partial laryngectomy. Annals of Otology, Rhinology, and Laryngology 2007;116:19-23. 10. Holsinger FC, McWhorter AJ, Menard M, Garcia D, Laccourreye O. Transoral lateral oropharyngectomy for squamous cell carcinoma of the tonsillar region: I. technique, complications, and functional results. Arch Otolaryngol Head Neck Surg 2005;131:583-591. 11. Greene FL, Page DL. Et al., editors. AJCC Cancer Staging Manual. 6th ed. New York, NY: Spring;2002 12. Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clinic 2006;56:106-130. 13. Parkin DM, Bray F, Feraly J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer 2001;94:153-156. 14. Zhen W, Karnell LH, Hoffman HT, et al. The national cancer database report on squamous cell carcinoma of the base of tongue. Head and Neck 2004;26:660-674. 15. Nisi KW, Foote RL, Bonner JA, McCaffrey TV. Adjuvant radiotherapy for squamous cell carcinoma of the tongue base: improved local-regional disease control compared with surgery alone. Int J Radiat Oncol Biol Phys 1998;41:371-377. 16. Zelefsky MJ, Harrison LB, Armstrong JG. Long-term treatment results of post operative radiation therapy for advanced stage oropharyngeal carcinoma. Cancer 1992;70:2388-2395. 17. Hockstein NG, Nolan JP, O’Malley BW, Woo YJ. Robotic assisted pharyngeal and laryngeal microsurgery: results of robotic cadaver dissections. Laryngoscope 2005;115:1003-1008.