Medical Screening and Evacuation
advertisement

[
RESIDENT’S CASE PROBLEM
]
MICHAEL S. CROWELL, PT, DPT¹DEHC7DM$=?BB" PT, DSC, OCS, FAAOMPT²
Medical Screening and Evacuation:
Cauda Equina Syndrome in a Combat Zone
ow back pain (LBP) is a prevalent condition, particularly in
primary care clinics, with billions of dollars spent each year
on treatment.33 It is the fifth most common reason for all
physician visits in the United States.11 Approximately 25% of
adults report LBP lasting at least 1 day within the past 3 months,11
with approximately 14% having an episode that lasts longer than 2
weeks.15 Prevalence ranges from 15% to 20% over a single year40
and approximately 70% over the course of a person’s lifetime.15,27,30,40
L
The majority of patients (85%)
with LBP have conditions that cannot
be reliably attributed to a specific disTIJK:O:;I?=D0 Resident’s case problem.
T879A=HEKD:0 Cauda equina syndrome (CES)
is a rare, potentially devastating, disorder and is
considered a true neurologic emergency. CES often
has a rapid clinical progression, making timely recognition and immediate surgical referral essential.
T:?7=DEI?I0 A 32-year-old male presented to a
medical aid station in Iraq with a history of 4 weeks
of insidious onset and recent worsening of low back,
left buttock, and posterior left thigh pain. He denied
symptoms distal to the knee, paresthesias, saddle
anesthesia, or bowel and bladder function changes.
At the initial examination, the patient was neurologically intact throughout all lumbosacral levels
with negative straight-leg raises. He also presented
with severely limited lumbar flexion active range of
motion, and reduction of symptoms occurred with
repeated lumbar extension. At the follow-up visit, 10
days later, he reported a new, sudden onset of saddle
anesthesia, constipation, and urinary hesitancy,
with physical exam findings of right plantar flexion
ease or spinal abnormality.11,15 Current
recommendations suggest classifying
patients into 3 broad categories: nonspeweakness, absent right ankle reflex, and decreased
anal sphincter tone. No advanced medical imaging
capabilities were available locally. Due to suspected
CES, the patient was medically evacuated to a neurosurgeon and within 48 hours underwent an emergent
L4-5 laminectomy/decompression. He returned to full
military duty 18 weeks after surgery without back or
lower extremity symptoms or neurological deficit.
T:?I9KII?ED0 This case demonstrates the importance of continual medical screening for physical therapists throughout the patient management
cycle. It further demonstrates the importance of
immediate referral to surgical specialists when
CES is suspected, as rapid intervention offers the
best prognosis for recovery.
TB;L;BE<;L?:;D9;0 Differential diagnosis,
level 4. J Orthop Sports Phys Ther 2009;39(7):541549. doi: 10.2519/jospt.2009.2999
TA;OMEH:I0 direct access, lumbar spine, low
back pain, red flags, spinal cord
cific LBP, nerve root syndrome (radiculopathy or stenosis), and serious spinal
pathology.11,30
LBP secondary to nerve root syndrome, although less common, is a potentially disabling condition.23 Nerve
root syndrome may be related to radiculopathy, spinal stenosis, or cauda equina
syndrome (CES).23 Due to the potential
for poor prognosis, timely recognition of
neurologic involvement is essential for
optimal patient outcomes.23
Acute lumbar disc herniation is one
potential source of both radiculopathy
and CES. Approximately 90% of cases of
sciatica are caused by a herniated disc.29
Overall incidence of symptomatic disc
herniation is 1% to 2%,29,39 for which
200 000 discectomies are performed annually.39 Peak incidence of this disorder is
between the ages of 30 to 55 years.15
Characteristics of acute disc herniation include abrupt, intense onset of
pain that is increased by bending or lifting.48 The most common levels of symptomatic herniation are L5-S1 and L4-5,
which comprise approximately 90% to
98% of cases11,15 and correspond to the
spinal levels that receive the majority of
compressive forces in the lumbar spine.
Clinically, disc herniation at these levels
frequently manifests as L5 and S1 nerve
root compression disorders characterized by radiating pain below the knee,
1
Brigade Combat Team Physical Therapist, Iraq. 2 Program Director and Associate Professor, US Army-Baylor University Postprofessional Doctoral Program in Orthopedic Manual
Physical Therapy, Brooke Army Medical Center, Fort Sam Houston, TX. This case was seen at a Troop Medical Clinic in Iraq. The opinions or assertions contained herein are the
private views of the authors and are not to be construed as official or reflecting the views of the United States Army or Department of Defense. Address correspondence to CPT
Michael Crowell, 235 Lancaster Way, Richmond Hill, GA 31324. E-mail: michael.crowell2@us.army.mil
journal of orthopaedic & sports physical therapy | volume 39 | number 7 | july 2009 | 541
[
RESIDENT’S CASE PROBLEM
]
:?7=DEI?I
TABLE 1
Red Flags
History of Present Illness
T
Unrelenting night pain
History of cancer or recent infection
Unexplained weight loss or gain
Recent trauma
Difficulty with micturation*
Loss of anal sphincter tone or fecal incontinence*
Saddle anesthesia*
Gait disturbance*
* Indicates elements specific to cauda equina syndrome.
decreased sensation in a dermatomal
pattern, myotomal weakness, reflex
changes, and positive straight-leg raise
tests.11,15 However, examination of patients with acute disc herniation should
always include careful screening for serious pathology, both before initiation
of and during ongoing conservative
interventions. 3,11 Red flag differential
diagnoses may include CES, metastatic
spinal disease, spinal infection, epidural hematoma, and spinal fracture
or dislocation. 3 Screening for red flag
conditions should include questions
regarding bowel and bladder function
changes, sensory function changes in
the perianal region and genitals, unexplained weight loss or gain, fever, night
pain, history of cancer or infection,
history of trauma, and any gait disturbances (TABLE 1). 3,22
In adults, the spinal cord is approximately 42 to 45 cm in length and terminates at the lower border of the first
lumbar vertebra or upper border of the
second lumbar vertebra at the conus medullaris.20 The spinal cord is ensheathed by
3 protective membranes from outward to
within: the dura mater, arachnoid, and
pia mater.20 These membranes extend
to the first segment of the coccyx as the
filum terminale.20 The outer layer of the
dura, arachnoid, and the subarachnoid
cavity is termed the thecal sac, which is
filled with cerebrospinal fluid.20
The term cauda equina describes the
lumbar and sacral spinal nerves descending from the conus medullaris. During
embryo development, the spinal cord and
vertebral column have relatively unequal
rates of growth.20 As a result, the lumbar
and sacral spinal nerves descend almost
vertically to reach their points of exit.20
This configuration resembles a “horse’s
tail,” from which the term cauda equina
is derived in Latin.
CES is a rare, potentially devastating
disorder that may arise from an acute
disc herniation and is considered a true
neurologic emergency.8,45,48 The estimated
prevalence of CES is 0.04% of all patients
presenting with a primary complaint of
LBP,11,15,45 and it is most prevalent in the
fourth or fifth decade of age.43,45 CES occurs in 1% to 2% of all lumbar disc herniations that progress to surgery.1,8,15,43,44
CES is most frequently associated with
a nontraumatic massive midline posterior disc herniation, commonly located at
L4-5, followed by L5-S1 and L3-4.43,44,45,48
The sacral nerves, which lie medially in
the cauda equina, are affected disproportionately in this disorder. A clear diagnosis or a high index of suspicion for CES
should prompt immediate referral to a
surgical specialist. Referral to an orthopaedic spine surgeon or neurosurgeon,
where available, is the most direct route
of referral; otherwise, the patient should
be sent to an emergency department.
The purpose of this resident’s case
problem is to describe the evaluation,
treatment, referral, and outcomes of a
patient exhibiting signs and symptoms
of CES evaluated by a physical therapist
in a direct-access environment.
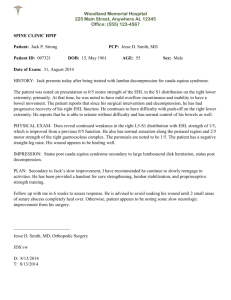
he patient was a 32-year-old
Caucasian male (height, 1.83 m;
body mass, 77.1 kg; body mass index, 23.1 kg/m2) who initially presented
to a physical therapist in a combat zone
with a chief complaint of insidious onset
low back and left posterior thigh pain. He
was deployed for combat with a primary
responsibility of training foreign military
officers. During convoy operations, he was
a machine gunner, standing in the turret
at the top of an armored vehicle. This job
required prolonged periods of wearing
protective equipment weighing in excess of 36 kg, often for periods exceeding 8 hours. His symptoms were located
in the lower lumbar spine (left greater
than right), left buttock, and left posterior thigh, as shown in <?=KH;'. The total
duration of symptoms was approximately
4 weeks, but the patient reported a significant increase in intensity of pain the
day prior to evaluation without any specific trauma. He described a dull, aching
pain, and a pain that was intermittently
sharp. The patient denied numbness or
tingling in any location or pain below the
level of the knee. Baseline numeric pain
rating scale (NPRS),25 where 0 is no pain
and 10 is the worst pain that the patient
could imagine, was 4/10 at rest and 7/10
at worst. The patient noted increased
pain with running and forward flexion of
the lumbar spine. Rest and lying supine
relieved his symptoms. His past medical
history was significant for 3 to 4 prior occurrences of LBP over the past 8 years,
with similar presentation that, he stated,
resolved without treatment. The patient
had no history of spine or extremity surgery. No previous imaging studies had
been performed. His stated goal was to
decrease his overall pain level during performance of his military duties.
Systems Review
The patient denied saddle anesthesia,
bowel or bladder function changes, unexplained weight loss or gain, night pain, or
542 | july 2009 | volume 39 | number 7 | journal of orthopaedic & sports physical therapy
Assessment, Intervention,
and Re-evaluation
<?=KH;'$Body chart of symptoms at initial presentation through day 9.
recent trauma, and had no history of cancer
or infection. In screening for nonmusculoskeletal pathology, the patient reported no
history of cancer, cardiovascular, or pulmonary disease, and no recent occurrence
of nausea, vomiting, fever, changes in appetite, difficulty swallowing, shortness of
breath, dizziness, or changes in balance.
Test and Measures
The patient was neurologically intact
bilaterally with 5/5 strength as assessed
with manual muscle testing26 throughout the L2 to S1 myotomes, sensation
was intact to light touch throughout the
L2 to S1 dermatomes, and knee jerk and
ankle jerk muscle stretch reflexes were
2+ (normal). Babinski reflex testing was
negative. He presented with decreased
lumbar lordosis and a guarded, obviously
painful, movement of the spine. The patient displayed a left-sided antalgic gait,
with decreased left hip extension and
early termination of the stance phase of
the gait cycle. Active range of motion was
severely limited in lumbosacral flexion,
with the ability to reach only the midanterior thigh region with the fingertips,
and moderate to severe pain in the low
back, left buttock, and left posterior thigh
at the end range of motion. Lumbosacral
extension and side bending were within
normal limits, without an increase in
pain from his baseline NPRS. Repeatedmotion testing was performed as described by McKenzie.35 Ten repetitions
of flexion in standing increased his back,
buttock, and posterior thigh pain, while
10 repetitions of extension in standing
reduced those symptoms. Straight-leg
raise tests did not produce radicular pain
but caused a severe increase in LBP at 15°
of hip flexion on the right and 45° of hip
flexion on the left. Hip flexion range of
motion during single knee to chest was
within normal limits bilaterally, with increased LBP that was approximately 50%
less than with straight-leg raise testing.
A lumbar quadrant test was negative bilaterally. Passive vertebral motion testing,
as described by Maitland,34 produced local pain at L3, L4, and L5 with central
passive posterior-anterior accessory intervertebral motion (PAIVM). Unilateral
PAIVM testing produced local pain at
L3-4, L4-5, and L5-S1, equal bilaterally.
No referral of pain was noted with passive accessory movement assessment.
Using a treatment-based classification
approach,6,7,18 the patient was classified
into the specific exercise classification
and prescribed extension-oriented exercises. Either standing or prone repeated
extension exercises were to be performed
every 2 waking hours, with 10 repetitions,
holding each repetition 2 to 3 seconds at
end range. Education consisted of avoidance of sitting for greater than 20 to 30
minutes, avoidance of full end-range
flexion positions, and the use of a lumbar
roll while sitting and wearing protective
equipment. The treating physical therapist, who had privileges for prescribing
nonnarcotic medication,5 prescribed 7.5
mg Meloxicam (Mobic, 2 tablets once
daily) and 500 mg acetaminophen (Tylenol, 2 tablets every 4-6 hours, as needed)
for pain relief during performance of his
military duties. Because this patient was
essential to the success of his unit’s mission, only a home exercise program was
prescribed, and a follow-up was scheduled for 2 weeks later. He was instructed
to return to the clinic at an earlier time
for re-evaluation if symptoms worsened.
The patient presented for follow-up on
day 4 (3 days after the initial evaluation)
with a complaint of increased pain unrelieved by positioning and only short-term
relief with the home exercise program.
His baseline NPRS at rest had increased
to 6/10. He reported a decreased NPRS
to 4/10 after performing home exercises,
but he would return to baseline after approximately 30 to 60 minutes. Since the
initial evaluation, he had continued to
perform all of his duties, including extended wear of protective equipment.
The physical examination, including the
neurological examination, did not differ
from the initial evaluation, with the exception of increased pain with all testing.
His case was discussed with a physician
and he was prescribed a narcotic pain
medication for use as needed, re-educated in the home exercises to ensure proper
performance, and instructed to continue
the home exercises as tolerated. The pa-
journal of orthopaedic & sports physical therapy | volume 39 | number 7 | july 2009 | 543
[
RESIDENT’S CASE PROBLEM
tient was to follow-up within 1 week to
monitor the stability of his symptoms and
assess his response to the modified treatment plan.
At a second follow-up 3 days later (day
7 after initial exam), the patient continued to have significant pain. He was able
to perform his duties, but the sharp pain
was becoming more frequent and intense. He also reported a recent onset
of numbness in his left posterior thigh.
He continued to deny any radiating pain
below the knee or right-sided symptoms.
The physical exam was unchanged from
initial evaluation and a neurological assessment continued to reveal no motor, sensory, or reflex deficits bilaterally.
Although strength of left ankle plantar
flexion was 3+/5, he was limited by pain
secondary to a recent ankle inversion
sprain on rocky, uneven terrain, which
he described as unrelated to his low back
symptoms and had occurred between the
first and second re-evaluation.
Due to increasing pain despite conservative therapy and medications, he was
restricted from missions that required the
wear of his protective gear and from any
lifting, bending, or twisting. Daily physical therapy intervention in the clinic was
initiated at that time. The therapist chose
to continue with a supervised exercise
program and adjunct pain-relieving modalities, because the high-load demands
of this patient’s work duties up to that
point made accurate assessment of the
patient’s response to treatment difficult.
Intervention consisted of interferential
electrical stimulation with 4 pads bracketing the symptomatic area of the lumbar
spine, the patient positioned in prone,
and the intensity at the patient’s level of
tolerance. Treatment was combined with
moist heat for 20 minutes, followed by
supervised extension exercises and left
lumbar rotation stretches, both of which
provided mild relief of the lower extremity pain. Lumbar extension exercises consisted of 3 sets of 10 repetitions, with a
2- to 3-second hold at end range, without
manual overpressure. Lumbar left rotation stretching consisted of 30-second
]
<?=KH;($Body chart of symptoms at 10-day follow-up.
holds, with 3 repetitions. The patient’s
home exercise program remained unchanged from the initial evaluation.
Upon presenting for his third day of
in-clinic treatment (10 days after initial
evaluation), the patient had a new complaint of numbness and tingling in the
saddle region and a change in bowel and
bladder function. Although he denied any
incontinence, he stated that it was difficult to control initiation and cessation
of urination and bowel movements. The
patient also described new symptoms
in the right lower extremity (previously
asymptomatic), with an inability to rise
up onto his toes and constant tingling in
the right calf, while his left lower extremity symptoms were unchanged from the
last evaluation. <?=KH;( shows the body
chart associated with the new symptom
presentation. He stated, however, that his
pain level had decreased to 4/10 at rest
and 5/10 at worst since he stopped wearing his protective gear 2 days prior.
A detailed physical examination was
performed, with an orthopaedic physician assistant on staff providing further
guidance on neurological assessment of
the S3-4 levels. Lumbar spine range of
motion was unchanged from the initial
evaluation. A straight-leg raise test bilaterally continued to provoke symptoms
only in the low back region. No sensory
deficiencies to light touch or sharp-dull
stimuli were noted throughout the lower
extremities bilaterally, including the L4S1 dermatomes. Strength was reduced in
right ankle plantar flexion to 3–/5. The
right ankle jerk (S1) reflex was absent. A
rectal examination revealed decreased
anal sphincter tone and an absent anal
wink reflex. The cremasteric reflex was
intact. The Babinski reflex was normal.
Gait was severely impaired with a decreased step length bilaterally and impaired toe-off present on the right.
Referral
Because of his rapidly progressive neurological symptoms and a suspicion of
cauda equina compression, the physical therapist scheduled the patient for
medical evacuation and referral to a
neurosurgeon. No advanced imaging was
performed, as magnetic resonance imaging (MRI) and computed tomography
(CT) scan capabilities were not available
at the local facility. Evacuation to neurosurgery care and advanced medical imaging occurred within 48 hours.
544 | july 2009 | volume 39 | number 7 | journal of orthopaedic & sports physical therapy
J78B;(
Radiology Impression of Computed Tomography
(CT) Scan Prior to Surgical Intervention
L1-2: No disk bulge, central canal, or neuroforaminal stenosis
L2-3: No disk bulge, central canal, or neuroforaminal stenosis
L3-4: Broad-based disk bulge with no sadistic and central canal or neural foraminal stenosis
L4-5: Moderate disk space narrowing; degenerative changes of the inferior endplate of L4; large disk protrusion with
moderate central canal stenosis, difficult to tell, but likely some extruded fragments posterior to L5; moderate to
severe lateral recess stenosis bilaterally; exiting nerve roots in the neural foramina appear relatively normal
L5-S1: No significant disk bulge, central canal, or neural frontal stenosis
D[kheikh]_YWbWdZ?cc[Z_Wj[
Postoperative Care
Upon arrival at a Combat Support Hospital, the patient was evaluated by a military neurosurgeon. Physical examination
findings were consistent with those at the
medical aid station. Additionally, bladder
function was evaluated and the patient
was found to have a postvoid residual
of 300 cc. Although MRI is the recommended imaging modality for CES, because of the detail provided to the soft
tissues and spinal canal,11 it was not available in that location either. Instead, a CT
of the lumbar spine with contrast, an alternate recommendation to image CES,11
was performed. The findings reported by
the radiologist were suggestive of underlying pathology that could be clinically
correlated with CES (J78B;().
Following neurosurgical evaluation,
he was prepped for immediate surgical intervention. A L4-5 laminectomy
and decompression was performed and
a large extruded disc fragment was removed from the epidural space. The next
day the patient was evacuated to Landstuhl Regional Medical Center in Germany for inpatient recovery. Three days
postsurgery, he was evaluated by a physical therapist. He had an NPRS of 2/10,
continued complaints of bowel and bladder dysfunction, and continued right calf
weakness. He was independent in bed
mobility, edge-of-bed activities, and sitto-stand transfers. Right ankle plantar
flexion was 3+/5, but the patient was able
to independently ambulate approximately
18 m. The patient was instructed in ankle
pumps along with progressive ambulation to prevent deep venous thrombosis2,9
and, to enhance functional recovery, with
lower extremity exercises aimed to maintain nervous tissue mobility to prevent
postoperative nerve root scarring. After
3 days in Germany, the patient was then
evacuated to his final destination, Brooke
Army Medical Center, Fort Sam Houston,
TX, for follow-up neurosurgical care and
recovery.
H[Yel[hoWdZEkjYec[
The patient arrived at Brooke Army Medical Center 6 days after surgery. An MRI
performed on admission demonstrated
normal postoperative changes and no
residual disc herniation. During his first
neurosurgery postoperative evaluation,
he presented with right buttock pain,
resolving saddle paresthesia, numbness
of the right lateral foot region and toes,
bladder incontinence, and erectile dysfunction. Ankle and knee muscle stretch
reflexes on the right were hypoactive, but
he had 5/5 strength throughout both lower extremities. Within 1 week he returned
to neurosurgery with some residual right
buttock and foot symptoms, resolved saddle paresthesia, and normal reflexes. He
was cleared by the surgeon for medical
convalescent leave for 30 days, with an
intended referral to a physical therapist
upon return. Upon return from convalescent leave (approximately 6 weeks after
surgery), he had regained full sensory
function and continued to demonstrate
normal motor function. No referral was
made to physical therapy, and the patient
was cleared by the surgeon to progress his
walking distance as tolerated and start
stationary bike exercising. By 12 weeks,
the patient had self-progressed to walk-
ing 1.6 km daily, doing pool exercises at
home, and using 1- to 2-kg weights for
upper extremity exercises. At 4-month
follow-up he had no residual neurological
or functional deficits and reported a current walking program with a 5-kg backpack. He was cleared by neurosurgery for
full return to military duties, including
redeployment.
:?I9KII?ED
T
his resident’s case problem describes what could be considered a
classic presentation of CES, recognized by a physical therapist practicing
in a direct-access setting. By a continual
medical-screening process over multiple
visits, the therapist recognized an atypical progression of mechanical LBP, which
then acutely manifested itself as CES.
Early recognition, confirmation, referral,
and surgical intervention were associated
with a good outcome, consistent with literature that suggests a good prognosis
with early detection and treatment.1,43,44
C[Y^Wd_YWbB8F
The patient in this case initially presented with a history and physical examination findings consistent with nonspecific
mechanical LBP and no red flag signs
or symptoms. Recent research supports
the use of a treatment-based classification approach for acute LBP of this nature.6,7,10,18,24 Due to centralization of his
symptoms with repeated movement in
extension, this patient was classified into
the specific exercise classification based
upon the first step in the algorithm described by Fritz et al.18 Browder et al7
examined the effectiveness of an extension-oriented treatment approach in a
subgroup of patients with LBP extending distal to the buttocks that centralized
with extension movements. In patients
meeting these criteria, treatment using
extension-oriented exercises resulted in
significantly greater reduction of pain
and disability than treatment using lumbar stabilization exercises. Additionally,
Long et al32 demonstrated that patients
journal of orthopaedic & sports physical therapy | volume 39 | number 7 | july 2009 | 545
[
RESIDENT’S CASE PROBLEM
with a movement directional preference
for symptom reduction (extension in this
case) significantly improved when performing specific exercises in that direction as opposed to general exercise, and
worsened performing exercises in the opposite direction.
compression. Although his finger-to-floor
distance was severely limited, this physical examination finding may also be associated with nonspecific LBP, which was
his initial classification.
The current case describes mechanical
LBP without initial evidence of nerve root
dysfunction, which rapidly progressed to
CES. A thorough evaluation is essential
for accurate identification of LBP with
nerve root syndrome and CES. The patient history should include any potential
mechanisms of injury, the location, description, nature, and intensity of pain,
the presence or absence of any sensory
abnormalities, aggravating factors, easing factors, and past medical history. The
physical examination should include a
neurologic screen, an assessment of lumbosacral range of motion, assessment of
passive vertebral motion, the straight-leg
raise test, tests for muscle flexibility, and
tests for sacroiliac dysfunction. Sensitivity, specificity, and likelihood ratios for
various physical examination and historical items with respect to nerve root
syndrome are listed in TABLE 3.
In general, information from the patient history is better for ruling out nerve
root syndromes and the physical examination is better for ruling in.50 Significant
indicators of nerve root syndrome include
focal muscle weakness and limited lumbar flexion, as indicated by a large fingerto-floor distance.23 Other predictors may
include lower extremity pain that is greater than back pain, a dermatomal pattern
of pain location, and increased pain with
coughing, sneezing, and straining.23
The patient in this case report did not
clearly fit into a nerve root classification
during the initial visits. He presented
with symptoms proximal to the knee,
and neurologic screening did not reveal
either motor loss, sensory impairment,
or diminished reflexes. Straight-leg raise
testing did not produce lower extremity symptoms consistent with nerve root
:_W]dei_ie\9;I
CES often has a rapid clinical progression
from other forms of LBP, which makes
timely diagnosis extremely important.
CES must be included in the differential
Diagnostic Test Properties for
Tests of Nerve Root Dysfunction
TABLE 3
D[hl[Heej:oi\kdYj_ed
]
I[di_j_l_jo
If[Y_ÓY_jo
!BH
ÅBH
Patient history
Presence of sciatica15
0.95
Lower extremity pain greater than back pain50
0.82
0.54
1.74
0.33
Dermatomal distribution of pain50
0.89
0.31
1.3
0.34
Physical examination
Paresis (weakness, not specific)50
0.27
0.93
4.11
0.78
Absent knee jerk or ankle jerk50
0.14
0.93
2.21
0.78
Finger-to-floor greater than 25 cm50
0.45
0.74
1.71
0.75
Straight-leg raise11,12,15,15,29*
0.91
0.26
1.23
0.35
Crossed straight-leg raise11,12,14,23,29†
0.29
0.88
2.42
0.81
Ankle dorsiflexion weakness15
0.35
0.7
1.17
0.93
0.71
Great toe extension weakness12,15,31
0.50-0.61
0.55-0.70
1.36-1.67
Impaired ankle jerk12,15,23,31
0.47-0.50
0.6-0.90
1.25-4.70
0.83
Ankle plantar flexion weakness15
0.47-0.60
0.76-0.95
1.96-12.0
0.42-0.70
Quadriceps weakness15
0.01-0.40
0.89-0.99
1.00-3.64
0.67-1.00
Abbreviations: +LR, positive likelihood ratio; –LR, negative likelihood ratio.
* Positive straight-leg raise defined as reproduction of radicular symptoms with elevation of the ipsilateral lower extremity between 30° and 70° of hip flexion.
†
Positive crossed straight-leg raise defined as reproduction of radicular symptoms with elevation of the
contralateral lower extremity between 30° and 70° of hip flexion.
TABLE 4
Differential Diagnosis of Low Back Pain (LBP)
With Potential Neurologic Involvement
HWZ_YkbefWj^o<hec
7Ykj[:_iY>[hd_Wj_ed
Spinal Stenosis
Cauda Equina Syndrome
Age (y)
30-55
60
40-60
History
Acute or recurrent episodes
Insidious onset of
chronic, progressive
LBP; more recent
onset of lower extremity symptoms
Insidious onset of severe LBP
with or without saddle
anesthesia, bowel/bladder
function changes, possible
history of chronic LBP
Pain pattern
Pain and/or numbness
radiating to 1 lower
extremity below the
knee, usually increased
with lumbar flexion
Lower extremity symptoms
increased with lumbar
extension, relieved by
lumbar flexion
Usually presents with radiating
pain and numbness/tingling
in both lower extremities,
increased with lumbar flexion
Neurological exam
Sensory and/or motor
changes, diminished/
absent deep tendon
reflexes unilaterally
Sensory and motor
changes
Bilateral sensory and/or motor
changes, diminished/absent
deep tendon reflexes, sensory
and motor changes at S3-4
levels
Range of motion
Guarded, limited
Pain and limited extension
Guarded, limited
Other tests
Straight-leg raise
Stage treadmill test
Straight-leg raise
546 | july 2009 | volume 39 | number 7 | journal of orthopaedic & sports physical therapy
diagnosis for patients presenting with
LBP with or without signs/symptoms of
nerve root compression,45 and the patient
history should include special questions
that attempt to identify patients with serious spinal pathology. TABLE 4 describes
common subjective and objective findings useful for the differential diagnosis
of possible neural involvement. Approximately 30% of patients present with
CES as the first manifestation of lumbar
disc herniation.1,44 More often, however,
patients will present with chronic LBP
that progresses rapidly to CES within 24
hours.43 Over a 10-day period of general
worsening but neurologic stability, the
patient in this case rapidly progressed
over 24 hours from a history without any
red flag symptoms to all of the red flags
associated with CES, including difficulty
with micturition, loss of anal sphincter
tone, saddle anesthesia, and severely impaired gait.
The physical examination to identify
CES must include assessment of the L1
to S3-4 levels, including anal sphincter
tone (S3-4), perianal sensation (S3-4),
the anal wink reflex (S3-4), and the cremasteric reflex (L1-2) (TABLE 5). The most
frequent physical exam finding is urinary
retention.11,15,23,45 A residual volume greater than 100 to 200 cc is considered positive for urinary retention.45 Decreased
anal sphincter tone is present in 60% to
80% of individuals with CES.15,45
Patients who present with severe or
progressive neurologic deficits should
have a prompt imaging work-up, with
MRI (preferred) or CT.11 While the advanced diagnostic imaging was delayed
in this case due to lack of availability, the
CT images demonstrating the patient’s
midline herniation at the L4-5 level were
consistent with the most common location and type of disc herniation associated with CES.11,15
Referral and Treatment of CES
The primary indicators for neurosurgical
referral for this patient were the presence
of bowel and bladder function changes,
saddle anesthesia, decreased anal sphinc-
Diagnostic Test Properties of
Tests for Cauda Equina Syndrome
TABLE 5
Urinary retention11,15,23,45
15,23
I[di_j_l_jo
If[Y_ÓY_jo
!BH
ÅBH
H[\[h[dY[i
0.9
0.95
18
0.01
Chou, Deyo, Haswell, Small
Unilateral or bilateral sciatica
0.80
Deyo, Haswell
Unilateral or bilateral motor/sensory deficits15,23
0.80
Deyo, Haswell
Positive straight-leg raise15,23*
0.80
Deyo, Haswell
Sensory deficit: buttocks, posterior-superior
thigh, perianal region3,15
0.75
Arce, Deyo
Abbreviations: +LR, positive likelihood ratio; –LR, negative likelihood ratio.
* Positive straight-leg raise defined as reproduction of radicular symptoms with elevation of the ipsilateral lower extremity between 30° and 70° of hip flexion.
ter tone, and progressive neurological
changes (new onset of significant motor
weakness in the S1 myotome).
CES is the primary absolute indication
for acute surgical treatment of lumbar
spine pathology.3 Rapid recognition coupled with timely referral and surgical care
provides the best chance of functional recovery.45 The treatment of choice is surgical decompression, usually a laminectomy
followed by discectomy.43,44 Performing
the laminectomy first allows excision of
the extruded disc material without undue
manipulation of the neural elements.43
The patient in this case had an emergent
laminectomy and decompression with removal of the extruded disc fragment from
the epidural space, confirming the diagnosis of CES. Surgical intervention was
performed within 72 hours of diagnosis,
which was extremely close to the length
of time where the risk of permanent neurologic deficit is increased. Although not
optimal, this delay was related to the realities of medical care in a combat environment, and every effort was made to
ensure a rapid evacuation of this patient
to a neurosurgeon. Even under standard
conditions, Shapiro44 previously reported
that only 45% of patients presenting to
the emergency room or primary care
physician underwent surgery within 48
hours.
Following surgery, the patient had limited inpatient physical therapy and was
later placed on a convalescent leave status
for 30 days. He was released with instructions to complete a progressive walking
program and given activity restrictions
consistent with discharge instructions for
patients receiving lumbar spine discectomy surgery. The patient was not referred
to outpatient physical therapy services as
part of his rehabilitation, possibly due to
his rapid symptom recovery, high level of
motivation to return to full function, and
ability to carefully progress on a general
home exercise program. Although this
patient did not receive postoperative outpatient physical therapy, there is strong
evidence to support intensive exercise
training beginning 4 to 6 weeks after
nonfusion lumbar spine surgery,13,16,37,42
which focuses on trunk/pelvis and lower
extremity strengthening,13,28,37 cardiovascular conditioning,41 and stretching of the
lumbopelvic musculature.41
Fhe]dei_ie\9;I
At his 18-week follow-up appointment,
the patient had an excellent result, with
no motor deficits, normal bowel and
bladder function, and return to full occupational duties. The excellent outcome
in this case highlights the importance of
early recognition of symptoms and immediate surgical referral.
Recent research has shown a significant advantage to treatment within 48
hours of onset.1,44 The risk of permanent
neurologic deficits is increased when
more than 72 hours elapses before definitive treatment1 and longer delays
correlate with worsening functional outcomes.8 In a meta-analysis of surgical
outcomes of CES, 3 factors suggestive
journal of orthopaedic & sports physical therapy | volume 39 | number 7 | july 2009 | 547
[
RESIDENT’S CASE PROBLEM
of a poor outcome were identified: history of chronic LBP, preoperative rectal
dysfunction (diminished motor or sensory function), and surgical intervention
greater than 48 hours after onset of CES.1
The patient in our case clearly recovered
better than expected, considering that all
3 of the items suggestive of a poor prognosis were present.
Attaching a numerical value to the
prognosis for patients with CES is difficult. A common problem in current research is the limited number of patients
studied, secondary to the rarity of the disorder. Subsequently, studies of CES often
have limited power to detect significant
differences in prognosis.1
F^oi_YWbJ^[hWfo:_h[Yj7YY[ii
During deployment in support of combat operations, military physical therapists provide direct access and primary
care for injured soldiers. The case of CES
presented here, however, is not necessarily unique to the military or combat
environment and a very similar presentation could be seen in any clinic with or
without direct access. Recent research
has shown that direct access to physical
therapy services does not compromise
patient safety. Physical therapists have
proven themselves able to identify serious
pathology that mimics a musculoskeletal
complaint4,17,19,21,36,38,49,51 and possess diagnostic accuracy equivalent to orthopaedic
surgeons.36,46
9ED9BKI?ED
P
hysical therapists must continually monitor patient status and
act appropriately when conditions
emerge that require immediate referral.
Physical therapists often treat a high volume of patients with LBP, the majority of
which are nonspecific and benign in nature. Although CES is a rare disorder, the
potential devastating consequences of a
missed diagnosis make a thorough evaluation and continuous medical screening
throughout the patient management
cycle essential. The current case problem
describes a unique episode of nonspecific
LBP with rapid progression to CES during
ongoing management, and correct diagnosis and referral by a physical therapist
in a direct-access setting. Timely referral
and surgical intervention in this case was
associated with an excellent outcome and
full functional recovery. T
13.
14.
H;<;H;D9;I
15.
1. Ahn UM, Ahn NU, Buchowski JM, Garrett ES,
Sieber AN, Kostuik JP. Cauda equina syndrome secondary to lumbar disc herniation:
a meta-analysis of surgical outcomes. Spine.
2000;25:1515-1522.
($ Aquila AM. Deep venous thrombosis. J Cardiovasc Nurs. 2001;15:25-44.
3. Arce D, Sass P, Abul-Khoudoud H. Recognizing
spinal cord emergencies. Am Fam Physician.
2001;64:631-638.
4. Baxter RE, Moore JH. Diagnosis and treatment
of acute exertional rhabdomyolysis. J Orthop
Sports Phys Ther. 2003;33:104-108.
5. Benson CJ, Schreck RC, Underwood FB,
Greathouse DG. The role of Army physical
therapists as nonphysician health care providers who prescribe certain medications:
observations and experiences. Phys Ther.
1995;75:380-386.
6. Brennan GP, Fritz JM, Hunter SJ, Thackeray A,
Delitto A, Erhard RE. Identifying subgroups of
patients with acute/subacute “nonspecific” low
back pain: results of a randomized clinical trial.
Spine. 2006;31:623-631.
7. Browder DA, Childs JD, Cleland JA, Fritz JM.
Effectiveness of an extension-oriented treatment approach in a subgroup of subjects
with low back pain: a randomized clinical
trial. Phys Ther. 2007;87:1608-1618; discussion 1577-1609. http://dx.doi.org/10.2522/
ptj.20060297
8. Busse JW, Bhandari M, Schnittker JB, Reddy
K, Dunlop RB. Delayed presentation of cauda
equina syndrome secondary to lumbar disc herniation: functional outcomes and health-related
quality of life. CJEM. 2001;3:285-291.
9. Cayley WE, Jr. Preventing deep vein thrombosis
in hospital inpatients. BMJ. 2007;335:147-151.
http://dx.doi.org/10.1136/bmj.39247.542477.AE
10. Childs JD, Fritz JM, Flynn TW, et al. A clinical
prediction rule to identify patients with low
back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med.
2004;141:920-928.
11. Chou R, Qaseem A, Snow V, et al. Diagnosis
and treatment of low back pain: a joint clinical
practice guideline from the American College of
Physicians and the American Pain Society. Ann
Intern Med. 2007;147:478-491.
'($ Cleland J. Orthopedic Clinical Examination: An
16.
548 | july 2009 | volume 39 | number 7 | journal of orthopaedic & sports physical therapy
17.
18.
19.
(&$
('$
(($
()$
(*$
(+$
(,$
(-$
]
Evidence-Based Approach for Physical Therapists. Carlstadt, NJ: Icon Learning Systems;
2005.
Danielsen JM, Johnsen R, Kibsgaard SK, Hellevik E. Early aggressive exercise for postoperative rehabilitation after discectomy. Spine.
2000;25:1015-1020.
Deville WL, van der Windt DA, Dzaferagic
A, Bezemer PD, Bouter LM. The test of
Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine.
2000;25:1140-1147.
Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low
back pain? JAMA. 1992;268:760-765.
Filiz M, Cakmak A, Ozcan E. The effectiveness of
exercise programmes after lumbar disc surgery:
a randomized controlled study. Clin Rehabil.
2005;19:4-11.
Fink ML, Stoneman PD. Deep vein thrombosis
in an athletic military cadet. J Orthop Sports
Phys Ther. 2006;36:686-697. http://dx.doi.
org/10.2519/jospt.2006.2251
Fritz JM, Cleland JA, Childs JD. Subgrouping
patients with low back pain: evolution of a classification approach to physical therapy. J Orthop
Sports Phys Ther. 2007;37:290-302. http://
dx.doi.org/10.2519/jospt.2007.2498
Goss DL, Moore JH, Thomas DB, DeBerardino
TM. Identification of a fibular fracture in an
intercollegiate football player in a physical
therapy setting. J Orthop Sports Phys Ther.
2004;34:182-186. http://dx.doi.org/10.2519/
jospt.2004.1310
Gray H. Anatomy of the Human Body. 20th ed.
New York, NY: Bartleby; 2000.
Greathouse DG, Schreck RC, Benson CJ. The
United States Army physical therapy experience:
evaluation and treatment of patients with neuromusculoskeletal disorders. J Orthop Sports
Phys Ther. 1994;19:261-266.
Greene G. ‘Red Flags’: essential factors in
recognizing serious spinal pathology. Man Ther.
2001;6:253-255. http://dx.doi.org/10.1054/
math.2001.0423
Haswell K, Gilmour J, Moore B. Clinical decision rules for identification of low back pain
patients with neurologic involvement in primary
care. Spine. 2008;33:68-73. http://dx.doi.
org/10.1097/BRS.0b013e31815e3949
Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction
rule for determining which patients with low
back pain will respond to a stabilization exercise
program. Arch Phys Med Rehabil. 2005;86:17531762.
Jensen MP, Turner JA, Romano JM. What is
the maximum number of levels needed in pain
intensity measurement? Pain. 1994;58:387-392.
Kendall FP. Muscles: Testing and Function.
4th ed. Baltimore, MD: Lippincott, Williams
&Wilkins; 1993.
Kinkade S. Evaluation and treatment of acute
low back pain. Am Fam Physician. 2007;75:11811188.
(.$ Kjellby-Wendt G, Carlsson SG, Styf J. Results
of early active rehabilitation 5-7 years after
surgical treatment for lumbar disc herniation. J
Spinal Disord Tech. 2002;15:404-409.
(/$ Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ.
2007;334:1313-1317. http://dx.doi.org/10.1136/
bmj.39223.428495.BE
30. Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ.
2006;332:1430-1434. http://dx.doi.org/10.1136/
bmj.332.7555.1430
31. Lauder TD, Dillingham TR, Andary M, et al.
Effect of history and exam in predicting electrodiagnostic outcome among patients with
suspected lumbosacral radiculopathy. Am J
Phys Med Rehabil. 2000;79:60-68; quiz 75-66.
)($ Long A, Donelson R, Fung T. Does it matter
which exercise? A randomized control trial of exercise for low back pain. Spine. 2004;29:25932602.
33. Luo X, Pietrobon R, Sun SX, Liu GG, Hey
L. Estimates and patterns of direct health
care expenditures among individuals with
back pain in the United States. Spine.
2004;29:79-86. http://dx.doi.org/10.1097/01.
BRS.0000105527.13866.0F
34. Maitland GD. Vertebral Manipulation. 6th ed.
Oxford, UK: Butterworth-Heinemann; 2002.
35. McKenzie R, May S. The Lumbar Spine: Mechanical Diagnosis and Therapy. 2nd ed. Waikanae,
New Zealand: Spinal Publication, Ltd; 2003.
36. Moore JH, Goss DL, Baxter RE, et al. Clinical
diagnostic accuracy and magnetic resonance
37.
38.
39.
40.
41.
*($
43.
44.
imaging of patients referred by physical therapists, orthopaedic surgeons, and nonorthopaedic providers. J Orthop Sports Phys Ther.
2005;35:67-71. http://dx.doi.org/10.2519/
jospt.2005.1344
Ostelo RW, de Vet HC, Waddell G, Kerckhoffs
MR, Leffers P, van Tulder MW. Rehabilitation
after lumbar disc surgery. Cochrane Database
Syst Rev. 2002;CD003007. http://dx.doi.
org/10.1002/14651858.CD003007
Pendergrass TL, Moore JH. Saphenous neuropathy following medial knee trauma. J Orthop
Sports Phys Ther. 2004;34:328-334. http://
dx.doi.org/10.2519/jospt.2004.1269
Rhee JM, Schaufele M, Abdu WA. Radiculopathy
and the herniated lumbar disc. Controversies
regarding pathophysiology and management. J
Bone Joint Surg Am. 2006;88:2070-2080.
Rubin DI. Epidemiology and risk factors for
spine pain. Neurol Clin. 2007;25:353-371.
Saal J. Post-operative rehabilitation and training. In: Mooney V, Gatchel R, Mayer T, eds. Contemporary Conservative Care for Painful Spinal
Disorders. Philadelphia, PA: Lea & Febiger;
1991:318-327.
Scrimshaw SV, Maher CG. Randomized controlled trial of neural mobilization after spinal
surgery. Spine. 2001;26:2647-2652.
Shapiro S. Cauda equina syndrome secondary to lumbar disc herniation. Neurosurgery.
1993;32:743-746; discussion 746-747.
Shapiro S. Medical realities of cauda equina
syndrome secondary to lumbar disc herniation.
Spine. 2000;25:348-351; discussion 352.
45. Small SA, Perron AD, Brady WJ. Orthopedic pitfalls: cauda equina syndrome. Am J Emerg Med.
2005;23:159-163.
46. Springer BA, Arciero RA, Tenuta JJ, Taylor DC.
A prospective study of modified Ottawa ankle
rules in a military population. Am J Sports Med.
2000;28:864-868.
47. Springer BA, Gill NW, Freedman BA, Ross AE,
Javernick MA, Murphy MP. Acetabular labral
tears: diagnostic accuracy of clinical examination by a physical therapist, orthopaedic surgeon, and orthopaedic resident [abstract]. J
Orthop Sports Phys Ther. 2006;36:A82.
48. Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin. 2007;25:387-405. http://dx.doi.
org/10.1016/j.ncl.2007.01.008
49. Vath SA, Owens BD, Stoneman P. Insidious onset
of shoulder girdle weakness. J Orthop Sports
Phys Ther. 2007;37:140-147.
50. Vroomen PC, de Krom MC, Wilmink JT, Kester
AD, Knottnerus JA. Diagnostic value of history
and physical examination in patients suspected
of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry. 2002;72:630-634.
51. Weishaar MD, McMillian DM, Moore JH. Identification and management of 2 femoral shaft
stress injuries. J Orthop Sports Phys Ther.
2005;35:665-673. http://dx.doi.org/10.2519/
jospt.2005.2180t
@
CEH;?D<EHC7J?ED
WWW.JOSPT.ORG
CHECK Your References With the JOSPT Reference Library
JOSPT has created an EndNote reference library for authors to use in
conjunction with PubMed/Medline when assembling their manuscript
references. This addition to “INFORMATION FOR AUTHORS” on the JOSPT
website under “Complete Author Instructions” offers a compliation of all
article reference sections published in the Journal from 2006 to date as
well as complete references for all articles published by JOSPT since
1979—a total of nearly 10,000 unique references. Each reference has been
checked for accuracy.
This resource is updated monthly with each new issue of the Journal. The
JOSPT Reference Library can be found at http://www.jospt.org/aboutus/
for_authors.asp.
journal of orthopaedic & sports physical therapy | volume 39 | number 7 | july 2009 | 549