Human Anatomy & Physiology
advertisement

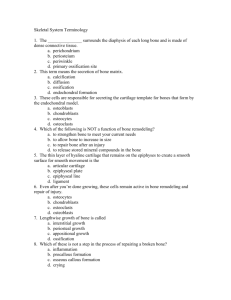
Anatomy & Physiology I Dr. L. Bacha Chapter Outline (Marieb & Hoehn 2013) SKELETAL CARTILAGES ◦ does cartilage contain blood vessels and nerves? ◦ name the layer of dense irregular connective tissue that surrounds cartilage: - indicate the two important functions of the perichondrium: ◦ name and read about (to refresh your memory) the three types of cartilages: CLASSIFICATION OF BONES - how many named bones form the human skeleton? - examine Fig. 6.1 for an overview of the skeleton Axial Skeleton it consists of bones that lie around the longitudinal central axis of the body it includes the bones of what structures? Appendicular Skeleton it consists of bones of what structures? - what do “girdles” attach? Chapt. 6 Bones and Skeletal Tissues Page 1 List and briefly describe the 4 types of bones (based on shape) and give examples of each type: 1. 2. - what are sesamoid bones and what are their functions? 3. 4. FUNCTIONS OF BONES List (and read about!) the 7 important functions of bones: Chapt. 6 Bones and Skeletal Tissues Page 2 BONE STRUCTURE - are bones organs?! Gross Anatomy Bone Textures: Compact And Spongy Bone there are two types of bone tissue: compact bone tissue and spongy bone tissue ◦ describe compact bone tissue: ◦ describe spongy bone tissue: - what are the open spaces between trabeculae filled with in living bones? Structure of Short, Irregular, and Flat Bones ◦ what do these bones all consist of? - what is the spongy bone called in flat bones? Structure of a Typical Long Bone As you study the parts of a long bone, locate the parts in Fig. 6.4 Diaphysis the long, tubular shaft of the bone - constructed of a relatively thick collar of what? name the central cavity of the diaphysis: - in adults, what does the medullary cavity contain? Epiphyses the ends of the bone; usually broader than the diaphysis what forms the exterior and interior of the epiphysis? what covers the joint surface of each epiphysis? where is the epiphyseal line found? - what is the epiphyseal line a remnant of? Chapt. 6 Bones and Skeletal Tissues Page 3 what is the epiphyseal plate? - what is the flared portion of the bone where the diaphysis and epiphysis meet called? Membranes periosteum: - describe the appearance and location of the periosteum: - name and describe the two layers of the periosteum: - is the periosteum richly supplied with nerve fibers and blood vessels? - what is the significance of the nutrient foramen? - the periosteum provides anchoring points for what? endosteum: - a layer of simple squamous cells and connective tissue that covers what? - does the endosteum contain osteogenic cells? Location of Hematopoietic Tissue in Bones Where is red marrow, which is hematopoietic tissue, typically found? - these cavities are often called what? Chapt. 6 Bones and Skeletal Tissues Page 4 BONE MARKINGS Bone markings serve as what? In most cases, bone projections indicate what? depressions and openings in bones usually serve to allow what? The following bone markings are important! Be able to describe/define each (see p. 180 Table 6.1): Projections That Are Sites of Muscle And Ligament Attachment: tuberosity crest trochanter line tubercle epicondyle spine process - Projections That Help Form Joints: head facet condyle ramus - Chapt. 6 Bones and Skeletal Tissues Page 5 Depressions and Openings: groove fissure – foramen (plural = foramina) notch meatus (canal) sinus fossa - Others (not in your textbook): fovea - little pit body - the main part neck – constriction between the head and body margin or border - edge angle – bend Microscopic Anatomy of Bone Cells of Bone Tissue (see Fig. 6.5) Osteogenic Cells ◦ what are osteogenic cells also called? ◦ osteogenic cells are mitotically active cells found where? ◦ osteogenic cells differentiate into what cells? Osteoblasts ◦ osteoblasts are located on the surface of bone matrix ◦ when they are active, they are cuboidal in shape; when they are inactive, they appear flattened ◦ they synthesize the organic components (including collagen fibers) of bone matrix, which initially does not yet have minerals deposited in it; unmineralized bone matrix is called what? ◦ osteoblasts initiate calcification (mineralization) of bone matrix ◦ when osteoblasts become completely surrounded by the bone matrix, they become what type of cells? Chapt. 6 Bones and Skeletal Tissues Page 6 Osteocytes ◦ ◦ ◦ ◦ are mature cells found embedded in bone matrix they arise from osteoblasts that have become surrounded by bone matrix the cell body of each osteocyte occupies a space called a lacuna (pleural = lacunae) osteocytes have numerous cytoplasmic processes that occupy tiny channels in the bone matrix called canaliculi (singular = canaliculus) ◦ osteocytes monitor and maintain what? - what happens to the surrounding bone matrix if osteocytes die? Bone Lining Cells ◦ found on bone surfaces where bone remodeling is not going on - what are they called on the external bone surface? - what are they called on the internal bone surface? Osteoclasts ◦ are very large, multinucleated cells that are on the surface of bone matrix ◦ are derived from the fusion of monocytes ◦ are responsible for resorption of bone matrix; i.e., they release enzymes and acids that dissolve bone matrix Compact Bone Tissue (Figs. 6.6 and 6.7 ) Osteon (Haversian System) ◦ what is the structural unit of compact bone tissue called? - describe an osteon: ◦ each osteon (Haversian system) consists of the following components: 1. concentric lamellae = ring-like layers of bone matrix ∙ how do the collagen fibers of a single lamella run? ∙ describe the collagen fibers of adjacent lamellae: ∙ what is the significance of this alternating pattern? 2. a central canal (Haversian canal) ∙ what do the central canals contain? Chapt. 6 Bones and Skeletal Tissues Page 7 observe Fig. 6.7 to answer the following: ∙ are central canals transverse channels or longitudinal channels through compact bone? ∙ what canals do the central canals connect with? 3. osteocytes ∙ the cell body of each osteocyte is situated in a space called lacuna between the concentric lamellae ∙ cytoplasmic processes extending from the cell body of each osteocyte occupy tiny channels called canaliculi;∙ canaliculi and lacunae contain extracellular fluid ∙ what do the canaliculi connect? - the canaliculi tie all the osteocytes in an osteon together; what does this allow and permit? ◦ perforating canals (Volkmann's canals) ∙ do perforating canals run transversely or longitudinally through compact bone tissue? ∙ like the central canals, the perforating canals contain blood vessels and nerves ∙ what do the perforating canals connect? ◦ interstitial lamellae ∙what are interstitial lamellae and what do they lie between? ∙ they fill the gaps between what? Spongy Bone Tissue ◦ it consists of trabeculae with large spaces between them (review the definition of trabeculae on p.177) ◦ how are the trabeculae aligned and what does this help? Chapt. 6 Bones and Skeletal Tissues Page 8 ◦ what do the trabeculae contain? ◦ does spongy bone tissue contain osteons? ◦ how do nutrients reach the osteocytes of spongy bone? Chemical Composition of Bone bone is a type of connective tissue with cells and a hard extracellular matrix ( “bone matrix”) bone has organic components and inorganic components: ORGANIC COMPONENTS organic components of bone include what? - define osteoid: - i.e., osteoid is unmineralized bone matrix ∙ what does osteoid include? ∙ what cells make and secrete the components of osteoid? these organic substances, particularly collagen, contribute to what? INORGANIC COMPONENTS consist of hydroxyapatite crystals (hydroxyapatites) of mineral salts, mainly calcium and phosphate - what percent of bone matrix is formed by hydroxyapatites? ∙ these are needle-like crystals with the following chemical formula: Ca10 (PO4)6 (OH) 2 ∙ they are deposited in and around what part of the extracellular matrix? the crystals of mineral salts account for what characteristic of bone? BONE DEVELOPMENT define ossification (osteogenesis): ossification leads to formation of the bony skeleton in the embryo, bone growth, and bone remodeling and repair Chapt. 6 Bones and Skeletal Tissues Page 9 Formation of the Bony Skeleton - bone tissue begins to develop at about what week in a human embryo? - when a bone develops from a fibrous membrane, what is the process called? - what is development of bone that involves the replacement of hyaline cartilage called? Intramembranous Ossification (jump to page 185) results in the formation of what bones of the skeleton? Study the steps of intramembranous ossification in Fig. 6.9 on page 185. Write below the titles of each numbered step (shown in bold blue print): 1. in the ossification center (site where bone will form) mesenchyme cells differentiate into what cells? 2. what do osteoblasts secrete? - when does the osteoid calcify? remember, osteoid is unmineralized bone matrix (organic bone matrix) produced by osteoblasts that subsequently becomes mineralized (calcified) when osteoblasts become trapped in bone matrix, what do they become? 3. osteoid is laid down randomly between embryonic blood vessels; the network of trabeculae that results is called what? vascularized mesenchyme condenses on the external face of the woven bone and becomes what? 4. trabeculae of the woven bone just deep to the periosteum thicken and become replaced with mature lamellar bone, forming what? what persists internally? vascular tissue becomes what? Chapt. 6 Bones and Skeletal Tissues Page 10 Endochondral Ossification (back to page 183) in summary, bone tissue replaces a hyaline cartilage model; the cartilage acts as a framework for deposition of bone matrix bones of the base of the skull, bones of the extremities, the vertebrae, and most of the remaining skeleton develop in this way; long bones grow in length by endochondral ossification NOTE: This following information is my summary of the information on endochondral ossification on pages 183 to 186 (which you should still read !) e.g., endochondral ossification of a long bone of an extremity: 1. Mesenchyme cells produce a hyaline cartilage model in which bone will form. (Thus, much of what will become the bony skeleton begins as a miniature model made up of hyaline cartilages.) (Cartilage begins to form at the end of the 4th week of development. Endochondral ossification begins at the 8th week of development.) 2. a. The diaphysis is the primary center of ossification in long bones. b. In the primary center of ossification, the chondrocytes hypertrophy (enlarge). c. The cartilage matrix between the hypertrophied chondrocytes becomes mineralized (calcified) with calcium carbonate and is called calcified cartilage. The hypertrophied chondrocytes die, leaving enlarged lacunae separated by thin pieces of calcified cartilage matrix. 2a. 2b. 2c. 3. Blood vessels from the developing periosteum grow into the primary center of ossification, introducing osteoblasts, osteoclasts, cells of bone marrow, etc., to the area. The osteoblasts produce bone matrix on the surface of the pieces of calcified cartilage matrix, forming trabeculae of spongy bone tissue. Thus, calcified cartilage matrix acts as a framework for deposition of bone matrix! 4. As bone development proceeds and the hyaline cartilage of the primary center of ossification in the diaphysis continues to grow and undergo the changes described above (hypertrophy, calcification, and replacement by bone tissue). Meanwhile, osteoclasts resorb bone tissue in the diaphysis to form the medullary cavity in which bone marrow forms. Chapt. 6 Bones and Skeletal Tissues Page 11 The overall length of the diaphysis increases as the hyaline cartilage model continues to grow and be replaced by bone tissue at the ends of the diaphysis. Here the chondrocytes are organized into longitudinal columns and undergo changes that are organized into zones: (see Fig. 6.10) zone of resting cartilage: nearest the epiphysis zone of proliferation: chondrocytes divide and form columns resembling stacks of coins zone of hypertrophy: chondrocytes from the zone of proliferating cartilage mature and enlarge zone of calcified cartilage: a very narrow zone and consists of calcified cartilage matrix zone of ossification: osteoblasts deposit bone matrix onto the remnants of calcified cartilage matrix As new chondrocytes form in the zone of proliferation, and as they enlarge in the zone of hypertrophy, the overall length of the diaphysis increases. 5. In long bones, additional sites of ossification called secondary centers of ossification appear in the epiphyses later in development. The hyaline cartilage in the epiphyses undergoes hypertrophy, calcification, etc., and is replaced by bone tissue. Chapt. 6 Bones and Skeletal Tissues Page 12 6. With the diaphysis and epiphyses now replaced by bone tissue, hyaline cartilage remain, on the articular surfaces of the developing bone and in the epiphyseal plates. The epiphyseal plate is hyaline cartilage situated in the metaphysis between the epiphysis and diaphysis. It is organized into the zones described previously, but in a narrower, disk-like region. As new chondrocytes form in the zone of proliferation, and as they enlarge in the zone of hypertrophy, the overall length of the diaphysis increases. The thickness of the epiphyseal plate does not increase because the rate of cartilage growth on the epiphyseal side is equal to the rate at which the cartilage is replaced by bone tissue on the opposite side. Postnatal Bone Growth (back to the textbook; page 185) during infancy and youth, long bones lengthen entirely by growth of the cartilage of the epiphyseal plate and its replacement by bone tissue. Growth in Length of Long Bones Read the text on page 185 under the heading of “Growth in Length of Long Bones”, then see Fig. 6.10, which is a magnified view of a portion of the epiphyseal plate. Note that the cartilage of the epiphyseal plate is organized into zones, as described above. During growth, how does the epiphyseal plate maintain a constant thickness (yet the bone on the diaphyseal side increases in length)? So, as long as the epiphyseal cartilage continues to grow (by cartilage cells undergoing cell division) at its epiphyseal surface, bone tissue will continue to replace the cartilage on the shaft side of the epiphyseal plate. longitudinal growth is accompanied by almost continuous what? - see Fig. 6.11 Chapt. 6 Bones and Skeletal Tissues Page 13 bone remodeling involves what? as adolescence ends, the cartilage cells of the epiphyseal plate stop dividing and the epiphyseal plates are entirely replaced by what? when does longitudinal bone growth end? - what is this process called? - when does epiphyseal plate closure happen in males and females? the location of closure of the epiphyseal plate is often evident as the epiphyseal line Growth in Width (Thickness) growing bones increase in thickness or, in the case of long bones, diameter, by what? define appositional growth (from the glossary in the back of the book!): (it is a type of intramembranous ossification; in this case the periosteum acts as the membrane) describe the role of osteoblasts and osteoclasts during growth in width of a bone: Hormonal Regulation of Bone Growth list hormones that control the growth of bones that occur until young adulthood: BONE HOMEOSTASIS: REMODELING AND REPAIR bone continuously replaces itself throughout life (just like skin) Bone Remodeling in the adult skeleton, name the two processes that constitute bone remodeling: Chapt. 6 Bones and Skeletal Tissues Page 14 what cells form remodeling units? - with help from stress-sensing osteocytes in healthy young adults, does total bone mass remain constant? - are the rates of bone deposit and bone resorption essentially equal? Bone deposit what cells deposit unmineralized bone matrix called osteoid? - osteoid then calcifies (mineralizes) - is the precise trigger for calcification well understood? - local concentrations of what ions are critical for calcification to occur? Bone resorption is accomplished by what cells? - osteoclasts release lysosomal enzymes that do what? - osteoclasts also release hydrogen ions, creating an acid environment that does what to the calcium salts? - osteoclasts may phagocytize what? Control of remodeling remodeling is regulated by what? - list the two control loops that regulate continuous remodeling: - give specific examples of what ionic calcium is necessary for in the body? - what percent of the body’s calcium is present as bone minerals? - what is the normal range of Ca+2 in the blood? Chapt. 6 Bones and Skeletal Tissues Page 15 1. Hormonal Controls the hormonal controls (of bone remodeling) primarily involve what hormone? what gland produces parathyroid hormone? what is the other hormone produced by the thyroid gland that is involved? parathyroid hormone is released when? what does the increased parathyroid hormone level stimulate? 2. Response to Mechanical Stress what does Wolff’s law say? a bone’s anatomy reflects what? read about observations explained by Wolff’s law how mechanical forces communicate with the cells responsible for remodeling: - deforming a bone produces what? - the electrical current stimulates osteoblasts to deposit osteoid so, hormonal controls determine what? mechanical stress determines what? Bone Repair define fracture: we will define these two terms in class: traumatic fracture = pathologic (spontaneous) fracture = Chapt. 6 Bones and Skeletal Tissues Page 16 distinguish between the following types of fractures: nondisplaced displaced complete incomplete open (compound) closed (simple) - name the 4 major steps involved in the repair of a simple bone fracture, read about them, and observe Fig. 6.15: HOMEOSTATIC IMBALANCES OF BONE Osteomalacia and Rickets define osteomalacia: define rickets: what are osteomalacia and rickets caused by? Osteoporosis what does osteoporosis refer to? Chapt. 6 Bones and Skeletal Tissues The End! Page 17