Cranial Nerve/Oral Mech Exam: What Every SLP Needs to Know
advertisement
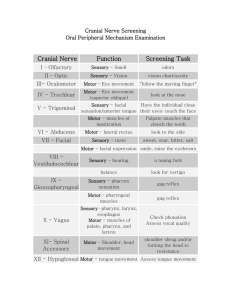
Cranial Nerve/Oral Mech Exam: What Every SLP Needs to Know Kelly Dailey Hall, Ph.D. CCC/SLP Pediatric Speech & Language Services, Inc. University of North Carolina Greensboro kdhall2@uncg.edu What’s in a name? Oral Mechanism Exam Oral Motor Exam Oral Peripheral Exam Speech Mechanism exam Why We Do The Things We Do SLPs should ALWAYS look inside the mouth Stroke Language Delay Articulation Disorder Feeding/swallow We’ve studied the head/neck indepth (not the whole body) Longer look Look for more things Myasthenia Gravis Undiagnosed cleft Tumor Shortened frenulum VPI Medical conditions Thyroid disease Purpose of the Oral Mechanism Examination • Determine the structural and functional adequacy of the oral mechanism for speech. • Should be routine part of every speech/language evaluation, regardless of client’s particular communication disorder findings may help shape theory of etiology, diagnosis and prognosis for change, direction for treatment. May save someone’s life Tools gloves Tongue depressor Pen light Small hand held mirror Stop watch Other tools: Cotton gauze, Sucker Make a game (where’s the mouse) What stuctures do we look at? Teeth Tongue Jaw (mandible) Tonsils Hard/soft palate cheeks Face (symmetry) Neck Ears Nose Skin Any facial deviancies that my contribute to speech/hearing/swallow ing disorders What CNs do we screen? CN V (trigeminal) CN VII (facial) CN VIII (acoustic) CN IX (glossopharyngeal) CN X (vagus CN XI (spinal accessory) CN XII (hypoglossal) You can have disorders of structure/function or both Or have none When structure or function is impaired, we refer the pt back to the physician Speech therapy continues or is put on hold Team approach SLP often forgo them because they don’t think it’s necessary It is! Fast, easy to do NO eval is complete without one You are the ONLY one that really takes time to look inside/outside the mouth and the CNS system Cranial Nerve Review CN V Trigeminal Sensory/Motor – sensory to the face and motor to the muscles of mastication Sensory nerve branches Ophthalmic: forehead, eyes, nose Maxillary: upper lip, maxilla, maxillary sinus, upper teeth, cheeks, palate Mandibular: mandible, lower lip, a portion of the external ear, the first 2/3 of the tongue, the bottom set of teeth CN VII Facial (Finn) Sensory/motor – face Muscles of facial expression Taste sensation from anterior 2/3 of tongue Bell’s Palsy http://www.webmd.com/hw/health_guide_atoz/zm2734.asp Effects on Communication Facial muscle weakness Facial expressions Production of speech -Bilabials -Labiodental -Vowels Stapedius Muscle -Hyperacusis CN VIII Acoustic Sensory – hearing/balance CN IX Glossopharyngeal Sensory: taste and general sensation to the posterior 1/3 of tongue Motor: laryngeal elevation, pharyngeal constriction Communication/swallowing Elevates and dilates pharynx Regulation of saliva Saliva: Underproduction Overproduction Saliva necessary CN X Vagus Sensory/Motor – larynx 3 branches Pharyngeal Superior recurrent CN XI Spinal Accessory Motor – larynx/pharynx, Sternocleidomastoid shrugging CN XII Hypoglossal Motor and Sensory Innervates all intrinsic and extrinsic muscles Receives taste and tactile info Facilitates speech Allows for precise articulation CN Screening CN V Trigeminal Sensory: swipe quadrants Motor: clench teeth-palpate masseter, temporalis Open-close mouth: symmetry, ROM Mandible side-side Open mouth-don’t let me shut (strength) CN VII Facial Sensory: taste Motor: Observe face at rest (symmetry) look at ceiling-symmetry of wrinkles; don’t let me open your eyes Smile-symmetry Puff cheeks-don’t let me push in Frogs neck CN VIII Acoustic Observe balance during walking Brush fingers IX/X glossopharyngeal/vagus Motor Dry swallow /a/ prolonged-look for symmetry of pharyngeal mvt Deviated uvula? Voice quality Gag—no way! XI spinal accessory Motor Shrug shoulders against resistance Look left/right-palpate SCM XII hypoglossal Motor Tongue protruded (no lip assistance) Side-to-side Lateral resistance to tongue depressor Don’t let me push it in Tip elevation without jaw assistance Back elevation (ka ka or ga ga) Look for fasciculations, tremors Look for migration Apraxia "apraxia of speech is an articulation disorder that results from impairment due to brain damage, of the capacity to order the positioning of speech musculature and the sequencing of muscle movements for volitional production of phonemes and sequences of phonemes; but it is not accompanied by significant weakness, slowness, or incoordination of these same muscles in reflex and automatic acts (Chapey, 1986, p.422) 1. Inconsistent Errors: Repetitions, Substitutions, Simplifications, Distortions Additions, Deletions 2. Articulatory Breakdowns Increase With: Word Complexity, Word Length 3. Well rehearsed utterances better than spontaneous utterances 4. Struggling behaviors to self correct articulatory errors Dysarthria Term for a collection of motor speech disorders due to impairment originating in the central or peripheral nervous system. Respiration, articulation, phonation, resonation, and/or prosody may be affected Ataxic Dysarthria Damage of bilateral or unilateral cerebellar hemispheric lesions or damage to the cerebellar outflow tracts produce discoordination and dysmetria in the oral speech musculature as well as the muscles of the axial and appendicular skeleton. Speech Characteristics: Consonant imprecision, omissions, and distortions particularly at word, phrase, and sentence endings. Speech has an intoxicated quality. Unilateral Upper Motor Neuron (UUMN) Dysarthria Damage resulting from a focal, unilateral corticobulbar tract lesion. Speech Characteristics: Imprecise consonants, decreased loudness, limited pitch range, low pitch, short phrases and slow rate. Spastic Dysarthria Damage resulting from bilateral corticibulbar tract lesion, bihemispheric disease along with involvement of periventricular white matter and internal capsules. Speech Characteristics: Imprecise articulation, slow diadochokinesis, variable hypernasality, nasal emissions, strainstrangled phonation, frequent lapses of laughing or crying, decreased rate, and reduced breath support Hypokinetic Dysarthria Damage caused by unilateral or bilateral lesions of the substantia nigra or its projections. Characteristic of Parkinson's Disease Speech Characteristics: Decreased loudness, reduced pitch inflections, and breathy-harsh voice. Variable articulatory precision and rapid diadochokinesis, decreased loudness, silent intervals or inappropriate pausing followed by short rushes of rapid speech. Hyperkinetic Dysarathria Results from a lesion in the basal ganglia or biochemical imbalance. Speech Characteristics: Imprecise articulation, irregular diadochokinesis, inappropriate prolongations of sounds, inappropriate silences between and among words, variable or fast rate, vocal harshness, reduced pitch and loudness variations, phonatory arrest, and tremor. When there is velopharyngeal and Flaccid Dysarthria Damage caused by neuropathy (e.g., progressive bulbar palsy, infarct, trauma), myoneuropathy (e.g., myastenia gravis, Eaton-Lambert syndrome), or myopathy (e.g., myotonis dystrophy, polymyositis). Speech Characteristics: Severity and extent of speech involvement depends on the number of and degree to which the cranial nerves/ muscles and spinal nerves/muscles are involved. Bilateral IX and X nerve lesions - continuous hypernasality and nasal emission due to velopharyngeal involvement; hoarse, gurgly voice, weak or absent cough, dysphonia, decreased loudness and unstable pitch, short phrases, reduced stress, decreased respiratory support for speech, inspiratory and/or expiratory stridor. V, VII, and XII nerve lesions - imprecise, slow-labored articulation, reduced diadochokinesis. Mixed Amyotrophic Lateral Schlerosis flaccid-spastic Multiple Sclerosis Wilson's Disease ataxic-spastic and hypokinetic Progressive Supranuclear Palsy spastichypokinetic-ataxic and flaccid spastic-ataxic