Gas Exchange
advertisement

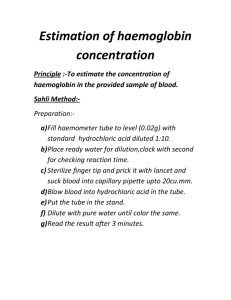
Gas Exchange Week 4 PDF created with pdfFactory Pro trial version www.pdffactory.com Daltons Law PDF created with pdfFactory Pro trial version www.pdffactory.com PDF created with pdfFactory Pro trial version www.pdffactory.com PDF created with pdfFactory Pro trial version www.pdffactory.com The partial pressures of the 4 gases add up to 760mm Hg. Dalton’s Law; in a mixture if gases, the total pressure equals the sum of the pa partial pressures exerted by each gas. PDF created with pdfFactory Pro trial version www.pdffactory.com Important Point • Gases in our bodies are dissolved in fluids, such as blood plasma. • According to Henry’s law, – gases dissolve in liquids in proportion to their partial pressures, depending also on their solubilities in the specific fluids and on the temperature. PDF created with pdfFactory Pro trial version www.pdffactory.com The Site of Gas Exchange • External Respiration • • CO2 diffuses from pulmonary capillaries into alveoli O2 Diffuses from alveoli into pulmonary capillaries •Internal respiration •O2 diffuses from systemic capillaries into cells •CO2 diffuses from cells into systemic capillaries PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Influencing External Respiration • Efficient external respiration depends on 3 main factors 1) Surface area and structure of the respiratory membrane 2) Partial Pressure gradients 3) Matching alveolar airflow to pulmonary capillary blood flow. PDF created with pdfFactory Pro trial version www.pdffactory.com Important Point • Partial pressure gradients affect gas exchange between the alveoli and pulmonary capillaries. PDF created with pdfFactory Pro trial version www.pdffactory.com External respiration: Partial Pressures • The Partial pressures of gases in the alveoli differ from those in the atmosphere. 1) Humidification of inhaled air 2) Gas exchange between alveoli and pulmonary capillaries 3) Mixing of new and old air PDF created with pdfFactory Pro trial version www.pdffactory.com Oxygen Loading • Oxygen diffuses along its partial pressure gradient, from the alveolus into the blood, until equilibrium is reached • Equilibrium is reached within the first third of the capillary. PDF created with pdfFactory Pro trial version www.pdffactory.com Oxygen Loading PDF created with pdfFactory Pro trial version www.pdffactory.com Carbon Dioxide Uploading • Carbon dioxide diffuses along its partial pressure gradient, from the blood into the alveolus, until equilibrium is reached • Equilibrium is reached within the first 4 4/10’s of the capillary PDF created with pdfFactory Pro trial version www.pdffactory.com This Occurs Simultaneously •Carbon dioxide is very soluble in blood, allowing many molecules to diffuse along this small pressure gradient. •Oxygen is less soluble, requiring a larger concentration gradient. PDF created with pdfFactory Pro trial version www.pdffactory.com Other Factors Affecting External Respiration 1) Matching alveolar airflow to pulmonary capillary blood flow. 2) Watch the following clip. 3) This is Know as the Ventilation-Perfusion Coupling PDF created with pdfFactory Pro trial version www.pdffactory.com Internal Respiration • Internal Respiration • O2 diffuses from systemic capillaries into cells • CO2 diffuses from cells into systemic capillaries. PDF created with pdfFactory Pro trial version www.pdffactory.com Internal Respiration Depends on: 1) Available surface area, which varies in different tissues. 2) Partial Pressure gradients 3) Rate of blood flow varies (e.g. metabolic rate of tissue) PDF created with pdfFactory Pro trial version www.pdffactory.com Internal Respiration CO2 and O2 Exchange PDF created with pdfFactory Pro trial version www.pdffactory.com Summary PDF created with pdfFactory Pro trial version www.pdffactory.com AS Level Sport and Physical Education Please complete the questions on a separate sheet of paper. Respiratory Exam Questions 1) Describe the anatomical structures involved in pulmonary ventilation. (5 marks) 2) Identify the muscles associated with breathing and their function in pulmonary ventilation a) at rest (3 marks) b) during exercise (3 marks) 3) What are the partial pressures of oxygen and carbon dioxide in inspired air, alveolar air and arterial and mixed venous blood? (4 marks) 4) In what forms are oxygen and carbon dioxide transported in the blood? (3 marks) PDF created with pdfFactory Pro trial version www.pdffactory.com Introduction to the Respiratory System Review of the Structures Involved in Breathing Week 3 PDF created with pdfFactory Pro trial version www.pdffactory.com Lets start by reviewing the anatomical structures of the respiratory system Can anyone name any of the structures involved in breathing? Now we’ve got a list can you put them in order? PDF created with pdfFactory Pro trial version www.pdffactory.com Overview of the Structures of the Respiratory System PDF created with pdfFactory Pro trial version www.pdffactory.com The air continues into many branching airways known as the bronchial tree The trachea and bronchi have supporting cartilage to keep the airways open Bronchiole walls contain more smooth muscle. The air is moistened, warmed and filtered as it flows through these passageways The airways from the nasal cavity through the terminal bronchioles are called the conducting zone PDF created with pdfFactory Pro trial version www.pdffactory.com The air then reaches the respiratory zone The respiratory zone The respiratory zone contains alveoli, tiny thin walled sacs where gas exchanges occurs. Terminal bronchi Alveoli Lets now look at the actual site of diffusion, the respiratory membrane PDF created with pdfFactory Pro trial version www.pdffactory.com The structure of the respiratory membrane nIs composed of. The alveolar wall, t The capillary wall, and, t Their basement membranes. t nIt is very thin, measuring only 0.5 to 4.0 Цm. nThis membrane presents a barrier for gas exchange. PDF created with pdfFactory Pro trial version www.pdffactory.com Summary • The respiratory system consists of the nose, pharynx, larynx, trachea, bronchi and lungs. • The lungs contain the bronchial tree, the branching airways from the primary bronchi through the terminal bronchioles. • The respiratory zone of the lungs is the region containing alveoli, tiny thin-walled sacs where gas exchange occurs. • Oxygen and carbon dioxide diffuse between the alveoli and the pulmonary capillaries across the very thin respiratory membrane. PDF created with pdfFactory Pro trial version www.pdffactory.com Pulmonary Ventilation Week 3 PDF created with pdfFactory Pro trial version www.pdffactory.com Pulmonary Ventilation Pulmonary ventilation, or breathing, is the exchange of air between the atmosphere and the lungs. As air moves into and out of the lungs, it travels from regions of high pressure to regions of low pressure. PDF created with pdfFactory Pro trial version www.pdffactory.com Boyle’s Law – the relationship between pressure and volume In this smaller larger volume, sphere the the gas molecules molecules strike the walls strike more the wall frequently, lessmolecules thus Pressure is caused by gas frequently, increasing pressure. thus exerting less striking the walls of a container. The pressure. pressure is related to the volume of the container Boyle’s Law: The pressure of a gas is inversely proportional to the volume of its container. Increasing volume decreases pressure, decreasing volume increases pressure PDF created with pdfFactory Pro trial version www.pdffactory.com Quiet Breathing During quiet inspiration, the diaphragm and the external intercostal muscles contract. PDF created with pdfFactory Pro trial version www.pdffactory.com Inspiration Increasing the volume What does decreases the pressure this the do??? within thoracic cavity and the lungs. Quiet Breathing Expiration Quiet expiration is a passive process, in which the diaphragm and the external intercostals muscles relax,and the elastic lungs and thoracic wall recoil inward. PDF created with pdfFactory Pro trial version www.pdffactory.com This decreases the volume and therefore increases the pressure in the thoracic cavity. Deep or Forced Breathing Deep breathing uses forceful contractions of the inspiratory muscles and additional accessory muscles to produce larger changes in the volume of the thoracic cavity during both inspiration and expiration. PDF created with pdfFactory Pro trial version www.pdffactory.com Intrapulmonary Pressure Changes Intrapulmonary press is the pressure within the alveoli. Between breaths, it equals atmospheric pressure (760mm Hg) Inspiration PDF created with pdfFactory Pro trial version www.pdffactory.com Expiration Lets Recap Inspiration Diaphragm and external intercostals contract Volume of thoracic cavity increases Lungs expand Intrapulmonary pressure becomes negative Air flows into the lungs PDF created with pdfFactory Pro trial version www.pdffactory.com Lets Recap Expiration Diaphragm and external intercostal muscles relax Volume of the thoracic cavity decreases Lungs recoil Intrapulmonary pressure rises above atmospheric pressure Air flows out of the lungs PDF created with pdfFactory Pro trial version www.pdffactory.com Other Factors Affecting Ventilation Resistance As air flows into the lungs, the gas molecules encounter resistance when they strike the walls of the airway. Therefore the diameter of the airways affects resistance. PDF created with pdfFactory Pro trial version www.pdffactory.com Lung Compliance The ease which the lungs expand is called lung compliance. Summary • Muscle activity causes changes in the volume of the thoracic cavity during breathing. • Changing the thoracic cavity volume causes intrapulmonary changes, which allow air to move from high pressure to low pressure regions. • Lung Compliance and Resistance affect ventilation. PDF created with pdfFactory Pro trial version www.pdffactory.com Who wants to be a millionaire To start the game click here PDF created with pdfFactory Pro trial version www.pdffactory.com Wrong !!!!! PDF created with pdfFactory Pro trial version www.pdffactory.com £100 Question • What is the respiratory system? a) b) c) d) The The The The body's body's body's body's breathing system system of nerves food-processing system blood-transporting system PDF created with pdfFactory Pro trial version www.pdffactory.com £200 Question • a) b) c) d) What is the purpose of the little hairs inside the nose? To fight disease. They serve no purpose. To keep dust out of the lungs. To tickle the nose and cause sneezes. PDF created with pdfFactory Pro trial version www.pdffactory.com £400 Question • What is another name for the windpipe? a) Lungs b) Larynx c) Trachea d) Oesophagus Audience PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty Fifty • What is another name for the windpipe? b) Larynx d) Oesophagus PDF created with pdfFactory Pro trial version www.pdffactory.com £1000 Question • a) b) c) d) What is the primary waste gas diffused out of the blood into the alveoli? Carbon dioxide Oxygen Methane Ammonia PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty / Fifty £1000 • What is the primary waste gas diffused out of the blood into the alveoli? a)Carbon dioxide b)Methane PDF created with pdfFactory Pro trial version www.pdffactory.com £2000 • a) b) c) d) What is the anatomical term for the voice box? Pharynx Bronchi Trachea Larynx PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty / Fifty £2000 • What is the anatomical term for the voice box? a)Pharynx b)Larynx PDF created with pdfFactory Pro trial version www.pdffactory.com £4000 • a) b) c) d) What are the tiny clusters of chambers for diffusion of gases in the lungs? Alveolar Sacs Lobes Pleura Bronchioles PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty / Fifty 4000 • What are the tiny clusters of chambers for diffusion of gases in the lungs? a)Alveolar Sacs b)Bronchioles PDF created with pdfFactory Pro trial version www.pdffactory.com £8000 • a) b) c) d) What is the name of the division between the middle and lower lobes of the right lung? Oblique fissure Pleura Median Sulcus Sagittial Suture PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty / Fifty 8000 • What is the name of the division between the middle and lower lobes of the right lung? a)Oblique fissure b)Pleura PDF created with pdfFactory Pro trial version www.pdffactory.com £16000 • a) b) c) d) The lungs contain how many lobes in total? 3 5 2 4 PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty / Fifty 16000 • The lungs contain how many lobes in total? a)3 b)5 PDF created with pdfFactory Pro trial version www.pdffactory.com £32000 • a) b) c) d) What encloses the lungs and protects the lobes from friction against the thorax? Diaphragm Myelin Sheath Pericardium Pleura PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty / Fifty £32000 • What encloses the lungs and protects the lobes from friction against the thorax? a)Myelin Sheath b)Pleura PDF created with pdfFactory Pro trial version www.pdffactory.com £64000 The airways from the nasal cavity through the terminal bronchioles are called the? a) conducting zone b) Respiratory zone c) respiratory membrane d) alveolar wall PDF created with pdfFactory Pro trial version www.pdffactory.com Fifty / Fifty 64000 The airways from the nasal cavity through the terminal bronchioles are called the? a) conducting zone b) Respiratory zone PDF created with pdfFactory Pro trial version www.pdffactory.com 125000 • a) b) c) d) Name the fluid found between the alveolus and pulmonary capillary. Mucus Visceral pleurae fluid Parietal Pleurae fluid Interstitial fluid PDF created with pdfFactory Pro trial version www.pdffactory.com 50 / 50 125000 • Name the fluid found between the alveolus and pulmonary capillary. a)Visceral pleurae fluid b)Interstitial fluid PDF created with pdfFactory Pro trial version www.pdffactory.com £50000 • Name the cells within the alveoli where diffusion actually occurs. a) Alveolar Macrophage b) Simple squamous epithelium c) Surfactant secreting cells d) Capillary PDF created with pdfFactory Pro trial version www.pdffactory.com 50000 50 / 50 • Name the cells within the alveoli where diffusion actually occurs. a) b) Simple squamous epithelium c) Surfactant secreting cells d) PDF created with pdfFactory Pro trial version www.pdffactory.com £1 million • a) b) c) d) Roughly what is the total service area of the alveoli? Football Pitch 4 Desk tops 2 Frying Pan 3 badminton courts PDF created with pdfFactory Pro trial version www.pdffactory.com 50 / 50 1 million • Roughly what is the total service area of the alveoli? a)2 Frying Pan b)3 badminton courts PDF created with pdfFactory Pro trial version www.pdffactory.com PDF created with pdfFactory Pro trial version www.pdffactory.com Ventilation Lung Volumes PDF created with pdfFactory Pro trial version www.pdffactory.com Did You Know? • The lung volume of the average male resting is 3 litres. • Normal inspiration increases this volume by half a litre. • Forced maximum inspiration raises the volume to 6 litres. • Forced maximum expiration lowers the volume to 1 litre. PDF created with pdfFactory Pro trial version www.pdffactory.com The Type of Lung Volume • The total lung capacity is calculated by adding the vital capacity of the lungs to the residual volume: • Lets now look at the types of lung volume. You need to know this as we will be looking at spirographs soon (which will be on your exam). PDF created with pdfFactory Pro trial version www.pdffactory.com Vital Capacity • The largest volume of air that can be expired (maximum expiration) after a maximum inspiration. • VC is made up of components we will look at them shortly. PDF created with pdfFactory Pro trial version www.pdffactory.com Residual Volume • The volume of air that remains in the lungs after forced maximum expiration. PDF created with pdfFactory Pro trial version www.pdffactory.com Types of Lung Volume • The vital capacity figure takes into account such factor as: PDF created with pdfFactory Pro trial version www.pdffactory.com Tidal Volume • The amount of air inspired and expired with each normal breath at rest or during any stated activity. PDF created with pdfFactory Pro trial version www.pdffactory.com Inspiratory Reserve Volume • The volume able to be inspired, during forced inspiration, after quiet inspiration. PDF created with pdfFactory Pro trial version www.pdffactory.com Expiratory Reserve Volume • The volume able to expired, forced expiration, after quiet expiration. PDF created with pdfFactory Pro trial version www.pdffactory.com Therefore: • Total lung capacity = vital capacity + residual volume. = Tidal volume + inspiratory reserve volume + expiratory reserve volume + residual volume. PDF created with pdfFactory Pro trial version www.pdffactory.com Bit of an Aside • Lung volume figures are not particularly important in determining athletic performance. • What is more important is the efficiency of the exchange of oxygen and carbon dioxide between the lungs and the blood, and between the blood and the muscle fibres. PDF created with pdfFactory Pro trial version www.pdffactory.com Bit of an Aside • Smoking interferes with lung volumes. The irritation from tobacco smoke causes mucous secretion which narrows the air passages. One cigarette can reduce the vital capacity of the lungs by 10 – 15 %. PDF created with pdfFactory Pro trial version www.pdffactory.com Ventilation • Ventilation is the amount of air breathed in one minute. • It can be defined by this equation: PDF created with pdfFactory Pro trial version www.pdffactory.com • Ventilation = Tidal volume x respiratory rate • Normal = 0.5 litres x 12 breaths/min = 6 litres per minute. Respiratory Volumes Average Respiratory Volumes for a 20 year- old male 3500 3100 3000 Milli Litres 2500 2000 1500 1200 1200 1000 500 500 0 Tidal Volume Inspiratory Reserve Volume PDF created with pdfFactory Pro trial version www.pdffactory.com Expiratory Reserve Volume Residual Volume Homework Please complete these questions and hand back to me in next lesson. 1) The lungs have no skeletal tissue, so how do they increase in size on breathing in? 2) Identify the major vascular substances that determine the amount of oxygen that can be delivered to body tissues and explain how it functions. 3) Describe how alveolar ventilation changes during exercise. 4) What three factors affect oxygen dissociation during exercise and how? 5) Describe the relationships between haemoglobin, pO2, acidity, pCO2 and temperature. 6) Explain how CO2 is picked up by the tissue capillary blood and then released into the alveoli. PDF created with pdfFactory Pro trial version www.pdffactory.com Transport of Oxygen and Carbon Dioxide How Gases Are Transported PDF created with pdfFactory Pro trial version www.pdffactory.com Introduction PDF created with pdfFactory Pro trial version www.pdffactory.com Goals For Learning • To explore how O2 is transported in the blood. • To explore how Co2 is transported in the blood. • This will include understanding the oxygen dissociation curve. PDF created with pdfFactory Pro trial version www.pdffactory.com • What you need to know • Definition of partial pressure • Processes of external respiration and internal respiration. Oxygen Transport • O2 is transported by the blood either, – Combined with haemoglobin (Hb) in the red blood cells (>98%) or, – Dissolved in the blood plasma (<2%). PDF created with pdfFactory Pro trial version www.pdffactory.com Oxygen Transport • The resting body requires 250ml of O2 per minute. • We have four to six billion haemoglobin containing red blood cells. • The haemoglobin allows nearly 70 times more O2 than dissolved in plasma. PDF created with pdfFactory Pro trial version www.pdffactory.com Haemoglobin Haemoglobin molecules can transport up to four O2’s When 4 O2’s are bound to haemoglobin, it is 100% saturated, with fewer O2’s it is partially saturated. PDF created with pdfFactory Pro trial version www.pdffactory.com Co-operative binding: haemoglobin’s affinity for O2 increases as its saturation increases. Oxygen binding occurs in response to the high PO2 in the lungs Lets Now Look at Haemoglobin Saturation • Haemoglobin saturation is the amount of oxygen bound by each molecule of haemoglobin • Each molecule of haemoglobin can carry four molecules of O2. • When oxygen binds to haemoglobin, it forms OXYHAEMOGLOBIN; • Haemoglobin that is not bound to oxygen is referred to as DEOXYHAEMOGLOBIN. PDF created with pdfFactory Pro trial version www.pdffactory.com Haemoglobin Saturation • The binding of O2 to haemoglobin depends on the PO2 in the blood and the bonding strength, or affinity, between haemoglobin and oxygen. • The graph on the following page shows an oxygen dissociation curve, which reveals the amount of haemoglobin saturation at different PO2 values. PDF created with pdfFactory Pro trial version www.pdffactory.com The Oxygen Dissociation Curve • Reveals the amount of haemoglobin saturation at different PO2 values. PDF created with pdfFactory Pro trial version www.pdffactory.com The Oxygen Disassociation Curve Haemoglobin saturation isIn the lungs the partial pressure is approximately determined by the partial pressure 100mm of Hg at this Partial haemoglobin has oxygen. When these values Pressure are a high affinity to 02 and is 98% saturated. graphed they produce the Oxygen Disassociation Curve In the tissues of other organs a typical PO2 is 40 mmHg here haemoglobin has a lower affinity for O2 and releases some but not all of its O2 to the tissues. When haemoglobin leaves the tissues it is still 75% saturated. PDF created with pdfFactory Pro trial version www.pdffactory.com Haemoglobin Saturation at High Values Lungs at sea level: PO2 of 100mmHg haemoglobin is 98% SATURATED When the PO2 in the lungs declines below typical sea level values, haemoglobin still has a high affinity for O2 and remains almost fully saturated. PDF created with pdfFactory Pro trial version www.pdffactory.com Lungs at high elevations: PO2 of 80mmHg, haemoglobin 95 % saturated Even though PO2 differs by 20 mmHg there is almost no difference in haemoglobin saturation. Haemoglobin Saturation at Low Values PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Altering Haemoglobin Saturation PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Altering Haemoglobin Saturation (Exercise) PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Affecting Haemoglobin Saturation • Blood acidity… • Blood temperature… • Carbon Dioxide concentration PDF created with pdfFactory Pro trial version www.pdffactory.com Respiratory Response to Exercise Factors affecting Disassociation BLOOD TEMPERATURE • increased blood temperature • reduces haemoglobin affinity for O2 • hence more O2 is delivered to warmed-up tissue BLOOD Ph • lowering of blood pH (making blood more acidic) • caused by presence of H+ ions from lactic acid or carbonic acid • reduces affinity of Hb for O2 • and more O2 is delivered to acidic sites which are working harder CARBON DIOXIDE CONCENTRATION • the higher CO2 concentration in tissue • the less the affinity of Hb for O2 • so the harder the tissue is working, the more O2 is released PDF created with pdfFactory Pro trial version www.pdffactory.com Key Point • Increased temperature and hydrogen ion (H+) (pH) concentration in exercising muscle affect the oxygen dissociation curve, allowing more oxygen to be uploaded to supply the active muscles. PDF created with pdfFactory Pro trial version www.pdffactory.com Carbon Dioxide Transport • Carbon dioxide also relies on the blood fro transportation. Once carbon dioxide is released from the cells, it is carried in the blood primarily in three ways… • Dissolved in plasma, • As bicarbonate ions resulting from the dissociation of carbonic acid, • Bound to haemoglobin. PDF created with pdfFactory Pro trial version www.pdffactory.com Dissolved Carbon Dioxide • Part of the carbon dioxide released from the tissues is dissolved in plasma. But only a small amount, typically just 7 – 10%, is transported this way. • This dissolved carbon dioxide comes out of solution where the PCO2 is low, such as in the lungs. • There it diffuses out of the capillaries into the alveoli to be exhaled. PDF created with pdfFactory Pro trial version www.pdffactory.com In Review 1) Oxygen is transported in the blood primarily bound to haemoglobin though a small amount is dissolved in blood plasma. 2) Haemoglobin oxygen saturation decreases. 1) 2) 3) When PO2 decreases. When pH decreases. When temperature increases. PDF created with pdfFactory Pro trial version www.pdffactory.com In Review Each of these conditions can reflect increased local oxygen demand. They increase oxygen uploading in the needy area. 3) Haemoglobin is usually about 98% saturated with oxygen. This reflects a much higher oxygen content than our body requires, so the blood’s oxygen-carrying capacity seldom limits performance. PDF created with pdfFactory Pro trial version www.pdffactory.com In Review 4) Carbon dioxide is transported in the blood primarily as bicarbonate ion. This prevents the formation of carbonic acid, which can cause H+ to accumulate, decreasing the pH. Smaller amounts of carbon dioxide are carried either dissolved in the plasma or bound to haemoglobin PDF created with pdfFactory Pro trial version www.pdffactory.com Gas Exchange at the Muscles PDF created with pdfFactory Pro trial version www.pdffactory.com Gas Exchange at the Muscles • Now we have considered how our respiratory and cardio-vascular system brings air into our lungs, exchange oxygen and carbon dioxide in the alveoli, and transport oxygen to the muscles (and CO2 away from them). • All that remains is for us to consider the delivery of oxygen to the muscles from the capillary blood. • This gas exchange between the tissue and the blood in the capillaries is known as – internal respiration. PDF created with pdfFactory Pro trial version www.pdffactory.com The Arterial-venous Oxygen Difference • At rest, the oxygen content of arterial blood is about 20ml of oxygen per 100 ml of blood. • This value drops to 15 or 16ml of O2 per 100ml as the blood passes through the capillaries into the venous system. • This difference in oxygen content between arterial and venous blood is referred to as the arterial-venous oxygen difference (a-VO2diff). PDF created with pdfFactory Pro trial version www.pdffactory.com ARTERIOVENOUS OXYGEN DIFFERENCE a-vO2 diff • this expresses the difference between the oxygen carried by blood in arteries and veins • and represents the amount of oxygen delivered to working tissue in the capillary system venule a-vO2 diff - AT REST capillary 15ml O2 per 100ml blood a-vO2 diff = 5ml per 100ml blood arteriole 20ml O2 per 100ml blood a-vO2 diff - DURING INTENSE EXERCISE venule capillary arteriole 5ml O2 per 100ml blood a-vO2 diff = 15ml per 100ml blood PDF created with pdfFactory Pro trial version www.pdffactory.com blood flow 20ml O2 per 100ml blood blood flow The Arterial-venous Oxygen Difference • It reflects the 4-5 ml of oxygen per 100 ml of blood taken up by the tissues. • The amount of oxygen taken up is proportional to its use for oxidative energy production. Thus as the rate of oxygen use increases, the a-vO2 diff also increases. PDF created with pdfFactory Pro trial version www.pdffactory.com The Arterial-venous Oxygen Difference • E.g. during intense exercise the a-vO2 diff in contracting muscles can increase to 15 to 16 ml per 100ml of blood. During such an effort, the blood unloads more oxygen to the active muscles because the PO2 in the muscles is drastically lower than in arterial blood. PDF created with pdfFactory Pro trial version www.pdffactory.com Key Point • The a-vO2 diff increases from a resting value of about 4 to 5 ml per 100 ml of blood up to values of 15 to 16 ml per 100 ml of blood during exercise. • This increase reflects an increase extraction of oxygen from arterial blood by active muscle, thus decreasing the oxygen content of the venous blood. PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Influencing Oxygen Delivery and Uptake. • The rates of oxygen delivery and uptake depend on the three major variables. • The oxygen content of blood. • The amount of blood flow. • The local conditions. • As we begin to exercise, each of these variables must be adjusted to ensure increased oxygen delivery to our active muscles. PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Influencing Oxygen Delivery and Uptake. • We have discussed in class that under normal circumstances haemoglobin is 98% saturated with oxygen. • Any reduction in the blood’s normal oxygen carrying capacity would hinder oxygen delivery and reduce cellular uptake of oxygen. PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Influencing Oxygen Delivery and Uptake. • Exercise causes increased blood flow through the muscles. As more blood carries oxygen through the muscles, less oxygen must be removed from each 100 ml of blood (assuming the demand remains unchanged). • Thus increasing blood flow improves oxygen delivery and uptake. PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Influencing Oxygen Delivery and Uptake. • Many local changes in the muscle during exercise affect oxygen delivery and uptake. • Muscle activity increases muscle acidity because of lactate production. • Muscle temperature and carbon dioxide concentration both increase because of increased metabolism. • All of these increase oxygen uploading from haemoglobin molecule, facilitating oxygen delivery and uptake by the muscles. PDF created with pdfFactory Pro trial version www.pdffactory.com Factors Influencing Oxygen Delivery and Uptake. • During maximal exercise,however, when we push our bodies to the limit, changes in any of these areas can impair oxygen delivery and restrict out abilities to meet oxidative demands. PDF created with pdfFactory Pro trial version www.pdffactory.com The Respiratory System External and Internal Respiration Learning Objectives nHow gases move into and out of the body (external respiration). nHow gases move within the body (internal respiration). nAn understanding of partial pressure. nThe relationship between partial pressure and movement of gases within the body. Introduction Introduction nThe respiratory and cardiovascular system combine to provide an efficient delivery system. uCarries oxygen (O2) to body tissues. uRemoves (CO 2). nThis transport system involves four separate process…. Transportation nPulmonary ventilation (breathing). nPulmonary diffusion. nTransport of oxygen and carbon dioxide via blood. nCapillary gas exchange. Pulmonary Ventilation nCommonly referred to as breathing. nIt is the process by which air moves in and out of the lungs. Pulmonary Ventilation nAir is typically drawn into the lungs through the nose. nThe mouth can be used. nBring air in through the nose has advantages over mouth breathing. uAir is warmed and humidified. uDust and other particles can be filtered out. Pulmonary Ventilation (Transport Summary) nIn through nose and mouth. nDown the pharynx. nDown the larynx. nThrough the trachea. nThrough the bronchi. nThrough the bronchioles. nThen reaches the sites of gas exchange the alveoli. Pulmonary Ventilation Inspiration Inspiration nInspiration is… tAn active process. tInvolving the diaphragm and the external intercostals. nThe ribs and sternum are moved by the external intercostals muscles. tThe ribs swing up and out. tThe sternum swings up and forward. tAt the same time the diaphragm contracts. Inspiration nThese actions expand all three dimensions of the thoracic cage. uIn tern this expands the lungs. nThis action reduces the air pressure in the lungs (intrapulmonary pressure). uThis is less than the pressure outside the body. PDF created with pdfFactory Pro trial version www.pdffactory.com nAir rushes into the lungs to reduce the pressure difference. is brought into the lungs during inspiration. uThus air Exercise and Inspiration nDuring forced or laboured breathing – as in exercise, inspiration is further assisted by, uOther muscles such as scalenes (anterior, middle and posterior). uSternocleidomastoid (in the neck). uPectorals. nThese help raise the ribs even more than during regular breathing. Inspiration nThe pressure changes required for adequate ventilation at rest are really quite small. For example, at standard atmospheric pressure (760mmHg), inspiration may decrease the pressure in the lungs (intrapulmonary pressure) by only about 3mmHg. However, during maximal respiratory effort, such as during exhaustive exercise, the intrapulmonary pressure may decrease by 80 – 100 mmHg. Pulmonary Ventilation Expiration Expiration nExpiration is… uUsually a passive process. uInvolves the relaxation of the inspiratory muscles and the recoil of the tissues. nThe diaphragm relaxes. nThe external intercostals relax. nThe elastic nature of the lung tissue causes the lungs to recoil to its resting size. Expiration nAll this activity increases the pressure in the thorax. uSo air is forced out. uThus expiration is accomplished. Expiration and Exercise nDuring exercise expiration becomes a more active process. uThe internal intercostals muscles can actively pull the ribs down. uThis can be assisted by the latissimus dorsi and quadratus lumborum muscles. tThis increases the pressure on the diaphragm, causing faster contraction, therefore accelerating return. Review of Pulmonary Respiration nPulmonary ventilation (breathing) is the process by which air is moved into and out of the lungs. It has two phases: inspiration and expiration. nInspiration is an active process through which the diaphragm and the external intercostal muscles increase the dimensions, and thus the volume, of the thoracic cage. This decreases the pressure in the lungs and draws air in. Review of Pulmonary Respiration nNormal expiration is a passive process. The inspiratory muscles relax and the elastic tissue of the lungs recoil, retuning the thoracic cage to its smaller, normal dimensions. This increases the pressure in the lungs and forces air out. nForced or laboured inspiration and expiration are active processes, dependant on muscle action. Pulmonary Diffusion Gas Exchange in the Lungs Pulmonary Diffusion nAir was brought into the lungs during pulmonary ventilation; tGas exchange must occur between this air and the blood. nThis process is known as pulmonary diffusion. Pulmonary Diffusion nPulmonary diffusion is the process by which gases are exchanged across the respiratory membrane in the alveoli. PDF created with pdfFactory Pro trial version www.pdffactory.com Functions of Pulmonary Diffusion nIt replenishes the blood’s O2 supply. nIt removes CO2 from returning venous blood. The Process of Pulmonary Diffusion nBlood from most of the body returns through the ______ (shown in red) to pulmonary (______) The Venae Cava and Pulmonary Side of the Heart The Process of Pulmonary Diffusion nFrom the right ventricle, this blood is pumped through the pulmonary artery to the lungs, ultimately working its way into the pulmonary capillaries. nThese capillaries form a dense network around the alveolar sacs. nThe vessels are small enough that the red blood cells can pass through but in single file. The Respiratory Membrane nGas exchange between the air and the alveoli and the blood in the pulmonary capillaries occurs across the respiratory membrane. The Respiratory Membrane The Respiratory Membrane nIs composed of. tThe alveolar wall, tThe capillary wall, and, tTheir basement membranes. nIt is very thin, measuring only 0.5 to 4.0 Цm. nThis membrane presents a barrier for gas exchange. nLets now look how this gas exchange occurs. Partial Pressure nThe air we breathe is a mixture of gases. uEach exerts a pressure in proportion to its concentration in the gas mixture. nThe individual pressures from each gas in a mixture is referred to as partial pressures. nTherefore as according to Dalton’s law, the total pressure of a mixture of gases equals the sum of the partial pressures of the individual gases in the mixture. Key Point nThe total pressure of a mixture of gases equals the sum of the partial pressures of the individual gases in that mixture. The Air We Breathe uThe air we breathe is composed of: n79.04% Nitrogen (N2). n20.93% Oxygen (O2). n0.03% Carbon Dioxide (CO2). The standard atmospheric pressure is approximately. q760mmHg. qThis is considered the total pressure of the three gases or 100%. Partial Pressures of the Gases We Breathe nNitrogen. n% of air = 79.04%. n79.04% of total atmospheric pressure. n(0.7904 x 760mmHg). n = 600.7mmHg. nPN2 = 600.7mmHg. Partial Pressures of the Gases We Breathe nOxygen: PDF created with pdfFactory Pro trial version www.pdffactory.com n% of air = 20.93%. n20.93% of total atmospheric pressure. n(0.2093 x 760mmHg). n= 159.0mmHg. nPO 2= 159.0mmHg. Partial Pressures of the Gases We Breathe nCarbon Dioxide: n% of air = 0.03%. n0.03% of total atmospheric pressure. n(0.003 x 760mmHg). n= 0.3mmHg. nPCO2 = 0.3mmHg. Important Point nGases in our bodies are dissolved in fluids, such as blood plasma. nAccording to Henry’s law, ugases dissolve in liquids in proportion to their partial pressures, depending also on their solubilities in the specific fluids and on the temperature. Important Point nA gas’s solubility in blood is constant, and blood temperature is relatively constant. nThus the most critical factor for gas exchange between the alveoli and blood is: uThe pressure gradient between the gases in the two areas. Gas Exchange in the Alveoli nDifferences in the partial pressure of the gases in the alveoli and the gases in the blood create a pressure gradient across the respiratory membrane. nThis forms the basis of gases exchange during pulmonary diffusion. nWhat would happen if the pressures were equal? Key Point nThe greater the pressure gradient across the respiratory membrane, the more rapidly oxygen will diffuse across it. Gas Exchange in the Alveoli Oxygen Exchange nPO2 = 159mmHg. nThis drops to 100 –105mmHg when air is inhaled and enters the alveoli. nThe blood, stripped of much of its O2 enters the pulmonary capillaries with a PO2 = 40 –45mmHg. nThis is about 55 mmHg less than PO2 in the alveoli. nIt is this pressure gradient that drives the O2 from the alveoli into the blood. Oxygen Exchange Oxygen Exchange nThe rate in which O2 diffuses from the alveoli into the blood is referred to as the oxygen diffusion capacity. nAt rest approx 23 ml of O2 diffuses per minute. nDuring maximal exercise this can raise to 45 ml in the untrained athlete and 80 ml in the trained athlete. Training and O2 Diffusion Capacity nAthletes with large aerobic capacities often also have greater oxygen diffusion capacities. nThis is likely the combined result of: uIncreased cardiac output. uIncreased alveolar surface area, and, uReduced resistance to diffusion across respiratory membranes. Carbon Dioxide Exchange PDF created with pdfFactory Pro trial version www.pdffactory.com nCO 2 exchange, like O2 exchange, moves along a pressure gradient. nBlood passing through the. uAlveoli has PCO 2 of about 45mmHg. uThe alveoli air has PCO2 = 40mmHg. nThis results is a relatively small pressure gradient of about 5mmHg. nIs this a problem? How do we over come this problem? Pulmonary Diffusion Review nPulmonary diffusion is the process by which gases are exchanged across the respiratory membrane in the alveoli. Pulmonary Diffusion Review nThe amount of gas exchange that occurs across a membrane primarily depends on the partial pressure of each gas, though gas solubility and temperature are also important. Gases diffuse along a pressure gradient, moving from an area of higher pressure to one of lower pressure. Thus oxygen enters the blood and carbon dioxide leaves it. Pulmonary Diffusion Review nOxygen diffusion capacity increases as you move from rest to exercise. When your body needs more oxygen, oxygen exchange is facilitated. nThe pressure gradient for carbon dioxide exchange is less than for oxygen exchange, but carbon dioxide’s membrane solubility is 20 times greater than that of oxygen, so carbon dioxide crosses the membrane easily, even without a large pressure gradient. Transport of Oxygen and Carbon Dioxide How Gases Are Transported Transport of Oxygen and Carbon Dioxide nNow we have considered how we bring air into our lungs via pulmonary ventilation and how gas exchange occurs via pulmonary diffusion. Next we must consider how gases are transported in our blood to deliver the oxygen to the tissues and to remove the carbon dioxide that the tissues produce. We will consider separately the transport of each gas. Oxygen Transport nO2 is transported by the blood either, u Combined with haemoglobin (Hb) in the red blood cells (>98%) or, uDissolved in the blood plasma (<2%). Oxygen Transport nOnly about 3 ml of O2 are dissolved in each litre of plasma. nAssuming we have a total plasma volume of 3 to 5 litres, only about 9 – 15 ml of O2 can be carried in the dissolved state. Oxygen Transport nThis is not enough to supply even the resting body, which requires 250ml per minute. nFortunately we have four to six billion haemoglobin containing red blood cells. nThe haemoglobin allows nearly 70 times more O2 than dissolved in plasma. Haemoglobin Saturation nHaemoglobin saturation is the amount of oxygen bound by each molecule of haemoglobin Haemoglobin Saturation nEach molecule of haemoglobin can carry four molecules of O2. nWhen oxygen binds to haemoglobin, it forms OXYHAEMOGLOBIN; nHaemoglobin that is not bound to oxygen is referred to as DEOXYHAEMOGLOBIN. nShow the haemoglobin. Haemoglobin Saturation PDF created with pdfFactory Pro trial version www.pdffactory.com nThe binding of O2 to haemoglobin depends on the PO2 in the blood and the bonding strength, or affinity, between haemoglobin and oxygen. nThe graph on the following page shows an oxygen dissociation curve, which reveals the amount of haemoglobin saturation at different PO 2 values. Dissociation Curve nReveals the amount of haemoglobin saturation at different PO values. 2 Haemoglobin Saturation nA high blood PO2 results in almost complete haemoglobin saturation, which means the maximum amount of oxygen is bound. nBut as the PO2 is reduced, so is haemoglobin saturation. Factors Affecting Haemoglobin Saturation nBlood acidity… nBlood temperature… Factors Affecting Haemoglobin Saturation – Blood Acidity nIf the blood becomes more acidic the dissociation curve shifts right. nThis means that more oxygen is being uploaded from the haemoglobin at tissue level. nSee overhead. Factors Affecting Haemoglobin Saturation – Blood Acidity nLook at the overhead. nThe rightward shift of the curve is due to a decline in pH. This is referred to as the BOHR effect. nSo why is this important to us????? Factors Affecting Haemoglobin Saturation – Blood Acidity nThe pH in the lungs is generally high. tWhat does this mean? nSo haemoglobin passing through the lungs has a strong affinity for oxygen, encouraging high saturation. nAt the tissue level, however the pH is lower, causing oxygen to dissociate from haemoglobin, thereby supplying oxygen to the tissues. Factors Affecting Haemoglobin Saturation – Blood Acidity nWith exercise, the ability to upload oxygen to the muscles increases as the muscle ph decreases. Factors Affecting Haemoglobin Saturation – Blood Temperature nLook at overhead. nIncreased blood temperature shifts the dissociation curve to the right, indicating that oxygen is uploaded more efficiently. Factors Affecting Haemoglobin Saturation – Blood Temperature nBecause of this, the haemoglobin will upload more oxygen when blood circulates through the metabolically heated active muscles. nIn the lungs, where the blood might be a bit cooler, haemoglobin’s affinity for oxygen is increased. This encourages oxygen binding. Key Point nIncreased temperature and hydrogen ion (H+) (pH) concentration in exercising muscle affect the oxygen dissociation curve, allowing more oxygen to be uploaded to supply the active muscles. Carbon Dioxide Transport nCarbon dioxide also relies on the blood fro transportation. Once carbon dioxide is released from the cells, it is carried in the blood primarily in three ways… nDissolved in plasma, nAs bicarbonate ions resulting from the dissociation of carbonic acid, nBound to haemoglobin. Dissolved Carbon Dioxide PDF created with pdfFactory Pro trial version www.pdffactory.com nPart of the carbon dioxide released from the tissues is dissolved in plasma. But only a small amount, typically just 7 – 10%, is transported this way. nThis dissolved carbon dioxide comes out of solution where the PCO2 is low, such as in the lungs. nThere it diffuses out of the capillaries into the alveoli to be exhaled. Bicarbonate Ions nThe majority of carbon dioxide ions is carried in the form of bicarbonate ion. n60 - 70% of all carbon dioxide in the blood. nThe following bit is quite heavy just listen hard. Bicarbonate Ions nCarbon Dioxide and water molecules combine to form carbonic acid (H2CO3). nThis acid is unstable and quickly dissociates, freeing a hydrogen ion (H+) and forming a bicarbonate ion (HCO3-): nCO2 + H2O H2CO3 CO 2 + H2O Bicarbonate Ions nThe H+ subsequently binds to haemoglobin and this binding triggers the BOHR effect (mentioned earlier). nThis shifts the oxygen-haemoglobin dissociation curve to the right. nThus formation of bicarbonate ion enhances oxygen uploading. Bicarbonate Ions nThis also plays a buffering as the H+ is neutralised therefore preventing any acidification of the blood. nWhen blood enters the lungs, where the PCO2 is lower, the H+ and bicarbonate ions rejoin to form carbonic acid, which then splits into carbon dioxide and water. nIn other words the carbon dioxide is re-formed and can enter the alveoli and then be exhaled. Key Point nThe majority of carbon dioxide produced by the active muscles is transported back to the lungs in the form of bicarbonate ions. Carbaminohaemoglobin nCO2 transport also can occur when the gas binds with haemoglobin, forming a compound called Carbaminohaemoglobin. nIt is named so because CO2binds with the amino acids in the globin part of the haemoglobin, rather than the haeme group oxygen does. In Review nOxygen is transported in the blood primarily bound to haemoglobin though a small amount is dissolved in blood plasma. nHaemoglobin oxygen saturation decreases. nWhen PO2 decreases. nWhen pH decreases. nWhen temperature increases. In Review Each of these conditions can reflect increased local oxygen demand. They increase oxygen uploading in the needy area. 3) Haemoglobin is usually about 98% saturated with oxygen. This reflects a much higher oxygen content than our body requires, so the blood’s oxygen-carrying capacity seldom limits performance. In Review 4) Carbon dioxide is transported in the blood primarily as bicarbonate ion. This prevents the formation of carbonic acid, which can cause H+ to accumulate, decreasing the pH. Smaller amounts of carbon dioxide are carried either dissolved in the plasma or bound to haemoglobin Gas Exchange at the Muscles Gas Exchange at the Muscles nNow we have considered how our respiratory and cardio-vascular system brings air into our lungs, exchange oxygen and carbon dioxide in the alveoli, and transport oxygen to the muscles (and CO2 away from them). PDF created with pdfFactory Pro trial version www.pdffactory.com nAll that remains is for us to consider the delivery of oxygen to the muscles from the capillary blood. nThis gas exchange between the tissue and the blood in the capillaries is our fourth and final step in gas transportation – internal respiration. The Arterial-venous Oxygen Difference nAt rest, the oxygen content of arterial blood is about 20ml of oxygen per 100 ml of blood. nSee over head. nThe value drops to 15 or 16ml of oxygen per 100ml as the blood passes through the capillaries into the venous system. nThis difference in oxygen content between arterial and venous blood is referred to as the arterial-venous oxygen difference (a-VO2diff). The Arterial-venous Oxygen Difference nIt reflects the 4-5 ml of oxygen per 100 ml of blood taken up by the tissues. nThe amount of oxygen taken up is proportional to its use for oxidative energy production. Thus as the rate of oxygen use increases, the a-vO2 diff also increases. The Arterial-venous Oxygen Difference nE.g. during intense exercise (figure see OHP) the a-vO2 diff in contracting muscles can increase to 15 to 16 ml per 100ml of blood. During such an effort, the blood unloads more oxygen to the active muscles because the PO2 in the muscles is drastically lower than in arterial blood. Key Point nThe a-vO2 diff increases from a resting value of about 4 to 5 ml per 100 ml of blood up to values of 15 to 16 ml per 100 ml of blood during exercise. This increase reflects an increase extraction of oxygen from arterial blood by active muscle, thus decreasing the oxygen content of the venous blood. Factors Influencing Oxygen Delivery and Uptake. nThe rates of oxygen delivery and uptake depend on the three major variables. tThe oxygen content of blood. tThe amount of blood flow. tThe local conditions. nAs we begin to exercise, each of these variables must be adjusted to ensure increased oxygen delivery to our active muscles. Factors Influencing Oxygen Delivery and Uptake. nWe have discussed in class that under normal circumstances haemoglobin is 98% saturated with oxygen. nAny reduction in the blood’s normal oxygen carrying capacity would hinder oxygen delivery and reduce cellular uptake of oxygen. Factors Influencing Oxygen Delivery and Uptake. nExercise causes increased blood flow through the muscles. As more blood carries oxygen through the muscles, less oxygen must be removed from each 100 ml of blood (assuming the demand remains unchanged). nThus increasing blood flow improves oxygen delivery and uptake. Factors Influencing Oxygen Delivery and Uptake. nMany local changes in the muscle during exercise affect oxygen delivery and uptake. nMuscle activity increases muscle acidity because of lactate production. nMuscle temperature and carbon dioxide concentration both increase because of increased metabolism. nAll of these increase oxygen uploading from haemoglobin molecule, facilitating oxygen delivery and uptake by the muscles. Factors Influencing Oxygen Delivery and Uptake. nDuring maximal exercise,however, when we push our bodies to the limit, changes in any of these areas can impair oxygen delivery and restrict out abilities to meet oxidative demands. Carbon Dioxide Removal nCarbon dioxide exits the cells by simple diffusion in response to the partial pressure gradient between the tissue and the capillary blood. nE.g. Muscles generate carbon dioxide through oxidative metabolism, so the PCO2 in muscles would be relatively high compared to that in the capillary blood. Consequently, CO2 diffuses out of the muscles and into the blood to be transported to the lungs. PDF created with pdfFactory Pro trial version www.pdffactory.com AS Level Sport and Physical Education Class Home Work – Please answer the following questions on a piece of paper and hand it to me either before or in Thursday’s lesson Respiration and The Respiratory System 1) Explain in detail external respiration – include both the inspiration (including the passage of oxygen along the respiratory passageways) and expiration. It would be advantageous to include information on partial pressure plus other relevant information. (15 marks) 2) Explain in detail gaseous exchange at the lungs – include the pressure gradient, respiratory membrane, and diffusion plus any other relevant information. (15 marks) NB - Please note the topics I have highlighted in these questions will not give a definitive answer. For full marks I will need to see more detail. 3) What substances carries oxygen in the blood? (1 mark) 4) Why is carbon monoxide so dangerous to the respiratory system? Clue - think about oxygen and the substance named above. (2 marks) 5) What is tidal volume? (1 mark) 6) What is the inspiratory reserve volume? (1 mark) 7) Identify the muscles used in respiration at rest and during exercise. (4 marks) 8) Identify and explain four factors that influence the efficiency of gaseous exchange between the lungs and the pulmonary capillaries. (4 marks) Clue – the answer can be found in the respiratory chapter in your textbook. AS Level Sport and Physical Education Homework of 30th October PDF created with pdfFactory Pro trial version www.pdffactory.com Hand in Thursday 7h November Name_____________________ Answer all the questions on the sheet. 2 3 4 PDF created with pdfFactory Pro trial version www.pdffactory.com 5 6 7 PDF created with pdfFactory Pro trial version www.pdffactory.com Name_____________________ Answer all the questions on the sheet. 2 3 4 PDF created with pdfFactory Pro trial version www.pdffactory.com 5 6 7 PDF created with pdfFactory Pro trial version www.pdffactory.com The breathing characteristics of games players may alter during performance. Figure 3 shows the proportion of oxygen and carbon dioxide breathed during exercise compared with rest. Figure 3 (i) Use the information in Figure 3 to describe the effects of exercise on gas exchange in the lungs. Suggest why these changes occur. (3 marks) (ii) In what form are carbon dioxide and oxygen transported by the blood? (2 marks) (iii) Explain the causes of the increase in breathing rate experienced during exercise. (3 marks) PDF created with pdfFactory Pro trial version www.pdffactory.com