JBMR
CLINICAL VIGNETTE
Glucocorticoids Are Not Always Deleterious for Bone
Antoon HJM van Lierop, Neveen AT Hamdy, and Socrates E Papapoulos
Department of Endocrinology and Metabolic Diseases, Leiden University Medical Center, Leiden, The Netherlands
ABSTRACT
A 23-year-old man with the rare sclerosing bone disorder van Buchem disease presented with progressively worsening headaches that
eventually became persistent and associated with papilledema. Increased intracranial pressure was diagnosed, and the patient had a
ventriculoperitoneal drain inserted as well as simultaneously receiving treatment with prednisone. Before starting treatment, there was
biochemical evidence for increased bone turnover and for steady increases in bone mineral density (BMD) at the spine and total hip
despite the patient having reached his peak height of 197 cm at the age of 19 years. Treatment with prednisone for 2 years resulted in
biochemical and histologic suppression of bone formation as well as of bone resorption and arrest of further bone accumulation. Our
data suggest that glucocorticoids (GCs) may represent an attractive alternative to the high-risk surgical approaches used in the
management of patients with progressive sclerosing bone disorders. Our findings also suggest that whereas sclerostin may not be
required for the action of GCs on bone formation, it may well be important for the action of GCs on bone resorption. The exact
mechanism by which sclerostin may be involved in the regulation of bone resorption is as yet to be explored. ß 2010 American Society
for Bone and Mineral Research.
KEY WORDS: BONE RESORPTION; BONE FORMATION; VAN BUCHEM DISEASE; PREDNISONE; SCLEROSTIN
Introduction
V
an Buchem disease is a rare bone sclerosing disorder
described for the first time in 1955.(1) It belongs to the group
of craniotubular hyperostoses and is characterized by progressive generalized osteosclerosis, particularly of the mandible and
the skull, owing to excessive bone formation.(2) It is caused by a
52-kb deletion 35 kb downstream of the SOST gene, which
encodes sclerostin, on chromosome 17q12-21.(3,4) This protein is
produced in the skeleton exclusively by the osteocytes and
inhibits bone formation by antagonizing the Wnt signaling
pathway.(5) Clinical manifestations of the disease are due to
entrapment of cranial nerves often associated with facial palsy
and loss of hearing and smell.(2) Van Buchem disease is thought
to have milder clinical manifestations than sclerosteosis, a
craniotubular hyperostosis with similar phenotype owing to
inactivating mutations of the SOST gene.(6,7) Management of the
complications of both these sclerosing dysplasias is surgical,
aiming at removal of the excess of bone, a technically difficult
and sometimes dangerous procedure.(8–10) No medical treatment is available for either sclerosing disease. Glucocorticoids
(GCs) are known inhibitors of bone formation,(11,12) and we
hypothesized that administration of these agents to patients
with complications due to bone overgrowth may arrest its
further progress.
We present here sequential observations of a patient with van
Buchem disease with life-threatening increased intracranial
pressure who was treated successfully with prednisone.
Case Report
The patient first came under our care at the age of 10 years
with an established diagnosis of van Buchem disease. The
disease was diagnosed clinically and radiologically in infancy
and later confirmed genetically by the finding of a 52-kb
homozygous deletion 35 kb downstream the SOST gene on
chromosome 17q12-q21 [the patient was briefly described
(patient 15) by Staeling-Hampton and colleagues(3)]. The
parents are consanguineous and were both confirmed to be
heterozygotes for the disease. There were 3 phenotypically
normal sisters in whom no genetic testing has been so far
undertaken.
As described in this disorder, clinical manifestations started
early in childhood. The patient had a facial palsy at the age of 3
years and developed progressive deafness requiring the use of a
hearing aid by the age of 10 years, followed by bilateral boneanchored hearing aids. He has otherwise been well with normal
growth development along the 95th centile, reaching a final
height of 197 cm by the age of 19 years. He completed his
Received in original form March 24, 2010; revised form April 21, 2010; accepted June 4, 2010. Published online June 14, 2010.
Address correspondence to: Socrates E Papapoulos, Department of Endocrinology and Metabolic Diseases, Leiden University Medical Center, Albinusdreef 2, 2333
ZA Leiden, The Netherlands. E-mail: m.v.iken@lumc.nl
Journal of Bone and Mineral Research, Vol. 25, No. 12, December 2010, pp 2796–2800
DOI: 10.1002/jbmr.151
ß 2010 American Society for Bone and Mineral Research
2796
The December 2010 issue of Journal of Bone and Mineral Research
was published online on 23 Nov 2010. A pagination error was
subsequently identified. This notice is included to indicate that the
pagination is now correct and authoritative [20 January 2011].
secondary education and is employed as office assistant
manager. He married at the age of 20 years, and he is the
father of 3 healthy children.
The patient demonstrated the typical clinical and radiologic
features of van Buchem disease, with enlarged head and
mandible and no syndactyly or other digit malformations. During
the 15-year duration of follow-up, there were no other clinical
signs or symptoms, and blood pressure was normal. Hematologic
and biochemical parameters, including those of mineral
metabolism, demonstrated no abnormalities over the years.
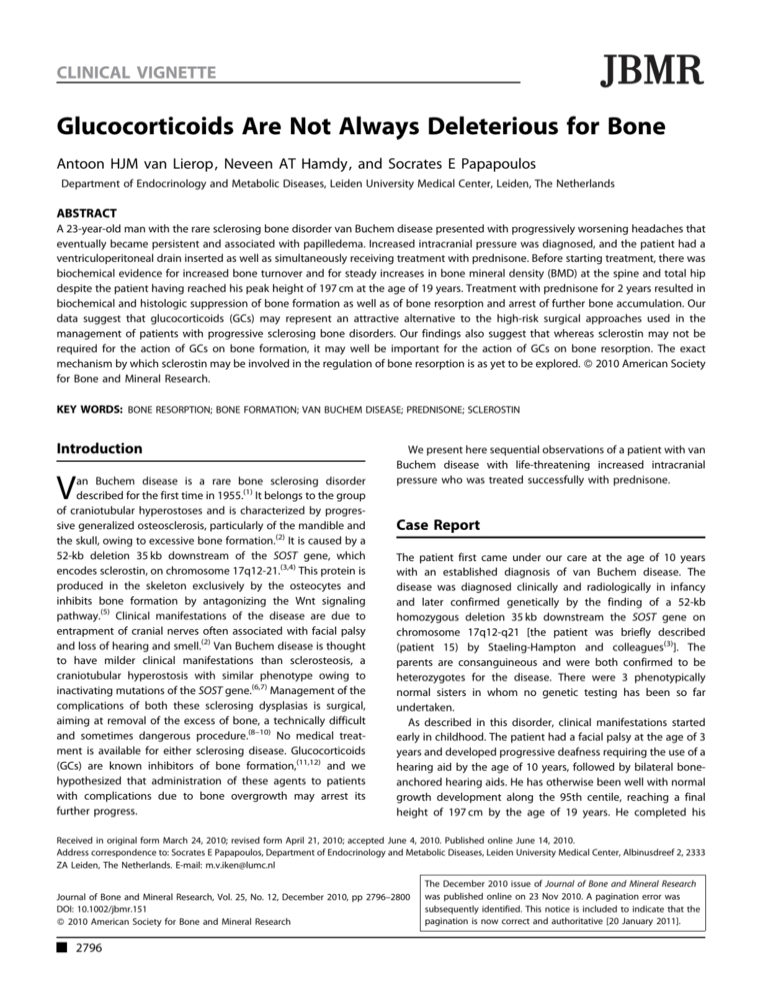
Skeletal radiographs showed thickening of the calvarium, base of
the skull, and long bones and sclerosis of the vertebrae (Fig. 1).
Bone mineral density (BMD) values of the spine and hip were
markedly increased at presentation (Z-score þ6.2) and continued
to increase in parallel with that of his healthy peers without,
however, attaining a peak (highest Z-score being 7.7).
Biochemical markers of bone turnover always were increased
compared with normal values for age but followed a normal
pattern of change with a further increase during the growth
spurt and a progressive decline thereafter, although never
reaching the normal range (Fig. 2).
At the age 23 years, the patient complained of progressive
headaches that eventually became persistent and were
associated with dizziness and signs of increased intracranial
pressure in the form of papilledema. The diagnosis was
confirmed radiologically, and a ventricular-peritoneal drain
was implanted, and the patient was concomitantly started on
prednisone 30 mg/day that was reduced to 10 mg/day within
1 month. In the following 2 years he received different doses of
prednisone, as depicted in Fig. 3, but no calcium or vitamin D
supplements. These interventions were followed by rapid
improvement of his symptoms, and the improvement was
sustained during the follow-up period. There were no
appreciable changes in metabolic parameters with treatment
(highest values of serum cholesterol and glucose were 5.6 and
6.1 mmol/L, respectively, and of urinary calcium excretion
7.8 mmol/24 hours).
Methods
The biochemical markers of bone turnover procollagen type I N
propeptide (P1NP) and C-terminal telopeptide of type I collagen
(b-CTX) were measured in serum at regular intervals using the
E-170 system (Roche BV, Woerden, Holland). BMD was measured
by dual-energy X-ray absorptiometry (DXA; Hologic QDR 4500,
Waltham, MA, USA). An iliac crest biopsy was obtained after in
vivo labeling with two courses of tetracycline separated by
12 days. Bone histomorphometry was performed on undecalcified histologic bone sections by Dr Pascale Chavassieux (INSERM
Unit 831, University of Lyon, Faculty of Medicine R Laennec,
Lyon, France). Immunohistochemical staining for sclerostin was
performed in our laboratory using a previously described
technique.(13)
Results
Biochemical markers of bone turnover
The changes in serum P1NP and b-CTX before and during
prednisone treatment are depicted in Fig. 3. Before treatment,
values of both markers of bone turnover were elevated and
decreased to within the normal reference adult range within
4 weeks of starting treatment with prednisone. The effect of
prednisone on bone turnover depended on the dose administered, and attempts to reduce the dose below 5 mg/day were
associated with increases in serum markers of bone turnover. It
was notable that during treatment, there was a close relationship
between serum b-CTX and P1NP values, with the two markers
demonstrating parallel changes during adjustments of the dose
of prednisone, suggesting a tight coupling of bone resorption
and bone formation. There was a highly significant correlation
between the two markers throughout the 2-year period of follow
up (R2 ¼ 0.765).
BMD
The changes in BMD measured at the spine and hip for the
6 years preceding the start of prednisone treatment and for
2 years thereafter are shown in Table 1. Despite high baseline
values, BMD continued to increase steadily during adulthood by
about 4% every 2 years, demonstrating no further increase after
2 years of treatment with prednisone.
Bone histology
Fig. 1. Radiographs of the skull showing thickening of the calvarium and
the base of the skull and of the hand illustrating the absence of
syndactyly or other malformations.
GLUCOCORTICOIDS IN VAN BUCHEM DISEASE
On an iliac crest biopsy taken 2 years after the start of prednisone
treatment, there was sclerosis and no evidence of active bone
remodeling. Cancellous bone volume was clearly increased,
and bone trabeculae were thick and well connected. The extent
of eroded surfaces was very low (0.4%; normal 3.1% 1.1%),
and Howship’s lacunae were devoid of osteoclasts. In addition,
no osteoid seams were seen, and there was no tetracycline
uptake on examination under fluorescent light. As expected
and described previously,(14) osteocytes did not stain for
sclerostin.
Journal of Bone and Mineral Research
2797
Fig. 2. Sequential measurement of serum alkaline phosphate activity (AP) in units/L, urinary hydroxyproline/creatinine ratio (OHP/Cr) in mmol/mmol, and
height (cm) in a patient with van Buchem disease over a 10-year period. Interrupted lines indicate the upper limit of normal range.
Discussion
This case illustrates the beneficial effect of prednisone treatment
on bone metabolism in a patient with van Buchem disease and
life-threatening increased intracranial pressure. Treatment
resulted in a histologically documented dramatic decrease in
bone formation. Following therapy, there was also no further
increase in BMD at the spine and hip. Although clinical
manifestations of increased intracranial pressure improved
significantly, this cannot be attributed solely to treatment with
prednisone because the patient had a ventriculoperitoneal drain
implanted simultaneously at the time of starting prednisone.
Before prednisone treatment, the patient had an increased
rate of bone turnover, as assessed biochemically, associated with
a continuous increase in BMD of the spine and hip. The
biochemical markers of bone formation, P1NP and osteocalcin,
have been reported previously to be elevated in 6 patients with
van Buchem disease compared with their levels in disease
carriers, being above the upper limit of the normal range in 3 of
them.(15) Urinary cross-linked N-telopeptide of type I collagen
(NTX) levels were higher in 4 patients with the disease compared
with carriers. Bone density measured in the phalanges by
radiographic absorptiometry was elevated in all these
patients.(15) There are, however, no longitudinal data reported
to date in patients with van Buchem disease. In our patient, at
least up to the age of 23 years, both biochemical markers of
resorption and formation were increased. The clinical progression of the disease, which was due to bone overgrowth, as also
evidenced by the steady increase in BMD, prompted us to use
GCs in an attempt to arrest the process of bone accumulation.
The beneficial use of GCs has been reported previously in a
patient with craniotubular hyperostosis owing to an unidentified
genetic defect.(16) In this patient, prednisone given for three
courses of 10 weeks each reduced serum osteocalcin but had no
effect on urinary deoxypyridinoline (DPD) and there were no
reported changes in BMD. In a few patients with progressive
diaphyseal dysplasia, a craniotubular hyperostotic disorder
distinct from van Buchem disease, which is due to mutations
of the gene encoding transforming growth factor b (TGF-b),
prednisone treatment during childhood and adolescence led to
clinical(17,18) and in one case radiologic improvement.(19)
Table 1. Bone Mineral Density Measurements and Height of a
Patient With van Buchem Disease Before and After 2 Years of
Prednisone Treatment (Date: Month/Year)
Date
Fig. 3. Biochemical markers of bone formation and resorption before
and during treatment with prednisone. P1NP ¼ diamonds and solid line;
b-CTX ¼ closed circles and interrupted line.
2798
Journal of Bone and Mineral Research
2-2001
4-2003
1-2005
2-2007
5-2007
6-2009
Height
193.9
197.0
197.0
197.0
Start prednisone
197.0
LS
BMD
Change
(%)
TH
BMD
Change
(%)
1.634
1.787
1.855
1.934
—
9.4
3.8
4.3
1.410
1.741
1.820
1.888
—
23.5
4.5
3.7
1.921
–0.7
1.895
0.4
2
Note: Height in cm, LS BMD ¼ lumbar spine BMD in g/cm , TH
BMD ¼ total hip BMD in g/cm2.
VAN LIEROP ET AL.
GCs have a deleterious effect on the skeleton, increasing bone
fragility by systemic and local actions.(11) Their main action on
bone metabolism is to decrease bone formation by inhibiting the
proliferation and differentiation of osteoblasts and increasing
their rate of apoptosis.(12,20) CCs also have been reported to
increase bone resorption, particularly during the early phase of
treatment, by stimulating osteoclastic activity and survival
through an effect on the RANKL/OPG signaling pathway.(21–23)
Consistent with these findings, studies in animals(24) and in
humans(25–33) have shown that administration of GCs significantly reduce biochemical markers of bone formation but have
no effect or even increase those of bone resorption. Remarkably,
administration of prednisone to our patient decreased not only
bone formation but also bone resorption within 4 weeks of
starting of treatment. Serum P1NP and b-CTX decreased and
increased concurrently during alterations of prednisone dose,
suggesting a tight coupling of bone resorption and formation
during treatment. This was further supported by the strong
correlation between the two biochemical markers of bone
turnover before and during prednisone treatment.
The reason for this unique response of bone resorption to
prednisone is not apparently clear but may well be related to the
genetic defect of our patient with van Buchem disease. Recent
studies have indicated that at least some of the negative effects
of GCs on osteoblast function are due to inhibition of the
canonical Wnt signaling pathway through stimulation of the
Wnt antagonists Dkk1, Sfr1, and sclerostin and activation of
GSK3b.(34–36) In addition, it has been reported that in osteoblasts,
Wnt signaling decreases bone resorption by downregulating the
expression of RANKL and upregulating that of OPG,(37–40) an
action that can be reversed by GCs.(21–23) It thus may be that
sclerostin is not required for the action of GCs on bone formation,
as suggested by the clear reduction of bone formation in our
patient in the absence of sclerostin. In contrast, sclerostin may
well be important for the action of GCs on bone resorption. We
propose that in the absence of sclerostin, GCs may lose their
ability to stimulate RANKL and decrease OPG by a mechanism
that is as yet to be explored. In support of this hypothesis are the
data in above-mentioned patient with craniotubular hyperostosis treated with prednisone.(16) This patient was phenotypically
very similar to ours and had increased bone turnover before
treatment, although genetic analysis excluded abnormalities
in the SOST gene. In this patient, prednisone treatment was
associated with a significant decrease in serum osteocalcin but
with no parallel change in urinary DPD excretion, a response
compatible with that reported in other human studies. It may be,
therefore, that sclerostin, besides its critical role in the regulation
of bone formation, is also involved in the regulation of bone
resorption, as also has been reported for Dkk1, another inhibitor
of the Wnt signaling pathway.(41) Alternatively, it may be that in
the absence of sclerostin, bone resorption may be driven by
bone formation through an as yet unknown action of GCs
downstream the Wnt signaling pathway.
The long-term follow-up of this patient with life-threatening
complications as a result of excess bone formation illustrates the
beneficial effect of prednisone treatment on bone metabolism
and suggests that using GCs may represent an attractive medical
alternative to the currently used, technically difficult, and
GLUCOCORTICOIDS IN VAN BUCHEM DISEASE
complication-associated surgical treatments of such patients.
The results suggest further that sclerostin may be involved in the
regulation of bone resorption by a mechanism that needs to be
explored further.
Disclosures
All the authors state that they have no conflicts of interest.
Acknowledgments
Special thanks to Dr Pascale Chavassieux for performing the
histomorphometric analysis of the bone biopsy. This work was
funded by EU FP7 (TALOS:Health-F2-2008-201099).
References
1. Van Buchem FS, Hadders HN, Ubbens R. An uncommon familial
systemic disease of the skeleton: hyperostosis corticalis generalisata
familiaris. Acta Radiol. 1955;44:109–120.
2. Vanhoenacker FM, Balemans W, Tan GJ, et al. Van Buchem disease:
lifetime evolution of radioclinical features. Skeletal Radiol. 2003;32:
708–718.
3. Staehling-Hampton K, Proll S, Paeper BW, et al. A 52-kb deletion in
the SOST-MEOX1 intergenic region on 17q12-q21 is associated with
van Buchem disease in the Dutch population. Am J Med Genet. 2002;
110:144–152.
4. Balemans W, Patel N, Ebeling M, et al. Identification of a 52-kb
deletion downstream of the SOST gene in patients with van Buchem
disease. J Med Genet. 2002;39:91–97.
5. van Bezooijen RL, Papapoulos SE, Hamdy NAT, Lowik CWGM. SOST/
sclerostin: An osteocyte-derived inhibitor of bone formation that
antagonizes canonical Wnt signaling. In: Bilezikian JP, Raisz LG,
Martin TJ, eds. Principles of Bone Biology, Vol. 1 3rd ed. San Diego:
Academic Press, 139–152. 2008.
6. Balemans W, Ebeling M, Patel N, et al. Increased bone density in
sclerosteosis is due to the deficiency of a novel secreted protein
(SOST). Hum Mol Genet. 2001;10:537–543.
7. Brunkow ME, Gardner JC, Van NJ, et al. Bone dysplasia sclerosteosis
results from loss of the SOST gene product, a novel cystine knotcontaining protein. Am J Hum Genet. 2001;68:577–589.
8. du Plessis JJ, Sclerosteosis: neurosurgical experience with 14 cases.
J Neurosurg. 1993;78:388–392.
9. Hamersma H, Gardner J, Beighton P. The natural history of sclerosteosis. Clin Genet. 2003;63:192–197.
10. Marmary Y, Horne T, Azaz B. Hyperostosis corticalis generalisata:
surgical management and long-term follow-up of one patient. Int J
Oral Maxillofac Surg. 1989;18:155–157.
11. Canalis E, Mazziotti G, Giustina A, Bilezikian JP. Glucocorticoidinduced osteoporosis: pathophysiology and therapy. Osteoporos
Int. 2007;18:1319–1328.
12. Weinstein RS. Glucocorticoid-induced osteoporosis. Rev Endocr
Metab Disord. 2001;2:65–73.
13. van Bezooijen RL, Roelen BA, Visser A, et al. Sclerostin is an osteocyteexpressed negative regulator of bone formation, but not a classical
BMP antagonist. J Exp Med. 2004;199:805–814.
14. van Bezooijen RL, Bronckers AL, Gortzak RA, et al. Sclerostin in
mineralized matrices and van Buchem disease. J Dent Res. 2009;
88:569–574.
15. Wergedal JE, Veskovic K, Hellan M, et al. Patients with Van Buchem
disease, an osteosclerotic genetic disease, have elevated bone for-
Journal of Bone and Mineral Research
2799
mation markers, higher bone density, and greater derived polar
moment of inertia than normal. J Clin Endocrinol Metab. 2003;88:
5778–5783.
28. Kuroki Y, Kaji H, Kawano S, et al. Short-term effects of glucocorticoid
therapy on biochemical markers of bone metabolism in Japanese
patients: a prospective study. J Bone Miner Metab. 2008;26:271–278.
16. Lopez JM, Balemans W, Piters E, Van HW, Gonzalez G. Genetic analysis
and effect of triiodothyronine and prednisone trial on bone turnover
in a patient with craniotubular hyperostosis. Bone. 2008;43:405–
409.
29. Paglia F, Dionisi S, De GS. et al. Biomarkers of bone turnover after a
short period of steroid therapy in elderly men. Clin Chem. 2001;
47:1314–1316.
17. Allen DT, Saunders AM, Northway WH Jr, Williams GF, Schafer IA.
Corticosteroids in the treatment of Engelmann’s disease: progressive
diaphyseal dysplasia. Pediatrics. 1970;46:523–531.
18. Janssens K, Vanhoenacker F, Bonduelle M, et al. Camurati-Engelmann
disease: review of the clinical, radiological, and molecular data of
24 families and implications for diagnosis and treatment. J Med
Genet. 2006;43:1–11.
19. Minford AM, Hardy GJ, Forsythe WI, Fitton JM, Rowe VL. Engelmann’s
disease and the effect of corticosteroids. A case report. J Bone Joint
Surg Br. 1981;63B:597–600.
20. Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC. Inhibition of
osteoblastogenesis and promotion of apoptosis of osteoblasts and
osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J Clin Invest. 1998;102:274–282.
21. Hofbauer LC, Gori F, Riggs BL, et al. Stimulation of osteoprotegerin
ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: potential paracrine
mechanisms of glucocorticoid-induced osteoporosis. Endocrinology.
1999;140:4382–4389.
30. Pearce G, Tabensky DA, Delmas PD, Baker HW, Seeman E. Corticosteroid-induced bone loss in men. J Clin Endocrinol Metab. 1998;83:
801–806.
31. Prummel MF, Wiersinga WM, Lips P, Sanders GT, Sauerwein HP. The
course of biochemical parameters of bone turnover during treatment
with corticosteroids. J Clin Endocrinol Metab. 1991;72:382–386.
32. Ton FN, Gunawardene SC, Lee H, Neer RM. Effects of low-dose
prednisone on bone metabolism. J Bone Miner Res. 2005;20:464–470.
33. Frediani B, Falsetti P, Bisogno S, et al. Effects of high dose methylprednisolone pulse therapy on bone mass and biochemical markers
of bone metabolism in patients with active rheumatoid arthritis: a 12month randomized prospective controlled study. J Rheumatol. 2004;
31:1083–1087.
34. Hayashi K, Yamaguchi T, Yano S, et al. BMP/Wnt antagonists are
upregulated by dexamethasone in osteoblasts and reversed by
alendronate and PTH: potential therapeutic targets for glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun. 2009;
379:261–266.
22. Humphrey EL, Williams JH, Davie MW, Marshall MJ. Effects of dissociated glucocorticoids on OPG and RANKL in osteoblastic cells.
Bone. 2006;38:652–661.
35. Yao W, Cheng Z, Busse C, Pham A, Nakamura MC, Lane NE. Glucocorticoid excess in mice results in early activation of osteoclastogenesis and adipogenesis and prolonged suppression of osteogenesis: a
longitudinal study of gene expression in bone tissue from glucocorticoid-treated mice. Arthritis Rheum. 2008;58:1674–1686.
23. Vidal NO, Brandstrom H, Jonsson KB, Ohlsson C. Osteoprotegerin
mRNA is expressed in primary human osteoblast-like cells: downregulation by glucocorticoids. J Endocrinol. 1998;159:191–195.
36. Yun SI, Yoon HY, Jeong SY, Chung YS. Glucocorticoid induces
apoptosis of osteoblast cells through the activation of glycogen
synthase kinase 3beta. J Bone Miner Metab. 2009;27:140–148.
24. Ogoshi T, Hagino H, Fukata S, Tanishima S, Okano T, Teshima R.
Influence of glucocorticoid on bone in 3-, 6-, and 12-month-old rats
as determined by bone mass and histomorphometry. Mod Rheumatol. 2008;18:552–561.
37. Fujita K, Janz S. Attenuation of WNT signaling by DKK-1 and -2
regulates BMP2-induced osteoblast differentiation and expression of
OPG, RANKL and M-CSF. Mol Cancer. 2007;6:71.
25. Bornefalk E, Dahlen I, Michaelsson K, Ljunggren Ljunghall S.
Age-dependent effect of oral glucocorticoids on markers of bone
resorption in patients with acute asthma. Calcif Tissue Int. 1998;63:
9–13.
26. Dovio A, Perazzolo L, Osella G, et al. Immediate fall of bone formation
and transient increase of bone resorption in the course of high-dose,
short-term glucocorticoid therapy in young patients with multiple
sclerosis. J Clin Endocrinol Metab. 2004;89:4923–4928.
27. Gram J, Junker P, Nielsen HK, Bollerslev J. Effects of short-term
treatment with prednisolone and calcitriol on bone and mineral
metabolism in normal men. Bone. 1998;23:297–302.
2800
Journal of Bone and Mineral Research
38. Glass DA, Bialek P, Ahn JD, et al. Canonical Wnt signaling in differentiated osteoblasts controls osteoclast differentiation. Dev Cell.
2005;8:751–764.
39. Spencer GJ, Utting JC, Etheridge SL, Arnett TR, Genever PG. Wnt
signalling in osteoblasts regulates expression of the receptor activator of NFkappaB ligand and inhibits osteoclastogenesis in vitro.
J Cell Sci. 2006;119:1283–1296.
40. Holmen SL, Zylstra CR, Mukherjee A, et al. Essential role of betacatenin in postnatal bone acquisition. J Biol Chem. 2005;280:21162–
21168.
41. Diarra D, Stolina M, Polzer K, et al. Dickkopf-1 is a master regulator of
joint remodeling. Nat Med. 2007;13:156–163.
VAN LIEROP ET AL.
NIH Public Access
Author Manuscript
Bone. Author manuscript; available in PMC 2014 June 01.
NIH-PA Author Manuscript
Published in final edited form as:
Bone. 2013 June ; 54(2): 279–284. doi:10.1016/j.bone.2013.01.034.
Glucocorticoids and Osteocyte Autophagy
Wei Yao1, Weiwei Dai1, Jean X. Jiang2, and Nancy E. Lane1
1Department of Medicine, University of California at Davis Medical Center Sacramento, CA 95818
2Department
of Biochemistry, University of Texas Health Science Center, San Antonio, TX 78229
Abstract
NIH-PA Author Manuscript
Glucocorticoids are used for the treatment of inflammatory and autoimmune diseases. While they
are effective therapy, bone loss and incident fracture risk is high. While previous studies have
found GC effects on both osteoclasts and oteoblasts, our work has focused on the effects of GCs
on osteocytes. Osteocytes exposed to low dose GCs undergo autophagy while osteocytes exposed
to high doses of GCs or for a prolonged period of time undergo apoptosis. This paper will review
the data to support the role of GCs in osteocyte autophagy.
Keywords
Glucocorticoids; autophagy; bone fragility
Introduction
NIH-PA Author Manuscript
Glucocorticoids (GCs) are used in clinical medicine as effective therapy for inflammatory/
autoimmune diseases. However, GC use creates rapid bone loss that results in a high
incident fracture risk. Epidemiologic studies find 50% of rheumatoid arthritis (RA) patients
in the United States today are still treated with chronic GCs and; baseline data from clinical
trials in RA patients report a prevalence in vertebral fracture of 30-50% [1-6]. Other studies
find that both old and young, men and women and all ethnic groups studied have bone loss
with GC treatment, making this an important public health problem [7]. Because patients
treated with GCs may require the treatment for a long period of time, there is a high medical
need to understand the biology of GC induced bone loss so that clinicians can effectively
prevent and treat this disease. Interestingly, the loss of trabecular mass, trabecular
architecture, and integral bone mass does not explain the increase in fracture risk from GCs,
as individuals treated with GCs frequently experience fractures at higher Bone Mineral
Densities (BMDs) than women with postmenopausal osteoporosis [8]. In addition, after
withdrawal of GC treatment, there can be some recovery of BMD suggesting maintenance
of bone architecture despite a change in bone fragility [8-10]. Recently, atypical fractures
have been documented to occur more often in the shaft or subtrochanteric regions of the
femur in patients treated with long-term bisphosphonates, especially for those who were
treated for 6 months or longer with GCs (Girgis C. et al., ASBMR 2010). Although more
epidemiologic and pathophysiologic research is needed to better define the risk, the adverse
© 2012 Elsevier Inc. All rights reserved.
Corresponding Author Information: Nancy E. Lane, MD, Center for Musculoskeletal Health, 4625 2nt Avenue, Suite 1002,
Sacramento, California 95817, Telephone: 916-734-0758, FAX: 916-734-4773, nelane@ucdavis.edu.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our
customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of
the resulting proof before it is published in its final citable form. Please note that during the production process errors may be
discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Yao et al.
Page 2
effects of GCs on the cortical bone quality that may be independent of BMD loss warrant
further investigation [11].
NIH-PA Author Manuscript
Biology of GC-Induced Bone Loss
GC treatment results in changes in bone remodeling [12, 13]. Observations of surface and
biochemically-based turnover in clinical studies of GC-induced osteoporosis show a
reduction in trabecular bone volume, thickness and bone formation [12, 14-16]. The
influence of glucocorticoids (GCs) on bone resorption was thought to be indirect and related
in part to reduced calcium absorption and increased renal calcium excretion [17]. However,
recent studies have found that GCs act directly on osteoclasts to decrease the apoptosis of
mature osteoclasts [18]. Kim et al. found that GCs in vitro inhibited the proliferation of
osteoclasts from bone marrow macrophages in a dose-dependent manner. In addition, higher
GC doses had no effect on osteoclast maturation but inhibited osteoclasts from reorganizing
their cytoskeleton [19]. Therefore, excess GC results in an increase in osteoclast number, but
in an apparent inhibition of function with impaired spreading and degradation of mineralized
matrix [19].
NIH-PA Author Manuscript
GCs also alter osteoblast and osteocyte function, which contributes to GC-induced
osteoporosis [17]. GCs directly inhibit cellular proliferation and differentiation of osteoblast
lineage cells [20], reduce osteoblast maturation and activity [13], and also induce osteoblast
and osteocyte apoptosis in vivo [21]. The suppression of osteoblast function by GCs is
reported to be associated with alteration of the Wnt signaling pathway [22], a critical
pathway for osteoblastogenesis [23, 24]. GCs enhance Dickkopf 1 expression [25], one of
the Wnt antagonists that prevents soluble Wnt proteins from binding to their receptor
complex [26]. GCs maintain levels of glycogen-synthase kinase-3β [27], a key kinase that
phosphorylates β-catenin, thereby preventing the translocation of β-catenin into the nucleus
and the initiation of transcription in favor of osteoblastogenesis. GCs may also enhance bone
marrow stromal cell development towards the adipocyte lineage rather than towards the
osteoblast lineage [24, 28]. Moreover, the loss of osteocytes by GC-induced apoptosis [29]
may disrupt the osteocyte-canalicular network, resulting in a failure to direct bone
remodeling at the trabecular surface. GC-induced changes in osteocyte function also result
in a weakening of the localized material properties around osteocytes as well as in decreased
whole bone strength [30].
Mineral Metabolism and Osteocytes
NIH-PA Author Manuscript
GC treatment is known to alter calcium metabolism. Treatment with GCs reduces the
gastrointestinal absorption of calcium and increases urinary excretion of calcium, which
leads to a calcium deficit [17, 31, 32]. Over time this calcium deficit and low serum ionized
calcium levels can stimulate PTH release; PTH then catalyzes 1-α- hydroxylase enzyme
production in the kidney, which in turn increases 1,25(OH)2 vitamin D3 levels, and this is
followed by gastrointestinal absorption of both calcium and phosphorus. If the calcium
deficit continues, gastrointestinal absorption of these minerals continues, resulting in
elevation of serum phosphorus that then stimulates the production of fibroblast growth
factor 23 (FGF23) by osteocytes in an attempt to lower serum phosphorus. FGF23 is a
hormonal factor that is produced primarily by osteocytes and reduces serum phosphorus and
1,25(OH)2 vitamin D3 levels by acting on the kidney through FGF receptors and Klotho
[33-35]. The production and circulating levels of FGF23 appear to be tightly regulated but
the mechanisms responsible are still under investigation.
The association between FGF23, osteocytes and mineralization has recently been explored
[36]. FGF23 serves as a phosphaturic factor synthesized by osteocytes and inhibits
1,25(OH)2 vitamin D3 production by the kidney to maintain the balance between phosphate
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 3
NIH-PA Author Manuscript
NIH-PA Author Manuscript
homeostasis and skeletal mineralization [37]. A recent in vitro study demonstrated that
overexpression of FGF23 suppressed osteoblast differentiation and matrix mineralization
[38]. Another study evaluated the proteins associated with osteocytes and bone
mineralization and found that FGF23 co-localized to the secondary spongiosa of trabecular
bone and areas of cortical bone where the osteocyte lacunar system was mature, suggesting
that FGF23 produced by osteocytes would then be part of the bone-renal axis that is central
to proper mineral metabolism [39, 40]. Elevated levels of serum FGF23 have been found in
individuals with autosomal hypophosphatemic rickets with mutations in DMP-1 (dentin
matrix protein-1) and other forms of rickets and chronic kidney disease exhibit elevated
levels of FGF23 despite normal calciuria [41, 42]. In contrast, mice with deletion of Klotho
developed elevated DMP-1, hyperphosphatemia and low FGF23 levels [43]. Overexpression
of FGF23 in primary rat calvaria cell cultures suppressed matrix mineralization [38]. In one
pilot study, increased FGF23 expression in ovine callus was associated with delayed fracture
healing [44]. It appears that changes in the production and local concentration of this
phosphaturic factor by the osteocyte may result in a reduction in osteocyte-driven mineral
metabolism, thereby compromising local bone strength [45-47]. In GC-treated mice, we
have observed a dose-dependent increase in serum FGF23, with a decrease in serum
phosphorus and 1,25(OH) vitamin D3, suggesting that GC use may influence mineral
metabolism through FGF23 [48]. The altered perilacunar mineralization around GC- treated
osteocytes may be secondary to increased FGF23 production. If this was the case, adequate
calcium supplementation or restricted phosphate dietary intake may prevent some of the
changes in the bone renal axis that occur with GC treatment.
GC induced bone loss clearly does affect the osteocyte
NIH-PA Author Manuscript
Osteocytes are terminally differentiated osteoblasts that lie below the bone surface and are
connected both to other osteocytes and the bone surface via dendritic processes that travel
through canaliculi [46, 49-53]. Our in vivo mouse studies showed that with GC treatment, a
number of the osteocyte lacunae were enlarged as measured by a modified atomic force
microscopy/scanning probe microscopy (AFM/SPM). Raman microscopy of the perilacunar
area of GC treated osteocytes revealed an enlarged area of demineralization, and AFM/SPM
revealed reduced elastic modulus around the enlarged osteocyte lacunae (nearly 40% below
the other bone matrix) in a number of the osteocytes [30]. A review of the literature
described that we had rediscovered “osteocytic osteolysis” a term initially used to described
enlarged lacunae in patients with hyperparathyroidism [54], immobilized rats [55], X-linked
hypophosphophatemic rickets, and lactation [56, 57]. Osteocyte lacunar architecture can also
be modified by poor mineralization when the bone is being formed, such as with renal
osteodystrophy which is distinctly different from “osteocytic osteolysis”. Our observation of
the removal of mineral by osteocytes (over weeks or months) would certainly be slower than
the bone removal by osteoclasts and may involve a different process. As we also found
reduced mineral and elastic modulus surrounding the GC treated osteocyte, we postulated
that the osteocyte in the presence of GCs modified the pre-existing mineral of its
surrounding matrix creating “osteocyte halos” as initially used by Heuck for the
pericanicular demineralization in X-linked hypophophatemic rickets [58].
To try to elucidate how the osteocyte could be changing its perilacunar matrix we performed
microarray analysis, RT-PCR and immunohistochemistry on selected genes and found with
GC (1.4 mg/kg/d, low dose) exposure for either 28 or 56 days, the expression of genes
associated with inhibition of bone formation (Dkk-1, SOST, Wif1), inhibition of
mineralization (FGF23) and lysosomes/matrix degradation (MMPs, cathepsin, proteinases)
were significantly higher compared to the placebo-control at day 0 (preliminary data). In
summary, we determined that GC induced changes in the osteocyte metabolism resulted in a
number of the osteocytes developing an increase in osteocyte lacunar size with perilacunar
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 4
NIH-PA Author Manuscript
demineralization, localized reduction in elastic modulus and production of proteins that
inhibit osteoblast formation and bone mineralization. However, we did not find much
evidence for either pro-apoptotic gene expression, or the presence of apoptotic osteocytes at
the low GC dose (1.4 mg/kg/d). In contrast, mice treated for 28 days with a higher GC dose
(2.4 mg/kg/d) had apoptotic osteocytes present in the cortical bone. Their changes to the
osteocyte in its localized microenvironment with exposure to low dose GC for 28 days
suggested to our research group that non-apoptotic programmed cell death, such as
autophagy, may also play a role in osteocyte's response to the GC induced stress.
Does autophagy explain the osteocyte response to GCs?
NIH-PA Author Manuscript
NIH-PA Author Manuscript
The autophagy pathway is one of the most important biologic processes that enable cells to
survive stress and helps to maintain cellular homeostasis by degrading damaged organelles
[59-62]. Autophagy is defined by the formation of autophagosomes, also known as
autophagic vacuoles that are lined by two membranes with the recruitment of microtubuleassociated protein light-chain 3 (LC3)-phosphatidylethanolamine conjugate (LC3-II) to the
autophagosomal membrane, a characteristic for autophagosome [63]. When the
autophagosomes fuse with the lysosomes and form autolysosomes, degradation occurs and
the amino acids or other small molecules are delivered to the cytoplasm for energy
production or recycling. If the cells are subjected to long periods of time under GC stress,
this may result in extensive recycling of damaged organelles that may lead to cell death or
apoptosis [60, 64, 65]. Autophagy can be inhibited by chloroquine (CQ) as it accumulates
within autophagosomes, and inhibits the fusion with lysosomes thereby preventing the
formation of autolysosomes. This reduction by chloroquine in the final phase of autophagy
that provides a pathway for the breakdown of proteins and removal of metabolic debris from
the cell, may augment apoptosis [66-68] or rescue osteocyte from cell death [69]. Recently
Xia et al reported that dexamethasone treatment of an osteocytic cell line, MLO-Y4 cells,
increased autophagy markers and the accumulation of autophagosome vacuoles as detected
by several standard approaches based on recently published guidelines including fluorescent
GFP-LC3 punctate dots, MDC fluorescence, LC3 lipidation and electron microscopy
imaging in addition to conventional acridine orange staining [70]. The enhancement of
autophagy was also validated in isolated primary osteocytes isolated from embryonic chicks
treated with dexamethasone and in vivo from osteocytes in bone from mice chronically
treated with prednisolone. In addition, gene microarray analysis of the cortical bone from
mice after 28 days of prednisolone treatment showed increased messenger RNA for several
autophagy markers including autophagy-related 16 like 2, autophagy-related 7, LC-3α and
LC-3β. Conversely, gene markers for pro-apoptosis were not significantly increased until
after a longer prednisolone treatment (56 days of chronic GC exposure) [24, 30]. We also
observed gene and protein expression for matrix proteolysis, including matrix
metalloproteinases, caspases and cathepsins increased in the cortical bones following GC
treatment [24]. Because the interior of a lysosome is strongly acidic, as it releases the
contents of its vacuole through autophagic flux into the microenvironment of the osteocyte,
it may induce matrix proteolysis, and demineralization of bone around the osteocyte that
over time may weaken both the localized bone tissue and whole bone strength [30].
We also found that dexamethasone reduced the number of metabolically normal osteocytes
and this effect was augmented when autophagy was inhibited [70]. This study implies that
autophagy could be an attempt by osteocytes to attenuate the effect of GC on osteocyte.
Autophagy is reported to act as a “double-edge sword” involved in both cell protection and
cell death [62, 71]. The cell protective function of autophagy is likely to occur under short or
moderate stress conditions. Our cell viability study showed that cells under the autophagic
state are very much alive and are likely under metabolic stress. Autophagy is a probable
mechanism by which osteocytes can repair damaged organelles or cell membranes.
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 5
NIH-PA Author Manuscript
However, higher, or more prolonged stress may result in an accumulation of
autophagosomes and cell death. Interestingly, after 56 days of a treatment with a relatively
high dose of prednisolone (5.6mg/kg/d) in mice, we studied the trabecular bone from the
vertebral bodies and observed increased apoptotic tunnel-positive labeling [21, 72].
Therefore, these studies demonstrate that low dose GC (less than 2.8 mg/kg/d in mice)
treatment resulted in osteocyte autophagy both in vitro and in vivo. During the initial period
of GC treatment, gene array studies revealed that the oxidative pathway [73-77] was
activated and simultaneously autophagy was activated suggesting that the osteocytes
responded with autophagy in an attempt to “save themselves”. However, with the prolonged
GC exposure or higher doses of GCs (5.6mg/kg/d), the cell may undergo apoptosis and or
necrosis. The outcome may be related to either the duration of GC treatment or the dose of
GC or both [78, 79]. It is possible that suppression or the prevention of autophagy may be a
promising new target in the prevention of GC induced bone fragility. If we find that low
dose GCs induce osteocyte autophagy that does not affect bone formation and whole bone
strength, as opposed to higher doses of GCs that induce osteocyte apoptotic induced bone
remodeling and increased fragility, this represent a major paradigm shift for the mechanism
responsible for GC-induced bone fragility. Treatments for GC-induced osteoporosis would
focus on the inhibition or augmentation of autophagy.
Why do GCs induce osteocyte autophagy
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Chronic GC treatment decreases bone formation and increases bone fragility that resembles
an accelerated aging process [12, 13]. We found that there was a dose-dependent decrease in
the activation of autophagy and anti-oxidative defense gene expression in the cortical bone
of mice. GCs at a lower dose increased anti-oxidative responsive as well as autophagic
pathways by an average of 30-fold (Figure 1A). In addition, the DNA damage and antioxidant pathways were significantly increased both at the lower GC dose and within the first
days of the GC exposure, suggesting that cells were being “over-activated” in response to
the initial GC treatment. Prolonged exposure or higher doses of GCs reduced both the
expression of genes encoding proteins that are anti-oxidants and the number of autophagic
osteocytes [80], supporting a relationship between the cells anti-oxidant ability and
autophagy following GC exposure [81, 82] (Figure 1B). Bone formation, measured by
serum osteocalcin and surface based histomorphometry was greatly reduced by chronic or
high dose GC treatments. MicroCT evaluation of trabecular structure showed reduced
trabecular bone volume and thickness, as compared to control mice [30, 83]. Similar
observations of surface and biochemical based turnover in clinical studies of GIOP have
been made including the reduction in trabecular bone volume, thickness and reduced bone
formation [12, 14-16]. In summary, GC treatment effects on bone formation were very
similar to that observed with aging in that GCs reduced the activation of anti-oxidant gene
expression, decreased bone marrow osteogenic potential, reduced autophagy and bone
formation. Based on these studies, we propose that modulation of the oxidative and
autophagic pathways may provide promising new targets for maintaining bone formation in
the presence of GCs or aging, which over time may preserve bone mass.
Therefore, these studies demonstrate that low dose GC treatment (1.4mg/kg/d for 28 days)
resulted in autophagy in osteocytes both in vitro and in vivo. However, with the continued
stress of prolonged GC exposure or higher doses of GCs (5.6mg/kg/d for 28 days), the cell
may undergo apoptosis and or necrosis. The outcome may be related to either the duration of
GC treatment or the dose of GC or both [78, 79]. Autophagy may provide a promising new
target in the prevention of GC induced bone fragility (Figure 2). If we find that low dose
GCs induce osteocyte autophagy that does not affect bone formation and whole bone
strength, as opposed to higher doses of GCs that induce osteocyte apoptotic induced bone
remodeling and increased fragility, this represents a major paradigm shift for the mechanism
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 6
responsible for GC-induced bone fragility. Treatments for GC-induced osteoporosis would
focus on the inhibition or augmentation of autophagy.
NIH-PA Author Manuscript
Acknowledgments
This work was funded by National Institute of Health grants nos. 1K12HD05195801 that are co-funded by National
Institute of Child Health and Human Development (NICHD), the Office of Research on Women's Health (ORWH),
the Office of Dietary Supplements (ODS) and the National Institute of Aging (NIA); R01 AR043052; K24
AR-048841 and 5R21AR57515.
References
NIH-PA Author Manuscript
NIH-PA Author Manuscript
1. Sebaldt RJ, Ioannidis G, Adachi JD, Bensen WG, Bianchi F, Cividino A, Gordon M, Kaminska E,
Scocchia T, Petrie A, Stephenson GF, Goldsmith CH. 36 month intermittent cyclical etidronate
treatment in patients with established corticosteroid induced osteoporosis. J Rheumatol. 1999;
26:1545–9. [PubMed: 10405943]
2. Adachi JD, Bensen WG, Brown J, Hanley D, Hodsman A, Josse R, Kendler DL, Lentle B,
Olszynski W, Ste-Marie LG, Tenenhouse A, Chines AA. Intermittent etidronate therapy to prevent
corticosteroid-induced osteoporosis. N Engl J Med. 1997; 337:382–7. [PubMed: 9241127]
3. Bolland MJ, Grey AB, Horne AM, Briggs SE, Thomas MG, Ellis-Pegler RB, Woodhouse AF,
Gamble GD, Reid IR. Annual zoledronate increases bone density in highly active antiretroviral
therapy-treated human immunodeficiency virus-infected men: a randomized controlled trial. J Clin
Endocrinol Metab. 2007; 92:1283–8. [PubMed: 17227801]
4. Saag KG, Shane E, Boonen S, Marin F, Donley DW, Taylor KA, Dalsky GP, Marcus R.
Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med. 2007; 357:2028–
39. [PubMed: 18003959]
5. Saag KG, Emkey R, Schnitzer TJ, Brown JP, Hawkins F, Goemaere S, Thamsborg G, Liberman
UA, Delmas PD, Malice MP, Czachur M, Daifotis AG. Alendronate for the prevention and
treatment of glucocorticoid-induced osteoporosis. Glucocorticoid-Induced Osteoporosis
Intervention Study Group. N Engl J Med. 1998; 339:292–9. [PubMed: 9682041]
6. Reid DM, Devogelaer JP, Saag K, Roux C, Lau CS, Reginster JY, Papanastasiou P, Ferreira A,
Hartl F, Fashola T, Mesenbrink P, Sambrook PN. Zoledronic acid and risedronate in the prevention
and treatment of glucocorticoid-induced osteoporosis (HORIZON): a multicentre, double-blind,
double-dummy, randomised controlled trial. Lancet. 2009; 373:1253–63. [PubMed: 19362675]
7. Caplan L, Saag KG. Glucocorticoids and the risk of osteoporosis. Expert Opin Drug Saf. 2009;
8:33–47. [PubMed: 19236216]
8. Van Staa TP, Laan RF, Barton IP, Cohen S, Reid DM, Cooper C. Bone density threshold and other
predictors of vertebral fracture in patients receiving oral glucocorticoid therapy. Arthritis Rheum.
2003; 48:3224–9. [PubMed: 14613287]
9. Mart G, Gomez R, Jodar E, Loinaz C, Moreno E, Hawkins E. Long-term follow-up of bone mass
after orthotopic liver transplantation: effect of steroid withdrawal from the immunosuppressive
regimen. Osteoporos Int. 2002; 13:147–50. [PubMed: 11905524]
10. Lane NE, Mroczkowski PJ, Hochberg MC. Prevention and management of glucocorticoid-induced
osteoporosis. Bull Rheum Dis. 1995; 44:1–4. [PubMed: 7550788]
11. Black DM, Kelly MP, Genant HK, Palermo L, Eastell R, Bucci-Rechtweg C, Cauley J, Leung PC,
Boonen S, Santora A, de Papp A, Bauer DC. Fracture Intervention Trial Steering C, Committee
HPFTS. Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur. N Engl J Med.
2010; 362:1761–71. [PubMed: 20335571]
12. Dalle Carbonare L, Arlot ME, Chavassieux PM, Roux JP, Portero NR, Meunier PJ. Comparison of
trabecular bone microarchitecture and remodeling in glucocorticoid-induced and postmenopausal
osteoporosis. J Bone Miner Res. 2001; 16:97–103. [PubMed: 11149495]
13. Weinstein RS. Glucocorticoid-induced osteoporosis. Rev Endocr Metab Disord. 2001; 2:65–73.
[PubMed: 11708295]
14. Dempster DW. Bone histomorphometry in glucocorticoid-induced osteoporosis. J Bone Miner Res.
1989; 4:137–41. [PubMed: 2658477]
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 7
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
15. Dalle Carbonare L, Chavassieux PM, Arlot ME, Meunier PJ. Bone histomorphometry in untreated
and treated glucocorticoid-induced osteoporosis. Front Horm Res. 2002; 30:37–48. [PubMed:
11892269]
16. Saag KG. Glucocorticoid use in rheumatoid arthritis. Curr Rheumatol Rep. 2002; 4:218–25.
[PubMed: 12010606]
17. Mazziotti G, Angeli A, Bilezikian JP, Canalis E, Giustina A. Glucocorticoid-induced osteoporosis:
an update. Trends Endocrinol Metab. 2006; 17:144–9. [PubMed: 16678739]
18. Jia D, O'Brien CA, Stewart SA, Manolagas SC, Weinstein RS. Glucocorticoids act directly on
osteoclasts to increase their life span and reduce bone density. Endocrinology. 2006; 147:5592–9.
[PubMed: 16935844]
19. Kim HJ, Zhao H, Kitaura H, Bhattacharyya S, Brewer JA, Muglia LJ, Ross FP, Teitelbaum SL.
Glucocorticoids suppress bone formation via the osteoclast. J Clin Invest. 2006; 116:2152–60.
[PubMed: 16878176]
20. Canalis E, Bilezikian JP, Angeli A, Giustina A. Perspectives on glucocorticoid-induced
osteoporosis. Bone. 2004; 34:593–8. [PubMed: 15050888]
21. Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC. Inhibition of osteoblastogenesis and
promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of
their deleterious effects on bone. J Clin Invest. 1998; 102:274–82. [PubMed: 9664068]
22. Ohnaka K, Tanabe M, Kawate H, Nawata H, Takayanagi R. Glucocorticoid suppresses the
canonical Wnt signal in cultured human osteoblasts. Biochem Biophys Res Commun. 2005;
329:177–81. [PubMed: 15721290]
23. Krishnan V, Bryant HU, Macdougald OA. Regulation of bone mass by Wnt signaling. J Clin
Invest. 2006; 116:1202–9. [PubMed: 16670761]
24. Yao W, Cheng Z, Busse C, Pham A, Nakamura MC, Lane NE. Glucocorticoid excess in mice
results in early activation of osteoclastogenesis and adipogenesis and prolonged suppression of
osteogenesis: a longitudinal study of gene expression in bone tissue from glucocorticoid-treated
mice. Arthritis Rheum. 2008; 58:1674–86. [PubMed: 18512788]
25. Ohnaka K, Taniguchi H, Kawate H, Nawata H, Takayanagi R. Glucocorticoid enhances the
expression of dickkopf-1 in human osteoblasts: novel mechanism of glucocorticoid-induced
osteoporosis. Biochem Biophys Res Commun. 2004; 318:259–64. [PubMed: 15110782]
26. Li J, Sarosi I, Cattley RC, Pretorius J, Asuncion F, Grisanti M, Morony S, Adamu S, Geng Z, Qiu
W, Kostenuik P, Lacey DL, Simonet WS, Bolon B, Qian X, Shalhoub V, Ominsky MS, Zhu Ke H,
Li X, Richards WG. Dkk1-mediated inhibition of Wnt signaling in bone results in osteopenia.
Bone. 2006; 39:754–66. [PubMed: 16730481]
27. Smith E, Frenkel B. Glucocorticoids inhibit the transcriptional activity of LEF/TCF in
differentiating osteoblasts in a glycogen synthase kinase-3beta-dependent and -independent
manner. J Biol Chem. 2005; 280:2388–94. [PubMed: 15537647]
28. Ito S, Suzuki N, Kato S, Takahashi T, Takagi M. Glucocorticoids induce the differentiation of a
mesenchymal progenitor cell line, ROB-C26 into adipocytes and osteoblasts, but fail to induce
terminal osteoblast differentiation. Bone. 2007; 40:84–92. [PubMed: 16949358]
29. O'Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA, Manolagas SC, Weinstein RS.
Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce
bone formation and strength. Endocrinology. 2004; 145:1835–41. [PubMed: 14691012]
30. Lane NE, Yao W, Balooch M, Nalla RK, Balooch G, Habelitz S, Kinney JH, Bonewald LF.
Glucocorticoid-treated mice have localized changes in trabecular bone material properties and
osteocyte lacunar size that are not observed in placebo-treated or estrogen-deficient mice. J Bone
Miner Res. 2006; 21:466–76. [PubMed: 16491295]
31. Boulos P, Ioannidis G, Adachi JD. Glucocorticoid-induced osteoporosis. Curr Rheumatol Rep.
2000; 2:53–61. [PubMed: 11123040]
32. Lukert BP. Glucocorticoid-induced osteoporosis. South Med J. 1992; 85:2S48–51. [PubMed:
1502614]
33. Yoshiko Y, Wang H, Minamizaki T, Ijuin C, Yamamoto R, Suemune S, Kozai K, Tanne K, Aubin
JE, Maeda N. Mineralized tissue cells are a principal source of FGF23. Bone. 2007; 40:1565–73.
[PubMed: 17350357]
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 8
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
34. Mirams M, Robinson BG, Mason RS, Nelson AE. Bone as a source of FGF23: regulation by
phosphate? Bone. 2004; 35:1192–9. [PubMed: 15542045]
35. Fukumoto S, Martin TJ. Bone as an endocrine organ. Trends Endocrinol Metab. 2009; 20:230–6.
[PubMed: 19546009]
36. Dupond JL, Mahammedi H, Prie D, Collin F, Gil H, Blagosklonov O, Ricbourg B, Meaux-Ruault
N, Kantelip B. Oncogenic osteomalacia: diagnostic importance of fibroblast growth factor 23 and
F-18 fluorodeoxyglucose PET/CT scan for the diagnosis and follow-up in one case. Bone. 2005;
36:375–8. [PubMed: 15777669]
37. Liu S, Tang W, Zhou J, Vierthaler L, Quarles LD. Distinct roles for intrinsic osteocyte
abnormalities and systemic factors in regulation of FGF23 and bone mineralization in Hyp mice.
Am J Physiol Endocrinol Metab. 2007; 293:E1636–44. [PubMed: 17848631]
38. Wang H, Yoshiko Y, Yamamoto R, Minamizaki T, Kozai K, Tanne K, Aubin JE, Maeda N.
Overexpression of fibroblast growth factor 23 suppresses osteoblast differentiation and matrix
mineralization in vitro. J Bone Miner Res. 2008; 23:939–48. [PubMed: 18282132]
39. Ubaidus S, Li M, Sultana S, de Freitas PH, Oda K, Maeda T, Takagi R, Amizuka N. FGF23 is
mainly synthesized by osteocytes in the regularly distributed osteocytic lacunar canalicular system
established after physiological bone remodeling. J Electron Microsc (Tokyo). 2009
40. Weber TJ, Liu S, Indridason OS, Quarles LD. Serum FGF23 levels in normal and disordered
phosphorus homeostasis. J Bone Miner Res. 2003; 18:1227–34. [PubMed: 12854832]
41. Liu S, Zhou J, Tang W, Menard R, Feng JQ, Quarles LD. Pathogenic role of Fgf23 in Dmp1-null
mice. Am J Physiol Endocrinol Metab. 2008; 295:E254–61. [PubMed: 18559986]
42. Juppner H, Wolf M, Salusky IB. FGF-23: More than a regulator of renal phosphate handling? J
Bone Miner Res. 2010; 25:2091–7. [PubMed: 20593414]
43. Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblatt KP, Baum MG, Schiavi S,
Hu MC, Moe OW, Kuro-o M. Regulation of fibroblast growth factor-23 signaling by klotho. J
Biol Chem. 2006; 281:6120–3. [PubMed: 16436388]
44. Goebel S, Lienau J, Rammoser U, Seefried L, Wintgens KF, Seufert J, Duda G, Jakob F, Ebert R.
FGF23 is a putative marker for bone healing and regeneration. J Orthop Res. 2009; 27:1141–6.
[PubMed: 19215029]
45. Bonewald L. Osteocytes as multifunctional cells. J Musculoskelet Neuronal Interact. 2006; 6:331–
3. [PubMed: 17185811]
46. Bonewald LF. Osteocytes as dynamic multifunctional cells. Ann N Y Acad Sci. 2007; 1116:281–
90. [PubMed: 17646259]
47. Sitara D, Kim S, Razzaque MS, Bergwitz C, Taguchi T, Schuler C, Erben RG, Lanske B. Genetic
evidence of serum phosphate-independent functions of FGF-23 on bone. PLoS Genet. 2008;
4:e1000154. [PubMed: 18688277]
48. Martin A, Liu S, David V, Li H, Karydis A, Feng JQ, Quarles LD. Bone proteins PHEX and
DMP1 regulate fibroblastic growth factor Fgf23 expression in osteocytes through a common
pathway involving FGF receptor (FGFR) signaling. FASEB J. 2011; 25:2551–62. [PubMed:
21507898]
49. Bonewald LF. Mechanosensation and Transduction in Osteocytes. Bonekey Osteovision. 2006;
3:7–15. [PubMed: 17415409]
50. Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, Yu X, Rauch F, Davis SI, Zhang S, Rios H,
Drezner MK, Quarles LD, Bonewald LF, White KE. Loss of DMP1 causes rickets and
osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet. 2006;
38:1310–5. [PubMed: 17033621]
51. Harris SE, Gluhak-Heinrich J, Harris MA, Yang W, Bonewald LF, Riha D, Rowe PS, Robling AG,
Turner CH, Feng JQ, McKee MD, Nicollela D. DMP1 and MEPE expression are elevated in
osteocytes after mechanical loading in vivo: theoretical role in controlling mineral quality in the
perilacunar matrix. J Musculoskelet Neuronal Interact. 2007; 7:313–5. [PubMed: 18094489]
52. Irie K, Ejiri S, Sakakura Y, Shibui T, Yajima T. Matrix mineralization as a trigger for osteocyte
maturation. J Histochem Cytochem. 2008; 56:561–7. [PubMed: 18319272]
53. Noble BS. The osteocyte lineage. Arch Biochem Biophys. 2008; 473:106–11. [PubMed:
18424256]
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 9
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
54. Belanger LF. Osteocytic osteolysis. Calcif Tissue Res. 1969; 4:1–12. [PubMed: 4310125]
55. Krempien B, Manegold C, Ritz E, Bommer J. The influence of immobilization on osteocyte
morphology: osteocyte differential count and electron microscopical studies. Virchows Arch A
Pathol Anat Histol. 1976; 370:55–68. [PubMed: 818789]
56. Mercer RR, Crenshaw MA. The role of osteocytes in bone resorption during lactation:
morphometric observations. Bone. 1985; 6:269–74. [PubMed: 4052275]
57. Qing H, A L, Dusevich V, Dallas M, Wysolmerski JJ, Bonewald LF. Osteocytic Perilacunar
Remodeling as a Significant Source of Calcium During Lactation. Journal Bone Miner Res. 2008;
23:S410.
58. Heuck F. Investigations of the mineral content of the osteocyte halos. Calcif Tissue Res. 1968;
(Suppl):81–81a. [PubMed: 5721099]
59. Eisenberg-Lerner A, Bialik S, Simon HU, Kimchi A. Life and death partners: apoptosis, autophagy
and the cross-talk between them. Cell Death Differ. 2009; 16:966–75. [PubMed: 19325568]
60. Hotchkiss RS, Strasser A, McDunn JE, Swanson PE. Cell death. N Engl J Med. 2009; 361:1570–
83. [PubMed: 19828534]
61. Martinet W, Agostinis P, Vanhoecke B, Dewaele M, De Meyer GR. Autophagy in disease: a
double-edged sword with therapeutic potential. Clin Sci (Lond). 2009; 116:697–712. [PubMed:
19323652]
62. Tsujimoto Y, Shimizu S. Another way to die: autophagic programmed cell death. Cell Death
Differ. 2005; 12(Suppl 2):1528–34. [PubMed: 16247500]
63. Tanida I, Ueno T, Kominami E. LC3 conjugation system in mammalian autophagy. Int J Biochem
Cell Biol. 2004; 36:2503–18. [PubMed: 15325588]
64. Cross CE, Halliwell B, Borish ET, Pryor WA, Ames BN, Saul RL, McCord JM, Harman D.
Oxygen radicals and human disease. Ann Intern Med. 1987; 107:526–45. [PubMed: 3307585]
65. Monastyrska I, Rieter E, Klionsky DJ, Reggiori F. Multiple roles of the cytoskeleton in autophagy.
Biol Rev Camb Philos Soc. 2009; 84:431–48. [PubMed: 19659885]
66. van Lierop AH, Witteveen JE, Hamdy NA, Papapoulos SE. Patients with primary
hyperparathyroidism have lower circulating sclerostin levels than euparathyroid controls. Eur J
Endocrinol. 2010; 163:833–7. [PubMed: 20817762]
67. Fernandez LA, Macsween JM. The spontaneous shedding of the lymphocyte receptor for sheep red
blood cells. Dev Comp Immunol. 1977; 1:385–94. [PubMed: 306355]
68. Gooi JH, Pompolo S, Karsdal MA, Kulkarni NH, Kalajzic I, McAhren SH, Han B, Onyia JE, Ho
PW, Gillespie MT, Walsh NC, Chia LY, Quinn JM, Martin TJ, Sims NA. Calcitonin impairs the
anabolic effect of PTH in young rats and stimulates expression of sclerostin by osteocytes. Bone.
2010; 46:1486–97. [PubMed: 20188226]
69. Rondanelli EG, Magliulo E, Carosi G, Dionisi D. Cytoplasmic shedding as a mode of formation of
lymphocyte- like blast cells by newt histiocytes. Acta Haematol. 1968; 40:67–74. [PubMed:
4974796]
70. Xia X, Kar R, Gluhak-Heinrich J, Yao W, Lane NE, Bonewald LF, Biswas SK, Lo WK, Jiang JX.
Glucocorticoid induced autophagy in osteocytes. J Bone Miner Res. 2010
71. Gurusamy N, Das DK. Is autophagy a double-edged sword for the heart? Acta Physiol Hung. 2009;
96:267–76. [PubMed: 19706370]
72. Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T. Prevention of
osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest. 1999;
104:1363–74. [PubMed: 10562298]
73. Orzechowski A, Ostaszewski P, Wilczak J, Jank M, Balasinska B, Wareski P, Fuller J Jr. Rats with
a glucocorticoid-induced catabolic state show symptoms of oxidative stress and spleen atrophy:
the effects of age and recovery. J Vet Med A Physiol Pathol Clin Med. 2002; 49:256–63.
[PubMed: 12126140]
74. Adcock IM, Ito K. Glucocorticoid pathways in chronic obstructive pulmonary disease therapy.
Proc Am Thorac Soc. 2005; 2:313–9. discussion 340-1. [PubMed: 16267355]
75. Jilka RL, Weinstein RS, Parfitt AM, Manolagas SC. Quantifying osteoblast and osteocyte
apoptosis: challenges and rewards. J Bone Miner Res. 2007; 22:1492–501. [PubMed: 17542686]
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 10
NIH-PA Author Manuscript
NIH-PA Author Manuscript
76. Komatsu F, Kudoh H, Kagawa Y. Evaluation of oxidative stress and effectiveness of low-dose
glucocorticoid therapy on exacerbation of chronic obstructive pulmonary disease. J Gerontol A
Biol Sci Med Sci. 2007; 62:459–64. [PubMed: 17452743]
77. Ong SL, Zhang Y, Whitworth JA. Reactive oxygen species and glucocorticoid-induced
hypertension. Clin Exp Pharmacol Physiol. 2008; 35:477–82. [PubMed: 18307745]
78. Planey SL, Abrams MT, Robertson NM, Litwack G. Role of apical caspases and glucocorticoidregulated genes in glucocorticoid-induced apoptosis of pre-B leukemic cells. Cancer Res. 2003;
63:172–8. [PubMed: 12517795]
79. Bonapace L, Bornhauser BC, Schmitz M, Cario G, Ziegler U, Niggli FK, Schafer BW, Schrappe
M, Stanulla M, Bourquin JP. Induction of autophagy-dependent necroptosis is required for
childhood acute lymphoblastic leukemia cells to overcome glucocorticoid resistance. J Clin Invest.
2010; 120:1310–23. [PubMed: 20200450]
80. Jia J, Yao W, Guan M, Dai W, Shahnazari M, Kar R, Bonewald L, Jiang JX, Lane NE.
Glucocorticoid dose determines osteocyte cell fate. FASEB J. 2011; 25:3366–76. [PubMed:
21705669]
81. Maiuri MC, Tasdemir E, Criollo A, Morselli E, Vicencio JM, Carnuccio R, Kroemer G. Control of
autophagy by oncogenes and tumor suppressor genes. Cell Death Differ. 2009; 16:87–93.
[PubMed: 18806760]
82. Tasdemir E, Maiuri MC, Orhon I, Kepp O, Morselli E, Criollo A, Kroemer G. p53 represses
autophagy in a cell cycle-dependent fashion. Cell Cycle. 2008; 7:3006–11. [PubMed: 18838865]
83. Weinstein RS, Jia D, Powers CC, Stewart SA, Jilka RL, Parfitt AM, Manolagas SC. The skeletal
effects of glucocorticoid excess override those of orchidectomy in mice. Endocrinology. 2004;
145:1980–7. [PubMed: 14715712]
NIH-PA Author Manuscript
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 11
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Figure 1.
RNA was extracted from the tibial cortical bone in mice that were treated with PL or various
doses of GC. RT-PCR gene arrays were performed for antioxidant defense (A). Correlations
between gene expressions associated with antioxidant and autophagy following GC
treatments (B).
Bone. Author manuscript; available in PMC 2014 June 01.
Yao et al.
Page 12
NIH-PA Author Manuscript
Figure 2. Proposed mechanisms for osteocyte autophagy and glucocorticoid-induced bone
fragility
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Bone. Author manuscript; available in PMC 2014 June 01.
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
clinical practice
Glucocorticoid-Induced Bone Disease
Robert S. Weinstein, M.D.
This Journal feature begins with a case vignette highlighting a common clinical problem.
Evidence supporting various strategies is then presented, followed by a review of formal guidelines,
when they exist. The article ends with the author’s clinical recommendations.
A 55-year-old woman with severe, persistent asthma requiring glucocorticoid therapy for the past 3 months presents for care. Her medications include albuterol, inhaled
fluticasone with salmeterol, montelukast, and prednisone (at a dose of 10 mg per
day). In the past, she received several intermittent courses of prednisone at a dose of
15 mg or more per day. Her weight is 45.5 kg (100 lb), and her height 157.5 cm (62 in.);
the body-mass index (the weight in kilograms divided by the square of the height in
meters) is 18. Scattered wheezing is heard during expiration. Findings on vertebral
percussion and rib-cage compression are unremarkable. How should her case be
evaluated and managed to minimize the risk of fractures?
The Cl inic a l Probl em
From the Division of Endocrinology and
Metabolism, the Center for Osteoporosis
and Metabolic Bone Diseases, the Department of Internal Medicine, and the Central
Arkansas Veterans Healthcare System at the
University of Arkansas for Medical Sciences,
Little Rock. Address reprint requests to
Dr. Weinstein at the Division of Endocrinology and Metabolism, University of Arkansas
for Medical Sciences, 4301 W. Markham St.,
Slot 587, Little Rock, AR 72205-7199, or at
weinsteinroberts@uams.edu.
N Engl J Med 2011;365:62-70.
Copyright © 2011 Massachusetts Medical Society.
An audio version
of this article
is available at
NEJM.org
Glucocorticoid therapy is the most common cause of secondary osteoporosis and the
leading iatrogenic cause of the disease.1-3 Often, the presenting manifestation is
fracture, which occurs in 30 to 50% of patients receiving long-term glucocorticoid
therapy.4 Glucocorticoid-induced osteoporosis predominantly affects regions of the
skeleton that have abundant cancellous bone, such as the lumbar spine and proximal
femur. In patients with glucocorticoid-induced osteoporosis, the loss of bone mineral density is biphasic; it occurs rapidly (6 to 12% loss) within the first year and
more slowly (approximately 3% loss yearly) thereafter.5 However, the risk of fracture
escalates by as much as 75% within the first 3 months after the initiation of therapy,
typically before there is a substantial decline in bone mineral density, suggesting
that there are adverse effects of glucocorticoids on bone that are not captured by
bone densitometry.6 Several large case–control studies have shown strong associations between exposure to glucocorticoids and the risk of fractures.4,6,7 An increase
in the risk of vertebral and hip fractures occurs rapidly after the start of treatment
and has been reported to occur with doses as small as 2.5 to 7.5 mg of prednisolone
per day (equivalent to 3.1 to 9.3 mg of prednisone per day). In a cohort study involving patients 18 to 64 years of age, continuous treatment with 10 mg of prednisone
per day for more than 90 days, for a variety of indications, as compared with no exposure to glucocorticoids, was associated with an increase in hip fractures by a factor of 7 and an increase in vertebral fractures by a factor of 17.7 Furthermore, an
increase in the risk of fractures has been reported with the use of inhaled glucocorticoids, as well as with alternate-day and intermittent oral regimens.3
Risk Factors
Risk factors associated with glucocorticoid-induced osteoporosis are listed in Table 1.
One factor whose importance has been recognized in the past decade is the activity
of the 11β-hydroxysteroid dehydrogenase (11β-HSD) system, a prereceptor modulator of glucocorticoid action.11 Two isoenzymes, 11β-HSD1 and 11β-HSD2, catalyze
62
n engl j med 365;1 nejm.org july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
clinical pr actice
conversion between hormonally active glucocorticoids (e.g., cortisol or prednisolone) and inactive
glucocorticoids (e.g., cortisone or prednisone).
The 11β-HSD1 enzyme is an activator, and the
11β-HSD2 enzyme is an inactivator. The increased
risk of fracture with glucocorticoid administration in the elderly may be explained in part by the
increase in 11β-HSD1 that occurs with aging. The
risk of glucocorticoid-induced osteoporosis appears
to be similar in men and women and among various ethnic groups.13
Pathogenesis
Histomorphometric studies in patients with glucocorticoid-induced osteoporosis consistently show
fewer osteoblasts and an increased prevalence of
osteocyte apoptosis, as compared with normal controls1,3,4,14,15 (Fig. 1). The increased osteocyte apoptosis is associated with decreases in vascular endothelial growth factor, skeletal angiogenesis, bone
interstitial fluid, and bone strength.16 Thus, glucocorticoid-induced apoptosis of osteocytes could
account for the loss of bone strength that occurs
before the loss of bone mineral density17 and the
observed mismatch between bone mineral density
and the risk of fracture in patients with glucocorticoid-induced osteoporosis.3,4 Gluco­corticoid excess also directly reduces osteoclast production,
but the lifespan of osteoclasts is prolonged, in
contrast to the decrease in the lifespan of osteoblasts. Therefore, with long-term therapy, the number of osteoclasts is usually maintained in the
normal range, whereas the number of osteoblasts
plummets and bone formation is substantially reduced.14,18 These histologic features contrast with
the increased bone formation and resorption that
are typical of postmenopausal osteoporosis or increased parathyroid hormone secretion and indicate that, contrary to previous assumptions, hypogonadism and secondary hyperparathyroidism are
not central to the pathogenesis of glucocorticoidinduced osteoporosis.19-22
S t r ategie s a nd E v idence
Evaluation
Physicians who prescribe glucocorticoids should
educate their patients about side effects and complications, including not only osteoporosis and
osteonecrosis but also cataracts and glaucoma,
Table 1. Risk Factors for Glucocorticoid-Induced Osteoporosis.*
Risk Factor
Evidence of a Contribution
Advanced age
Patients 60 to 80 years of age receiving glucocorticoid therapy, as compared
with patients 18 to 31 years of age, had a relative risk of vertebral fracture
of 26 and a shorter interval between initiation of treatment and the occurrence of fracture8
Low body-mass index (<24)†
Low body-mass index is a risk factor for glucocorticoid-induced osteoporosis
and probably fractures as well9
Underlying disease
Rheumatoid arthritis, polymyalgia rheumatica, inflammatory bowel disease,
chronic pulmonary disease, and transplantation are independent risk factors4
Prevalent fractures, smoking, excessive
alcohol consumption, frequent
falls, family history of hip fracture
All are independent risk factors for osteoporosis but have not been extensively studied in patients receiving glucocorticoids
Glucocorticoid receptor genotype
Individual glucocorticoid sensitivity may be regulated by polymorphisms in
the glucocorticoid receptor gene10
Increased 11β-HSD1 expression
11β-HSD1 expression increases with the age of the patient and with glucocorticoid administration11
High glucocorticoid dose (high current
or cumulative dose; long duration
of therapy)
Risk of fracture escalates with increased doses and duration of therapy;
­alternate-day or inhaled therapies also confer risks of glucocorticoidinduced osteoporosis4,12
Low bone mineral density
Glucocorticoid-induced fractures occur independently of a decline in bone mass,
but patients with very low bone mineral density may be at higher risk4,8
*11β-HSD1 denotes 11β-hydroxysteroid dehydrogenase 1.
†The body-mass index is the weight in kilograms divided by the square of the height in meters.
n engl j med 365;1 nejm.org july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
63
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Glucocorticoid excess
Osteoclasts
Osteoblasts
Decreased osteoblastogenesis
Decreased osteoclastogenesis
Early, transient increase in
• osteoclast survival
• cancellous osteoclasts
• bone resorption
Increased apoptosis
Osteocytes
Early and continual decrease in
• cancellous osteoblasts
• synthetic ability
• bone formation
Increased apoptosis
Decreased canalicular circulation
Decreased bone quality
Fracture
Osteonecrosis
Figure 1. Direct Effects of Glucocorticoids on Bone Cells.
Shown are the adverse skeletal changes that result from an excess of glucocorticoids and lead to osteoporosis and
osteonecrosis. The brown, condensed cells are apoptotic osteoblasts and osteocytes. Apoptotic osteocytes disrupt
the osteocyte–lacunar–canalicular network.
COLOR FIGURE
hypokalemia, hyperglycemia, hypertension, hyperlipidemia, weight gain, fluid retention, susceptibility to bruising, decreased resistance to infection,
impaired healing, myopathy, adrenal insufficiency,
and the glucocorticoid withdrawal syndrome.3 Patients receiving long-term glucocorticoid therapy
should wear medication identification jewelry.
Malpractice suits precipitated by a failure of physicians to document disclosure of the skeletal
complications to patients are not rare,23 yet these
complications are often ignored in clinicians’
discussions with patients about the use of glucocorticoids.13
Measurement of the patient’s height is important, since loss of height suggests the possibility
of prevalent vertebral fractures, with an associated
64
n engl j med 365;1
Version 2
05/16/11
increase in the risk of future fractures.
Laboratory
Author
Weinstein
Fig #
1 treatment
testing that should be performed
before
Title
is prescribed includes measurements
of serum
ME
CS
DE and calcium
25-hydroxyvitamin D, creatinine,
levArtist
JM
els (in addition to glucose, potassium,
and NOTE:
lipid
AUTHOR PLEASE
Figure has been redrawn and type has been reset
Please check carefully
levels). Since bone turnover after long-term
glucoIssue date 7/7/11
corticoid therapy is low, tests of biochemical
markers of bone metabolism are usually not helpful.4,24-27 Measurement of bone mineral density
and vertebral morphologic assessment or plain
films are often recommended to assess the patient
for vertebral fractures, but the disparity between
bone quantity and bone quality in glucocorticoidinduced osteoporosis makes measurements of bone
mineral density insensitive for identifying patients
at risk.2 However, measurements of bone mineral
nejm.org
july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
clinical pr actice
density may be useful for follow-up assessments
after an intervention. The use of the World Health
Organization fracture prevention algorithm (FRAX)
is not recommended in the case of patients with
glucocorticoid-induced osteoporosis, since it does
not take into account the current and cumulative dose of glucocorticoids and the duration of
therapy and underestimates the risk of glucocorticoid-induced fractures. Furthermore, bone
mineral density at the femoral neck is used in the
algorithm, but vertebral fractures are more common than hip fractures in patients with glucocorticoid-induced osteoporosis, and the inclusion
of the common risk factors for postmenopausal
osteoporosis in the algorithm may not be applicable to patients with glucocorticoid-induced osteoporosis.24
In patients treated with glucocorticoids who
report persistent hip, knee, or shoulder pain,
especially pain that occurs with joint movement
or that is associated with tenderness or reduced
range of motion, magnetic resonance imaging
should be performed to rule out osteonecrosis.23
The incidence of osteonecrosis among patients
who take glucocorticoids has been estimated to
be between 5 and 40%; higher doses of glucocorticoids and prolonged treatment are associated
with greater risk, although osteonecrosis may also
occur with short-term exposure to high doses,
including those administered intraarticularly (typically 40 to 80 mg of methylprednisolone) and in
the absence of osteoporosis. The mechanisms that
have been postulated for the development of osteonecrosis include fat embolism, vascular thrombosis, and osteocyte apoptosis.28,29
Treatment
All patients should receive adequate calcium supplementation (1200 mg per day in divided doses)
and adequate vitamin D supplementation (800 to
2000 U per day), but these precautions alone are
not sufficient to prevent fractures.4,24-27 Bisphosphonates are considered to be the first-line options for the treatment of glucocorticoid-induced
osteoporosis (Table 2)4; alendronate, risedronate,
and zoledronic acid are approved by the Food and
Drug Administration (FDA) for this indication, although there is controversy regarding the doses
and duration of glucocorticoid treatment that necessitate intervention to reduce the risk of fractures. In randomized, double-blind, placebo-controlled trials, including patients with a variety of
underlying diseases and irrespective of bone minn engl j med 365;1
eral density, alendronate and risedronate increased
bone mineral density at the lumbar spine and
femoral neck and reduced the relative risk of glucocorticoid-induced vertebral fractures by about
40%4,27,32,33; patients in these trials typically had
been taking 10 to 20 mg of prednisone daily or the
equivalent for at least 1 year before enrollment,
although the dose range and the duration of treatment varied widely. In another randomized trial
involving patients treated with glucocorticoids,
zoledronic acid was noninferior to risedronate in
increasing bone mineral density at the lumbar
spine.30
Alendronate decreases glucocorticoid-induced
apoptosis of osteocytes,34 which may play a role
in the preservation of bone strength.17 However,
glucocorticoids antagonize the effects of nitrogencontaining bisphosphonates in inducing apoptosis
of osteoclasts and inhibiting bone resorption.35,36
Perhaps as a consequence, bisphosphonates appear to be less effective in the protection of bone
mineral density in patients with glucocorticoidinduced osteoporosis than they are in patients
with other forms of osteoporosis. The average
percentage increase in bone mineral density at
the lumbar spine and femoral neck in patients
with glucocorticoid-induced osteoporosis after
treatment with alendronate at a dose of 10 mg per
day for 2 years was 3.9% and 0.6%, respectively
— considerably less than that reported in women
with postmenopausal osteoporosis (about 7% and
3.6%, respectively) or in men with osteoporosis
(7% and 2.5%, respectively), even though the latter
two groups were, on average, 10 years older than
the patients with glucocorticoid-induced osteoporosis.32,37,38 Moreover, the evidence to support
the use of bisphosphonates in the treatment of
patients with glucocorticoid-induced osteoporosis
is not as strong as the evidence for their use in the
treatment of patients with postmenopausal osteoporosis; the primary end point in the trials of
glucocorticoid treatment was bone mineral density rather than the occurrence of fractures, and
most trials were only 12 to 24 months in duration
and were not powered to study hip fractures.
A limitation of oral bisphosphonate therapy is
poor adherence to treatment — a well-recognized
problem even in the case of agents that are administered weekly or monthly. Administration of
zoledronic acid as a once-yearly infusion avoids
this problem and provides rapid skeletal protection. For protection from fractures in patients
who have received prolonged glucocorticoid thernejm.org
july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
65
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Table 2. Treatment of Glucocorticoid-Induced Osteoporosis.*
Intervention
Advantages
Disadvantages
Osteoclast inhibition reduces bone loss and reduces vertebral fractures in patients with glucocorticoid-induced osteoporosis; alendronate also prevents glucocorticoid-induced
osteocyte apoptosis; if glucocorticoid therapy
is discontinued, these drugs can be stopped
Antiresorptive agents do not directly address the decreased bone formation that is characteristic of glucocorticoid-induced bone disease and have not been
shown to reduce hip fractures; gastrointestinal side
­effects may occur; musculoskeletal discomfort, osteonecrosis of the jaw, uveitis, and atypical femoral fractures have occurred in rare cases; bisphosphonates
should be avoided in patients with creatinine clearance of ≤30 ml/min; patients have poor adherence to
oral therapy; as compared with intravenous therapy, a
longer time is required to obtain skeletal protection
Osteoclast inhibition reduces bone loss; as
compared with oral treatment, there is increased adherence to intravenous treatment
and more rapid onset of skeletal effects;
gastrointestinal side effects are unlikely
Acute-phase reaction (influenza-like syndrome) may occur
within 2 to 3 days and last 3 days or less, particularly
after first dose,30 but can be effectively managed with
acetaminophen or ibuprofen
Teriparatide, 20 µg/day,
given subcutaneously,
for 2 years, followed by
bisphosphonate treatment for as long as
­glucocorticoids are
­required
Teriparatide directly addresses the increase in
osteoblast and osteocyte apoptosis and the
decrease in osteoblast number, bone formation, and bone strength that are characteristic of glucocorticoid-induced osteo­
porosis and reduces vertebral fractures
Costs are greater than with oral or intravenous bisphosphonates; daily injections are required; response is reduced when teriparatide is given with high-dose glucocorticoids; it has not been studied in patients with elevated parathyroid hormone levels; adverse effects include mild hypercalcemia, headache, nausea, leg
cramps, and dizziness; caution must be taken in patients with preexisting nephrolithiasis; serum calcium
should be checked at least once 16 hours or more after
injection and oral calcium intake adjusted as needed31
Denosumab, 60 mg every
6 mo, subcutaneously
Denosumab is a potent inhibitor of osteoclasts, with ease of administration; it can
be stopped if glucocorticoids are discontinued; it can be used in patients with creatinine clearance of ≤30 ml/min
Denosumab does not address the reduced bone formation caused by glucocorticoid excess; hypocalcemia
and vitamin D deficiency must be treated before the
use of denosumab
Bisphosphonates
Alendronate, 10 mg/
day or 70 mg/wk,
taken orally
Risedronate, 5 mg/day
or 35 mg/wk, taken
orally
Zoledronic acid, 5 mg/yr,
given intravenously
*Alendronate, risedronate, zoledronic acid, and teriparatide have been approved by the Food and Drug Administration for the treatment of gluco­
corticoid-induced osteoporosis. In Europe, only once-daily oral bisphosphonate regimens, zoledronic acid, and teriparatide are approved for the
treatment of glucocorticoid-induced osteoporosis.
apy (e.g., 10 mg per day or more of prednisone
for longer than 90 days), intravenous bisphosphonate therapy may be preferable to oral therapy. On
the basis of estimates that the maximal absorption of alendronate when it is taken orally on an
empty stomach is about 0.7% and that the molar
potency of alendronate is lower than that of intravenous zoledronic acid by a factor of 10, it is estimated that a patient would need 90 days of treatment with alendronate at a dose of 70 mg per
week to receive a dose equivalent to 5 mg of zoledronic acid delivered in 15 minutes,39 although
these regimens have not been compared with
respect to rates of fracture in patients with glucocorticoid-induced osteoporosis. Since substantial
loss of bone mineral density has been observed in
patients who discontinue bisphosphonate therapy
while continuing to take glucocorticoids, it is usually recommended that bisphosphonate therapy be
66
continued for at least as long as the glucocorticoids are prescribed3,4,27,40; drug holidays are not
considered to be appropriate for patients who are
being treated with glucocorticoids.
In a 2-year, randomized, controlled, open-label
trial involving patients with osteonecrosis of the
femoral head, patients who received alendronate
therapy, as compared with those who received no
treatment, had decreased pain and delayed expansion of lesions and were less likely to need surgery.41 A prospective, observational study showed
that patients with osteonecrosis had a sustained
reduction in pain and improvement in ambulation
within months after the initiation of alendronate
therapy.42 In both studies, the most common cause
of osteonecrosis was the use of glucocorticoids.
Although bisphosphonates are useful in treating osteonecrosis of the hip, these drugs are
associated with the development of osteonecro-
n engl j med 365;1 nejm.org july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
clinical pr actice
sis of the jaw.43 Osteonecrosis of the jaw is characterized by exposed maxillofacial bone for at
least 8 weeks and typically occurs after a dental
extraction or other invasive procedure.43 Most reported cases of osteonecrosis of the jaw have occurred in patients with osteolytic breast cancer
or multiple myeloma who have received frequent,
high doses of intravenous bisphosphonates. In patients with osteoporosis treated with bisphosphonates, the estimated risk of osteonecrosis of the
jaw is 1 case per 10,000 to 100,000 patient-years.43
Before prescribing bisphosphonates, the clinician
should perform an oral examination and encourage
the patient to be examined by a dentist. Concurrent use of bisphosphonates and glucocorticoids
may slightly increase the risk of osteonecrosis of
the jaw. Bisphosphonates may also be associated
with atypical subtrochanteric femoral fractures,
but if there is an association, the risk is low (about
2 cases per 10,000 patient-years).44
An alternative to bisphosphonates is teriparatide, recombinant human parathyroid hormone
1-34, which is approved by the FDA for the treatment of glucocorticoid-induced osteoporosis. In
an 18-month, randomized, double-blind trial comparing teriparatide with alendronate in patients
with glucocorticoid-induced osteoporosis, teripar­
atide increased spinal bone mineral density over
a shorter period and to a greater extent than did
alendronate and also reduced vertebral fractures
by 90%.45 Daily subcutaneous administration of
parathyroid hormone prevents the expected glucocorticoid-induced increase in osteoblast and osteocyte apoptosis and decrease in osteoblast number,
bone formation, and bone strength.46 However, the
effect of teriparatide is somewhat compromised
by high-dose glucocorticoid therapy47; a lesser increase in bone mineral density at the lumbar spine
has been noted in patients taking more than 15 mg
of prednisone per day, as compared with those taking less than 5 mg per day. In addition, host factors
(e.g., the underlying illness and associated weight
loss, medications, reduced renal function, and low
levels of insulin-like growth factor I) may contribute to the diminished efficacy of teriparatide
in patients with glucocorticoid-induced osteoporosis, as compared with patients who have other
forms of osteoporosis.46 Disadvantages of teri­par­
atide include the cost and the risk of mild hypercalcemia (Table 2).31
Another potential treatment option is denos­
umab, a humanized monoclonal antibody to the
receptor activator of nuclear factor-κB ligand
(RANKL), which is approved by the FDA for the
prevention of vertebral, nonvertebral, and hip fractures in women with postmenopausal osteoporosis but is not currently approved for the treatment of glucocorticoid-induced osteoporosis.48
Administered as a subcutaneous injection every
6 months, denosumab rapidly decreases bone resorption. In a subgroup analysis of a 12-month,
randomized, placebo-controlled trial of denosu­
mab in patients receiving methotrexate treatment
for rheumatoid arthritis, patients receiving denos­
umab, prednisone (≤15 mg per day), and methotrexate had increases in bone mineral density at
the lumbar spine and total hip that were similar
to those in patients receiving methotrexate and
denosumab alone, and the rate of side effects
was similar in these groups.49 Denosumab may
have a role in treating patients taking glucocorticoids who have stable serum calcium levels and
who are not candidates for bisphosphonate or
teriparatide therapy because of side effects or a
history of renal insufficiency, although, as with
other agents, more data are needed regarding
the effect of denosumab on the risk of fracture.
Vertebroplasty and kyphoplasty are sometimes
performed to treat painful vertebral fractures, but
in controlled trials, these procedures have not been
found to be superior to sham procedures, and the
risks include leakage of the cement and an increase
in the risk of additional fractures in patients receiving glucocorticoids.50
A r e a s of Uncer ta in t y
More data are needed to predict the risk of fractures among patients taking glucocorticoids and
to establish clinical thresholds for intervention.2
Effective strategies are required to educate physicians about the importance of counseling patients who are receiving long-term glucocorticoid
therapy regarding the risk of fractures. Additional
studies are needed to determine the minimum dose
of glucocorticoids and duration of therapy that
warrant interventions to prevent fractures and to
better understand the ways in which other risk factors for bone loss should guide decisions regarding therapy. Some clinicians prescribe drugs for
the prevention of fractures for virtually every patient who requires glucocorticoid therapy and discontinue these drugs only when the glucocorticoids are discontinued, but the benefits, risks, and
cost-effectiveness of this strategy, as compared
with a more selective approach to the initiation of
n engl j med 365;1 nejm.org july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
67
The
n e w e ng l a n d j o u r na l
of
m e dic i n e
Table 3. Guidelines for Management of Glucocorticoid-Induced Osteoporosis.*
American College of
­Rheumatology24
National Osteoporosis
Foundation25
Royal College of
­Physicians of London26
Dose and duration of
glucocorticoid
treatment warranting pharmacologic
intervention†
≥7.5 mg/day for at least
3 months, but patients
at increased risk require
treatment with any dose
or duration
≥5 mg/day for at least
3 months
Any oral dose for at least
3 months in patients
≥65 years of age and
those with a prior fragility fracture
≥9.3 mg/day for at least
3 months
BMD threshold for
treatment if dose
and duration
qualify
Threshold to be based on
the FRAX algorithm in
addition to “higher daily
and cumulative dose,
­intravenous usage, and
declining BMD”
T score, −2.5, unless
patient is at high
risk on the basis of
a modified FRAX
model
T score, −1.5
T score, −1.0 to −1.5
Yearly BMD testing
recommended
Yes
Yes
Yes
Yes
Prevalent vertebral
fractures as justification for pharmacologic intervention
Yes
Yes
Yes
Yes
Variable
Belgian Bone Club27
Calcium and vitamin D
supplementation
1200–1500 mg of calcium
per day and 800–1000
units of vitamin D per
day for all patients‡
1200 mg of calcium per
day and 2000 units
of vitamin D per
day for all patients‡
Only for patients with low
calcium intake (<1 g/
day) or vitamin D deficiency (not defined)‡
For all patients
Pharmacologic intervention
Bisphosphonates; teriparatide reserved for patients
at highest risk
Bisphosphonates;
teriparatide only for
patients at high risk
Bisphosphonates as firstline options, followed
by teriparatide
Bisphosphonates
*BMD denotes bone mineral density, and FRAX fracture prevention algorithm.
†Glucocorticoid doses are given in prednisone equivalents.
‡The recommended calcium intake refers to the total daily intake (diet and supplements).
pharmacotherapy, have not been assessed. There
is no evidence that medication to prevent fractures
is needed with occasional dose-pack prescriptions,
annual short-term (e.g., 7 to 10 days) high-dose
intravenous or oral therapy (<1 g of cumulative
exposure), or replacement therapy for patients with
hypopituitarism, adrenal insufficiency, or congenital adrenal hyperplasia, provided that the replacement doses are not excessive.
Guidel ine s
Guidelines from the American College of Rheumatology, the National Osteoporosis Foundation, the
Royal College of Physicians, and the Belgium Bone
Club vary somewhat in their recommendations
(Table 3).24-27 The well-recognized early increase
in the risk of fracture associated with the use of
glucocorticoids, the lack of certainty with respect
to a known minimum dose and duration of glucocorticoid therapy that does not increase the risk
of fracture, and available trials showing increased
bone density (and in some cases reductions in
68
the rate of vertebral fracture) with antiresorptive
therapy in patients taking prolonged courses of
glucocorticoids (mostly at doses greater than 10
to 20 mg of prednisone per day) serve as the basis of the recommendations. However, high-quality data are lacking to determine the precise risk
of fractures associated with doses of prednisone
that are less than 5 to 7.5 mg daily or with intermittent regimens of glucocorticoids, as well as
the appropriate care of patients who are taking
these regimens.
C onclusions a nd
R ec om mendat ions
The woman described in the vignette, who is
slender, has been taking prednisone at a dose of
10 mg daily for 3 months, and previously received higher doses of glucocorticoids, is at considerable risk for glucocorticoid-induced osteo­
porosis. Other asthma therapies should be used
as efficiently as possible in an effort to taper the
prednisone. The assessment should include a mea-
n engl j med 365;1 nejm.org july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
clinical pr actice
surement of bone mineral density, and I would also
recommend a vertebral morphologic assessment
or plain films to look for vertebral fractures. Adequate intake of calcium and vitamin D should be
encouraged. Because of her long-term use of glucocorticoids, her age, and the low body-mass index,
if prednisone cannot be discontinued (or if she has
low bone mineral density or vertebral fractures),
she should be advised about therapies to reduce
her risk of fracture; bisphosphonates (alendronate,
risedronate, and zoledronic acid) and teriparatide
are approved by the FDA for these indications and
should be continued for as long as the patient requires prednisone. In the absence of data from
trials directly comparing the risk of fracture associated with the various therapies, the choice of
medication should take into account the cost, the
convenience of administration, and the side effects.
The more rapid onset of action with zoledronic acid
or teriparatide, as compared with oral bisphosphonates, is a potential advantage of these medications, but that advantage must be weighed against
the greater costs of those drugs and, in the case
of teriparatide, the need for daily injections.
Dr. Weinstein reports holding a patent for in vitro and in vivo
models for screening compounds to prevent glucocorticoid-induced
bone destruction. No other potential conflict of interest relevant to
this article was reported.
Disclosure forms provided by the author are available with the
full text of this article at NEJM.org.
I thank Drs. Stavros C. Manolagas, Charles A. O’Brien, and
Robert L. Jilka for their helpful discussions; Dr. Paula J. Anderson (Department of Pulmonary and Critical Care Medicine, University of Arkansas for Medical Sciences) for help with the case
vignette; and Drs. Paul D. Miller, Nelson B. Watts, Robert A.
Adler, and Henry G. Bone for reviewing an earlier version of the
manuscript.
References
1. Canalis E, Mazziotti G, Giustina A,
Bilezikian JP. Glucocorticoid-induced osteoporosis: pathophysiology and therapy.
Osteoporos Int 2007;18:1319-28.
2. Angeli A, Guglielmi G, Dovio A, et al.
High prevalence of asymptomatic vertebral fractures in post-menopausal women
receiving chronic glucocorticoid therapy:
a cross-sectional outpatient study. Bone
2006;39:253-9.
3. Weinstein RS. Glucocorticoid-induced
osteoporosis. In: Rosen C, ed. The ASBMR
primer on the metabolic bone diseases and
disorders of mineral metabolism. 7th ed.
Washington, DC: ASBMR, 2008:267-72.
4. Adler RA, Curtis JR, Saag K, Weinstein
RS. Glucocorticoid-induced osteoporosis.
In: Marcus R, Feldman D, Nelsen DA, Rosen
CJ, eds. Osteoporosis. 3rd ed. San Diego,
CA: Elsevier-Academic Press, 2008:1135-66.
5. LoCascio V, Bonucci E, Imbimbo B, et al.
Bone loss in response to long-term glucocorticoid therapy. Bone Miner 1990;8:39-51.
6. Van Staa TP, Laan RF, Barton IP, Cohen S, Reid DM, Cooper C. Bone density
threshold and other predictors of vertebral fracture in patients receiving oral
glucocorticoid therapy. Arthritis Rheum
2003;48:3224-9.
7. Steinbuch M, Youket TE, Cohen S.
Oral glucocorticoid use is associated with
an increased risk of fracture. Osteoporos
Int 2004;15:323-8.
8. Tatsuno I, Sugiyama T, Suzuki S, et al.
Age dependence of early symptomatic vertebral fracture with high-dose glucocorticoid
treatment for collagen vascular diseases.
J Clin Endocrinol Metab 2009;94:1671-7.
9. Thompson JM, Modin GW, Arnaud
CD, Lane NE. Not all postmenopausal
women on chronic steroid and estrogen
treatment are osteoporotic: predictors of
bone mineral density. Calcif Tissue Int
1997;61:377-81.
10. Russcher H, Smit P, van den Akker
ELT, et al. Two polymorphisms in the glucocorticoid receptor gene directly affect
glucocorticoid-regulated gene expression.
J Clin Endocrinol Metab 2005;90:5804-10.
11. Cooper MS, Rabbitt EH, Goddard PE,
Bartlett WA, Hewison M, Stewart PM. Osteoblastic 11β-hydroxysteroid dehydrogenase type 1 activity increases with age and
glucocorticoid exposure. J Bone Miner Res
2002;17:979-86.
12. van Staa TP, Leufkens HG, Cooper C.
Use of inhaled glucocorticoids and risk of
fractures. J Bone Miner Res 2001;16:581-8.
13. Curtis JR, Westfall AO, Allison JJ, et al.
Longitudinal patterns in the prevention of
osteoporosis in glucocorticoid-treated patients. Arthritis Rheum 2005;52:2485-94.
14. Weinstein RS, Jilka RL, Parfitt AM,
Manolagas SC. Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids:
potential mechanisms of their deleterious
effects on bone. J Clin Invest 1998;102:27482.
15. O’Brien CA, Jia D, Plotkin LI, et al.
Glucocorticoids act directly on osteoblasts
and osteocytes to induce their apoptosis
and reduce bone formation and strength.
Endocrinology 2004;145:1835-41.
16. Weinstein RS, Wan C, Liu Q, et al. Endogenous glucocorticoids decrease skeletal
angiogenesis, vascularity, hydration, and
strength in aged mice. Aging Cell 2010;9:
147-61.
17. Seeman E, Delmas PD. Bone quality
— the material and structural basis of
bone strength and fragility. N Engl J Med
2006;354:2250-61.
18. Jia D, O’Brien CA, Stewart SA, Manolagas SC, Weinstein RS. Glucocorticoids
act directly on osteoclasts to increase their
life span and reduce bone density. Endocrinology 2006;147:5592-9.
19. Weinstein RS, Jia D, Powers CC, et al.
The skeletal effects of glucocorticoid excess
override those of orchidectomy in mice. Endocrinology 2004;145:1980-7.
20. Pearce G, Tabensky DA, Delmas PD,
Baker HW, Seeman E. Corticosteroidinduced bone loss in men. J Clin Endocrinol Metab 1998;83:801-6.
21. Tauchmanovà L, Pivonello R, Di Somma C, et al. Bone demineralization and
vertebral fractures in endogenous cortisol
excess: role of disease etiology and gonadal status. J Clin Endocrinol Metab 2006;91:
1779-84.
22. Rubin MR, Bilezikian JP. The role of
parathyroid hormone in the pathogenesis
of glucocorticoid-induced osteoporosis: a
reexamination of the evidence. J Clin Endocrinol Metab 2002;87:4033-41.
23. Mankin HF. Nontraumatic necrosis of
bone (osteonecrosis). N Engl J Med 1992;
326:1473-9.
24. Grossman JM, Gordon R, Ranganath
VK, et al. American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoidinduced osteoporosis. Arthritis Care Res
(Hoboken) 2010;62:1515-26.
25. National osteoporosis foundation’s clinician’s guide to the prevention and treatment of osteoporosis. Washington, DC:
National Osteoporosis Foundation, 2009.
26. Bone and Tooth Society of Great Britain.
Guidelines on the prevention and treatment
of glucocorticoid-induced osteoporosis.
Lon­don: Royal Collage of Physicians, 2003.
27. Devogelaer J-P, Goemaere S, Boonen S,
et al. Evidence-based guidelines for the prevention and treatment of glucocorticoidinduced osteoporosis: a consensus document of the Belgian Bone Club. Osteoporos
Int 2006;17:8-19.
28. Calder JDF, Buttery L, Revell PA,
Pearse M, Polak JM. Apoptosis — a significant cause of bone cell death in osteonecrosis of the femoral head. J Bone Joint
Surg Br 2004;86:1209-13.
n engl j med 365;1 nejm.org july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
69
clinical pr actice
29. Weinstein RS, Nicholas RW, Manola-
gas SC. Apoptosis of osteocytes in glucocorticoid-induced osteonecrosis of the hip.
J Clin Endocrinol Metab 2000;85:2907-12.
30. Reid DM, Devogelaer J-P, Saag K, et al.
Zoledronic acid and risedronate in the
prevention and treatment of glucocorticoid-induced osteoporosis (HORIZON): a
multicentre, double-blind, double-dummy,
randomised controlled trial. Lancet 2009;
373:1253-63.
31. Miller PD. Safety of parathyroid hormone for the treatment of osteoporosis.
Curr Osteoporos Rep 2008;6:12-6.
32. Adachi JD, Saag KG, Delmas PD, et al.
Two-year effects of alendronate on bone
mineral density and vertebral fracture in
patients receiving glucocorticoids: a randomized, double-blind, placebo-controlled
extension trial. Arthritis Rheum 2001;44:
202-11.
33. Reid DM, Hughes RA, Laan RF, et al.
Efficacy and safety of daily risedronate in
the treatment of corticosteroid-induced
osteoporosis in men and women: a randomized trial. J Bone Miner Res 2000;15:
1006-13.
34. Plotkin LI, Weinstein RS, Parfitt AM,
Roberson PK, Manolagas SC, Bellido T.
Prevention of osteocyte and osteoblast
apoptosis by bisphosphonates and calcitonin. J Clin Invest 1999;104:1363-74.
35. Weinstein RS, Roberson PK, Manolagas
SC. Giant osteoclast formation and longterm oral bisphosphonate therapy. N Engl J
Med 2009;360:53-62.
36. Weinstein RS, Chen JR, Powers CC, et al.
Promotion of osteoclast survival and antag-
onism of bisphosphonate-induced osteoclast apoptosis by glucocorticoids. J Clin
Invest 2002;109:1041-8.
37. Liberman UA, Weiss SR, Bröll J, et al.
Effect of oral alendronate on bone mineral density and the incidence of fractures
in postmenopausal osteoporosis. N Engl J
Med 1995;333:1437-43.
38. Orwoll E, Ettinger M, Weiss S, et al.
Alendronate for the treatment of osteoporosis in men. N Engl J Med 2000;343:604-10.
39. Fleisch H. Bisphosphonates in bone
disease: from the laboratory to the patient.
4th ed. San Diego, CA: Academic Press,
2000:42.
40. Emkey R, Delmas PD, Goemaere S, et al.
Changes in bone mineral density following
discontinuation or continuation of alendronate therapy in glucocorticoid-treated patients: a retrospective, observational study.
Arthritis Rheum 2003;48:1102-8.
41. Lai K-A, Shen W-J, Yang C-Y, Shao C-J,
Hsu J-T, Lin R-M. The use of alendronate
to prevent early collapse of the femoral
head in patients with nontraumatic osteonecrosisd: a randomized clinical study.
J Bone Joint Surg Am 2005;87:2155-9.
42. Agarwala S, Shah S, Joshi VR. The use
of alendronate in the treatment of avascular necrosis of the femoral head: followup to eight years. J Bone Joint Surg Br
2009;91:1013-8.
43. Khosla S, Burr D, Cauley J, et al. Bis­
phosphonate-associated osteonecrosis of
the jaw: report of a task force of the American Society for Bone and Mineral Research.
J Bone Miner Res 2007;22:1479-91.
44. Black DM, Kelly MP, Genant HK, et al.
Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur. N Engl J
Med 2010;362:1761-71.
45. Saag KG, Shane E, Boonen S, et al.
Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med
2007;357:2028-39.
46. Weinstein RS, Jilka RJ, Roberson PK,
Manolagas SC. Intermittent parathyroid
hormone administration counteracts the
adverse effects of glucocorticoids on osteoblast and osteocyte viability, bone formation, and strength in mice. Endocrinology 2010;151:2641-9.
47. Devogelaer J-P, Adler RA, Recknor C,
et al. Baseline glucocorticoid dose and
bone mineral density response with teripar­
atide or alendronate therapy in patients
with glucocorticoid-induced osteoporosis.
J Rheumatol 2010;37:141-8.
48. Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal
women with osteoporosis. N Engl J Med
2009;361:756-65. [Erratum, N Engl J Med
2009;361:1914.]
49. Dore RK, Cohen SB, Lane NE, et al.
Effects of denosumab on bone mineral
density and bone turnover in patients
with rheumatoid arthritis receiving concurrent glucocorticoids or bisphosphonates. Ann Rheum Dis 2010;69:872-5.
50. Syed MI, Patel NA, Jan S, Shaikh A,
Grunden B, Morar K. Symptomatic refractures after vertebroplasty in patients with
steroid-induced osteoporosis. AJNR Am J
Neuroradiol 2006;27:1938-43.
Copyright © 2011 Massachusetts Medical Society.
images in clinical medicine
The Journal welcomes consideration of new submissions for Images in Clinical
Medicine. Instructions for authors and procedures for submissions can be found
on the Journal’s Web site at NEJM.org. At the discretion of the editor, images that
are accepted for publication may appear in the print version of the Journal,
the electronic version, or both.
70
n engl j med 365;1 nejm.org july 7, 2011
The New England Journal of Medicine
Downloaded from nejm.org on August 3, 2013. For personal use only. No other uses without permission.
Copyright © 2011 Massachusetts Medical Society. All rights reserved.
The FASEB Journal • Research Communication
Glucocorticoid dose determines osteocyte cell fate
Junjing Jia,*,1 Wei Yao,*,1 Min Guan,* Weiwei Dai,* Mohammad Shahnazari,*
Rekha Kar,† Lynda Bonewald,‡ Jean X. Jiang,† and Nancy E. Lane*,2
*Department of Medicine, University of California at Davis Medical Center, Sacramento, California,
USA; †Department of Biochemistry, University of Texas Health Science Center, San Antonio, Texas,
USA; and ‡School of Dentistry, Department of Oral Biology, University of Missouri at Kansas City,
Kansas City, Missouri, USA
In response to cellular insult, several
pathways can be activated, including necrosis, apoptosis, and autophagy. Because glucocorticoids
(GCs) have been shown to induce both osteocyte
apoptosis and autophagy, we sought to determine
whether osteocyte cell fate in the presence of GCs
was dose dependent by performing in vivo and in
vitro studies. Male Swiss-Webster mice were treated
with slow-release prednisolone pellets at 1.4, 2.8, and
5.6 mg/kg/d for 28 d. An osteocyte cell line, MLO-Y4
cells, was treated with various doses of dexamethasone. We found that GC treatments dose dependently decreased activation of antioxidant-, autophagy-, and antiapoptosis-focused RT-PCR gene
pathways in mouse cortical bone. The activation of
antioxidant genes was correlated with autophagy
gene expression after the GC treatments. The presence of osteocyte autophagy, as detected by immunostaining for LC3, increased ⬃50% at the distal
femur cortical bone region but not at trabecular bone
region at the 1.4 and 2.8 mg/kg/d GC dose levels.
The number of apoptotic osteocytes was increased at
the cortical bone region by ⬃40% initially observed
at the 2.8 mg/kg/d dose level. In addition, the
presence of the osteocyte autophagy was associated
with an increased protein level of cathepsin K in vitro
after the GC treatments. In summary, we found that
GC treatment dose-dependently decreased antioxidant gene expression, with lower GC doses activating
autophagy, whereas a higher dose increased apoptosis. These data suggest that autophagy may provide a
mechanism for osteocytes to survive the stress after
GC exposure and provide further insight into how
GCs alter bone cell fate.—Jia, J., Yao, W., Guan, M.,
Dai, W., Shahnazari, M., Kar, R., Bonewald, L., Jiang,
J. X., Lane, N. E. Glucocorticoid dose determines
osteocyte cell fate. FASEB J. 25, 3366 –3376 (2011).
www.fasebj.org
ABSTRACT
Key Words: osteoporosis 䡠 apoptosis 䡠 autophagy 䡠 antioxidant
䡠 MLO-Y4 cell 䡠 LC3
chronic GCs will have an osteoporotic fracture; baseline data from randomized clinical trials report the
prevalence in vertebral fracture is nearly 30% (1– 4).
Patients treated with GCs may require the treatment
for a long period of time, thereby increasing their
risk of fractures. Clinical studies of GC-treated subjects observed that the initiation of GC treatment is
associated with a change in bone metabolism. In
turn, this leads to a rapid reduction in bone mass at
sites rich in trabecular bone, e.g., the vertebrae and
femur, with incident vertebral fracture risk elevated
within 1 yr of initiation of GC treatment (5–7).
However, the loss of trabecular mass and architecture
does not explain the increase in fracture risk in
individuals treated with GCs, because these GCtreated subjects frequently experience fractures with
higher bone mineral density values than do women
with postmenopausal osteoporosis (6). Therefore, a
more comprehensive understanding of the biology of
GC-induced bone loss could empower clinicians to
effectively prevent and treat this disease.
Osteocytes, the most abundant type of cells in
bone, are buried in the bone matrix and are now
known to contribute bone mineral homeostasis (8).
Osteocytes are connected to one another and to the
bone surface. Osteocyte lacunae have been reported
to change size in clinical situations when there is a
calcium deficiency, including with lactation, GC
treatment, hypophosphatemic rickets, and prolonged estrogen deficiency (9 –12). The increase in
osteocyte lacunae size in these metabolic states may
occur because of an insufficient trabecular and endocortical bone surface area for osteoclasts to reabsorb bone and maintain serum calcium balance when
calcium is in high demand (13). For example, in the
case of lactation, osteocyte lacunae are enlarged
during lactation and return to the normal size postlactation, presumably after the calcium demand from
lactation is diminished (10). Osteocytes synthesize
and secrete a number of “osteocytic” specific pro1
Glucocorticoids (GCs) are frequently used in
clinical medicine to treat noninfectious inflammatory diseases. Epidemiological studies show that 50%
of patients with rheumatoid arthritis treated with
3366
These authors contributed equally to this work.
Correspondence: Department of Medicine, 4800 2nd
Ave., Suite 2600, Sacramento, CA 95817, USA. E-mail:
nelane@ucdavis.edu
doi: 10.1096/fj.11-182519
2
0892-6638/11/0025-3366 © FASEB
teins, such as dentin matrix acidic phosphoprotein,
matrix extracellular phosphoglycoprotein, and fibroblast growth factor 23, that contribute to the regulation of both calcium and phosphorus metabolism
(14 –18), and the synthesis of these proteins by the
osteocyte has been associated with changes in the
perilacunar mineral around the osteocyte. However,
it is unclear whether GC would affect osteocyte cell
fates and would alter localized perilacunar mineralization changes around the osteocyte and whole
bone strength.
Aging and glucocorticoid treatments are associated
with accumulations of destroyed proteins, damaged
nucleic acids, and accumulated oxygen radicals (19 –
21). Cells rely on autophagy, the only known intracellular degradative mechanism, to remove the dysfunctional organelles and/or oxidized proteins (22–24).
The autophagic process is also activated when the cell is
under stress, as an attempt to survive (25, 26). Once the
autophagic process is initiated, parts of the cytoplasm
and intracellular organelles are sequestered within
autophagic vacuoles, which are eventually delivered to
lysosomes for bulk degradation (27). Although the
process of autophagy can preserve cell viability as a
survival strategy, it can also lead to a self-destructive
process, resulting in programmed cell death with excessive activation of this self-degrading system (28, 29).
Although autophagy may prolong cell survival under
stressful conditions, it is an inefficient process, and over
time cells accumulate metabolic debris, which results in
a decline in both cell and organ functions (30). Endogenous GCs, secreted by the adrenal glands, are essential
in the body’s ability to respond to stress. GCs are known
to impair the enzymatic antioxidant defenses or directly
induce oxidative stress in various tissues (31–36) and
are associated with cell fate in a number of disease
states. In lymphoid malignancies, Laane et al. (37)
reported that dexamethasone (Dex) induced lymphoid
cell death through the induction of autophagy before
apoptosis. The induction of osteocyte apoptosis was
thought to be the primary mechanism for GC-induced
osteoporosis and changes in bone quality (38 – 42). We
recently reported that prolonged GC treatment in mice
resulted in osteocyte autophagy. Inhibition of autophagy with 3-methyladenine, an inhibitor of endogenous protein degradation, led to osteocyte apoptosis
(19, 43). Based on these data, we hypothesized that
autophagy is one of the pathways in which osteocytes
respond to GC exposure. The purpose of this investigation was to further characterize the dose-dependent
effects of GC-induced osteocyte cell fates in vivo and
in vitro.
MATERIALS AND METHODS
Animals and experimental procedures
Three-month-old male Swiss-Webster mice were obtained
from Charles River, Inc. (San Jose, CA, USA). The mice were
GLUCOCORTICOIDS ON OSTEOCYTE AUTOPHAGY
maintained on commercial rodent chow (22/5 Rodent Diet;
Teklad, Madison, WI, USA) with 0.95% calcium and 0.67%
phosphate, available ad libitum. Mice were housed in a room
that was maintained at 20°C with a 12-h light-dark cycle. The
mice were randomly assigned to 4 experimental groups of
6 –16 animals/group. Slow-release pellets (Innovative Research of America, Sarasota, FL, USA) of prednisolone
(GC) were implanted as follows: group 1, the control
group, was implanted with a placebo pellet (PL); group 2
was implanted with a 2.5 mg/60 d slow-release GC pellet,
which is equivalent to 1.4 mg/kg/d for 28 d; group 3 was
implanted with a 5 mg/60 d slow-release GC pellet, which
is equivalent to 2.8 mg/kg/d for 28 d; and group 4 was
implanted with a 10 mg/60 d slow-release GC pellet, which
is equivalent to 5.6 mg/kg/d for 28 d. At 48 h before the
mice were sacrificed, a fluorescent-conjugated monoclonal
antibody for the autophagy marker, LC3 (LC3-5F10; 30
g/mouse; NanoTools, San Diego, CA, USA) was injected
into 3 mice in each of the 4 experimental groups to label
the autophagic osteocytes. All animals were treated according to the U.S. Department of Agriculture animal care
guidelines with the approval of the University of California
at Davis Committee on Animal Research.
Biochemical methods
Serum levels for cortisol (R&D Systems, Minneapolis, MN,
USA), osteocalcin (Biomedical Technology, Stoughton, MA,
USA), and cathepsin K (Alpco, Salem, NH, USA) were
measured in duplicate by ELISA, following the manufacturers’ instructions. The within-run variations in our laboratory
are between 4 and 6%, and between-run variations are ⬃5%,
which allow us to determine true changes between treatment
groups (43–50).
Osteocyte culture and experiments
MLO-Y4 cells were cultured on collagen-coated (rat tail
collagen type I, 0.15 mg/ml) surfaces (BD, Franklin Lakes,
NJ, USA) and were grown in phenol red-free ␣-modified
essential medium (␣-minimal essential medium) supplemented with 2.5% FBS and 2.5% bovine calf serum (Invitrogen, Carlsbad, CA, USA) and incubated in a 5% CO2 incubator at 37°C as described previously. The cells were treated
with Dex (Sigma-Aldrich Corp., St. Louis, MO, USA) at 10⫺8
to 10⫺5 M for 24 h (19, 51).
For the cell GFP-LC3 transfection experiments, the cells
were transfected with the GFP-LC3 vector for 48 h. The cells
were then treated with 10⫺8 to 10⫺6 M doses of Dex for 24 h,
fixed with 4% paraformaldehyde, and examined under an
Olympus BX61 motorized reflected fluorescence microscope
(Olympus, Tokyo, Japan) with an AMCA filter (excitation,
350 nm; emission, 460 nm) for DAPI and FITC filter (excitation, 480 nm; emission, 535 nm) using SlideBook4.1 software
(Intelligent Imaging Innovations, Denver, CO, USA). Autophagic cells were quantified by counting cells exhibiting
GFP-LC3 punctate staining.
To evaluate the colocalization of the LC3 and lysosomes,
MLY-O4 cells were plated on coverslips in a 12-well plate at
1 ⫻ 104 cells/cm2. After 24 h of plating, the cells were
transfected with 1 g of GFP-LC3 using 5 l of lipofectamine
in optimum I reduced serum medium (Invitrogen). Both
GFP-LC3 and lipofectamine were diluted in optimum I reduced serum medium in two separate tubes to a final volume
of 100 l. After 5 min of incubation, GFP-LC3 and lipofectamine were mixed together in one tube and were incubated for 15 min at room temperature. Then the mixture of
DNA-lipofectamine was added to cells dropwise in 1 ml of
3367
optimum I medium, and the plates were swirled gently and
incubated in a 37°C incubator. After 3 h of transfection,
medium was replaced with full-growth medium. After 24 h of
transfection, cells were treated with 10⫺8 to 10⫺6 M Dex in
1% serum (FBS⫹bovine calf serum) phenol red-free medium
for 24 h. Serum starvation was used as a positive control for
autophagy (52, 53). The cells were then incubated with 1 M
LysoSensor Blue (Invitrogen) that was added directly to the
treatment medium. The medium was removed after 30 min of
incubation with LysoSensor Blue. Cells were washed once
with fresh medium, and live cell images were taken to
visualize the colocalization of GFP-LC3 puncta and the lysosomes.
dant, autophagy, or apoptosis pathways, housekeeping genes,
and no primer or cDNA controls. Detailed gene information
can be found online (http://www.sabiosciences.com/RTPCR.
php). We excluded genes that had values of Ct ⱖ 35 because
low expression levels can result in large fold changes, but the
differences were not significant. After the exclusions, we
reported 80 test genes in the autophagy RT-PCR gene array
(see Fig. 2) and genes that were significantly different from
PL after GC treatments for antioxidant and antiapoptosis
(Tables 1 and 2).
Real-time RT-PCR
The right distal femurs were decalcified in 10% EDTA for 2 wk
and embedded in paraffin. Sections (4 m) were prepared for
immunohistochemistry using primary antibodies against the
autophagy protein LC3-phosphatidylethanolamine conjugate
antibody (LC3B antibody; Cell Signaling Technology, Danvers,
MA, USA). LC3 detection was performed using a Vectastain
ABC system (Vector Laboratories, Burlingame, CA, USA). Sections were counterstained with methyl green. Apoptosis was
determined using an In Situ Fluorescein Cell Death Detection
Kit (Roche, Indianapolis, IN, USA) following the manufacturer’s instructions. Results are presented as the percentage of
the positive stained osteocytes/trabecular or cortical bone volume 0.5 to 3 mm distal to the growth plate at the distal femurs.
Total RNA was obtained from the tibiae or from MLO-Y4 cell
cultures. For the tibiae, joint and bone marrow was removed,
and total RNA was isolated using a modified two-step purification protocol with homogenization (PRO250 Homogenizer, 10 mm⫻105-mm generator; PRO Scientific Inc., Oxford, CT, USA) in TRIzol (Invitrogen) followed by
purification over an RNeasy column (Qiagen, Valencia, CA,
USA). The antioxidation autophagy and antiapoptosis focus
RT-PCR gene pathway arrays were purchased from SABioscience (Frederick, MD, USA). Each pathway gene array has a
preselected panel of 96 genes, which are related to antioxiTABLE 1.
Immunohistochemistry
Antioxidant gene expression after GC treatment (fold change from PL)
Symbol
Description
1.4 mg
2.8 mg
5.6 mg
Als2
Apc
Apoe
Aqr
Cat
Ctsb
Cygb
Fancc
Fmo2
Gab1
Gpx3
Gpx5
Hbq1
Ift172
Il19
Il22
Kif9
Lpo
Mb
Noxa1
Noxo1
Nxn
Park7
Prdx1
Prnp
Recql4
Slc41a3
Sod1
Sod2
Sod3
Tpo
Txnip
Txnrd3
Ucp3
Amyotrophic lateral sclerosis 2 (juvenile) homolog (human)
Adenomatosis polyposis coli
Apolipoprotein E
Aquarius
Catalase
Cathepsin B
Cytoglobin
Fanconi anemia, complementation group C
Flavin containing monooxygenase 2
Growth factor receptor bound protein 2-associated protein 1
Glutathione peroxidase 3
Glutathione peroxidase 5
Hemoglobin, 1
Intraflagellar transport 172 homolog (Chlamydomonas)
Interleukin 19
Interleukin 22
Kinesin family member 9
Lactoperoxidase
Myoglobin
NADPH oxidase activator 1
NADPH oxidase organizer 1
Nucleoredoxin
Parkinson disease (autosomal recessive, early onset) 7
Peroxiredoxin 1
Prion protein
RecQ protein-like 4
Solute carrier family 41, member 3
Superoxide dismutase 1, soluble
Superoxide dismutase 2, mitochondrial
Superoxide dismutase 3, extracellular
Thyroid peroxidase
Thioredoxin interacting protein
Thioredoxin reductase 3
Uncoupling protein 3 (mitochondrial, proton carrier)
12.87
12.29
67.28
10.31
13.32
10.06
79.92
12.59
84.42
23.55
56.67
50.16
68.71
14.09
44.51
77.14
42.55
35.09
36.01
33.46
31.01
19.21
11.58
9.62
9.21
7.69
16.12
12.59
15.07
30.87
129.29
34.52
9.39
42.34
8
4.04
26.44
8.86
7.65
8.17
26.05
7.14
13.15
15.79
31.72
42.9
67.88
10.67
17.21
37.96
40.83
34.72
29.65
36.66
16.23
9.78
8.62
3.56
7.12
5.07
8.71
6.93
6.45
23.55
59.1
24
4.17
14.71
7.53
7.11
29.19
6.58
5.29
5.76
23.79
4.55
29.47
13.08
21.45
14.53
38.25
5.79
21.33
36.59
23.56
27.84
15.8
12.56
-6.91
11.74
8.41
5.98
6.73
4.36
8.48
9.52
6.8
11.67
41.94
15.81
3.29
13.25
All genes expressed significantly from PL (P⬍0.05).
3368
Vol. 25
October 2011
The FASEB Journal 䡠 www.fasebj.org
JIA ET AL.
TABLE 2.
Antiapoptotic gene expression after GC treatment (fold change from PL)
Symbol
Api5
Bag1
Bag3
Bcl2
Bcl2l1
Bcl2l10
Bcl2l2
Birc2
Birc3
Bnip2
Bnip3
Casp2
Cflar
Dad1
Tsc22d3
Fas
Il10
Lhx4
Mcl1
Nfkb1
Nme5
Pak7
Pim2
Polb
Prdx2
Rnf7
Sphk2
Tnf
Cd40lg
Zc3hc1
Description
1.4 mg
2.8 mg
5.6 mg
Apoptosis inhibitor 5
Bcl2-associated athanogene 1
Bcl2-associated athanogene 3
B-cell leukemia/lymphoma 2
Bcl2-like 1
Bcl2-like 10
Bcl2-like 2
Baculoviral IAP repeat-containing 2
Baculoviral IAP repeat-containing 3
BCL2/adenovirus E1B interacting protein 2
BCL2/adenovirus E1B interacting protein 3
Caspase 2
CASP8 and FADD-like apoptosis regulator
Defender against cell death 1
TSC22 domain family, member 3
Fas (TNF receptor superfamily member 6)
Interleukin 10
LIM homeobox protein 4
Myeloid cell leukemia sequence 1
Nuclear factor of light polypeptide gene enhancer in B-cells 1, p105
Nonmetastatic cells 5, protein expressed in (nucleoside-diphosphate kinase)
P21 (CDKN1A)-activated kinase 7
Proviral integration site 2
Polymerase (DNA directed), beta
Peroxiredoxin 2
Ring finger protein 7
Sphingosine kinase 2
Tumor necrosis factor
CD40 ligand
Zinc finger, C3HC type 1
1.37
⫺1.31
1.18
1.24
⫺1.11
3.79
1.04
1.03
1.05
⫺1.23
2.26
⫺1.28
3.14
4.22
⫺1.16
3.84
3.53
2.40
3.03
⫺1.36
5.02
2.72
2.84
1.02
⫺1.21
1.64
⫺1.77
2.45
2.02
⫺1.37
⫺2.33
⫺1.12
⫺1.41
⫺1.64
⫺1.14
⫺1.60
⫺1.38
⫺1.79
1.05
1.11
⫺1.43
⫺1.30
⫺1.11
⫺2.59
⫺1.50
⫺2.61
⫺6.28
⫺2.86
⫺1.23
⫺1.96
⫺2.02
⫺2.47
⫺1.71
1.48
1.36
⫺3.53
1.20
⫺1.12
⫺6.15
⫺1.43
⫺2.15
⫺3.70
⫺1.94
⫺3.05
⫺3.15
⫺8.97
⫺3.36
⫺1.90
⫺1.76
⫺2.18
⫺1.36
⫺1.88
⫺3.60
⫺10.18
⫺2.27
⫺2.81
⫺35.84
⫺3.86
1.06
⫺5.45
⫺5.36
⫺3.50
⫺5.34
⫺4.64
⫺3.17
⫺7.89
⫺19.57
⫺3.93
⫺10.40
⫺2.14
A Bioquant imaging analyzing system (Bioquant, Nashville, TN,
USA) was used for the measurements.
RESULTS
Western blot
Dose-dependent effects of GC on serum chemistry
values, bone turnover, and strength
The cells were lysed in RIPA buffer with homogenization.
The bone lysates or cell lysates were resolved on SDS-PAGE
and electrophoretically transferred to polyvinylidene difluoride membranes. Membranes were incubated with primary antibodies that included -actin (1:2000; Santa Cruz
Biotechnology, Santa Cruz, CA, USA), anti-LC3 (1:1000;
Cell Signaling Technology) or anti-cathepsin K (Cell Signaling Technology) followed by species-specific horseradish peroxidase secondary antibody. Anti-LC3 antibody recognizes both LC3-I, which is cytoplasmic and LC3-II that
binds to the autophagic membranes. Immunoreactive materials were detected by chemiluminescence (Pierce Laboratories,
Thermo Fisher Scientific, Rockford, IL, USA), imaged with a
Kodak Gel Logic 100 Digital Imaging System, and quantitated by
Kodak 1D 3.6 image analysis software (Eastman Kodak, Rochester, NY, USA).
The serum cortisol level was not changed at the 1.4
mg/kg/d GC dose level but increased by ⬎200% at
the 2.8 mg/kg/d dose level and 600% at the 5.6
mg/kg/d dose level after 28 d of treatment. Bone
formation, measured by the serum osteocalcin level
or surface-based mineralizing surface at the distal
femurs, decreased nonsignificantly by ⬃10 – 40% at a
1.4 mg/kg/d GC dose level and 40 – 60% at the two
higher GC dose levels (P⬍0.05). The maximum
vertebral compressive stress was significantly lowered
at the 5.6 mg/kg/d GC dose level compared with that
for PL (Fig. 1).
Excess GC induced an osteocyte autophagy in vivo
Statistical analysis
Group means and sds were calculated for all outcome
variables. The nonparametric Kruskal-Wallis test was used
to determine the differences between the groups. The
2-tailed Spearman correlation test was used to determine
the association between the activation (fold changes from
PL) for all genes in the antioxidation, autophagy, or
antiapoptosis gene arrays (version 12; SPSS Inc., Chicago,
IL, USA).
GLUCOCORTICOIDS ON OSTEOCYTE AUTOPHAGY
To evaluate the dynamic and integrative nature of GCs
on osteocyte stress response and cell fate, we obtained
RNA from the long bones (tibiae, n⫽6/group) of mice
treated with PL or 3 doses of GCs for 28 d and
performed real time RT-PCR gene arrays for antioxidants, autophagy, and antiapoptosis. We found that GC
dose-dependently decreased the activation of oxidative
stress responsive gene expressions (Table 1). For exam3369
Figure 1. Three-month-old male Swiss-Webster mice were treated with a placebo
pellet (PL), or a 2.5 mg/60 d (1.4 mg/kg/d), 5 mg/60 d (2.8 mg/kg/d), or 10
mg/60 d (5.6 mg/kg/d) slow-release prednisolone pellet. A, B) Mice were
sacrificed at d 28, and serum was collected for cortisol (A) and osteocalcin (B).
C, D) Bone histomorphometry was performed on the distal femur; surface-based
bone turnover was assessed by mineralizing surface (MS/BS; C), and the sixth
lumbar vertebra was tested for compressive strength (max stress; D). n ⫽
6 –16/group. aP ⬍ 0.05 vs. PL; bP ⬍ 0.05 vs. GC 1.4 mg; cP ⬍ 0.05 vs. GC 2.8 mg.
ple, the expression of superoxide dismutase (Sod) 1,
soluble increased ⬃12-fold at the 1.4 mg/kg/d dose
level and increased 6- and 9-fold, respectively, at the 2.8
and 5.6 mg/kg/d GC dose levels, Sod2 (mitochondrial)
increased 15 fold at the 1.4 mg/kg/d dose level and
increased 6-fold at the 2.8 and 5.6 mg/kg/d GC dose
levels; and Sod3 (extracellular) increased 30-fold at the
1.4 mg/kg/d GC dose level and increased 23- and
11-fold, respectively, at 2.8 and 5.6 mg/kg/d GC dose
levels. GC at the 1.4 mg/kg/d dose level activated a
number of genes that are associated with autophagy by
an average increase of 20- to 30-fold from the PL
treatment and by ⱕ10-fold at the 2.8 mg/kg/d dose
level and was similar to PL (1-fold) at the 5.6 mg/kg/d
dose level (Fig. 2A). Activation of the antioxidant gene
pathway was positively correlated with activation of the
autophagic gene array, especially at the 1.4 mg/kg/d
GC dose level (Fig. 2B). For example, the expressions
of autophagy-related proteins (Atg) 12 and 7, both of
which are essential for the formation of double-membrane vesicles and autophagosomes, increased 23- and
42-fold, respectively, at the 1.4 mg/kg/d GC dose level
and increased 14- and 11-fold, respectively, at the 2.8
mg/kg/d GC dose but did not differ from PL at the 5.6
mg/kg/d GC dose level. In contrast, the expression of
genes associated with antiapoptosis increased by ⱕ5fold from PL at the 1.4 mg/kg/d GC group but were
significantly decreased by an average of ⫺1 to ⫺6-fold
in the 2.8 mg/kg/d GC dose group and ⫺2 to ⫺30-fold
in the 5.6 mg/kg/d GC dose group (Table 2). For
example, the expression of B-cell leukemia/lymphoma 2 (Bcl2) was not changed at the 1.4 mg/kg/d
GC dose level but decreased 1.6-fold at the 2.8
mg/kg/d GC dose and decreased 3-fold at the 5.6
mg/kg/d GC dose level; the expression of IL-10
increased 3-fold at the 1.4 mg/kg/d GC dose level
but decreased 6-fold at the 2.8 mg/kg/d GC dose and
decreased 35-fold at the 5.6 mg/kg/d GC dose level.
There was no significant correlation between the
3370
Vol. 25
October 2011
activation of antioxidant and antiapoptosis genes. In
addition, there was no significant correlation between activation of autophagy and antiapoptosis
genes (data not shown).
GC treatment at all three doses did not increase the
percentage of LC3⫹ osteocytes in the trabecular bone
region (Fig. 3A). However, GC treatment increased
autophagic osteocytes in the cortical bone region of the
distal femurs at the 1.4 and 2.8 mg/kg/d (Fig. 3B)
measured by immunohistochemical staining against
LC3 (Fig. 3C) or by injecting the fluorescent-conjugated LC3 antibody (LC3-5F10) into the mice (Fig.
3D). GC exposure did not significantly change osteocyte apoptosis in the trabecular bone region of the
distal femur at either dose level but increased apoptotic
osteocytes significantly in the cortical bone region at
the 2.8 and 5.6 mg/kg/d GC dose levels (Fig. 4).
GC increased osteocyte autophagy and cathepsin K
secretion in vitro
To determine the dose-dependent effect of GCs on
autophagy in vitro, osteocytic MLO-Y4 cells were transfected by GFP-LC3 for 48 h and then were treated with
various concentrations of Dex (10⫺8 to 10⫺6 M) for
24 h. GFP-LC3 was diffusely distributed in the cytoplasm in the absence of Dex (control). In contrast,
treatment with Dex increased the number of GFP-LC3
puncta, indicating that LC3 was recruited and aggregated in the cytoplasm (Fig. 5A). Increased colocalization of GFP-LC3 was seen, and lysosomes were observed
accumulating in the cytoplasm in Dex-treated cells,
especially in 10⫺7 to 10⫺6 M Dex (Fig. 5B). Western
blot confirmed the increase in GFP-LC3-II levels after
Dex treatment at all doses starting from the lowest dose
(10⫺8 M), and the maximal response was seen at 10⫺7
M Dex (Fig. 5C, D). The enzyme for matrix metabolism,
cathepsin K, was increased in the MLO-Y4 cells (Fig. 5C,
The FASEB Journal 䡠 www.fasebj.org
JIA ET AL.
Figure 2. RNA was extracted from the tibial shafts of PL- or GC-treated mice at d 28. RT-PCR gene arrays for antioxidants and autophagy
were performed. A) RT-PCR data are expressed as fold changes from the PL-treated mice. Approximately 70% of the autophagic genes
expressed were significantly different from the those for PL. B) Correlation of fold changes from placebo between antioxidant and
autophagy gene expression was performed on the same samples for all three GC doses or at the 1.4 mg/kg/d dose level. n ⫽ 6/group.
D) treated with Dex, as well as in the culture medium,
which was most significant at the 10⫺7 M dose level
(Fig. 5E). Interestingly, when the MLO-Y4 cells were
treated with Dex (10⫺8 to 10⫺5 M) and evaluated for
the antioxidant gene expressions, we did not find that
Dex treatment in vitro activated the antioxidant pathway significantly (data not shown).
DISCUSSION
After 28 d of low-dose GC treatment in mice, there was
significant activation of the autophagy pathway and
increased osteocyte autophagy in the cortical bone
region of the distal femur that were significantly differGLUCOCORTICOIDS ON OSTEOCYTE AUTOPHAGY
ent from placebo treatment. A decreased antiapoptosis
response and osteocyte apoptosis were observed at the
cortical bone region after the higher-dose GC treatment.
Weinstein et al. (38, 42) reported that reduced bone
formation in GC-treated mice was associated with increased apoptosis of osteoblasts and osteocytes. Plotkin
et al. (54) also reported in vitro evidence of apoptosis of
osteocytes exposed to GCs using 3 separate assays
(trypan blue exclusion, nuclear morphology, and annexin V/propidium iodine ratios by FACS analysis) to
accurately confirm that there was osteocyte apoptosis
present (54). However, these investigations were performed before reagents were available to assess the
3371
Figure 3. Distal femurs from PL- or GC-treated mice were embedded in paraffin at d 28. A, B) Numbers of LC3⫹ osteocytes
present in a defined trabecular bone area (A) or cortical bone area (B) were calculated. C) Immunohistochemical staining was
performed using an anti-LC3 antibody (LC3⫹ cells were stained in red; red arrows). D) Autophagic osteocytes were also
quantitated by injecting fluorescent-conjugated monoclonal antibody for LC3 (LC3–5F10; green arrows) into mice at 48 h
before sacrifice. n ⫽ 8/group, 3 sections/animal were analyzed. aP ⬍ 0.05 vs. PL.
presence of autophagy. Our study evaluated the dose
response of osteocytes to GCs and found that osteocyte
apoptosis increased after a higher dose of GC at
the cortical bone region. Our results (43) are similar to
those reported by Weinstein et al. (38, 42), who also
reported that in male mice treated with higher doses of
GCs nearly 20% of the osteocytes at the cortical bone
region of the tibiae had undergone apoptosis. These
investigators also demonstrated that the increased osteocyte apoptosis was significantly associated with a
reduction in whole bone strength.
In additional to apoptosis, we found that autophagic
osteocytes were observed in the cortical bone region of
the lumbar vertebral bodies in mice that had received
56 d of GC treatment (19). The autophagy pathway is
one of the most important biological processes that
Figure 4. Presence of apoptosis
in the trabecular and cortical
bone of the right distal femurs in
mice treated with PL or GC. Apoptosis was determined by in situ
fluorescence TUNEL staining.
Apoptotic osteocytes (A, yellow
arrows) in both the trabecular
bone (B) and cortical bone (C)
regions were measured. n ⫽
8/group. aP ⬍ 0.05 vs. PL.
3372
Vol. 25
October 2011
The FASEB Journal 䡠 www.fasebj.org
JIA ET AL.
Figure 5. In vitro assessment of autophagy in ML0-Y4 cells treated with GCs. A) MLO-Y4 cells were cultured on collagen-coated
plates and grown in phenol red-free ␣-modified essential medium supplemented with 2.5% FBS and 2.5% bovine calf serum.
Cells were transfected with GFP-LC3 for 48 h before they were treated with Dex at 10⫺8 to 10⫺6 M and LysoSensor for 24 h. A
few autophagosomes (GFP-LC3⫹ dots, yellow arrows) were seen in the cytoplasm in the control (Con) cells. Treatment with Dex
increased in GFP-LC3⫹ vacuoles (⫻100 original view for all images). B) GFP-LC3⫹ vacuoles (stained in green) and lysosomes
(stained in blue) were increased in 10⫺7 to 10⫺6 M Dex dose levels. C) Western blots of LC3 and cathepsin K (CtsK) contents
in MLO-Y4 cells treated with DEX, as indicated, for 24 h. D) Arbitrary units of Western blots in C for LC3-II/actin, LC3-II/LC3-I,
and cathepsin K (CatK)/actin. LC3-I protein level was not changed by Dex treatment, whereas LC3-II protein level was increased
after treatment with 10⫺8–10⫺6 M Dex. Maximum increase was observed with 10⫺7 and 10⫺6 M Dex. Cathepsin K levels were
also increased after Dex treatment, measured by Western blot in cell lysates. E) LC3⫹ cell numbers. Percentage of LC3⫹ cells
was measured by ELISA in the culture medium. F) Cathepsin K levels measured by ELISA in the culture medium. Cathepsin K
levels were increased after Dex treatment. Each experiment was repeated 4 times. aP ⬍ 0.05 vs. control; bP ⬍ 0.05 vs. 10⫺8 M
Dex.
enables the cells to survive stress and starvation and
helps to maintain cellular homeostasis by degrading
damaged organelles (22, 25, 28, 55). The hallmark of
autophagy is the formation of autophagosomes, also
known as autophagic vacuoles that are lined by two
membranes with the recruitment of LC3-II to the
autophagosomal membranes, a characteristic for autophagosomes, whereas LC3-I remains in the cytoplasm
(56). Aging is associated with an increase in the intracellular overabundance of oxidative products, including reactive oxygen species (e.g., oxygen ions and free
radicals) and increased defense mechanisms for oxidative stress such as glutathione (GSH), thioredoxin, and
GSH peroxidase, which convert the peroxides to harmless materials, and the expressions of superoxide dismutase, the antioxidant enzymes in bone tissues (57–
62). Likewise, GCs also activate the oxidative pathway
and accelerate the aging process in bone tissue (34, 36,
GLUCOCORTICOIDS ON OSTEOCYTE AUTOPHAGY
63– 65). GC treatment in vitro did not activate the
antioxidant pathway but significantly increased the
overall stress level in vivo in mice by increasing
the systemic circulating cortisol levels. On the basis of
our data, it appears that antioxidative responses were
provoked by GC-induced stress, and the osteocytes may
have responded with autophagy. An increased LC3-II
protein level and autophagic osteocytes were observed
primarily in the cortical bone regions. This autophagic
attempt to “survive” the insult from the GC exposure
may be successful if the dose is low. However, with the
increasing doses of GCs, the cells’ antioxidant defenses
were overwhelmed, and the ability of the osteocyte to
survive was reduced, which could then direct the cells
to apoptosis. Other investigators have suggested that
osteocyte cell fate may be related to the dose of GC (66,
67). Our data clearly demonstrate the dynamics of the
osteocyte cell fate with different GC doses within the
3373
cortical bone. The lack of osteocyte response in the
trabecular bone regions may due to the fact that
trabecular and cortical bone have different remodeling
rates, and these two bone compartments have different
responses to various stimuli, such as immobilization
and exercise (68 –72). The life spans of trabecular bone
osteocytes and cortical bone osteocytes are also different: cortical bone osteocytes live significantly longer,
and this may help to explain the differing response to
GC treatment (73). The activation of the autophagic
gene pathway and osteocyte autophagy was significantly
increased when the cells or mice were treated with a low
dose of GC. The higher doses of GC activated the gene
pathway for apoptosis and osteocyte apoptosis was then
significantly increased.
During the initial autophagic process, cells may be able
to remain viable during periods of metabolic stress (26,
74, 75). However, in the later stage of autophagy, the
digestion of autophagic materials involves the fusion of
autophagosomes with lysosomes to form autolysosomes or
the degradative autophagic vacuole. This catabolic process releases cathepsins and other hydrolases from the
lysosomal lumen into the cytosol or, if the autolysosome
fuses with the plasma membrane, into the surrounding
tissue (76, 77). This extrusion of the contents of the
phagolysosomes is in some degree similar to the virus
shedding from a lymphocyte (78, 79). We observed increased colocalization of GFP-LC3 and lysosomes in osteocytes treated with Dex as well as increased cathepsin K
levels both in the osteocytes and in the circulation. Our
findings suggest that GC increased the release of the
cathepsins and other hydrolases secreted into the perilacunar bone matrix. Over time, the localized release
of cathepsin K with other hydrolases from the lysosome
may change the perilacunar matrix composition, and over
time it may also change the localized material properties
of the bone. Therefore, osteocyte cell fate through autophagy may have a different effect on the localized
perilacunar composition and bone quality than death by
apoptosis. Histological sections of osteocyte death by
apoptosis generally have only empty lacunae. However,
the apoptotic cell may send signals to the bone cell
surface to activate osteoclast-mediated bone remodeling.
Unlike necrosis and possibly autophagy, the cellular debris from apoptosis does not appear to damage the bone
tissue and may not alter the perilacunar matrix. On the
other hand, osteocyte autophagy may induce the autolysosomal secretion of degradative enzymes and hydrolases into the perilacunar region that may eventually
affect localized bone mineralization after chronic GC
exposure (43).
In summary, GC treatment dose dependently decreased antioxidant, autophagy, and antiapoptosis responses. A low GC dose induced osteocyte autophagy,
and higher GC doses induced osteocyte apoptosis,
principally in the cortical bone. Although GC-induced
autophagy has been reported, the dose response of
autophagy and apoptosis within the cortical bone is
novel, and additional studies are now warranted to
elucidate these findings and determine whether inter3374
Vol. 25
October 2011
ventions directed to alter autophagy or the inhibition
of cathepsin K may be a useful approach to reduce
GC-induced bone fragility.
The authors thank Dr. Frank Chuang (Center for Biophotonics and Science Technology, University of California at
Davis Medical Center) for generously providing GFP-tagged
LC3 expression vector and photographing the cells. This
work was funded by U.S. National Institutes of Health grants
1K12-HD05195801 (cofunded by the National Institute of
Child Health and Human Development, the Office of Research on Women’s Health, the Office of Dietary Supplements, and the National Institute of Aging), R01-AR04305207, K24-AR048841, 5R21-AR57515-2, and P01-AR46798 (to L
F.B. and J.X.J), and Welch Foundation grant AQ-1507 (to
J.X.J.).
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
Saag, K. G. (2002) Glucocorticoid use in rheumatoid arthritis.
Curr. Rheumatol. Rep. 4, 218 –225
Saag, K. G., Shane, E., Boonen, S., Marin, F., Donley, D. W.,
Taylor, K. A., Dalsky, G. P., and Marcus, R. (2007) Teriparatide
or alendronate in glucocorticoid-induced osteoporosis. N. Engl.
J. Med. 357, 2028 –2039
Lane, N. E., Sanchez, S., Modin, G. W., Genant, H. K., Pierini,
E., and Arnaud, C. D. (1998) Parathyroid hormone treatment
can reverse corticosteroid-induced osteoporosis. Results of a
randomized controlled clinical trial. J. Clin. Invest. 102, 1627–
1633
Lane, N. E., Sanchez, S., Modin, G. W., Genant, H. K., Pierini,
E., and Arnaud, C. D. (2000) Bone mass continues to increase at
the hip after parathyroid hormone treatment is discontinued in
glucocorticoid-induced osteoporosis: results of a randomized
controlled clinical trial. J. Bone Miner. Res. 15, 944 –951
Dalle Carbonare, L., Arlot, M. E., Chavassieux, P. M., Roux, J. P.,
Portero, N. R., and Meunier, P. J. (2001) Comparison of
trabecular bone microarchitecture and remodeling in glucocorticoid-induced and postmenopausal osteoporosis. J. Bone. Miner.
Res. 16, 97–103
Van Staa, T. P., Laan, R. F., Barton, I. P., Cohen, S., Reid, D. M.,
and Cooper, C. (2003) Bone density threshold and other
predictors of vertebral fracture in patients receiving oral glucocorticoid therapy. Arthritis Rheum. 48, 3224 –3229
Chiodini, I., Carnevale, V., Torlontano, M., Fusilli, S., Guglielmi,
G., Pileri, M., Modoni, S., Di Giorgio, A., Liuzzi, A., Minisola, S.,
Cammisa, M., Trischitta, V., and Scillitani, A. (1998) Alterations
of bone turnover and bone mass at different skeletal sites due to
pure glucocorticoid excess: study in eumenorrheic patients with
Cushing’s syndrome. J. Clin. Endocrinol. Metab. 83, 1863–1867
Bonewald, L. (2006) Osteocytes as multifunctional cells. J.
Musculoskelet. Neuronal Interact. 6, 331–333
Boass, A., Ramp, W. K., and Toverud, S. U. (1981) Hypocalcemic, hypophosphatemic rickets in rat pups suckling vitamin
D-deprived mothers. Endocrinology 109, 505–512
Qing, H., and Bonewald, L. F. (2009) Osteocyte remodeling of
the perilacunar and pericanalicular matrix. Int. J. Oral. Sci. 1,
59 – 65
Lester, D. R., Jr., and Seifert, M. F. (1996) Maternal high
calcium diet fails to reverse rickets in the osteosclerotic mouse.
Clin. Orthop. Relat. Res. 330, 271–280
Rasmussen, P. (1977) Calcium deficiency, pregnancy, and lactation in rats. Microscopic and microradiographic observations
on bones. Calcif. Tissue Res. 23, 95–102
Teti, A., and Zallone, A. (2009) Do osteocytes contribute to
bone mineral homeostasis? Osteocytic osteolysis revisited. Bone
44, 11–16
Belanger, L. F. (1969) Osteocytic osteolysis. Calcif. Tissue Res. 4,
1–12
Bonewald, L. F. (2007) Osteocytes as dynamic multifunctional
cells. Ann. N. Y. Acad. Sci. 1116, 281–290
The FASEB Journal 䡠 www.fasebj.org
JIA ET AL.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
Feng, J. Q., Ye, L., and Schiavi, S. (2009) Do osteocytes
contribute to phosphate homeostasis? Curr. Opin. Nephrol. Hypertens. 18, 285–291
Fukumoto, S. (2009) The role of bone in phosphate metabolism. Mol. Cell. Endocrinol. 310, 63–70
Fukumoto, S., and Martin, T. J. (2009) Bone as an endocrine
organ. Trends Endocrinol. Metab. 20, 230 –236
Xia, X., Kar, R., Gluhak-Heinrich, J., Yao, W., Lane, N. E.,
Bonewald, L. F., Biswas, S. K., Lo, W. K., and Jiang, J. X. (2010)
Glucocorticoid induced autophagy in osteocytes. J. Bone Miner.
Res. 25, 2479 –2488
Harman, D. (1992) Role of free radicals in aging and disease.
Ann. N. Y. Acad. Sci. 673, 126 –141
Harman, D. (1988) Free radicals in aging. Mol. Cell. Biochem. 84,
155–161
Hotchkiss, R. S., Strasser, A., McDunn, J. E., and Swanson, P. E.
(2009) Cell death. N. Engl. J. Med. 361, 1570 –1583
He, C., and Klionsky, D. J. (2009) Regulation mechanisms and
signaling pathways of autophagy. Annu. Rev. Genet. 43, 67–93
Chen, J. L., Lin, H. H., Kim, K. J., Lin, A., Ou, J. H., and Ann,
D. K. (2009) PKC␦ signaling: a dual role in regulating hypoxic
stress-induced autophagy and apoptosis. Autophagy 5, 244 –246
Martinet, W., Agostinis, P., Vanhoecke, B., Dewaele, M., and De
Meyer, G. R. (2009) Autophagy in disease: a double-edged
sword with therapeutic potential. Clin. Sci. (Lond.) 116, 697–712
Todde, V., Veenhuis, M., and van der Klei, I. J. (2009) Autophagy: principles and significance in health and disease.
Biochim. Biophys. Acta 1792, 3–13
Mizushima, N., Levine, B., Cuervo, A. M., and Klionsky, D. J.
(2008) Autophagy fights disease through cellular self-digestion.
Nature 451, 1069 –1075
Tsujimoto, Y., and Shimizu, S. (2005) Another way to die:
autophagic programmed cell death. Cell Death Differ. 12(Suppl.
2), 1528 –1534
Maiuri, M. C., Zalckvar, E., Kimchi, A., and Kroemer, G. (2007)
Self-eating and self-killing: crosstalk between autophagy and
apoptosis. Nat. Rev. Mol. Cell Biol. 8, 741–752
Shibata, M., Lu, T., Furuya, T., Degterev, A., Mizushima, N.,
Yoshimori, T., MacDonald, M., Yankner, B., and Yuan, J. (2006)
Regulation of intracellular accumulation of mutant Huntingtin
by Beclin 1. J. Biol. Chem. 281, 14474 –14485
Walther, F. J., Jobe, A. H., and Ikegami, M. (1998) Repetitive
prenatal glucocorticoid therapy reduces oxidative stress in the
lungs of preterm lambs. J. Appl. Physiol. 85, 273–278
Ferioli, M. E., Pinotti, O., and Pirona, L. (1999) Polyamine
oxidase activity in lymphoid tissues of glucocorticoid-treated
rats. Biochem. Pharmacol. 58, 1907–1914
Ogasawara, M., Nomura, K., Shibata, N., Ujihara, M., Kobayashi,
M., and Demura, H. (1999) Surgical stress increases renal
glutathione content via increased glucocorticoid, and resistance
to subsequent oxidative injury in the rat: significant link between endocrine response and cell defense system under the
stress. Endocr. J. 46, 99 –106
Adcock, I. M., and Ito, K. (2005) Glucocorticoid pathways in
chronic obstructive pulmonary disease therapy. Proc. Am. Thorac.
Soc. 2, 313–319; discussion 340 –341
Lee, C. W., Chuang, J. H., Wang, P. W., Chang, N. K., Wang,
H. C., Huang, C. C., Tiao, M. M., and Lo, S. K. (2006) Effect of
glucocorticoid pretreatment on oxidative liver injury and survival in jaundiced rats with endotoxin cholangitis. World J. Surg.
30, 2217–2226
Ong, S. L., Zhang, Y., and Whitworth, J. A. (2008) Reactive
oxygen species and glucocorticoid-induced hypertension. Clin.
Exp. Pharmacol. Physiol. 35, 477– 482
Laane, E., Tamm, K. P., Buentke, E., Ito, K., Khahariza, P., Oscarsson,
J., Corcoran, M., Bjorklund, A. C., Hultenby, K., Lundin, J., Heyman,
M., Soderhall, S., Mazur, J., Porwit, A., Pandolfi, P. P., Zhivotovsky, B.,
Panaretakis, T., and Grander, D. (2009) Cell death induced by
dexamethasone in lymphoid leukemia is mediated through initiation
of autophagy. Cell Death Differ. 16, 1018–1029
O’Brien, C. A., Jia, D., Plotkin, L. I., Bellido, T., Powers, C. C.,
Stewart, S. A., Manolagas, S. C., and Weinstein, R. S. (2004)
Glucocorticoids act directly on osteoblasts and osteocytes to
induce their apoptosis and reduce bone formation and
strength. Endocrinology 145, 1835–1841
Weinstein, R. S. (2001) Glucocorticoid-induced osteoporosis.
Rev. Endocr. Metab. Disord. 2, 65–73
GLUCOCORTICOIDS ON OSTEOCYTE AUTOPHAGY
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
Weinstein, R. S. (2007) Is long-term glucocorticoid therapy
associated with a high prevalence of asymptomatic vertebral
fractures? Nat. Clin. Pract. 3, 86 – 87
Weinstein, R. S., Chen, J. R., Powers, C. C., Stewart, S. A.,
Landes, R. D., Bellido, T., Jilka, R. L., Parfitt, A. M., and
Manolagas, S. C. (2002) Promotion of osteoclast survival and
antagonism of bisphosphonate-induced osteoclast apoptosis by
glucocorticoids. J. Clin. Invest. 109, 1041–1048
Weinstein, R. S., Jilka, R. L., Parfitt, A. M., and Manolagas, S. C.
(1998) Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential
mechanisms of their deleterious effects on bone. J. Clin. Invest.
102, 274 –282
Lane, N. E., Yao, W., Balooch, M., Nalla, R. K., Balooch, G.,
Habelitz, S., Kinney, J. H., and Bonewald, L. F. (2006) Glucocorticoid-treated mice have localized changes in trabecular
bone material properties and osteocyte lacunar size that are not
observed in placebo-treated or estrogen-deficient mice. J. Bone
Miner. Res. 21, 466 – 476
Lane, N. E., Yao, W., Nakamura, M. C., Humphrey, M. B.,
Kimmel, D., Huang, X., Sheppard, D., Ross, F. P., and Teitelbaum, S. L. (2005) Mice lacking the integrin 5 subunit have
accelerated osteoclast maturation and increased activity in the
estrogen-deficient state. J. Bone Miner. Res. 20, 58 – 66
Yao, W., Cheng, Z., Shahnazari, M., Dai, W., Johnson, M. L., and
Lane, N. (2010) Overexpression of secreted frizzled-related
protein 1 inhibits bone formation and attenuates PTH bone
anabolic effects. J. Bone Miner. Res. 25, 190 –199
Yao, W., Cheng, Z., Busse, C., Pham, A., Nakamura, M. C., and
Lane, N. E. (2008) Glucocorticoid excess in mice results in early
activation of osteoclastogenesis and adipogenesis and prolonged suppression of osteogenesis: a longitudinal study of gene
expression in bone tissue from glucocorticoid-treated mice.
Arthritis Rheum. 58, 1674 –1686
Yao, W., Cheng, Z., Koester, K. J., Ager, J. W., Balooch, M.,
Pham, A., Chefo, S., Busse, C., Ritchie, R. O., and Lane, N. E.
(2007) The degree of bone mineralization is maintained with
single intravenous bisphosphonates in aged estrogen-deficient
rats and is a strong predictor of bone strength. Bone 41, 804 – 812
Yao, W., Cheng, Z., Pham, A., Busse, C., Zimmermann, E. A.,
Ritchie, R. O., and Lane, N. E. (2008) Glucocorticoid-induced
bone loss in mice can be reversed by the actions of parathyroid
hormone and risedronate on different pathways for bone formation and mineralization. Arthritis Rheum. 58, 3485–3497
Kalajzic, I., Braut, A., Guo, D., Jiang, X., Kronenberg, M. S.,
Mina, M., Harris, M. A., Harris, S. E., and Rowe, D. W. (2004)
Dentin matrix protein 1 expression during osteoblastic differentiation, generation of an osteocyte GFP-transgene. Bone 35,
74 – 82
Rowe, P. S., Matsumoto, N., Jo, O. D., Shih, R. N., Oconnor, J.,
Roudier, M. P., Bain, S., Liu, S., Harrison, J., and Yanagawa, N.
(2006) Correction of the mineralization defect in hyp mice
treated with protease inhibitors CA074 and pepstatin. Bone 39,
773–786
Kato, Y., Windle, J. J., Koop, B. A., Mundy, G. R., and Bonewald,
L. F. (1997) Establishment of an osteocyte-like cell line, MLOY4. J. Bone Miner. Res. 12, 2014 –2023
Edinger, A. L. (2009) Starvation in the midst of plenty: making
sense of ceramide-induced autophagy by analysing nutrient
transporter expression. Biochem. Soc. Trans. 37, 253–258
Mizushima, N., Yamamoto, A., Matsui, M., Yoshimori, T., and
Ohsumi, Y. (2004) In vivo analysis of autophagy in response to
nutrient starvation using transgenic mice expressing a fluorescent autophagosome marker. Mol. Biol. Cell 15, 1101–1111
Plotkin, L. I., Weinstein, R. S., Parfitt, A. M., Roberson, P. K.,
Manolagas, S. C., and Bellido, T. (1999) Prevention of osteocyte
and osteoblast apoptosis by bisphosphonates and calcitonin.
J. Clin. Invest. 104, 1363–1374
Eisenberg-Lerner, A., Bialik, S., Simon, H. U., and Kimchi, A.
(2009) Life and death partners: apoptosis, autophagy and the
cross-talk between them. Cell Death Differ. 16, 966 –975
Tanida, I., Ueno, T., and Kominami, E. (2004) LC3 conjugation
system in mammalian autophagy. Int. J. Biochem. Cell Biol. 36,
2503–2518
Almeida, M., Han, L., Martin-Millan, M., Plotkin, L. I., Stewart,
S. A., Roberson, P. K., Kousteni, S., O’Brien, C. A., Bellido, T.,
Parfitt, A. M., Weinstein, R. S., Jilka, R. L., and Manolagas, S. C.
3375
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
3376
(2007) Skeletal involution by age-associated oxidative stress and
its acceleration by loss of sex steroids. J. Biol. Chem. 282,
27285–27297
Muthusami, S., Ramachandran, I., Muthusamy, B., Vasudevan, G.,
Prabhu, V., Subramaniam, V., Jagadeesan, A., and Narasimhan, S.
(2005) Ovariectomy induces oxidative stress and impairs bone antioxidant system in adult rats. Clin. Chim. Acta 360, 81–86
Jilka, R. L., Almeida, M., Ambrogini, E., Han, L., Roberson,
P. K., Weinstein, R. S., and Manolagas, S. C. (2010) Decreased
oxidative stress and greater bone anabolism in the aged, when
compared to the young, murine skeleton with parathyroid
hormone administration. Aging Cell 9, 851– 867
Almeida, M., Han, L., Ambrogini, E., Bartell, S. M., and Manolagas, S. C. (2010) Oxidative stress stimulates apoptosis and
activates NF-B in osteoblastic cells via a PKC/p66shc signaling
cascade: counter regulation by estrogens or androgens. Mol.
Endocrinol. 24, 2030 –2037
Manolagas, S. C. (2010) From estrogen-centric to aging and
oxidative stress: a revised perspective of the pathogenesis of
osteoporosis. Endocr. Rev. 31, 266 –300
Almeida, M., Martin-Millan, M., Ambrogini, E., Bradsher, R.,
3rd, Han, L., Chen, X. D., Roberson, P. K., Weinstein, R. S.,
O’Brien, C. A., Jilka, R. L., and Manolagas, S. C. (2010)
Estrogens attenuate oxidative stress and the differentiation and
apoptosis of osteoblasts by DNA-binding-independent actions of
the ER␣. J. Bone. Miner. Res. 25, 769 –781
Orzechowski, A., Ostaszewski, P., Wilczak, J., Jank, M., Balasinska, B., Wareski, P., and Fuller, J., Jr. (2002) Rats with a
glucocorticoid-induced catabolic state show symptoms of oxidative stress and spleen atrophy: the effects of age and recovery. J.
Vet. Med. A Physiol. Pathol. Clin. Med. 49, 256 –263
Jilka, R. L., Weinstein, R. S., Parfitt, A. M., and Manolagas, S. C.
(2007) Quantifying osteoblast and osteocyte apoptosis: challenges and rewards. J. Bone Miner. Res. 22, 1492–1501
Komatsu, F., Kudoh, H., and Kagawa, Y. (2007) Evaluation of
oxidative stress and effectiveness of low-dose glucocorticoid
therapy on exacerbation of chronic obstructive pulmonary
disease. J. Gerontol. A Biol. Sci. Med. Sci. 62, 459 – 464
Planey, S. L., Abrams, M. T., Robertson, N. M., and Litwack, G.
(2003) Role of apical caspases and glucocorticoid-regulated
genes in glucocorticoid-induced apoptosis of pre-B leukemic
cells. Cancer Res. 63, 172–178
Bonapace, L., Bornhauser, B. C., Schmitz, M., Cario, G., Ziegler, U.,
Niggli, F. K., Schafer, B. W., Schrappe, M., Stanulla, M., and Bourquin,
J. P. (2010) Induction of autophagy-dependent necroptosis is required for childhood acute lymphoblastic leukemia cells to overcome
glucocorticoid resistance. J. Clin. Invest. 120, 1310–1323
Vol. 25
October 2011
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
Ke, H. Z., Jee, W. S., Ito, H., Setterberg, R. B., Li, M., Lin, B. Y.,
Liang, X. G., and Ma, Y. F. (1993) Greater bone formation
induction occurred in aged than young cancellous bone sites.
Bone 14, 481– 485
Jee, W. S., Li, X. J., and Schaffler, M. B. (1991) Adaptation of
diaphyseal structure with aging and increased mechanical usage
in the adult rat: a histomorphometrical and biomechanical
study. Anat. Rec. 230, 332–338
Jee, W. S., and Li, X. J. (1990) Adaptation of cancellous bone to
overloading in the adult rat: a single photon absorptiometry and
histomorphometry study. Anat. Rec. 227, 418 – 426
Yao, W., Jee, W. S., Chen, J., Liu, H., Tam, C. S., Cui, L., Zhou,
H., Setterberg, R. B., and Frost, H. M. (2000) Making rats rise to
erect bipedal stance for feeding partially prevented orchidectomy-induced bone loss and added bone to intact rats. J. Bone
Miner. Res. 15, 1158 –1168
Yao, W., Jee, W. S., Chen, J., Tam, C. S., Setterberg, R. B., and
Frost, H. M. (2000) Erect bipedal stance exercise partially
prevents orchidectomy-induced bone loss in the lumbar vertebrae of rats. Bone 27, 667– 675
Bonewald, L. F. (2011) The amazing osteocyte. J. Bone Miner.
Res. 26, 229 –238
Srinivas, V., Bohensky, J., Zahm, A. M., and Shapiro, I. M. (2009)
Autophagy in mineralizing tissues: microenvironmental perspectives. Cell Cycle 8, 391–393
Tsuchihara, K., Fujii, S., and Esumi, H. (2009) Autophagy and
cancer: dynamism of the metabolism of tumor cells and tissues.
Cancer Lett. 278, 130 –138
Kroemer, G., and Jaattela, M. (2005) Lysosomes and autophagy
in cell death control. Nat. Rev. Cancer 5, 886 – 897
Gonzalez-Polo, R. A., Boya, P., Pauleau, A. L., Jalil, A., Larochette, N., Souquere, S., Eskelinen, E. L., Pierron, G., Saftig, P.,
and Kroemer, G. (2005) The apoptosis/autophagy paradox:
autophagic vacuolization before apoptotic death. J. Cell Sci. 118,
3091–3102
Bardeguez, A. D., Skurnick, J. H., Perez, G., Colon, J. M., Kloser,
P., and Denny, T. N. (1997) Lymphocyte shedding from genital
tract of human immunodeficiency virus-infected women: immunophenotypic and clinical correlates. Am. J. Obstet. Gynecol. 176,
158 –165
Evans, B. J., McDowall, A., Taylor, P. C., Hogg, N., Haskard,
D. O., and Landis, R. C. (2006) Shedding of lymphocyte
function-associated antigen-1 (LFA-1) in a human inflammatory
response. Blood 107, 3593–3599
The FASEB Journal 䡠 www.fasebj.org
Received for publication January 31, 2011.
Accepted for publication June 9, 2011.
JIA ET AL.