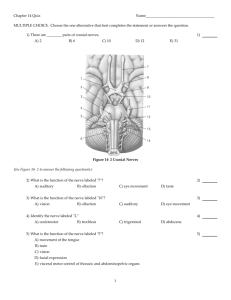
Cranial Nerves Assessment
advertisement

Neuro4Nurses Cranial Nerves Assessment There are twelve pairs of cranial nerves. When conducting a cranial nerves assessment, the patient must be awake, cooperative, and cognitively intact. Cranial Nerve I: Olfactory (Sensory) CN I is not routinely tested. However, if the patient has a base of skull fracture or complained of altered or loss of sense of smell, CN I assessment should be performed2. Testing: Patient’s nostril must be patent. Ask patient to close his/her eyes and close one nostril. Breathe through the nose and identify the odor such as coffee or lemon. Do not use strong odor such as ammonia or alcohol. Strong odor may stimulate the pain sensation of the trigeminal nerve and interfere with the assessment results1,3. Test the other nostril in the same manner. Dysfunction of CN I Changes or loss of the sensation of smell is the malfunction of the frontal lobe3. It can be caused by trauma, congenital causes, infection (sinusitis, rhinitis), cigarette smoking, normal aging, and epilepsy3. Cranial Nerve II: Optic (Sensory) The optic nerve (CN II) controls the visual acuity and visual field2. It is also involves in the pupil response to light. Testing: Visual acuity: Patient wears the appropriate glasses if required. Cover one eye and ask patient to read from the chart. Use the Snellen chart if patient is mobile and the Rosenbaum Pocket Vision Screener if patient is bed ridden. If patient is illiterate or unable to read English, ask patient to identify objects in pictures2. Repeat the process for the other eye. Testing: Visual field: Visual field is the area that a person can see with one eye4. Instruct patient to cover one eye and look at the examiner’s eye. Move fingers from peripheral to central. Patient is asked to say “now” once he/she starts to see your finger. Patient’s visual field should be similar to the examiner’s visual field. Dysfunction of CN II Dysfunctions of optic nerve include blindness, visual field deficits, blurring of vision, scotoma, and diplopia5. Cranial Nerve III: Oculomotor (Motor) Cranial Nerve IV: Trochlear (Motor); Cranial Nerve VI: Abducens (Motor) Cranial nerves III, IV, VI control the extraocular eye movement. CN III also controls the eye opening and dilation and constriction of the pupils1,2. Testing of cranial nerves III, IV, and VI Usually cranial nerve III, IV, and V are tested in one simple assessment. Patient is asked to look at and follow the examiner’s finger while examiner is drawing a large H in the air. This can assess the patient’s extraocular movement in all six directions2. CN III CN III CN III CN VI CN VI VI V VI VI V VI CN III CN III CN IV CN III VIVV Diagram showing the movement of the eyes in relation to the I cranial nerves control of the Dysfunction of the cranial nerve III, IV, and VI Patients with a frontal lobe stroke may have eye deviate to the affected side. Patients with a cerebral hemorrhage may have eye deviation away from the affected side7.Diplopia or double vision is usually related to dysfunction or asynchronous of the extraocular muscle movement. Ptosis is the drooping of eyelid. It is resulted from the dysfunction of CN III or neuromuscular diseases such as myasthenia gravis or Horner’s syndrome7. Cranial Nerve V: Trigeminal (Sensory & Motor)) The trigeminal nerve has three branches. It is involved in the pain and temperature sensation of the face, corneal reflex, and mastication8. Testing: Motor: Ask patient to clench the teeth. The jaw should be tightly close. Testing Sensory: Ask patient to close his/her eyes and test pain sensation on both sides of the face. Corneal reflex: Patient should blink briskly and bilaterally when the eye is slightly touched with a piece of cotton. Dysfunction of CN V Trigeminal neuralgia may be may be idiopathic or due to demyelination of the nerve root. The patient experiences severe pain when stimulated especially in the maxillary and mandibular branch areas8. Cranial Nerve VII: Facial (Motor) The facial nerve controls facial movement. Testing: Observe the patient’s face for any asymmetry at rest and when the patient is smiling, raising both eye brows, showing teeth, or puffing out both cheeks. Dysfunction of CN VII CN VII dysfunction may cause facial asymmetry. The commonly dysfunction of CN VII is Bell’s Palsy. It’s causes include idiopathic, infection, tumor, or trauma. Patients with Bell’s palsy may experience pain, transient loss of sensation and paralysis on one side of the face8. Cranial Nerve VIII: Acoustic (Sensory) Cranial nerve VIII is also known as vestibulocochlear nerve. It’s functions include hearing and balancing. Testing: Hearing: Ask the patient to cover one ear and whisper to the unoccluded ear. Use words or numbers with two equally accented syllables such as baseball or five-four4. Perform the same test on the other ear. Balancing: Vestibular function is not commonly tested unless the patient complains about dizziness or vertigo. Dysfunction of CN VIII Deafness, decreased hearing acuity, or tinnitus (perception of a continuous high-pitched ringing sound without any actual auditory input) may be a resulted of congenital causes, obstruction, aging, infection, trauma, or extreme noise exposure9. Dizziness is a sensation of imbalance and vertigo is a false sensation of turning9. Cranial Nerve IX (CN IX): Glossopharyngeal (Sensory & Motor) The glossopharyngeal nerve supplies the tongue and pharynx and is part of the parasympathetic system. It involves in the swallowing gagging, and vomiting process, and sensation of the posterior third of the tongue 10. Testing: To avoid vomiting, gag reflex is not assessed normally. Assess the sweet taste and observe the upward and forward movement of the larynx when swallowing9. Dysfunction of CN IX Patient who has CN IX dysfunction may be able to swallow without aspiration11. Cranial Nerve X: Vagus Nerve (Sensory & Motor) The vagus nerve has sensory, motor, and parasympathetic functions. It receives sensation from the larynx, pharynx, and abdominal organs10. The motor division of the vagus nerve controls the posterior portion of the tongue during swallowing, speech, and breathing10. Testing: Common test for CN X includes listening for any hoarseness of the voice during conversation. Ask the patient to open his/her mouth and say “ah” and observe for uvula deviation. Uvula will deviate away from the side of lesion. Assess for swallowing reflex 4,11 . Dysfunction of CN X Dysphagia is defined as difficulty in swallowing. A proper swallowing assessment must be performed by a trained professional (e.g. speech language pathologist) for patients suspected to have dysphagia because of the risk of aspiration. Dysartharia is the dysfunction of motor speech when the patient has poor articulation of words. Cranial Nerve XI: Accessory or Spinal Accessory (Motor) The accessory nerve is also called spinal accessory nerve. It controls the neck and shoulder movement. Testing: Place both hands on the patient’s shoulder and ask him/her to shrug both shoulders. Assess for the muscle strength and symmetrical movement. Place one hand on the patient’s cheek and ask the patient to turn his/her head against your hand. Test for motor strength. Then repeat on the other side of cheek. Cranial Nerve XII (CN XII): Hypoglossal (Motor) The hypoglossal nerve controls the intrinsic muscle of the tongue12. Testing: Ask the patient to open his/her mouth and protrude his/her tongue. Observe for any atrophy, difficulty in protrusion, and deviation of the tongue. The tongue deviates to the weakness side. Also observe for any dysarthria when the patient talks12. Reference 1) Hickey, J.V. (2009). The Clinical Practice of Neurological and th Neurosurgical Nursing. (6 ed.). Philadelphia: J.B.Lippincott Company. 2) Barker, E, & Moore, K. (1992). Cranial nerve assessment. RN, 55(5), 62-69. 3) Sanders, R.D., & Gillig, P.M. (2009a). Cranial nerve I: Olfactory. Psychiatry, 6(7), 30-35. 4) Palmieri, R.L. (2009). Wrapping your head around cranial nerves. Nursing, 39(9), 24-30. 5) Gillig, P.M., & Sanders, R.D. (2009). Cranial nerve II: Vision. Psychiatry, 6(9), 32-37. 6) Brazis, P.W. (2009). Isolated palsies of cranial nerves III, IV, and VI. Seminars in Neurology, 20(1), 14-28. 7) Sanders, R.D., & Gillig, P.M. (2009b). Cranial nerve III, IV, and VI: Ocular function. Psychiatry, 6(11), 34-39. 8) Gillig, P.M., & Sanders, R.D. (2010a). The trigeminal (V) and facial (VII) cranial nerve: Head and face sensation and movement. Psychiatry, 7(1), 25-30. 9) Sanders, R.D., & Gillig, P.M. (2010). Cranial nerve . Psychia 10) Erman, A.B., Kejner, A.E., Hogikyan, N.D., & Feldman, E.L. (2009). Disorders of cranial nerves IX and X. Seminars in Neurology, 29 (1), 8592. 11) Gillig, P.M., & Sanders, R.D. (2010b). Cranial nerves IX, X, XI, and XII. Psychiatry, 7(5), 37-41. 12) Loh, C., Maya, M.M., & Go, J.L. (2002). Cranial nerve XII: The hypoglossal nerve. Seminars in Ultrasound, CT, and MRI, 23(3), 256265. ©2013 Disclaimer: The author of this article neither represents nor guarantees that the practices described herein, if followed, ensure safe and effective patient care. The author further assumes no responsibility or liability in connection with any information or recommendations contained in this article. The recommendations and instructions in this article are based on the knowledge and practice in neuroscience as of the date of publication. These recommendation and instructions are subject to change based on the availability of new scientific information.