IOM/QSEN Competencies in Nursing Education
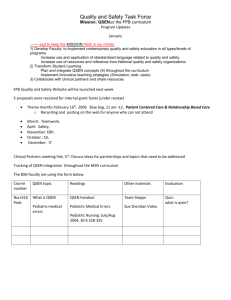
advertisement

12/17/2012 IOM/QSEN Competencies Health professions education: A bridge to quality(2003) An Introduction to the Competencies and Knowledge, Skills, and Attitudes QSEN Funded by Robert Wood Johnson Foundation Focused on transforming basic education for nurses Reflects a new identity for nurses that demonstrates knowledge, skills and attitudes that emphasize quality and safety in patient care Gerry Altmiller, EdD, APRN, ACNS‐BC Phase I Development Phase II Implementation Phase III Dissemination Relevance to Nursing Education and Clinical Practice Baccalaureate Essentials /Master’s Essentials ©Altmiller Transition to Practice Program Objectives Patient Centered Care Participants will be able to identify knowledge, skills, Patient is in control and a full partner; care is based and attitudes that emphasize the IOM/QSEN competencies. on respect for patient’s preferences, values, and needs. (Offer more control, choice, self‐efficacy, and individualization of care) Consider patient’s cultural preferences Participants will identify at least one strategy that can be incorporated into their classroom or clinical teaching. White board initiatives for patient goals IHI Home Page Patient Centered Care 101 1.5 contact hrs The Picker Institute‐Advancing the Principles of Patient‐ Centered Care http://pickerinstitute.org Participants will identify resources for linking strategies that promote quality and safety to their specific theory or clinical teaching. ©Altmiller Institute for Patient‐ and Family‐Centered Care http://www.ipfcc.org https://www4.georgetown.edu/uis/keybridge/keyform/for m.cfm?formID=277 ©Altmiller Patient Centered Care Patient Centered Care Keeping the focus on the patient Value added nursing care (rounding) Non‐value added nursing care (waiting for assistance, delays, looking for supplies) Necessary but non‐value added nursing care (medication preparation, documentation Keep focused on patient goals and solving problems at Transforming care (TJC) http://www.centerfortransforminghealthcare.org/projects /detail.aspx?Project=6 ©Altmiller the point of care Promote relationship building with patients First Touch – Home Involve patient in all we do Situational Awareness Rapid response teams to avoid codes on Med‐Surg units Personal accountability in all we do Reducing admission rates Helping nurses obtain new skill sets http://www.ihi.org/offerings/Initiatives/PastStrategicIn itiatives/TCAB/Pages/Materials.aspx Improve patient satisfaction 1 12/17/2012 Teamwork and Collaboration Achieve quality patient outcomes by effectively communicating with nurses and inter‐professional teams having mutual respect and shared decision making. Synergistic effects of effective interdisciplinary collaboration System based solutions for Safe hand‐offs Acknowledging other team members contributions Ability to raise concerns; Assertion CUS (concerned, uncomfortable, safety) 2 challenge rule Critical Language “I need some clarity.” Teamwork and Collaboration Effective Communication SBAR Situation Background Assessment Recommendation Rapid Response Teams ©Altmiller Teamwork and Collaboration Leadership during high stress team efforts P Integrate best current evidence, clinical expertise, and patient preferences and values to deliver optimal health care. Reduce Variability through evidence U D Evidence Based Practice F Integration of Standards “It’s less of a thing to do…it’s more of a way to be” Conflict Management Strategies TeamSTEPPS Tools and Videos TeamSTEPPS http://www.ahrq.gov/teamsteppstools/instructor/videos. htm Evidence Based Practice Translate new knowledge into practice Provide guidance in weighing evidence Share the evidence that links studies to optimum clinical outcomes and business results http://www.guidelines.gov/ National Guideline Clearinghouse | Home The Cochrane Collaboration Identify those at risk for infection Bundles and protocols http://www.jointcommission.org/infection_control.aspx Handwashing Proper hygiene for in and out of room Pressure ulcer prevention Ventilator associated pneumonia prevention Influenza/pneumococcal disease prevention Quality Improvement (QI) Monitor outcomes of care processes and use improvement methods to design and test changes to improve the health care system. Culture of Safety Report errors/adverse events/near misses Systematic Investigations of problems Safe to ask for help System wide transformation IHI Open School Quality Improvement 101‐106 9 contact hrs Look at waste and variation and eliminate it Identify where to make changes in the system Tools and Strategies for Quality Improvement and Patient Safety ‐ http://www.ncbi.nlm.nih.gov/books/NBK2682 2 12/17/2012 Quality Improvement (QI) Quality Improvement (QI) Familiarity with Nursing Sensitive Indicators https://www.nursingquality.org/data.aspx Presentation of data; Describe Aim PDSA (Plan, the change, how tested, how studied) Use of Tools (flow charts, check sheets, run charts, bar graphs) PDSA (Plan, Do, Study, Act) What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make that will result in improvement? Personal Improvement Project using Model for Improvement: What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make that will result in improvement? ©Altmiller Quality Improvement (QI) Safety Minimize risk of harm to patients and providers Mistake proofing ©Altmiller Mistake‐proofing the Design of Health Care Processes: Chapter 2 http://www.ahrq.gov/qual/mistakeproof/mistake2.htm through both system effectiveness and individual performance. IHI Open School Patient Safety 100‐106 8.25 contact hrs Two patient identifiers NDNQI Pressure Ulcer Training National Database of Nursing Quality Indicators https://www.nursingquality.org/Default.aspx Patient armbands where standardized Correct surgery/Correct site Medication reconciliation Standardization of medications Patient Safety Solutions Identify Work‐arounds Patient Safety Solutions ‐ Joint Commission Resources – Intranet http://www.ccforpatientsafety.org/Patient‐Safety‐ Solutions/ Time outs Huddles Non‐verbal communication requires confirmation ©Altmiller Safety One Minute Safety Check Provide learning opportunities to identify errors in a safe environment Speak the language of quality and Safety AHRQ Glossary http://www.psnet.ahrq.gov/glossary.aspx Resources for patient safety information National Patient Safety | Joint Commission http://www.jointcommission.org/PatientSafety/Nationa lPatientSafetyGoals AHRQ Patient Safety Network http://www.psnet.ahrq.gov/ National Patient Safety Foundation http://www.npsf.org Used for clinical setting Helps students prioritize safety concerns ©Altmiller ©Altmiller 3 12/17/2012 C S F VS C B A Use information and technology to communicate, manage knowledge, mitigate error and support decision making. Navigate resources 1 D 2 D 3 D Medical Record 4 C 5 D A ◦ Informatics F A 8 7 YPU M ©Altmiller And in the midst of this…..”mindfulness and sensemaking (Weick & Sutcliff, 2001) Mindfulness Staying focused and tuned in Ability to see the significance of early and weak signals and to take strong decisive action to prevent harm Trouble starts small and is signaled by weak symptoms that are easy to miss Situational Awareness Utilize data bases effectively Use technology to seek information Creating Run Charts‐You Tube Use technology to report concerns Institute For Safe Medication Practices http://www.ismp.org/ Model life long learning ©Altmiller Resources QSEN Teaching Strategies http://www.qsen.org/ Sensemaking Using multiple cues; critical thinking ©Altmiller ©Altmiller Questions? Thank you! Altmiller@Lasalle.edu ©Altmiller 4