Sustainably improving health care
advertisement

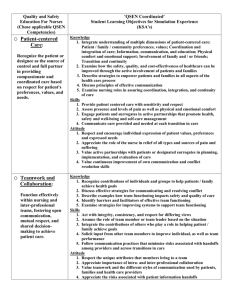
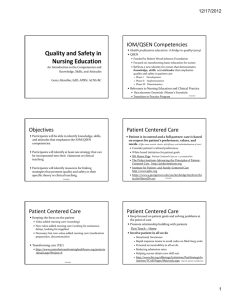
Developing and Maintaining Quality and Safety Competencies Linda Cronenwett, PhD, RN, FAAN Professor and Former Dean Co-Director, RWJF Executive Nurse Fellows THE UNIVERSITY of NORTH CAROLINA at CHAPEL HILL General Aim for Health Professions (Paul Batalden, IHI Co-Founder) To prepare health professionals — as part of their usual professional formation — to lead the continual improvement of the quality, safety and value of health care: to know how to identify good care from the scientific evidence to know the actual measured performance in the context where the health professional is learning/practicing, and the nature of the gaps — if any — between good care and actual local care, and to know what activities are necessary — if any — to close the gap(s). What is the new work of nursing and other health professionals? Quality and safety cultures require new ways of thinking, specifically inviting nurses and others to: Keep the patient experience of care the primary focus for all decisions Understand and apply the basics of safety sciences Use systems thinking Adhere to evidence-based guidelines and interventions Embrace continuous quality improvement as part of daily work Continuum of Systems Thinking What does it mean to be a good nurse? I will turn my patient I will post a note above the bed to remind others I will ask other nurses about products to prevent ulcers I will look at the ulcer rate on our unit I will compare our unit ulcer rate with benchmarks From: M. Dolansky & S.Moore. Systems Thinking Scale, available at: http://fpb.case.edu/systemsthinking/sts.shtm End goal (Cronenwett) I will work with others to improve our unit’s ulcer rate Patient Centered Care QSEN Definition: Gaps: • Need to know patient values and preferences Recognize the patient or designee as the source of • Need to welcome patient and families as partners in control and full partner in providing compassionate ensuring safety • Need to ensure that patient and coordinated care and family needs are based on respect for microsystem’s top priority patient's preferences, • Need to coordinate values, and needs. complex care with multiple caregivers Teamwork and Collaboration QSEN Definition: Gaps: • Need training in team and Function effectively in nursing and interprofessional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care team-based care • Need to value patient and family members as essential parts of the health care team • Need to appreciate the role of communication in errors and near misses • Need to value and earn respect of team members Evidence-based Practice QSEN Definition: Gaps: • Need to approach practice Integrate best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care with a spirit of inquiry • Need to know how to identify good care from scientific evidence • Need to scan sources of new knowledge relevant to one’s practice • Need to develop expertise in balancing evidence, clinical expertise and patient values and preferences when planning care Quality Improvement QSEN Definition: Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems Gaps: • Need to own accountability for practice of one’s microsystem • Need to know how the actual care in one’s microsystem compares to best practice • Need to use quality improvement methods to close gaps between actual local care and good care Safety QSEN Definition: Minimize risk of harm to patients and providers through both system effectiveness and individual performance Gaps: • • • Need to know how to create and support “just cultures” and “safety cultures” Need to learn from open reporting about adverse events, errors, and near misses Need to support a culture that holds teammates accountable for reliable attention to safety practices Informatics QSEN Definition: Gaps: • Need improved EHRs and Use information and technology to communicate, manage knowledge, mitigate error, and support decision making alert systems • Need to understand the errors that are likely to be introduced with new technologies and minimize risks • Need involvement in design and evaluation of knowledge management and communication systems Embracing System-Level Quality and Safety What does it take to embrace continuous improvement efforts as a part of one’s daily work? Answers (like the problem) found at both individual and systems levels Current Definitions of Daily Work What constitutes daily work? What constitutes “add-on work”? For: APRNs Nurses in basic practice Nurses in administrative positions Faculty members Triangle of Professional Aims Better professional development Better outcomes (individuals, communities) (competence, joy, mastery) Better system performance (quality, safety, value) From Batalden & Foster (2012). Sustainably improving health care. Radcliffe: London and New York. Professional Aims: Current Silos Nursing Careers Better outcomes Better system performance Better professional development Cronenwett, L. & Ironside, P. (2012). Triangle synergies in a national quality and safety education initiative in nursing. In Batalden & Foster (Eds). Sustainably improving health care. Radcliffe: London and New York, pp. 159-174. Barriers to Linking Aims Among Faculties Limited (if any) accountability for patients or systems of care Limited (if any) understanding of improvement science Collegiate institutional rewards not aligned with patient care or system performance Scientists rewarded for laser focus on research and scholarship Relatively new discipline to academe Barriers to Linking Aims for Practitioners Education focused almost solely on patient care Limited (if any) accountability for professional development Limited preparation for leading system improvements Freedom to engage in precepting students limited by employers Barriers to Linking Aims for Administrators Limited (if any) accountability for professional development Limited (if any remaining) expertise in patient care Need to exert self in midst of other powerful administrators Salaries make movement across the Triangle unlikely Focus on continued professional development of staffs rather superficial