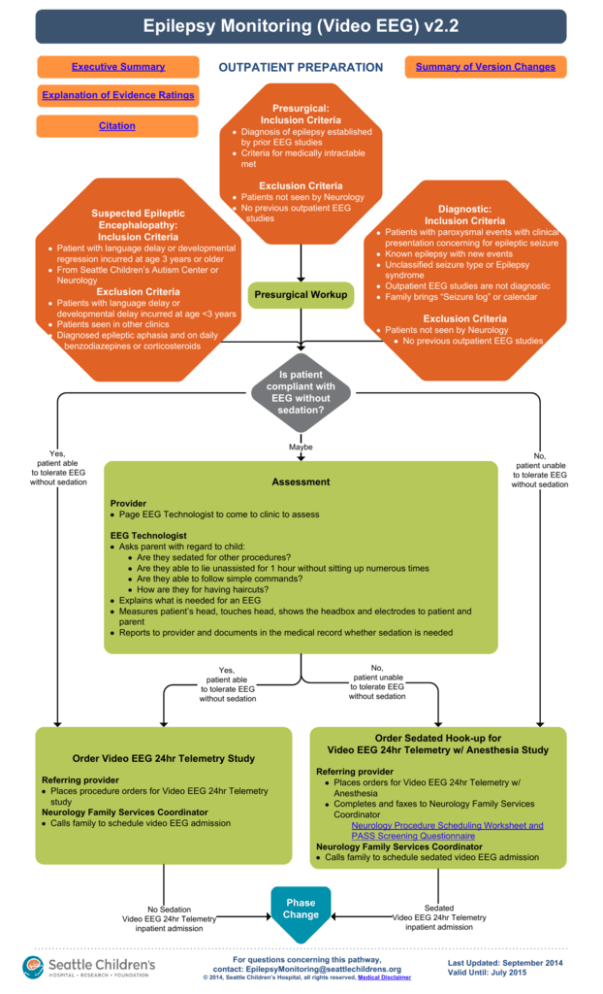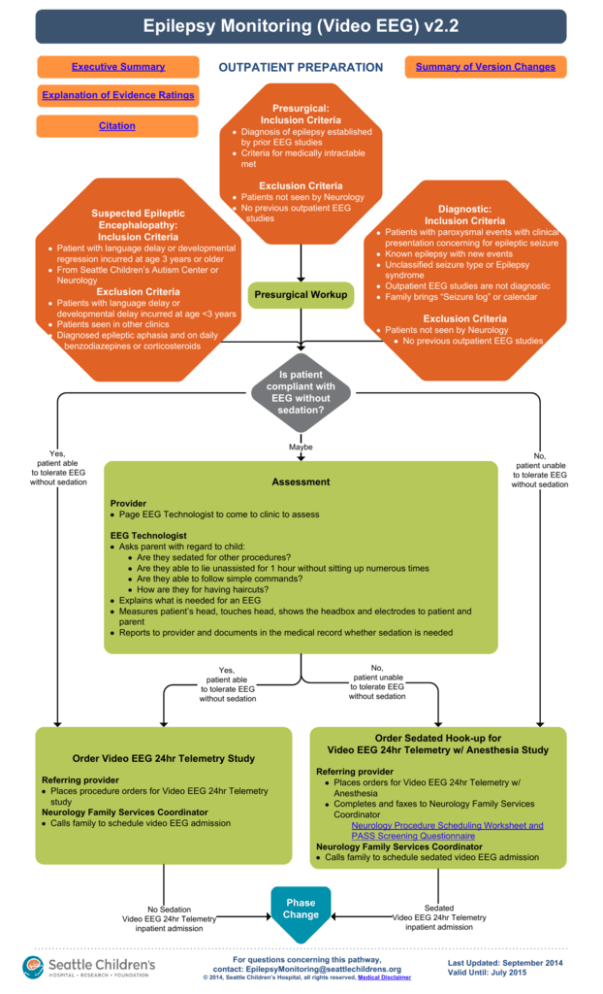
Epilepsy Monitoring (Video EEG) v2.2
Executive Summary
Summary of Version Changes
OUTPATIENT PREPARATION
Explanation of Evidence Ratings
Presurgical:
Inclusion Criteria
Citation
Diagnosis of epilepsy established
by prior EEG studies
Criteria for medically intractable
met
Exclusion Criteria
Patients not seen by Neurology
No previous outpatient EEG
studies
Suspected Epileptic
Encephalopathy:
Inclusion Criteria
Patient with language delay or developmental
regression incurred at age 3 years or older
From Seattle Children’s Autism Center or
Neurology
Exclusion Criteria
Patients with language delay or
developmental delay incurred at age <3 years
Patients seen in other clinics
Diagnosed epileptic aphasia and on daily
benzodiazepines or corticosteroids
Presurgical Workup
Diagnostic:
Inclusion Criteria
Patients with paroxysmal events with clinical
presentation concerning for epileptic seizure
Known epilepsy with new events
Unclassified seizure type or Epilepsy
syndrome
Outpatient EEG studies are not diagnostic
Family brings “Seizure log” or calendar
Exclusion Criteria
Patients not seen by Neurology
No previous outpatient EEG studies
Is patient
compliant with
EEG without
sedation?
Maybe
Yes,
patient able
to tolerate EEG
without sedation
No,
patient unable
to tolerate EEG
without sedation
Assessment
Provider
Page EEG Technologist to come to clinic to assess
EEG Technologist
Asks parent with regard to child:
Are they sedated for other procedures?
Are they able to lie unassisted for 1 hour without sitting up numerous times
Are they able to follow simple commands?
How are they for having haircuts?
Explains what is needed for an EEG
Measures patient’s head, touches head, shows the headbox and electrodes to patient and
parent
Reports to provider and documents in the medical record whether sedation is needed
No,
patient unable
to tolerate EEG
without sedation
Yes,
patient able
to tolerate EEG
without sedation
Order Sedated Hook-up for
Video EEG 24hr Telemetry w/ Anesthesia Study
Order Video EEG 24hr Telemetry Study
Referring provider
Places procedure orders for Video EEG 24hr Telemetry
study
Neurology Family Services Coordinator
Calls family to schedule video EEG admission
No Sedation
Video EEG 24hr Telemetry
inpatient admission
Referring provider
Places orders for Video EEG 24hr Telemetry w/
Anesthesia
Completes and faxes to Neurology Family Services
Coordinator
Neurology Procedure Scheduling Worksheet and
PASS Screening Questionnaire
Neurology Family Services Coordinator
Calls family to schedule sedated video EEG admission
Phase
Change
Sedated
Video EEG 24hr Telemetry
inpatient admission
For questions concerning this pathway,
contact: EpilepsyMonitoring@seattlechildrens.org
© 2014, Seattle Children’s Hospital, all rights reserved, Medical Disclaimer
Last Updated: September 2014
Valid Until: July 2015
Epilepsy Monitoring (Video EEG) v2.2
INPATIENT VIDEO EEG
No Sedation
Sedation
Patient checks in at 4th floor admitting
Patient checks in at 4th floor admitting
Patient transported to room
Patient transported to OPC
EEG Lead Placement
EEG Lead Placement
Orders
Team places admission orders (Video EEG Admit Orderset)
Select “Follow Video EEG Monitoring Pathway” order
Seizure precautions
Casper for violent behavior
Child Life consult
Notify Dietitian if ketogenic diet
If history of epileptic seizures, Video EEG Acute Seizure
Management Plan
Lead Placement
Child life (if needed, page inpatient)
Electrodes placed in treatment room
Presurgical: special electrodes if indicated
Baseline EEG study if needed
Place arm restraints, if ordered
Patient/family escorted to room
Sedation and Lead Placement
Sedation
Sedation for
for video
video EEG
EEG hook-up
hook-up
Outpatient Procedure Center (OPC) calls EEG technologist
Labs if needed: CBC, PT/INR, PTT, drug levels, BUN/
creatinine, glucose, lytes, LFTs
Electrodes placed in OPC
Presurgical: special electrodes if indicated
Order and place arm restraints (page provider if order
needed) per Neuro Diagnostics Sedation Policy for
Patients Undergoing Neurodiagnostic Studies
Transfer to recovery
Orders
Team places admission orders (Video EEG Admit Orderset)
Select “Follow Video EEG Monitoring Pathway” order
Seizure precautions
Casper for violent behavior
Child Life consult
Notify Dietitian if ketogenic diet
If history of epileptic seizures, Video EEG Acute Seizure
Management Plan
Monitoring Begins/Admission Assessment
Electrodes connected to acquisition machine, and study started
Patient/family receives education by tech and RN
EEG technologist assures EEG data quality
Patient seen by ARNP NP/PA / Epilepsy Fellow
Examination findings presented to attending
Team sees family
Determine medication hold plan, if needed
Presurgical considerations:
IV placement
Bleeding history and lab studies (PT/INR, PTT)
Social work consult
Daily Assessment
EEG technologist assures EEG data quality
Patient seen and examined by NP/PA / Epilepsy Fellow /
Epileptologist and writes daily note
Examination findings presented to attending
Study objectives met
or maximum number of
scheduled days completed
Discharge Criteria
Ensure data integrity/quality
Study discontinued (acquisition machine
disconnected, electrodes removed)
Scalp examined for skin breakdown
Preliminary EEG results discussed among Team
Team sees family
Renew orders for arm restraints, if needed
Report any falls using eFeedback
Daily
Review
Longer study needed
Continue Monitoring
EEG tech initiates another 24-hour recording
Team and family consider activation procedures
Adjust orders including medications if necessary
Discharge Instructions
Activity restrictions if
indicated
Skin Care after EEG Lead
Removal PE1518
Follow-up appointment with
referring provider
Medication changes if
indicated
Study Reviewed
Communication of critical values
Report dictated or typed in template
Report signed
Copy sent to referring provider
Return to Home
For questions concerning this pathway,
contact: EpilepsyMonitoring@seattlechildrens.org
© 2014, Seattle Children’s Hospital, all rights reserved, Medical Disclaimer
Last Updated: September 2014
Valid Until: July 2015
Video EEG Seizure Acute Management – Midazolam
Minute 0
1st Step
Drug Treatment
General Measures
None unless customized plan
ordered for this admission
Nursing assessment and
narration
Cardiorespiratory support as
needed
Parent presses the event button to
document the episode and call RN
Position child to avoid injury
Document seizure start time
Optimize view of the child
seizure continues
General Measures
Minute 3
2nd Step
Drug Treatment
IV access
Midazolam 0.1 mg/kg max 5mg/
dose administered IV 4mg/min
No IV access
Midazolam 0.2mg/kg max 10mg/
dose, ½ dose in each nostril
Midazolam 0.5mg/kg buccally max
dose 10mg if nares not available
Prepare/obtain next medication
Notify Contact Provider if medication
given
SpO2 and cardiorespiratory
monitoring; support respiration
including provision of high
concentration oxygen
seizure
stops
seizure continues
Minute 13
3rd Step
Drug Treatment
General Measures
IV access
Midazolam 0.1 mg/kg max 5mg/
dose administered IV 4mg/min
No IV access
Midazolam 0.2mg/kg max 10mg/
dose, ½ dose in each nostril
Midazolam 0.5mg/kg buccally max
dose 10mg if nares not available
Continued cardiorespiratory
monitoring
Notify Epileptologist and Contact
Provider if medication given
Vital signs q 5 minutes
Request next medication
Call Rapid Response Team
seizure continues
General Measures
Customize treatment plan if available.
If not available, use default below:
Age <2 months old
Phenobarbital 20mg/kg loading dose
Age ≥ 2 months old
Fosphenytoin 20mg PE/kg
Above plus
Blood pressure support
if needed
Identify and treat
medical complications
Request next
medication
seizure continues
General Measures
Minute >38
5th Step
Drug Treatment
Age <2 months old
May give additional phenobarbital
5mg/kg doses every 15-30 minutes
until 30mg/kg maximum is met
Age ≥ 2 months old
Phenobarbital 20mg/kg if seizure
continues 15 minutes after
phosphenytoin load
May give 2 additional phenobarbital
5mg/kg doses every 15-20 minutes
(max total 30mg/kg maximum)
Return to Inpatient
seizure
stops
General Measures
Post-Ictal
Minute 23
4th Step
Drug Treatment
As above
Ongoing vital signs q 10 minutes
until stable
Ongoing cardiorespiratory and
SpO2 monitoring until return to
baseline
Family support
seizure
stops
seizure continues
For questions concerning this pathway,
contact: EpilepsyMonitoring@seattlechildrens.org
© 2014, Seattle Children’s Hospital, all rights reserved, Medical Disclaimer
Off
Pathway
Last Updated: September 2015
Valid Until: July 2015
Video EEG Seizure Acute Management – Diazepam
Minute 0
1st Step
Drug Treatment
General Measures
None unless customized plan
ordered for this admission
Nursing assessment and
narration
Cardiorespiratory support as
needed
Parent presses the event button to
document the episode and call RN
Position child to avoid injury
Document seizure start time
Optimize view of the child
Minute 3
2nd Step
seizure continues
General Measures
Drug Treatment
IV access
Diazepam 0.1 mg/kg max 10mg/
dose administered IV over at least
3 min (max 5mg/min)
SpO2 and cardiorespiratory
monitoring; support respiration
including provision of high
concentration oxygen
Prepare/obtain next medication
Notify Contact Provider if
medication given
seizure
stops
seizure continues
General Measures
Minute 18
3rd Step
Drug Treatment
IV access
Diazepam 0.1 mg/kg max 10mg/
dose administered IV over at least
3 min (max 5mg/min)
Continued cardiorespiratory
monitoring
Notify Epileptologist and Contact
Provider if medication given
Vital signs q 5 minutes
Request next medication
Call Rapid Response Team
General Measures
Drug Treatment
Customize treatment plan if available.
If not available, use default below:
Age <2 months old
Phenobarbital 20mg/kg loading dose
Age ≥ 2 months old
Fosphenytoin 20mg PE/kg
Above plus
Blood pressure support
if needed
Identify and treat
medical complications
Request next
medication
seizure continues
General Measures
Minute >40
5th Step
Drug Treatment
Age <2 months old
May give additional phenobarbital
5mg/kg doses every 15-30 minutes
until 30mg/kg maximum is met
Age ≥ 2 months old
Phenobarbital 20mg/kg if seizure
continues 15 minutes after
phosphenytoin load
May give 2 additional phenobarbital
5mg/kg doses every 15-20 minutes
(max total 30mg/kg maximum)
Return to Inpatient
seizure
stops
General Measures
Post-Ictal
Minute 33
4th Step
seizure continues
As above
Ongoing vital signs q 10 minutes
until stable
Ongoing cardiorespiratory and
SpO2 monitoring until return to
baseline
Family support
seizure
stops
seizure continues
For questions concerning this pathway,
contact: EpilepsyMonitoring@seattlechildrens.org
© 2014, Seattle Children’s Hospital, all rights reserved, Medical Disclaimer
Off
Pathway
Last Updated: September 2014
Valid Until: July 2015
Return to Inpatient
Return to Inpatient
Executive Summary
To Pg 2
Return to Home
Executive Summary
Back
Return to Home
Executive Summary
Back
Return to Home
Evidence Ratings
We used the GRADE method of rating evidence quality. Evidence is first assessed as to
whether it is from randomized trial, or observational studies. The rating is then adjusted in
the following manner:
Quality ratings are downgraded if studies:
• Have serious limitations
• Have inconsistent results
• If evidence does not directly address clinical questions
• If estimates are imprecise OR
• If it is felt that there is substantial publication bias
Quality ratings can be upgraded if it is felt that:
• The effect size is large
• If studies are designed in a way that confounding would likely underreport the magnitude
of the effect OR
• If a dose-response gradient is evident
Quality of Evidence:
High quality
Moderate quality
Low quality
Very low quality
Expert Opinion (E)
Reference: Guyatt G et al. J Clin Epi 2011: 383-394
To Bibliography
Return to Home
Summary of Version Changes
Version 1 (12/22/2012): Go live, epilepsy monitoring for patients with suspected epileptic
encephalopathy
Version 2 (7/11/2012): Added diagnostic and presurgical epilepsy monitoring
Version 2.1 (10/30/2013): Reduced IV midazolam dosing
Version 2.2 (9/30/2014): Changed assessment for tolerance of EEG leads from Child Life to
EEG Technologist, added approval and citation pages
Return to Home
Medical Disclaimer
Medicine is an ever-changing science. As new research and clinical experience
broaden our knowledge, changes in treatment and drug therapy are required.
The authors have checked with sources believed to be reliable in their efforts to
provide information that is complete and generally in accord with the standards
accepted at the time of publication.
However, in view of the possibility of human error or changes in medical sciences,
neither the authors nor Seattle Children’s Healthcare System nor any other party
who has been involved in the preparation or publication of this work warrants that
the information contained herein is in every respect accurate or complete, and
they are not responsible for any errors or omissions or for the results obtained
from the use of such information.
Readers should confirm the information contained herein with other sources and
are encouraged to consult with their health care provider before making any
health care decision.
Return to Home
Bibliography
Search Methods for Sedation for EEG Hook-up
Studies were identified by searching electronic databases using search strategies developed and executed
by a medical librarian, Jamie Graham. Searches were performed on July 11th, 12th & 14th, 2011 in the
following databases: on the Ovid platform – Medline (1996 to date), Cochrane Database of Systematic
Reviews (2005 – June 2011), PsycInfo (1987-2011); elsewhere – National Guidelines Clearinghouse, Clinical
Evidence, DynaMed and TRIP. Retrieval was limited to literature from 2001 forward, and children between
the ages of 0-18. Originally the publication limiters for the Scout Search were applied (Consensus
Development Conference; Consensus Development Conference, NIH; Guideline; Meta Analysis; Practice
Guideline); additional searches were conducted using the clinical queries filters and exp epidemiologic
studies command where appropriate. In Medline and PsycInfo, appropriate Medical Subject Headings
(MeSH) were used, along with keyword searching, and the search strategy was adapted for other databases
using their controlled vocabularies, where available, along with text words. Search terms are listed below.
Search Terms: electroencephalography, EEG, epileptic seizures, seizures, audiogenic seizures, petit mal
seizures, grand mal seizures, sedatives, sedation, dexmedetomidine, autism, deep sedation, conscious
sedation, hypnotics & sedatives, seizures febrile,
Jamie Graham, MLS
December 21, 2011
Identification
61 records identified through
database searching
2 additional records identified
through other sources
Screening
64 records after duplicates removed
64 records screened
40 records excluded
24 full-text articles assessed for eligibility
17 full-text articles excluded, did not answer
clinical question
Eligibility
Included
7 studies included in pathway
Flow diagram adapted from Moher D et al. BMJ 2009;339:bmj.b2535
To Bibliography Pg 2
Return to Home
Bibliography
Sedation for EEG Hook-Up
Aksu R, Kumandas S, Akin A, Bicer C, Gümüş H, Güler G, Per H, Bayram A, Boyaci A. The
comparison of the effects of dexmedetomidine and midazolam sedation on electroencephalography
in pediatric patients with febrile convulsion. Paediatr Anaesth. 2011 Apr;21(4):373-8. doi: 10.1111/
j.1460-9592.2010.03516.x. PubMed PMID: 21371166.
Al-Ghanem SS, Al-Oweidi AS, Tamimi AF, Al-Qudah AA. Anesthesia and electrocorticography for
epilepsy surgery: A jordanian experience. Middle East J Anesthesiol [sedation]. 2009 Feb;20(1):31-7.
Berkenbosch JW, Wankum PC, Tobias JD. Prospective evaluation of dexmedetomidine for
noninvasive procedural sedation in children. Pediatr Crit Care Med [seizures]. 2005 Jul;6(4):435,9;
quiz 440.
Everett LL, van Rooyen IF, Warner MH, Shurtleff HA, Saneto RP, Ojemann JG. Use of
dexmedetomidine in awake craniotomy in adolescents: report of two cases. Paediatr Anaesth. 2006
Mar;16(3):338-42. PubMed PMID: 16490103.
Mehta UC, Patel I, Castello FV. EEG sedation for children with autism. Journal of Developmental &
Behavioral Pediatrics [sedation]. 2004 Apr;25(2):102-4.
Meyer S, Shamdeen MG, Kegel B, Mencke T, Gottschling S, Gortner L, et al. Effect of propofol on
seizure-like phenomena and electroencephalographic activity in children with epilepsy vs children
with learning difficulties. Anaesthesia [sedation]. 2006 Nov;61(11):1040-7.
Ray T, Tobias JD. Dexmedetomidine for sedation during electroencephalographic analysis in children
with autism, pervasive developmental disorders, and seizure disorders. J Clin Anesth [seizures]. 2008
Aug;20(5):364-8.
Additional References for Epilepsy Monitoring
American Clinical Neurophysiology Society. Guideline twelve: guidelines for long-term monitoring
for epilepsy. Am J Electroneurodiagnostic Technol. 2008 Dec;48(4):265-86. PubMed PMID:
19203080.
Atkinson M, Hari K, Schaefer K, Shah A. Improving safety outcomes in the epilepsy monitoring unit.
Seizure. 2012 Mar;21(2):124-7. Epub 2011 Nov 16. PubMed PMID: 22093593.
Labiner DM, Bagic AI, Herman ST, Fountain NB, Walczak TS, Gumnit RJ; National Association of
Epilepsy Centers. Essential services, personnel, and facilities in specialized epilepsy centers--revised
2010 guidelines. Epilepsia. 2010 Nov;51(11):2322-33. PubMed PMID: 20561026.
Noe KH, Drazkowski JF. Safety of long-term video-electroencephalographic monitoring for
evaluation of epilepsy. Mayo Clin Proc. 2009 Jun;84(6):495-500. PubMed PMID: 19483165; PubMed
Central PMCID: PMC2688622.
Perkins AM, Buchhalter JR. Optimizing patient care in the pediatric epilepsy monitoring unit. J
Neurosci Nurs. 2006 Dec;38(6):416-21, 434. PubMed PMID: 17233511.
Velis D, Plouin P, Gotman J, da Silva FL; ILAE DMC Subcommittee on Neurophysiology.
Recommendations regarding the requirements and applications for long-term recordings in epilepsy.
Epilepsia. 2007 Feb;48(2):379-84. PubMed PMID: 17295634.
Back
Return to Home
Epilepsy Monitoring Citation
Title: Epilepsy Monitoring
Authors:
Seattle Children’s Hospital
John Kuratani
Jennifer Hrachovec
Ryan Leininger
Mike Leu
Delia Nickolaus
Coral Ringer
Date: 7/30/12
Retrieval Website: http://www.seattlechildrens.org/pdf/video-EEG-monitoring-for-suspectedepileptic-pathway.pdf
Example:
Seattle Children’s Hospital, Kuratani J, Hrachovec J, Leininger R, Leu M, Nickolaus D, Ringer C.
2012 July. Epilepsy Monitoring Pathway. Available from: http://www.seattlechildrens.org/pdf/videoEEG-monitoring-for-suspected-epileptic-pathway.pdf
Return to Home