Tourette's Syndrome 1 Tourette's Syndrome Introduction to
advertisement

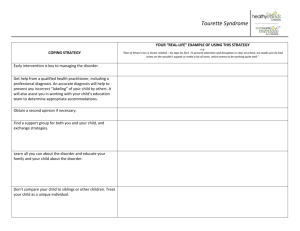
Tourette’s Syndrome 1 Tourette’s Syndrome Introduction to Psychology 85-102 Kathy Chen Tourette’s Syndrome 2 Abstract This paper describes of the symptoms of Gilles de la Tourette’s Syndrome and the treatment options available for those who have this disorder. One case study of a man with Tourette’s is examined, which provides information about the disorder’s effect on his social interactions with others as well as his explanations for the irresistible tics he experiences. The three main types of treatment methods – medicinal, behavioral, and the natural reduction of symptoms with time – are discussed. Then, a specific experiment which describes a girl named Susan and her successful treatment with a behavioral remedy is discussed. Tourette’s Syndrome 3 Tourette’s Syndrome Tourette’s is an intriguing disorder. Fully known as Gilles de la Tourette’s Syndrome, this disorder was so named because French neurologist Georges Albert Edouard Brutus Gilles de la Tourette first described the medical symptoms for this condition in 1884. The bizarre symptoms, often including visible and frequent motor tics and the screaming of obscenities, as well as its rarity, make this disorder a topic of interest. This paper examines Tourette’s syndrome with a focus on the symptoms and causes, the kinds of treatments available for this disorder, and what may be the best treatment method for patients. Tourette’s Syndrome typically onsets during childhood. The most obvious symptoms are the motor and verbal tics, known as coprolalia and copropraxia, respectively referring to the involuntary display of rude words and gestures. “Tics” are defined as repeated and involuntary muscle contractions and sounds. The frequency of the tics is known to fluctuate and include eye blinking, twitching, grunting, and head shaking. (Phelps, 2008) The afflicted often will have social inappropriateness, trouble with the law, coprolalia, and copropraxia (Channon et al, 2009). Both types of tics must be present in order to diagnose the person with Tourette’s. If only one symptom is present, the patient’s disorder would be diagnosed as either chronic motor or visual tic disorder. Tics may occur from one to a thousand times per hour (Friedman, 1980). In addition to this criteria, the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) dictates that these symptoms must be present for more than one year. This disorder typically appears at the age of 9 for children and is three times more common in males than in females. Its prevalence rates are 0.6% and 0.8% for children and adolescents. The broader category of chronic tic disorders has a higher prevalence rate of 3% to 5% (Phelps, 2008). Tourette’s Syndrome 4 The specific cause of Tourette’s is still under debate. However, it is clearly caused by a combination of many different factors. Genetics, for example, plays a role – if one identical twin has Tourette’s, for example, the other is highly likely to have either Tourette’s as well or another tic disorder. A recent longitudinal study on children concerning Tourette’s has revealed that those with both parents diagnosed with Tourette’s were three times more likely to develop it as children who had only one parent with this disorder. Genetic studies have been conducted in an attempt to find the erroneous genes that cause Tourette’s, but no results have shown consistent and conclusive results. Scientists have concluded that Tourette’s is a disorder that involves a complex interaction between multiple genes. Although environmental factors cannot be ruled out, the evidence found so far has pointed to primarily genetic causes of Tourette’s (Phelps, 2008). What may give further and more detailed insight into this disorder are the case studies. There is one 34-year-old doctor (at the time of the case study) who experienced tics since four years of age. He began with vocal tics – a sharp, intense shriek in the very beginning, then a harsh gulp of air as he entered his early school years. He also developed motor tics such as a twitching of the head between the ages of 8 and 10. As is typical of communities of young students, these tics singled him out. The first case was in the school choir, where his choirmaster suggested he be “tranquilized” for his distracting head tics. In secondary school, he was often bullied for his gulps and head twitches. Although he did have friends, few consistently stood up for him. “I remember feeling thoroughly miserable,” he describes of this time period in the case study. In university, however, he had a much easier time integrating himself with the campus community. From then on, his life went smoothly – his medical career was successful and he later married. Tourette’s Syndrome 5 In describing the tics, this person noted that they came and went in intensity but never fully disappeared, from the onset of his tics at age four to today. Tics were most intense when he made an active effort to suppress them -- in times when he most didn’t want the tics to appear, such as when meeting an attractive girl or making an important presentation, they did. Later on in life, he notes that there was a physical sensation accompanied with the tics. They were not truly involuntary, as many people believe; rather, there is a strong mental or physical sensation that occurs and triggers the need to tic. Ticking, as this person describes it, is a reflex to relieve this sensation – much like when one reaches to scratch a mosquito bite. The person does have control over himself and the movement is not involuntary (Turtle and Robertson, 2008). In addition to the tics, he has noticed that he has obsessive compulsive behaviors. This in fact is common amongst Tourette’s patients. This particular patient has, for example, an obsessive worry about whether his car is locked or not. It bothers him to the point that he must return to the vehicle and check to make sure it has been locked. He also fidgets a lot and has a short attention span. Another compulsive behavior is his need to have a banknote pressed in the center of his palm. These compulsions are more conscious than the tics and can be suppressed if he makes an active effort to do so (Turtle and Robertson, 2008). In addition to obsessive and compulsive behaviors, Tourette’s is also linked to attention-deficit hyperactivity disorder (ADHD) for which a short attention span is characteristic. Successful treatment for Tourette’s is usually defined as a significant reduction in the frequency and intensity of both verbal and motor tics. Typically, antipsychotic medications, otherwise known as “typical and atypical neuroleptics”, are used as they are considered the most effective medicinal treatments. The most effective medications, with their efficiency established through numerous double-blind and placebo-controlled tests, include haloperidol and pimozide. Tourette’s Syndrome 6 This type of medication, however, has side-effects including Parkinson-like symptoms such as muscular rigidity, tremors, shuffling walk, and drooling. For children, risperidone and ziprasidone were found to be superior to the aforementioned medications because they have fewer side-effects. Other medicinal options include clonidine and gaunfacine, which were intended to treat high blood pressure, but reduce tics and impulsivity (Phelps, 2008). Those who do not wish to consult medicine might opt to try a behavioral remedy. One method is called “response prevention”, in which patients experience two-hour long sessions of exposure to the urges that precede tics; these patients become used to the pre-tic sensations which reduces tics. Or else, children may predict oncoming tics and learn to suppress these in what is called “habit reversal” (Phelps, 2008). One study was conducted over a period of 18 months with a 11-year-old patient named Susan with coprolalia – the tic that involved uttering obscenities. She was taught to substitute in non-obscene words, such as “fun”, when she felt the need to yell obscene ones. From an initial average of 150 obscenities per hour, Susan was able to decrease her verbal tics significantly with the encouragement of her parents. Within a few weeks, her cursing had almost disappeared. Susan was taught relaxation techniques as well as positive imagery in order to help reduce her motor tics. During these practice sessions, her motor tics disappeared completely. However, during stressful times, Susan often forgot to utilize these techniques and her ticking returned. At the end of this 18-month therapy, Susan’s ticking had decreased dramatically; she and her parents felt that these techniques were highly beneficial (Friedman, 1980). Susan’s treatment was clearly very effective. Although her therapy was lengthy, perhaps the time required could be decreased in older patients who, perhaps due to social reasons, have a stronger desire to suppress verbal and motor ticking. Nevertheless, the treatment used for Susan, Tourette’s Syndrome 7 habit reversal, appears to be a good alternative for Tourette’s patients who do not wish to use medicinal treatments due to the side-effects or other reasons. Response prevention has been shown to have about the same high level of efficacy as habit reversal (Phelps, 2008). The final method of treatment, as of now, is simply time. A significant reduction in tics occurs naturally by the age of 19 or 20, and one affected by Tourette’s could choose to wait for that (Phelps, 2008). Of course, waiting for the tics to recede naturally is not guaranteed; Tourette’s-afflicted adults still tic although often to a lesser degree. Going without treatment may not be the best option, however. Those who have Tourette’s experience the worst of the symptoms during their childhood and adolescence. The social consequences of freely exhibiting tics often include teasing, bullying, and estrangement, as seen in the case study examined. The psychological impact on the child may have very negative effects for self-esteem, especially during school age years when the child’s peers are more prone to making hurtful comments, The best treatment of Tourette’s symptoms out of the methods described – between antipsychotic medications, behavioral remedies, and simply letting time take its toll – is perhaps the behavioral method. As in Susan’s case, the symptoms were drastically reduced within the length of the experiment. Those who use this method will not have to deal with recurring and costly medication fees and also would not have to deal with the side-effects involved in taking medication. By learning to suppress tics, one can maintain a more long-term effect of tic reduction. Behavioral methods such as response prevention, therefore, may be the best option for Tourette’s patients. To conclude, Tourette’s is a fascinating disorder. It usually onsets in early childhood and is characterized by motor and vocal tics, both of which often draw unwanted attention to the affected. Tourette’s patients are likely to have ADD and OCD as well, but experience no Tourette’s Syndrome 8 neurological impairment compared to the average human. In dealing with the disorder, one can undertake any of the treatment methods mentioned above. The literature present was effective in answering the main question of this paper. There were several different studies done to test treatment methods detailed in the database I consulted alone; outside of this one database, surely there is a much larger base of information about Tourette’s. Only further research and experimentation can provide more information about the disorder and treatment methods. Tourette’s Syndrome 9 References Channon, S., Drury, H., Martinos, M., Robertson, M. M., Orth, M., & Crawford, S. (2009). Tourette's Syndrome (TS). Neuropsychology. 23(3), 359-366. Friedman, S. (1980). Self-control in the treatment of Gilles de la Tourette's syndrome: Case study with 18-month follow-up. Journal of Consulting and Clinical Psychology. 48(3), 400-402. Phelps, L. (2008). Tourette's Disorder. School Psychology Quarterly. 23(2), 282-289. Turtle, L., & Robertson, M. M. (2008). Tics, Twitches, Tales. American Journal of Orthopsychiatry. 78(4), 449-455.