SAMPLE QUESTIONS WRITTEN CASE STUDIES EXAMINATION
advertisement

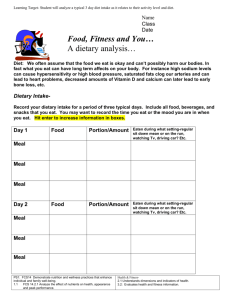
SAMPLE QUESTIONS WRITTEN CASE STUDIES EXAMINATION Sample Clinical Nutrition Case Study George T is a 42 year old man with severe chronic obstructive pulmonary disease. He has been referred to the Respiratory Clinic for a nutrition assessment in view of lung transplantation. George receives sickness benefits, lives alone and is often anxious and depressed. His health affects his day to day functions and he is very limited in what he is able to do. He attends physiotherapy at the hospital twice a week for rehabilitation. He has never seen a dietitian before. Weight history: Height: 183cm Current Weight: 61kg BMI 18 Usual weight: 77kg Weight loss has occurred gradually over the last 6 years. George has had 5 hospital admissions this year. To receive a lung transplant, George must reach a goal weight of 67 kg. Diet history: Breakfast: Lunch: Dinner: Snacks: 1x Weetbix, milk, sugar Soup, occasionally yogurt Small meal of meat, potato and vegetables, (sometimes too tired to eat) Rarely Questions 1. Provide a summary nutrition assessment for George, noting any assumptions made. 2. Identify and justify the optimal clinical goals and objectives of dietary management for George in order of priority. Include quantifiable goals. 3. Outline a client-focused approach for implementing these goals, including your suggested changes. 4. Prepare a plan to evaluate the effectiveness of your intervention. Clinical Case Sample Answer 1. Provide a summary nutrition assessment for this client, noting any assumptions made. BMI places George in the underweight category. His usual BMI is 23 so the weight loss is significant. He has lost greater than 10% of his body weight indicating malnutrition is likely. No biochemistry results provided. Clinically he reports insufficient energy to be able to do ADL’s (Activities of daily living). Tiredness suggests the possibility of anaemia. Dietary intake compared to core food groups: About 1 serve cereal (should be at least 4). No fruit 2 vegetable serves (should be 4-5) Meat/ alternatives – may be sufficient but not for weight gain Dairy/ alternatives – inadequate Inadequate protein, energy and nutrient intake His psychosocial history suggests support will be important/ what support does George have?. 2. Identify and justify the optimal clinical goals and objectives of dietary management for George in order of priority. Answer should include quantities for all of these ( eg how much weight gain) Adequate nutrients and energy to meet requirements (include calculation/reference to protein and energy requirements for weight gain); (consider if patient may have fluid or sodium restrictions) Acceptable food that client can manage Gradual weight gain (indicate rate of weight gain and link to energy requirements) Continual follow-up and goal setting Consider social/psychological assistance from other team members 3. Outline a client-focused approach for implementing these goals, including your suggested meal plan. Consult with client re food preferences and high energy and protein requirements at the moment explaining that usual dietary restrictions or practices may need to be altered (however, must consider if patient may have fluid or sodium restrictions important for health and well being) Discuss options with client, family/ client support group for high protein and energy supplements in a variety of forms and possible sources eg hospital supply, family bring in Arrange with appropriate personnel (hospital staff) for supplements to be provided and monitoring of intake to occur Clarify any concerns of client/ family/ support group Sample meal plan should show small frequent meals/ snacks spread over the day using variety of high protein, high energy products/ dishes, including easy and cheap options such as adding skim milk powder to breakfast milk, biscuits and snacks or toast, butter and jam; nourishing drinks such as coffee made on milk. The hospital may supply oral supplements and these can be included in the meal plan. Note: Providing a detailed meal plan is a useful way of demonstrating your implementation plan, but still detailing priorities is important. Suggest help groups such as meals on wheels, meal programs, shopping or cooking services etc Ensure practical, realistic and feasible strategies and support provided Note: ensure that your implementation plan is designed to meet the goals you set in question 2 above. That is can the suggested meal plan provide enough energy and protein to achieve restoration of nutritional status and weight gain? 4. Prepare a plan to evaluate the effectiveness of your intervention. Measures to monitor: o Anthropometry – increased weight, waist measurements, skin-fold thickness o Biochemistry – Appropriate albumin levels and iron status achieved and or maintained o Clinical - symptoms to diminish, improvement in general well being o Dietary – can identify changes required, (knowledge), diet history indicates better food choices and intake, improvements in attitudes, skills and behaviour changes eg cooking methods, label reading OR if in hospital monitor food intake via food record. Short term vs long term goals considered Time line provided (that is what are the expected changes and over what time frame?) Recording or documentation noted Consider process ( client satisfaction, willingness and actual returning or providing feedback) and effectiveness ( achievement of goals and objectives set) Could include contingency plan for failure to attend. Interpretation of failure to attend follow up. In this case you need to describe a contingency plan for failure of client in achieving adequate food intake.