- Asian Nursing Research
advertisement

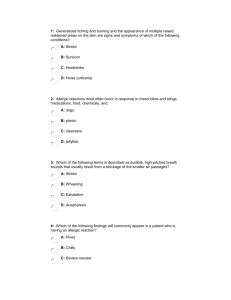
O R I G I NA L A R T I C L E Geographical and Sociodemographic Risk Factors for Allergic Diseases in Korean Children Hyejung Lee, PhD, RNC, APRN, Gwang Suk Kim*, PhD, RN Assistant Professor, College of Nursing, Yonsei University, Seoul, Korea Purpose (a) To examine geographical distribution of childhood allergic diseases in Korea and (b) to identify geographical and sociodemographic risk factors for allergic diseases. Methods Data on doctor-diagnosed asthma during lifetime and allergic rhinitis and atopic dermatitis during the past 12 months of 8,631 children (≤ 18 years) were obtained from the Third Korea National Health and Nutrition Examination Survey, along with information on housing type and presence of an indoor smoker. The SaTScan program identified geographical case clusters of allergic diseases, and multiple logistic regression determined risk factors, including geographical case clusters, for each allergic disease. Results Prevalence of asthma, allergic rhinitis, and atopic dermatitis was 3.2%, 13.2%, and 15.5%, respectively. Older children (10–18 years) were more likely to have allergic rhinitis whereas younger children were more likely to have atopic dermatitis. It is noteworthy that children living in areas of geographical risk for asthma and atopic dermatitis were more likely to develop the respective allergic disease than children living in other areas (odds ratio [OR] = 3.47 for asthma, and OR = 9.74 for atopic dermatitis). Conclusions This study indicates that the areas in which children live may influence the development of certain allergic diseases. Implications include the need to assess geographical location of children with allergic diseases and to develop community-based preventive programs for children with allergic diseases. [Asian Nursing Research 2011;5(1):1–10] Key Words allergic rhinitis, asthma, atopic dermatitis, geographic factor, Korea INTRODUCTION During the past 2 decades, the increasing prevalence of allergic diseases such as asthma, allergic rhinitis, and atopic dermatitis has become a significant public health issue in Asia as well as in Westernized countries (Barnetson & Rogers, 2002; Lee & Hwang, 2008; Zar, Ehrlich, Workman, & Weinberg, 2007). In Korea, the current prevalence in children and adolescents ranges from 8% to 10% for asthma, 10% to 30% for allergic rhinitis, and 16% to 29% for atopic dermatitis, which reports a rapid increase compared to the past decade (Korean National Health Insurance Corporation, 2008). Allergic diseases are well known to be highly heredity (Larsson et al., 2008). When parents have an allergic disease, children are more likely to develop the same allergic disease as well as concomitant allergic diseases (Sarafino, 2000; Sebok, Schneider, & Harangi, 2006). However, the fact that some children *Correspondence to: Gwang Suk Kim, PhD, RN, College of Nursing, Yonsei University, 134 Shinchondong, Seodaemun-gu, Seoul, Korea 120-752. E-mail: gskim@yuhs.ac Received: July 6, 2010 Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 Revised: September 27, 2010 Accepted: December 10, 2010 1 H.J. Lee, G.S. Kim develop allergic diseases even though their parents do not have any, and that the prevalence of allergic diseases varies by country and regions within a country suggest that environmental factors may also play an important role in the development of childhood allergic diseases (Asher & Dagli, 2004; Kurt et al., 2007; Tomac, Demirel, Acun, & Ayoglu, 2005; Williams et al., 1999). Children living in urban areas and developed countries are more likely to experience asthma and other allergic diseases than children living in rural areas and developing countries (Asher et al., 2006; Dorner, Lawrence, Rieder, & Kunze, 2007; Majeed, Rajar, Shaikh, Majeed, & Arain, 2008; Priftis et al., 2007). These results may be attributed to the air pollution associated with industrialization and to the Westernized lifestyle (Lindgren et al., 2009; Tomac et al., 2005; Zuraimi, Tham, Chew, Ooi, & David, 2008). Several particular environmental risk factors such as exposure to indoor allergens, including pollens, fur of pets, smoking, heating systems, and air pollution, have been reported to be risk factors to develop allergic diseases (Asher & Dagli, 2004; English et al., 1999; Tomac et al.). A higher prevalence of childhood allergic disease is also associated with living in areas of lower altitude (< 1,000 m), higher mean annual temperature (> 15°C), and higher humidity (Kurt et al., 2007). Particular geographical features seem to be associated with the development of allergic diseases (Lindgren et al., 2009; Tomac et al.; Zuraimi et al., 2008). Thus, geographical features should be assessed along with other known risk factors, such as age, gender, and home environment; few studies have investigated the influence of geography on childhood allergic diseases. This study examined the geographical distribution of childhood allergic diseases in Korea and identified geographical and sociodemographic risk factors for allergic diseases in children. The results of this study should assist public health nurses in better understanding how the environment including geographic location may affect a child’s health in relation to allergic diseases. The research questions of this study were (a) what is the geographical distribution of the three childhood allergic diseases such as asthma, allergic rhinitis, and atopic dermatitis in Korea and (b) how the 2 geographical and sociodemographic risk factors, including age, gender, comorbidity of allergic disease, presence of indoor smokers and housing type are associated with the incidence of childhood allergic disease. METHODS Study sample and data In 2009, the population of South Korea was estimated to be approximately 49.0 million. About 70% of South Korea’s land area (100,032 km2) is mountainous, and thus, highly densely populated areas are concentrated in several metropolitan cities, such as Seoul and Pusan, and Gyeonggi province, in the lowland areas. Data for this study were obtained from the Third Korea National Health and Nutrition Examination Survey (KNHNES III) conducted in 2005. This national survey included a basic household and health interview, a medical examination, and a nutrition survey. As the KNHSNES III uses a stratified multistage probability sampling method, with selections made from sampling units based on geographical area, sex, and age groups using household registries, the KNHSNES III data represent the entire Korean population in both urban and rural areas and in all types of housing. For the survey, trained interviewers visited each selected household and interviewed a member of the household using the structured survey questionnaire. The most frequent respondent for the interview was the wife/mother for the family in the survey. Of a total of 34,145 participants who completed the health interview, 8,631 participants who were less than 19 years of age were included in this study. Their age, gender, housing type (house vs. high-rise apartment), and existence of a family member who smokes at home were obtained from the KNHNES III. The allergic disease status in this study was defined by a “yes” response to the following question: “Has your child had asthma diagnosed by a physician during his/her lifetime?” and “Has your child had allergic rhinitis (and/or atopic dermatitis) diagnosed by a physician during the past 12 months?” Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 Risk Factors for Allergic Diseases Analytical strategy Geographic information systems (GIS) have been extensively used to map the incidence of disease and to locate environmental risk factors in relation to geographical areas at both the state and national level (Cromley & McLafferty, 2002; Choi, Afzal, & Sattler, 2006). Because the original KNHNES III does not provide detailed information for GIS analysis in order to keep individual health information confidential, administrative district information of each child which is appeared in the original dataset was used to locate the geographical area of the child. Geographical areas under the same administrative unit of GIS were combined to represent geographical unit data for the study analysis. To map the incidence of allergic diseases to geographical area of Korea, administrative district electronic maps provided by the Korean National Geographic Information Institute were then used (Shin & Um, 2006). The longitude and latitude for each geographical unit were identified using ArcView 3.3 (Environmental Systems Research Institute Inc., Redlands, CA, USA, 2003) GIS software program. To estimate risk ratios for childhood asthma, allergic rhinitis, and atopic dermatitis in a cluster, the number of children by each allergic disease and total number of children surveyed were calculated according to geographical units. The risk ratios and the total number of children for the three allergic diseases (individually and combined) were then used as an input for SaTScan version 8.0 software program (Kulldorff & Information Management Services, 2009). The SaTScan software was originally developed by Martin Kulldorff to perform geographical surveillance of disease, to detect areas of significantly high or low rates. This program is also able to identify statistically significant spatial disease clusters using chi-square tests, allowing the assessment of potential spatial epidemiological risk factors. Finally, multiple logistic regression analysis was used to identify significant risk factors, including the geographical cluster information for each allergic disease in Korean children. All statistical analyses were conducted using SAS, version 9.1 (SAS Institute Inc., Cary, NC, USA) and STATA 10.0 to handle complex survey sampling Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 design and unequal weights. The prevalence of each allergic disease was presented as percentages using weighted sample. Survey logistic regression model was used to estimate the odds ratios in order to examine the association between allergic diseases and other risk factors. RESULTS Prevalence of allergic diseases Table 1 presents the prevalence of allergic diseases in children according to sociodemographic factors. Of 8,631 children, 4,274 (49.5%) were 9 years or under, and 4,463 (51.7%) were boys. The overall prevalence of allergic diseases was 256 (3.15%) for asthma, 1,203 (13.21%) for allergic rhinitis, and 1,379 (15.45%) for atopic dermatitis. Asthma and atopic dermatitis were more prevalent in younger children (≤ 9 years) than in older children (10–18 years). Atopic dermatitis was more common in girls than in boys. Both asthma and atopic dermatitis were more prevalent in children living in high-rise apartments than in children living in regular houses. Children residing in homes with indoor smokers had more allergic rhinitis than children living in homes with no indoor smokers. Geographical distribution of allergic diseases Figure 1 shows the identified geographical clusters on a map of South Korea. Three different symbols indicate areas with relatively high prevalence of certain allergic diseases, for example, circle for asthma, diamond shape for allergic rhinitis, and heart shape for atopic dermatitis. Childhood asthma was significantly more prevalent in southeastern Korea, with 21 southeastern clusters identified. Cases of allergic rhinitis were concentrated in northwestern Korea, with 70 clusters. The prevalence of atopic dermatitis was high in one cluster, in northwestern Jeju Island. Table 2 shows geographical risk regions where prevalence of each allergic disease was relatively high, the number of cases indicating the actual number of children with respective allergic disease, and expected cases calculated statistically. The expected cases 3 H.J. Lee, G.S. Kim Table 1 Prevalence of Allergic Diseases According to Sociodemographic Factors Asthma Characteristics n (%) n %a Allergic rhinitis n %a Atopic dermatitis n %a Age (yr) ≤9 10–18 4,274 (49.5) 4,357 (50.5) 145 111 3.49 2.78 578 625 11.13 15.48 920 459 21.45 8.92 Gender Boy Girl 4,463 (51.7) 4,168 (48.3) 163 93 3.81 2.46 711 492 15.04 11.30 641 738 14.30 16.66 256 1,203 1,379 78 30.47 78 61 7.29 5.93 61 292 29.12 24.24 292 20.72 Living in a high-rise apartment Yes No 4,434 (51.4) 4,197 (48.6) 139 117 3.40 2.85 695 508 12.90 13.59 721 658 15.58 15.31 Indoor smoking Yes No 1,028 (11.9) 7,603 (88.1) 39 217 .00 3.19 139 1,064 27.48 13.05 95 1,284 15.44 15.47 Total 8,631 256 3.15 1,203 13.21 1,379 15.45 Comorbidity Asthma Allergic rhinitis Atopic dermatitis a This indicates weighted prevalence rate. refer to the same number of inside and outside the cluster when the null hypothesis is true, that is, when the risk of inside and outside is same. In the Table 2, annual rate per 100,000 is calculated based on the average length of a year of 365.2425, taking leap years into account and relative risk is the estimated risk (the actual number of cases divided by the expected within the cluster) divided by the estimated risk (the actual divided by the expected outside the cluster) outside the cluster. The log likelihood ratio testing whether the geographical risk clusters is statistically different from the other geographical cluster in terms of incidence of allergic disease found that the geographical clusters for all three allergic diseases were statistically significant with p of .003 for asthma, .003 for allergic rhinitis, and .001 for atopic dermatitis. The p is calculated for the detected clusters using computer simulations (Monte Carlo randomization) due to unknown probability distribution of the clusters (Kulldorff, 2010). The Monte Carlo p is 4 the rank of the observed maximum log likelihood ratio among the 999 maximum log-likelihood ratios from the Monte Carlo replicates divided by 1,000 (Abrams, Kulldorff, & Keinman, 2006). Table 3 shows whether or not living in geographical risk regions affect the incidence of allergic disease using weighted chi-square tests on geographical risk regions. All three allergic diseases were significantly associated with living in certain geographical areas. This indicates a strong association between living in areas where is highly prevalent of an allergic disease and development of an allergic disease. Risk factors for allergic diseases Table 4 shows the results of weighted multiple logistic regression analyses. Younger children (< 10 years) were 2.86 times for atopic dermatitis than older children (10–18 years) whereas allergic rhinitis was 1.74 times more likely to be found in older children. Boys were 1.39 times more likely to have allergic rhinitis Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 Risk Factors for Allergic Diseases than girls. Children with one allergic disease were more likely to have another allergic disease. Both living in a high-rise apartment and exposure to indoor smoking were not associated with the incidence of any allergic diseases. The odds ratios for geographical area risk factors were 3.47 for asthma, and 9.74 for atopic dermatitis when other risk factors were controlled for. In other words, children living in high prevalence areas for asthma and atopic dermatitis were more likely to have the respective allergic disease than those living in other areas. DISCUSSION Asthma Allergic rhinitis Atopic dermatitis Figure 1. Geographical distribution of childhood allergic diseases in Korea. This is the first study demonstrating the significant relationship of geographical location as well as sociodemographic risk factors to the incidence of childhood allergic diseases using a nationally representative sample of Korean children. The estimated prevalence of allergic diseases was 3.15% for asthma, 13.21% for allergic rhinitis, and 15.45% for atopic dermatitis in Korean children under age of 18. Compared to Table 2 Geographical High Risk Areas for Allergic Diseases Geographical risk region No. of cases Expected cases Annual cases/100,000 Relative risk Log likelihood ratio Monte Carlo rank p Asthma Allergic rhinitis 96, 95, 101, 98, 91, 100, 99, 93, 92, 97, 94, 79, 74, 75, 83, 72, 71, 84, 57, 176, 175 44 20.28 6,418.3 2.41 11.59 3/1,000 228, 227, 226, 218, 219, 225, 102, 220, 104, 105, 103, 107, 106, 35, 217, 216, 48, 73, 46, 47, 221, 40, 12, 13, 24, 29, 53, 26, 25, 71, 72, 81, 41, 27, 52, 213, 214, 223, 5, 224, 21, 6, 7, 32, 23, 37, 39, 42, 22, 203, 36, 204, 33, 34, 215, 38, 199, 160, 127, 159, 126, 49, 208, 50, 30, 198, 154, 31, 153, 128 491 402.39 16,965.7 1.22 14.21 3/1,000 22 5.89 59,499.0 3.73 12.97 1/1,000 .003 .003 .001 Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 Atopic dermatitis 209 5 H.J. Lee, G.S. Kim Table 3 Prevalence of Allergic Diseases by Geographical Risk Region Allergic diseases High-risk region (weighted %) Low-risk region (weighted %) c2 p 0.62 6.49 2.53 90.36 16.073 <.001 5.05 27.44 8.16 59.35 4.678 <.05 0.19 0.13 15.27 84.42 9.459 <.01 Asthma Yes No Allergic rhinitis Yes No Atopic dermatitis Yes No Table 4 Multiple Logistic Regression to Examine Sociodemographic and Geographical Risk Factors for Allergic Diseases Asthma Allergic rhinitis Atopic dermatitis Variable OR 95% CI OR 95% CI OR 95% CI Age (10–18 yr) 0.88 0.49–1.58 1.74* 1.26–2.40 0.35* 0.24–0.51 Gender (Boy) 1.54 0.86–2.75 1.39* 1.06–1.83 0.79 0.58–1.07 Comorbidity Asthma Allergic rhinitis Atopic dermatitis 2.74* 1.47–5.09 2.70* 2.10* 1.44–5.05 1.15–3.85 2.04* 2.18* 1.09–3.80 1.46–3.26 2.14* 1.44–3.18 Living in a high-rise apartment 1.24 0.68–2.26 0.93 0.69–1.25 1.00 0.72–1.39 Exposure to indoor smoking 0.71 0.26–1.96 0.83 0.52–1.34 0.86 0.46–1.61 Living in high geographical risk area 3.47* 2.04–5.92 1.31 0.94–1.84 9.74* 7.56–12.54 Note. OR = odds ratio; CI = confidence interval. *p < .05. recent study on childhood prevalence of allergic diseases, which reported asthma, allergic rhinitis, and atopic dermatitis in children aged 6–13 at 7.8%, 27.9%, and 28.2%, respectively (Jee et al., 2009), the results of our study report somewhat lower prevalence. This may be attributed to the greater age ranges in our study than in the other and differences in assessing atopic diseases. Jee et al. (2009) used data from self-reported symptoms of allergy in elementary school students while our study used the survey answers to the question “Have you have been diagnosed any allergic diseases by physician during the last year?” Thus, our data can be considered to be 6 based on doctor-diagnosed allergic disease, although self-report measure was used. In general, prevalence using doctor-diagnosed allergic disease is lower than other measures, such as self-reported allergic symptoms. In addition, during the past decade, a nationwide campaign on awareness of childhood allergic diseases has been carried out in Korea and this campaign might have contributed to people being aware of symptoms of allergic diseases, resulting in the increase in incidence of allergic disease symptoms. The results of the present study show remarkable geographical differences in the incidence of childhood asthma in Korea. The highest prevalence of asthma Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 Risk Factors for Allergic Diseases is shown in southeastern Korea, concentrated in Daegu City and its surrounding areas, such as Ulsan. The high prevalence of asthma in Daegu may be explained by its geographical features; it is a large, industrialized city located in a valley surrounded by mountains. In general, the air flow in valleys is more sluggish than it is over flat land or along coast; thus it may result in atmospheric congestion and possibly an elevation in the degree of air pollution (Meng et al., 2010). Air pollution is often reported to be associated with morning cough, bronchitis, and respiratory symptoms including asthma (Hirsch et al., 1999; Lindgren et al., 2009). Daegu is often covered with smoke because the industrial complex is located at the entry point for seasonal winds (Shin & Um, 2006; Um & Shin, 2002). It is likely that these geographical features of Daegu, the valley formation and the construction of industrial facilities, seem to contribute to children’s vulnerability to asthma. Ulsan, located in the coastal region, is another highly industrialized area, where the big automobile factories are located, resulting in the highest air pollution in Korea. A higher prevalence of asthma is reported in coastal regions, which have relatively higher temperatures and humidity as well (Kurt et al., 2007). Thus, these findings of high asthma prevalence in Daegu and Ulsan are in line with the results of previous studies (Ciccone et al., 1998; Hirsch et al., 1999; Jee et al., 2009). When a geographical risk is included as a variable in the logistic regression with sociodemographic risk factors to identify the association with development of asthma, only comorbidity and living in high geographical risk area are significantly associated with the incidence of asthma in children. This is interesting result because even after the known risk factors for childhood asthma such as gender and indoor smoking were adjusted for, geographical risk area was still found to be significant to associate with asthma. Strachan, Golding, and Anderson (1990) also reported regional effects of current residence upon wheezing illness using British children who experienced interregional migration. Higher prevalence of wheeze among children was highly associated with living in a high risk region, while there were no difference between region Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 of birth and prevalence of wheezing illness. Thus, these studies stressed where to reside is a significant factor for childhood asthma incidence and may suggest that public health nurses be alert to assess geographical factors as well as other known sociodemographic risk factors. In terms of allergic rhinitis, the geographical clusters are mostly concentrated in the northwestern area of Korea, an area of highly populated and densely crowded cities, including the capital city Seoul, and Gyeonggi province. These areas have undergone rapid Westernization and economic development during the past 2 decades, and there are newly constructed high-rise apartments to resolve the housing problems of the recent migrant population. Although the exact cause of the effect that living in a newly constructed apartment has on developing allergic diseases has to be determined, Platts-Mills, Vervloet, Thomas, Aalberse, and Chapman (1997) and Hirsch et al. (2000) pointed out the increased prevalence of allergic sensitization to indoor allergens occurred in the newly constructed apartments, which are equipped with insulated windows and central heating. Venn et al.’s (2001) study also showed strong positive associations between allergic symptoms and the domestic use of modern fuels for cooking and heating in urban areas. Based on these studies, it can be said, with caution, which living in a high-rise apartment in a westernized city might be associated with the development of childhood allergic diseases. In the logistic regression, only older age and being a boy are associated positively with allergic rhinitis. Unlike asthma, allergic rhinitis was not associated with living in high geographical risk area. Allergic rhinitis was not associated with indoor smoking, although higher prevalence showed in children living in homes with indoor smokers in descriptive analysis. This finding was inconsistent with other studies that reported that symptoms of allergic rhinitis were associated with exposure to environmental tobacco smoke in young children (Zuraimi et al., 2008). Although a few metropolitan cities show significantly higher prevalence in the geographical distribution of allergic rhinitis in Korea, allergic rhinitis in this study seems to be less correlated with environmental factors. 7 H.J. Lee, G.S. Kim In our study, one specific geographic area in the geographical distribution shows a high prevalence for atopic dermatitis. The children living in Aeweol area were nearly 10 times more likely to be developed atopic dermatitis than children living in all other areas of Korea. Aeweol is located on the north side of Jeju Island, which is the biggest island in Korea and is less industrialized than other parts of Korea; thus it retains its natural beauty. Because Aeweol is a very small village with a population of 25,000 in 201.88 km2 and is located near a harbor, the causative factor in the development of atopic dermatitis living in this area may possibly be related to environmental hazards, such as the harbor or perinatal exposure to allergens, although this phenomenon remains to be investigated. Bae and Shin (2009) reported that the students who had atopic dermatitis in Jeju had a higher number of recurrences compared with the students in other communities, however they did not provide explanation about why a higher recurrence rate of atopic dermatitis was noted. Interestingly, among risk factors for atopic dermatitis, including younger age, comorbidity, and living in geographical risk region, living in geographical risk region had relatively the strongest relation with the development of atopic dermatitis in Korean children (odds ratio = 9.74). This finding suggests that other possible factors in terms of geographical area need to be investigated for atopic dermatitis incidence and to develop preventive interventions for children living in that area as well. In this study, strong associations between comorbidity of allergic diseases were also found. The fact that children with one allergic disease are more likely to have other allergic diseases may in part support the role that genetic influences play in developing allergic diseases. Gustafsson, Sjoberg and Foucard (2000) showed that among children with atopic dermatitis at 3 years of age, 43% developed asthma and 45% developed allergic rhinitis during the 4-year followup period. Hamouda, Karila, Connault, Scheinmann, and de Blic (2008) found that 58.7% of the asthmatic children in their sample also had allergic rhinitis, and they stressed that allergic rhinitis and asthma were frequently associated. Lee and Hwang (2008) 8 confirmed that Korean children with asthma or allergic rhinitis were 1.6 times more likely to have atopic dermatitis.Allergic diseases in regions with high prevalence may also be attributed to genetic background by exposure of parents to different environmental allergenic factors that are then passed on to their children. Thus, the risk factors for developing childhood allergic diseases should include genetic and sociodemographic factors as well as geographical area factors. There are several limitations to this study. As this study was a cross-sectional study design, it is difficult to assess if geographical area risk is associated with the onset of allergic diseases or only triggers an existing allergic disease. The fact that the data were obtained from respondents to interviews, mostly by the mother, instead of medical records can be a limitation of the study. Although the interviewers were trained in advance in how to collect data and how to ask questions using the same questionnaire, we could not control interrater reliability. Because this study did not include detailed environmental characteristics of the regions, further study is recommended to address the precise etiology of factors contributing to disease in relation to the characteristics of the regions that have a high prevalence of these diseases. CONCLUSIONS The results of this study distinctly demonstrate the existence of high-risk areas for physician-diagnosed allergic diseases in Korean children and a significant association with geographical areas in explaining in the incidence of childhood asthma and atopic dermatitis. Each of the three allergic diseases was found to be distributed in the respective region, and thus, the distribution of diseases may be related to environmental hazards that may contribute to differences in the prevalence of allergic diseases in Korea. The results of this study suggest that public health nurses should assess environmental factors of the area as well as other known sociodemographic risk factors when caring for children with allergic diseases, and they should plan prevention programs that take Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 Risk Factors for Allergic Diseases geographical epidemiological risk characteristics into account. Identification of geographical risk areas has been targeted in efforts to prevent the spread of disease because environmental factors not only affect large portions of the population, but are also modifiable. As shown in this study, Aeweol, a village on Jeju Island, deserves an investigation of environmental features that are potentially associated with allergic diseases in children. Policy on environmental health, including air quality, toxic waste, and healthy homes and communities, also needs to be developed based on the characteristics of each region. Public health nurses should play an important role in continuously monitoring indoor and outdoor environments that may affect the incidence of childhood allergic disease. Considering the risk of particular geographical areas, national initiatives and further study could be suggested to prevent allergic diseases in these populations and geographical areas. REFERENCES Abrams, A. M., Kulldorff, M., & Kleinman, K. (2006). Empirical/asymptotic p-values for Monte Carlo-based hypothesis testing: an application to cluster detection using the Scan statistic. Advances in Disease Surveillance, 1, 1. Asher, I., & Dagli, E. (2004). Environmental influences on asthma and allergy. Chemical Immunology & Allergy, 84, 36–101. Asher, M., Montefort, S., Bjorksten, B., Lai, C., Strachan, D., Weiland, S., et al. (2006). Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet, 368, 733–743. Bae, J. M., & Shin, K. S. (2009). Estimating the prevalence of atopic dermatitis in school students of Jejudo, Korea. Journal of Preventive Medicine & Public Health, 42, 171–176. Barnetson, R. S. C., & Rogers, M. (2002). Childhood atopic eczema. British Medical Journal, 324, 1376–1379. Choi, M., Afzal, B., & Sattler, B. (2006). Geographic information systems: a new tool for environmental health assessments. Public Health Nursing, 23, 381–391. Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1 Ciccone, G., Forastiere, F., Agabiti, N., Biggeri, A., Bisanti, L., Chellini, E., et al. (1998). Road traffic and adverse respiratory effects in children. Occupational & Environmental Medicine, 55, 771–778. Cromley, E. K. & McLafferty, S. (2002). GIS and public health. New York: Human Sciences Press. Dorner, T., Lawrence, K., Rieder, A., & Kunze, M. (2007). Epidemiology of allergies in Austria: Results of the first Austrian allergy report. Wiener Medizinische Wochenschrift, 157(11–12), 235–242. English, P., Neutra, R., Scalf, R., Sullivan, M., Waller, L., & Zhu, L. (1999). Examining associations between childhood asthma and traffic flow using a geographic information system. Environmental Health Perspectives, 107, 761–767. Gustafsson, D., Sjoberg, O., & Foucard, T. (2000). Development of allergies and asthma in infants and young children with atopic dermatitis—A prospective followup to 7 years of age. Allergy, 55, 240–245. Hamouda, S., Karila, C., Connault, T., Scheinmann, P., & de Blic, J. (2008). Allergic rhinitis in children with asthma: a questionnaire-based study. Clinical & Experimental Allergy, 38, 761–766. Hirsch, T., Hering, M., Burkner, K., Hirsch, D., Leupold, W., Kerkmann, M. L., et al. (2000). House-dust-mite allergen concentrations (Derf 1) and mold spores in apartment bedrooms before and after installation of insulated windows and central heating systems. Allergy, 55, 79–83. Hirsch, T., Weiland, S. K., von Mutius, E., Safeca, A. F., Grafe, H., Csaplovics, E., et al. (1999). Inner city air pollution and respiratory health and atopy in children. The European Respiratory Journal, 14, 669–677. Jee, H. M., Kim, K. W., Kim, C. S., Sohn, M. H., Shin, D. C., & Kim, K. E. (2009). Prevalence of asthma, rhinitis and eczema in Korean children using the ISAAC questionnaires. Korean Journal of Pediatric Allergy Respiratory Disorders, 19, 165–172. Korean National Health Insurance Corporation. (2008). Report on number of allergic disease as a medical treatment. Retrieved October 5, 2009, from http://www. nhic.or.kr/wbn/wbnc/wbnc_0100.html Kulldorff, M. (2010). SaTScan TM User Guide for version 9.0. Retrieved September 29, 2010, http://www.satscan. org/cgi-bin/register.pl/SaTScan_ Users_Guide.pdf Kulldorff, M., Information Management Services, Inc. (2009). SaTScanTM v8.0: Software for the spatial and space-time scan statistics. Retrieved March 24, 2010, from http://www.satscan.org/ 9 H.J. Lee, G.S. Kim Kurt, E., Metintas, S., Basyigit, I., Bulut, I., Coskun, E., Dabak, S., et al. (2007). Prevalence and risk factors of allergies in Turkey: results of a multicentric cross-sectional study in children. Pediatric Allergy & Immunology, 18, 566–574. Larsson, M., Hagerhed-Engman, L., Sigsgaard, T., Janson, S., Sundell, J., & Bornehag, C. G. (2008). Incidence rates of asthma, rhinitis and eczema symptoms and influential factors in young children in Sweden. Acta Paediatrica, 97, 1210–1215. Lee, Y., & Hwang, S. (2008). Prevalence and risk factors for atopic dermatitis in pre-school and school aged children. Journal of Korean Academy in Child Health Nursing, 14, 285–294. Lindgren, A., Stroh, E., Nihlen, U., Montnemery, P., Axmon, A., & Jakobssson, K. (2009). Traffic exposure associated with allergic asthma and allergic rhinitis in adults: a cross-sectional study in southern Sweden. International Journal of Health Geographics, 8, 25. Retrieved July 23, 2009 from http://www.ij-healthgeographics.com/content/8/1/25 Majeed, R., Rajar, U. D., Shaikh, N., Majeed, F., & Arain, A. (2008). Risk factors associated with childhood asthma. Journal of the College of Physicians & Surgeons Pakistan. 18, 299–302. Meng,Y., Rull, R. P.,Wilhelm, M., Lombardi, C., Balmes, J., & Ritz, B. (2010). Outdoor air pollution and uncontrolled asthma in the San Joaquin Valley, California. Journal of Epidemiology & Community Health, 64, 142–147. Platts-Mills, T.A.E., Vervloet, D., Thomas, W.R., Aalberse, R.C., & Chapman, M. D. (1997). Indoor allergens and asthma: report of the third international workshop. Journal of Allergy & Clinical Immunology, 100(6 Pt 1), S2–S24. Priftis, K. N., Anthracopoulos, M. B., Nikolaou-Papanagiotou, A., Mantziou, V., Paliatsos, A. G., Tzavelas, G., et al. (2007). Increased sensitization in urban vs. rural environment—rural protection or an urban living effect? Pediatric Allergy & Immunology, 18, 209–216. Sarafino, E. P. (2000). Connections among parent and child atopic illnesses. Pediatric Allergy & Immunology, 11, 80–86. 10 Sebok, B., Schneider, I., & Harangi, F. (2006). Familiar and environmental factors influencing atopic dermatitis in the childhood. Journal of European Academy of Dermatology & Venereology, 20, 418–422. Shin, D., & Um, J. (2006). Visualization of asthmatic distribution patterns in accordance with administrative dong using GIS: a case study of Daegu. Korean Environmental Impact Assessment, 15(3), 179–191. Strachan, D. P., Golding, J., & Anderson, H. R. (1990). Regional variations in wheezing illness in British children: effect of migration during early childhood. Journal of Epidemiology & Community Health, 44, 231–236. Tomac, N., Demirel, F., Acun, C., & Ayoglu, F. (2005). Prevalence and risk factors for childhood asthma in Zonguldak, Turkey. Allergy & Asthma Proceedings, 26, 397–402. Um, J., & Shin, S. (2002). Development of a user-friendly information system for river water quality using Web GIS. Korean Journal of Geographical Information System Association, 10, 49–63. Venn, A. J., Yemaneberhan, H., Bekele, Z., Lewis, S. A., Parry, E., & Britton, J. (2001). Increased risk of allergy associated with the use of kerosene fuel in the home. American Journal of Respiratory & Critical Care Medicine, 164, 1660–1664. Williams, H., Robertson, C., Stewart, A., Ait-Khaled, N., Anabwani, G., Anderson, R., et al. (1999). Worldwide variations in the prevalence of symptoms of atopic eczema in the international study of asthma and allergies in childhood. Journal of Allergy & Clinical Immunology, 103(1 Pt 1), 125–138. Zar, H. J., Ehrlich, R. I., Workman, L., & Weinberg, E. G. (2007). The changing prevalence of asthma, allergic rhinitis and atopic eczema in African adolescents from 1995 to 2002. Pediatric Allergy & Immunology, 18, 560–565. Zuraimi, M. S., Tham, K. W., Chew, F. T., Ooi, P. L., & David, K. (2008). Home exposures to environmental tobacco smoke and allergic symptoms among young children in Singapore. International Archives of Allergy & Immunology, 146, 57–65. Asian Nursing Research ❖ March 2011 ❖ Vol 5 ❖ No 1