Hemodynamic Calculations
advertisement

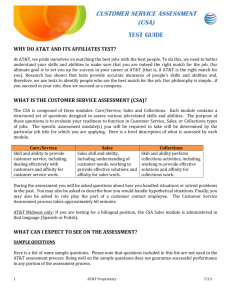
TEE Hemodynamics Amanda J. Rhee, MD Assistant Professor, Dept of Anesthesiology Mount Sinai Medical Center May 4 2010 Outline Volumetric Flow Calculations Velocity and Flow Regurgitant Volume Intracardiac Shunts Stroke Volume and Cardiac Output The Continuity Equation: Valve Area PISA Pressures and Pressure Gradients The Bernoulli Equation Intracavitary Pressures Pressure half-time and deceleration time Velocity and Flow Velocity – the distance blood travels in a given direction per unit time d V = d/t cm/s t Flow – the volume blood passing a given point per unit time Q = CSA * V CSA d t CSA = π * r2 cm3/s Qinstantaneous and Qmean Q = CSA * V Qinstantaneous – volume of blood passing a given point per unit time Qmax = CSA * Vmax Qmean – volume of blood passing a given distance per unit time Qmean = CSA * Vmean VTI = Vmean * t Qmean * t = CSA * Vmean * t SV = CSA * VTI Savage 2005 Stroke Volume Stroke Volume - The volume that is produced by a systolic ejection Step 1: Use Doppler to obtain VTI through area of interest LVOT - Deep transgastric view or Transgastric long axis view Step 2: Use 2-D images to measure diameter and calculate CSA LVOT - Mid-esophageal long axis view SV = CSA * VTI CSA = π * r2 CSA CSA = π * r2 Structure Cross-sectional shape Formula for area LVOT Circle π * r2 or 0.785d2 PISA Hemisphere 2π * r2 MV annulus Ellipse (or circle) π(r1 *r2) or 0.785(d1*d2) AV Equilateral triangle 0.433s2 SV = CSA * VTI Other Applications Right Ventricular Stroke Volume - volume produced by each cardiac cycle by the right side of the heart Pulmonary Artery, RVOT Mid-esophageal ascending aorta short axis, Upper esophageal aortic arch short axis view. Ratio of pulmonic to systemic SV = Qp/Qs Useful to assess the severity of intracardiac shunts Qp/Qs = SVRight heart (RVOT, PA)/SVLeft heart (AoV, LVOT) SV = CSA * VTI Regurgitant Volume Volume that travels opposite to normal direction of flow through a regurgitant lesion in a single cardiac cycle Regurgitant Volume = Flow travelling forward through regurgitant valve – Flow through reference valve RVMV = SV MV – SV AV RVAV = SV AV – SV MV Regurgitant Fraction = RV / SV SV = CSA * VTI Continuity Equation Continuity Equation – mass or volume of blood passing through one site equals the mass or volume passing through another site Based on the principle of conservation of mass CSA 1 * VTI 1 = CSA 2 * VTI 2 CSA AV * VTI AV = CSA LVOT * VTI LVOT SV = CSA * VTI PISA PISA – Proximal Isovelocity Surface Area CSA 1 * VTI 1 = CSA 2 * VTI 2 EROA * VMR peak = 2π r2 * Nyquist Limit * α/180 RV MV = EROA * VTIMR Perrino 2008 SV = CSA * VTI jet Cardiac Output Cardiac Output = SV x HR Cardiac Index = CO/BSA CSA 1 * VTI 1 = CSA 2 * VTI 2 SV = CSA * VTI Bernoulli Equation Describes the relationship between pressure gradients and increases in blood flow velocity across a narrowed orifice Perrino 2008 During peak flow, flow acceleration can be ignored Viscous friction can be ignored because it only contributes significantly in very small orifices In clinically significant lesions, v2 is significantly more than v1, thus v1 can be ignored Simplified Bernoulli Equation: ΔP = 4v22 Bernoulli Equation Perrino 2008 ΔP = P1 - P2 = 4v22 Estimation of RV and PA systolic pressures RVSP (mmHg) = PASP = 4(VTR)2 + RAP In patients without significant RV obstruction or pulmonic valve stenosis, RV and PA systolic pressures are similar RVSP = LV systolic pressure – VSD systolic gradient RVSP (mmHg) = systolic blood pressure - 4(VVSD)2 In the setting of AV stenosis or LVOT obstruction this formula is invalid. ΔP = P1 - P2 = 4v22 PA mean and diastolic pressure PAMP = 4(Vearly PI)2 + CVP PADP = 4(Vlate PI)2 + CVP ΔP = P1 - P2 = 4v22 Estimation of LAP and LVEDP LAP = LV systolic pressure = LA and LV systolic pressure gradient LAP (mmHg) = systolic blood pressure - 4(VMR)2 Invalid with AV stenosis or LVOT obstruction LVEDP = aortic diastolic pressure – end-diastolic aortic and LV pressure gradient LVEDP (mmHg) = diastolic blood pressure - 4(Vend AR)2 In the setting of AV stenosis or LVOT obstruction this formula is invalid. ΔP = P1 - P2 = 4v22 Pressure Half- Time Pressure half-time (PHT) – time required for the peak pressure gradient to decline by 50%. PHT = time required for peak Doppler velocity (Vpeak) to decline to Vpeak√2 MVA = 220/PHT ΔP = P1 - P2 = 4v22 Deceleration Time Deceleration time – time from maximum to zero pressure gradient (which is the same as time from maximum to zero velocity) MVA = 759/DT ΔP = P1 - P2 = 4v22 Thank You References Perrino AC, Reeves ST. A Practical Approach to Transesophageal Echocardiography. Philadelphia: Lippincott W &W, 2008. Sidebotham D, Merry A, Legget M. Practical Perioperative Transesophageal Echocardiography. Philadelphia: Elsevier, 2008. Savage RM, Aronson S. Intraoperative Transesophageal Echocardiography. Philadelphia Lippincott W&W, 2005.