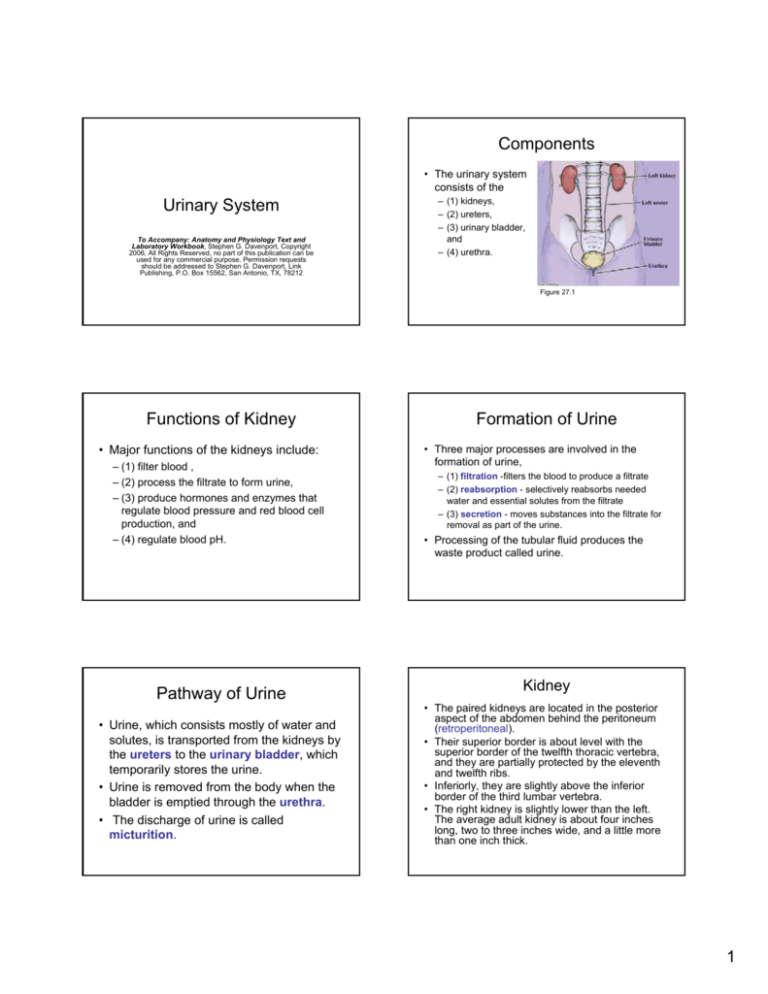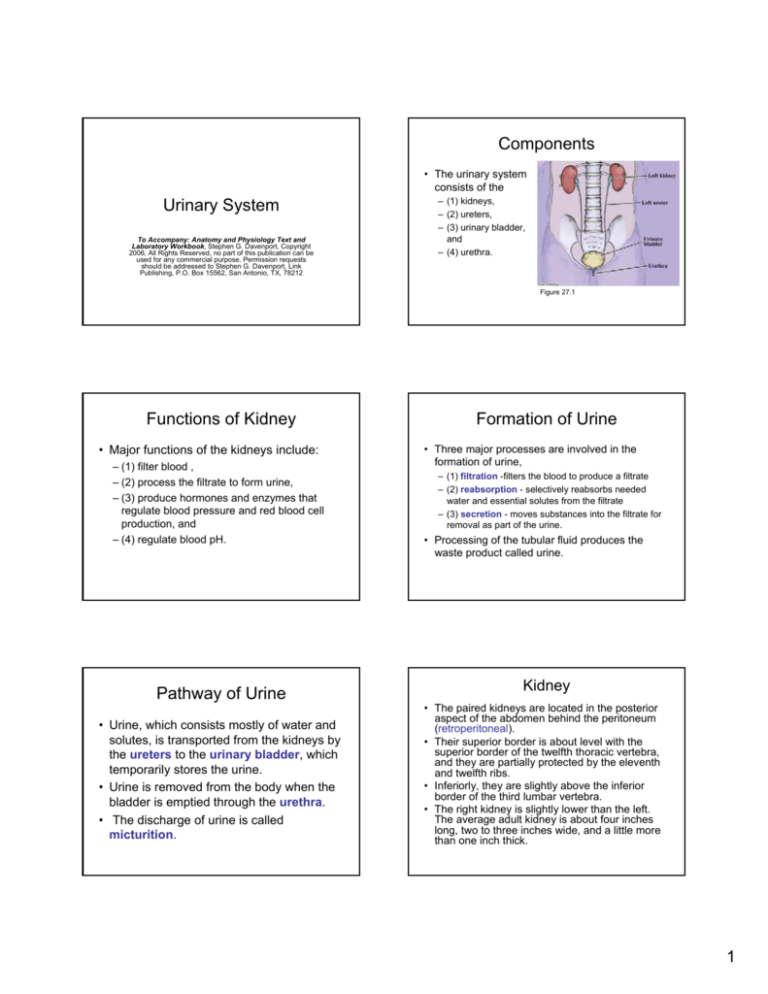
Components
• The urinary system
consists of the
Urinary System
To Accompany: Anatomy and Physiology Text and
Laboratory Workbook, Stephen G. Davenport, Copyright
2006, All Rights Reserved, no part of this publication can be
used for any commercial purpose. Permission requests
should be addressed to Stephen G. Davenport, Link
Publishing, P.O. Box 15562, San Antonio, TX, 78212
– (1) kidneys,
– (2) ureters,
– (3) urinary bladder,
and
– (4) urethra.
Figure 27.1
Functions of Kidney
• Major functions of the kidneys include:
– (1) filter blood ,
– (2) process the filtrate to form urine,
– (3) produce hormones and enzymes that
regulate blood pressure and red blood cell
production, and
– (4) regulate blood pH.
Pathway of Urine
• Urine, which consists mostly of water and
solutes, is transported from the kidneys by
the ureters to the urinary bladder, which
temporarily stores the urine.
• Urine is removed from the body when the
bladder is emptied through the urethra.
• The discharge of urine is called
micturition.
Formation of Urine
• Three major processes are involved in the
formation of urine,
– (1) filtration -filters the blood to produce a filtrate
– (2) reabsorption - selectively reabsorbs needed
water and essential solutes from the filtrate
– (3) secretion - moves substances into the filtrate for
removal as part of the urine.
• Processing of the tubular fluid produces the
waste product called urine.
Kidney
• The paired kidneys are located in the posterior
aspect of the abdomen behind the peritoneum
(retroperitoneal).
• Their superior border is about level with the
superior border of the twelfth thoracic vertebra,
and they are partially protected by the eleventh
and twelfth ribs.
• Inferiorly, they are slightly above the inferior
border of the third lumbar vertebra.
• The right kidney is slightly lower than the left.
The average adult kidney is about four inches
long, two to three inches wide, and a little more
than one inch thick.
1
Kidney
Anatomy of the Kidney
Lab Activity 2 - Dissection
External Anatomy
• Curvatures
– The kidney has two major curvatures, a large lateral curvature
and a small medial curvature. The smaller medial curvature has
an indented area (notch) called the hilus.
• Renal hilus
– The renal hilus is a notch on the medial surface of the kidney
that serves as a passageway for the ureter, blood vessels,
nerves, and lymphatics. The hilus opens into a central area of
the kidney called the renal sinus
• Renal capsule
– The renal capsule is a thin, fibrous capsule that is attached to
the surface of the kidney.
Figure 27.2
Illustration of the kidney (in frontal section) showing general structures.
Anatomy of the Kidney
Lab Activity 2 - Dissection
Figure 27.3
After identification of the kidney’s external anatomy, make a frontal
section through the kidney. This photograph of the sectioned kidney shows the
presence of injected red latex in the ureter, renal pelvis, and calyces. Usually,
the red latex is NOT present in the kidney’s internal cavities.
Anatomy of the Kidney
Lab Activity 2 - Dissection
Anatomy of the Kidney
Lab Activity 2 - Dissection
Figure 27.4
Frontal section of the preserved sheep kidney showing the
general structure of the kidney.
Anatomy of the Kidney
• Renal hilus
– The renal hilus is a notch on the medial surface of the kidney
that serves as a passageway for the ureter, blood vessels,
nerves, and lymphatics.
• Renal sinus
– The renal sinus is the cavity of the kidney that contains the renal
pelvis and the calyces. The renal sinus serves as a passageway
for the renal blood vessels, nerves, and lymphatics.
• Renal cortex
– The cortex is the outer region of the kidney. It is lighter in color
and more granular than the inner region called the medulla. The
cortex contains numerous units of capillaries, the glomeruli,
which give the cortex its granular appearance.
Figure 27.5
Frontal section of the dissected sheep
kidney showing details of internal structures.
2
Anatomy of the Kidney
Anatomy of the Kidney
• Minor calyces
• Renal medulla
– The medulla is the region located to the inside of the renal
cortex. The medulla is formed by striated conical masses called
renal pyramids. The striations are produced by the parallel
arrangement of collecting ducts and loops of Henle.
• Renal pyramids
– The renal pyramids are conical areas that form the renal
medulla. The pyramids are mostly composed of parallel tubules
that give the pyramids a striated appearance. The bases of the
pyramids border the cortex. The apices of the pyramids are
called the renal papillae and project inward into the minor
calyces.
– The minor calyces are small cavities that encircle the renal
papillae. Fluid (urine) that leaves the papillary ducts of the renal
papillae enters the minor calyces and continues into the major
calyces.
• Major calyces
– The major calyces are large cavities that receive several
minor calyces. The major calyces (only two or three in the
kidney) converge inward into the renal pelvis. Urine from the
major calyces drains into the renal pelvis.
• Renal pelvis
– The renal pelvis is the cavity that is located at the convergence
of the major calyces. It is continuous with the ureter.
• Ureter
• Renal columns
– The renal columns are areas of renal cortex that separate the
pyramids. The renal columns mostly serve as routes for
vessels and nerves.
– The ureter is the tube that transports urine from the kidney’s
renal pelvis to the urinary bladder.
Nephrons
Renal Tubule
• The functional units of the kidney are called
nephrons.
• The nephrons begin in the kidney’s cortex
and end with their convergence into
collecting ducts.
• A nephron consists of two major regions,
– (1) a group of capillaries called the glomerulus
and
– (2) a renal tubule.
Collecting Ducts
• Collecting ducts
– receive many distal convoluted tubules and
converge to the papillary ducts.
• Papillary ducts,
– located in the renal papillae, empty into small
cavities, the minor calyces.
• The renal tubule consists of four
divisions, the
– (1) glomerular (Bowman’s) capsule, the
– (2) proximal convoluted tubule, the
– (3) loop of Henle (ascending and descending
limbs), and the
– (4) distal convoluted tubule.
• The distal convoluted tubule unites with a
collecting duct.
Two Types of Nephrons
• There are two major classifications of
nephrons, the
– (1) cortical nephrons and the
– (2) juxtamedullary nephrons.
• Their classification is based mostly upon
the location of the loop of Henle and their
vascularization.
3
Cortical Nephrons
• Cortical nephrons are mostly located in the
kidney’s cortex, with a small portion of
their loop of Henle descending into the
renal medullary pyramids.
• The cortical nephron is associated with
capillaries called peritubular capillaries,
which branch from the efferent arteriole.
• The peritubular capillaries surround the
convoluted tubules and the loop of Henle
Location and Structure of Nephrons
Figure 27.6
Illustration showing the location and structure of cortical and juxtamedullary
nephrons.
Juxtamedullary Nephrons
• Juxtamedullary nephrons begin near the
kidney’s medullary pyramids and their loop of
Henle descends deep into the medullary
pyramids.
• The nephron is associated with two capillaries,
the peritubular and the vasa recta capillaries,
both branching from the efferent arteriole.
– The peritubular capillaries are associated with the
convoluted tubules and
– The vasa recta are associated with the loop of Henle.
Location and Structure of Nephrons
Figure 27.7
Illustration showing the general structure and vascularization of a
juxtamedullary nephron.
Renal corpuscle
• The renal corpuscle consists of the
Anatomy of the Nephron
• glomerulus and its
• glomerular capsule.
4
Glomerulus
• The glomerulus consists of a group of capillaries
housed within the glomerular capsule. The
glomerular capillaries are fenestrated
capillaries, capillaries that are formed from
endothelial cells that have minute membrane
covered pores that enhance filtration
• The glomerulus is covered by cells (podocytes)
of the inner (visceral) layer of the glomerular
(Bowman’s) capsule and a basement
membrane, located between the glomerulus and
the podocytes.
Glomerular (Bowman’s) capsule
•
The glomerular (Bowman’s) capsule is
the cup-shaped end of the nephron which
surrounds the glomerular capillaries.
• It consists of two layers, the
– inner (1) visceral layer and the
– outer (2) parietal layer.
• A capsular space is located between the
visceral and parietal layers.
Visceral Layer of Capsule
Filtration Membrane
• The inner visceral layer, which consists of
specialized cells called podocytes, is
located on the surfaces of the capillaries.
• The podocytes have small extensions call
pedicles that form minute narrow
openings, the filtration slits, which
function in forming a portion of the
filtration membrane.
• The filtration membrane is formed from the
Parietal Layer and Capsular Space
Glomerular (Bowman’s) capsule
– (1) fenestrated endothelium of the
glomerular capillaries, the
– (2) filtration slits of the podocytes (visceral
membrane), and the
– (3) basement membrane (fused basal
laminas of visceral layer and endothelium)
between the capillaries and the podocytes
(visceral membrane).
• Parietal Layer
– The outer parietal layer is the boundary of
the glomerular capsule and consists of
simple squamous epithelium.
• Capsular Space
– Located between the visceral and parietal
layers is the capsular space.
– The capsular space receives filtrate through
the filtration membrane and leads to the
proximal convoluted tubule.
Figure 27.8
The glomerular (Bowman’s) capsule is formed from two layers, the outer
parietal layer and the inner visceral layer. The visceral layer consists of specialized
cells called podocytes. Podocytes form filtration slits that function as part of the
filtration membrane.
5
Renal Tubule
• The renal tubule begins with the glomerular capsule and
leads to the proximal convoluted tubule
• Proximal convoluted tubule
– The proximal convoluted tubule is the twisted portion of the
nephron that leaves the glomerular capsule. It receives filtrate
from the glomerular capsule.
• Loop of Henle
– The loop of Henle follows the proximal convoluted tubule. The
loop of Henle makes a sharp U-turn, with its two portions the
descending limb and the ascending limb lying parallel to each
other.
• Distal convoluted tubule
– The twisted distal convoluted is the last portion of the nephron
and leads into a collecting duct.
Peritubular capillaries
• The peritubular capillaries arise from the
efferent arteriole and surround the renal
tubules located in the cortex.
• They function in
– absorption of water and solutes recovered by
the tubular cells and
– secretion of waste products into the tubules.
• The peritubular capillaries drain into the
interlobular veins.
Afferent and Efferent Arterioles
• Afferent Arteriole
– The afferent arteriole arises from the interlobular
arteries and leads to the glomerular capillaries. It is
larger in diameter than the efferent arteriole.
• Efferent Arteriole
– The efferent arteriole arises from the glomerular
capillaries.
– The efferent arteriole is considerably smaller than the
afferent arteriole which leads to the glomerular
capillaries. The smaller diameter of the efferent
arteriole results in increased blood pressure in the
glomerular capillaries, which promotes capillary
filtration.
Vasa recta
• The vasa recta are capillaries which arise
from the efferent arteriole and paralleling
the loops of Henle descend into the
medulla and then ascend to unite with
veins at the cortical-medullary junction.
• The vasa recta functions in maintaining
the solute concentration (osmolarity
gradient) of the renal medulla.
Juxtaglomerular Apparatus
• The juxtaglomerular apparatus is formed
by the association of the
– distal convoluted tubule with the arterioles
of the glomerulus.
• The modified cells of the afferent arteriole
are called juxtaglomerular cells
• The modified cells of the distal convoluted
tubule are called the macula densa.
• The juxtaglomerular apparatus produces
the hormone erythropoietin and the
enzyme renin.
Microscopic Observation of
Kidney
Lab Activity 4
6
Lab Activity 4 – Microscopic
Observation of the Kidney
Figure 27.10
Scanning power photograph of a kidney preparation showing a cross (or
horizontal) section.
Lab Activity 4 – Microscopic
Observation of the Kidney
Lab Activity 4 – Microscopic
Observation of the Kidney
Figure 27.11
A scanning power photograph of a section of the kidney.
Lab Activity 4 – Microscopic
Observation of the Kidney
Figure 27.13
High power photograph showing the structure of the renal corpuscle, the
glomerular (Bowman’s) capsule and the glomerulus.
Figure 27.12
Low power view of the cortex (and medulla).
Lab Activity 4 – Microscopic
Observation of the Kidney
Figure 27.14
High power photograph showing the structure of the glomerular
(Bowman’s) capsule, the glomerulus, and the proximal convoluted tubule.
Lab Activity 4 – Microscopic
Observation of the Kidney
Figure 27.15
Low power view of the medulla (and cortex).
7
Lab Activity 4 – Microscopic
Observation of the Kidney
Figure 27.16
A low power view of a medullary pyramid. The vasa recta are capillaries
associated with the loops of Henle (and collecting ducts) of the juxtamedullary
nephrons.
Juxtaglomerular Apparatus
Figure 27.9
The juxtaglomerular apparatus is formed by the association of the
distal convoluted tubule with the arterioles of the glomerulus.
Filtration
Processes of Urine Formation
Three processes are involved in the
production of urine
(1) filtration,
(2) reabsorption, and
(3) secretion.
• Filtration is the process of separation by
passing through a filter.
• A filter separates substances based upon
the size of the filter’s pores (openings).
• The kidney’s filtration membranes function
as filters.
Reabsorption
Secretion
• Reabsorption is the process where substances
are absorbed, again.
• The process of filtration allows some substances
that were absorbed from the digestive tract or
interstitial fluid into the blood, to leave the blood
and to enter the nephron, ultimately to become a
component of urine.
• Reabsorption is the process where instead of
allowing the substances to form urine, the
substances are absorbed back into the blood
(mostly by the peritubular capillaries).
• Secretion is the process where substances are
moved from the cells or blood.
• In the formation of urine, secretion involves the
movement of substances from the blood of the
peritubular capillaries and the tubular cells into
the tubular fluid.
• The tubular fluid is excreted as urine.
• Excretion is the process of disposal of waste,
such as urine (or sweat) from the body’s organs
or blood.
8
Processes of Urine Formation
Filtration at the Glomerulus
Filtration Membrane
Figure 27.17
Filtration of blood occurs at the glomerulus. The nephron functions in
reabsorption and secretion.
Filtration
•
Filtration is the process of separation by
passing through a filter. A filter separates
substances based upon the size of the filter’s
pores (openings).
• The kidney’s filtration membranes function as
filters in the filtration of blood and are formed
from the
– (1) fenestrated endothelium of the glomerular
capillaries, the
– (2) filtration slits formed by the podocytes (visceral
membrane of glomerular capsule), and the
– (3) basement membrane (fused basal laminas of
visceral layer and endothelium) located between the
capillaries and the podocytes (visceral membrane).
Filtration Membrane
Figure 24.18
Filtration occurs at the glomerulus, with the filtrate entering
the glomerular capsular space.
Filtration Membrane
• The filtration membrane restricts
– the passage of the blood’s formed elements
(cells and platelets) and
– most of the plasma proteins.
• Only the smallest of substances such as
water, ions, simple sugars, and amino
acids are allowed to pass into the capsular
space as filtrate.
Filtration Membrane
Figure 24.19
The filtration membrane is formed from the (1) fenestrated endothelium of
the glomerular capillaries, the (2) filtration slits formed by the podocytes (visceral
membrane of glomerular capsule), and the (3) basement membrane (fused basal
laminas of visceral layer and endothelium) located between the capillaries and the
podocytes (visceral membrane).
9
Filtration Membrane
Filtration Pressure
• The driving force for filtration is glomerular
hydrostatic pressure, HPg, (or glomerular
capillary blood pressure).
• Forces opposing glomerular hydrostatic
pressure are
– glomerular (blood) osmotic pressure, OPg, and
– capsular hydrostatic pressure, HPc.
• Net filtration pressure (NFP) is determined by
– subtracting the opposing forces, glomerular (blood)
osmotic pressure plus capsular hydrostatic pressure,
– from glomerular hydrostatic pressure
Figure 24.20
High power photograph that shows the details of the renal corpuscle (and
juxtaglomerular apparatus). The filtration membrane is formed from the
association of the glomerular capillaries, podocytes, and the basement membrane
(not shown in this photograph).
Glomerular hydrostatic pressure
•
• NFP = HPg - (OPg + HPc).
Glomerular osmotic pressure
Glomerular hydrostatic pressure is the
pressure of blood within the glomerular
capillaries, and is about 60 mm Hg.
Glomerular blood pressure is relatively
high because the efferent arteriole is
smaller than the incoming afferent
arteriole.
• Glomerular osmotic pressure is mostly produced
by the blood’s albumins (and other plasma
proteins).
• Water pushed into the glomerular capsule by
blood hydrostatic pressure (HPg) tends to
diffuse back into blood (osmosis) as a result of
its higher concentration of solutes (lower
concentration of water).
• Glomerular osmotic pressure opposes
glomerular hydrostatic pressure and is
measured at about 28 mm Hg.
Capsular hydrostatic pressure
Net Filtration Pressure
• Capsular hydrostatic pressure is the
pressure due to the presence of fluid
(filtrate) in the glomerular capsule.
• Capsular hydrostatic pressure is mostly
produced as a back-pressure due to
resistance of the fluid to flow.
• Capsular hydrostatic pressure opposes
glomerular hydrostatic pressure and is
measured at about 15 mm Hg.
• Net filtration pressure is the net pressure
at the filtration membrane and is
– determined by subtracting the forces
opposing filtration (OPg + HPc) from the force
promoting filtration, HPg.
• Applying approximate numerical values,
NFP = 60 mm Hg - (28 mm Hg. + 15 mm
Hg), or NFP = 17 mm Hg.
10
Filtration Pressure
Glomerular Filtration
Maintenance of Glomerular
Filtration
Figure 24.21
Net filtration pressure is determined by subtracting the forces opposing
filtration (OPg + HPc) from the force promoting filtration, or applying approximate
numerical values, NFP = 60 mm Hg - (28 mm Hg. + 15 mm Hg), or NFP = 17 mm
Hg.
Glomerular Filtration
• The amount of filtrate produced by the kidneys
per minute is called the glomerular filtration rate
(GFR).
• Considering the filtration membrane, the most
significant variable in the regulation of the
filtration rate is glomerular (blood) hydrostatic
pressure.
– Other factors that can change glomerular filtration
rates, such as changes in the permeability of the
filtration membrane, changes in filtration membrane
surface area, and changes in the blood osmotic and
capsular pressures may result from illness or disease.
Maintenance of Glomerular
Filtration
• Maintenance of a normal glomerular
filtration rate results from the adjustment of
glomerular blood pressure by directly
influencing either the
– (1) afferent and efferent arterioles or
– (2) systemic blood pressure.
Myogenic mechanism
Tubuloglomerular mechanism
Myogenic means that the mechanism
originates from the muscles, which in this case is
the vascular smooth muscle of the afferent
arteriole.
• The myogenic mechanism functions to maintain
glomerular hydrostatic pressure because the
smooth muscle of the afferent arteriole
contracts in response to stretch.
• Tubuloglomerular means the mechanism
originates from the interaction of the nephron
(tube) and the glomerulus.
• Specifically, this interaction occurs at the
juxtaglomerular apparatus, the association of
the distal convoluted tubule with the arterioles of
the glomerulus. The mechanism operates
through the macula densa cells, a dense group
of cells in the distal convoluted tubule of the
juxtaglomerular apparatus.
•
– Increased blood pressure causes the contraction of
the smooth muscle of the afferent arteriole, thus,
reducing blood flow and pressure at the glomerular
capillaries. If systemic blood pressure decreases, the
smooth muscle of the afferent arteriole dilates,
resulting in increased blood flow and pressure.
11
Tubuloglomerular mechanism
Tubuloglomerular mechanism
• The macula densa cells respond to increased
osmolarity (mostly due to increased sodium
ions) by releasing a chemical mediator that
targets the afferent arteriole and produces
vasoconstriction.
– High osmolarity indicates that blood pressure is too
high and tubular flow is too fast to allow adequate
adjustment (decrease) of tubular fluid osmolarity.
Vasoconstriction of the afferent arteriole decreases
pressure, thus, flow and allows for increased
reabsorption time.
Renin-Angiotensin Mechanism
• Renin is an enzyme released into the blood by
the juxtaglomerular cells of the afferent arteriole,
especially when the juxtaglomerular cells are
subjected to reduced stretch, resulting from low
systemic blood pressure.
• Renin functions to convert the inactive plasma
enzyme angiotensinogen into angiotensin I.
Angiotensin I is converted to angiotensin II by
enzymes (mostly by enzymes in the endothelium
of the lungs called angiotensin converting
enzymes, or ACE).
Renin-Angiotensin Mechanism
Figure 24.22
Increased osmolarity of the fluid in the distal convoluted tubule results in
the macula densa cells releasing a chemical mediator that causes vasoconstriction
of the afferent arteriole.
Renin-Angiotensin Mechanism
• Angiotensin II is a powerful vasoconstrictor and
promotes an increase in systemic blood
pressure.
• Angiotensin II also targets the cortex of the
adrenal glands and results in the release of
aldosterone.
– Aldosterone, the primary mineralocorticoid of the
adrenal cortex, mostly targets the distal convoluted
tubules and promotes the reabsorption of sodium
ions from the tubular fluid. As sodium ions move
back into the blood water osmotically follows, thus
increasing blood volume. Increase blood volume
results in increased systemic blood pressure.
Sympathetic Nervous System
• Decreased systemic blood pressure results in stimulation
of the vascular center resulting in systemic arteriole
vasoconstriction and stimulation of the juxtaglomerular
cells to release the enzyme renin.
• Vasoconstriction of systemic arterioles results in
increased systemic blood pressure. Renin ultimately
results in production of angiotensin II, which also
promotes systemic arteriole vasoconstriction, and it
promotes the release of aldosterone from the adrenal
cortex. Aldosterone promotes increased sodium ion
reabsorption and the osmotic reabsorption of water.
Increased blood water volume results in increased
systemic blood pressure.
Figure 24.23
Decreased systemic blood pressure results in the release of renin from
the juxtaglomerular cells.
12
Reabsorption
Reabsorption
Reabsorption is the process
where substances are absorbed,
again.
Reabsorption at Proximal
Convoluted Tubule
• The process of filtration allows some substances
that were absorbed from the digestive tract or
interstitial fluid into the blood, to leave the blood
and to enter the nephron, ultimately to become a
component of urine.
• Reabsorption is the process where instead of
allowing the substances to form urine, the
substances are absorbed back into the blood
(mostly of the peritubular capillaries).
Reabsorption at Proximal
Convoluted Tubule
– All of the organic molecules such as glucose
and amino acids, many ions, and water are
reabsorbed into the peritubular capillaries.
Reabsorption involves both passive and
active processes.
• About 65% of the sodium ions are reabsorbed in
the proximal convoluted tubule.
• As sodium moves back into the blood water
osmotically follows (along its concentration
gradient).
• The osmotic movement of water along its
concentration gradient established by the
movement of solutes (sodium ions) is called
obligatory water reabsorption.
Reabsorption at Proximal
Convoluted Tubule
Reabsorption at the Loop of Henle
• Most of the tubular reabsorption occurs in
the proximal convoluted tubules.
• The loop of Henle is the loop portion of the nephron
located between the proximal and distal convoluted
tubules. The loop of Henle consists first of a descending
limb, which is followed by the ascending limb.
• The descending limb is permeable to water, which is
reabsorbed either in the peritubular capillaries of the
cortical nephron or by the vasa recta of the
juxtamedullary nephron.
• The ascending limb is permeable to sodium and
chloride ions, or NaCl.
Figure 24.24
Most tubular reabsorption occurs in the proximal convoluted tubule.
All organic molecules are reabsorbed along with most of the tubular water and
ions.
– Sodium and chloride ions are reabsorbed into the peritubular
capillaries of the cortical nephron and the vasa recta of the
juxtamedullary nephron.
13
Reabsorption at the Loop of Henle
Reabsorption at the Distal Convoluted
Tubule and Collecting Duct
• The distal convoluted follows the
ascending limb of the loop of Henle.
– Reabsorption is mostly under hormonal
control.
• Three major substances that are
reabsorbed are
Figure 24.25
The loop of Henle consists of the descending limb followed by the
ascending limb. The descending limb is permeable to water, and the ascending
limb is permeable to sodium and chloride ions. In the juxtamedullary nephrons,
water and salt are reabsorbed by the vasa recta.
Water Reabsorption and Antidiuretic
Hormone (ADH)
• Water reabsorption is mostly regulated by
antidiuretic hormone, or ADH.
• ADH is released from the posterior
pituitary gland in response to high blood
osmolarity (or low water volume).
• ADH targets the distal convoluted tubule
and the collecting duct and increases
water reabsorption, thus blood volume
and blood pressure are increased.
Sodium Reabsorption and ReninAngiotensin Mechanism
• Aldosterone targets the distal convoluted
tubule and the collecting duct and results
in increased sodium reabsorption.
• As sodium is reabsorbed, water
osmotically follows, thus, increasing
blood volume and pressure.
– water,
– sodium ions, and
– calcium ions.
Sodium Reabsorption and ReninAngiotensin Mechanism
• Sodium reabsorption is mostly regulated by the
hormone aldosterone and functions through the
renin-angiotensin mechanism. A
• Aldosterone is the primary mineralocorticoid
produced by the adrenal cortex. Increased
aldosterone secretion is triggered by the release
of the enzyme renin by the juxtaglomerular cells
of the afferent arteriole in response to low blood
pressure (reduced stretch of the juxtaglomerular
cells).
Calcium Ion Reabsorption and
Parathyroid Hormone (PTH)
• Calcium ion reabsorption is influenced by
parathyroid hormone, or PTH.
• Parathyroid hormone is produced by the
parathyroid glands in response to low
levels of blood ionic calcium.
• PTH increases calcium ion
reabsorption in the distal convoluted
tubule.
14
Reabsorption at the Distal Convoluted
Tubule and Collecting Duct
SECRETION
Secretion is the process where
substances are moved from the
cells or blood.
Figure 24.26
Reabsorption at the distal convoluted tubule and the collecting duct.
Three major substances that are reabsorbed are water, sodium ions, and
calcium ions.
Secretion
• In the formation of urine, secretion
involves the movement of substances
from the blood of the peritubular
capillaries and the tubular cells into the
fluid of tubules of the nephron and the
collecting duct.
Secretion
Secretion
• Common substances that are secreted
include
– hydrogen ions (H+),
– bicarbonate ions (HCO3-, and
– ammonium ions (NH4-).
– Most secretion occurs in the proximal
convoluted tubule, with the distal convoluted
tubule and collecting duct having a secondary
role.
Secretion
• Secretion mostly functions in the regulation of
the body’s pH and the removal of excess
potassium.
• With increasing acidosis, hydrogen ions are
increasingly secreted into the tubular fluid.
• With increasing alkalosis, bicarbonate ions
(HCO3-) are increasingly secreted into the
tubular fluid.
• Potassium secretion occurs mostly in the
collecting duct and is under the influence of
aldosterone; as sodium ions are reabsorbed,
potassium ions are secreted.
Figure 24.27
Secretion functions in the balance of the body’s pH and the removal of
excessive or unnecessary substances.
15
Production of the Medullary
Osmotic Gradient
Production of the Medullary
Osmotic Gradient
An osmotic gradient is established in
the kidney’s medulla (renal pyramids)
for the regulation of the osmotic
movement of water
Starting with the ascending limb
•
Sodium ions are pumped out of the
tubular fluid (Cl- follows) into the
interstitial fluid.
– This reduces the solute (salt)
concentration of the tubular fluid in the
ascending limb.
– However, the solute concentration around
the descending limb is increased.
• The process that establishes the osmotic gradient is
called the countercurrent mechanism because of the
opposing directions of tubular fluid flow in the
descending and the ascending loops of Henle.
• The osmotic gradient ranges from about 300 mOsm in
the proximal convoluted tubule (cortex) to about 1200
mOsm in the bend of the loop of Henle (medulla). The
gradient is established because
– (1) sodium ions are actively transported out of the water
impermeable ascending limb,
– (2) the descending limb is only permeable to water, and
– (3) glomerular filtration continually keeps fluid entering the
nephron.
Descending limb
• Now, water osmotically leaves the
descending limb increasing the solute
(salt) concentration in the tubular fluid.
• The tubular fluid high is solute (salt) is
pushed by incoming filtrate from the
glomerulus into the ascending limb.
Ascending limb
Countercurrent Multiplication
Mechanism
• Sodium is additionally pumped out of
the tubular fluid into the interstitial fluid
making the interstitial fluid solute (salt)
more concentrated.
• The fluid in the ascending limb becomes
less concentrated in solute (salt).
• The countercurrent mechanism is further
described as the countercurrent
multiplication mechanism because the
solute concentration in the tubular fluid
of the descending limb increases as
filtrate moves through the lumen of the
tubule.
16
Vasa Recta
Figure 24.28
Solute (salt) is actively transported out of the ascending limb, which increases the
osmolarity of the interstitial fluid. Then, water osmotically moves from the
descending limb, resulting in an increase in solute (salt) concentration of the
descending limb’s tubular fluid. This more solute concentrated tubular fluid moves
into the ascending limb and is again used as a source for the transport of solute
(salt) into the interstitial fluid, resulting in an increase (multiplication) of interstitial
fluid solute (salt) concentration.
• Specialized capillaries, the vasa recta, are
associated with the loop of Henle. The vasa
recta is permeable to both salt and water and
thus, is maintained at an equal salt and water
concentration with the interstitial fluid.
• Because the vasa recta exchanges both salt and
water to maintain the osmolarity of the interstitial
fluid it is called the countercurrent exchanger.
Final Regulation of urine Water
Volume
Figure 24.29
The vasa recta are specialized capillaries associated with the loop of Henle
of juxtamedullary nephrons. The vasa recta allows the maintenance of the highly
concentrated medullary interstitial fluid by being permeable to both water and salt.
•
Final Regulation of Urine Water
Volume
Water Elimination by Forming
Dilute Urine
By the time tubular filtrate reaches the
distal convoluted tubule two essential
events have occurred,
• When the body does not need to conserve
water, excessive water is removed by the
production of increased amounts of dilute urine.
• Dilute urine is produced by allowing the
continued passage of the hypotonic (low solute
concentration) tubular fluid into the minor
calyces.
• As the tubular fluid passes into and through the
collecting system little reabsorption of water
occurs.
– (1) the medullary interstitial fluid has a
high osmotic gradient (ranging from 400
mOsm to 1200 mOsm) and
– (2) tubular fluid that enters the distal
convoluted tubule has a low osmotic
gradient (about 100 mOsm).
– Additionally, selective solutes may be actively
reabsorbed, contributing to a further lowering the
solute concentration of the tubular fluid (producing a
more dilute urine).
17
Water Elimination by Forming
Dilute Urine
Water Conservation by Forming
Concentrated Urine
• When the body needs to conserve water
(osmoreceptors in the hypothalamus detect
increased osmolarity of blood), antidiuretic
hormone (ADH) is released by the posterior
pituitary gland.
– ADH is a powerful vasoconstrictor and increases
systemic blood pressure by causing vasoconstriction
of arterioles.
– ADH also targets the distal convoluted tubule and
the collecting duct causing both to increase
permeability to water. Water diffuses from the
tubules (hypotonic) into the interstitial fluid
(hypertonic) where it is reabsorbed by blood
capillaries.
Figure 24.30
Mechanism for the production of dilute urine.
Water Conservation by Forming
Concentrated Urine
• Thus, conservation of water increases blood
volume and blood pressure.
Water Conservation by Forming
Concentrated Urine
• Depending upon the needs of the body, various
concentrations of tubular fluid are produced
depending upon the amount of ADH present,
which is dependent upon the release of ADH at
the posterior pituitary.
• The reabsorption of water is called facultative
reabsorption as the amount of water
reabsorption is contingent upon the amount of
ADH present.
Figure 24.31
Mechanism for the production of concentrated urine.
Ureters
URETERS
• Like the kidneys and the urinary bladder the
ureters are retroperitoneal.
• Histologically, the walls of the ureter consist of
three layers,
– (1) an inner mucosa.
• The epithelium of the mucosa is transitional epithelium
The ureters are the tubes that
transport urine from the kidneys to
the urinary bladder.
– (2) a middle muscularis.
• The muscularis consists of two layers of smooth muscle, an
inner longitudinal layer and an outer circular layer. The
stretch of the muscularis by urine functions as the primary
control for initiation and production of peristaltic waves that
move urine toward and into the urinary bladder.
– (3) an outer adventitia.
18
The Urinary Bladder
• Histologically, the wall of the urinary bladder consists of
four layers,
– (1) an inner mucosa.
• The epithelium of the mucosa is transitional epithelium
The Urinary Bladder
– (2) a submucosa.
– (3) a middle muscularis.
• The muscularis consists of three layers of smooth muscle and is
called the detrusor muscle.
– (4) an outer adventitia..
The urinary bladder functions as a
temporary storage site for urine.
• Internally, an area called the trigone is identified as the
triangular region marked by three sites, the entrance of
each ureter and the origin of the urethra.
• A muscular sphincter, the internal urethral sphincter,
provides for involuntary flow of urine into the urethra.
URETHRA
Figure 24.32
Low power photograph of the urinary bladder (fetal, human). The wall of
the urinary bladder is divided into four primary regions, the mucosa, submucosa,
muscularis externa, and serosa. Bundles of smooth muscle form the detrusor
muscle, the muscle that controls the emptying of the urinary bladder.
Urethra
• The urethra is the tube that serves as the
pathway for the exit of urine from the urinary
bladder.
– In the male, the urethra also serves as the
passageway for semen.
• Two sphincters are associated with the flow of
urine, the internal urethral sphincter and the
external urethral sphincter.
– The internal urethral sphincter is a continuation and
modification of the detrusor muscle and is located at
the origin of the urethra. The internal urethral
sphincter is under involuntary control.
– The external urethral sphincter surrounds the
urethra as it passes through the floor of the pelvic
cavity at the urogenital diaphragm. The external
urethral sphincter is under voluntary control.
The urethra is the tube that serves
as the pathway for the exit of urine
from the urinary bladder.
Urethra
• Compared with the urethra of the male
(about 8 inches long), the urethra of the
female is short (about 1.5 inches long).
• The urethra of the male is divided into
three regions, the
– (1) prostatic urethra, the
– (2) membranous urethra, and the
– (3) spongy, or penile, urethra.
19
Micturition
MICTURITION
Micturition is the term that
describes the discharge of urine.
Micturition
• Micturition is the term that describes the
discharge of urine. Two other commonly
used terms for the discharge of urine are
urination and voiding. Micturition is
controlled through a two stage cycle called
the micturition reflex. The micturition reflex
is divided into the filling (storage) phase
and the emptying phase.
Emptying Phase
• During the emptying phase, the micturition
center in the pons is activated. Stretch
receptors in the wall of the urinary bladder send
sensory information (by visceral afferent fibers of
pelvic nerves) into the sacral region of the spinal
cord.
• The sensory information is conveyed to the
micturition center of the pons which
establishes parasympathetic control of
micturition.
– Parasympathetic outflow results in relaxation of the
internal urethral sphincter and contraction of the
bladder’s detrusor muscle (sympathetic
stimulation is inhibited).
– The somatic motor fibers are inhibited resulting in
relaxation of the external urethral sphincter.
• Two other commonly used terms for the
discharge of urine are urination and
voiding.
• Micturition is controlled through a two
stage cycle called the micturition reflex.
The micturition reflex is divided into the
– filling (storage) phase and the
– emptying phase.
Filling Stage
• During the filling (storage) phase, stretch
receptors in the wall of the urinary bladder send
sensory information (by visceral afferent fibers of
pelvic nerves) into the sacral region of the spinal
cord.
– A reflex circuit is activated to somatic motor
fibers that results in contraction of the external
urethral sphincter.
– A circuit is also activated with sympathetic fibers
resulting in contraction of the internal urethral
sphincter and inhibition of the bladder’s detrusor
muscle.
• Afferent (sensory) information is directed to the
cerebral cortex producing conscious awareness
of the need for micturition when the bladder fills
to about 200 ml.
Emptying Phase
• Voluntarily withholding micturition interrupts the
emptying phase by the relaxation of the
bladder’s detrusor muscle.
• The bladder is allowed to continue the filling
(storage) phase until about another 200 ml. of
urine is stored. After which, cortical awareness
becomes more intense for allowing the initiation
of the emptying phase.
• The reflex arc cycle can continue until the
bladder reaches maximal filling and the internal
urethral sphincter is forced open, followed by the
reflexive opening of the external urethral
sphincter which allows involuntary micturition.
20