Unit 20 Urinary
advertisement

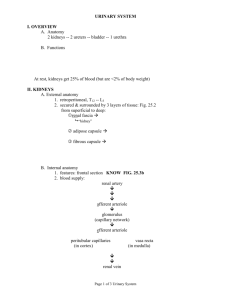
Unit 20 - Urinary System UNIT OBJECTIVES 1. Define the terms urology, retroperitoneal, hilum, renal cortex, renal medulla, renal pyramid, and urinalysis. 2. Identify the primary functions of the urinary system. 3. Locate and identify at least one function for each of the following structures: kidney, nephron, collecting ducts, renal sinus, renal calyx, renal pelvis, ureters, urinary bladder, detrusor muscle, urethra, tubular network, glomerular capsule, renal corpuscle, proximal convoluted tubule, Henle’s loop, descending limb of Henle, ascending limb of Henle, distal convoluted tubule, vascular network, renal artery, segmental artery, interlobar artery, arcuate artery, cortical artery, afferent arteriole, glomerulus, efferent arteriole, peritubular capillaries, vasa recta, cortical vein, arcuate vein, interlobar vein, segmental vein, and renal vein. carrier molecules, glucose, sodium ions, water, chloride ions, urea, aldosterone, and ADH. 13. Discuss and explain tubular secretion by relating it to the control of blood pH, be sure to include: distal convoluted tubule, peritubular capillaries, carbon dioxide, water, carbonic anhydrase, carbonic acid, bicarbonate ions, hydrogen ions, sodium ions, chloride ions, ammonia, and ammonium ions. 14. Discuss and explain the countercurrent multiplier mechanism, be sure to include: descending limb of Henle, ascending limb of Henle, vasa recta, collecting duct, renal cortex, renal medulla, sodium ions, chloride ions, water, ADH, and the glomerular filtrate. 15. Identify the effects of the following on urinary output and urine concentration: the blood’s sodium concentration, aldosterone, the blood’s water level, ADH, blood pressure, and diuretics. 4. Identify three factors that assist the movement of urine through a ureter. 16. Name the main urinary pigment and identify its origin. 5. Define the term micturition and describe how this process is controlled by the micturition reflex and the urethra’s sphincters. 17. Differentiate between the following and identify a cause for each: bilirubinuria, glycosuria, albuminuria, hematuria, pyuria, ketosis, kidney stones, and anuria. 6. List the three main activities necessary for urine formation and define each. 7. Explain glomerular filtration using the following terms: glomerular hydrostatic pressure, capsular hydrostatic pressure, glomerular osmotic pressure, capsular osmotic pressure, effective filtration pressure. 8. Define the term glomerular filtration rate and explain how the autonomic nervous system and the juxtaglomerular apparatus control it. 9. Compare the chemical composition of plasma with that of urine and the glomerular filtrate. 10. Identify the purposes of tubular reabsorption, tubular secretion and the countercurrent multiplier mechanism. 11. Define the following terms: active reabsorption, passive reabsorption, obligatory reabsorption, and facultative reabsorption. 12. Discuss and explain tubular reabsorption, be sure to include: proximal convoluted tubule, distal convoluted tubule, collecting duct, peritubular capillaries, 18. State how the following systems are involved in excretion: integumentary system, digestive system, and respiratory system. NOTES I. Introduction to the System A. Urology is the study of the urinary system. This system maintains the blood’s volume and composition by removing the unwanted materials (i.e., ammonia, urea, etc.) produced by metabolism. It does this by producing a fluid called urine. B. The urinary system also regulates the blood’s pH, produces erythropoietin to regulate erythropoiesis, and produces renin to control blood pressure. II. Organs of the Urinary System A. The kidneys are a pair of organs that are embedded in the posterior aspect of the abdominal wall. This retroperitoneal position covers the kidneys with parietal peritoneum. The parietal peritoneum protects the kidneys and holds them in place. 210 Unit 20 - Urinary System 1. A kidney’s external depression is called its hilum. This is the site of nerve and vessel penetration. Behind the hilum is a cavity called the renal sinus. 2. Internally, a kidney is organized into two regions: an outer renal cortex and an inner renal medulla. a. These layers both contain parts of a nephron. This functional unit is responsible for urine formation. b. A kidney’s nephrons are clustered into about 12 wedge-like structures called renal pyramids. Each of the pyramid’s nephrons convey their urine into collecting ducts. These tubes conduct the urine through the renal medulla to the kidney’s hilum. c. The kidney’s renal sinus is lined by a large sac called the renal pelvis. This sac’s margin possesses several small extensions called the renal calyces. Each renal calyx collects urine from the collecting ducts of one or two renal pyramids. The renal pelvis empties its urine into the system’s ureters. 3. The bladder’s apex points downward. This region contains the urinary bladder’s sphincters. These circular pieces of muscle control the flow of urine into the urethra. a. The internal sphincter is a piece of smooth muscle that is involuntarily controlled by the urinary bladder’s stretch receptors. These receptors automatically dilate this sphincter, when the urinary bladder is full. This response is called the micturition reflex. b. The external sphincter is a piece of skeletal muscle that is voluntarily controlled by the cerebrum. Usually, this control does not develop until two years of age. The reason, it takes about two years to innervate the external sphincter. D. The urethra is a tube that connects the urinary bladder to the body’s outside. Because of its position, the urethra removes urine from the body. In men, this tube also transports semen. III. The Nephron: Tubular and Vascular Components B. The ureters are a pair of tubes that convey urine to the urinary bladder. These tubes are composed of mucous membranes and smooth muscle. 1. The ureter’s mucous membrane lines its lumen. This layer protects the ureter from the highly acidic urine. 2. The ureter’s smooth muscle performs peristalsis. This rhythmic contraction propels urine to the urinary bladder. Urine is also propelled by gravity and hydrostatic pressure. C. The urinary bladder is a sac-like organ that lies near the base of the pelvic cavity. When full, this sac resembles an inverted pear. 1. The urinary bladder temporarily stores urine. Therefore, it solves the problem of constant urination. 2. The wall of the urinary bladder contains smooth muscle and stretch receptors. a. The bladder’s smooth muscle is called the detrusor muscle. This muscle’s contraction causes the bladder to empty. This process is called urination or micturition. b. The bladder’s stretch receptors trigger the micturition reflex. This is accomplished by controlling the bladder’s detrusor muscle and its sphincters. A. A nephron’s tubular network is responsible for the collection and production of urine. Therefore, it regulates the blood’s composition and volume. 1. The opening to the tubular network is called the glomerular capsule or Bowman’s capsule. This cup-like structure is located within the kidney’s renal cortex and it surrounds a capillary bed called the glomerulus. a. The glomerular capsule and its glomerulus are collectively called a renal corpuscle. b. The renal corpuscle functions in producing a glomerular filtrate by way of filtration. This happens as plasma filters through the pores of the corpuscle’s walls. 2. The glomerular capsule moves its glomerular filtrate into a highly coiled tube called the proximal convoluted tubule. This tube functions in reabsorption and secretion. These processes help to convert the glomerular filtrate into urine. 3. The proximal convoluted tubule conveys the filtrate to Henle’s loop. This series of tubes (i.e., descending limb, loop, and ascending limb) enters the renal medulla. Here, they continue to refine the filtrate by using the countercurrent multiplier mechanism. 211 Unit 20 - Urinary System 4. The ascending limb of Henle returns the filtrate to the renal cortex. Here, it merges with the distal convoluted tubule. The distal convoluted tubule uses reabsorption and secretion to modify the glomerular filtrate as it moves to the collecting duct. 5. The collecting duct connects the distal convoluted tubule to a renal calyx. Besides conveying the glomerular filtrate, the collecting duct uses reabsorption to finish the refining process. When it leaves this tube, the glomerular filtrate has been transformed into urine. B. A nephron’s vascular network is responsible for the delivery and removal of blood. This network also assists the tubular network with the formation of urine. 1. Blood is conveyed to the kidneys by the renal arteries. Once inside the kidney, the renal arteries branch. These branches are called the segmental arteries. The segmental arteries deliver blood to the interlobar arteries. 2. The interlobar arteries follow the renal columns to deliver blood to the arcuate arteries. 3. The arcuate arteries arc over the renal pyramids and branch into many cortical arteries. 4. Each cortical artery travels into the renal cortex. Here, the blood vessel delivers blood to a nephron by attaching to its afferent arteriole. 6. The afferent arteriole delivers its blood to the nephron’s glomerulus. 7. The glomerulus generates a glomerular filtrate from its blood. After this filtration occurs, the blood exits the glomerulus through an efferent arteriole. 8. The efferent arteriole delivers blood to the nephron’s peritubular capillaries and vasa recta. These capillary beds assist the nephron’s tubular network in refining the glomerular filtrate. a. The peritubular capillaries surround the nephron’s proximal and distal convoluted tubules. These capillaries help to refine the urinary filtrate into urine by assisting in reabsorption and secretion. b. The vasa recta surround Henle’s loop. These capillaries assist with the countercurrent multiplier mechanism. 9. The peritubular capillaries and vasa recta deliver blood to the kidneys cortical veins. These veins merge to form the arcuate veins. 10. The arcuate veins arc over the renal pyramids to deliver blood to the interlobar veins. 11. The interlobar veins travel down the renal columns to deliver blood to the kidney’s renal vein. 12. The renal vein removes the blood from the kidney by delivering it to the inferior vena cava. IV. Nephrons perform three activities to produce urine. These activities are: glomerular filtration, tubular reabsorption, and tubular secretion. Let’s examine these activities in more detail. A. Glomerular filtration is a process that produces a glomerular filtrate from the body’s blood. This happens as the filtrate passes through the wall of the renal corpuscle. 1. Glomerular filtration separates the blood’s larger particles from its smaller particles. Because of this action, the glomerular filtrate does not contain blood cells or many of the plasma’s proteins. Instead, it contains water, glucose, sodium, and urea, among others. 2. Like capillary filtration, glomerular filtration is controlled by pressure gradients. These gradients involve: glomerular hydrostatic pressure, capsular hydrostatic pressure, glomerular osmotic pressure, and capsular osmotic pressure. a. Glomerular hydrostatic pressure (GHP) is the fluid (blood) pressure within the glomerulus. This pushing pressure (about 60mm of mercury) forces fluid into the glomerular capsule. b. Capsular hydrostatic pressure (CHP) is the fluid (filtrate) pressure within the glomerular capsule. This pushing pressure (about 15mm of mercury) forces fluid into the glomerulus. c. Glomerular osmotic pressure (GOP) is determined by the concentration of proteins in the glomerulus. These proteins pull fluid into the glomerulus. Since the glomerular blood contains many proteins, its osmotic pressure is about 27mm of mercury. d. Capsular osmotic pressure (COP) pulls fluid into the glomerular filtrate. However, this force is essentially zero because the filtrate contains little or no protein. 3. Using these figures, we can calculate the nephron’s effective filtration pressure (EFP). 212 Unit 20 - Urinary System EFP = (GHP + COP)–(CHP + GOP) or EFP = (60 + 0)–(15 + 27) or EFP = 18 4. An effective filtration pressure of 18mm of mercury causes about 10% of the plasma that enters the glomerulus to enter the capsule. This amount is equivalent to 48 gallons of filtrate generated by the kidneys per day. This amount is called the glomerular filtration rate (GFR). 5. The kidney’s GFR is directly proportional to the GHP. Therefore, an increase in the GHP causes an increase in the GFR and vice versa. If the GHP falls below 42mm of mercury, glomerular filtration stops. This problem is called anuria or renal failure. 6. Since the GHP is so important, its regulation is independent of the cardiovascular system’s pressure. This enables the GFR to remain constant with drastic changes in the systemic blood pressure. The regulation of the nephron’s GHP is controlled by: an autoregulation mechanism, hormonal secretion, or by the autonomic nervous system. a. The autoregulation mechanism of the GHP is controlled by the nephron’s juxtaglomerular apparatus. The apparatus is located within the walls of the afferent and efferent arterioles and it is designed to control their diameter. Therefore, the mechanism is autoregulatory because the vessels control their own diameter. 1. Under normal circumstances, the afferent arteriole is larger in diameter than the efferent arteriole. This design causes pressure to build within the glomerulus because more blood enters the capillary bed than leaves it. As a result, the glomerulus can maintain a higher pressure than the average capillary. However, this can be adjusted by the juxtaglomerular apparatus. 2. The juxtaglomerular apparatus monitors the flow of blood into the glomerulus and its pressure. If the systemic pressure is low, the arterioles respond by dilating the afferent arteriole and constricting the efferent arteriole. This elevates the GHP which maintains the GFR. If the systemic pressure is high, the opposite occurs to maintain the GFR. b. If the autoregulation mechanism cannot compensate for changes in the systemic pressure, the apparatus secretes hormones to help solve the problem. 1. Renin is secreted by the apparatus to invoke the renin-angiotensin pathway. This culminates in the production of angiotensin II by the lungs. Remember, angiotensin II has two functions. One, it stimulates the secretion of aldosterone (hopefully to increase blood volume by retaining sodium ions). Two, it is a potent vasoconstrictor (hopefully to decrease the size of the system). Hopefully, these actions raise blood pressure to prevent renal failure. 2. Erythropoietin is released by the apparatus to increase blood volume. Remember, erythropoietin stimulates red blood cell production. The higher number of circulating red blood cells thicken the blood. This concentration attracts water to it. c. The arterioles’ vasomotor responses are also controlled by the autonomic nervous system. The ANS uses a sympathetic nerve to control constriction in the nephron’s afferent arteriole. This nerve fiber uses epinephrine to stimulate vasoconstriction. Therefore, the greater the stimulation by the ANS, the slower the GFR. 7. Because the glomerular filtrate consists of both good and bad materials, it must be refined before it can be eliminated as urine. Therefore, the tubular network performs reabsorption and filtration before urine is removed from the body. B. Tubular reabsorption removes materials from the glomerular filtrate and places them within the nephron’s vascular network. Although this process predominately occurs in the proximal convoluted tubule, reabsorption happens throughout the tubular network. Because reabsorption removes most of the glomerular filtrate’s contents, only 1 to 2 liters of urine are produced each day. 1. The tubular network can reabsorb a variety of materials: water, glucose, amino acids, sodium, chloride, urea, etc. These materials may be reabsorbed actively or passively. a. Active reabsorption is a process requiring energy. The body uses this process to remove valuable solutes from the glomerular filtrate (i.e., glucose and sodium). b. Passive reabsorption is a process that does not require energy. This reabsorption is driven by concentration gradients (i.e., water) or ionic attraction (i.e., chloride ions). 213 Unit 20 - Urinary System 2. Reabsorption may also be obligatory or facultative. a. Obligatory reabsorption happens because the body does not have a choice (i.e., some tubules must reabsorb water because of the concentration gradient). b. In facultative reabsorption, the body selects the materials to reabsorb. The body uses hormones to indicate its choices and the tubules carry out the directives (i.e., the distal convoluted tubule facultatively reabsorbs sodium, when stimulated by aldosterone). 3. The proximal convoluted tubule is responsible for most of the nephron’s tubular reabsorption. This reabsorption occurs from the from the tubule into the peritubular capillary. a. The proximal convoluted tubule actively reabsorbs glucose. This active transport mechanism is obligatory (running continually) and is limited by the number of glucose permeases present. Glucose is rarely found in the urine, because the number of sugar permeases is usually sufficient to remove all the glucose that is found in the filtrate. However, glucose will be found in the urine, if the filtrate’s level of glucose exceeds the tubule’s number of sugar permeases. This is called glycosuria and it usually happens as a manifestation of diabetes mellitus. b. Like glucose, sodium is actively reabsorbed by the proximal convoluted tubule. Like glucose, this mechanism is obligatory and restricted by the number of sodium permeases present. c. The sodium ions are not exchanged for another cation. Therefore, an electrolytic imbalance occurs between the filtrate and the surrounding tissue. The tissue becomes more positive as the sodium ions accumulate. Therefore, the filtrate’s chloride ions passively follow because of their attraction to sodium. d. The accumulation of solutes outside the proximal convoluted tubule establishes a concentration gradient. Therefore, water passively moves from the filtrate into the tissues because the tissues are more concentrated than the filtrate. This movement is obligatory and it reabsorbs 80% of the water from the filtrate. 4. The distal convoluted tubule is responsible for most of the nephron’s facultative reabsorption. This reabsorption is under the control of aldosterone and it provides additional support, should the proximal convoluted tubule fail to supply the body’s needs. a. Aldosterone stimulates the distal convoluted tubule to actively reabsorb sodium ions by exchanging them for potassium ions. This exchange is not equal because sodium is more permeable to the duct than potassium. Therefore, more sodium is reabsorbed from the tubule than potassium is secreted into it. The result, a little water is passively reabsorbed as it follows the sodium back into the peritubular capillary. b. Note, the body monitors the level of potassium ions in the blood to control this mechanism. Remember, hyperkalemia causes an irregular heartbeat. This mechanism will help to solve that problem. It also helps to compensate for sodium ions lost through sweating. 5. The collecting duct uses an active mechanism to facultatively reabsorb water from the filtrate. This mechanism occurs when a person is dehydrated and it is initiated by the secretion of ADH. Antidiuretic hormone uses energy to open pores within the walls of the collecting duct. This allows water to move out of the collecting duct into the more concentrated renal medulla by osmosis. This concentration gradient is established by the countercurrent multiplier mechanism. In summary, ADH causes an increase in the concentration of urine as it decreases the urine’s volume. C. Tubular secretion or tubular excretion removes materials from the nephron’s vascular network and places them within the glomerular filtrate. This process predominately occurs along the proximal convoluted tubule and the collecting duct. 1. The nephron’s peritubular capillaries can secrete: drugs, ammonia, sodium ions, hydrogen ions, potassium ions, creatinine, etc. Like reabsorption, tubular secretion can be active, passive, obligatory, or facultative. 2. Tubular secretion plays an integral role in regulating the blood’s pH. The proximal convoluted tubule accomplishes this task by secreting hydrogen ions or bicarbonate ions to solve acidotic and alkalotic problems. Cells of the proximal convoluted tubule have this ability because they contain carbonic anhydrase. a. During acidosis (respiratory or metabolic), the cells in this area increase their metabolic rate. This creates carbon dioxide which carbonic anhydrase combines with water to form carbonic acid. As the acid ionizes, it produces hydrogen and bicarbonate ions. 1. The hydrogen ions created within the cells are exchanged for sodium ions within the filtrate. Once inside the tubule’s cells, these sodium ions are exchanged for hydrogen ions within the blood. Once 214 Unit 20 - Urinary System inside the tubule’s cells, the hydrogen ions are exchanged for more sodium ions from the filtrate. The result, sodium ions are reabsorbed by the blood while its hydrogen ions are secreted. 2. The bicarbonate ions created within the cells are exchanged for chloride ions within the blood. Once inside the cells, these chloride ions are exchanged for bicarbonate ions from the filtrate. Once inside the tubule’s cells, these bicarbonate ions are exchanged for more chloride ions from the blood. The result, bicarbonate ions are reabsorbed by the blood while its chloride ions are secreted. 3. The proximal convoluted tubule may also respond to acidosis by creating ammonium ions (NH4). This occurs when the acidosis has been happening for a while and the filtrate is becoming too acidic. The proximal convoluted tubule has this ability because it can deaminate amino acids. Remember, deamination creates ammonia. Ammonia is a strong base that will accept the hydrogen ions entering from the blood or those being created from carbonic acid. The creation of ammonium ions neutralizes the acid because the hydrogen ions are no longer free. The result, the ammonium ions can be safely traded for more sodium ions from the filtrate without changing its pH. 4. In summary, the proximal convoluted tubule responds to acidosis by secreting hydrochloric acid and ammonium chloride while reabsorbing sodium bicarbonate. This makes the kidney very efficient in controlling the blood’s acidosis. It removes acid from the blood while adding additional buffer. b. During alkalosis (respiratory or metabolic), the cells in this area solve this problem by adding acids to the blood while removing buffers from it. 1. Like acidosis, the proximal convoluted tubule responds to alkalosis by increasing its metabolism to create carbonic acid from carbon dioxide and water. However, it reverses its exchange of ions. 2. The tubule reabsorbs the hydrogen ions by exchanging them for sodium ions from the blood. The tubule secretes bicarbonate ions by trading them for chloride ions from the filtrate. The result, the tubule compensates for the alkalosis by adding hydrochloric acid to the blood while removing sodium bicarbonate. D. The countercurrent multiplier mechanism (CMM) is responsible for elevating the ion concentration within the renal medulla. Its purpose is to enable the nephron to produce a concentrated urine under any circumstance. It does this by making the collecting duct’s reabsorption of water more efficient. The actions of the loop of Henle and the vasa recta make the CMM possible. 1. The countercurrent multiplier mechanism got its name because the fluids with the loop of Henle and the vasa recta flow opposite to one another. Their action also results in multiplying the concentration of ions within the renal medulla (examine the countercurrent multiplier mechanism diagram). 2. The descending limb of Henle is relatively impermeable to sodium and chloride ions yet permeable to water. This causes the filtrate’s concentration to increase as it moves through the descending limb because water leaves the limb to enter the medulla’s more concentrated tissues. This water has little impact on the concentration of the medullary tissues because the ascending part of the vasa recta absorbs and carries this water away. 3. The ascending limb of the vasa recta wants to absorb this water so that its concentration matches that of the surrounding tissues. As blood moves through the ascending limb of this blood vessel, the tissues become more dilute. Therefore, the limb loses sodium and chloride ions to the tissue and absorbs water to lower its concentration. 4. The ascending limb of Henle actively transports chloride ions into the surrounding tissues. Sodium ions passively follow because the chloride ions are negative. The movement of sodium and chloride ions causes the filtrate’s concentration to decrease as it travels through the ascending limb because this limb is impermeable to water. These ions remain trapped within the medulla because: a. They will not be absorbed by the descending limb of Henle. b. If they are absorbed by the descending limb of the vasa recta, they will be dragged back down into the renal medulla. Upon moving through the ascending limb of the vasa recta, the sodium and chloride ions diffuse back out into the medulla before the blood enters the renal cortex. 5. In brief, the CMM causes the kidney’s cortical tissues to be dilute and its medullary tissues to be concentrated. This concentration gradient is always maintained and it enables the body to concentrate its urine under any circumstance. a. The collecting duct carries the dilute filtrate through the more concentrated medulla. If the body has plenty of water, the filtrate remains dilute and it passes into the urinary bladder. As a result, the body releases a 215 Unit 20 - Urinary System large volume, dilute urine. If the body is dehydrated, the body releases ADH. b. ADH opens pores within the walls of the collecting duct (an active movement). This action causes rapid reabsorption water from the collecting duct because of the concentration gradient maintained within the renal medulla. Therefore, the urinary filtrate becomes more concentrated and its concentration is proportional to the amount of ADH released. The result, the body voids a low volume, more concentrated urine. c. Reabsorption of water from the collecting duct does not effect the concentration of the renal medulla. This water will eventually move into the ascending limb of the vasa recta by osmosis. Here, it remains as the blood tries to match the concentration of the dilute cortical tissues. V. Under normal conditions, urinary output is about 1 to 2 liters per day. However, this value can be influenced by a variety of factors. A. The blood’s concentration influences the secretion of aldosterone and ADH. These hormones reduce urinary output as they perform their job. 1. Aldosterone is secreted to replenish low sodium levels. This decreases urinary output because water is passively reabsorbed from the filtrate as sodium is actively reabsorbed. 2. ADH is secreted to rehydrate the body. This decreases urinary output because water is reabsorbed from the urinary filtrate. Urinary output will increase if ADH is chronically low. This ailment is called diabetes insipidus. B. Diuretics are drugs that inhibit the facultative reabsorption of water. Therefore, they increase urinary output. Diuretics accomplish this task by blocking the action or secretion of ADH or aldosterone. The frequent urination stimulated by diuretics will also lower the blood’s volume. Therefore, doctors administer diuretics to treat patients with hypertension. 1. Hypertension can be caused for several reasons. However, many middleaged men experience hypertension because they lose control over their renin-angiotensin pathway and hypersecrete renin. 2. Remember, this pathway should only be initiated when blood pressure is chronically low. If a person with normal blood pressure accidentally hypersecretes renin, they will experience high blood pressure. Doctors treat this problem by administering an ACE inhibitor. This drug blocks the conversion of angiotensin I into angiotensin II. Thus, it returns the blood pressure to normal. VI. Urine consists of 95% water and 5% solute. The urinary solute is composed of a variety of substances (i.e., urea, creatinine, etc.). By studying the composition of urine (urinalysis), doctors can diagnose several ailments. Let’s examine this topic more closely. A. The amber color of urine is attributed to urochrome. This pigment is produced by the liver from hemoglobin as the liver catabolizes old red blood cells. As urochrome is produced, it is placed in the bloodstream, where it is removed by the kidneys. Urine becomes darker as urochrome’s concentration increases. Doctors use this coloration to determine the hydration of a patient. B. Bilirubin is seldom found in urine because its blood level is low. Like urochrome, this material is produced by the liver from red blood cell (hemoglobin) catabolism. When bilirubin is found in urine, it is called bilirubinuria. This condition is a sign of liver dysfunction. C. Sugar is seldom found in urine because the convoluted tubules have more than enough carriers to remove it. When sugar is found in the urine, it is called glycosuria. Glycosuria can be a temporary as the result of a poor diet. It can also be long-term, a sign of diabetes mellitus. D. Albumin is seldom found in urine because it is not permeable to the glomerular capsule. When albumin is found in urine, it is called albuminuria. This ailment can be caused by hypertension or be part of a disease process. Some ailments will perforate the glomerular capsule. If this occurs, the capsule will not be able to filter out the proteins from the urinary filtrate. E. Erythrocytes are seldom found in the urine. However, their presence is called hematuria. Like, albuminuria, hematuria can be caused by a perforated glomerular capsule or by hypertension. F. Leukocytes are seldom found in urine. However, their presence is called pyuria. Pyuria is usually the result of a tubular infection. G. Keto acids and ketones are seldom found in urine because their blood levels are low. When ketones are found in the urine, it is called ketosis or acetonuria. This ailment is caused by excessive beta oxidation. Excessive beta oxidation is associated with diabetes mellitus, starvation, a low carbohydrate diet, etc. H. Renal calculi or kidney stones are seldom found in urine. Kidney stones are caused by high blood salt concentrations or by prolonged dehydration. These conditions cause the stones to form within the renal pelvis and they block the flow of urine. This causes a considerable amount of pain because 216 Unit 20 - Urinary System the stones are insoluble in urine. Doctors use ultrasound techniques and diuretics to disintegrate the stones. 20. Urine formation requires three activities: reabsorption, filtration, and secretion. Answers in Appendix A VII. Because the removal of metabolic wastes is a big burden, other body systems assist the kidneys with this task. A. The integumentary system primarily removes heat, water, salts, and urea. This occurs as the body sweats. B. The digestive system primarily removes water and salts. This occurs as the body defecates. C. The respiratory system primarily removes carbon dioxide. This occurs as the body respires. URINARY SYSTEM SELF QUIZ True or False 1. ANS can control GFR. 2. The ascending limb of Henle actively transports sodium ions; chloride ions passively follow. 3. Aldosterone stimulates the distal convoluted tubule to actively reabsorb sodium ions. 4. The nephron is the functional unit of the kidney. 5. GHP will increase, if the afferent arteriole is constricted and the efferent arteriole is dilated. 6. Most of the body’s water is conserved through active reabsorption. 7. The kidneys secrete hydrogen ions in the form of ammonium ions. These ions are exchanged for sodium ions. 8. Renal tubules can buffer blood because they can produce hydrogen and bicarbonate ions from carbon dioxide and water. 9. The urethra transports urine from the kidney to the urinary bladder. 10. Urinary output is directly proportional to the blood’s aldosterone level. 11. The glomerular filtrate contains glucose and urea, but not proteins. 12. A decrease in the GOP causes an increase in GFR. 13. The countercurrent multiplier mechanism enables the kidney to produce a concentrated urine. 14. A renal corpuscle functions in secretion. 15. Pyuria is the presence of protein in the urine. 16. ADH causes the facultative reabsorbtion of water by the collecting duct. 17. The juxtaglomerular apparatus monitors the systemic blood pressure to control the nephron’s GFR. 18. Ketosis is the presence of glucose in the urine. 19. The cortical vein delivers blood directly to the interlobar vein. 217 Unit 20 - Urinary System URINARY PARTS TO KNOW Kidney hilum renal cortex renal medulla renal pyramids renal column major calyx minor calyx renal pelvis renal sinus renal artery renal vein segmental artery interlobar artery interlobar vein arcuate artery arcuate vein cortical artery cortical vein peritubular capillaries vasa recta Ureter Urinary Bladder Urethra Nephron renal corpuscle glomular capsule glomerulus proximal convoluted tubule descending limb of Henle loop of Henle ascending limb of Henle distal convoluted tubule collecting duct afferent arteriole efferent arteriole 218 Unit 20 - Urinary System Urinary Crossword 1 2 3 4 5 6 7 8 9 11 20 12 13 17 18 21 22 10 14 15 19 23 26 24 27 30 29 32 34 37 38 35 39 40 42 36 41 43 44 49 50 45 46 47 51 48 52 53 56 25 28 31 33 16 54 55 57 58 62 66 63 68 71 61 69 65 70 72 74 75 77 79 60 64 67 73 59 76 78 80 ACROSS 1 stimulates facultative reabsorption of water 2 wrds. 9 Arts and Entertainment channel abbv. 11 renal corpuscle does this 13 collects urine from the collecting ducts 2 wrds. 17 elemental symbol for cobalt abbv. 18 movie monster 19 Occupational Therapy abbv. 20 Caribbean music 22 secretion of chloride ions will help correct this 24 diabetes insipidus causes urine volume to be this 26 secretion and reabsorption refine the filtrate into this 27 holy woman 28 alone 29 pinna 30 this ion can be traded for hydrogen ion abbv. 31 lack of iodine can cause this 32 rodent 33 functional unit of the kidney 35 electronics company 37 __ Ladd, actor 38 to color a house again 40 to salivate 42 network that contains the urinary filtrate 43 world's fair 44 hypersecretion of this chemical can cause hypertension abbv. 46 fluid pressure within the filtrate that is essentially zero abbv. 47 et cetera abbv. 49 to remove materials from the blood and place them in the filtrate 51 ocular 53 once held 55 hairlike projection from the surface of a cell 56 tax collection agency abbv. 57 by mouth 58 tubules can do this process to buffer secreted hydrogen ions 63 to become hostile 64 kitchen convenience 65 election month abbv. 66 mistakes 68 classical musical play 70 proximal convoluted tubule passively reabsorbs this 71 performing platform 73 people with diabetes mellitus may pass this in their urine 74 lyrical poem 75 each 77 actor/director Howard 79 study of urine 80 renal pelvis lines this chamber 2 wrds. DOWN 219 Unit 20 - Urinary System 1 this vessel deliver blood to the glomerulus 2 wrds. 2 this system can also remove urea 3 up to the time of 4 MSH stimulates this 5 enzyme used by tubular cells to cope with changes in pH 2 wrds. 6 location of the calcaneal bones 7 to take out of the filtrate and place in the blood 8 snake-like fish 10 this sphincter is voluntarily controlled 12 drug used to control the renin-angiotensin pathway 2 wrds. 14 meaningless sounds 15 this ion is used in trading for bicarbonate 16 a Hindu theistic philosophy 21 elemental symbol for argon abbv. 22 prefix for flight 23 a pair 25 location of kidney within the body 33 aldosterone stimulates facultative reabsorption of this ion abbv. 34 National Rifle Association abbv. 36 waterfowl 39 a major division of geological time 41 prescription 45 Drug Enforcement Agency abbv. 48 the loop of Henle does this abbv. 50 this describes the reabsorption of water by the proximal convoluted tubule 52 fluid found within the tubular network 53 this will be reabsorbed during alkalosis 54 micturition 59 Russian space station 60 type of immune cell abbv. 61 neither 62 this tube conveys urine to the urinary bladder 63 old soap: ____ the World Turns 67 regional term for kidney 69 physical education abbv. 72 hustle and bustle 75 respiratory system is concerned with this 76 this can adjust the glomerular filtration rate abbv. 78 elemental symbol for lithium abbv. Answers in Appendix B 220