LIPIDS II
advertisement

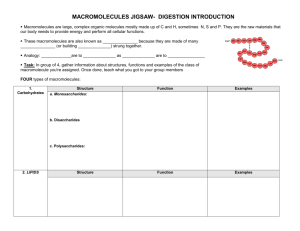
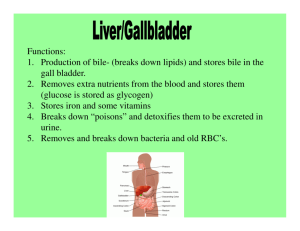
LIPIDS II Key words: lipids, triacylglycerols, 2-monoacylglycerols, fatty acids, ester bond, hydrolytic cleavage of fats, pancreatic lipase (EC 3.1.1.3.), tensides, bile salts, free radicals, chain reaction, cell membranes, peroxides, reaction of aldehydes with amino groups, antioxidants, chelates. Reagents: 1. Extract of pancreatic lipase (dissolve 40 pills of Pancreolan (ZENTIVA) in a 400 ml blend of water and glycerol (1:1) and filtrate) 2. Sunflower oil 3. Ethanol 0,01 mol/l 4. Sodium hydroxide solution 5. Solution of phenolphtaleine in ethanol 2 g/l 40 g/l 6. Solution of cod-liver oil in hexane 7. Phosphate buffer, pH 7.0 0.05 mol/l 0.05 mol/l 8. Phosphate buffer, pH 9.0 9. Bile salts solution 100g/l 10 g/l in ethanol 10. Oleic acid solution Lipid digestion and absorption Fats should consistitute about 25%-30% of the total daily caloric intake. Most of the consumed lipids are triacylglycerols (TAGs, esters derived from glycerol and 3 fatty acids), which serve as the main energetic reservoir in human. TAG digestion occurs mainly in the small intestine, where the activity of pancreatic lipase results in a complex mixture of diacylglycerols, monoacylglycerols and free fatty acids (FFA). The main path (due to the lipase specificity) progresses from triacylglycerol to 2,3-diacylglycerol and finally to 2-monoacylglycerol. Only a small percentage of the TAGs (20%) is completely hydrolyzed to free glycerol upon isomerization of 2-monoacylglycerol to 1or 3-monoacylglycerol. After the absorption of FFA and 2-monoacylglycerol into the enterocytes, TAGs are resynthetised intracellularly and pass from the cell into the lymphatic vessels as chylomicrons (lipoprotein particles), whereas short-chain fatty acids (C<12) pass into the portal blood directly. Role of bile acids in fat digestion and absorption Bile acids facilitate the digestion of TAGs by emulsifying them (fat globules are broken down or emulsified into small droplets) that makes fats accessible to pancreatic lipases in the intestine. Bile acids are amphipathic, they contain both hydrophobic (lipid soluble cyklopentanoperhydrophenantrene) and polar (hydrophilic hydroxyl and carboxyl groups that can be conjugated by glycine or taurine) regions. Bile acids are the end products of cholesterol metabolism in the liver. The primary bile acids, chenodeoxycholic acid and cholic acid (the primary bile acids) represent the most abundant bile acids in human bile (45%, 31%, respectively). These undergo a deconjugation process in the intestine (the glycine or/and taurine residues are removed). The secondary bile acids (i.e. deoxycholate (from cholate) and lithocholate (from chenodeoxycholate)) are modified primary bile acids by anaerobic bacteria present in the colon. Bile acids are further excreted (~ 5%) or reabsorbed by the distal ileum and returned to the liver (95% of total bile acids). The process of secretion from the liver to the gallbladder, to the intestines and finally reabsorption is termed the enterohepatic circulation. Pancreatic lipase Pancreatic lipase is the primary enzyme that hydrolyzes TAGs. Gastric and lingual lipases, comprise the two acidic lipases. These lipases, unlike the alkaline pancreatic lipase, do not require bile acid or colipase for optimal enzymatic activity. Acidic lipases contribute to lipid hydrolysis in human adult by 30%, with gastric lipase contributing the most of the two. However, acidic lipases provide 50% of total lipolytic activity in neonates, because of the insufficient alkaline lipase secretion from the immature pancreas. Pancreatic lipase is secreted into the duodenum through the duct system of the pancreas together with its cofactor (colipase), which enhances its activity. The TAG hydrolysis occurs on the surface of lipid droplets (size 200-500 nm). The resulting monoacylglycerols, diacylglycerols and free fatty acids form polymolecular aggregates with bile acids, cholesterol, lysophospatides and lipid-soluble vitamins. These aggregates have much smaller diameter than the unhydrolyzed precursor particles (3-10 nm) allowing them access to the intramicrovillus spaces of the intestinal membranes. Micelles interact with the enterocyte and lipid content of the micelle diffuse into the enterocyte, moving down a concentration gradient. Inside a cell, TAG re-forms and pass from the cell into the lymphatic vessels and portal blood as chylomicrons (lipoprotein particles), whereas short-chain fatty acids (C<12) pass into the portal blood directly. The aim of this practical lesson is to demonstrate the emulsifying ability of bile acids and their importance for the activity of pancreatic lipase. Clinical notes: * High level of pancreatic lipase in the plasma is associated with pancreatic disorders. Determination of pancreatic lipase together with the pancreatic isoenzyme α-amylase are test used to diagnose acute pancreatitis. * Orlistat (tetrahydrolipstatin) is used for obesity treatment by irreversible inhibiting the gastric and pancreatic lipases. The decreased absorbtion of the dietary fat (up to 30%) implies the most frequent side effect, which is steatorhea. * Pancreatic insufficiency is the inability of the pancreas to produce and/or transport enough digestive enzymes to digest and absorb lipids and lipid-soluble vitamins in the intestine. Pancreatic insufficiency is most frequently associated with cystic fibrosis in children and with chronic pancreatitis in adults, but sometimes also with pancreatic cancer. Usually weight loss, nausea and steatorhea appear. A non-invasive breath test for assessment of fat digestion has been developed based on the hydrolysis of 13C labelled triacylglycerols. Low levels of pancreatic enzymes can be supplied by enterosolvent tablets. * Apolipoproteinemia (Bassen-Kornzweig syndrom) is a rare disorder caused by a mutation in microsomal triglyceride transfer protein resulting in deficiencies in the apolipoproteins B-48 and B-100, which are used in the synthesis and export of chylomicrons and VLDL, respectively. The inability to absorb fat results in steatorrhea, and impaired function of the nervous system. 1.Lipase mediated cleavage of fats – the influence of bile salts Principle: Bile salts emulsify lipids in the small intestine and facilitate interactions of fats and pancreatic lipase. This enzyme is insoluble in fats and acts on the surface of fat droplets. The emulsification increases the total surface of lipids. Lipase is activated indirectly by this way. Pancreatic lipase catalyses the cleavage of ester bond of triacylglycerols, usually at positions 1 and 3 of the glycerol residue. Free fatty acids and 2-monoacylglycerol are the main products of lipids hydrolysis. Procedure: a. Pipette 1 ml of lipase extract into the tube 1 and heat for 3 min in the boiling water bath. Cool under the flow of cold water (blank). b. Pipette 1 ml of lipase extract into the tubes 2 and 3. c. Proceed in the preparation of reaction mixtures according to the table 1. Table 1. Test tube N° 1 2 3 Lipase extract (ml) 1,0 1.0 1.0 Incubate at 100°C 3 min - - Distilled H2O (ml) 0.5 0.5 - - - 0.5 0.25 0.25 0.25 Bile acid solution (ml) Olive oil (ml) Volume of NaOH (ml) Net volume of NaOH (ml) Free fatty acids (mmol) d. Mix the content of the tubes and incubate for 30 min at 37o C. e. Transfer the content of the tubes into a small flask and rinse out the tubes twice with 1 ml of ethanol. Add the rinsed ethanol into the appropriate flask. f. Titrate the samples containing free fatty acids with NaOH in the presence of a few drops of phenolphthalein until the solution turns pink. g. Note the added volume of NaOH. h. Subtract the NaOH volume for blank (test tube 1, free fatty acids in oil without lipolytic digestion) from the NaOH volume in the tubes 2 and 3. Note the results into the table 1. Calculate the amount of FFA in mmol. 2 Emulsification of oil by bile salts Principle: Hydrolysis of monoacylglycerols and FFAs in the small intestine depends on their dispersion in aqueous phase. Bile acids act as anion active tensides (Lipids I, 3.2.), decreasing the surface tension between oil-water interface. Procedure: Pipette the substances in the test tubes, see table below: Table 1 Test tube no. Buffer pH 7 (ml) Buffer pH 9 (ml) Distilled water (ml) Solution of bile salts (ml) Ethanol (ml) Solution of olei acid (drops) Result (+/-) 1 1 0.5 2 2 1 0.5 2 3 1 0.5 2 a. Shake well and incubate in water bath for 10 min at 37° C. b. Compare the emulsification ability of bile acids, ethanol and pH. 4 1 0.5 2