Social Information Processing in Elementary
advertisement

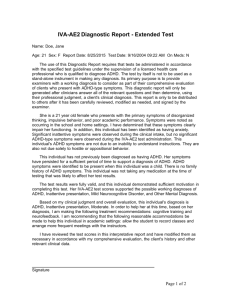
J Abnorm Child Psychol (2009) 37:579–589 DOI 10.1007/s10802-008-9294-9 Social Information Processing in Elementary-School Aged Children with ADHD: Medication Effects and Comparisons with Typical Children Sara King & Daniel A. Waschbusch & William E. Pelham Jr & Bradley W. Frankland & Brendan F. Andrade & Sophie Jacques & Penny V. Corkum Published online: 24 December 2008 # Springer Science + Business Media, LLC 2008 Abstract Examined social information processing (SIP) in medicated and unmedicated children with ADHD and in controls. Participants were 75 children (56 boys, 19 girls) aged 6–12 years, including 41 children with ADHD and 34 controls. Children were randomized into medication conditions such that 20 children with ADHD participated after receiving placebo and 21 participated after receiving methylphenidate (MPH). Children were shown scenarios depicting peer interactions and asked to interpret each scenario and to generate possible responses to the scenario. This work was supported by an NSHRF Student Research Award awarded to Dr. King. During the preparation of this manuscript, Dr. Pelham was supported in part by grants from the National Institute of Mental Health (MH53554, MH069614. MH069434, MH078051, MH080791, MH064154), National Institute of Alcohol Abuse and Alcoholism (AA11873), National Institute on Drug Abuse (DA12414), Department of Education—Institute of Educational Sciences (L03000665A, R324B060045, R324J060024), Department of Health and Human Services—Administration for Children and Families (90YR0017/01), and by Eli Lilly Corporation. Dr. Waschbusch was also supported by some of these grants. S. King (*) Centre for Pediatric Pain Research, IWK Health Centre, Dalhousie University and IWK Health Centre, Departments of Pediatrics and Psychology, 5850/5980 University Ave., Halifax, NS, B3K 6R8, Canada e-mail: sara.king@dal.ca D. A. Waschbusch : W. E. Pelham Jr Departments of Pediatrics and Psychology, Center for Children and Families, University at Buffalo, Buffalo, NY, USA B. W. Frankland : B. F. Andrade : S. Jacques : P. V. Corkum Dalhousie University, Department of Psychology, Halifax, NS, B3H 4J1, Canada Results showed that children with ADHD who received MPH generated more hostile responses to provocation than controls, but children with ADHD on placebo did not. Results also showed that children with ADHD regardless of medication generated more hostile responses to provocation than to peer entry, whereas controls did not. Findings suggest that children with ADHD generate more aggressive responses to provocation than controls and that this may be exacerbated by administration of MPH. Limitations and future directions are discussed. Keywords ADHD . Methylphenidate . Social information processing . Peer relationships . Aggression Attention deficit hyperactivity disorder (ADHD) is one of the most common and most studied disorders of childhood (Rowland, Lesesne, and Abramowitz 2002; Tannock 1998; Wolraich 1999). ADHD is characterized by persistent, impairing, and developmentally inappropriate inattention, hyperactivity, and impulsivity (American Psychiatric Association 2000). Long-term outcomes for individuals diagnosed with ADHD are varied but individuals diagnosed with the disorder often experience difficulties across many areas of functioning (e.g., academics, social functioning) (Mannuzza and Klein 1999; Satterfield and Schell 1997; Weiss and Hechtman 1993) Children with ADHD are especially impaired in the area of peer relationships (Hoza 2007; Milich and Landau 1989; Pelham and Milich 1984). Research shows that at least 50% of children with ADHD have peer relationship problems (Guevremont and Dumas 1994; Hoza et al. 2005a; Milich and Landau 1982; Stormont 2001). These difficulties seem to be pervasive, as children with ADHD are often less liked 580 by peers within days or even minutes of first meeting them (Hinshaw and Melnick 1995; Pelham and Bender 1982). Further, peer relationship problems in children with ADHD have proven to be unresponsive to many treatments, even when other important outcomes show significant improvement (Hoza et al. 2005b; Pelham and Bender 1982; Pelham et al. 1988). These findings are important because dysfunctional peer relations in childhood are one of the strongest predictors of poor outcomes in adolescence and adulthood (Cowen, Pederson, Babigian, Izzo and Trost 1973; Landau et al. 1998a; Parker and Asher 1987). Though it is clear that children with ADHD tend to have peer relationship problems, the reasons for these difficulties remain unclear. For example, research has shown that children with ADHD have both knowledge deficits and performance deficits when engaging in social interactions (Guevremont and Dumas 1994; Landau et al. 1998b). That is, children with ADHD appear less knowledgeable than typically developing children about appropriate social behaviors and they are less likely to behave in socially appropriate ways when interacting with peers. Given such findings, it is possible that using a social information processing framework may aid in understanding the extent of the social difficulties experienced by children with ADHD. Social information processing refers to the mental processes involved in an individual’s perceptions of and reactions to other individuals in his or her social environment. Social information processing theory asserts that social cognitions lead to observable behaviors that, in turn, provide the basis by which the individual is evaluated by others (Crick and Dodge 1994; Dodge et al. 1986; Huesmann 1998; Rubin and Coplan 1992). Successful evaluation of social information is a key component of competent social performance and behaviour and of positive relationships with peers. Conversely, inaccurate evaluation of social information results in incompetent social performance and behaviour and poor relationships with peers. One of the most commonly used models of social information processing was proposed by Dodge (1986) and later reformulated by Crick and Dodge (1994). This model suggests that individuals execute a series of six interdependent social information processing steps when evaluating a social situation: (1) encoding of relevant stimulus cues; (2) interpretation of cues; (3) clarification of goals; (4) response access or construction; (5) response decision; and (6) behavioural enactment. This model of social information processing has been used extensively to examine social behaviour in aggressive children. Studies have demonstrated that aggressive children, as identified by classroom peers and teachers, show differences in social information processing patterns when compared to nonaggressive children. Specifically, when compared to nonaggressive children, aggressive children are more likely to J Abnorm Child Psychol (2009) 37:579–589 encode less information before making a decision regarding a peer’s intentions, to assume that a peer is acting in a hostile manner, and to generate more aggressive and incompetent solutions to social problems (Dodge 1980; Milich and Dodge 1984; Rubin et al. 1991). For example, early research on social information processing showed that aggressive children were more likely than nonaggressive children to attribute hostility to peer provocateurs in ambiguous social situations that have negative outcomes (Dodge 1980; Dodge and Frame 1982). Based on this and other evidence, Dodge (1986) has argued that aggressive children often demonstrate a hostile attribution bias in ambiguous social situations. That is, when faced with a social situation in which a provocateur’s intent is unclear and the outcome of the provocateur’s action is negative, aggressive children will be more likely to interpret the other child’s intent as hostile and to respond in a hostile, aggressive manner. Additionally, when faced with hypothetical social problems, aggressive children have been found to have a response decision bias in that they generate a higher number of aggressive solutions than their nonaggressive peers, (Dodge 1980; Milich and Dodge 1984). For instance, research shows that when aggressive children are presented social dilemmas they are more likely to generate and subsequently choose aggressive strategies such as bribery, affect manipulation or antagonism, whereas other children are more likely to generate and chose prosocial strategies (Rubin et al. 1991). Although numerous studies have examined the social information processing abilities of children with high rates of aggressive behaviors, relatively little is known about the social information processing abilities of children with ADHD. This is an important area of study for a number of reasons. First, a substantial portion of children with aggressive behaviour also meet criteria for ADHD (Hinshaw 1987; Waschbusch 2002). In fact, in clinical samples it is rare to find aggressive children who do not also meet criteria for ADHD (Pliszka Carlson and Swanson 1999). Second, children with ADHD share many of the same social difficulties as aggressive children. That is, like aggressive children, children with ADHD display inappropriate behaviour with peers (Milich et al. 1982; Whalen et al. 1979), have poor social judgment (Melnick and Hinshaw 1996; Whalen et al. 1990), and are often rejected by peers (Frankel and Feinberg 2002; Henker and Whalen 1999). Third, research suggests that behaviors associated with ADHD make unique contributions to understanding peer relationship problems, even after controlling for behaviors associated with aggression (Atkins et al. 1989; Pope et al. 1989; Waschbusch 2002). Given these findings, it is possible that the social problems often experienced by children with ADHD are a manifestation of deviant social information processing, just as it appears to be in aggressive children. J Abnorm Child Psychol (2009) 37:579–589 Very little research has examined social information processing in children with ADHD, but the few studies that exist suggest difficulties in this area. One early study compared response decision biases, hostile attribution biases, and cue utilization deficits in control, ADHD-only, ADHD-aggression and aggressive-only groups (Milich and Dodge 1984). Results showed that the ADHD-aggressive group was more deviant than controls on all three measures and more deviant than the ADHD-only and aggressive-only groups on the response decision and cue utilization measures. Another study found that ADHD-aggressive children have difficulty anticipating the consequences of their actions and are more likely than typical children to generate aggressive solutions to problems (Bloomquist et al. 1997). Likewise, in a study examining knowledge of appropriate social behaviour in hyperactive and typically developing children, hyperactive participants’ social knowledge was found to be deficient when compared to that of their typically developing peers (Grenell et al. 1987). Finally, it has been found that children with ADHD-only encode fewer social cues and generate fewer responses to social problems than controls, whereas children with oppositional defiant disorder or conduct disorder (ODD/ CD) and children with both ADHD and ODD/CD are also more likely to display confidence in their ability to enact an aggressive response and to select an aggressive response when given a choice (Matthys et al. 1999). Taken together, these studies suggest that children with ADHD may have biased social cognitive styles in general, and impaired social information processing in particular. This may be especially true for children with both ADHD and aggression. If, as suggested above, children with ADHD have deviant social information processing abilities, then a key question is whether treatments that have been found to be effective for behavioural and performance decrements associated with ADHD are also effective for remediating their social information processing deficits. For example, if treatment improves attention, it could allow children with ADHD to encode a greater percentage of relevant social cues (i.e., improve their cue encoding), which in turn could improve the subsequent social processing steps. Likewise, if treatment improves impulse control, it could lead children to generate more responses and make more considered decisions about which response they choose to enact. Thus, there are sound theoretical arguments to suggest that effective treatment of ADHD symptoms may also improve social information processing deficits, but little research has examined this empirically. Stimulant medication such as methylphenidate (MPH), which is better known by the brand name Ritalin®, is one of the most widely used and well established treatments for ADHD (Centers for Disease Control 2005; Swanson et al. 1995). MPH has been shown to significantly decrease the 581 high rates of hyperactive, impulsive, and inattentive behaviours associated with ADHD in about two-thirds of children with the disorder (MTA Cooperative Group 1999). In addition, MPH has been found to have a positive effect on the overt negative social behaviours of children with ADHD in that both the rate and intensity of aversive behaviours such as aggression decrease (Connor et al. 2002; Hinshaw 1991; Hinshaw and Lee 2000). However, MPH seems to have no effect, or perhaps a negative effect, on increasing prosocial behaviour (Buhrmester et al. 1992; Hinshaw et al. 1989). Further, while there is mixed evidence regarding whether MPH improves peer relationships in children with ADHD, there is consistent evidence that even when improvements are demonstrated they remain impaired relatively to typical children (Hoza et al. 2005a; Whalen et al. 1989). Thus, there is clear evidence that MPH is associated with acute improvement on the core behaviours associated with ADHD (inattention, impulsivity, hyperactivity), but mixed evidence regarding the impact of MPH on social functioning, leaving unclear what impact MPH may have on social information processing. Only one study has examined the effects of MPH on social information processing skills of children with ADHD (Murphy et al. 1992). The authors of this study argued that MPH might have an effect on social information processing in children with ADHD due to the medication’s effects on the CNS pathways regulating attention and impulsivity. In particular, the authors posited that medication would lead to greater regulation of attention and impulse control, which in turn would lead to more complete encoding of social cues and more appropriate responses to ambiguous social situations. However, results indicated that, with respect to social information processing, MPH had no significant effects except for increased cue recall. However, the study lacked a control group of typically developing children and used a small sample, with just 10–11 children per group, raising the possibility that the lack of effects may have resulted from low statistical power. In fact, within-subject effect sizes from this study suggested that there was a decrease in hostile attributions in response to MPH for the ADHD children with low levels of aggression (Cohen’s D=0.91), but an increase in hostile attributions in response to MPH for the ADHD children with high levels of aggression (Cohen’s D=−0.70). These nonsignificant, yet interesting findings, combined with the overall dearth of research investigating the effects of MPH on social information processing in children with ADHD clearly indicate that more research in this area is warranted. The current study examined whether the social information processing skills of children with ADHD differed from those of typical children and whether children with ADHD differed as a function of whether or not they received stimulant medication. Based on previous literature (Milich 582 J Abnorm Child Psychol (2009) 37:579–589 and Dodge 1984; Murphy et al. 1992), it was hypothesized that: (1) children with ADHD would show a more pronounced hostile attribution bias when compared to typically developing children; (2) children with ADHD would choose more aggressive, unfriendly responses compared to typically developing children; (3) MPH would not significantly affect either hostile attribution or response generation measures in children with ADHD. Method Participants Participants were 75 children (56 boys, 19 girls) between the ages of 6 and 12 years (M=9.15, SD=2.00), including 41 children with ADHD and 34 typically developing children who participated in the study as controls. Children with ADHD were randomly assigned to participate after receiving MPH (n=21) or a placebo (n=20). Participants were recruited from two locations: Buffalo, NY and Halifax, Nova Scotia. Groups from the two locations did not differ on age, F (1,73)=1.82, p=.18 or sex, χ2(1)=1.81, p=0.18. With respect to ethnicity, 69 (92%) of participants were identified as Caucasian, whereas 6 (8%) were identified as African American. Site differences in ethnicity showed a trend towards significance, χ2(1)=3.46, p=0.06, as all African American children were part of the Buffalo sample. Table 1 summarizes demographic and rating scale measures for the ADHD group randomly assigned to receive placebo (ADHD-placebo), the ADHD group randomly assigned to receive medication (ADHD-med), and for the control group. As can be seen, control and ADHD groups differed in expected ways on measures of ADHD, ODD, and CD, whereas children in medication and placebo groups did not differ on measures of ADHD, ODD, and CD. The children with ADHD were enrolled in an eight-week comprehensive summer treatment program (STP) for children with ADHD (Pelham et al. 1998). ADHD was evaluated using DSM-IV criteria (American Psychiatric Association 2000) as determined by parent and teacher ratings on the Disruptive Behavior Disorders Rating Scale (DBD, Pelham et al. 1992) and the Impairment Rating Scale (Fabiano et al. 2006), and by a structured diagnostic interview with parent(s) on the Diagnostic Interview Schedule for Children (DISC; NIMHDISC Editorial Board 1999). Diagnoses were made by doctoral level clinicians using all available information. Control children (n=34) were recruited from two sources. Eight children were enrolled as control children in the STP in Buffalo (for research purposes only), two children had been enrolled as controls in a previous STP in Halifax and were contacted to participate in the study, and the remaining control children (n=24) were recruited from the community using radio and television advertising, as well as flyers posted in public places (grocery stores, libraries, health centres). Control children were screened for behaviour and other adjustment difficulties using parent ratings on the DBD (Pelham, et al. 1992), Aggression Scales (Dodge and Coie 1987), the DISC (NIMH-DISC Editorial Board 1999), and the Impairment Rating Scale (Fabiano et al. 2006). Control children with evidence of clinically significant behaviour problems, defined as having a score above the published Table 1 Demographic and rating scale data as a function of group No diagnosis n=34 Number (%) boys 22 (64.7%) Age in years 8.91 (1.93) # of symptoms endorsed by parent on the DBD ADHD-Inattentive 0.32a (0.77) ADHD-Hyp/Imp 0.21a (0.59) ODD 0.15a (0.36) CD 0a (0) Clinical diagnoses ADHD 0a (0%) ODD 0a (0%) CD 0a (0%) ODD or CD 0a (0%) ADHD Placebo n=20 ADHD Med n=21 F-value / χ2 value 15 (75.0%) 9.82 (2.02) 19 (90.5%) 8.93 (2.04) χ2 =4.56 F= 1.50 7.25b 5.85b 4.85b 1.30b 7.10b 6.43b 4.52b 1.10b (1.84) (1.94) (2.34) (1.14) F=183.51* F=141.92* F=61.62* F=16.18* 21b (100%) 11b (52.4%) 4b (19.0%) 15b (71.4%) χ2 =75.00* χ2 =25.81* χ2 =8.83* χ2 =44.13* (2.10) (2.06) (2.41) (1.34) 20b (100%) 11b (55.0%) 5b (25.0%) 16b (80.0%) Values in Tables are means with standard deviations in parentheses or frequency counts with percentages in parentheses. DBD = Disruptive Behavior Disorders Rating Scale (Pelham et al. 1992). ADHD = Attention-deficit/hyperactivity disorder; Hyp/Imp = Hyperactive/Impulsive; ODD = Oppositional Defiant Disorder; CD = conduct disorder. * denotes F-value or chi-square value differs at p<.05. Means or frequency counts within same row with different subscripts differ significantly at p<.05 in post hoc tests (Bonferroni adjusted pairwise comparisons for means and pairwise-chi square tests for frequencies). J Abnorm Child Psychol (2009) 37:579–589 norms on one or more of the measures, were excluded from participation. Behavioural Measures Disruptive Behavior Disorders Rating Scale (DBD, Pelham et al. 1992). The DBD is a 45-item rating scale comprised of the DSM-IV diagnostic criteria for ADHD, ODD, and CD. Raters are required to evaluate the presence or absence of a specific symptom by using a four-point Likert scale ranging from 0 (not at all) to 3 (very much). As recommended (Pelham et al. 1992), a symptom is considered to be present if it is rated as “pretty much” or “very much”. The number of symptoms rated as present was computed using DSM-IV criteria for ADHD, ODD, and CD (see Table 1). Parents of children recruited from the community were given a package of questionnaires (including the DBD) to complete while their children were taking part in the experimental protocol. Parents of children in the STP completed the DBD as part of the clinical assessment conducted prior to treatment. Reliability and validity of the DBD has been demonstrated in other samples (Massetti et al. 2005; Owens and Hoza 2003; Wright et al. 2007). Reliability in the current sample was adequate (αplacebo =0.59; αMPH =0.58; αcontrol =0.61). Diagnostic Interview Schedule for Children Version IV (NIMH-DISC Editorial Board 1999).The DISC is a highly structured diagnostic tool designed for use by nonclinicians (Shaffer et al. 2000). The instrument is based on diagnostic criteria drawn from DSM-IV (American Psychiatric Association 2000) and ICD-10 (World Health Organization 1993) and was designed to assess more than 30 psychiatric disorders occurring in children and adolescents. Questions on the DISC are all relatively short and responses are generally limited to “yes” or “no”, although some questions have a “sometimes” or “somewhat” option. Questions are read from the computer screen by the interviewer, the interviewee (i.e., the parent) indicates his or her response, and the examiner notes this response. To date, there have been no studies of reliability or validity carried out on the DISC; however, the agreement between earlier versions of the DISC and clinician ratings has been moderate to very good, with the exception of parent report of separation anxiety and youth report of ADHD, neither of which was included in this study. Experimental Measures Picture Stories (Dodge et al. 2002; Dodge et al. 1997; Dodge et al. 1995) . A series of eight picture stories were used to measure participant’s social information processing. Picture stories consisted of a cartoon picture and a short story about at least two children participating in various 583 social interactions and were based on the social information processing model proposed by Dodge (Crick and Dodge 1994; Dodge et al. 1986). Stories depicted either peer entry or peer provocation situations, with four stories of each type included in this task. The experimenter read the story to the child and the child was asked to pretend he or she was one of the children portrayed in the scenario. Examples of situations included in this series are being hit in the back with a ball thrown by another child (peer provocation) and asking to join a baseball game and being denied the opportunity (peer entry). Immediately after each picture/ story was presented to the child, he or she was asked (a) why he or she thought the other child(ren) in the picture behaved the way they did (Interpretation) and (b) what he or she would do in the same situation (Generation). Responses to parts (a) and (b) of the social information processing scenarios were recorded and coded immediately by the research assistant. Responses to part (a) were coded as either 1 (accommodating) or 2 (hostile) and responses to part (b) were coded as 0 (don’t know), 1 (nothing), 2 (ask again/ask why), 3 (command), 4 (seek adult punishment), or 5 (retaliate). Responses to each question were averaged over the stories after excluding “don’t know” responses. Therefore, scores indexing interpretation of scenarios ranged from 1 (accommodating) to 2 (hostile) and scores indexing response generation ranged from 1 (nothing) to 5 (retaliate). Higher scores represent more aggressive responding. A second coder, blind to the condition of the participants, coded 22 of the interviews (26 %) for reliability purposes. Inter-rater correlations for peer entry interpretation of intent and peer provocation interpretation of intent were 0.77 and 0.73, respectively. Inter-rater correlations for peer entry response generation and peer provocation response generation were .80 and .96, respectively. Procedure Parents of all children gave informed written consent for their children to participate in the study and children gave verbal assent to participate. All participants were treated in accordance with the requirements of the Research Ethics Board of the IWK Health Centre and the Child and Youth Institutional Review Board of the State University of New York at Buffalo. Medication Procedure As part of a larger study, all children who met the diagnostic criteria for ADHD participated in a placebo controlled, randomized medication assessment where medication condition (i.e., placebo, 0.15 mg/kg, 0.3 mg/kg, and 0.6 mg/kg) varied on a day-to-day basis (see Pelham 1993; Pelham et al. 2002 for a detailed description of the procedure). Varying medication dose on a daily basis has been widely used in other studies examining medication effects in children with ADHD (e.g., Hinshaw et al. 1989; 584 Pelham et al. 2001; Pelham et al. 2002; Pelham et al. 2001; Swanson et al. 2003) and is considered an optimal method of evaluating medication effects (Pelham 1993). In the current study, children who were randomly assigned to be tested on medication were tested on a day when they had received a dose of MPH equivalent to 0.3 mg/kg of body weight, rounded to the nearest 1.25 mg dose. Children assigned to the placebo condition received an inactive capsule. Medication and placebo were identically encapsulated in opaque pills so that neither staff members nor children were aware of the medication condition. A member of the research staff administered medication to ensure that children received the correct pill at the correct time each day. Testing took place at least 30 min and not more than three and a half hours after administration of the pill. Thirty-four (83%) of children with ADHD had previous experience with stimulant medication (i.e., methylphenidate, Adderall, Concerta). Assessment of Social Information Processing After obtaining parental consent and child assent to participate in the study, children accompanied a research assistant to a small office where they completed the Picture Stories. Children were presented with eight cartoon pictures of children engaging in various social situations; these pictures were black and white, with the exception of one child in the picture whose shirt was coloured in using a yellow highlighter. Children were asked to pretend that they were the highlighted child and to pretend that they were taking part in the pictured social situation. The research assistant then read a short paragraph describing the scene to the child. Following this description, the participant was asked two short questions regarding the social situation: (a) why do you think the other child acted this way? (Interpretation) and (b) what would you do if you were in this situation? (Generation). Responses were recorded verbatim and coded. Data Analyses Data were examined using 2 (Scenario: Entry vs. Provocation) × 3 (Group: Control vs. ADHD-Placebo vs. ADHD-med) mixed analyses of variance (ANOVAs), with Scenario as a within subjects factor and Group as a between subjects factor. The first ANOVA examined group differences in interpretation of intent; the dependent measure was average response to part (a) over the eight stories (maximum score of 2). The second ANOVA examined response generation to each scenario; the dependent measure was average response to part (b) over eight stories (maximum score of 5). Significant interactions were followed up with simple effects tests and Bonferroni adjusted pairwise comparisons and by examining means, standard deviations, and eta-squared (η2) effect sizes. J Abnorm Child Psychol (2009) 37:579–589 Table 2 Means (standard deviations in parentheses) of intent and response generation scores as a function of group Control Interpretation of intent Peer Entry 1.49 (0.33) Provocation 1.60 (0.32) Response generation Peer entry 1.77 (0.61) Provocation 2.07a (0.83) ADHD-Placebo ADHD-Med 1.58 (0.30) 1.65 (0.27) 1.46 (0.30) 1.62 (0.27) 1.66 (0.53) 2.60ab (1.08) 1.86 (0.94) 2.92b (1.30) Means within same row with different subscripts differ significantly at p<.05 in post hoc comparisons (simple effects tests and Bonferroni adjusted pairwise comparisons). Results Interpretation of Intent Means and standard deviations for dependent measures are summarized in Table 2. Results of the 2 (Scenario) x 3 (Group) ANOVA indicated a significant main effect of Scenario, F (1, 70)=6.24, p=0.015, η2 =0.082 such that children interpreted the provocation scenarios (M=1.62, SD=0.29) in a more hostile manner than the entry scenarios (M=1.52, SD=0.32), regardless of group. Neither the main effect of Group, F (2, 70)=0.45, p=0.641, η2 =0.013, nor the Group x Scenario interaction, F (2, 72)=0.38, p=0.682, η2 =0.011, were significant. Response Generation Results of the 2 (Scenario) x 3 (Group) ANOVA indicated a significant main effect of Scenario, F (1, 72)=42.58, p=0.000, η2 =0.37, a marginal effect of Group, F (2, 72)= 2.57, p=0.083, η2 =0.067, but these were qualified by a significant Group x Scenario interaction, F (2, 72)=4.30, p=0.012, η2 =0.120. The Group x Scenario interaction was followed up using two simple effects tests. First, Group was examined at each level of Scenario and results showed that Group was significant in the peer provocation condition, F (2, 72)=4.52, p=0.014, η2 =0.09, but not in the peer entry condition, F (2, 72)=0.40, p=0.674, η2 =0.01. Examination of means (see Table 2 and Fig. 1) and Bonferroni adjusted pairwise comparison showed that the ADHD-med group generated more hostile responses to peer provocation scenarios than the control group (p=0.014), with the ADHD-placebo group between (but not different than) either the control group (p=0.233) or ADHD-med group (p=1.00). Second, Scenario was examined separately for each group and results showed that Scenario was significant for ADHDplacebo, F (1, 72)=18.00, p=0.000, η2 =0.20, and ADHDmed, F (1, 72)=24.14, p=0.000, η2 =0.25, but not controls, F (1, 72)=3.16, p=0.080, η2 =0.04. As can be seen in Table 2 J Abnorm Child Psychol (2009) 37:579–589 5 R e s p o n s e Discussion 4.5 Control 4 G e n e r a t i o n 3.5 R a t i n g 2 585 ADHD-Placebo ADHD-Med 3 2.5 1.5 1 Peer Entry Provocation Scenario Type Note: Higher Scores = More Aggressive Fig. 1 Means and standard errors of response generation scores as a function of Scenario and group and Fig. 1, the two ADHD groups generated significantly more aggressive response to provocation as compared to peer entry scenarios but controls did not. Age and Sex Although groups did not differ with regard to age or sex, there was variation within and between groups on these factors (see Table 1). To evaluate whether these factors influenced the study results, analyses were repeated after including age and gender as covariates. Results were unchanged. Conduct Problems The majority of the two ADHD groups (n=31) consisted of children with both ADHD and conduct problems (i.e., ODD/CD) (ADHD/CP) with the remainder of the group (n=10) consisting of children without conduct problems (ADHD-only). The small number of children with ADHDonly did not allow for a direct comparison of ADHD/CP and ADHD-only. However, to evaluate whether results were unduly influenced by this heterogeneity, we repeated analyses after excluding the ADHD-only children. Results were unchanged. This study examined whether children with ADHD have social information processing deficits in comparison to typically developing children, and whether MPH influenced these abilities. It was hypothesized that: (1) children with ADHD would show a greater hostile attribution bias when compared to typically developing children; (2) children with ADHD would choose more aggressive, unfriendly responses compared to typically developing children; and (3) MPH would not significantly affect either hostile attribution or response generation measures in children with ADHD. Results showed mixed support for these hypotheses. Specifically, the ADHD and control groups did not differ on the measure of hostile attributions, but children with ADHD who were on medication, unlike those who had been given the placebo, generated more hostile responses to provocation scenarios than did control participants. These results are discussed in turn. Examination of the measure of hostile attribution bias showed that all children in the study inferred more hostile intent from scenarios depicting peer provocation relative to scenarios that depicted denial of entry into a peer group activity. This finding replicates other research showing that children infer more hostility in response to provocation than in response to refusal to join a peer activity (Dodge et al. 1986) and suggests that the measure we used is valid. However, this finding did not differ as a function of group; medicated and unmedicated children with ADHD did not differ from each other or from the control group on the measure of hostile attributions. Numerous studies have demonstrated that aggressive children tend to infer negative intentions in peers whose actions are ambiguous in situations with negative outcomes (Crick and Dodge 1996; Dodge et al. 1990; Dodge and Somberg 1987). The failure to find this same pattern in the present study, which used a sample of children with ADHD, suggests that the hostile attribution bias may be specific to aggression. However, this suggestion is speculative and future research should aim to clarify the relation between ADHD, aggression, and the hostile attribution bias. Results from the measure of response generation showed that children with ADHD in the MPH group generated more hostile and aggressive responses to peer provocation situations as compared to typically developing children, whereas children with ADHD on placebo did not differ from controls or from children in the medication group. Although these results may seem counter-intuitive, the findings are somewhat consistent with past research. As noted previously, the only other published study to examine the effects of medication on social cognition also provided evidence that MPH increased aggressive responses in at least some children with ADHD (Murphy et al. 1992). 586 Likewise, other research has also reported increased aggressive behaviour in both children and adults following MPH administration (Alioto 1999; Hinshaw et al. 1992; Murphy et al. 1992). The increased aggressive responses generated by medicated children with ADHD should be interpreted in light of the finding that both groups of children with ADHD (medicated and unmedicated) generated more hostile responses to peer provocation scenarios than they did to peer entry scenarios, whereas the control children did not show this pattern. This result is consistent with other research indicating that children with ADHD, and particularly children with ADHD and conduct problems, are especially reactive to provocation from peers (Murphy et al. 1992; Pelham et al. 1991; Waschbusch et al. 2002). These results suggest that children with ADHD are more likely than controls to generate aggressive responses to provocation, and that this may be exacerbated by administration of MPH. The implication of these findings is that response to provocation is an area of impairment in children with ADHD and this may be an important target for intervention (Hinshaw et al. 1989; Hinshaw et al. 1984). It is not clear why children in the MPH group generated more hostile responses to peer provocation scenarios but possible explanations can be speculated. One possible explanation is that MPH may have increased attention, which was used to selectively focus on hostile, negative cues presented in the vignettes, which in turn prompted the children to generate more hostile responses. Support for this explanation comes from research demonstrating that hostile responses are typically generated when children attend selectively to hostile cues and that one way to reduce hostile responding in aggressive children is to teach them to attend to more than just the hostile cues (Dodge and Newman 1981). An alternative explanation is that MPH may have allowed children to generate and select nonimpulsive yet aggressive responses. That is, by reducing impulsivity in children with ADHD (i.e., by administering MPH), it is conceivable that their reactive/impulsive aggressive tendencies might be suppressed thereby allowing for the emergence of proactive/planned aggressive tendencies; this possibility has been raised in other contexts (Hinshaw and Lee 2000). However, these explanations are speculative and don’t take into account several other factors that have been shown to be associated with hostile responding on these tasks, such as a history of physical maltreatment (Dodge et al. 1994; Dodge et al. 1995) and poor emotional regulation (Lemerise and Arsenio 2000). In other words, it is clear from this study that children with ADHD who were randomly assigned to receive stimulant medication had more hostile responses than did controls, whereas children with ADHD who were randomly assigned to receive a placebo did not differ from controls. However, the results of this study do not J Abnorm Child Psychol (2009) 37:579–589 shed light on what causes this association; inferring from this study that MPH causes children to generate more hostile responses is not warranted. It is also important to note that the finding of increased aggressive responses among children who received MPH is in contrast to numerous (but not entirely consistent) studies that show MPH decreases aggressive behaviour (see Connor et al. 2002; Hinshaw and Lee 2000 for a review). This seeming contradiction suggests that further research in this area is needed for two reasons: (a) to determine whether stimulant medication such as MPH actually does have a negative impact on specific aspects of social information processing, as suggested by some of the current results and (b) if so, to determine why aggressive behaviour seemingly decreases despite decrements in social information processing. It is possible that medication effects on aggressive behaviour may be independent of medication effects on social information processing. In fact, previous research suggests that medication effects on cognition and behaviour are often not correlated (Swanson et al. 1995). There were a number of limitations to this study. First, the majority of children were tested in the context of an intensive behavioural treatment program, which may have had an effect on their social information processing abilities. Indeed, research has shown that interventions using social skills training and problem solving discussions, both of which were used in the behavioural treatment, may help improve social competence in aggressive and “hard-tomanage” children (Fraser et al. 2005; Nangle et al. 2002). It should also be noted that children completed the current study at various points throughout their participation in the treatment program, meaning that some children may have had more experience with social skills training than others. Second, in administering the task, children were given as much time as they wished to respond, and this may have influenced the results. Dodge and Newman (1981) suggest that the hostile attribution bias is often not observed if aggressive children are given ample time to respond to hypothetical scenarios, which may account for the lack of group differences on this measure. On the other hand, the fact that differences emerged between the peer entry and provocation scenario argues against this explanation. Third, the current study used a between subjects design to examine medication effects, whereas within-subjects studies of medication effects are more powerful (Pelham 1993). A between subjects design was chosen due to the fact that, for practical reasons, it was only possible to test children one time. The current sample consisted of children ranging in age from 6 to 12 years and this may have affected responding to the social information processing scenarios. However, this explanation is likely to be inadequate, as groups did not differ with regard to age (or sex). Finally, because of a small sample size, it was not possible to distinguish J Abnorm Child Psychol (2009) 37:579–589 between ADHD children with and without aggression and/ or conduct problems (CP). However, the two ADHD groups did not differ significantly as a function of aggression or CP (see Table 1), and the distribution of CP in the current sample was typical of clinical samples of children with ADHD. Additionally, the primary goal of the current study was to examine stimulant medication effects on social information processing in children with ADHD. Nonetheless, it would be interesting and informative to replicate and extend the current study using a sample large enough to allow for a fully crossed design that would allow for the examination of medication effects, comorbid aggression and/or CP, and ADHD. The results of this study provide insight into the social information processing abilities of children with ADHD, but how these abilities relate to overt social behaviour remains unclear. It would be valid to include measures of social behaviour and/or development in future studies to elucidate the relation between laboratory measures of social information processing and in vivo social functioning. Further, future research should aim to clearly delineate correlates of social information processing in children with ADHD to determine the exact nature and extent of social difficulties in this population. Overall, the results of the current study suggest strongly that some aspects of social information processing may be impaired in ADHD, and that processing skills may be affected by drug interventions, although not necessarily in a positive way. Further research in this area is clearly needed and the findings of such research could ultimately lead to more streamlined and effective treatments for the disorder. Acknowledgement The authors wish to thank the children and families who participated in this study. References Alioto, A. (1999). The effects of methylphenidate on aggressive behavior in adults with and without Attention Deficit Hyperactivity Disorder symptomatology (Doctoral dissertation, Kent State University, 1999). Disseration Abstracts International, 60(1-B), 356. American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th text revision ed.). Washington, DC: American Psychiatric Association. Atkins, M. S., Pelham, W. E., & Licht, M. H. (1989). The differential validity of teacher ratings of inattention/overactivity and aggression. Journal of Abnormal Child Psychology, 17(4), 423–435. doi:10.1007/BF00915036. Bloomquist, M. L., August, G. J., Cohen, C., Doyle, A., & Everhart, K. (1997). Social problem solving in hyperactive-aggressive children: How and what they think in conditions of automatic adn controlled processing. Journal of Clinical Child Psychology, 26(2), 172–180. doi:10.1207/s15374424jccp2602_5. Buhrmester, D., Whalen, C. K., Henker, B., MacDonald, V., & Hinshaw, S. P. (1992). Prosocial behavior in hyperactive boys: 587 Effects of stimulant medication and comparison with normal boys. Journal of Abnormal Child Psychology, 20(1), 103–121. doi:10.1007/BF00927119. Centers for Disease Control (2005). Prevalence of diagnosis and medication treatment for attention-deficit / hyperactivity disorder— United States, 2003. Morbidity and Mortality Weekly Report, 54 (34), 842–847. Connor, D. F., Glatt, S. J., Lopez, I. D., Jackson, D., & Melloni, R. H. (2002). Psychopharmacology of aggression I: A meta-analysis of stimulant effects on overt/covert aggression-related behaviors in ADHD. Journal of the American Academy of Child and Adolescent Psychiatry, 41(3), 253–261. doi:10.1097/00004583-200203000-00004. Cowen, E. L., Pederson, A., Babigian, H., Izzo, L. D., & Trost, M. A. (1973). Long-term follow-up of early detected vulnerable children. Journal of Consulting and Clinical Psychology, 41(3), 438–446. doi:10.1037/h0035373. Crick, N. R., & Dodge, K. A. (1994). A review and reformulation of social information-processing mechanisms in children’s social adjustment. Psychological Bulletin, 115(1), 74–101. doi:10.1037/ 0033-2909.115.1.74. Crick, N. R., & Dodge, K. A. (1996). Social information-processing mechanisms in reactive and proactive aggression. Child Development, 67(3), 993–1002. doi:10.2307/1131875. Dodge, K. A. (1980). Social cognition and children’s aggressive behavior. Child Development, 51, 162–170. doi:10.2307/1129603. Dodge, K. A., & Coie, J. D. (1987). Social information processing factors in reactive and proactive aggression in children’s peer groups. Journal of Personality and Social Psychology, 53, 1146– 1158. doi:10.1037/0022-3514.53.6.1146. Dodge, K. A., & Frame, C. L. (1982). Social cognitive biases and deficits in aggressive boys. Child Development, 53, 620–635. doi:10.2307/1129373. Dodge, K. A., Laird, R., Lochman, J. E., & Zelli, A. (2002). Multidimensional latent-construct analysis of children’s social information processing patterns: Correlations with aggressive behavior problems. Psychological Assessment, 14(1), 60–73. doi:10.1037/1040-3590.14.1.60. Dodge, K. A., Lochman, J. E., Harnish, J. D., Bates, J. E., & Pettit, G. S. (1997). Reactive and proactive aggression in school children and psychiatrically impaired chronically assaultive youth. Journal of Abnormal Psychology, 106(1), 37–51. doi:10.1037/0021843X.106.1.37. Dodge, K. A., & Newman, J. P. (1981). Biased decision-making process in aggressive boys. Journal of Abnormal Psychology, 90 (4), 375–379. doi:10.1037/0021-843X.90.4.375. Dodge, K. A., & Somberg, D. R. (1987). Hostile attributional biases among aggressive boys are exacerbated under conditions of threats to the self. Child Development, 58, 213–224. doi:10.2307/1130303. Dodge, K. A., Price, J. M., & Bachorowski, J. (1990). Hostile attribution bias in severly aggressive adolescents. Journal of Abnormal Psychology, 99(4), 385–392. doi:10.1037/0021-843X.99.4.385. Dodge, K. A., Pettit, G. S., & Bates, J. E. (1994). Effects of physical maltreatment on the development of peer relations. Development and Psychopathology, 6(1), 43–55. Dodge, K. A., Pettit, G. S., Bates, J. E., & Valente, E. (1995). Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. Journal of Abnormal Psychology, 104(4), 632–643. doi:10.1037/0021843X.104.4.632. Dodge, K. A., Pettit, G. S., McClasky, C. L., & Brown, M. M. (1986). A social information processing model of social competence in children. With commentary by John M. Gottman. Monographs of the Society for Research in Child Development, 51(2), 1–85. doi:10.2307/1165906. Fabiano, G. A., Pelham, W. E., Waschbusch, D. A., Gnagy, E. M., Lahey, B. B., Chronis, A. M., et al. (2006). A practical 588 impairment measure: Psychometric properties of the Impairment Rating Scale in samples of children with attention-deficit/ hyperactivity disorder and two school-based samples. Journal of Clinical Child and Adolescent Psychology, 35(3), 369–385. doi:10.1207/s15374424jccp3503_3. Frankel, F., & Feinberg, D. (2002). Social problems associated with ADHD vs. ODD in children referred for friendship problems. Child Psychiatry and Human Development, 33(2), 125–146. doi:10.1023/A:1020730224907. Fraser, M. W., Galinsky, M. J., Smokowski, P. R., Day, S. H., Terzian, M. A., Rose, R. A., et al. (2005). Social information processing skills training to promote social competence and prevent aggressive behavior in third grade. Journal of Consulting and Clinical Psychology, 73(6), 1045–1055. doi:10.1037/0022006X.73.6.1045. Grenell, M. M., Glass, C. R., & Katz, K. S. (1987). Hyperactive children and peer interaction: Knowledge and performance of social skills. Journal of Abnormal Child Psychology, 15(1), 1–13. doi:10.1007/BF00916462. Guevremont, D. C., & Dumas, M. C. (1994). Peer relationship problems and disruptive behavior disorders. Journal of Emotional and Behavioral Disorders, 2, 164–172. Henker, B., & Whalen, C. K. (1999). The child with attention-deficit/ hyperactivity disorder in school and peer settings. In H. C. Quay, & A. E. Hogan (Eds.), Handbook of disruptive behavior disorders (pp. 157–178). New York: Kluwer Academic / Plenum Publishers. Hinshaw, S. P. (1987). On the distinction between attentional deficits/ hyperactivity and conduct problems/aggression in child psychopathology. Psychological Review, 101(3), 443–463. Hinshaw, S. P. (1991). Stimulant medication and the treatment of aggression in children with attentional deficits. Journal of Clinical Child Psychology, 20(3), 301–312. doi:10.1207/s1537 4424jccp2003_9. Hinshaw, S. P., & Melnick, S. M. (1995). Peer relationships in boys with attention-deficit hyperactivity disorder with and without comorbid aggression. Development and Psychopathology, 7(4), 627–647. Hinshaw, S. P., & Lee, S. S. (2000). Ritalin effects on aggression and antisocial behavior. In L. L. Greenhill, & B. B. Osman (Eds.), Ritalin: Theory and patient management (pp. 237–251, 2nd ed.). Larchmont, NY: M. A. Liebert Publishers. Hinshaw, S. P., Henker, B., & Whalen, C. K. (1984). Self-control in hyperactive boys in anger-inducing situations: Effects of cognitivebehavioral training and of methylphenidate. Journal of Abnormal Child Psychology, 12(1), 55–77. doi:10.1007/BF00913461. Hinshaw, S. P., Heller, T., & McHale, J. P. (1992). Covert antisocial behavior in boys with attention deficit hyperactivity disorder: External validation and effects of methylphenidate. Journal of Consulting and Clinical Psychology, 60, 274–281. doi:10.1037/ 0022-006X.60.2.274. Hinshaw, S. P., Henker, B., Whalen, C. K., Erhardt, D., & Dunnington, R. E. (1989). Aggressive, prosocial, and nonsocial behavior in hyperactive boys: Dose effects of methylphenidate in naturalistic settings. Journal of Consulting and Clinical Psychology, 57(5), 636–643. doi:10.1037/0022-006X.57.5.636. Hoza, B. (2007). Peer functioning in children with ADHD. Journal of Pediatric Psychology, 32(6), 655–663. doi:10.1093/jpepsy/jsm024. Hoza, B., Gerdes, A. C., Mrug, S., Hinshaw, S. P., Bukowski, W. M., Gold, J. A., et al. (2005a). Peer-assessed outcomes in the Multimodal Treatment Study of Children with Attention Deficit Hyperactivity Disorder. Journal of Clinical Child and Adolescent Psychology, 34(1), 74–86. doi:10.1207/s15374424jccp3401_7. Hoza, B., Mrug, S., Gerdes, A. C., Hinshaw, S. P., Bukowski, W. M., Gold, J. A., et al. (2005b). What aspects of peer relationshps are impaired in children with attention-deficit/hyperactivity disorder? Journal of Consulting and Clinical Psychology, 73(5), 411–423. doi:10.1037/0022-006X.73.3.411. J Abnorm Child Psychol (2009) 37:579–589 Huesmann, L. R. (1998). The role of social information processing and cognitive schema in the acquisition and maintenance of habitual aggressive behavior. In R. G. Geen, & E. Donnerstein (Eds.), Human aggression: Theories, research, and implications for policy (pp. 73–109). New York, NY: Academic Press. Landau, S., Milich, R., & Diener, M. B. (1998a). Peer relations of children with attention-deficit hyperactivity disorder. Reading and Writing Quarterly: Overcoming Learning Difficulties, 14, 83–105. Landau, S., Milich, R., & Diener, M. B. (1998b). Peer relations of children with attention deficit hyperactivity disorder. Reading and Writing Quarterly: Overcoming Learning Difficulties, 14, 83–105. Lemerise, E. A., & Arsenio, W. F. (2000). An integrated model of emotion processes and cognition in social information processing. Child Development, 71(1), 107–118. Mannuzza, S., & Klein, R. G. (1999). Adolescent and adult outcomes in attention-deficit/hyperactivity disorder. In A. E. Hogan, & H. C. Quay (Eds.), Handbook of disruptive behavior disorders (pp. 279– 294). New York: Plenum Press. Massetti, G. M., Pelham, W. E., & Gnagy, E. M. (2005, June). Situational variability of ADHD, ODD, and CD: Psychometric properties of the DBD interview and rating scale for an ADHD sample. Paper presented at the Annual Meeting of the International Society for Research in Child and Adolescent Psychopathology, New York, NY. Matthys, W., Cuperus, J. M., & Van Engeland, H. (1999). Deficient social problem solving in boys with ODD/CD, with ADHD, and with both disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 38(3), 311–321. doi:10.1097/ 00004583-199903000-00019. Melnick, S. M., & Hinshaw, S. P. (1996). What they want and what they get: The social goals of boys with ADHD and comparison boys. Journal of Abnormal Child Psychology, 24(2), 169–186. doi:10.1007/BF01441483. Milich, R., & Landau, S. (1982). Socialization and peer relations in hyperactive children. In K. Gadow, & I. Bailer (Eds.), Advances in learning and behavioral disabilities (vol. Vol. 1, (pp. 283– 339)). Greenwich, CT: JAI. Milich, R., & Dodge, K. A. (1984). Social information processing in child psychiatric populations. Journal of Abnormal Child Psychology, 12(3), 471–490. doi:10.1007/BF00910660. Milich, R., & Landau, S. (1989). The role of social status variables in differentiating subgroups of hyperactive children. In J. Swanson, & L. Bloomingdale (Eds.), Attention deficit disorders: IV. Current concepts and emerging trends in attentional and behavioral disorders of childhood (pp. 1–16). London: Pergamon. Milich, R., Landau, S., Kilby, G., & Whitten, P. (1982). Preschool peer perceptions of the behavior of hyperactive and aggressive children. Journal of Abnormal Child Psychology, 10(4), 497– 510. doi:10.1007/BF00920750. MTA Cooperative Group. (1999). A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 56(12), 1073–1086. doi:10.1001/archpsyc.56.12.1073. Murphy, D. A., Pelham, W. E., & Lang, A. R. (1992). Aggression in boys with attention deficit-hyperactivity disorder: Methylphenidate effects on naturalistically observed aggression, response to provocation, and social information processing. Journal of Abnormal Child Psychology, 20(5), 451–466. doi:10.1007/BF00916809. Nangle, D. W., Edrley, C. A., Carpenter, E. M., & Newman, J. E. (2002). Social skills training as treatment for aggressive children and adolescents: A developmental-clinical integration. Aggression and Violent Behavior, 7, 169–199. doi:10.1016/S1359-1789(00)00040-9. NIMH-DISC Editorial Board. (1999). The National Institute of Mental Health Diagnostic Interview Schedule for Children. Columbia University. Owens, J. S., & Hoza, B. (2003). Diagnostic utility of DSM-IV-TR symptoms in the prediction of DSM-IV-TR ADHD subtypes and J Abnorm Child Psychol (2009) 37:579–589 ODD. Journal of Attention Disorders, 7(1), 11–27. doi:10.1177/ 108705470300700102. Parker, J. G., & Asher, S. R. (1987). Peer relations and later personal adjustment: Are low-accepted children at risk? Psychological Bulletin, 102(3), 357–389. doi:10.1037/0033-2909.102.3.357. Pelham, W. E. (1993). Pharmacotherapy for children with attention-deficit hyperactivity disorder. School Psychology Review, 22(2), 199–227. Pelham, W. E., & Milich, R. (1984). Peer relations in children with hyperactivity/attentions deficit disorder. Journal of Learning Disabilities, 17, 560–567. Pelham, W. E., & Bender, M. E. (1982). Peer relationships in hyperactive children: Description and treatment. In K. Gadow, & I. Bailer (Eds.), Advances in learning and behavioral disabilities (vol. Vol. 1, (pp. 365–436)). Greenwhich, CT: JAI. Pelham, W. E., Gnagy, E. M., & Greiner, A. R. (1998). Children’s summer day treatment program manual. Buffalo, NY: CTADD. Pelham, W. E., Milich, R., Cummings, E. M., Murphy, D. A., Schaughency, E. A., & Greiner, A. R. (1991). Effects of background anger, provocation, and methylphenidate on emotional arousal and aggressive responding in attention-deficit hyperactivity disordered boys with and without concurrent aggressiveness. Journal of Abnormal Child Psychology, 19(4), 407–426. doi:10.1007/BF00919086. Pelham, W. E., Gnagy, E. M., Greenslade, K. E., & Milich, R. (1992). Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child and Adolescent Psychiatry, 31(2), 210–218. doi:10.1097/ 00004583-199203000-00006. Pelham, W. E., Gnagy, E. M., Burrows-MacLean, L., Williams, A., Fabiano, G. A., Morrisey, S. M., et al. (2001). Once-a-day Concerta methylphenidate versus t.i.d. methylphenidate in laboratory and natural settings. Pediatrics (on-line article), 107(6) http://www.pediatrics.org/cgi/content/full/107/106/e105. Pelham, W. E., Schnedler, R. W., Bender, M. E., Nilsson, D. E., Miller, J., Budrow, M. S., et al. (1988). The combination of behavior therapy and methylphenidate in the treatment of attention deficit disorders: A therpy outcome study. In L. Bloomingdale (Ed.), Attention deficit disorders III: New research in attention, treatment, and psychopharmacology (pp. 29–48). London: Pergamon. Pelham, W. E., Hoza, B., Pillow, D. R., Gnagy, E. M., Kipp, H. L., Greiner, A. R., et al. (2002). Effects of methylphenidate and expectancy on children with ADHD: Behavior, academic performance, and attributions in a Summer Treatment Program and regular classroom setting. Journal of Consulting and Clinical Psychology, 70(2), 320–335. doi:10.1037/0022-006X.70.2.320. Pope, A. W., Bierman, K. L., & Mumma, G. H. (1989). Relations between hyperactive and aggressive behavior and peer relations at three elementary grade levels. Journal of Abnormal Child Psychology, 17(3), 253–267. doi:10.1007/BF00917397. Rowland, A. S., Lesesne, C. A., & Abramowitz, A. J. (2002). The epidemiology of attention-deficit/hyperactivity disorder (ADHD): A public health view. Mental Retardation and Developmental Disabilities Research Reviews, 8, 162–170. doi:10.1002/mrdd.10036. Rubin, K. H., & Coplan, R. J. (1992). Peer relationships in childhood. In M. H. Bornstein, & M. E. Lamb (Eds.), Developmental Psychology: An advanced textbook (pp. 519–578, 3rd ed.). Hillsdale, NJ: Lawrence Erlebaum Associates. Rubin, K. H., Bream, L. A., & Rose-Krasnor, L. (1991). Social problem solving and aggression in childhood. In D. J. Pepler, & K. H. Rubin (Eds.), The development and treatment of childhood aggression (pp. 219–248). Hillsdale, NJ: Erlbaum. Satterfield, J. H., & Schell, A. (1997). A prospective study of hyperactive boys with conduct problems and normal boys: 589 Adolescent and adult criminality. Journal of the American Academy of Child and Adolescent Psychiatry, 36(12), 1726– 1735. doi:10.1097/00004583-199712000-00021. Shaffer, D., Fisher, P., Lucas, C. P., Dulcan, M. K., & Schwab-Stone, M. E. (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39(1), 28–38. doi:10.1097/00004583-20000100000014. Stormont, M. (2001). Social outcomes of children with AD/HD: Contributing factors and implications for practice. Psychology in the Schools, 38(6), 521–531. doi:10.1002/pits.1040. Swanson, J. M., McBurnett, K., Christian, D. L., & Wigal, T. (1995). Stimulant medications and the treatment of children with ADHD. In T. H. Ollendick, & R. J. Prinz (Eds.), Advances in clinical child psychology (vol. Vol. 17, (pp. 265–322)). New York: Plenum Press. Swanson, J. M., Gupta, S., Williams, L., Agler, D., Lerner, M., & Wigal, S. (2003). Efficacy of a new pattern of delivery of methylphenidate for the treatment of ADHD: Effects on activity level in the classroom and on the playground. Journal of the American Academy of Child and Adolescent Psychiatry, 41(11), 1306–1314. doi:10.1097/00004583-200211000-00011. Tannock, R. (1998). Attention deficit hyperactivity disorder: Advances in cognitive, neurobiological, and genetic research. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 39(1), 65–99. doi:10.1017/S0021963097001777. Waschbusch, D. A. (2002). A meta-analytic examination of comorbid hyperactive/impulsive/inattention problems and conduct problems. Psychological Bulletin, 128, 118–150. doi:10.1037/00332909.128.1.118. Waschbusch, D. A., Pelham, W. E., Jennings, J. R., Greiner, A. R., Tarter, R. E., & Moss, H. B. (2002). Reactive aggression in boys with disruptive behavior disorders: Behavior, physiology, and affect. Journal of Abnormal Child Psychology, 30(6), 641–656. doi:10.1023/A:1020867831811. Weiss, G., & Hechtman, L. T. (1993). Hyperactive children grown up: ADHD in children, adolescents, and adults. New York: Guilford. Whalen, C. K., Henker, B., & Granger, D. A. (1990). Social judgement processes in hyperactive boys: Effects of methylphenidate and comparisons with normal peers. Journal of Abnormal Child Psychology, 18(3), 297–316. doi:10.1007/BF00916567. Whalen, C. K., Henker, B., Collins, B., McAuliffe, S., & Vaux, A. (1979). Peer interaction in a structured communication task: Comparisons of normal and hyperactive boys and of methylphenidate (ritalin) and placebo effects. Child Development, 50, 388–401. Whalen, C. K., Henker, B., Buhrmester, D., Hinshaw, S. P., Huber, A., & Laski, K. (1989). Does stimulant medication improve the peer status of hyperactive children. Journal of Consulting and Clinical Psychology, 57(4), 545–549. doi:10.1037/0022-006X.57.4.545. Wolraich, M. L. (1999). Attention deficit hyperactivity disorder: The most studied and yet most controversial diagnosis. Mental Retardation and Developmental Disabilities Research Reviews, 5, 163–168. doi:10.1002/(SICI)1098-2779(1999)5:3<163::AIDMRDD1>3.0.CO;2-T. World Health Organization. (1993). The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. Geneva, Switzerland: Author. Wright, K. D., Waschbusch, D. A., & Frankland, B. W. (2007). Combining data from parent ratings and parent interview when assessing ADHD. Journal of Psychopathology and Behavioral Assessment, 29(3), 141–148. doi:10.1007/s10862-006-9039-4.