1 The Human Respiratory System Mary McKenna Lab Partners
advertisement

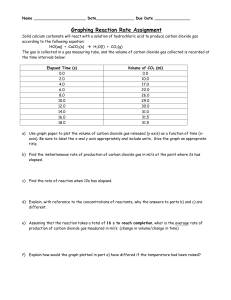
1 The Human Respiratory System Mary McKenna Lab Partners: Jennifer Daciolas-Semon Veronika Mach Colette Roblee TA: Pearl Chen NPB 101L Section 1 November 25, 2014 2 Introduction The average human will typically breath in and out at a rate of 22,000 times per day. Although the act of breathing is an unconscious doing, the respiratory system allows for this gas exchange between an organism and its environment. The respiratory system is a tightly governed bodily process and has multiple processes in order to keep the body functioning properly (Douglas & Haldane, 1909, pg. 420). In this experiment, multiple factors of the respiratory system were looked into. Specifically, measuring lung volume, the effects of inspired gas composition and lung volume on respiration, and exercise hyperpnea. In order to understand the experiment at hand, the basic physiology of the human respiratory system must be stated. Respiratory itself is defined as the act of obtaining oxygen from the environment and eliminating carbon dioxide from the body. The key organs involved are the lungs, which are composed of the respiratory passages, gas exchange surfaces, and pulmonary circulation (Sherwood, 2013, pg. 457). There are two types of respiration; internal and external. Internal involves the intracellular metabolism in mitochondria and the making of ATP. External is the main type of respiration that was tested in this experiment and is the exchange of oxygen and carbon dioxide. There are two main stages comprising external respiration. The first being the most simple – breathing. The second includes the alveolar gas exchange, which is the exchange of oxygen and carbon dioxide between gas in the alveoli and blood in the pulmonary capillary. Alveoli are small, air-filled, thin-walled sacs where gas exchange occurs. They are surrounded by capillaries and increase the surface area for exchange. They are made of two types of cells. Type II cells secrete pulmonary surfactant that decreases surface tension, preventing collapse of the lungs. Type I cells are very thin so gases can diffuse through them easily. The method leading gas exchange is easily explained by the gradient in pressure between the alveoli and the atmosphere. This provides the force to move air in and out. Although this process appears to be relatively clear, respiration can be affected by various factors. For the purpose of this experiment, a term that will be used often is ventilation. This is normally expressed as an amount of time. For example, minute ventilation is the amount of gas moved in and out of the lungs in one minute and is well controlled in a normal resting individual. Now that there is an understanding of the major elements in respiration, there are three parts of the experiment that test different mechanisms. The first deals with measuring static lung volume by measuring four different volumes of air. There is a subject’s tidal volume (normal 3 volume of entering and exiting air), the inspiratory reserve volume (additional volume above the tidal volume), the expiratory reserve volume (air forcefully expired), and the residual volume (the small amount of air left in the lungs). The vital capacity is the volume that best represents our breathing range, and is found by adding together the volumes mentioned above. The justification behind this portion is to determine which volumes exhibited large or small amounts and to examine the reasons for the differences. The second aspect of this experiment was to observe the differences between normal breathing, re-breathing, hyperventilation, and the effects of lung volume on respiration. These exercises were done to examine the effects of altered alveolar gases respiration. It was expected that hyperventilation would prove to be the best option to have a longer duration of breath-hold. To examine the effects of exercising causing an increase of respiration, the last part of the experiment dealt with exercise hyperpnea. These three tests together provide an overall understanding of the mechanics of the human respiratory system in regards to how it deals with carbon dioxide and additional environmental factors. Materials and Methods The tools and detailed procedures can all be found in the NPB 101L Physiology Lab Manual 2nd Edition written by Bautista & Krober. The instruments that were needed included the disposable cardboard mouthpieces, nose clip, spirometer, plastic bags, an exercise bicycle, and the BioPac system to use for analysis. In all three parts of the experiment, the subject had to wear a nose clip and breath into a disposable mouthpiece to capture the expelled air. Minute ventilation and alveolar ventilation were the first values calculated and recorded. The following values that were recorded were the percent of carbon dioxide before breath-hold, after breath hold, and how long the duration of the breath hold was. The duration of breath hold in normal expiration/inspiration and forced inhalation/exhalation was additionally recorded. It is important to note that in all aspects of the second part of this experiment, the subject was given a minimum of 2-3 minutes to recover between each breathing type. When using the exercise bike, the increased workload was recorded along with the carbon dioxide expired. The workload started at 0 pKa and increased by 0.5 every two minutes until a final workload of 2 pKa was reached. All the BioPac systems were calibrated prior to the beginning of testing and there were no experimental changes that differed from the lab manual. 4 Results Part 1. Measuring Static Lung Volumes To test static lung volume, the subject was required to use a nose clip and breath into a mouthpiece that was connected to a spirometry station and the BioPac system. The program was calibrated at the appropriate levels and the subject breathed normally and then had to inhale and exhale deeply. During this time, the subject appeared to be calm and collected to guarantee there was consistency in his normal breaths. As the data recorded, there was a large peak from the normal breath from the inhalation, along with a large drop from the exhalation. The inspiratory reserve volume (IRV) was calculated to be 1.62 L/min, the expiratory reserve volume (ERV) 3.33 L/min, the tidal volume (TV) was 0.32 L/min, and the vital capacity (VC) was -1.43 L/min. By using these values, the minute ventilation (VE) was analyzed to be 4.48 L/min. Since gas exchange occurs only across alveoli and not the dead-space volume of the upper airways, this amount needs to be removed in order to obtain the true value of alveolar ventilation. In order to determine the dead-space volume, it had to be extrapolated because the weight of the subject was not recorded. Instead, a weight of 165 lbs and height of 73 inches was used to do the calculations. The alveolar ventilation (VA) was found to be at a volume of 2.5 L/min. These values expressing the different static lung volumes can be seen in Table 1 and all calculations of these can be found in the Appendix. Table 1. Static Lung Volumes Volume (L/min) Inspiratory Reserve Volume (IRV) 1.62 Expiratory Reserve Volume ERV -3.33 Tidal Volume (TV) 0.32 Vital Capacity (VC) 4.48 Minute Ventilation (VE) 4.98 Alveolar Ventilation (VA) 2.5 L/min = Liters/minute Part 2. Effects of Inspired Gas Composition and Lung Volume on Respiration The results of this part of the experiment dealt with observing what happened to the arterial pressure of carbon dioxide in the lungs by breathing into a bag or by hyperventilation. One subject was used for the three different types of breathing conditions. The subject’s normal 5 breath was first conducted and the last 20-50% of their air expired was collected in a bag and contained 1.2% carbon dioxide. After a 56.5 second breath hold was done, the carbon dioxide percentage increased to 3.6%. The next condition, which was the re-breathing exercise, soon followed. After breathing in a bag for three minutes, the air in the bag had a measurement of 5.2% carbon dioxide. The subject then held their breath for 23.2 seconds, and the last 20-50% of their air expired contained 5.5% carbon dioxide. The hyperventilation test was the next to follow suit. The subject breathed deeply at their normal rate for four minutes and their percent carbon dioxide before the breath hold was 3.6%. The subject was able to hold their breath longer, and held it for 68.8 seconds and ended with have a carbon dioxide percentage of 2.7%. In table 2, these varying carbon dioxide percentages and their corresponding durations of breath-hold can be compared. Normal breathing had the largest increase in carbon dioxide and re-breathing had the smallest. In hyperventilation, carbon dioxide percentage decreased and had the longest duration of breath-hold. The relationship between ventilation type and breath hold can be seen in Figure 1, and another relationship between ventilation type and percent carbon dioxide is represented in Figure 2. Figure 2 clearly shows the dramatic rise of the percentage of carbon dioxide before and after breath-hold, along with the decrease in carbon dioxide from hyperventilation. After the subject was completely recovered from the two earlier challenges, the effects lung volume on respiration was then observed. Table 3 shows the length of a breath hold after four specific inhalations and exhalations. Each time the subject held their breath after a specific effect, there was always a two-minute recovery period. The subject breathed normally as a control for two minutes and held their breath after a normal inspiration for 51 seconds. The subject then held their breath for 43 seconds after a normal expiration, for 79 seconds after a forced inhalation, and for 32 seconds after a forced exhalation. Graph 3 shows this relationship of static lung volume to breath hold. Table 2. Percent Carbon Dioxide Before and After Breath Hold in Four Breathing Conditions: normal breathing, re-breathing, and hyperventilation. Condition % Carbon Dioxide % Carbon Dioxide Duration of BreathBefore Breath-Hold After Breath-Hold Hold (seconds) Normal Breathing 1.2% 3.6% 56.6 secs Re-Breathing 5.2% 5.5% 23.2 secs Hyperventilation 3.6% 2.7% 68.8 secs 6 Duration of Breath-­‐Hold (seconds) Table 3. Duration of Breath Hold After Four Effects of Lung Volume: normal expiration, normal inspiration, forced inhalation, and forced exhalation. Duration of Breath-Hold (seconds) Normal Expiration 43 secs Normal Inspiration 51 secs Forced Inhalation 79 secs Forced Exhalation 32 secs 68.8 70 60 56.5 50 40 30 23.2 20 10 0 Normal Breathing Re-­‐Breathing Hyerventalation Condition Figure 1. The relationship between ventilation conditions (normal, re-breathing, and hyperventilation) versus the duration of breath-hold. Between each condition there was a threeminute rest period. 7 6 5.2 5.5 % Carbon Dioxide 5 4 3.6 3.6 2.7 3 % Carbon Dioxide Before Breath-­‐Hold % Carbon Dioxide After Breath-­‐Hold 2 1.2 1 0 Normal Breathing Re-­‐Breathing Hyerventalation Condition Figure 2. The relationship between three ventilation conditions (normal, re-breathing, and hyperventilation) versus percent carbon dioxide before and after breath-hold. There is an increase of carbon dioxide percentage after normal breathing, and a decrease in carbon dioxide percentage after hyperventilation. Re-breathing had a relatively constant percentage of carbon dioxide. Part 3. Exercise Hyperpnea The final aspect of this lab was to observe how exercise and the anticipation of it influences respiration. At the beginning, the subject on the exercise bike did not breath heavily and seemed to be relatively relaxed. As the workload increased, the subject began to breath more forcefully and deeply. As seen in Table 4, and represented on Figure 3, in all ventilatory responses there was a positive correlation with increased workload. These ventilatory responses included tidal volume, respiratory rate, minute ventilation, percent-expired carbon dioxide, and minute carbon dioxide. In comparing these, the greatest change in response was in the minute ventilation. The minute ventilation at rest was 5.38 L/min, and increased to 32.48 L/min after a workload of 2 pKa. Another notable response was minute carbon dioxide. The subject at rest had a minute carbon dioxide reading of 0.36 L/min and amplified to 2.73 L/min after a workload of 2 pKa. The witnessed deep and faster breathing was also validated by the respiratory rate increasing with the workload. The nature of all the curves in Figure 3 displays a linear progression of change in response to workload. 8 Table 4. Ventilatory Responses from an Increase in Workload from Exercise. Workload increased in increments of 0.5 starting from 0 pKa and ending at 2.0 pKa. Respiratory responses include tidal volume (TV), respiratory rate (RR), minute ventilation (VE), percent-expired carbon dioxide (FECO2), and minute carbon dioxide. Workload TV (L/sec) RR VE (L/min) FECO2 (%) Minute CO2 (pKa) (Breaths/min) (L/min) Rest 0.38 14 5.38 6.6 % 0.36 0.0 0.50 24 11.95 6.8 % 0.81 0.5 0.61 20 12.1 6.9 % 0.84 1.0 0.69 20 13.76 7.0 % 0.96 1.5 0.85 26 22.2 7.7 % 1.71 2.0 1.16 28 32.48 8.4 % 2.73 L/sec = Liters/second; Breaths/min = Breaths/minute; L/min = Liters/minutes 35 Change in Response 30 25 TV (L/sec) 20 RR (breaths/min) 15 VE (L/min) 10 FE CO2 % Minute CO2 (L/min) 5 0 0 0.5 1 1.5 2 Workload pKa Figure 3. The Relationship between Ventilatory Responses versus Increase in Workload during Exercise. Workload increased in increments of 0.5 starting from 0 pKa and ending at 2.0 pKa. Respiratory responses include tidal volume (TV), respiratory rate (RR), minute ventilation (VE), percent-expired carbon dioxide (FECO2), and minute carbon dioxide. 9 Discussion There are several mechanisms that respond to various stimuli when placed on the lungs. The intent of this study was to isolate these specific stimuli and observe what relationships happen to these respiratory responses. We demonstrated the effects of static lung volumes, the different durations of breath-hold following normal breathing, re-breathing, and hypertension, as well as exercise hyperpnea. Before the data is analyzed, let’s first recap the events that happen in respiratory physiology. As stated previously, alveoli are the sites of gas exchange specifically in the Type I cells. The pressure between the alveoli and the atmosphere creates a gradient that provides the force to move air in and out. This process follows Boyle’s Law, which states that at constant temperature, pressure is inversely related to volume (Sherwood, 2013, pg. 463). So as pressure increases, volume decreases and vice versa. For the lungs, intra-pleural pressure is always below intra-alveolar pressure, so the gradient always exists. If the intra-alveolar pressure is less than atmospheric pressure, air will go into the lungs. If this pressure is greater than atmospheric pressure then air will exit the lungs. The first portion of this experiment dealt with the various volumes that the lungs can hold. The subject was a male who was roughly 165 lbs and 73 inches. The calculated vital capacity was 4.48 liters. The tidal volume was at a normal level of 0.32 liters. When comparing the IRV and ERV, the ERV resulted in a larger volume ejected. This could be because if there were more force exhibited to remove air, the air that would normally stay in the dead space would also become expelled. Conversely, inhaling air above the tidal volume is more difficult because there is already air that remains in the lungs. In another study focused on lung volume, the body provides mechanisms to prevent over inflation (Albaiceta et al., 2008). This could be another reason to why in this experiment exhalation had a larger volume than inhalation. However, this is not to say that someone can fully deflate his or her lungs. The principle reason to why we can never completely deflate our lungs is that otherwise the lungs would collapse. Continuing onto the next portion of the experiment, this dealt with the aspects of the interactions of carbon dioxide and the duration of a breath-hold. The two key regulators in noticing changes in pressure are the central and peripheral chemoreceptors. The central chemoreceptors input into the respiratory control centers and are the major driver in ventilation rate. More specifically, they respond to changes in partial pressures of carbon dioxide. Peripheral 10 chemoreceptors are a last resort to maintain breathing, they respond when the partial pressure of oxygen falls below normal levels (60 mmHg). During normal breathing, an increase of carbon dioxide was seen after the subject held their breath for around 56 seconds. The amount of carbon dioxide actually doubled from the start of the hold to the end. Hypoventilation, or re-breathing, is breathing too slowly. The partial pressure of carbon dioxide increases to above normal and the partial pressure of oxygen decreases below normal. The results showed that the amount of carbon dioxide relatively stayed the same; it just had a minor increase. There was 5.12 % of carbon dioxide at the beginning of the breath hold, and 5.5 % carbon dioxide at the end. However, it is important to mention that the duration of the breath-hold was dramatically shorter than in normal breathing, it was 23 seconds. Even though the amount of carbon dioxide didn’t largely increase, it still was higher in levels than oxygen, thus shorting the ability to hold breath for longer. The same result is found in a study about hypoventilation and also used a bag to breath in from. It was found that when a subject was rebreathing their same air, carbon dioxide accumulated and eventually increased its overall pressure (Domnik et al., 2013, pg. 361-369). On the contrary, hyperventilation is breathing too quickly. This is when the partial pressure of carbon dioxide decreases to below normal and the partial pressure of oxygen increases to slightly above normal. It was hypothesized that this condition would allow the subject to hold their breath for longer – and it did. The subject was able to hold their breath for about 69 seconds, which is more than the normal breathing and almost triple the time than that of hypoventilation. The second aspect of this part of the experiment involved the effects of lung volume on the duration of breath-hold instead of carbon dioxide. Expiration and inspiration were the two conditions that were tested. Inspiration is the act of breathing in, and is always an active process. The diaphragm contracts and pulls down to increase vertical length or thoracic activity. The external intercostal muscles elevate the ribcage and increase horizontal volume of thoracic activity. Expiration is breathing out, and is a passive process. It is normally due to the elastic recoil of the diaphragm and the relaxation of the intercostal muscles. The results showed that forced exhalation had the shortest breath-hold at 32 seconds, then normal expiration at 43 seconds, followed by normal inspiration at 51 seconds, and finally forced inhalation being the longest at 79 seconds. Since forced inhalation is largely an active process, there was an ample amount of oxygen to prolong the breath-hold, so these results were expected. 11 Exercise hyperpnea was the last item to be investigated in the experiment. Hyperpnea is the increase in ventilation that corresponds to an increase in metabolic activity. Typically in the event of hyperpnea, it will occur in two phases. The first phase involves a rapid ventilation increase in response to exercise. The second is when the exercise is maintained at a certain level, the increases become slower. Overall, the ventilation rate matches the demand for carbon dioxide removal, and there isn’t a decrease in carbon dioxide pressure. Our results indicate that all ventilatory responses as mentioned in Table 4 showed to increase in regard to an increase of workload. However, this does not fall in line with the typical ventilatory response during exercise. FECO2 should have remained constant, but our data indicates a steady linear increase as seen in Figure 3. Another trend that is seen is the Herring Breuer reflex. In the event that the lungs will try to expand more during exercise, the Herring-Breuer reflex is initiated. This is a reflex that is enlisted to prevent the over-stretching of the lungs. The reflex is caused when pulmonary stretch receptors indicate that an over inflation is occurring. In this lab, the tidal volume is increasing, but not that much. The workload was getting intensely higher however the normal volume of breathing in and out stayed relatively the same. Another crucial thing to mention is that there was a steady increase of minute carbon dioxide. This is because exercise increases the demand for oxygen and produces more carbon dioxide as a consequence. Carbon dioxide will actually become more prevalent in the blood in order for more oxygen to be able to go directly to the tissues. The results of the minute ventilation showed that it increased with workload, and it was similar to another study examining the effects of hyperpnea. This study, which intended to mimic hyperpnea, found that with exercise, minute ventilation increased in a linear fashion (Dominelli et al., 2014, pg. 15-23), which can be also explicitly seen in the observed data from our experiment and represented in Figure 3. Overall, this last portion of the experiment shows how with vigorous exercise, total carbon dioxide pressures increase along with respiratory rate in order to try to create more oxygen available throughout the body compared to that of a body at rest. Beyond the scope of this experiment there are a couple of outstanding questions that should be addressed. One deals with the most efficient way to increase alveolar ventilation. The best mechanism would be to increase the tidal volume since this would reduce the proportion of each breath occupied by anatomical dead space. Another way that it could be increased is by 12 raising the respiratory rate. Based on the trends in Table 4, our results show that with in increase of respiratory rate there was an increase in alveolar ventilation. Another thing to indicate is the potential errors that could have made an impact on the data. A major error was that the height and weight of the subject was never recorded so both of these numbers were based off of pure observation. Due to this approximation, it could explain the reason why in Table 1 the vital capacity is larger than the minute ventilation. The vital capacity in theory should be larger since it is the normal breathing range. The equation to determine vital capacity involved both the height and weight, two values that were never recorded, thus resulting in error. A last error, which could be negligible, is that the subject on the bike dropped the mouthpiece at once point and caused the data to be skewed for about ten seconds. However, other than these error mentioned above, the other values that were recorded were on track. The experiments in this study allowed for the investigation of the human respiratory system. Expiratory reserve volume proved to encompass a greater volume than the inspiratory reserve volume. This is what was hypothesized since the act of exhalation is a passive process that allows the muscles to relax to resting position instead of the being forced to expand in the case of inhalation. In the breathing exercises, hyperventilation was thought to allow for the pressure of oxygen to increase and for the percentage of carbon dioxide to decrease. This proved to be true and can be viewed in the numerical decrease of carbon dioxide along with the increase duration of breath-hold. During exercise, an increase in workload caused an increase of ventilatory responses, all of which were mentioned above. Minute ventilation had the most significant increase as expected since it is directly proportional to the amount of oxygen and carbon dioxide consumed. Further studies examining the potential effects of long term endurance athletes and their minute ventilation could be done since it is common for these types of people to exhibit a lower minute ventilation in response to strenuous activity. Although the act of breathing goes unnoticed, it is proven to be a complex system that has specific responses geared for changes in pressures, pH, and workload. All of which aid humans in various activities such as exercise, blowing out candles on a cake, or just having the ability to take a breather at the end of the day. 13 References Albaiceta, G., Blanch, L., & Lucangelo, U. (2008). Static pressure–volume curves of the respiratory system: Were they just a passing fad? Current Opinion in Critical Care, 80-86. Bautista, E., & Korber, J. (2009). The Human Respiratory System. In NPB 101L: Physiology Lab Manual (2nd ed.). Ohio: Cengage Learning. Dominelli, P., Render, J., Molgat-Seon, Y., Foster, G., & Sheel, A. (2014). Precise mimicking of exercise hyperpnea to investigate the oxygen cost of breathing. Respiratory Physiology & Neurobiology, 201, 15-23. Domnik, N., Turcotte, S., Yuen, N., Iscoe, S., & Fisher, J. (2013). CO2 rebreathing: An undergraduate laboratory to study the chemical control of breathing. AJP: Advances in Physiology Education, 361-369. Douglas, C. G., & Haldane, J. S. (1909). The regulation of normal breathing.The Journal of physiology, 38(5), 420-440. Sherwood, L. (2013). The Respiratory System. In Human physiology: From cells to systems(8th ed.). Pacific Grove, Calif.: Brooks/Cole. Appendix Normal Breathing: Inhale/Exhale Normal Breathing, Re-Breathing, Hyperventilation Exercise Hyperpnea Sample Calculations: Minute Ventilation VE = TV x RR = 0.32 L x 15.57 breaths/min = 4.98 L/min 14 Alveolar Ventilation VDS = DS x RR = 165 x 15.57 breaths/min = 2475 mL 15 VA = VE – VDS = 4.98 L/min – 2475 mL = 4980 mL/min – 2475 mL = 2505 mL/min = 2.5 L/min Minute CO2 Minute CO2 = VE x average end tidal CO2 = 5.38 L/min x 6.6 % = 0.36 L/min Respiratory Rate RR = # breaths in 30 seconds x 2 = 7 breaths/30 sec x 2 = 14 breaths/min