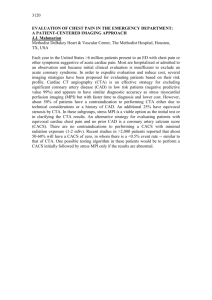
CT Protocol Booklet - Cardio Gallery Home Page
advertisement

Table of Contents
CTA Exams
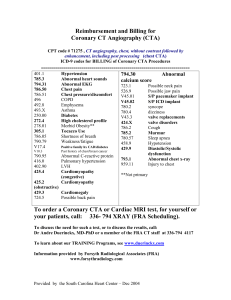
Coronary CT Angiography
Coronary CTA Code(s)
Cardiac Scoring
Coronary Calcium Scoring and Medical Waiver
Advanced Beneficiary Notice
Body Weight Chart
New Pricing Structure for CT Calcium Scoring
CTA Carotids/Vertebrals
CTA Thoracic Aorta
CTA Chest (Ascending Aorta)
CTA Abdomen Aorta (renals, mesentery, SMA)
CTA Aorta Iliofemoral Run Off
CTA Thoracic-Abd. Aorta, Iliofemoral Run Off
CT Venography: Upper Extremity
CT Venography: Lower Ext. for Vein Mapping
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
Routine Exams
Brain
Internal Auditory Canals/ Facial Bones, Sinuses, Orbits
Sella Tursica/ Pituitary and Temporal Bones
Neck – Soft Tissue
(Routine non-vascular) Chest
Sternum
Chest for Pulmonary Embolus
Chest for Pulmonary Vein Stenosis
Thoracic Outlet (CTA of the Chest)
Cervical Spine
Thoracic Spine
Lumbar Spine
Routine Abdomen/Pelvis
Routine Pelvis
Upper Extremity
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
Forms
CT Flow Chart for Abnormal Findings
31
CT Ordering Criteria
32
Contrast and Renal Insufficiency Issues
33
Policy: Request for CT exams from patients and outside physician offices 34
CT Scan Suite and equipment
35
CT Meds
36
Toshiba CT Scanner Information
37
Vital Imaging (Vitrea 3D Workstation)
38
Medical Metrx Systems (MMS)
39
Step by Step Process of MMS
40
Medical Management of Severe Anaphylactoid & Anaphylactic Reactions 41
CT Ordering Form (Front)
42
CT Ordering Form (back)
CT Scan Superbill
Contrast CT Exams Policy
43
44
45
Case Studies
Case Study I
Case Study II
Case Study III
Case Study IV
46
47
48
49
Anatomy
Neck
Coronary
Upper body
Coronary Blood Flow
COW anatomy
Thorax venous
Extremities
Aorta peripheral arteries
Pelvis
Pelvis 2
Lower extremities
Lower extremities 2
50
51
52
53
54
55
56
57
58
59
60
61
Policy and Procedure Updates
Radiologist Overreads of Vascular CT Angio Scans
CTA Protocol Change Memo
CTA Renal Memo
CT of the Chest Memo
62
63
64
65
Contact Information
IP Addresses
CT Contact Information
66
67
Coronary CT Angiography
0147T: Coronary CTA with Calcium Scoring
done with Isovue 370 - contrast (110cc’s)
Give Test dose: 20cc’s of contrast prior to actual scan
0146T: Coronary CTA without Calcium Scoring {Post CABG} (contrast increased to 125cc’s)
Two Reports: Radiology (for post CABG pt’s only-mediastinum images are sent) and Cardiology.
Two reports: a vascular report (consisting of a Calcium Score computer generated report and a coronaryCTA (For
CABG pt.’s-inject in Right Arm)
Protocol
Calcium Scoring first
Image Xact technique
Coronary CTA Candidacy & Requirements:
Target Heart rate-55BPM or under
BMI (Body Mass Index)=36 or lower
Vein access Adequacy
Pacemakers allowed if anatomy specifiedsuboptimal results possible
No Bi-V or ICD
No patients with A-Fib
Calcium Score above 500
Give Lopressor routinely
Consider 100 mg the night before and/or
100mg one prior to exam
(inappropriate patients such
as patients with already low blood pressures
should be assessed differently)
Give two squirts of nitroglyerine under
tongue prior to exam (3-4 minutes)(instruct
the pt. not to take Viagra, Cialis, Levitra,
etc.)
Only consider to give IV betablocker
(lopressor) if heart rate is between 65-70.
You may have to give more than the standard
15mg dose used for acute MI protocol to
decrease the heart rate.
Recommend patient has a family member to
drive the patient home due to the affects of
beta blockers such as dizziness and faint may
have on the patient.
Recommend Anxiolytics such as Xanax
.25mg 1 hour
prior (enforce patients who are already on
Anxiolytics to especially continue their
medication for coronary CTA)
HBOC Sched.: CT8
Medicare Indications:
•
Emergency evaluation of acute chest pain syndrome for
coronary etiology, including emergency evaluation,
pulmonary embolism, aortic dissection, and coronary
artery disease
•
Cardiac evaluation of a patient with chest pain syndrome
(e.g. angina equivalent, angina) who is not a candidate for
catheterization
•
Management of a symptomatic patient with known
coronary artery disease (e.g., post stent, post CABG)
when the results of the MDCT may guide the decision for
repeat invasive intervention
•
Assessment of suspected congenital anomalies of
coronary circulation or great vessels
•
Assessment of coronary Veins prior to biventricular
pacing lead placement
IV Beta-Blockers:
IV Beta Blocker to be given with
heart rates above 55 BPM (Max.
50mg) (Blood Pressure
dependent)
Scan will be performed if heart
rate is below 65 after IV betablocker is given.
Above 65 BPM, the exam will
not be performed.
If BP is < 100 Systolic, do not
give IV beta blocker
Notes: Also use Coronary CTA brochure to give to
patient.
1
Coronary CTA Code(s):
0146T-CT Angiography of coronary arteries (including native and
anomalous coronary arteries, coronary by-pass grafts), without
quantitative coronary calcium
0147T-CCTA with quantitative evaluation of coronary calcium
0148T-Cardiac structure & morphology and CCTA without
quantitative evaluation of coronary calcium
0149T- Cardiac structure & morphology and CCTA with quantitative
evaluation of coronary calcium
0144T-CT, heart, without contrast material, including image postprocessing & quantitative evaluation of coronary calcium
0145T- CT, heart, without contrast material, followed by contrast
material(s) & further sections including cardiac gating and 3D image
post processing, cardiac structure and morphology
0150T- cardiac structure and morphology in congenital heart disease.
0151T- CT, heart, without contrast material, followed by contrast
material(s) & further sections including cardiac gating and 3D image
post processing, cardiac structure and morphology function evaluation
(L & R ventricular function, ejection fraction, & segmental wall
motion)
2
Cardiac Scoring
Code: 0144TS (use this code for self pay patients)($150)(Screening)
Code: 0144T (Non-Screening)(pt. must be symptomatic) (use coronary
Use Waiver when necessary
Note: CT of the Chest(s) is bundled with 0144T
CTA indications)
Who should have one?
Male over 45 years old
Female & over 55 years of age
Or passed menopause or had ovaries removed and is
not taking estrogen
Father or brother had a heart attack before age 55 or
mother or sister had an heart attack at age 65
Smoker or live/work around someone who does
Cholesterol level of 240 mg/dl or higher
High Blood Pressure
Does not exercise on a regular basis for at least 30
minutes
20lbs overweight
Diabetes or medicine to control diabetes
2 or more of these indications qualifies for a CACS.
Calcium Score Guidelines:
Without contrast
This is a computer generated report that must be
signed by a certified Coronary CT physician. On
the back, there is a place where the physician
signs off on the report
There will be only one report (by a CIS
physician) that is qualified to read coronary CT
exams; no Radiologist over read
Calcium Score---Plaque Burden---Probability of Significant
CAD--- Implications for future risk (MI, unstable angina)--Recommendations
0 ---No identifiable (calcified) plaque---Very low,
generally less than 5%---Very Low---Reassure patient.
Discuss general public health guidelines for primary
prevention of CV disease.
A calcium Score is always performed prior to a
Coronary CTA
1-10---Minimal identifiable plaque burden---Very
unlikely, less than 10%---Low---Discuss general public
health guidelines for primary prevention of CV diseases
The following guiding principles should be used in
interpreting a patient's score: The presence of any
detectable coronary calcium implies the presence of
coronary artery disease. This can affect patient
management by providing impetus for more aggressive
hypertension control, lipid lowering, and low-dose
aspirin therapy. Investigators have also noted that
patients, when informed of their score, or shown actual
images, have displayed much more willingness to
undertake healthy lifestyle changes. Since patients with
very high scores (e.g., over 400) have a high likelihood
of harboring a significant stenosis, they should
probably undergo stress testing to evaluate for
inducible ischemia. Patients with intermediate scores
may require further testing based upon other factors
(age, other risk factors, etc). In an asymptomatic
patient, a score of zero would imply no need for further
imaging tests for coronary disease.
11-100 ---Definite, at least mild plaque burden---Mild or
minimal coronary stenoses likely---Moderate---Counsel
about risk factor modification, strict adherence
with&Mac240;primary prevention goals. Daily ASA.
101-400 ---Definite, at least moderate plaque burden--Non-obstructive CAD highly likely, although obstructive
disease possible---Moderately High---Institute risk factor
modification and secondary prevention goals. Consider
exercise testing for further risk stratification. Daily ASA
>400&Mac240;---Extensive plaque burden---High
likelihood (>90%) of at least one significant coronary
stenosis---High---Institute very aggressive risk factor
modification. Consider exercise for pharmacologic
nuclear stress testing to evaluate for inducible ischemia.
Daily ASA.
3
4
Patient’s Name:
Medicare # (HICN):
ADVANCE BENEFICIARY NOTICE (ABN)
NOTE: You need to make a choice about receiving these health care items or services.
We expect that Medicare will not pay for the items(s) or service(s) that are described below. Medicare does not pay for all of your
health care costs. Medicare only pays for covered items and services when Medicare rules are met. The fact that Medicare may not
pay for a particular item or service does not mean that you should not receive it. There may be a good reason your doctor
recommended it. Right now, in your case, Medicare probably will not pay for item(s) or service(s) indicated below for the
following reasons:
Items or Services:
Because:
MEDICARE does not pay for this service for your condition.
MEDICARE does not pay for these tests as often as this (denied as too frequent).
MEDICARE does not pay for experimental or research use tests.
The purpose of this form is to help you make an informed choice about whether or not you want to receive these item(s) or
service(s), knowing that you might have to pay for them yourself. Before you make a decision about your options, you should read
this entire notice carefully.
Ask us to explain, if you don’t understand why Medicare probably won’t pay.
Ask us how much these laboratory tests will cost you (Estimated Cost: $________________),
in case you have to pay for them yourself or through other insurance.
PLEASE CHOOSE ONE OPTION. CHECK ONE BOX. SIGN & DATE YOUR CHOICE.
Option 1. YES. I want to receive these laboratory item(s) or service(s).
I understand that Medicare will not decide whether to pay unless I receive these item(s) or service(s). Please submit my
claim to Medicare. I understand that you may bill me for item(s) or service(s) and that I may have to pay the bill while
Medicare is making its decision. If Medicare does pay, you will refund to me any payments I made to you that are due to
me. If Medicare denies payment, I agree to be personally and fully responsible for payment. That is, I will pay personally,
either out of pocket or through any other insurance that I have. I understand I can appeal Medicare’s decision.
Option 2. NO. I have decided not to receive these item(s) or service(s).
I will not receive these item(s) or service(s). I understand that you will not be able to submit a claim to Medicare and that I
will not be able to appeal your opinion that Medicare won’t pay.
____________
Date
____________________________________________
Signature of patient or person acting on patient’s behalf
NOTE: Your health information will be kept confidential. Any information that we collect about you on this form will be
kept confidential in our offices. If a claim is submitted to Medicare, your health information on this form may be shared with
Medicare. Your health information which Medicare sees will be kept confidential by Medicare.
OMB Approval No. 0938-0566
Form No. CMS-R-131-G (June 2002)
5
6
Memorandum
DATE:
August 17, 2006
TO:
All Office Team Leaders
RE:
New Pricing Structure for CT Calcium Scoring
On Monday, August 21, the pricing structure on CT calcium scoring procedures will increase from $75 to
$150.
It is imperative that the determination is made as to whether the patient meets the indications for CMS
reimbursement versus a true screening. It will be the responsibility of the nurses to work with the physicians
and make this determination.
If the patient meets the indications for a calcium score, then they may be processed as any
other diagnostic study would be processed.
If the patient does not meet the indications for the calcium score procedure, then the
procedure is considered screening.
o All screening patients will need to sign an advanced beneficiary notice (ABN) prior to
having the exam performed and any fees collected.
o All screening patients will be required to pay the $150 fee at the time of service.
Thanks in advance for your assistance
7
CTA Carotids/Vertebrals
Code: 70498
With contrast
(2 reports: a vascular and a non-vascular radiology overread report)
HBOC Sched.: CT7
Perform a CT Angio of the carotids/vertebrals
Post portal CT of the neck afterwards
60cc’s of contrast {Isovue 370
5cc’s per second
Surestart aorta arch (180 hu)
Indications:
Scanned the same way for
subclavian –axilla evaluation
Bruit
Syncope
Dizziness
Vertigo
Abnormal US
Planning for CEA
Diplopia
Visual disturbance
Ataxia
8
CTA Thoracic Aorta
Not for Ascending Aorta aneurysm
HBOC Sched.: CT7
Code: 71275, 72191, 74175 {CT11}
(CTA of the Chest)
100cc’s of Isovue 370
With contrast
3cc’s per second
May have 2 reports: vascular / (non-vascular-includes lungs, mediastinum, abdomen/pelvis)
(Radiologist Overread annually-for follow up or first CTA scan or previous pathology)
Surestart Aorta Arch (180hu)
Perform CT Angio of the chest by beginning above the aorta arch and ending the scan below the bifurcation of the
internal and external iliac bifurcations
Perform post portal Abdomen-Pelvis with contrast after CTA
\
Indications:
TAA
AAA
Dissection
Atypical chest pain
Coarctation of the Aorta
Truncus arteriosis
Persistant L Superior Vena Cava
Interrupted Inferior Vena Cava
Suspected Pulmonary Embolism
9
CTA Chest (Ascending Aorta)
HBOC: Sched.: CT8
Code: 71275 (CTA of the Chest)
With contrast
Not Thoracic Aorta through bilat.
internal-external iliac bifircation
100cc’s of Isovue 370
3cc’s per second
Surestart Aorta Arch (180hu)
This is exam is performed similar to Coronary CTA. The heart is gated to eliminate the motion of the ascending
aorta. The exam ends through the adrenal glands.
Beta-blockers can be used to lower the heart rate.
Motion artifact below non-gated
Gated to eliminate motion artifact
Indications:
Ascending Aorta Aneurysm
Truncus Arteriosis
Coarctation of the Ascending Aorta
Double Aorta Arch
Right Sided Aorta Arch
10
CTA Abdomen Aorta
(renals, mesentery, SMA)
Code: 72191 & 74175 (CT8)
with contrast
May have 2 reports (a vascular and a non vascular report)
(Radiologist Overread annually-for follow up or first CTA scan or pervious pathology)
3cc’s per sec.-100cc’s Isovue 370
HBOC Scheduling: CT7
Perform CTA of the Aorta (Abd./Pelvis)…begin above diaphragm and end through internal and external iliacs
(Small slice thickness (.5mm) may be sent to M2S (formerly Medical Metrx Systems) (use code: G0288)
Indications:
Aorta aneurysm and dissection
Suspected renal artery stenosis
Investigating potential kidney donors
Mesenteric ischemia
Renal and/or splenic artery aneurysm
Visceral artery aneurysm
Prior to and following liver transplanatation
11
CTA Aorta Iliofemoral Run Off
Code: 75635 with contrast
scan begins above diaphragm, and ends through the feet
HBOC Sched.: CT7
(125cc’s Isovue 370)
Also known as “CTA Lower Extremity”
Perform CTA Aorta with Run Off
May have 2 reports: (a vascular and a non vascular report)
(Radiologist Overread annually-for follow up or first CTA
scan or pervious pathology)
Indications:
AAA
PVD & Claudication
Abnormal ABI
Lower extremity pain, numbness, weakness
Stent patentcy (SFA, Iliac)
Popliteal aneurysm
Pre op & post op for Lower Ext. Grafts
Iliac AAA aneurysm(s)
12
CTA Thoracic – Abd. Aorta
Iliofemoral Run Off
To evaluate axillary-bifemoral bypass grafts
Code: 71275 & 75635
with contrast
scan begins above apex of the chest above graft insertion , and ends through the feet
HBOC Sched.: CT7
(125cc’s Isovue 370)
May have 2 reports:
(vascular & non vascular-Radiologist Over read
{Not in Lafayette})
(Radiologist Overread annually-for follow up or first
CTA scan or previous pathology)
Indications:
To evaluate axillary-bifemoral bypass grafts
AAA
PVD & Claudication
Lower extremity pain, numbness, weakness
Stent patentcy (SFA, Iliac)
Popliteal aneurysm
Pre op & post op for Lower Ext. Grafts
Iliac AAA aneurysm(s)
13
CT Venography:
Code: 73201
Upper Extremity
with contrast
Notes:
This exam requires a hand injection
100cc’s of contrast used (Isovue 370)
Indications:
Upper ext. swelling-pain
Shunt evaluation
Demonstrates Axilla-subclavian-ulnar
Power Inject all Venography exams
Note for Lafayette Patients:
The Radiologist
will read both the
14
CT Venography:
Lower Ext. for Vein Mapping
HBOC Sched.: CT7
Code: CT10=72193, 73701, 74160
with contrast
one report: from Radiologist only
(includes Abdomen/Pelvis-above diaphragm as well as lower extremity) not for DVT
Notes:
This exam requires a foot injection
“Vein clinic” protocol
125cc’s of contrast used (Isovue 370)
no more than 2cc’s per sec.
specify for “Vein Mapping”
Use power injection on all Venography exams
It is important to specify or mention “vein
mapping”
15
Brain
Indications for Non CTA-Non Vascular-routine:
without contrast (5 min.exam)vs. with and without contrast (10 min exam)
Without contrast Code: 70450
Radiologist Report Only
With & Without Contrast Code: 70470
Radiologist Report Only
Trauma
memory loss
Headache
confusion
Subdural Hematoma
dizziness/vertigo
Post OP {if surgery is for tumor}
mental status change
st
Acute CVA {1 2 days following onset of symptoms}
R/O hemorrhage
weakness
Follow up atrophy
decreased LOC
Hydrocephalus
aphasia
VP Shunt
Psychiatric work up
Seizure
Non-specific complaints
Dementia and Alzheimer’s
CVA symptoms (such as ext. numbness-weakness, dysathria, etc.)
Syncope-Syncopal Episodes
Facial numbness/drooping
Note(s):
100 cc’s of Isovue 370@ 1cc/sec
Aneurysm/AVM
Multiple Sclerosis
For Tumor and to (R/O mets)-hx of Cancer
1st time seizure work up (excluding febrile symptoms)
Inflammatory conditions (meningitis, abscess)
Posterior Fossa/Brain Stem/CP Angle tumor
Whenever another CT exam with contrast
is performed.
Consider MRI whenever contrast needs to be given for CT Brain
Never perform a CT of the Brain with contrast only. Always order with and without contrast.
Neurologists orders a CTA Brain And a MRI of the brain as a Protocol to evaluate the brain.
CT of Brain and Posterior Fossa are the same order. The Posterior Fossa is always included in the scan.
FYI: 5mm slice thickness through brain and posterior fossa.
CTA Brain-Circle of Willis (Cerebral Vessels)
Code: 70496
Radiologist Report Only..The CTA portion will be included in this report also
A Carotid CTA can be performed also with this exam on the same day at the same time.
..includes:
HBOC Sched.: CT7
100cc’s of Isovue 370
injection rate: 5cc’s per sec.
Head without contrast performed first (5mm slice thickness)
CTA of Brain performed second (.5mm slice thickness)
Post CTA Brain (Head with cont.) third (5mm slice thickness)
Post processing of .5mm slice thickness images=3D images (MIPs only), axial and coronal MIPS
Attn: Vertebral –Basilar system:
Imbalance, unsteady gait, dizziness, nausea & vomiting
Headaches with family history of berry aneurysm
Chronic persistant Migrane work up
Clinical signs of Brainstem/Cerebellar pathology
Subarachnoid Hemorrhage with mass
Eye Pain (retroorbital)
Droopy eyelid
Hoerner’s Syndrome > (scan from arch upward through head)
Blurred Vision
Cavernous sinus (CC fistula)
Empty Sella Syndrome: Presenting symptoms tend to non-specific - frequent headache and transient visual problems. Endocrine disturbance is unusual but when present, includes
amenorrhoea in one - third of cases, usually due to hypogonadotropism. However, many patients enjoy normal pituitary function.. There is a risk that aneurysms may develop within the
dilated sella which should be examined for by angiography.
16
Internal Auditory Canals
Note: To image the IAC’s, an MRI exam is superior to CT.
Recommend MRI of IAC’s
Radiologist Report Only; Non-Vascular-Non CTA exam
Code: 70482
Protocol:
1st :Head without contrast (5mm slice thickness)
2nd: Temporal bones (.5mm slice thickness) W & WO contrast (100cc’s
3rd: Head with contrast (5mm slice thickness)
of Isovue 370)
Indications are same as Temporal bones
Facial Bones, Sinuses, Orbits
Note: The patient is scanned in the supine position.
The images are post processed on the Vitrea 3D workstation where
Coronal, sagittal, and 3D images (if needed) are created. (Code 76377 can be used when the 3D workstation is utilized
for this exam.)
Radiologist Report Only-Non-Vascular-Non CTA exam
With Contrast
Without Contrast
100cc’s of Isovue 370
Code 70486
Code: 70487
Trauma
Facial Bone(s)
abnormality
Facial pain and or
pressure,
tenderness
Orbital
osteoporosis
Pertaining to bone
Sinuses-sinusitis
Malignancy
Retinal detachment with defect
Retinoschisis & retinal cysts
External ophthalmoplegia
Disorder of optic chiasm associated
with vascular disorders
Disorder of visual pathways
associated with vascular disorders
Orbital cellulitis
Swelling or mass of eye
Orbital cyst(s)
Exophthalmia
Other otitis externa
Any disorder-symptom(s) pertaining
to optic nerve
17
Sella Tursica / Pituitary
Note: To image the Sella Tursica, an MRI exam is superior to CT.
Recommend: MRI of Sella Tursica with Gadolinium
Code: 70482
Radiology Report Only; Non-Vascular-Non-CTA
Protocol:
1st-Head without contrast
2nd-Sella Tursica with contrast
3rd rescan head after injection of contrast for Sella
Pituitary Adenoma/Tumor
Lactating Breast
Cushing’s disease
Temporal Bones
Code: 70480
Note: CT exam is done without IV contrast
(Attn. To bone detail)
Radiology Report Only; Non-Vascular-Non-CTA
Tinnitis
Cholesteatoma
Any disorder of labyrinth
Unspecified vertiginous syndromes and labyrinth disorders
Otosclerosis
Labyrinth dysfunction
Labyrinthine dysfunction
Labyrinthine fistula
Labyrinthitis
Osteopetrosis
Osteogenesis imperfecta
Anomalies of ear causing hearing impairment
Osteitis deformans without mention of bone
Polyostotic fibrous dysplasia of bone
For Acoustic neuroma:
Do With contrast
(MRI is best modality
for this indication)
18
Neck – Soft Tissue
Code: 70491
Not Cervical spine
Note: Should ALWAYS BE DONE WITH CONTRAST
Contrast used: 80cc’s of Isovue 370; 2cc’s per second
Radiology Report Only; Non-Vascular-Non-CTA
Palpable neck mass-nodule
Lymphoma
Abscess-infection
Lymphadenitis
Malignancy
Evaluate tongue, mouth, mandibular abnormalities, disorder
Nasopharnyx evaluation
Salivary gland(s)
Lipoma
Oral Cavity
Larynx, pharynx mass, abnormality, disease, evaluation
Persistent hoarseness
Peritonsillar abscess
Hypertrophy of adenoids
Acute pulmonary manifestations due to radiation
Vocal cord paralysis
Anomalies of larynx, trahea, and bronchus
Larynx/trachea fracture
Acute periodontitus
Soft tissue pain, discomfort, tenderness-localized
Persistant dysphagia with pain/discomfort
Cyst vs. mass of larynx-pharynx
Lymphangioma , any site
Cyst(s)
Submandibular nodule-mass
Enlargement of parotid(s)
Cellulitis
Persistant dysphagia
Note: this CT exam is performed each time (post portal) whenever a Carotid CTA is performed but it
is not billed.
19
(Routine-non vascular)
Chest
Without Contrast
{esopho-cat eaten to visualized the
esophagus)
Code: 71250
Hemoptysis
Lung mass
Persistant cough
SOB
Pneumonia & F/U
Pleural effusion
Atypical chest pain
Lung CA
Granuloma evaluation
Enlarged mediastinum
Post op-CABGcomplications-infectionabscess
Metastatic disease
Trauma
Turberculosis
Cystic Fibrosis
Myocardial degeneration
Asthma
Pleurisy
Empyema
Pneumothorax
Esophagus evaluationstricture-stenosisesophagitis
Diaphragm
Dyspnea & respiratory
abnormalities
If severe allergy to dye
Follow up of pleural
effusion if neoplasm is
ruled out
Follow fibrosis only
To evaluate sternum-post
op-painful-esp when
moving-tenderness
HBOC Sched.: CT3 (15min. duration)
Sternum
With contrast (CTA)
{esopho-cat eaten to visualized the esophagus}
100cc’s of Isovue 370 @ 3cc’s
per second
Code: 71275
For widening-enlarged mediastinum
Radiologist Report Only; Non-Vascular-Non CTA
CT Sternum is a CT Chest Without cont.
(71250)
Patient lies flat on back (supine) with arms above
head; the patient advances feet first into the gantry
20
Without contrast
Sternum
Code: 71250 (Chest without contrast)
Costochondritis (Tietze’s syndrome)
post op CABG pain and tenderness
sternal separation
trauma
sternal fracture(s)
retrosternal Hematoma (may want to order routine CT of the Chest with contrast)
Technical Factors: small slice thickness (1-2mm) bone and soft tissue algorithum (helical scan)
3D imaging can be helpful as well as sagittal and curved coronal reformations
21
Chest for Pulmonary Embolus
Code: 71275
Note: done with IV contrast and Esopho-cat
75cc’s of Isovue 370 @ 4cc’s per sec.
Venous thrombo-embolism; Lung blood clot; Blood clot - lung; Embolus; Tumor embolus; Pulmonary emboli are most often caused
by blood clots in the veins, especially veins in the legs or in the pelvis (hips). More rarely, air bubbles, fat droplets,
amniotic fluid, or clumps of parasites or tumor cells may obstruct the pulmonary vessels. The most common cause of a
pulmonary embolism is a blood clot in the veins of the legs, called a deep vein thrombosis (DVT). Many clear up on
their own, though some may cause severe illness or even death.
Symptoms of pulmonary embolism may be vague, or they may resemble symptoms associated with other diseases.
Symptoms can include:
Cough
o
o
Begins suddenly
May produce bloody sputum (significant amounts of visible blood or lightly blood streaked sputum)
Sudden onset of shortness of breath at rest or with exertion
Splinting of ribs with breathing (bending over or holding the chest)
Chest pain
o Under the breastbone or on one side
o Especially sharp or stabbing; also may be burning, aching or dull, heavy sensation
o May be worsened by breathing deeply, coughing, eating, bending, or stooping
Rapid breathing
Rapid heart rate (tachycardia)
Additional symptoms that may be associated with this disease:
Wheezing
Clammy skin
Bluish skin discoloration
Nasal flaring
Pelvis pain
Leg pain in one or both legs
Swelling in the legs (lower extremities)
Lump associated with a vein near the surface of the body (superficial vein), may be painful
Low blood pressure
Weak or absent pulse
Lightheadedness or fainting
Dizziness
Sweating
Anxiety
This exam will be treated as a Call report
Patient will wait until radiologist results are faxed/called in
22
Chest for Pulmonary Vein Stenosis
Perform a Coronary CTA (protocol)
Code: 0147T
Note: pre and post pulmonary ablation
Performed with IV contrast and Esopho-cat
R/O Pulmonary Vein Stenosis
90cc’s of Isovue 370
Two Reports-Radiologist Overrerad
CT of the Chest (performed after)
Measurements needed:
A CIS vascular report with the measurements below.
Measurements Needed
Maximum AP measurement of L. Atrium
Maximum Transverse measurement of L. Atrium
The LSPV measurement is:
The LIPV measurement is:
The RSPV measurement is:
The RIPV measurement is:
Pulmonary stenosis is a congenital (present at birth) defect that occurs due to abnormal development
of the fetal heart during the first 8 weeks of pregnancy.
The pulmonary valve is found between the right ventricle and the pulmonary artery. It has three
leaflets that function like a one-way door, allowing blood to flow forward into the pulmonary artery, but
not backward into the right ventricle.
With pulmonary stenosis, problems with the pulmonary valve make it harder for the leaflets to open
and permit blood to flow forward from the right ventricle to the lungs. In children, these problems can
include:
a valve that has leaflets that are partially fused together.
a valve that has thick leaflets that do not open all the way.
the area above or below the pulmonary valve is narrowed.
There are four different types of pulmonary stenosis:
valvar pulmonary stenosis - the valve leaflets are thickened and/or narrowed
supravalvar pulmonary stenosis - the pulmonary artery just above the pulmonary valve is
narrowed
subvalvar (infundibular) pulmonary stenosis - the muscle under the valve area is thickened,
narrowing the outflow tract from the right ventricle
branch peripheral pulmonic stenosis - the right or left pulmonary artery is narrowed, or both
may be narrowed
Pulmonary stenosis may be present in varying degrees, classified according to how much obstruction to
blood flow is present. A child with severe pulmonary stenosis could be quite ill, with major symptoms
noted early in life. A child with mild pulmonary stenosis may have few or no symptoms, or perhaps
none until later in adulthood. A moderate or severe degree of obstruction can become worse with time.
23
Thoracic Outlet
(CTA of the Chest)
Code: 71275
Radiologist Report only; even though the exam is performed like a CTA, the radiologist is
responsible for commenting on the Thoracic Outlet as well as the over read.
HBOC Sched.: CT7
100cc’s of Isovue 370 @ 5cc’s per second is given for this exam
The patient is scanned with the arms down (The CTA exam), then rescanned with arms above head (to evaluate
venous and arterial flow of the subclavian and any changes of blood flow in the subclavian artery in question)
Thoracic Outlet Syndrome (TOS) is a group of distinct disorders producing signs and symptoms attributed to compression of nerves and blood
vessels in the thoracic outlet region.
Indications:
Reflex Sympathetic Dystrophy (Complex Regional Pain Syndrome)
To show the importance of Air Plethysmography in the detection of Positional Subclavian Artery Obstruction and Sympathetic Tone.
To outline a Treatment Plan
To demonstrate a cost effective Neurovascular Machine used to diagnose Thoracic Outlet Syndrome, Large and Small vessel disease,
Entrapment, Neuropathy, Sympathetic Tone, and Impotence.
SYMPTOMS
NUMBNESS OF ARMS AND HANDS
ARTERIAL
TINGLING OF ARMS AND HANDS
POSITIONAL WEAKNESS OF ARMS AND HANDS
SWELLING OF FINGERS AND HANDS
VENOUS
HEAVINESS OF THE UPPER EXTREMITY
UPPER EXTREMITY
UPPER EXTREMITY PAIN
PARESTHESIAS OF ULNAR DISTRIBUTION
WEAKNESS OF THE HANDS
NERVES
CLUMSINESS OF THE HANDS
COLDNESS OF THE HANDS
TIREDNESS, HEAVINESS AND PARESTHESIAS ON ELEVATION OF
ARMS
SHOULDER AND NECK
~
CHEST WALL
~
PAIN - TIGHTNESS
ANGINAL CHEST PAIN
INTER-PARA SCAPULAR PAIN
HEADACHES
HEAD
~
FUNNY FEELINGS IN FACE AND EAR
DIZZINESS, LIGHTHEADNESS
VERTIGO, SYNCOPE
VERTEBRAL ARTERY
~
DIPLOPIA, DYSARTHRIA, DYSPHONIA, DYSPHAGIA
TINNITUS, EAR PAIN
24
Cervical Spine
Code: 72125
WITHOUT CONTRAST
One Radiology Report Only-Non-Vascular-Non CTA exam
Almost always done without contrast; very rarely contrast is given. If contrast is given, the
exam must be performed with and without contrast.
1mm slice thickness from the base of the skull through T1; bone and soft tissue filters
curved coronal reformations as well as sagittal reformations are always done (usually on the 3D
workstation) and sent to the radiologist.
Exam takes approx. 5minutes; patient is lying supine with hands down by the side; patient goes
into the gantry (hole) head first
Indications:
Neck pain with radiculapathy
Degenerative disc disease
Fracture-trauma
Spinal Stenosis in cervical region
Postlaminectomy syndrome
Cervical Spondylosis
Anomaly of spine, unspecified
Atypical chest pain with radiculapathy
Consider MRI for disc-nerve related symptoms
25
Thoracic Spine
Code: 72128 (consider MRI)
Radiology Report only (non vascular CT exam)
Upper back pain
Trauma-fracture
Spondylosis
Spinal Stenosis
Degeneration of thoracic or thoracolumbar intervertebral disc
Myeloma
Metastatic disease to spine
Fracture with spinal cord injury
Anomaly of spine, unspecified
Technical Factors: done without contrast; 2mm slice thickness; sagittal, curved coronal reformations and/or 3D
can be obtained. (Bone and soft tissue algorithums)[ Scan begins from C7 through L1.
26
Lumbar Spine
Code: 72131 (consider MRI)
Radiology Report only (non vascular CT exam)
Lower back pain
Trauma-fracture
Spondylosis
Spinal Stenosis
Degeneration of thoracic or thoracolumbar intervertebral disc
Myeloma
Metastatic disease to spine
Fracture with spinal cord injury
Anomaly of spine, unspecified
Non-specific pain in legs while walking
Leg-lower ext. weakness-numbness-pain
Lower ext. radiculaopathy
Entire Lumbar spine (levels 1-5) scanned helical
Technical Factors: done without contrast; 1mm slice thickness; sagittal, curved coronal reformations and/or 3D
can be obtained. (Bone and soft tissue algorithms)[ Scan begins from C7 through L1.
27
With contrast
{oral and IV}
Routine {CT4}
Code: 74170 & 72194
100cc’s of Isovue 370
routine
Abdomen/Pelvis
Without IV & Oral
contrast {CT 5}
With IV Contrast
only, {CT 5}
Code: 72192 & 74150
no Oral Contrast
Code: 74170 & 72194
Abdomen pain, tenderness, discomfort
Fever of Unknown Origin
Malignancy: prostate, Testes, Liver,
Breast, Lung, Bladder, Pancreas, etc.
Kidney Stones
Diverticulitis/Diverticulosis
Retroperitoneal Hematoma Post Cath
Hodkin’s & Non-Hodgkin’s
lymphoma
Rectal Bleeding
Peritonitis
Ascities
Severe Allergic reaction to dye
Abdominal Rigidity
Interstitial Cystitis
DVT
Inflammatory process
Intrabdominal abscess
Pancreatitis
Hepatomegaly
Splenomegaly
Increased LFT’s
Non Specific findings on prior exams
Abdominal trauma
Disorder(s) of Female Organs, mensuation
Abdominal swelling
Appendicitis
Pelvic pain
Colitis
Crohn’s Disease
Abdominal mass-palpable
Endometriosis
Fistula involving female tract
Enlarged Prostate
Renal CA F/U
Persistant N&V
Genital Prolapse
Extravasations of Urine
Stomach, Intestines,Colon CA
Leukemia
Anemia (Fe def.)
Cytopenia’s
Portal Vein Thrombosis
Hernia (inguinal/ventral,umbilical)
Cirrhosis
Hepatitis
Abnormal bowel sounds
Persistant Diarrhea/constipationalternating
Changes in bowel habits
Abnormal feces
Post Op Abd. Surg.-pain-discomfort,fever
Jaundice
Fatty Liver
Duodenal, Gastric Ulcer
With & Without IV
Contrast &Oral
Contrast {CT 6}
Intestinal Obstruction
-Volvulus,
-Intususseption
-Ileus
R/O AAA
Adrenal Mass, R/O
Kidney mass, pancreas
mass, liver mass
Technical Factors:
100cc’s of contrast(Isovue 370) 3cc’s per sec.
Abdomen/Pelvis with contrast {5mm slice thickness)
Pt. drinks 72 oz. Of water within one hour, and one cup prior to
exam
Or: Excerpt from Elliott Fishman's website:
After nearly 30 years of using 3% Hypaque for positive oral contrast we
have switched to using a solution of Omnipaque-350 mixed in water. We
mix 100cc of Omnipaque-350 in 1 gallon of water. It gives an excellent
contrast in bowel of 200-220HU and is tasteless so patients find it to be
better than other choices. For your information we have found that for
every 10cc of Omnipaque-350 in a gallon of water we add 20-21HU. This
allows you to make the contrast more or less bright depending on your
needs.
Notes:
One report from Radiologist (non vascular exam) only
Patient needs to drink lots of water (72oz.)
Oncology Follow-ups after initial CIS CT Scan should be done at the
hospital. It is imperative that oncology patients be scanned at the same
facility with the same radiologist (group) and the same CT Scanner.
28
routine
With IV and Oral
Contrast (water)
(Routine)
Code: 72193
Pelvic pain
Groin pain
R/O Ovarian cyst(s)
Seminal vesiculitis
Any disorder of the male & female organ
Disorders of mensuation-abnormal bleeding
Inflammatory & Noninflammatory disorders
of vagina, vulva, cervix, uterus, and ovaries
Soft tissue evaluation
Cystitis, any Bladder disorders/conditions
Pelvis
Without IV contrast
(Oral contrast-optional)
Code: 72192
Pelvis and hip(s) trauma
Evaluate acetabulum for trauma
Bony Pelvis and hips
Osteoporsis
Degenerative hip(s) disease
Difficulty ambulating due to hip-pelvic pain
Abnormal finding(s) (pertaining to bone) on
other examination(s)
Abnormal bones scan
Joint sepsis
R/O pelvic and/or hip (acetabulum) fracture
Any disorder pertaining to bone
Foreign body localization
Usually, Ultrasound is considered first for
female symptomatic patients
Technical Factors:
2mm slice thickness
Bone algorithm and soft tissue
scanned from above iliac crest through lesser
trochanters
Notes:
One Radiology Report only (non-vascular)
29
Upper Extremity
Notes:
Indications pertaining to “joints”-cartilage-ligaments and tendons conditions and symptoms should obtain an MRI. Rarely, a CT is
ordered.
Shoulder: CT is used only for trauma-such as to scapula or any non-specific fracture to shoulder girdle. Foreign Body localization.
Definitely not to evaluate joint-rotator cuff tear(s) or shoulder joint pain>use MRI instead
Humerus/Forearm: Cellulitis, osteomyelitis and/or abscess, abnormal palpable mass; Note: Humerus is difficult to scan due to
positioning problems. Artifact caused due to chest organs and bones, head, if placed above head.
Hand(s)/Wrist(s): {Do X-Ray first} Trauma with ? Fracture on x-ray; persistent swelling and pain of unknown origin; Infective
arthritis; osteomyelitis; Foreign Body Localization
CT Angiography of Upper Extremity code: 73206
Contrast injected in the opposite ext. of the affected side due to venous contamination of the affected side, hence
extremely difficult to do this procedure bilaterally. (4cc’s per sec. 100cc’s of Isovue 370) (not venography)(Not
Thoracic Outlet)
HBOC Sched.: CT7
Two Reports: Radiology over read and Vascular Report.
Pain;
Blisters and ulcers (sores);
Gangrene (tissue death);
Weak or absent pulse;
Muscle atrophy (wasting);
Cool skin temperature;
Bluish, slow-growing nails;
Hair loss in the arm;
Swelling;
A nerve condition called ischemic neuritis; and
Bruits (abnormal sounds of blood flow that are detected by stethoscope).
Arm weakness during exercise, pain in the fingers, or hypersensitivity to cold. As the disease progresses, painful ulcers may develop
on the fingers.
AVM; Aneurysm; Claudicating
CT Venography of Upper Extremity code: 73201 & 76377
One Report: Radiologist
Embolus and thrombosis; assess dialysis graft, central line; swelling, pain, tenderness
Contrast injected: 2cc’s per second; 100cc’s of Isovue 370
IV is started in the hand of the affected side; for bilateral extremities, inject both hands simultaneously (try to use “Y”
extension catheter)
3D images generated
30
Radiology Findings
Bud Landry reads CT
Sends Completed reports
to transcription
via e-mail
OUTSIDE CLINIC
transcription
E-mails to current contact
NP to review/sign
all reports
daily
Normal results
Back to transcription
Abnormal Results
Pull Chart
Order MRI, etc.
if recommended
by Dr. Landry
Speak to MD
for further orders
CT Ordering Criteria:
I.
CT Exam Ordering Form:
II.
Diagnosis/Indication (reason for exam): There must be a diagnosis-indication to support the type of
Always need a physician’s order to order any CT whether it is with contrast or not. Try to use our standard CIS CT Exam31
Ordering form. Make sure the correct CT exam type is correctly selected (check box). This form can be ordered through
Raganit. It is front and back. The back of the form reviews issues dealing with contrast and renal insufficient issues.
Outside physician forms are acceptable as long as there is a physician’s signature and an indication.
exam ordered. Specific indications are not only required by Medicare (such as ICD-9 codes), but also it is imperative to have
indications for interpretations (cardiologist-vascular reading and radiologist-non vascular reading). Also, specific indications
may indicate a change in protocol in the actual scan of the patient. (for example, depending on the indication, it could change
the way contrast is injected, or if the scan needs contrast at all.) Although writing the ICD 9 codes is helpful, mostly for the
coders, writing documentation of the indication(s) is also essential for the technologist and the interpreters of the exam.
III. Insurance Verification
IV. Progress Note(s): even though the reason for exam may be present on the exam ordering form, the progress note
(with the order on it) may be helpful as well because it is utilized as another important document that can be helpful in making a
diagnosis for the interpreting physician and the performing technologist. It may give more history and insight to the patient’s
condition and medication(s).
V.
Lab values/Bloodwork:
(for CT’s requiring contrast only) CIS requires that a Creatinine/BUN value should be
no more than one month old. If the physician decides that an older lab value is sufficient, then there should be some
documentation that verifies that the lab values were addressed and to proceed with the contrasted CT exam and placed in the
chart. The CIS protocol for Creatinine/BUN levels are: normal patients-Creat.=2 or under; BUN 40 or under; Diabetic
patients-Creat. 1.5 or under and BUN 30 or under. If the lab values are higher than these numbers then a physician must be
consulted.
Why is the test performed: A measurement of the serum creatinine level is used to evaluate kidney
function.Creatinine is a breakdown product of creatine, which is an important component of muscle.
Creatinine can be converted to the ATP molecule, which is a high-energy source. The daily production of
creatine and subsequently creatinine, depends on muscle mass, which fluctuates very little. Creatinine is
excreted from the body entirely by the kidneys. With normal renal excretory function, the serum creatinine
level should remain constant and normal.
VI.
Prior imaging reports and/or cath drawings/reports:
Prior CT reports, cath drawings
are especially essential for both peripheral and coronary CTA. Nuclear Medicine (perfusion scans) and/or
Echos are important also for Coronary CTA. Prior cath drawings is especially needed for Coronary CTA
for post CABG patients. These prior reports are helpful to the interperter because it may identify preexisting conditions such as known tumors, blockages, congenital anomalies, etc.
32
Contrast & Renal Insufficiency Issues
Pre-medication standing order:
32Mg Medrol 12 hrs prior & again 2 hrs prior to exam
50Mg Benadryl 30 minutes prior to exam
300Mg Cimetadine (Tagament) 30 min prior to exam
Hold Metformin Drugs 48 Hrs. after
(Glucophage, Glucovance, Metaglip, Riomet, Fortumet, Avandamet)
Consult Physician if:
Pregnant
Allergic to dye
Creatnine >2
BUN>40
Diabetes: Creatnine> 1.5
Diabetes:BUN>30
Creatnine/BUN> 1 month
CIS Renal Hydration Protocol
.9% solution normal saline 1 ml per kg per hour x 6 hrs
(dose calculation for each patient)
Creatinine/BUN 1 day post contrast CT exam
600mg Mucomyst BID day prior & day of CT Exam
BMP 1 day post contrast CT exam
May Coordinate with scheduled dialysis
33
Policy: Request for CT Exams from patients and outside physician
offices
Always discourage use of printing CT exam images on “X-ray film”. This is an expensive and an outdated method.
Although CIS has the capability of printing images on “X-ray film”, there are other ways of storing and viewing images
and reports that are far easier to store and view.
$5 per sheet of film for:
Requests from Attorney offices ($50 for CD/DVD)
Patient requests for (non-referral – for pt. personal use) (CD/DVD: $20)
No charge if:
Patient is being referred to another physician by a CIS physician
An outside physician’s office is requesting images
The patient needs the images for a second opinion (CD\DVD only)…charge for film
CT Angio exams consist of thousand of images:
CTA Circle of Willis (Cerebral Arteries) (usually ordered by a Neurologist): approx. 500-600 images {.5 GB}
CTA Carotids/Vertebrals : approx. 700-800 images {.75GB}
CTA Thoracic Aorta: approx. 1,000-1,200 images {approx. 1 GB}
CTA Coronary: approx. 2,500 to 3,000 images {approx. 2.5-3 GB}
CTA Abdomen Aorta:approx. 1,000 images {approx. 1 – 1.25 GB}
CTA Aorta with Iliofemoral Run Off: approx. 2,000 –2,500 images {approx. 2 GB}
Since the CTA exams consist of an enormous amount of images, one can imagine how many sheets of x-ray film will
be needed to copy all of the images (100 sheets – 12 images per sheets?). The reason why so many images are in a
CTA exam is because the images are scanned at .5mm slice thickness. If someone ask to copy a CTA exam on x-ray
film, the technologist must re-post process the images into larger slice thickness therefore decreasing the amount of
images and decreasing the amount of sheets of x-ray film as well vs putting the entire exam on a DVD or CD. Ask the
physician what slice thickness to batch to reduce the amount of images therefore reducing the amount x-ray film.
Routine exams such as Heads, chest, Abdomen/Pelvis, etc. all or small exam sizes that consist of 100 –300 images or
so and small enough so it can be copied to a CD.
Venues for viewing CT exams:
PACS web: view images remotely; (Southeast Neuroscience Centers, Dr. Michael Ellender, and Dr.
Abou-Isss offices has this capability)
CD: any routine CT exam (Heads, spines, chests, Abd/Pelvis, pelvis’; Circle of Willis CTA; Cardiac
Scoring)
DVD: CTA exams: (Carotids, Thoracic Aorta, Abdomen Aorta, Coronary CTA, Aorta with Iliofemoral Run
Off)
X-Ray film: any CT exam; CTA exams must be batched into larger slice thickness to reduce the amount of
images and sheets of x-ray film. (see pricing for this media)
Paper: used mostly for Color 3D images on chart
34
CT Scan Suite & equipment:
35
36
Toshiba CT Scanner Information
http://www.medical.toshiba.com/
Acquilion 64
Specifications
64 simultaneous .5 mm slice with each
400ms gantry rotation
ConeviewTM reconstruction utilizes a
proprietary algorithm based on the
Feldkamp principle to ensure the best
possible image quality when scanning
with 64 slices
Isotropic scanning
Dose Efficiency
Multi-detector CT has dramatically
improved clinicians' ability to
accurately diagnose disease at an early
stage. With the corresponding increase
in CT scans comes a concern about
minimizing dose for every examination.
Although 64-detector scanners naturally
make more efficient use of the X-ray
beam than previous multi-detector
systems, other design choices impact
dose efficiency. For example, Aquilion
systems are designed with tubes that
reduce off-focal X-rays and detectors
that provide excellent image quality at
lower dose than competitive systems.
37
Vital Imaging (Vitrea 3D Workstation)
http://www.vitalimages.com/
5850 Opus Parkway, Suite 300
Minnetonka, MN 55343-4414
+1 (800) 208-3005
http://www.vitalimages.com/
38
Medical Metrx Systems(MMS)
Code: G0288 (Preview Studies)
http://www.medicalmetrx.com/
(HBOC has a separate scheduling
selection for “MMS”)
Need a physician’s order to send .5mm slice thickness images to MMS
Aneurysm F/U: 1,3,6, & 12 months
Note: it is not uncommon for a physician to order an older exam to MMS.
A physician’s order is needed and a superbill is generated from HBOC
(MMS)
MMS develops and implements innovative medical imaging, measurement, and data analysis technology. Because accuracy always matters in medicine, our technology is
designed to be precise, detailed, and comprehensive, putting surgeons and their colleagues in total control of their patient's treatments including non-invasive pre-operative
strategy, surgery, post-operative evaluation, and long-term surveillance. MMS integrates advanced 3-D medical imaging, unparalleled measurement technology and dependable
service.
Using advanced graphics workstations and proprietary software, MMS technicians create patient-specific three-dimensional computer models from two-dimensional CT and MRI
scan data.Preview® Treatment Planning Software is a unique, imaging product that offers detailed, interactive 3D computer models, combined with corresponding twodimensional images and sophisticated quantification tools. This combination creates a powerful and unique methodology for patient selection, assessment of disease, treatment
planning, and surveillance. Preview® is easy to use, requires no additional software, and runs on a desktop or laptop computer.
39
Step by Step Process of MMS
1.
2.
3.
CT scan ordered with MMS (physician needs to have an order for MMS)
CT Exam ordering form filled out
Address Renal Insuff.-contrast issues
a. Check last lab report
b. Verify if any recent testing with contrast
c. When checking lab results, if within normal limits, and longer than one
month, but no longer than two months, notify ordering physician if recent lab
results are sufficient
4. Schedule CT-no later than one week
5. CT performed and sent to MMS (written on daily CT log sheet)
6. pt. usually scheduled for a follow up visit within two weeks
since a “EVT sticker” is put on the chart, Chart automatically goes to Mercedes
(within two days)
7. Verify that a follow up visit was scheduled
8. check the status if the patient was indeed sent and received to MMS
9. create a database (in a notebook or excel spreadsheet) for patients who were sent
and not received, and once finally received, highlight that particular pt. in the
notebook
10. the latest MMS measurements of the exam are ready to be downloaded and
displayed
a. download to RadInfo folder on PACS
b. email physician (with the link to click on) notifying the physician that the
exam is ready for previewing
c. also print the data measurement sheet and place into the red folder that is
created for MMS patients
11. at the patient’s follow up visit, the red chart is placed in the patient’s chart, the
updated data and report is readily available for the physician during the patient
visit.
40
Medical Management of Severe Anaphylactoid
and Anaphylactic Reactions
I.
Clinical Recognition
Early
Sensations of warmth, itching, especially in axillae and groins
Feelings of anxiety or panic
Progressive
Erythematous or urticaral rash
Oedema of face, neck, soft tissue
Severe
Hypotension (shock)
Bronchospasm (wheezing)
Laryngeal oedema (dyspnoea, stridor, aphonia, drooling)
Arrphythmias, cardiac arrest
Note: The onset of severe clinical features may be extremely rapid without prodromal features.
II.
Acute Managemant
A severe anaphylactic reaction is a life-threatening emergency. As in all medical emergencies, initial
management should be directed mat the ABC’s of resuscitation, namely: Airway, Breathing and
Circulation.
1. Cease administration of any suspected medication of diagnostic contrast material immediately.
2. Administer oxygen by face mask at 6-8 L/minutes
3. (a.) Adults
Inject adrenaline 1:1000 intramuscularly:
Small adults
Average adults
Large adults
(<50m kg)
(50>100kg)
(>100 kg)
0.25 mL
0.50 mL
0.75 mL
(b.) Children (to age 12)
Use adrenaline 1:10 000
Or
Dilute 1 ampoule (1 ml) of adrenaline 1:1000 with 9 ml
water for injection or normal saline
Inject intramuscularly 0.25 ml per year of age (approximates
to 5 micrograms/kg)
41
42
43
44
Contrast CT Exams policy
All contrast CT exams must require a Physician or a
Nurse Practioner for direct supervision. This means
that either has to be present in the clinic or in close
proximity of the area where contrast is being injected.
Close proximity meaning no further than one floor up
or down with stair accessibility.
All contrast allergy patients must be premeditated
accordingly:
Pre-medication standing order:
32Mg Medrol 12 hrs prior & again 2 hrs prior to exam
50Mg Benadryl 30 minutes prior to exam
300Mg Cimetadine (Tagament) 30 min prior to exam
It is against policy and procedure for same day
premedication techniques.
Hold Metformin Drugs 48 Hrs. after
Consult Physician if:
BUN>40
Diabetes: Creatnine> 1.5
Diabetes:BUN>30
Creatnine/BUN> 1 month
45
Case Studies I
46
Case Studies II
47
Case Studies III
48
Case Studies IV
49
Neck anatomy
50
51
52
Coronary Blood Flow
During contraction of the ventricular myocardium (systole), the subendocardial coronary vessels (the vessels that enter
the myocardium) are compressed due to the high intraventricular pressures. However the epicardial coronary vessels
(the vessels that run along the outer surface of the heart) remain patent. Because of this, blood flow in the
subendocardium stops. As a result most myocardial perfusion occurs during heart relaxation (diastole) when the
subendocardial coronary vessels are patent and under low pressure. This contributes to the filling difficulties of the
coronary arteries.
The primary determinant of coronary blood flow is the level of myocardial/cardiac oxygen consumption. As the heart
beats more vigorously, ATP is consumed at a greater rate due to the increased force and/or frequency of contraction
and the depolarization and repolarization of the cardiac membrane potential. The increase in oxygen consumption
results in the release of a vasodilator substance, the identity of which remains unknown. The vasodilator reduces
vascular resistance and allows more blood to flow through the heart during each diastole. Systolic compression remains
the same. Failure of oxygen delivery via increases in blood flow to meet the increased oxygen demand of the heart
results in tissue ischemia, a condition of oxygen debt. Brief ischemia is associated with intense chest pain, known as
angina. Severe ischemia can cause the heart muscle to die of oxygen starvation, called a myocardial infarction. Chronic
moderate ischemia causes contraction of the heart to weaken, known as myocardial hibernation.
In addition to metabolism, the coronary circulation possesses unique pharmacologic characteristics. Prominent among
these is it's reactivity to adrenergic stimulation. The majority of circulation in the body constrict to norepinephrine, a
sympathetic neurotransmitter the body uses to increases blood pressure. In the coronary circulation, norepinephrine
elicits vasodilation, due to the predominance of beta-adrenergic receptors in the coronary circulation. Agonists of
alpha-receptors, such as phenylephrine, elicit very little constriction in the coronary circulation.
53
The anterior cerebral artery supplies oxygen to most medial portions of frontal lobes and superior medial parietal
lobes. It arises from the internal carotid artery and is part of the Circle of Willis.
The left and right anterior cerebral arteries are connected by the anterior communicating artery.
The posterior cerebral artery is the blood vessel that supplies oxygenated blood to the posterior aspect of the brain
(occipital lobe). It arises from the basilar artery and connects with the ipsilateral middle cerebral artery and internal
carotid artery via the posterior communicating artery.
The branches of the posterior cerebral artery are divided into two sets, ganglionic and cortical.
54
55
56
57
58
59
60
61
62
63
64
65
IP Addresses:
Toshiba Scanners: 192.168.7.101 & 102
Vitrea (2) Houma: 192.168.7.104
WinRad (Houma): 192.168.7.108
Drystar (Houma): 192.168.7.110
Vitrea (5) (tgmc) 192.168.7.105
Vitrea (3) (Lafayette) 192.168.2.106
Vitrea (MCSW) 192.168.2.105
Lexmark C912: (Houma) 192.168.7.115
Vitrea (Opelousas): 192.168.4.105
66
CT Contact info:
Jason Hebert
(CT Corporate Team Leader)
(985) 873-5636 office
(985) 860-1925 cellular
Jason.Hebert@cardio.com
Houma CT Scanner:
OPX: 2101 ext. 5632 Console, ext. 5630 Vitrea
225 Dunn St., Houma, Louisiana 70360
CT Scan room (985) 873-5632;Vitrea-reading room: (985) 873-5630
CT Fax: (985) 876-0397; efax: (509) 692-3110
Lafayette CT Scanner: OPX:
2201 ext. 232 Console, ext. 338 Vitrea
2730 Ambassador Caffery Pkwy, Lafayette, Louisiana 70596-1160
CT Scan Room: (337) 291-6963
Laf. CT Fax#: (337) 988-9097; eFax#: (509)-278-3277
Opelousas CTA:
OPX: 2401 ext. 207 Console
1233 Wayne Gilmore Circle, Suite 450, Opelousas, Louisiana, 70570
CT Scan Room: (337) 407-3207
Opel. CT Fax#: (337) 942-3015; Vitrea-reading room: (337)-407-3216
CTA Scheduling Desk 337-407-3201
Thibodaux CT Scanner: OPX:
2601
1320 Martin Luther King Dr., Thibodaux, Louisiana 70301
CT Scan Room: (985) 446-2021 ext. 219 or 220
67