Microscopic structure of the alveolar wall
advertisement

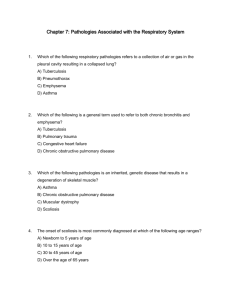
The Lung 1.Pneumonia 2.COPD 3.Pneumoconiosis 4.Lung vessels diseases 5.Chronic cor pulmonale 6. Lung cancer 7.Tuberculosis Pathology Department, Zhejiang University School of Medicine, Zhu keqing 竺可青,zhukeqing@yahoo.com, 2007-11-27 What is the diagnosis? 1. Pneumonia • • • • • Lobar pneumonia Lobular pneumonia Legionella pneumonia Viral pneumonia Mycoplasmal pneumonia Lobar pneumonia • 4 stages • Lobar pneumonia is an acute bacterial infection resulting in fibrinosuppurative consolidation of a large portion of a lobe or of an entire lobe. • Moreover, the same organisms may produce bronchopneumonia in one patient, whereas in the more vulnerable individual, a full-blown lobar involvement develops. • Most important from the clinical standpoint are identification of the causative agent and determination of the extent of disease. • In lobar pneumonia, four stages of the inflammatory response have classically been described: congestion, red hepatization, gray hepatization, and resolution. • Present-day effective antibiotic therapy frequently slows or halts the progression. • In the first stage of congestion, the lung is heavy, boggy, and red. It is characterized by vascular engorgement, intra-alveolar fluid with few neutrophils, and often the presence of numerous bacteria. 充血水肿期 The stage of red hepatization that follows is characterized by massive confluent exudation with red cells (congestion), neutrophils, and fibrin filling the alveolar spaces. On gross examination, the lobe now appears distinctly red, firm, and airless, with a liver-like consistency, hence the term hepatization. 红色肝样变期 The stage of gray hepatization follows with progressive disintegration of red cells and the persistence of a fibrinosuppurative exudate, giving the gross appearance of a grayish brown, dry surface. 灰色肝样变期 In the final stage of resolution, the consolidated exudate within the alveolar spaces undergoes progressive enzymatic digestion to produce a granular, semifluid, debris that is resorbed, ingested by macrophages, coughed up, or organized by fibroblasts growing into it.溶解消散期 • • • Pneumococcal pneumonia A, Acute pneumonia. The congested septal capillaries and extensive neutrophil exudation into alveoli corresponds to early red hepatization. Fibrin nets have not yet formed. B, Early organization of intra-alveolar exudate, seen in areas to be streaming through the pores of Kohn (arrow). C, Advanced organizing pneumonia (corresponding to gray hepatization), featuring transformation of exudates to fibromyxoid masses richly infiltrated by macrophages and fibroblasts. Lobar pneumonia-gray hepatization • • • • • Complications of pneumonia include (1) tissue destruction and necrosis, causing abscess formation (particularly common with type 3 pneumococci or Klebsiella infections); (2) spread of infection to the pleural cavity, causing the intrapleural fibrinosuppurative reaction known as empyema; (3) organization of the exudate, which may convert a portion of the lung into solid tissue; pulmonary carnification (4) bacteremic dissemination to the heart valves, pericardium, brain, kidneys, spleen, or joints, causing metastatic abscesses, endocarditis, meningitis, or suppurative arthritis. Bronchopneumonia • Foci of bronchopneumonia are consolidated areas of acute suppurative inflammation. • The consolidation may be patchy through one lobe but is more often multilobar and frequently bilateral and basal because of the tendency of secretions to gravitate into the lower lobes. • Well-developed lesions are usually 3 to 4 cm in diameter, slightly elevated, dry, granular, gray-red to yellow, and poorly delimited at their margins. • Histologically, the reaction usually elicits a suppurative, neutrophilrich exudate that fills the bronchi, bronchioles, and adjacent alveolar spaces. Comparison of bronchopneumonia and lobar pneumonia Clinical Course • The major symptoms of community-acquired acute pneumonia are abrupt onset of high fever, shaking chills, and cough productive of mucopurulent sputum; occasional patients may have hemoptysis. • When fibrinosuppurative pleuritis is present, it is accompanied by pleuritic pain and pleural friction rub. • The characteristic radiologic appearance of lobar pneumonia is that of a radio-opaque, usually well-circumscribed lobe, whereas bronchopneumonia shows focal opacities. Legionella pneumonia • Legionella pneumophilia ATYPICAL (VIRAL AND MYCOPLASMAL) PNEUMONIAS • Viral pneumonia • Mycoplasmal pneumonia • The term "primary atypical pneumonia" was initially applied to an acute febrile respiratory disease characterized by patchy inflammatory changes in the lungs, largely confined to the alveolar septa and pulmonary interstitium. • The term "atypical" denotes the moderate amount of sputum, no physical findings of consolidation, only moderate elevation of white cell count, and lack of alveolar exudate. • The pneumonitis is caused by a variety of organisms, the most common being Mycoplasma pneumoniae. • Other etiologic agents are viruses, including influenza virus types A and B, the respiratory syncytial viruses, adenovirus, rhinoviruses, rubeola, and varicella viruses; Chlamydia pneumoniae; and Coxiella burnetti (Q fever). • The histologic pattern depends on the severity of the disease. Predominant is the interstitial nature of the inflammatory reaction, virtually localized within the walls of the alveoli. • The alveolar septa are widened and edematous and usually have a mononuclear inflammatory infiltrate of lymphocytes, histiocytes, and occasionally plasma cells. In acute cases, neutrophils may also be present. • The alveoli may be free from exudate, but in many patients, there is intra-alveolar proteinaceous material, a cellular exudate, and characteristically pink hyaline membranes lining the alveolar walls. • 病毒包涵体 Usual interstitial pneumonia. The fibrosis, which varies in intensity, is more pronounced in the subpleural region. Usual interstitial pneumonia. Fibroblastic focus with fibers running parallel to surface and bluish myxoid extracellular matrix. Pyemic lung abscess in the center of section with complete destruction of underlying parenchyma within the focus of involvement 2. COPD • • • • Chronic bronchitis Pulmonary emphysema Bronchial asthma Bronchiectasis Disorders Associated with Airflow Obstruction: The Spectrum of Chronic Obstructive Pulmonary Disease Chronic bronchitis • • • • Bronchus Mucous gland hyperplasia, hypersecretion Tobacco smoke, air pollutants Cough, sputum production Bronchiectasis • • • • Bronchus Airway dilation and scarring Persistent or severe infections Cough, purulent sputum, fever Asthma • • • • Bronchus Smooth muscle hyperplasia, excess mucus, inflammation Immunologic or undefined causes Episodic wheezing, cough, dyspnea Emphysema • • • • Acinus Airspace enlargement; wall destruction Tobacco smoke Dyspnea • Clinical Term Anatomic Site Major Pathologic Changes Etiology Signs/Symptoms 2.1 Chronic bronchitis • Chronic bronchitis, so common among habitual smokers and inhabitants of smog-laden cities, is not nearly as trivial as was once thought. • When persistent for years, it may (1) progress to chronic obstructive airway disease, (2) lead to cor pulmonale and heart failure, or (3) cause atypical metaplasia and dysplasia of the respiratory epithelium, providing a rich soil for cancerous transformation. • Chronic bronchitis per se is defined clinically. It is present in any patient who has persistent cough with sputum production for at least 3 months in at least 2 consecutive years, in the absence of any other identifiable cause. • In simple chronic bronchitis, patients have a productive cough but no physiologic evidence of airflow obstruction. • Some individuals may demonstrate hyperreactive airways with intermittent bronchospasm and wheezing. This condition is called chronic asthmatic bronchitis. • Finally, some patients, especially heavy smokers, develop chronic airflow obstruction, usually with evidence of associated emphysema, and are classified as showing obstructive chronic bronchitis. Morphology • Grossly, there may be hyperemia, swelling, and edema of the mucous membranes, frequently accompanied by excessive mucinous to mucopurulent secretions layering the epithelial surfaces. • The characteristic histologic features of chronic bronchitis are chronic inflammation of the airways (predominantly lymphocytes) and enlargement of the mucus-secreting glands of the trachea and bronchi. • This increase can be assessed by the ratio of the thickness of the mucous gland layer to the thickness of the wall between the epithelium and the cartilage (Reid index). The Reid index (normally 0.4) is increased in chronic bronchitis, usually in proportion to the severity and duration of the disease. • The bronchial epithelium may exhibit squamous metaplasia and dysplasia. There is marked narrowing of bronchioles caused by goblet cell metaplasia, mucus plugging, inflammation, and fibrosis. Clinical Features • The cardinal symptom of chronic bronchitis is a persistent cough productive of sputum. For many years, no other respiratory functional impairment is present, but eventually, dyspnea on exertion develops. • With the passage of time, and usually with continued smoking, other elements of COPD may appear, including hypercapnia高碳酸血症, hypoxemia, and mild cyanosis. • Differentiation of pure chronic bronchitis from that associated with emphysema can be made in the classic case, but, as has been mentioned, many patients with COPD have both conditions. • Long-standing severe chronic bronchitis commonly leads to cor pulmonale with cardiac failure. 2.2 Pulmonary emphysema • Emphysema is a condition of the lung characterized by abnormal permanent enlargement of the airspaces distal to the terminal bronchiole, accompanied by destruction of their walls and without obvious fibrosis. • In contrast, the enlargement of airspaces unaccompanied by destruction is termed "overinflation," for example, the distention of airspaces that occurs in the remaining lung after unilateral pneumonectomy. Types of Emphysema • Although the term "emphysema" is sometimes loosely applied to diverse conditions, there are four major types: (1) centriacinar, (2) panacinar, (3) paraseptal, and (4) irregular. • Only the first two cause clinically significant airflow obstruction. • Centriacinar emphysema is far more common than the panacinar form, constituting more than 95% of cases. Pathogenesis of emphysema. The protease-antiprotease imbalance and oxidant-antioxidant imbalance are additive in their effects and contribute to tissue damage. α1-antitrypsin (α1-AT) deficiency can be either congenital or "functional" as a result of oxidative inactivation. Thus, emphysema is seen to result from the destructive effect of high protease activity in subjects with low antiprotease activity. A, Diagram of normal structures within the acinus, the fundamental unit of the lung. A terminal bronchiole (not shown) is immediately proximal to the respiratory bronchiole. B, Centriacinar emphysema with dilation that initially affects the respiratory bronchioles. C, Panacinar emphysema with initial distention of the peripheral structures (i.e., the alveolus and alveolar duct); the disease later extends to affect the respiratory bronchioles. Centriacinar emphysema. Central areas show marked emphysematous damage (E), surrounded by relatively spared alveolar spaces. Panacinar emphysema involving the entire pulmonary architecture Bullous Emphysema • Bullous emphysema refers merely to any form of emphysema that produces large subpleural blebs or bullae (spaces more than 2 cm in diameter in the distended state). • They represent localized accentuations of one of the four forms of emphysema, are most often subpleural, and occur near the apex, sometimes in relation to old tuberculous scarring. • On occasion, rupture of the bullae may give rise to pneumothorax. Bullous emphysema with large subpleural bullae Interstitial Emphysema • The entrance of air into the connective tissue stroma of the lung, mediastinum, or subcutaneous tissue is designated interstitial emphysema. • In most instances, alveolar tears in pulmonary emphysema provide the avenue of entrance of air into the stroma of the lung, but rarely, a wound of the chest that allows air to be sucked in or a fractured rib that punctures the lung substance may underlie this disorder. • Children with whooping cough and bronchitis, patients with obstruction to the airways (by blood clots, tissue, or foreign bodies) or who are being artificially ventilated, and individuals who suddenly inhale irritant gases provide classic examples. Predominant Bronchitis • • • • • • • • • • Predominant Emphysema Age (yr) 40-45 50-75 Dyspnea Mild; late Severe; early Cough Early; copious sputum Late; scanty sputum Infections Common Occasional Respiratory insufficiency Repeated Terminal Cor pulmonale Common Rare; terminal Airway resistance Increased Normal or slightly increased Elastic recoil Normal Low Chest radiograph Prominent vessels; large heart Hyperinflation; small heart Appearance Blue bloater Pink puffer 2.3 Bronchial asthma • • • Asthma is a chronic inflammatory disorder of the airways that causes recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night and/or in the early morning. It is thought that inflammation causes an increase in airway responsiveness (bronchospasm) to a variety of stimuli. Some of these stimuli would have little or no effect on nonasthmatics with normal airways. Many cells play a role in the inflammatory response, in particular eosinophils, mast cells, macrophages, T lymphocytes, neutrophils, and epithelial cells. 2.3 Asthma Airway remodeling • Thickening of the basement membrane of the bronchial epithelium • Edema and an inflammatory infiltrate in the bronchial walls, with a prominence of eosinophils and mast cells • An increase in size of the submucosal glands • Hypertrophy of the bronchial wall muscle 2.4 Various forms of atelectasis in adults 2.5 Bronchiectasis • Bronchiectasis is a disease characterized by permanent dilation of bronchi and bronchioles caused by destruction of the muscle and elastic tissue, resulting from or associated with chronic necrotizing infections. • To be considered bronchiectasis, the dilation should be permanent; reversible bronchial dilation often accompanies viral and bacterial pneumonia. Morphology • Bronchiectasis usually affects the lower lobes bilaterally, particularly air passages that are vertical, and is most severe in the more distal bronchi and bronchioles. • The airways are dilated, sometimes up to four times normal size. • These dilations may produce long, tubelike enlargements (cylindrical bronchiectasis) or, in other cases, may cause fusiform or even sharply saccular distention (saccular bronchiectasis). Bronchiectasis in a patient with cystic fibrosis, who underwent lung transplantation Bronchiectasis in a patient with cystic fibrosis, who underwent lung transplantation 3. Pneumoconiosis • Silicosis • Sarcoidosis Major Categories of Chronic Interstitial Lung Disease Fibrosing • Usual interstitial pneumonia (idiopathic pulmonary fibrosis) • Nonspecific interstitial pneumonia • Cryptogenic organizing pneumonia • Associated with collagen vascular diseases • Pneumoconiosis尘肺 • Drug reactions • Radiation pneumonitis Granulomatous • Sarcoidosis • Hypersensitivity pneumonitis EosinophilicSmoking-Related • Desquamative interstitial pneumonia • Respiratory bronchiolitis-associated interstitial lung disease Other • Pulmonary alveolar proteinosis Progressive massive fibrosis superimposed on coal workers' pneumoconiosis Silicosis • Silicosis is a lung disease caused by inhalation of crystalline silicon dioxide (silica).(5um) • Currently the most prevalent chronic occupational disease in the world, silicosis usually presents, after decades of exposure, as a slowly progressing, nodular, fibrosing pneumoconiosis. • Workers in a large number of occupations are at risk, especially sandblasters and many mine workers. Morphology • • • • Silicosis is characterized grossly in its early stages by tiny, barely palpable, discrete pale to blackened (if coal dust is also present) nodules in the upper zones of the lungs. As the disease progresses, these nodules may coalesce into hard, collagenous scars. Histologically, the nodular lesions consist of concentric layers of hyalinized collagen surrounded by a dense capsule of more condensed collagen. Examination of the nodules by polarized microscopy reveals the birefringent silica particles. Advanced silicosis seen on transection of lung. Scarring has contracted the upper lobe into a small dark mass (arrow). Note the dense pleural thickening. Several coalescent collagenous silicotic nodules Large saddle embolus from the femoral vein lying astride the main left and right pulmonary arteries Hemorrhagic pulmonary infarct 4. Lung vessels diseases • ARDS • Chronic pulmonary hypertension Diffuse alveolar damage (acute respiratory distress syndrome) Vascular changes in pulmonary hypertension 5. Chronic cor pulmonale • Cor pulmonale, as pulmonary HHD is frequently called, consists of right ventricular hypertrophy, dilation, and potentially failure secondary to pulmonary hypertension caused by disorders of the lungs or pulmonary vasculature. Chronic cor pulmonale Disorders Predisposing to Cor Pulmonale Diseases of the Pulmonary Parenchyma • Chronic obstructive pulmonary disease • Diffuse pulmonary interstitial fibrosis • Pneumoconioses • Cystic fibrosis • Bronchiectasis Diseases of the Pulmonary Vessels • Recurrent pulmonary thromboembolism • Primary pulmonary hypertension • Extensive pulmonary arteritis (e.g., Wegener granulomatosis) • Drug-, toxin-, or radiation-induced vascular obstruction • Extensive pulmonary tumor microembolism Disorders Affecting Chest Movement • Kyphoscoliosis • Marked obesity (pickwickian syndrome) • Neuromuscular diseases Disorders Inducing Pulmonary Arterial Constriction • Metabolic acidosis • Hypoxemia • Chronic altitude sickness • Obstruction to major airways • Idiopathic alveolar hypoventilation 6. Lung cancer • • • • Squamous cell carcinoma (25% to 40%) Adenocarcinoma (25% to 40%) Small cell carcinoma (20% to 25%) Large cell carcinoma (10% to 15%) Cytologic diagnosis of lung cancer is often possible Lung carcinoma Histologic appearance of lung carcinoma Numerous metastases from a renal cell carcinoma Malignant mesothelioma Malignant mesothelioma Hilar mass that was considered radiographically to be carcinoma but proved pathologically to be organized pneumonia. 7. Tucberulosis • • • • Mycobacterium tuberculosis Tuberculin reaction Tuberculous granuloma/tubercle Caseous necrosis 基本病变 • 渗出:浆液纤维蛋白性炎 • 增生:结核结节 • 变质:干酪样坏死 The morphologic spectrum of tuberculosis 结局 转向愈合 • 吸收消散(吸收好转期) • 纤维化钙化(硬结钙化期) 转向恶化 • 侵润进展(侵润进展期) • 溶解播散(溶解播散期) The natural history and spectrum of tuberculosis Primary Tuberculosis • In countries where bovine tuberculosis and infected milk have been eliminated, primary tuberculosis almost always begins in the lungs. • Typically, the inhaled bacilli implant in the distal airspaces of the lower part of the upper lobe or the upper part of the lower lobe, usually close to the pleura. As sensitization develops, a 1- to 1.5-cm area of gray-white inflammatory consolidation emerges, known as the Ghon focus. • In most cases, the center of this focus undergoes caseous necrosis. Tubercle bacilli, either free or within phagocytes, drain to the regional nodes, which also often caseate. This combination of parenchymal lung lesion and nodal involvement is referred to as the Ghon complex. Primary tuberculosis • Primary tuberculosis is the form of disease that develops in a previously unexposed, and therefore unsensitized, person. • About 5% of newly infected people develop clinically significant disease. The elderly and profoundly immunosuppressed persons may lose their immunity to the tubercle bacillus and so may develop primary tuberculosis more than once. • With primary tuberculosis, the source of the organism is exogenous. Primary pulmonary tuberculosis, Ghon complex. The gray-white parenchymal focus is under the pleura in the lower part of the upper lobe. Hilar lymph nodes with caseation are seen on the left. 结 局 1 痊愈 2 恶化 支气管播散 淋巴道播散 血道播散/ Systemic miliary tuberculosis • • • • Acute systemic miliary tuberculosis Chronic systemic miliary tuberculosis Acute pulmonary miliary tuberculosis Chronic pulmonary miliary tuberculosis • Miliary pulmonary disease occurs when organisms drain through lymphatics into the lymphatic ducts, which empty into the venous return to the right side of the heart and thence into the pulmonary arteries. • Individual lesions are either microscopic or small, visible (2-mm) foci of yellow-white consolidation scattered through the lung parenchyma (the word "miliary" is derived from the resemblance of these foci to millet seeds). • With progressive pulmonary tuberculosis, the pleural cavity is invariably involved, and serous pleural effusions, tuberculous empyema, or obliterative fibrous pleuritis may develop. • Systemic miliary tuberculosis ensues when infective foci in the lungs seed the pulmonary venous return to the heart; the organisms subsequently disseminate through the systemic arterial system. • Almost every organ in the body can be seeded. Lesions resemble those in the lung. • Miliary tuberculosis is most prominent in the liver, bone marrow, spleen, adrenals, meninges, kidneys, fallopian tubes, and epididymis. Miliary tuberculosis of the spleen. The cut surface shows numerous gray-white granulomas. Secondary tuberculosis • Secondary tuberculosis is the pattern of disease that arises in a previously sensitized host. • It may follow shortly after primary tuberculosis, but more commonly, it arises from reactivation of dormant primary lesions many decades after initial infection, particularly when host resistance is weakened. • It may also result from exogenous reinfection because of waning of the protection afforded by the primary disease or because of a large inoculum of virulent bacilli. Secondary pulmonary tuberculosis • • • • • • Focal pulmonary tuberculosis Infiltrative pulmonary tuberculosis Chronic fibro-cavitative pulmonary tuberculosis Caseous pneumonia Tuberculoma Tuberculous pleuritis Posteroanterior radiograph of a 54-year-old man with cough, fever, and a right upper lobe cavitary process due to Mycobacterium tuberculosis infection Secondary pulmonary tuberculosis Extrapulmonary tuberculosis • • • • • • • Intestinal tuberculosis 回盲部 Tuberculosis peritonitis Tuberculosis meningitis Tuberculosis of the kidney Tuberculosis of the genital system Tuberculosis of the bone/joint 冷脓肿 Tuberculosis of the lymph node • Isolated-organ tuberculosis may appear in any of the organs or tissues seeded hematogenously and may be the presenting manifestation of tuberculosis. • Organs that are typically involved include the meninges (tuberculous meningitis), kidneys (renal tuberculosis), adrenals (formerly an important cause of Addison disease), bones (osteomyelitis), and fallopian tubes (salpingitis). • When the vertebrae are affected, the disease is referred to as Pott's disease. Paraspinal "cold" abscesses in these patients may track along the tissue planes to present as an abdominal or pelvic mass. • In years past, intestinal tuberculosis contracted by the drinking of contaminated milk was fairly common as a primary focus of tuberculosis. • In developed countries today, intestinal tuberculosis is more often a complication of protracted advanced secondary tuberculosis, secondary to the swallowing of coughed-up infective material. • Typically, the organisms are trapped in mucosal lymphoid aggregations of the small and large bowel, which then undergo inflammatory enlargement with ulceration of the overlying mucosa, particularly in the ileum. Mycobacterium avium infection in a patient with AIDS, showing massive infection with acid-fast organisms • 推荐 • • • • • • 1. 2. 3. 4. 5. 6. 哲人后丛书 师从天才:一个科学王朝的崛起 哲人后丛书 激情澎湃:科学家的内心世界 哲人后丛书 PCR传奇 创世纪的第八天 Anderson’s Pathology (9th/10th) DNA双螺旋的故事