Thymus and Spleen
advertisement
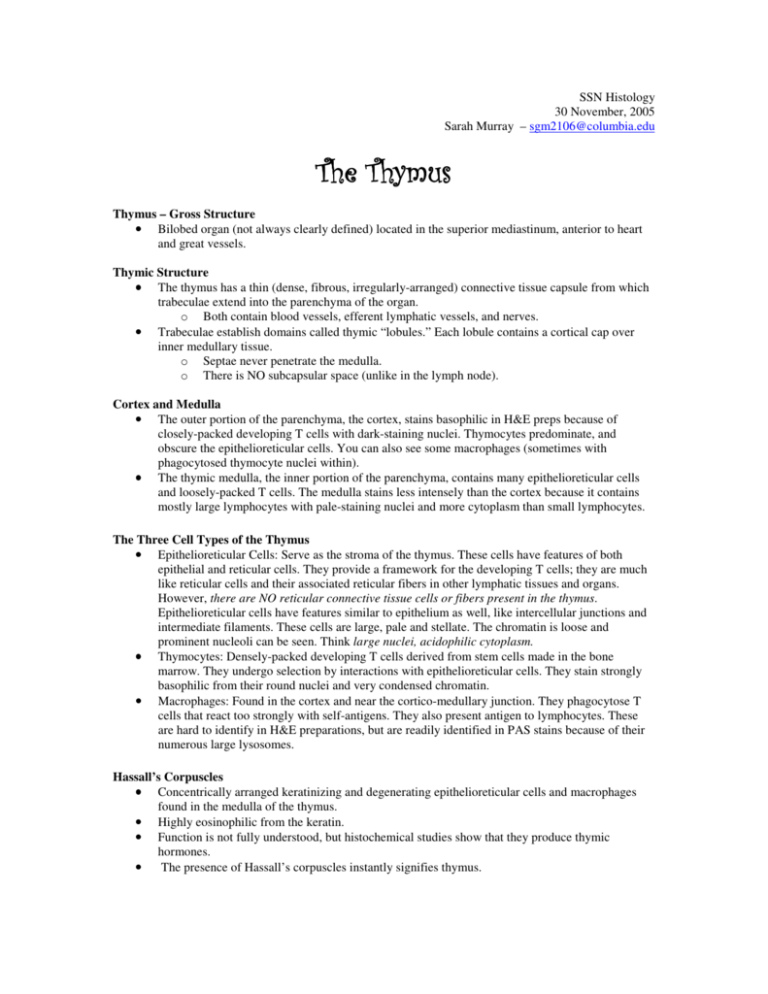
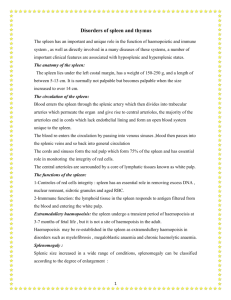
SSN Histology 30 November, 2005 Sarah Murray – sgm2106@columbia.edu The Thymus Thymus – Gross Structure • Bilobed organ (not always clearly defined) located in the superior mediastinum, anterior to heart and great vessels. Thymic Structure • The thymus has a thin (dense, fibrous, irregularly-arranged) connective tissue capsule from which trabeculae extend into the parenchyma of the organ. o Both contain blood vessels, efferent lymphatic vessels, and nerves. • Trabeculae establish domains called thymic “lobules.” Each lobule contains a cortical cap over inner medullary tissue. o Septae never penetrate the medulla. o There is NO subcapsular space (unlike in the lymph node). Cortex and Medulla • The outer portion of the parenchyma, the cortex, stains basophilic in H&E preps because of closely-packed developing T cells with dark-staining nuclei. Thymocytes predominate, and obscure the epithelioreticular cells. You can also see some macrophages (sometimes with phagocytosed thymocyte nuclei within). • The thymic medulla, the inner portion of the parenchyma, contains many epithelioreticular cells and loosely-packed T cells. The medulla stains less intensely than the cortex because it contains mostly large lymphocytes with pale-staining nuclei and more cytoplasm than small lymphocytes. The Three Cell Types of the Thymus • Epithelioreticular Cells: Serve as the stroma of the thymus. These cells have features of both epithelial and reticular cells. They provide a framework for the developing T cells; they are much like reticular cells and their associated reticular fibers in other lymphatic tissues and organs. However, there are NO reticular connective tissue cells or fibers present in the thymus. Epithelioreticular cells have features similar to epithelium as well, like intercellular junctions and intermediate filaments. These cells are large, pale and stellate. The chromatin is loose and prominent nucleoli can be seen. Think large nuclei, acidophilic cytoplasm. • Thymocytes: Densely-packed developing T cells derived from stem cells made in the bone marrow. They undergo selection by interactions with epithelioreticular cells. They stain strongly basophilic from their round nuclei and very condensed chromatin. • Macrophages: Found in the cortex and near the cortico-medullary junction. They phagocytose T cells that react too strongly with self-antigens. They also present antigen to lymphocytes. These are hard to identify in H&E preparations, but are readily identified in PAS stains because of their numerous large lysosomes. Hassall’s Corpuscles • Concentrically arranged keratinizing and degenerating epithelioreticular cells and macrophages found in the medulla of the thymus. • Highly eosinophilic from the keratin. • Function is not fully understood, but histochemical studies show that they produce thymic hormones. • The presence of Hassall’s corpuscles instantly signifies thymus. Thymus: The Education of T Cells • During fetal life, the thymus is populated by multipotential lymphoid stem cells that come from the bone marrow and are destined to become immunocompetent T cells. • Thymic cell education refers to stem cell maturation and differentiation that results in such immunocompetent T cells. • Positive Selection: The stem cells enter the medulla of the thymus via a postcapillary venue and then migrate to the periphery of the thymic lobule. The cells are presented with self and foreign antigens by epithelioreticular cells. If the lymphocyte recognizes self MHC and self or foreign antigen, it will survive the selection. If not, cell death will occur. • Negative Selection: Cells that pass positive selection test enter the medulla of the thymus. Here they undergo another selection process in which cells directed to self-antigen displayed by self MHC are eliminated. • From here, T cells either become cytotoxic CD8+ T cells or helper CD4+ T cells. Ready for the immune response, they leave the thymus from the medulla and enter the blood circulation. Only 5% of thymocytes survive to leave the thymus as functional naïve T cells! Blood-Thymic Barrier • Arterioles that branch into the cortex are surrounded by a perivascular connective tissue sheath containing macrophages, a basal lamina, and an epithelioreticular cell sheath. This forms a highly impermeable barrier to macromolecules and is called the blood-thymic barrier. • The blood-thymic barrier allows thymocytes to mature and undergo selection in an environment protected from contact with foreign antigens. The Adult Thymus • The thymus is critical for establishing the immune system during childhood, but begins to shrink just before puberty. • In adults, thymic tissue is replaced by adipose tissue ( involution); however, thymocytes are continually produced into old age. • In adults, it is difficult to distinguish between the cortex and medulla by the concentration of thymocytes. Still, Hassall’s corpuscles can still be identified in the medulla. Notes: • The thymus does not have lymphatic nodules (but can appear as if it does)! • The thymus does not have afferent lymphatic vessels! The Spleen The Spleen: What is it Good For? • Filters blood: removes old and damaged RBCs and platelets. • Iron retrieval and heme metabolism. • Reserve for red blood cells; it is engorged with blood. • Immune response against blood-borne antigens. • Fetal hematopoiesis. The Spleen – Structure • The spleen is enclosed by a dense connective tissue capsule from which trabeculae extend into the parenchyma. • The connective tissue of the capsule and trabeculae contain myofibroblasts. o The spleen holds large volumes of RBCs in reserve. Contraction in the capsule and trabeculae, via myofibroblasts, helps discharge stored RBCs into the systemic circulation. • • Most of the spleen consists of splenic pulp, which is divided into two functionally and morphologically different regions: white pulp and red pulp (based on color of fresh sections). White pulp appears as circular or elongated whitish gray areas surrounded by red pulp. The hilum, located on the medial surface of the spleen, is the site for the passage of the splenic artery and vein, nerves, and lymphatic vessels. Lymphatic vessels originate in the white pulp near the trabeculae and constitute a route for lymphatics leaving the spleen. Spleen – Capsule and Trabeculae • Dense, fibrous, irregularly-arranged connective tissue. • Contains reticular fibers (Foot’s silver and azo-carmine stain them black). The Spleen – Vascular Schematic • The spleen is supplied by a single splenic artery and drained by a single splenic vein; all vessels enter the hilum. Splenic artery ↓ Trabecular arteries ↓ Central arteries (PALS) ↓ Penicilli (arterioles) • • • Splenic Vein ↑ Trabecular veins ↑ Pulp Veins ↑ → Ellipsoids → Sinusoids White pulp vasculature: o Branches of the splenic artery course through the capsule and trabeculae of the spleen and then enter the white pulp. Within the white pulp, the branch of the splenic artery is called the central artery. o Lymphocytes that aggregate around the central artery constitute the periarterial lymphatic sheath (PALS). The PALS has a roughly cylindrical configuration the conforms to the course of the central artery. Lymphatic nodules appear as localized expansions of the PALS and displace the central artery, so that it occupies an eccentric rather than central position. o Penicilli (arterioles) branch off the central artery. o The central artery also sends branches to the marginal zone at the area between the white pulp and red pulp. It contains blood cells, lymphocytes, macrophages, and reticular cells. This is the site of immunological activities due to presence of blood antigens. No sinusoids here. Red pulp vasculature o Sheathed capillaries known as ellipsoids branch off the central artery. These are surrounded by aggregations of macrophages. o The ellipsoids empty directly into the reticular meshwork of splenic cords. Blood percolates through the cords and is exposed to the macrophages within before returning to the circulation by squeezing through the walls of the splenic sinuses. Sinusoids o The endothelial cells that line the splenic sinuses are extremely long. There are few contact points between adjacent cells, allowing blood cells to pass readily into and out of sinuses. o Processes of macrophages extend between the endothelial cells and into the lumen of the sinuses to monitor the passing blood for foreign antigens. o Sinuses don’t have a continuous basal lamina. The strands of basal lamina stain with silver-containing reagents or with PAS reaction, as demonstrated on the slides. The White Pulp • Immune function: site of B cell – T cell interaction and antibody production. • • Reticular connective tissue is filled with lymphocytes. Nodules appear as localized expansions of the PALS and displace the central artery. They are the territory of B cells; other lymphocytes of the PALS are T cells that surround the nodules. The nodules usually contain germinal centers that develop as B cells proliferate following their activation. The Red Pulp • Consists of sinuses separated by splenic Cords of Billroth. o Cords of Billroth are a loose meshwork of reticular cells and reticular fibers that contain many RBCs, macrophages, lymphocytes, plasma cells, and granulocytes. • Blood entering the red pulp percolates through the cords and is exposed to macrophages before returning to the circulation by squeezing through the walls of the splenic sinuses. • Splenic macrophages phagocytose damaged RBCs. The iron from these cells is used in formation of new RBCs. Answers to Review Questions Question 1: The answer is C. Hassal’s corpuscules should guide you to know that this is the thymus. The function of the thymus is to “educate T cells.” Maturation of T cells occurs in the thymus (only T cells that react weakly with self MHC and self antigens presented by epithelioreticular cells survive). Question 2: The answer is A. The capsule and trabeculae of the spleen are composed of dense fibrous irregularly arranged connective tissue. Type I collagen is the most prevalent kind of collagen in loose and dense connective tissues. Type II collagen is present in hyaline and elastic cartilage. Type I collagen resists tension, while type II resists pressure. Question 3: The answer is A. Arterioles that branch into the cortex of the thymus are surrounded by a perivascular sheath and an epithelioreticular cell sheath. These components make up the blood-thymic barrier. The barrier allows thymocytes to mature and undergo selection in an environment protected from contact with foreign antigens. Choice B is incorrect because there are no afferent lymphatics in the thymus. Once thymocytes mature, they leave the thymus and go to the periphery, never to return. Question 4: The answer is C. The structure at the pointer is a Cord of Billroth in the spleen. The Cords of Billroth are the parenchyma of the red pulp. They consist of reticular tissue with macrophages, lymphocytes and red blood cells. Type III collagen is found in reticular fibers. Type II collagen is not found in the Cords of Billroth. It is present in hyaline and elastic cartilage. Question 5: The answer is D. The order of blood flow through the spleen is: splenic artery trabecular arteries central arterioles penicillin ellipsoids sinusoids pulp veins trabecular veins splenic vein. Question 6: The answer is C. This is the spleen. The capsule of the spleen contains smooth muscle to pump stored blood into the circulation. Unlike the thymus, the capsule also contains reticular fibers that stain black with silver stain.