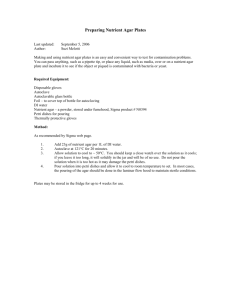
A laboratory Manual
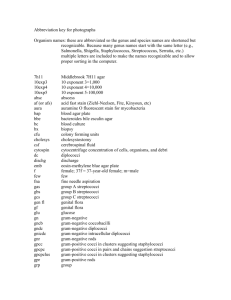
advertisement

Medical Microbiology BIOM 322 Laboratory Manual A Laboratory Manual Medical Microbiology (BIOM 322) Pre-request Microbiology (1062 241) Organized by: Dr. Adil Makkiya Dr. Asma Al-Thani Dr. Hala Bargal Qatar University Biomedical Program 1 Medical Microbiology BIOM 322 Laboratory Manual Table of Content: No Title Page 1 Course work details divided into weeks Course objectives divided according to course work weeks of Medical Microbiology (1066322) Experiment 1: Laboratory safety, precautions and sterilization & preparing culture media their classification dispensing Experiment 2: Use of blood differential and Selective Media Experiment 3: Microbial flora of throat, interteeth ,skin ,nails and hair Experiment 4: a) Identification of Human Staphylococcal Pathogens b) Chemical agent of control, Chemotherapeutic agents Experiment 5: Identification of Human Streptococcal Pathogens Experiment 6: Identification of Streptococcus pneumoniae Experiment 7: Intestinal Pathogens in the Family Enterobacteriaceae (Characterization of lactose fermenting enteric bacteria (E. coli &Klebsiella) Experiment 8: Characterization of non lactose fermenting enteric bacteria (Proteus&Pseudomonas) Experiment 9: Characterization of Salmonella and Shigella Experiment 10: a) API -20E b) Demonstration Experiment 11: Haemofilus influenzae, Neisseria ,Campylobacter &Identification of isolated unknown bacteria Experiment 12: Introduction to Mycology diagnosis Experiment 13: ELISA, Coomb׳s& Haemagglutination 3 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Qatar University Biomedical Program 5 8 29 33 38 48 60 64 67 71 74 76 91 93 102 106 2 Medical Microbiology BIOM 322 Laboratory Manual Course work details divided into weeks 1. First week: Laboratory safety & sterilization techniques & preparing routine primary isolation media (enriched, selective, differential, nutrient) description for the purpose of each media incubate media (Atmosphere, Temperature, Humidity, Length of incubation) dispensing methods. 2. Second week: The use of blood as differential & selective and enriched & standard inoculation and streaking techniques (swab, loop flaming, streaking for isolation, stab) normal microbial flora of throat & interteeth & skin & nails and hair. 3. Third week: Results of previous section & Differentiate colony morphologies and characterization of human Staphylococcus pathogen (salt tolerance growth & fermentation-colonial pigementation - DNase haemolysis). 4. Fourth week: Results of previous section (colony characteristics size, shape, elevation, form and margin, surface appearance, changes in media) biochemical reactions (catalase, coagulase). Chemical agents of control: Chemotherapeutic agents (novobiocin sensitivity). 5. Fifth week: Results of previous section & Differentiate colony morphologies and characterization of human Streptococcus & Enterococcus & Streptococcus pneumonia (Differentiate common growth characteristics with 5% Sheep Blood agar), Bacitracin test. 6. Sixth week: Results of previous section Differentiate hemolysis alpha beta gamma (none), Differentiate between (Streptococcus viridans & Streptococcus pneumonia) by bile solubility, Inulin fermentation & optochin test. 7. Seventh week: Characterization of Enterobacteriaceae (Lactorse fermenting enteric bacteria E.coli – Klebsiella sp) differentiate common growth characteristics on Mackonckey. 8. Eighth week: Biochemical reactions of L.F (Indole – MR/VP – Citrate utilization) + colonial morphology. Qatar University Biomedical Program 3 Medical Microbiology BIOM 322 Laboratory Manual Characterization of non lactose fermenter (Proteus & Pseudomonas). 9. Nineth week: Colonial morphology of Proteus & Pseudomonas. (Oxidase – Urease tests). Usage of indicators and identification of positive and negative results of IMVC. Characterization of Shigella & Salmonella + TSI test. 10. Tenth week: Identification of different results of TSI test + colonial morphology of Salmonella & Shigella. API – 20E Diagnostic system for Enterobacteriace. Demonstration of the following items: 1. Slides: a- Mycobacterium tuberculosis. b- Clostridium titani. 2. LoffleŕsSerum 3. L.J medium. 4. Cooked meat broth medium. 5. Anaerobic gas packs system. 11. Eleventh week: Campylobacter, Haemophylus influenzae, Neisseria. Scheme of identification of isolated unknown. 12. Twelvth week: Introduction to Mycology diagnosis (classification, taxonomy & morphologic structure). Characterization of Candida albicans (colonial morphology on Sabouraud׳s dextrose agar, Gram stain, Germ test tube and biochemical reactions). Cryptococcus neoformans, Malassezia furfur & Dermatophytes. 13. Thirteen week: ELISA , Coomb´s test, Haemagglutination. Note: There will be a presentation subject on Mycology discussed every week by one or two students presented by power point & on hard copy. Qatar University Biomedical Program 4 Medical Microbiology BIOM 322 Laboratory Manual Course objectives divided according to course work by weeks for Medical Microbiology (BIOM 322) First week: Upon completion of this laboratory, the student will be able to: 1) Descripe and apply with Microbiology Lab Safety Rules. 2) Distinguish different sterilization techniques. 3) Discuss preparation ,classification & utilization of routine primary media. Second week: Upon completion of this laboratory, the student will be able to: 1) Explain the use of differential and selective medium. 2) Identify the normal microbial flora. Third week: Upon completion of this laboratory, the student will be able to: 1) Explain the medical significance of Staphylococci species. 2) Identify laboratory procedures designed to differentiate among the major Staphylococcal species. Fourth week: Upon completion of this laboratory, the student will be able to: 1) Differentiate among major Staphylococcal species utilizing macroscopic, microscopic, biochemical reactions and by chemotherapeutic agents. 2) Explain and perform the disc –agar diffusion technique for determination of different chemotherapeutic agents. Fifth week: Upon completion of this laboratory, the student will be able to: 1) Explain the medical significance of Streptococcal species. 2) Identify laboratory procedures designed to differentiate Streptococci on the basis of their hemolytic activity and biochemical patterns associated with the Lance field group classification. Sixth week: Upon completion of this laboratory, the student will be able to: 1) Differentiate among major Streptococcal species on the basis of their hemolytic activity. 2)Select laboratory procedures that differentiates between Streptococcus pneumoniae and other hemolytic Streptococci . Qatar University Biomedical Program 5 Medical Microbiology BIOM 322 Laboratory Manual Seventh week: Upon completion of this laboratory, the student will be able to: 1) Explain the medical significance of the family Enterobacteriacae . 2) Define lactose fermenter and non lactose fermenter. 3) Identify laboratory procedures used to differentiate between E.coli &Klebsiella (IMVC). Eighth week: Upon completion of this laboratory, the student will be able to: 1) Differentiate between E.coli &Klebsiella according to (IMVC) results. 2) Explain the medical significance of Proteus & Pseudomonas as non lactose fermenter. 3) Identify laboratory procedures used to differentiate between Proteus & Pseudomonas. Ninth week: Upon completion of this laboratory, the student will be able to: 1) Differentiate between Proteus & Pseudomonas according to biochemical reactions results. 2) Explain the medical significance of Salmonella &Shigella . 3) Descripe laboratory procedure for TSI test. Tenth week: Upon completion of this laboratory, the student will be able to: Differentiate various TSI different results. 2) Prform laboratory procedures designed to identify family of Enterobacteriacae using commercial multi test Microsystems. 3) Demonstrate slides of:a) Mycobacterium tuberculosis . b) Clostridium tetani . c) Loffler´s serum medium. d)L.J. medium. e) Cooked meat broth medium. f)Anaerobic gas pack system. Eleventh week: Upon completion of this laboratory, the student will be able to: 1) Explain medical significance of Campylobacter ,Haemophylus influenzae &Neisseriae . 2) Design scheme of identification of isolated unknown organism. Twelveth week: Upon completion of this laboratory, the student will be able to: 1) Explain medical significance of fungi. 2) Identify laboratory procedures used to investigate Candida albicans. Qatar University Biomedical Program 6 Medical Microbiology BIOM 322 Laboratory Manual Thirteenth week: 1) Explain medical significance of Elisa ,Comb's test &haemagglutination test . 2) Identify laboratory procedures to perform these tests and analyze the results . Qatar University Biomedical Program 7 Medical Microbiology BIOM 322 Laboratory Manual Microbiology Lab Safety Safety DO’s: Keep your Safety DONT’s: workbench neat and Place cultures near the edge of the organized. bench. Label all cultures/containers. Mix unknown chemicals. Read Bergey’s Manual to obtain Think that a nice sounding name for information about a new organism. an organism means it harmless. Ask how to discard used cultures. Pour any live culture down the sink drain. Wear your safety glasses at all times. Take off your safety glasses or touch your face with soiled latex gloves . Report accidents to the instructor Attempt to clean up a spill by yourself immediately. or leave the lab to treat an injury by yourself. Take a rest break now and then. Be in a rush to Finish. AN EXPERIMENT DONE WELL IS… AN EXPERIMENT DONE SAFELY. The Microbiology Lab Safety Rules : Hazards exist in the lab for toxic chemicals and microorganisms. Microbes, in particular have a great versatility to grow and proliferate in different environments (i.e. opportunistic pathogens), and thus it is imperative that you conduct yourself safely at all times when in the laboratory. If the lab instructor becomes concerned for your safety, or the safety of others, you will be asked to leave the lab. 1. Note the location for the emergency exits, first aid kit, fire extinguisher, Hand wash station, emergency showers, and eye wash apparatus. Qatar University Biomedical Program 8 Medical Microbiology BIOM 322 Laboratory Manual 2. Do not smoke, eat or drink in the laboratory, or place any object on near your mouth. Keep your books, laboratory manual and workbook at a reasonable distance from your work area. 3. If a fire starts, or the fire alarm sounds, unplug any electrical apparatus and vacate the laboratory in an orderly manner. 4. Practice good aseptic techniques by performing the following before starting each class: (i) Long hair should be tied back. (ii) Wear closed footwear to protect the feet. (iii) Wear a clean lab coat. (iv) Wear protective glasses at all times. (v) Wash your hands thoroughly with soap and water before starting your exercises. (vi) Wear disposable latex gloves when handling blood products (e.g.) whole blood, plasma, serum, etc.). 5. Do not place any hazardous or infectious materials in the sink. Do not dispose of any solid material in the sink. 6. To clean up spills of microbial cultures, first contain the spill by placing a paper towel soaked in 70% ethanol over the spill area. Keep the towel on the spill for 20 minutes. In form your instructor of the spill. Place the towel in an autoclave (biohazard) waste bag provided. Ensure you wash your hands immediately after dealing with the spill. 7. Never place any instruments or materials into your mouth. i.e. Do not pipette by mouth. Use the mechanical apparatus provided. 8. Place pipettes that are used during class immediately into the appropriate waste container. 9. Place used glass slides and cover slips in glass dishes of disinfectant. Do not discard any demonstration slides. 10. Place all used bottles, tubes and cultures in the containers provided on each bench for staff to remove and autoclave. 11. Place contaminated waste in the autoclave bag-lined containers. All other (non-biohazard waste) can be disposed of in approproiately labeled containers. Qatar University Biomedical Program 9 Medical Microbiology BIOM 322 Laboratory Manual 12. All materials requiring incubation or refrigeration must be appropriately labeled and placed on the trays provided. 13. At the conclusion of each class clean the microscope provided for you. Use lens tissue to clean the oil immersion lenses and leave the microscope standing with the low power lens in place. Avoid jolting the microscope. 14. Decontaminate your work bench at the end of each exercise by applying an antiseptic wash. 15. Before leaving the laboratory for a coffee, lunch a nature break, or at the end of the day, wash your hands thoroughly with antiseptic soap and water. Preparing culture media&dispensing As all other living organisms microorganisms require certain basic nutrients and physical factors for continuity of life. Understanding these needs is necessary for successful cultivation of microorganisms in the laboratory. Nutritional needs: These needs are supplied through a variety of media. 1-Carbon: A-Autotrophy: use inorganic carbon in the form of carbon dioxide. B-Heterotrophs: can not be cultivitated in a media contain inorganic compounds, they must be supplied with organic nutrient, primarily glucose. 2- Nitrogen: Essential atom in protein –nucleic acid synthesis. 3-Non metallic element: a-Sulfur containing amino acid. b- Phosphorus: formation of nucleic acid DNA and RNA, ATP. 4-Metalic element: Ca++,Zn+,Na+,K+,Cu++,Mn++,Mg++,Fe+2,3 necessary for performance of varied cellular activities. 5-Vitamins: Contribute to cellular growth and essential in minute conc. For all activities. 6-Water: All cell require water Qatar University Biomedical Program 10 Medical Microbiology BIOM 322 Laboratory Manual 7-Energy: Phototrophs: These use radiant energy. Chemotrophs: These depend on oxidation of chemical compounds as energy source. Physical factors: 1-Temperature: Optimum temp. For enzymatic activities 20-40c. Low temp______________ decrease enzyme activity. High temp.______________Coagulation of enzymes 2-pH of the extra cellular environment: Optimum pH is in the neutral range of 7 either increases or decrease pH will slow down the rate of chemical reactions. 3-The gaseous requirement: O2 in most cells plays a vital role in ATP formation. Classification of media 1- according to the physical state: a- Liquid as: peptone water Nutrient broth b- Solid: Nutrient agar C-Semi solid: 0.5% only agar. 2- According to type of media: a- Simple media: Nutrient broth Nutrient agar. b- Enriched media: blood agar Chocolate agar c- Selective media: (L.J.) Lowenstein Jensen medium - Desoxycholate citrate agar (DCA). - T.C.B.S: for V.cholera. c- Differential (indicator) medium: Mac.conkey: differentiate between lactose fermented &non lactose fermented. e- Sugar media: bacteria vary in sugar fermentation so this media used for differentia. Qatar University Biomedical Program 11 Medical Microbiology BIOM 322 Laboratory Manual Artificial media Media that will be prepared this session are: 1-Nutrient broth 2-Nutrient agar 3-Mac conkey agar: It is composed of: *peptone as a nutrient. *agar as a solidifying agent. *lactose as test sugar. *neutral red as indicator that changes pink in the presence of acid which is produced as result of lactose fermentation. *bile salts inhibit non intestinal bacteria. *it differentiates between lactose fermented &non lactose fermented. Dispensing of the media All used media should be collected as bio hazards autocalved before get rid Preparing Culture Media Necessary skills Knowledge of the metric system of measurement Warning: Never pour liquefied agar media down the drain. They solidify in the pipes. Material : (This exercise is designed to be performed by students working in pairs.): At least 1.5 gm of peptone per pair At least 0.9 gm of beef extrac per pair At least 300 ml of deionized and / or distilled water per pair 1 Test tube per class containing 15 ml of colored water, marked “15 ml control” 1 Test tube per class containing 10 ml of colored water, marked “10 ml control” 1 500 ml Graduated cylinder per group 1 Balance per group 1 500 ml Erlenmeyer flask per pair 1 Tongue depressor per pair 3 Spatulas per pair At least 3 weighing papers per pair Qatar University Biomedical Program 12 Medical Microbiology BIOM 322 Laboratory Manual 1 Hot plate stirrer and magnetic stirring bar; or 1 ring stand, 1 piece of wire gauze, 1 Bunsen burner, and 1 stirring rod per pair 1 Magnetic stir bar retriever par class, if necessary 18 Test tubes per pair, all with equal diameter, at least 16 /150 mm, clean with caps Flask tongs or other devices for handling hot Erlenmeyer flasks 1 Plastic foam stopper per pair, used on flask (optional) 1 Paper bag per pair, used on flask with stopper (optional) 1 Scissors per group to trim bag of foil 1 Piece of aluminum foil per pair to cover mouth and neck of flask instead of stopper and bag 9 Sterile Petri plats per pair Baskets or racks to collect and autoclave slants, broths, and pours prepared by students (labeled “Slants,” ”Broths,” ”Pours”). 1Dispensing apparatus per class; see figure 16.1 Support and base Funnel Support ring elamped to stand Utility clamp Pinchcock clamp Rubber tubing 1 Large container of cool water per class Water baths, 50 oC, (enough surface area to hold 1500 ml Erlenmeyer flask per pair of students. Keep the water level very low so flasks do not float.) Enough slant trays to hold 6 slants per pair pH Equipment (per class): 1 L of 1 M NaOH with pipet and pipettor 1 L of 1 M HCl with pipet and pipettor pH Meter of papers 500 m Bottle of pH 7 buffer solution 10 Beakers, 20 ml Wash bottle of distilled and/or deionized water Box of Kimwipes or other lint-free tissue Labeled containers for storage of media in Petri plates Access to a current DIFCO Manual Access to the Manual of BBL Products and Laboratory Procedures (optional) Qatar University Biomedical Program 13 Medical Microbiology BIOM 322 Laboratory Manual Primary Objective : Prepare broths, slants, and plates of media for use in the microbiology laboratory. Other Objectives: 1. Describe two uses for each form of culture media: solid, semisolid, and liquid. 2. List five functional categories of media; describe the purpose of each and give an example of each. 3. Distinguish between a chemically defined medium and a chemically complex one. 4. Name two commercial sources of dehydrated culture media. 5. Define: infusion, extract, digests. 6. List the basic nutritional requirements of all bacteria. 7. Summarize attributes of agar that make it and adequate solidifying agent for the microbiology laboratory. 8. Wash glassware correctly for culture media preparation. 9. Discuss the advantages of utilizing a hot plate stirrer for preparing culture media. 10. Check the pH of a solution. 11. Explain why Petri plates of media are poured at a holding temperature of about 50 oC instead of 100 oC. 12. Demonstrate knowledge of proper media storage techniques. Introduction For this exercise you prepare, dispense, and sterilize culture media (nutrient solutions) for your own use in later experiments. Classification of Media Microbiological media are solid, semisolid, or liquid, each type of medium has its own uses. For separating bacteria and allowing them to grow into isolated colonies, or for maintaining stock cultures, a solid surface is utilized. To see if bacteria are motile or not, a semisolid medium can be employed. Medical specimens containing bacteria are often transported from the site of collection to the laboratory in semisolid media. Large quantities of microbes are generally cultivated in liquid media. Also, fermentation and other biochemical tests are often performed in tubes of liquid media. Media are categorized by their function. An all purpose medium, such as Tryptic Soy Agar, supports the growth of most bacteria cultured in the laboratory. Selective media inhibit the Qatar University Biomedical Program 14 Medical Microbiology BIOM 322 Laboratory Manual growth of some microbes. Mac-Conkey’s Agar, for example, inhibits gram-positive bacteria. The biochemical products of some bacteria reach with differential media, creating a visible result in the colony or the medium. For example, bacteria that form hydrogen sulfide blacken Triple Sugar Iron Agar. Enrichment media contain nutrients that favor the growth of certain microorganisms. Selenite Broth enriches members of the Salmonella group so that they multiply faster than other fecal organisms and soon outnumber their competitors. Another function of certain specialized media is conveyance, Transport media are designed to deliver living microbes from the collection site to the laboratory. Transport Medium Amies, for example, contains charcoal to adsorb bacterial waste products. This purification helps the organisms survive in transit. Media Ingredients Media are divided into two categories according to their components. If the exact ionic concentration of every chemical in the medium is known, the solution is called a chemically defined or synthetic medium. These media are often expensive and time consuming to prepare; see table 1.1 . More commonly, ingredients such as beef extract and peptone (partially digested protein) are included in nutrient recipes; see table 16.2. Media containing these more natural ingredients are called chemically complex or non-defined. While there are precise recipes for chemically complex media, no one knows the exact concentration of each ion, Na+ or Cl- for example, because this amount varies slightly between batches of natural ingredients. Many dehydrated media – standardized media prepared in large batches, desiccated, bottled, and sold – are available to microbiologists though companies such as DIFCO Laboratories and Baltimore Biological laboratory. Both of these companies publish reference manuals that you investigate to complete this exercise. Before dehydrated media were widely available and occasionally even today, microbiologists prepared their own infusions (substances steeped in water). Extracts (concentrated solvents that have removed active ingredients from animal or vegetable matter). And digests (organic matter made soluble with heat and moisture). Qatar University Biomedical Program 15 Medical Microbiology BIOM 322 Laboratory Manual Table 1. 1 A Chemicallly Delined Medium, Amino Acid Assay Medium (formula per liter) Dextrose 50 gm Guanine hydrochioride 0 02 gm Sodium acetate 40 gm Uracil 0.02 gm Ammonium chloride 6 gm Xanthine 0. 02 gm DL-Alanine 0.4 gm Thiamine hydrochloride 0 .001 gm L-Arginine hydrochloride 0.484 gm Pyridoxine hydrochloride 0. 002 gm Asparagine 0.8 gm Pyridoxamine hydrochloride 0.0006 gm L-Aspartic acid 0.2 gm Pyridoxal hydrochloride 0 0006 gm L-Cystine 0.1 gm Calcium pa^tothenale 0.001 gm L-G!ulamic acid 0. 6 gm Ribollavin 0 001 gm Glycine 0.2 gm Nicotinic acid 0.002 gm L-Histidine hydrochioride 0.124 gm p-Aminobenzoic acid 0.0002 gm DL-Phenylalanine 0 2 gm Biotin 0 000002 gm L-Proline 0-2 gm Folic acid 0.00002 gm DL-Serine 0.1 gm Monopotassium phosphate 1. 2 gm DL-Threonine 0.4 gm Dipotassium phosphate 1. 2 gm DL-Tryptophane 0 08 gm Magnesium sulfate 0 .4gm L-Tyrosine 0.2 gm Ferrous sulfate 0 .02gm DL-Valine 0.5 gm Manganese sulfate 0 .04 gm Adenine sulfate 0. 02 gm Sodium chloride 0 .02 gm 'This medium, available Irom D1FCO Laboialories, is a base for microbiological assay of the ammo acids leucine, methionine, lysine, or isoleucine. From the DIFCO Manual, 10th ed., 1984. DIFCO laboratories. Detroit, Ml 48232. Table 1 .2. A Chemically Complex Medium, Nulrient Agar (formula per 1,000 ml) Beef extract 3 gm Peptone 5 gm Agar 15 gm From the DIFCO manual 10th ed . 1984. DIFCO Laboratories. Detroit. Mi 48232 Qatar University Biomedical Program 16 Medical Microbiology BIOM 322 Laboratory Manual While the nutritional requirements of bacteria vary tremendously between species, all must have water, carbon, an energy source, nitrogen, and minerals including phosphorus, sulphur, and trace elements (metal ions). Frequently, growth factors such as vitamins and nucleosides are also required. And each species has its own optimal pH range. Notice that agar is not listed with the nutritional requirements of bacteria. This is because it almost never supplies nutrients. Very few microorganisms can utilize as a carbon source this complex carbohydrate extracted from red algae. Agar is a solidifying agent used to physically, not nutritionally, support bacterial growth. Performing in low concentrations of less than 2.0%—leaving room for peptones, carbohydrates, dyes, and so on—agar forms a firm, transparent gel with most nutrient solutions. Other attributes of agar also make it an excellent solidifying agent for the microbiology laboratory. Agar liquifies at about 100° C and remains liquified until its temperature falls to about 42° C. Thus microbes can be suspended in warm, liquified medium to separate the cells. After the medium has cooled and solidified, the bacteria can be incubated at temperatures up to 100" C in this same medium. It remains gelled and the microbes, if adequately diluted, may grow into individual, isolated colonies. Preparing Media When you prepare microbiologies media, cleanliness, accuracy, and sterility are your primary concerns. All glass-ware should be thoroughly washed. Use deionized or distilled water for the final rinse. Watch: for cracks that might cause breakage in the autoclave. The balance is a precision instrument for weighing. Whether you employ a small school scale or an analytical balance costing thousands of dollars, carefully observe Your instructor's demonstration of its operation and use the device properly. Remember that you will be measuring small amounts; 1 gram equals about 1/28 of an ounce. For media preparation, use only distilled or deionized water. When preparing agar solutions, utilize a flask that is at least twice the final volume of your recipe. Most ingredients go into clear solution when swirled in cool water. But some, including agar, require boiling. When heating the medium, stir it constantly to prevent scorching the bottom. A hot plate stirrer, which heats your solution while its magnetic stirrer motor spins a tefloncoated magnetic spinbar in your medium, frees you from the time-consuming task of stirring. But check the solution frequently; agar media tend to boil suddenly, overflowing the Qatar University Biomedical Program 17 Medical Microbiology BIOM 322 Laboratory Manual flask and making a mess of the hot plate and bench top. Have a pair of tongs or other device available for quickly removing your boiling solution from the heat source. If you are preparing dehydrated culture media, there is generally no need to check the pH of the solution. It has already been carefully adjusted. Other liquid media should be compared, at about room temperature, to a standardized buffer solution, a liquid with a stable pH that has been adjusted to a set value. Your instructor will demonstrate how to use a pH meter or pH lest papers. Media are dispensed into tubes or flasks before sterilizing, but in the autoclave (a sterilizer employing superheated steam under pressure) media boil-out of Petri dishes. So, plates are poured after autoclaving, utilizing sterile media and sterile Petri dishes. Before pouring plates, the tubes or flasks of media are brought down from boiling to a holding temperature of about 50° C. The tempered medium is easier to handle, and agar at a suitable pouring temperature does not cause excessive condensation to form inside the lid of a Petri plate. When the agar in a Petri dish has cooled sufficiently to solidify, the plates are inverted for storage. In this position any water from condensation helps hydrate the medium. Prepared, dehydrated media are stored at the temperatures indicated on the product description. This information is generally given on the bottle label. The Nutrient Agar you prepare is best stored between 15° and 30° C. Plates are stored upside down. Placing them back into their plastic sleeves or in other moisture-proof containers helps prevent desiccation of the medium. Use the media as soon as possible. PROCEDURES EXERCISE : Preparing Nutrient Broth a* Working in pairs you prepare a total of 300 ml of Nutrient Broth. You add agar to 200 ml of the broth, making Nutrient Agar. You dispense the media as follows; see figure l.2: Broth 10 broths, 10 ml each = 100 ml of broth in 10 lubes Qatar University Biomedical Program 18 Medical Microbiology BIOM 322 Laboratory Manual Agar 2 pours, 15 ml each = 30 ml of agar in 2 tubes (to be poured into 2 Petri plates after autoclaving and tempering) 60 ml ol agar in 6 tubes (to be cooled in a 6 slants, 10 ml each = 60 ml of agr in 6 tubes (to be cooled in a slanted position after autoclaving, as illustrated) 1flask, 110 ml = 110 ml of agar (to be dispensed into 6 or 7 Petri plates after autoclaving and tempering). b* Assemble the ingredients you and your partner need to prepare 300 ml of Nutrient Broth: peptone and beef extract. c* Assemble the equipment you need to apportion the ingredients: graduated cylinder, 500 ml; balance; tongue depressor; two spatulas; weighing papers, two per pair. d* Assemble the necessary glassware and accessories: a 500 ml Erlenmeyer flask and a test tube rack with 18 clean test tubes with closures. All test tubes must be of equal diameter. Qatar University Biomedical Program 19 Medical Microbiology BIOM 322 Laboratory Manual e* If you have access to a hot plate stirrer, you need a magnetic stirring rod. Otherwise, you can employ a standard hot plate or a ring stand and Bunsen burner to heat your medium. f* One liter (1,000 ml) of Nutrient Broth contains 3 gm of beef extract and 5 gm of peptone. How much of each do you need to prepare 300 ml of the medium? Beef extract Peptone Check with your instructor to be sure that your c a l culations are correct. g* Using the 500 ml graduated cylinder, obtain 300 ml of distilled and/or deionized water. Dispense about 100 ml into the Erlenmeyer flask. h* Fold a weighing paper twice. Weigh the weighing paper. Calculate the total of its weight plus the weight of the required peptone. i* Use a clean spatula to dispense the correct amount of peptone onto the paper. Add the powder to the water in your flask. Close the lid of the peptone bottle tightly and return the bottle to the class supply. j* Place a twice-folded weighing paper and then a tongue depressor on the balance. Calculate their total weight plus the weight of the required beef extract. k* Using a clean spatula for assistance, dispense the correct amount of beef extract onto the wooden blade. Add the beef extract to the water in your flask, using the blade and stirring rod to stir it into solution. Close the lid of the beef extract container and return it to the class supply. l* If the extract and powder do not go into solution quickly, heat the solution gently, stirring constantly. m* Mix in the remaining deionized and/or distilled H2O. Qatar University Biomedical Program 20 Medical Microbiology BIOM 322 Laboratory Manual n* If you have heated your solution, rapidly cool it to about 22° C in a container of cool water. o* Then, as demonstrated by your instructor, check the pH of your solution. It should be 6.8 ± 0.2. If necessary, adjust the pH with 1M HC1 and 1M NaOH. p* Pour 100 ml of Nutrient Broth back into your graduated cylinder. q* Using the class dispensing apparatus, pour the 100 ml of broth into 10 tubes, 10 ml each. Be sure all tubes have approximately equal diameters. Match the height of the broth in your tubes to the 10ml control tube of colored water. Cap the tubes of Nutrient Broth. Loosen screw caps one-quarter turn. For sterilization, add your tubes to the class baskets marked "Broths." Note: For sensitive, biochemical tests requiring precisely measured amounts of reactant, media is measured into each test tube with a pipet, syringe, or graduated cylinder. This is not generally required with the growth medium Nutrient Agar. • Follow your instructor's directions regarding return or disposal of the cylinder and other supplies. Preparing and Dispensing Nutrient Agar First Laboratory Session a* Nutrient Agar is prepared with 1.5% agar. You now have 200 ml of Nutrient Broth in an Erlenmeyer flask. How much agar should you add? Collect a jar of agar, a weighing paper, and a clean spatula. b* Check with your instructor to be sure your calculation is correct, then weigh out the appropriate amount of agar onto a twice-folded weighing paper. c* Add the agar to your Nutrient Broth. Return the tightly closed jar of agar to the class set. d* Obtain a magnetic stirrer or a s t i r r i n g rod. Use it to agitate the medium constantly while heating the liquid to boiling over medium heat. Avoid charring the medium with high heat. e* Have a pair of flask tongs, a folded paper towel, or other device handy to remove the Erlenmeyer flask from the heat as soon as the medium boils. f* When the medium boils, remove it from the heat. Qatar University Biomedical Program 21 Medical Microbiology BIOM 322 Laboratory Manual g* Using the class dispensing apparatus, pour about 30 ml of agar into 2 tubes, 15 ml each. Be sure all tubes have approximately equal diameters. Match the height of the agar in your tubes to the 15 ml control tube of colored water. Do not allow Nutrient Agar to cool below 45° C and solidify in the dispensing apparatus. Cap the tubes of Nutrient Agar; loosen screw caps one-quarter turn. For sterilization, add your media to the class baskets marked "Pours." g* Using the dispensing apparatus again, pour about 60 ml of agar into 6 tubes, 10 ml each. Be sure all tubes have approximately equal diameters. Match the height of the agar in your tubes to the 10 ml control tube of colored water. Do not allow cooled, solidified Nutrient Agar to clog the apparatus. Cap the tubes of nutrient Agar; loosen screw caps one-quarter turn. For sterilization, add the tubes to the class baskets marked "Slants." i* Follow your instructor's directions for returning the stirring rod. A magnetic stirrer is autoclavable. It can remain in the bottom of the flask, or you may remove it with a stir bar retriever. j* Cover both the mouth and neck of the flask loosely with aluminum foil or utilize a foam rubber stopper and a trimmed paper bag. Label the flask. Place the flask with the rest of the class media for sterilization. k* Your instructor will see that the Nutrient Agar and Nutrient Broth prepared by the class are autoclaved. l* The instructor will incubate two tubes of non-sterilized Nutrient Broth, one at room temperature and the other at 35° C until the next laboratory session. In your laboratory report, describe what you expect to see in the nonsterilized medium. Second Laboratory Session * Compare the appearance of autoclaved and nonsterilized Nutrient Broths. Note your observations in t h e laboratory report. Utilizing the DIFCO Manual and/or the Manual of BBL Products and Laboratory Procedures (Optional) * While the Nutrient Broth and Nutrient Agar are being sterilized, utilize your laboratory time to familiarize yourself with the DIFCO Manual and/or the BBL Manual of Products and Laboratory Procedures. These standards, culture media reference works are found in Qatar University Biomedical Program 22 Medical Microbiology BIOM 322 Laboratory Manual microbiology laboratories worldwide. Use either or both of the manuals to answer the following questions in your laboratory report. (i) What percentage of agar is included in each of these media: Nutrient Agar, Mueller Hinton Agar, Motility Test Medium, And Fluid Thioglycollate Medium? What is the purpose of each of these media? (ii) What carbon source(s) is/are present in each of these media: Simmons' Citrate Agar, Triple Sugar Iron Agar? Which of these media is chemically defined; which is chemically complex? (iii) What is the final pH of these media: Sabouraud Dextrose Agar, Brain Heart Infusion? Which microbes grow best on each of the two media? (iv) Find and examine the list of pH indicators in your manual(s). Name 5 pH indicators; describe their color changes and pH ranges. List 5 standard culture media, each of which contains a different one of your selected pH indicators. Dispensing Sterile Agar Media * When fluids are removed from the autoclave, they are superheated and may boil over if agitated. Do not jar them. * Place the 2 pours (deeps) and 1 flask in a 50° C water bath. * Place the 6 slants in a slant tray or other device where they tilt at an angle. This allows a large surface area to form. Do not allow the medium to spill out the top of the test tubes. * Take 2 sterile Petri dishes and label the outside of the bottoms (smaller diameter halves) of the plates. Your name, the date, and the type of medium Nutrient Agar). Use care to avoid contaminating the sterile plate. Qatar University Biomedical Program 23 Medical Microbiology BIOM 322 Laboratory Manual * When the pours have cooled to about 50cْ remove 1 from the water bath. You now have about 2 5 minutes before the agar medium solidifies, so work fast . Dry the bottom of the tube so it does not drip .Briefly flame the neck of the test tube. Working with your hands near the flame and your nose away from it, quickly and carefully pour the contents of the tube into the bottom of a sterile, labeled Petri plate. Use the lid of the plate shield the surface of the dish from your breath. Do not allow agar to splash out of the dish. Gently rotate * Gently tilt and rotate the dish so the medium completely covers the surface. Again, avoid splashing. Qatar University Biomedical Program 24 Medical Microbiology BIOM 322 Laboratory Manual *If there are any bubbles on the surface of the medium, burst them quickly with the flame, as in the illustration. Warning: Touch only the base of your Bunsen burner-the stem is hot! *Repeat steps with another tcmpered tube of Nutrient Agar. * Follow your instructor's directions concerning recycling of the empty, used test tubes and closures. * Label the bottoms of an additional 6 or 7 sterile Petri plates. * Obtain a flask of Nutrient Agar cooled to pouring temperature. Wipe the bottom of the flask. * Without touching the mouth of the flask, remove the closure. Briefly flame the lip. Qatar University Biomedical Program 25 Medical Microbiology BIOM 322 Laboratory Manual * Keep the flask tilted from this point on until you have completed pouring all your plates (see the illustration). * If you are right-handed, fill your plates from left to right to avoid scooping air into the flask. While avoiding splashes and working with your hands near the flame and your nose away from it, quickly pour enough agar into a plate to cover its bottom surface almost completely. * After pouring and closing the first plate, and before pouring the next one, gently tilt and rotate the partially filled Petri dish so the agar spreads out over the entire surface. * Repeat the pouring and tilting process until all plates are poured. * Holding the base of your Bunsen burner, quickly flame the surface of any plate with bubbles. * Follow your instructor's directions concerning recycling of the empty, used flask and its closure. * When all plates and tubes of Nutrient Agar have solidified, invert the plates and set the slants in an upright position. Tighten screw caps. Follow your instructor's directions concerning storage of the culture media. You grow bactcria in these agars and broths in future laboratory sessions. Qatar University Biomedical Program 26 Medical Microbiology BIOM 322 Laboratory Manual STERILIZATION Could be divided into: a-physical means 1-heat: a-Dry heat Red heat Hot air oven Incineration B-Moist heat Heat below 100ْc At 100ْc Above 100 cْ (Autoclave) 2-Radiation U.V Ionizing radiation 3-Filtration Membrane filter Vacuum filter Syringe filter Air filter B-Chemical means: 1-Phenol 2-Ethyl alcohol 3-Chlorine 4-Hydrogen peroxide Moist heat Below 100ْc: as in pasteurization of milk 72c for 20 sec At 100ْc: boiling for 10 min. as for glass or partly metals as scalpels, forceps. Qatar University Biomedical Program 27 Medical Microbiology BIOM 322 Laboratory Manual Above 100ْc: The autoclave When water is heated in a closed vessel under pressure the boiling point of water rises above 100ْc.This is the principle of both pressure cooker used for rapid cooking and autoclave. In autoclave water is heated under double atmospheric pressure and the boiling temp is 120ْc. Heating articles at this temp. For 20-30 min. is the most efficient method of sterilization. This is because of: 1-The high temp. It attains. 2-The high penetrating power of steam under pressure. The simple autoclave Is a metal cylinder with a closely fitting lid? The lid is connected to a steam discharge tap, a safety valve and a manometer. Direction for use: 1-Water is placed in the bottom and the articles to be sterilized are placed on top of a perforated tray above the water level and the lid is tightly closed. 2-The safety valve is adjusted to 15 ib. /in2 = double atmospheric pressure. 3-When the steam pressure reaches the desired level (2 atmospheric) the safety valve will allow excess steam to escape. 4-From this point the sterilization timing which is 20-30 min is calculated. 5-Then the heater is turned off, and the autoclave is allowed to cool down before opening the lid. Uses: 1-Sterilization of surgical instruments, bed linen, surgical dressing gowns, cotton, gauze, and for any culture media not destroyed by heat. For best results: 1-Don not over load the autoclave for better penetration of steam and contact with articles. 2-Start timing from the moment the manometer read 2 atmospheric pressure. Use of Differential and Selective Media 3- Don not opens the lid before pressure goes down to atmospheric pressure. To test efficiency: 1- Efficacy of dried bacterial spore killed at 120ْc. 2- Chemical indicator. Qatar University Biomedical Program 28 Medical Microbiology BIOM 322 Laboratory Manual Use of Differential and Selective Medium PURPOSE To become familiar with the use and function of specialized media for selection and differentiation of microrgamsms. PRINCIPLE Numerous special-purpose media are available for functions such as: 1. Isolation of bacterial types from a mixed population of organisms. 2-Differentiation among closely relatcd groups of bacteria on the basis of macroscopic appearance of the colonies and biochemical reactions within the medium. 3. Enumeration of bacteria in sanitary microbioiogy. Such as in water and sewage. And also in food and dairy products. 4. Assay of naturally occurring substanccs such as antibiotics. vitamins. and products of industrial fermentation. 5. Characterization and identification of bacteria by their abilities to produce chemical changes in different media. In addition to nutrients necessary for the growth of all bacteria, special-purpose media contain one or more chemical compounds that are essential for their functional specificity. In this exercise, two types of media will be studied and evaluated. Selective Media: These media are used to select (isolate) specific groups of bacteria. They incorporate chemical substances that inhibit the growth of one type of bacteria while permitting growth of another, thus facilitating bacterial isolation. Qatar University Biomedical Program 29 Medical Microbiology BIOM 322 Laboratory Manual Differential Media : These can distinguish among morphologically and biochemically related groups of organisms. They incorporace chemical compounds that, following inoculation and incubation. produce a characteristic change in the appearance of bacterial growth and/or the medium surrounding the colonies, which permits differentiation.The following media. which are representative of these two types, will be investigated in this exercise: 1. Mannitol salt agar: This medium contains a high salt concentration. 7.5%NaCl. which is inhibitory to the growth of most bacteria other than the Staphylococci. The medium also performs a differential function: It contains the carbohydrate mannitol. Which some Staphylococci are capable of fermenting, and phenol red a pH indicator for detecting acid produced by mannitol-ferminting Staphylococci. These Staphylococci exhibit a yeilow zone surrounding their growth; Staphylococci that do not ferment mannitol will not producc a change in coloration. 2-Blood agar: The blood that is incorporated into this medium is an enrichment ingredient for the cullivation of fastidious organisms such as the Strepcococcus sp. The blood also permits demonstralion, of the hemolytic properties of some microorganisms, particulary the Streptococci, Whose hemolytic activities are classified as: a. Gamma hemolysis: No lysis of red blood cells results in no significant change in the appearance of the medium surrounding the colonies. b. Alpha hemolysis: Incomplete lysis of red blood cells, with reduction of hemoglobin to methemoglobin, results in a greenish halo around the bacterial growth. c. Beta hemolysis: Lysis of red blood cells with complete destruction and use of hemoglobin by the organism results in a clear zone surrounding the colonies. This hemolysis is produced by two types of bela hemolysins, namely Streptolysin O. an antigenic. Oxygen-labile enzyme, and streptolysin S, a nonantigenic, oxygen –stable lysin. The hemolytic reaction is enhanced when blood agar plates are streaked and simultaneously stabbed to show subsurface hemolysis by streptolysin O in an enviroment with reduced oxygen tension. Qatar University Biomedical Program 30 Medical Microbiology BIOM 322 Laboratory Manual 3. MacConkey agar: The inhibitory action of crystal violet on the growth of gram-positive organisms allows for. The isolation of gramnegative bacteria. Incorporation of the carbohydrate lactose, bile salts, and the pH indicator neutral red permits differentiation of enteric bacteria on the basis of their ability to ferment lactose. On this basis, enteric bacteria are separated into two groups: a. Coliform bacilli produce acid as a result of lactose fermentation. The bacteria exhibit a red coloration on their surface. E.coli produces greater quantities of acid from lactose than other coliform species. When this occurs, the medium surrounding the growth also becomes red because of the action of the acid that precipitates the bile salts, followed by absorption of the neutral red. b. Dysentery, typhoid, and paratyphoid bacilli are not lactose fermenters and therefore do not produce acid. The colonies appear uncolored and frequently transparent. Materials Cultures: 24- to 48-hour trypticase soy broth cultures of Enterobacter aerogenes, Escherichia coli, Streptococcus var. Lancefield Group E. Streptococcus mitis. Enterococcus faecalis, Staphylococcus aureus, Staphylococcus epidermidis ,and Salmonella typhimurium. Media: Per designated student group: one each of mannitol salts agar plate, blood agar plate, MacConkey agar plate. Equipment Bunsen burner. inoculating loop, and glassware marking pencil . Procedure: Using the bacterial organisms listed in step 2. Prepare and inoculate each of the plates in the following manner: a. Appropriately label the cover of each plate , as indicated in the section entitled "laboratory Protocol." b. Divide each of the Petri dishes into the required number of sections (one section for each different organism) by marking the bottom of the dish. Label each section with the name of the organism to be inoculated as illustrated in Figure 2.1 Qatar University Biomedical Program 31 Medical Microbiology BIOM 322 Laboratory Manual c. Using sterile technique, inoculate all plates, except the blood agar plate. with the designated organisms by making a single line of inoculation of each organism in its appropriate section. Be sure to close the Petri dish and flame the inoculating needle between inoculations of the different organisms. Refer to Figure 2.1 for an illustration of this procedure. d. Using sterile technique. inoculate the blood agar plate as described in step J c. Upon completion of each single line of inoculation. use the inoculating loop and make three or four stabs at a 45° angle across the streak. 2. Inoculate each of the different media with the following: a. Mannitol salts agar: S. aureus, S. epidermidis. Group E, and E. coli. b. Blood agar: E. faecalis. S. mitis.and Streptococcus viridans. Lancefield Group E. c. MacConkey agar: E. coli, E. aerogenes. S. typhimurium. and S. aureus. 3.. Incubate the plates in an inverted position for 24 to 48 hours at 37°C. Qatar University Biomedical Program 32 Medical Microbiology BIOM 322 Laboratory Manual Microbial flora of teeth, throat, skin, nail&hair Microbial flora of the throat and skin include: normal flora -pathogenic flora *Normal flora: are heterogeneous population of micro-organisms that inhabit the skin and mucous membrane of healthy person. They consist of: 1-The resident flora which are relatively fixed types of bacteria and regularly found in a given area. 2-The transient flora are derived from the environment they may remain for hours, days, or weeks but don't become permanently established. Function of normal flora: 1-They perform importana metabolic functions e.g: a-Synthesis of vitamin K. b-Conversion of bile pigment and bile acids. c-Absorbtion of nutrients from the intestine. 2-They inhibit colonization and infection by pathogenic bacteria(bacterial antagonism). Factors which can disturb the normal flora: 1-Anti-microbial agents which lead to super-infection. 2-obstruction 3-Hormonal changes. **Under certain conditions flora or commensal bacteria may cause disease and are considered potential pathogen. Normal flora of skin e.g: Staphylococci(S.epidermidis),Streptococci(α-haemolytic,non haemolytic). Normal flora of upper respiratory tract e.g: Staphylococci,Streptococci . Pathogenic microbial flora: It is the micro-organism which infect the skin and m.m and cause diseases e.g Staphaureus &Beta haemolytic streptococci . Why we use blood agar for growing of microbial flora of throat: It is enriched media has high nutritive value ,it is an indicator media it can help in identifying bacteria by their haemolytic action on red cell either the alpha –hemolytic &beta –haemolytic reactions of some Streptococci& Staphylococci . Qatar University Biomedical Program 33 Medical Microbiology BIOM 322 Laboratory Manual Respiratory pecimens Throat Specimens A. Selection. Success with culture or with direct antigen detection depends on firmly and completely sampling an area of the inflamed throat. 1. Using a tongue blade to hold the tongue down, look at the back of the throat and the tonsillar area for localized areas of inflammation and exudate. 2. These areas are the most productive for producing cultures of the etiologic agents of acute pharyngitis. B. Collection l. Materials a. Dacron or calcium alginate swab and transport medium b. Tongue blade 2. Method a. Carefully but firmly rub the swab over several areas, of exudate or over the tonsils and posterior pharynx (Fig. 19). Figure 19. Firmly sampling only the inflamed areas of the throat and tonsils and avoiding other oral sites will enhance detection of etiologic agents. Qatar University Biomedical Program 34 Medical Microbiology BIOM 322 Laboratory Manual 1. Working with isolated, pure colonies from your TSA plates, Inoculate the Significant media that you selected and prepared in Activity 2. 2. Label your subcultures carefully, and incubate them at 37ْC for 48 hours or the appropriate time for the specific tests that you are doing. After incubation, gather your data, and record them in a self-designed table on the worksheet for this module. Draw a conclusion from these data as to the genus and species of your two significant throat organisms, if present. Submit these names in the appropriate place on your worksheet. Once again, it would be to your advantage to complete this module to the best of your ability in preparation for unknowns. Related Experience If you isolate normal flora organisms only, it is strongly recommended that you identify them. Phonetic Pronunciation Neisseria meningitidis = ny-seer'-ee-uh muh-nin-juh-ty'-dis Haemophilus influenzae = hee-mof-uh-Ius in-fioo-en'-zee Bordetella pertussis = borduh-tel!' -uh per-tuss' – is Specimen Collection and Processing b. Do not touch the cheeks, teeth, or gums with the swab as you withdraw it from the mouth. c. Insert the swab back into its packet, and crush the transport medium vial in the transport container. C. Labeling 1. Label the swab container with patient identification data, including the time of collection. 2. Note any antimicrobial agents currently being taken by the patient. 3. Note whether the specimen is for culture or direct antigen detection. Indicate whether it is for throat culture or a streptococcus screen. 4. Indicate the suspected pathogen if other than streptococci, e.g., N.gonorrhoeae. Qatar University Biomedical Program 35 Medical Microbiology BIOM 322 Laboratory Manual D. Transport 1. Transport the swab to the laboratory as soon as possible. 2. If transport is to be delayed beyond I h, refrigerate the swab. E. Comments 1. A streptococcus screen (culture) will test for and report only the presence or absence of beta-hemolytic Streptococci, including group A. A throat culture will, in addition to revealing group A Streptococci, reveal other Beta-hemolytic streptococci, Haemophilus spp., and significant numbers of other potential respiratory pathogens, including Streptococcus pneumoniae. Pseudomonas aeruginosa, Staphylococcus aureus, or other suspected pathogens as agreed upon by the users. 2. Beta-hemolytic streptococci are routinely identified and reported. They are the primary cause of acute bacterial pharyngitis and need not be tested, for succeptibility to antimicrobial agents. . 3. Haemophilus spp. may be reported in pediatric patients when requested, although they are part oi the normal flora in children and adults. 4. Throat culture for N. gonorrhoeae is available on request, but the laboratory must be alerted to the request. 5. Routine susceptibility testing is not routinely done on any isolate from the Throat, although a screen for methicillin-resistant S. aureus (MRSA) may be requested if the carrier state for MRSA is suspected. Qatar University Biomedical Program 36 Medical Microbiology BIOM 322 Laboratory Manual Name ------------------------------------Lab Section -----------------------------Experiment 3 throat culture: Activity 2 Gram stains reaction and cell arrangement of the predominating organism(s): ------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------Activity 3 Significant media used Results Blood agar -------------------------------------------------------------------------------Chocolate agar --------------------------------------------------------------------------Mac Conkey and / or EMB -----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------Other Tests performed -----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------Genus of predominating organism isolated: ---------------------------------------- Qatar University Biomedical Program 37 Medical Microbiology BIOM 322 Laboratory Manual Identification of Human Staphylococcal Pathogens PURPOSE To become familiar with 1. The medical significance of the Staphylococci 2. .Selected laboratory, procedures designed to differentiate among the major staphylococcal species. PRINCIPLE The genus Staphylococcus is composed of both pathogenic and nonpathogenic organisms. They are gram-positive cocci and occur most commonly as irregular clusters or spherical cells. They are mesophilic non-spore-formers; however, they are generally highly resistant to drying, especially when sequestered in organic maller such as blood Pus, and tissue fluids. They are capable of surviving outside of the body for extendcd periods of time, even up to several months. Many Staphylococci are indigenous to skin surfaces and mucous membranes of the upper respiratory tract. Breaks in the skin and mucous linings may serve as portals of entry into underlying tissues, with the possibility of infection by virulent strains. The three major species include S. aureus, S. saprophyticus , and S. epidermidis. Strains of the last two species are generally avirulent: however, under special circumstances in which a suitable portal of entry is provided, S. epidermidis may be the etiological agent for skin lesions and endocarditis, and S. saprophyticuS has been implicated in some urinary tract infections. Infections are primarily associated with S. aureus pathogenic strains that are often responsible for the formation of abscesses, locailzed pus-producing lesions. These lesions most commonly occur in the skin and its associated structures, resulting in boils, carbuncles, acne, and impetigo. Infections of internal organs and tissues are not uncommon, however, and induce pneumonia, osteomyelitis (abscesses in bone and bone marrow), endocarditis (inflammation of the endocardium), cystitis (inflammation or the ulinary bladder), pyelonephritis inflammation of the kidneys). Staphylococcal enteritis due to enterotoxin contamination or foods, and, on occasion, septicemia. Strains of S. aureus produce a variety of metabolic end products, some of which may play roles in the organisms' pathogenicity. Included among these are coagulase, which causes clot formation: leukocidin, which lyses white Qatar University Biomedical Program 38 Medical Microbiology BIOM 322 Laboratory Manual blood cells: hemolysins, which are active against red blood cells, and enterotoxin, which is responsible for a type of gastroenterilis. Additional metabolites of a nontoxic nature are DNase, lipase, gelatinase, and the fibrinolysin staphylokinase. When there is a possibility or staphylococcal infection. isolation of S. aureus is of clinical importance. These virulent strains can be differentiated from other staphylococci and identined by a variety of laboratory tests, some of which are illustrated in Table 3.1 Table 3.1 Laboratory tests for differentoation of staphylococcal species Test S.aureus S.epidermidis S.saprophyticus Growth + + + Fermentation + - - Colonial pigmentation Generally golden White White Mannitol salt agar yellow Coagulase + - - Dnase + - - Hemolysis Generally beta - - Novobiocin sensitivity Sensitive Sensitive Resistant In this exercise you will distinguish among the staphylococcal species by traditional test procedures both. The traditional and computer-based procedures are described below. The traditional procedures involve the following steps: 1. Mannitol salt agar: This medium is selective for salt-tolerant organisms such as staphylococci. Differentiation among the staphylococci is predicated on their ability to ferment mannitol Following incubation. Mannitol fermenting organisms, typically S. aurerus strains, exhibit a yellow halo surrounding their - growth, and non fermenting strains do not. 2. Coagulase test: Production of coagulase is indicative of an S. aureus strain. The enzyme acts within host tissues to conven fibrinogen to fibrin. It is theorized that the fibrin meshwork that is formed surrounds the bacterial cells or infected tissues, protecting the organism from nonspecific host resistance mechanisms such as phagocytosis and the antistaphylococcal Qatar University Biomedical Program 39 Medical Microbiology BIOM 322 Laboratory Manual activity of normal serum. In the coagulase tube test for bound and free coagulase, a suspension of the test organism in citrated plasma is prepared and the inoculated plasma is then periodically examined for fibrin formation, or coagulation. Clot formation within 4 hours is interpreted as a positive result and indicative of a virulent S. aureus strain. The absence of coagulation after 24 hours of incubation is a negative result, indicative of an avirulent strain. 3. Deoxyribonuclease (DNase) test: Generally. coagulase-positive staphylococci also produce the hydrolytic enzyme DNase thus this test can be used to reconfirm the identification of S. aureus. The test organism is grown on an agar medium containing DNA Following incubation. DNase activiry is detemined by the addition of 1N HCL to the surface of the agar. DNase-positive cultures capable of DNA hydrolysis will show transluecense around the area of growth. The absence of this halo is indicative of a negative result and the inability of the organism to produce DNase. 4. Novobiocin sensitivity: This test is used to distinguish S. epidirmidis from S. sapro- phticus It requires inoculation or a Mueller Hinton agar plate with the test organism And application of a 30-ug novobiocin antibioric disc to the surrace of the agar. Following incubation. The sensitivty of an organism to the antibiotic is determined by the Kirby Bauer method . A computer-assisted procedure is the STAPH IDENT system (developed by Analytab Products division or Sherwood Medical, Plainview, NewYork). STAPH-IDENl is a rapid, computer-based micromethod for the separation and identification of the newly proposed 13 species of staphylococci. The system consists of ten microcupules containing dehydrated substrates for the performance of conventional and chromagenic tests. The addition of a suspension of the test organism serves to hydrate the media and to initiate the biochemical reactions. The identification of the staphylococcal species is made th the aid of the differential charts or the API STAPH-IDEINT Profile Register that is part of the system 'Table 3.2), or both. Qatar University Biomedical Program 40 Medical Microbiology BIOM 322 Laboratory Manual Materials Cultures: 24 hour trypticase Soy agar Slant cluture of Staphylococcus epidermidis. Staphylococcus saprophyticus (ATCC 15305) and Staphylococcus aureus (ATCC e 27660) 24-hour blood agar cultures of the above arganisms for the STAPH-IDENT system. Media: Per designated student group: three mannitol salt agar plates, one deoxyriboncleic acid agar plate, three Mueller – Hinton agar plates, and the STAPH-IDENT svstem Reagents: Citrared human or rabbit plasma, 1n HCL, and McFarland barium sulfate standards. Equipment: Bunsen burner. Inoclating loop 13× 100 mm test tubes, sterile Pasteur pipetles, 1-m1 sterile pipettes. mechanical pipettes, mechanical pipetting device sterile cotton swabs. 30-ug novobiocin antibiotic discs glassware marking pencil. Forceps and beaker with 95% alcohol. Qatar University Biomedical Program 41 Medical Microbiology BIOM 322 Laboratory Manual Table 3.2 API S"7"APH-IDENT Profile Register Profile Identification P rofil e Identification 0040 STAPH CAPITIS 3560 STAPH HYICUS (An) 0060 STAPH HAEMOLYTICUS 3601 STAPH SIMULANS 0100 STAPH CAPITIS o 140 STAPH CAPITIS 0200 STAPH COHNII 4060 0240 STAPH CAPITIS 4210 STAPH SClURI 0300 STAPH CAPITIS 4310 STAPH SClURI 0340 STAPH CAPITIS 4420 STAPH HAEMOLYTICUS 0440 STAPH HAEMOLYTICUS 4440 STAPH HAEMOLYTICUS 0460 STAPH HAEMOLYTICUS 4460 STAPH HAEMOLYTICUS 0600 STAPH COHNII 4610 STAPH SClURI 0620 STAPH HAEMOLYTICUS 4620 STAPH HAEMOLYTICUS 0640 STAPH HAEMOLYTICUS 0660 STAPH HAEMOLYTICUS 1 000 STAPH EPIDERMIDIS 1 040 STAPH EPIDERMIDIS 1 300 NOVO S STAPH SAPROPHYTICUS NOV STAPH HAEMOLYTICUS STAPH HAEMOLYTICUS 4700 STAPH AUREUS COAG+ STAPH SClURI COAG- 4710 STAPH SClURI STAPH AUREUS 5040 STAPH EPIDERMIDIS 1 540 STAPH HYICUS (An) 5200 STAPH SClURI 1 560 STAPH HYICUS (An) 5 210 STAPH SClURI COAG+ 5300 STAPH AUREUS COAG- 2000 STAPH SAPROPHYTICUS STAPH SClURI NOVO R NOVO S STAPH HOMINIS 5310 STAPH SClURI 2001 STAPH SAPROPHYTICUS 5600 STA?H SClURI 2040 STAPH SAPROPHYTICUS 5610 STAPH SClURI NOVO R COAG+ STAPH HOMINIS 5700 STAPH AUREUS NOVO S COAG- 2041 STAPH SIMULANS STA?H SClURI 2061 STAPH SIMULANS 5710 STAPH SClURI 2 141 STAPH SIMULANS 5740 STAPH AUREUS 2 161 STAPH SIMULANS 2201 STAPH SAPROPHYTICUS 6001 STAPH XYLOSUS ARA+ XYL+ 2241 STAPH SIMULANS STAPH SAPROPHYTICUS ARA- XYL- 2261 STAPH SIMULANS 6 011 STAPH XYLOSUS 2341 STAPH SIMULANS 6021 STAPH XYLOSUS 2361 STAPH SIMULANS 6 101 STAPH XYLOSUS STAPH HOMINIS 6 121 STAPH SAPROPHYTICUS 6221 2 400 Qatar University STAPH XYLOSUS Biomedical Program NOVO S NOVO R 42 Medical Microbiology BIOM 322 Laboratory Manual 2401 STAPH SAPROPHYTICUS 6300 STAPH AUREUS 2421 STAPH SIMULANS 6301 STAPH XYLOSUS 2441 STAPH SIMULANS 6311 STAPH XYLOSUS 2461 STAPH SIMULANS 6321 STAPH XYLOSUS 2541 STAPH SIMULANS 6340 STAPH AUREUS COAG+ 2 561 ST.:l.PH SIMULANS STAPH WARNER COAG- 2601 STAPH SAPROPHYTICUS 6400 2611 STAPH SAPROPHYTICUS 6401 2661 STAPH SIMULANS 2721 STAPH COHNII (SSP1) 6421 STAPH XYLOSUS 2741 STAPH SIMULANS 6460 STAPH WARNERI 2761 STAPH SIMULANS 6501 6521 STAPH WARNERI STAPH XYLOSUS ARA+ XYL+ STAPH SAp.ROPHYTICUS ARA- XYL- STAPH XYLOSUS 3000 STAPH E?IDERMIDIS 6600 STAPH WARNERI 3040 STAPH EPIDERMIDIS 6601 STAPH SAPROPHYTICUS ARA- XYL- STA.PIi XYLOSUS ARA+ XYL+ 3 140 STAPH EPIDERMIDIS 3540 STAPH HYICUS (An) 6611 STAPH XYLOSUS 3541 5TAPH INTERMEDIUS(An) 6621 STAPH XYLOSUS Qatar University Biomedical Program 43 Medical Microbiology BIOM 322 Laboratory Manual Tabe, 3.2 (continued) PROFILE Identification Profile Identification 6700 STAPH AUREUS 7421 ST.APH XYLOSUS 6701 STAPH XYLOSUS 7 501 STAPH INTERMEDIUS (An) 6721 STAPH XYLOSUS 6731 STAPH XYLOSUS STA:PH 7000 EPIDERMIDIS STAPH ,XYLOSUS 7521 S"'APH XYLOSUS 7541 SAPH INTERMEDIUS (An) 7560 STAPH HYICUS (An) 7021 STAPH XYLOSUS 7601 STAPH XYLOSUS 7040 STAPH EPIDERMIDIS 7621 STAPH XYLOSUS 7 141 STAPH INTERMEDIUS(An) 7 63'1 STAPH XYLOSUS 7300 STAPH AUREUS 7700 STAPH AUREUS 7321 STAPH XYLOSUS 7701 STAPH XYLOSUS 7340 STAPH AUREUS 7721 STAPH XYLOSUS 7401 STAPH XYLOSUS 7740 STAPH AUREUS PROCEDURE I. Preparation of DNA agar plate culture: a. With a glassware marking pcncil divide the bottom of the plate into three sections. Label each section with the name of the organism to be inoculated. b. Aseptically make a single line of inoculation of each test organism in its respective sector on the agar plate. 2. Preparation of agar plate cultures for novobiocin sensitivity dctermination: a. Label the three Mueller-Hinton agar plates with the name of the test organism to be inoculated. Inoculate each plate with its respectivc organism according to the Kirby-Bauer procedure. b. Using alcohol-dipped and named forceps. Aseptically apply a novobiocin antibiotic disc to the surface of each inoculated plate. Gently press the discs down with sterile forceps to ensure that they adhere to the agar surface. Qatar University Biomedical Program 44 Medical Microbiology BIOM 322 Laboratory Manual 3. Preparation of mannitol salt agar plate cultures: Aseptically make a single line of inoculation of each test organism in the center of the appropriately labeled agar plates. 4. Incubate all plate cultures in an invrted position for 24 to 48 hours at 37ْC 5. Coagulase test procedure: a. Label three 13 x 100 mm test tubes with the name of the organism to be inoculated. b. Aseptically add 0.5 ml of a1:4 dilution of citratcd rabbit or human plasma a 0.1 ml of each test culture to its appropriately labeled test tube. c. At the end of the laboratory session incubate all tubes that are coagulase-negative for 20 hours at 37°C. 6. STAPH-1DETNT system procedure: a. Preparation of strip: i. Dispense: 5 ml of tap water into incubation tray ii. Place API strip in incubation tray. b. Preparation of inoculum: i. Add 2 ml of 0.85% saline (pH 5.5-7.0) 10 a sterile 15 x I50-mm test tube. ii. Using a sterile swab pick up a sufficient amount of inoculum to prepare a saline suspension with a final turbidity that is equivalent to a No. 3 McFarland (BaS04) turbidity standard. Caution: Be sure to use suspension within 15 minutes of preparation. c. with a sterile Pasteur pipette add 2 or 3 drops of the inoculum to each micro- cupule. d. Place plastic lid on tray and incubate for 5 hours at 37°C. OBSERVATIONS AND RESULTS 1. Examine the bacterial plasma suspensions for clot .formation 5 minutes, 20 minutes. 1 hour, and hours after inoculation by holding the test tubes in a standered position. Place all coagulase negative suspensions in an incubator at 37ْC for observation 24 hours after inoculation. Record vour observations and results in the chart. Qatar University Biomedical Program 45 Medical Microbiology BIOM 322 Laboratory Manual Staphylococcal Appearance of plasma clotted (+) or Unclotted (-) Coagulase Species 5 min (+) or (-) 20 min 1 hr 4 hr. 24 hr. s. aureus s. epidermidis s. saprophyticus 2. Examine the mannitol salt agar plate. Note and record the following in the chart: a. Presence (+) or absence (-) of growth of each test organism. b. Color of the medium surrounding the growth of each test organism. c. Whether each test organism is a mannitol fermentcr (+) or nonferrnenter (-). 3. Flood the DNA agar plate with 1N HCL . Observe for the delayed development of transluesent clear area surrounding the growth of each test organism. Record your color observation and indicate the presence (+) or absence (-) of DNase activity in the chart. 4. with a metric ruler measure the size of the zone of inhibition. If present surrounding each of the novobiocin discs on the agar plates. A zone of inhibition of 17 mm or less is indicative of novobiocin resistance. Whereas a zone greater than 17mm indicates that the organism is sensitive to this antibiotic. Record in the chart the susceptibility of each test organism to novobiocin as sensitive (S) or resistant (R). Refer to photo for illustration of the reactions : Procedure S. aureus S. epidermidis S.sapraphyticus -------------------------------- -------------------------------- ---------------------------- -------------------------------- -------------------------------- ---------------------------- -------------- -------------- ------------------- -------------------------------- -------------------------------- ---------------------------- -------------------- -------------------- ---------------------- -------------------------------- -------------------------------- ---------------------------- -------------------- -------------------- ---------------------- Mannitol salt agar Growth Color of medium Fermentation DNA agar Calor of medium DNase activity Novobiocin sensitivity Growth inhibition in mm Susceptibility-(R) or (S) Qatar University Biomedical Program 46 Medical Microbiology BIOM 322 Laboratory Manual 5. Interpret your STAPH-IDENT system reacrions on the basis of the observed color .changes in each of the microcupules described in the chart below. Record your color observation and result as (+) or (-) for each test in this chart. Microcupule No 1 PHS Interpretation of Reactions Reaction Results Substrate Positive Negative Color P-nitrophenyi- Yellow Clear phosphate or straw (+) or (-) – colored Disodium salt 2 3 URE GLS Urea p-nitrophenyl – B-D- Purple to red – Yellow orange orange Yellow Clear or glucopyranoside MNE Mannose Yellow yellow 5 MAN Mannitol orange 6 TRE Trehalose 7 SAL Salicin 8 GLC p-nitrophenyl B-D- Yellow glucuronide 9 10 ARG NGP Arginine yellow Straw – colored 4 – or Red or orange Clear or straw – colored Purple to red – Yellow or yellow – orange orange 2- naphthyl – B-D Add 1-2 drops of STAPH-IDENT galactopyranoside reagent Plum-purple Yellow or colorless (mauve) Qatar University Biomedical Program 47 Medical Microbiology BIOM 322 Laboratory Manual 6. Construct a four-digit profile for your unknown organism as follows: A four-digit profile is derived from the results obtaind with STAPH-IDENT. The 10 biochemical tests are divided into four groups as follows: PHS MNE SAL URE MAN GLC GLS TRE ARG NGP Only positive reacactions are assigned a numcrical value. The valuc depends on the location within the group. A value of I for the first biochemical in each group (i.e. PHS, MNE . . .) A value of 2 for the second biochemical in each group (i.e. URE. MAN . . .) Avalue of 4 for the third biochemical in each group (i.e. GLS. TRE . . .) Avalue Of 0 for all negative reactions. Chemical Agents of Control: Chemotherapeutic Agents Chemotherapeutic agents are chemical substances used in the treatment of infectious diseases, Their mode of action is to interfere with microbial metabolism, thereby producing a static or cidal effect on the microorganisms, without producing a like effect in host cells. These drugs can be separated into two categories: 1. Antibiotics are synthesized and secreted by some true bacteria. Actinomycetes, and fungi that destroy or inhibit the growth of other microorganisms . Today, some antibiotics are laboratory synthesized or modified; however, their origins are living cells. 2. Synthetic drugs are synthesized in the laboratory To determine a therapeutic drug of choice. One must know its mode of "action possible adverse side effects in the host, and the scope of its antimicrobial activity. The specific mechanism of action varies among differem drugs, and the short-term or long-term use of many drugs can produce systemic side effects in the host. These vary in severity from mild and temporary upsets to permanent tissue damage (Table 11.1) Qatar University Biomedical Program 48 Medical Microbiology BIOM 322 Laboratory Manual SYNTHETIC AGENTS: Antibiotic Penicillin Mode of Action Possible Side Effects Prevents transpeptidation of the N-acetyl muramic acids, producing a weakened Penicillin resistance; sensitivity (allergic reaction) peptidoglycan structure. Streptomycin Has an affinity for bacterial ribosomes, causing misreading of codons on mRNA, May produce damage to auditory nerve,causing deafness thereby interfering with protein synthesis Chloramphenicol Has an affinity for bacterial ribosomes, preventing between peptide amino bond acids formation during protein May cause aplastic anemia. which is fatal because of destruction of RBCforming and WBC-forming tissues synthesis Tetracyclines Have an affinity for bacterial ribosomes; prevent hydrogen bonding between the Permanent discoloration of teeth in young children anticodon on the tRNA-amino acid complex and the codon on mRNA during protein synthesis Bacitracin Inhibits cell-wall synthesis Nephrotoxic if taken internally; used ror topical application only Polymyxin Destruction of cell membrane Toxic if taken internally; used for topical application only Sulfadiazine (sulfonamide) produces a static effect on a wide range of microorganisms by mechanism of action called competitive inhibi-tion. The active component or the drug. sulfanilamide, acts as an antimetabolite that competes with the essential metabolite, p-aminobenzoic acid (PABA), during the synthesis of folic acid in the microbial cell. Folic acid is an essential cellular coenzyme involved in the synthesis of amino acids and purines. Many microorganisms possess enzymatic pathways for folic acid synthesis and can be adversely affected by sulfonamides. Human cells lack these enzymes, and the essential folic acid enters the cells in a preformed state . Table 11.1 Prototypic Antibiotics Qatar University Biomedical Program 49 Medical Microbiology BIOM 322 Laboratory Manual Therefore these drugs have no competitive effect on human cells. The similarity between the chemical structure of the antimetabolite sulfanilamide and the structure of the essential metabolite PABA is illustrated in Figure 11.1 PART A: THE KIRBY-BAUER ANTIMICROBIAL SUSCEPTIBILITY TEST PROCEDURE: PURPOSE To become acquainted with the Kirby-Bauer procedure for the evaluation of the antimicrobial activity of chemotherapeutic agents. PRINCIPLE The available chemotherapeutic agents vary in their scope of antimicrobial activity. Some have a limited spectrum of activity, being effective against only one group of microorganisms. Others exhibit broad-spectrum activity against a range of microorganisms. The drug susceptibilities of many pathogenic microorganisms are known, but it is sometimes necessary to test several agents to determine the drug of choice. A standardized filter-paper disc-agar diffusion procedure, known as the Kirby-Bauer method, is frequently used to determine the drug susceptibility of microorganisms isolated from infectious processes (Figure 11.21) This method allows for the rapid determination of the efficacy of a drug by measuring the diameter of the zone of inhibition that results from diffusion or the agen into the medium surrounding the disc. In this procedure, filter-paper discs of uniform size are impregnated with specified concentrations of different antibiotics and then Qatar University Biomedical Program 50 Medical Microbiology BIOM 322 Laboratory Manual placed on the surface of an agar plate that has been seeded with the organism to be tested. The medium of choice is Mueller-Hinton agar, with a pH of 7.2 to 7.4, which is poured into plates to a uniform depth of 5 mm and refrigerated on solidification. Prior to use, the plates are transferred to an incubator at 37ْC for 10 to 20 minutes to dry off the moisture that develops on the agar surface. The plates are then heavily inoculated with a standardized inoculum by means of a cotton swab to ensure the confluent growth of the organism. The discs are aseptically applied to the surface of the agar plate at well-spaced intervals. Once applied, each disc is gently touched with a sterile applicator stick to ensure its firm contact with the agar surface. Following incubation, the plates are examined for the presence of growth inhibition, which is indicated by a clear zone surrounding each disc. The susceptibility of an organism to a drug is determined by the size of this zone, which itself is dependent on variables such as: 1. The ability and rate of diffusion of the antibiotic into the medium and its interaction with the test organism. 2. The number of organisms inoculated. 3. The growth rate of the organism. 4. The degree of susceptibility of the organism to the anribiotic. A measurement of the diameter of the zone of inhibition in millimeters is made and its size is Qatar University Biomedical Program 51 Medical Microbiology BIOM 322 Laboratory Manual Compared to that contained in a standardized chart, which is shown in Table 11.2 Based on this comparison, the test organism is determined to be resistant. intermediate. or susceptible to the antibiotic. MATERIALS Cultures 0.85% saline suspensions of Escherichia coli. Staphylococcus aureus, Pseudomonas aeruginosa, Proteus vulgaris, Mycobaccerium smegmatis, Bacillus cereus, and Encerococcus faecalis adjusted to an O.D. of 0.1 at 600 mμ. Note: For enhanced growth of M. smegmacis, add Tween 80 (1 ml/liter broth medium) and incubate for 3 to 5 days in a shaking water bath, if available. Media Per designated student group: seven Mueller-Hinton agar plates. Antimicrobial Sensitivity Discs Penicillin-G, 10 ug , streptomycin, 10 ug: tetracycline, 30 ug; chloramphenicol, 30 ug; gentamicin, 10 ug; vancomycin, 30 ug and sulfanilamide, 300 ug. Equipment Sensi-disc dispensers or forceps,Bunsen burner, sterile cotton swabs, glassware marking pencil, and millimeter ruler. PROCEDURE I. Place agar plates right side up in an incubator heated to 37°C for 10 to 20 minutes with the covers adjusted so that the plates are slightly opened. 2. Label the covers of each of the plates with the name of the test organism to be inoculated. 3. Using sterile technique, inoculate all agar plates with their respective test organisms as follows: a. Dip a sterile cotton swab into a well-mixed saline test culture and remove excess inoculum by pressing the saturated swab against the inner wall of the culture tube. b. Using the swab streak the entire agar surface horizontally ,vertically and around the outer edge of the plate to ensure a heavy growth over the entire surface. Qatar University Biomedical Program 52 Medical Microbiology BIOM 322 Laboratory Manual 4. Allow all culture plates to dry for about 5 minutes.6 5. Using the Sensi-disc dispenser, apply the antibiotic discs by placing the dispenser over the agar surface and pressing the plunger, depositing the discs simultaneously onto the agar surface. If dispensers are not available, distribute the individual discs at equal distances with forceps-dipped in alcohol and flamed. 6. Gently press each disc down with the wooden end of a cotton swab or sterile forceps to ensure that the discs adhere to the surface of the agar. Do not press the discs into the agar. 7. Incubate all plate cultures in an inverted position for 24 to 48 hours at 37°C. Qatar University Biomedical Program 53 Medical Microbiology BIOM 322 Laboratory Manual The clindamycin disk is used for testing susceptibility to both clindamycin and lincomycin. Resistant strains of S .aureus ododuce b-lactamase and the testing of the 10-unit penicillin G disk is preferred. Penicillin G should be used to test the susceptibility of all penlclllinasesensitive penicillins. such as ampicillin, amoxacillin, azlocillin, bacampicillin, hetacillin, carbenicillin, meziocillin, piperacillin, and ticarcillin. Results may also be applied to phenoxymethyl penicillin or phenethicillin. For enterococci, aerococci, and non-enterococcal streptococci, the designation "moderately susceptible" implies the need for high dose penicillin or ampicilin for endocarcitis and serious invasive tissue infections that may require (always for enterococci) combined therapy with an aminoglycoside (gentamicin for improved therapeutic response and bactericidal action. Non enterococcal streptococci should have an MIC determined 10 case of endocarditis. Urinary isolates should be considered to be susceptible to ampicillin or penicillin alone. Ampicillin/sulbactam, azteronam, cefotetan, ceftazidime. ceftriaxone. and imipenem are among the most recently studied beta Iactams having a separate diagnostic disk and a generally wider spectrum of antimicrobial aetivity. Specialy against gram-negative bacilli when compared to previously approved cephalosporins such as cephalothin. The Cefazolin test results may not accurately predict susceptibility to other first-generation cephalosporins. Cephalothin should be tested instead to represent cephalothin. cefaclor (except for Haemophifus). cephapirin. cephradine. cephalexln. and cefadroxiI. S.aureus Strains exihibting resisrance to one of the pemcillinase-resistant penicillins (MRSA) must be reported as resistant to cephalosporins and other newer β -lactams such as amoxicillin /clavulanic acid, Ampicillinis/ sulbactam. imipenem and ticarcillin/clavulanic acid, regardless of in vitro rest results. This is primarily because in most cases of documented MRSA Infection, the patient has resoonded poorly to the cephalosporin therapy or convincing clinical data has yet to be derived confirming clinical efficacy (clavulanic acid or sulbactam combinations and imipenem). Methicillin-resistant, coagulase -negative Stapylococcus spp. also appears not to respond well to the above cited drugs. Qatar University Biomedical Program 54 Medical Microbiology BIOM 322 Laboratory Manual PART B: SYNERGISTIC EFFECT OF DRUG COMBINATIONS: PURPOSE To become acquainted with the disc-agar diffusion technique for determination of synergistic combinations of chemotherapeutic agents. PRINCIPLE Combination chemotherapy, the use of two or more antimicrobial or antineoplastic agencs, is being employed in medical practice with ever -increasing frequency. The rationale for using drug combinations is the expectation that effective combinations might lower the incidence of bacterial resistance, reduce host toxicity of the antimicrobial agents (because of decreased dosage requirements), or enhance the agents' bactericidal activity. Enhanced bactericidal activity is known as synergism. Synergistic activity is evident when the sum of the effects of the chemotherapeutic agents used in combination significantly greater than the sum of their effects when used individually. This result is readily differentiated from an additive (indifferent) Effect, which is evident when the interaction of two drugs produces a combined effect that is no greater than the sum of their separately measured individual effects. A varietv of in vitro methods are available to demonstrate synergisric activity. In this experiment a disc-agar diffusion technique will be performed to demonstrate this phenomenon. This technique uses the Kirby-Bauer antibiotic susceptibility test procedure, as descriped in Part A of this experiment, and requires both MuellerHinton agar plates previously seeded with the test organisms and commercially prepared, antimicrobial-impregnated discs . The two discs, representing the drug combination, are placed on the inoculated agar plate and separated by a distance (measured in mm) that is equal to or slightly greater than one-half the sum of their individual. Qatar University Biomedical Program 55 Medical Microbiology BIOM 322 Laboratory Manual Zones of inhibition when obtained separately. Following the incubation period, an additive effect is exhibited by the presence of two distinctly separate circles of inhibition. If the drug combination is synergistic, the two inhibitory zones merge to form a "bridge" at their juncture, as illustrated in Figure 11.3 the drug combinations to be used in this experimcntal procedure are: 1. Sulfisoxazolc, 150 μg, and trimethoprim, 5 μg. Both antimicrobial agents are enzyme inhibitors that act scquentially in the metabolic pathway leading to folic acid synthesis. The antimicrobial effect of each drug is enhanced when the two drugs are used in combination. The pathway thus exemplifies synergism. PABA Folate synthetase inhibited by sulfisoxazole Dihydrofolic reductase Dihydrotolic acid inhibited by trimethoprim Tetrahydrofolic acid 2. Trimethoprim 5μg, and tetracycline, 30 μg. The modes of antimicrobial activity of these two chemotherapeutic agents differ; tetracycline acts to interfere with protein synthesis at the ribosomes. Thus, when used in combination, these dnigs produce an additive effect. MATERIALS Cultures 0.85% saline suspensions of Escherichia coli and Staphylococcus aureus adjusted to anO.D. of 0.1 at 600 mμ. Media Per designated student group: four Mueller-Hinton agar plates. Antimicrobial Sensitivity Discs Tetracycline, 30 μg, trimethoprim, 5 μg; and sul- fisoxazole, 150 μg . Qatar University Biomedical Program 56 Medical Microbiology BIOM 322 Laboratory Manual Equipment Bunsen burner, forceps, sterile, cotton swabs, millimeter ruler, and glassware marking pencil. PROCEDURE 1. Inoculation of Mueller-Hinton agar plates: Follow steps 1 through 4 as described under the procedure in Part A of this experiment. 2. Using the millimeter ruler, determine the center of the underside of each plate and mark with a glassware marking pencil. 3. Using the glassware marking pencil, mark the underside of each agar plate culture at both sides from the center mark at the distances specified below a. E.coli--inoculated plate for trimethoprim and sulfisoxazole combination sensitivity: 12.5 mm on each side of center mark. b. S.aureus-inoculated plate for trimethoprim and sulfisoxazole combination sensitivity 14.5 mm on each side of center mark. . c. E. coli and S.aureus inoculated plates for trimethoprim and tetracycline combination sensitivity: 14.0 mm on each side of center mark. 4. Using sterile forceps, place the antimicrobial discs, in the combinations specified in step3, onto the surface of each agar plate culture at the previously marked positions. Gently press each disc down with the sterile forceps to ensure that it adheres to the agar surface. 5. Incubate all plate cultures in an inverted position for 24 to 48 hours at 37°C Qatar University Biomedical Program 57 Medical Microbiology BIOM 322 Laboratory Manual OBSERVATIONS AND RESULTS Part A: Kirby-Bauer Antimicrobial Susceptibility Test Procedure I. Examine all plate cultures for the presence or absence of a zone of inhibition surrounding each disc. 2. Using a ruler graduated in millimeters, carefully measure each zone of inhibition to the nearest millimeter and record your results in the chart. 3. Compare your results with Tablel1.2 and indicate in the chart the susceptibility or each test organism to the chemotherapeutic agent as resistant (R). intermediate (1), or sensitive (S). Refer to photo number 30 in the color-plate insert for illustration of this reaction. Chemotherapeutic Gram – Negative Agent E.coli Zone size p.aeruginosa Susceptibility Zone Susceptibility size p.vulgaris Zone Susceptibility size M. smegmatis Zone Susceptibility size Penicillin Streptomycin Tetracycline Chloramphenicol Gentamicin Vancomycin Sulfanilamide Chemotherapeutic Agent Gram Positive S. aureus Zone size E. faecalis B. cereus Susceptibility Zone Susceptibility Zone Susceptibility size size Penicillin Streptomycin Tetracycline Chloramphenicol Gentamicin Vancomycin Sulfanilamide Qatar University Biomedical Program 58 Medical Microbiology BIOM 322 Laboratory Manual 4. for each of the chemotherapeutic agents, indicate: a: The spectrum of its activity as broad or limited. b. The type or types of organisms it is effective against as gram-positive, gram-negative, or acid fast. Chemotherapeutic Spectrum of Activity Types (s) of Microorganisms agent Penicillin Streptomycin Tetracycline Chloramphenicol Gentamicin Vancomycin Sulfanilamide Part B: Synergistic Effect of Drug Combinations Examine all agar plate cultures to determine the zone of inhibition patterns exhibited. Distinctly separate zones of inhibition are indicative of an additive effect, whereas a merging of the inhibitory zones is indicative of synergism. Record your observations and results in the chart. Refer to photo number 29 in the color-plate insert for illustration of these reactions. Cultures Appearance of zone of Synergistic inhibition additive Effect or E. coli: Trimethoprim and sulfisoxazole trimethoprim and tetracycline S. aureus: Trimethoprim and sulfisoxazole trimethoprim and tetracycline Qatar University Biomedical Program 59 Medical Microbiology BIOM 322 Laboratory Manual Identification of Human Streptococcal athogens PURPOSE: To become familiar with 1. The medical significance of streptococci. 2. Selected laboratory procedures designed to differemiate streptococci on the basis of their hemolytic activity and biochemical patterns associated with the Lancefield group classifications. PRINCIPLE: Members of the genus Streptcococcus are perhaps responsible for a greater number of infectious diseases than any other group of microorganisms. Morphologically , they are cocci that divide in a single plane forming chains, They form circular translucent to opaque pinpoint colonies on solid media. All members of this group are gram -positive and many are nutritionally fastidious requiring enriched media such as blood for growth. The streptococci are classified by means of two major methods: (1) their hemolytic activity and (2) the serologic classification of Lancefield. The observed hemolytic reactions on blood agar are of the following three types: 1. (α) Alpha-hemolysis, an incomplete form of hemolysis, produces a green zone around the colony. Alpha-hemolytic streptococci, the Screpcococcus viridans species, are usually nonpathogenic opportunists, In some instances however, they are capable of inducing human infections such as subacute endocarditis, which may precipitate valvular damage and heart failure if untreated. Strepcococcus pneumoniae, the causative agent of 1obar pneumonia, will be studied in a separate experiment. 2. (β) Beta-hemolysis, a complete destruction of red blood cells, exhibits a clear zone of approximately two to four times the diameter of the colony. The streptococci capable of producing beta-hemolysins are most frequemly associated with pathogenicity. 3. (γ) Gamma-hemolysis is indicative of the absence of any hemolysis around the colony, most commonly, gamma-hemolytic streptococci are avirulent. Qatar University Biomedical Program 60 Medical Microbiology BIOM 322 Laboratory Manual Lancefield classified the streptococci into groups, designated A through 0, based on the presence of an antigenic group-specific hapten called the C-substance. This method of classification generally implicates the members of Groups A, B, C, and D in human infectious processes. Beta-hemolytic streptococci belonging to Group A, and collectively referred to as Streptococcus pyogenes, are the human pathogens of prime importance. Members of this group are the main etiological agents of human respiratory infections such as tonsillitis, bronchopneumonia, and scarlet fever as well as skin disorders such as erysipelas and cellulitis. In addition, these organisms are responsible for the development of complicating infections, namely glomerulonephritis and rheumatic fever, which may surface when primary streptococcal infections either go untreated or are not completely eradicated by antibiotics. The beta-hemolytic streptococci found in Group B are indigenous to the vaginal mucosa and have been shown to be responsible for puerperal fever (childbirth fever), a sometimes-fatal neonatal meningitis, and endocarditis. Members of Group C are also beta-hemolytic and have been implicated in erysipelas, puerperal fever, and throat infections. Group D streptococci generally exhibit alpha- or gamma-hemolysis on blood agar plates. This group includes .theenterococci such as S. faecalis (now reclassified as Enterococcus- faecalis), which may be the etiological agent of urinary tract infections, and the nonenterococci such as S. bovis, which is of lesser medical significance in humans. The virulence of the streptococci is associated with their ability to produce a wide variety of extracellular metabolites. Included among these are the hemolysins (alpha and beta), leucocidins that destroy phagocytes, and theerythrogenic toxin responsible for the rash of scarlet fever, Also of medical significance are the metabolites hyaluronidase (the spreading factor), which hydrolyzes the tissue cement hyaluronic acid; streptokinase, a fibrinolysin; and the nucleases, ribonuclease and deoxyribonuclease, which destroy viscous tissue debris. The last three metabolic end products facilitate the spread of the organisms, thereby initiating secondary sites of streptococcal infection. Although the different groups or streptococci have similar colonial morphology and microscopic appearance, they can be separated and identified by the perfonnance of a variety of laboratory tests. Toward this end, you will perfonn laboratory procedures to differentiate among the medically significant streptococci on the basis of their Lancefield group classification and their hemolytic patterns. Table 4.1 will aid in this separation. Identification of Group A streptococci involves the following procedures: Qatar University Biomedical Program 61 Medical Microbiology BIOM 322 Laboratory Manual 1. Bacitracin test: A filter-paper disc impregnated with 0.04 unit of bacitracin is applied to the surface of a blood agar plate previously streaked with the organism to be identified, Following incubation, the appearance of a zone of growth inhibition surrounding the disc is indicative of Group A streptococci. Absence of this zone suggests a non-Group A organism. Hemolytic activity is identified with a blood agar medium, The pathogenic streptococci, primarily the beta- hemolytic, can be separated from the generally avirulent alpha- and gamma -hemolytic streptococci by the type of hemolysis produced on blood agar as previously described. MATERIALS: Cultures: 24-hour blood agar slant cultures of Streptococcus pyogenes (ATCC 12385), Enterococcus faecalis and Streptococcus viridans . Media: Per designated student group: three blood agar plates. Equipment: Bunsen burner inoculating loop, staining tray, lens paper, bibulous paper, microscope, sterile canon swabs, glassware marking pencil PROCEDURE: 1. Prepare a Gram stain preparation of each streptococcal culture and observe under oil immersion. Record in the chart your observations of cell morphology and Gram reaction. Qatar University Biomedical Program 62 Medical Microbiology BIOM 322 Laboratory Manual 2. Prepare the blood agar plate cultures to identify the type of hemolysis as follows: a. With a glassware marking pencil, Write on the bottoms of blood agar plate to accommodate test organism, Label it with the name of the culture to be inoculated. b. Using sterile inoculating technique, make line streak of inoculation of each organism in its respective blood plate. 3. Prepare the blood agar plate cultures for the bacitracin test as follows: a. With a glassware marking pencil, label the cover of blood agar plate with the names of the organisms to be inoculated S. pyogenus . b. Using a sterile cotton swab, inoculate the agar surface of the plate with its respective test organism by streaking first in a horizontal direction, then vertically to ensure a heavy growth over the entire surface. c. Using alcohol-dipped and flamed forceps apply a single O.04-unit bacitracin disc to the surface of each plate; gently touch the disc to ensure its adherence to the agar surface. Qatar University Biomedical Program 63 Medical Microbiology BIOM 322 Laboratory Manual Identification of Streptococcus pneumoniae PURPOSE: To become familiar with laboratory procedures to differentiate between Streptococcus pneumoniae and other alpha-hemolytic streptococci. PRINCIPLE: The pneumococcus Streptococcus pneumoniae is the major etiological agent of lobar pneumonia, an infection characterized by acute inflammation of the bronchial and alveolar membranes. These organisms are gram-positive cocci. tapered or lancet-shaped at their edges , that occur in pairs or as short , tight chains, The large thick capsules formed in vivo are responsible for antiphagocytic activity; which is believed to enhance the organisms' virulence. In addition the pneumococci produce alpha-hemolysis on blood agar plates. Because of these properties (short-chain formation, alpha-hemolysis. and failure of the capsule to stain on Gram staining) the organ- isms closely resemble Streptococcus viridans species. The S. pneumoniae can be differemiated from other alpha-hemolytic streptococci on the basis of the following laboratory tests: Test S. pneumoniae S. mitis Hemolysis α α Bile solubility + - Optochin + - Inulin fermentation + - Brief descriptions of the tests and their mechanisms follow: 1. Bile solubility test: In the presence of surface-active agents such as bile and bile salts (sodium desoxycholate or sodium dodecyl sulfate), the cell wall of the pneumococcus undergoes lysis. Other members of the alpha-hemolytic streptococci will not be lysed by these agents and are bile-insoluble. Following incubation bile-soluble cultures will appear clear; bile-insoluble cultures will be turbid. Qatar University Biomedical Program 64 Medical Microbiology BIOM 322 Laboratory Manual 2. Optochin test: This is a growth inhibition test in which 6-mm filter-paper discs impregnated with 5 mg of ethylhydrocupreine hydrochloride (optochin) and called P-discs are applied to the surface of a blood agar plate streaked with the test organisms. The S.pneumoniae being sensitive to this surface-active agent, are lysed with the resultant formation of a zone of inhibition greater than 15 mm surrounding the P-disc. Nonpneumococcal alpha-hemolytic streptococci are resistant to optochin and fail to show a zone of inhibition or produce a zone less than 15 mm. 3. Inulin fennentation: The pneumococci are capable of fermenting inulin. while most other alpha-hemolytic streptococci are inulin-nonfermenters. Following incubation, the acid resulting from inulin fenT1entation will change the color of the culture from red to yellow. Cultures that are not capable of fermenting inulin will not exhibit a color change. which is a negative test result organisms. MATERIALS: Cultures: 24-hour blood agar slant cultures of Streptococcus pneumoniae and Srreptococcus viridan. Media: Per designated student group: One blood agar plate, two phenol red inulin broth tubes, and four 13 x .75-mm tubes containing 1 ml of nutrient broth. Reagents: Crystal violet, Gram's iodine, ethyl alcohol, safranin, methylene blue, 10% sodium desoxycholate, commercially available Taxo P-discs (5 mg of optochin) . Equipment: Bunsen burner, inoculating loop, sterile cotton swabs. sterile I-ml serological pipettes , mechanical pipetting device, 95%alcohol in beaker, forceps, and glassware marking pencil. PROCEDURE: I. Bile solubility test a. Label two nutrient broth tubes S. pneumoniae and two other tubes S.viridans b. Aseptically add 2 loopsful of the test organisms to the appropriately labeled sterile test tubes to affect a heavy suspension. Qatar University Biomedical Program 65 Medical Microbiology BIOM 322 Laboratory Manual c. Aseptically add 0.5 ml of sodium desoxycholate to one tube of each test culture. The remaining cultures will serve as controls. d. Incubate the tubes in a water bath at 37°C for 1 hour. 2. Optochin test: a. With a glassware marking pencil, divide the bottom of a blood agar plate into two equal sections and label one section S. pneumoniae and the other S. viridans . b. Using a sterile cotton swab, heavily inoculate the surface of each section with its respective test organism in a horizontal and then vertical direction, being careful to stay within the limits of each section. c. Using an alcohol-dipped and flamed forceps, apply a single Taxo P-disc (optochin) to the surface of the agar in each section of the inoculated plate. Touch each disc slightly to ensure its adherence to the agar surface. d. Incubate the plate in an inverted position for 24 to 48 hours at 37°C. 3. Inulin fennentation test: a. Label two phenol red inulin broth tubes with the name of each test organism to be inoculated. b. Using sterile technique and loop inoculation, inoculate each experimental organism in its appropriately labeled tube of medium. c. Incubate the tube cultures for 24 to 48 hours at 37°c . Qatar University Biomedical Program 66 Medical Microbiology BIOM 322 Laboratory Manual Characterization of lactose fermenting enteric bacteria Members of the family Enterobacteriacea are Gram –ve bacilli 3-5μ by 0.5μ .They are divided into two groups according to their effect on lactose. The lactose fermenters: are collectively called "Coli forms" and include E.coli, Klebsiella, and Citrobacter. The non lactose fermenters: Salmonella, Shigella, Proteus, Pseudomonas. E.coli These are normal inhabitants of intestine of man and animals however, some can cause disease in man. Morphology: Gram –ve bacilli, motile. Cultural characters: Aerobes and facultative anaerobes, they grow on simple media. ON Macconkey medium they give rose- pink colonies due to lactose fermentation. Biochemical activity: They ferment glucose, lactose, maltose, mannite, sucrose, with production of acid and gas. Qatar University Test E.coli Indole test +ve V.P. - ve M.R +ve Citrate test - ve Biomedical Program 67 Medical Microbiology BIOM 322 Laboratory Manual Klebsiella 27 serotype according to capsular polysaccharide. Morphology: Gram – ve bacilli, non motile, and capsulated. Cultural characters: Pink colonies on Macconkey colonies are mucoid due to extra cellular slime in abundant amount. Test Klebsiella Indole test -ve V.P. + ve M.R. - ve Citrate test + ve Qatar University Biomedical Program 68 Medical Microbiology BIOM 322 Laboratory Manual Carbohydrate Fermentation: Glucose fermentation: Depends on the varying ability of bacteria to ferment sugars with acid production which may or may not evolve gas. Experiment: growing the organism in fluid medium composes of peptone water to which a sugar is added in 1% conc. Results: Pink if acid is produced +ve result. Yellow -ve result. Indole test: Demonstrate the ability of certain bacteria to decompose the amino acid tryptophane present in peptone to Indole. Experiment: 1- Inoculate the organism in peptone water and after incubation for 24 h. At 37ْc . 2- Kovac´s reagent or Ehrlich´s reagent is added. 3- If pink ring is produced the organism is Indole +ve. 4- If yellow ring is produced it is Indole – ve. MRVP: Vogues- Proskaur´s reaction: Some bacteria ferment glucose with production of acetyl methyl carbinol. Exp.: Growing bacteria on glucose phosphate peptone then concentrated potassium hydroxide is added if an eosin –pink colour is produced it means positive results. Methyl red test (MR): This test is done to detect the ability of some bacteria to produce large amounts of acid on fermentation of glucose thus lowering the PH of the medium below 4. Qatar University Biomedical Program 69 Medical Microbiology BIOM 322 Laboratory Manual Exp: Growing the organism on glucose phosphate peptone . Incubate at 37 ْc for 48h. . Few drops of the Methyl red indicator are added. +ve test → bright red colour. - ve test → yellow colour. Qatar University Biomedical Program 70 Medical Microbiology BIOM 322 Laboratory Manual Characterization of non lactose –fermenting organisms Proteus Are found in stools of man and animals, they cause wound infection, otitis media&UTI. Two important species are Proteus vulgaris &Proteus mirabilis. Morphology: Gram –ve bacilli, very pleomorphic, highly motile, and non capsulated. Cultural characters: Nutrient agar: they give colonies which swarm in successive waves. Macconkey: Compact pale non –lactose fermenting colonies are formed. Biochemical activities: Urease test +VE Ferment glucose VE+ Indole test VE+ M.R. VE+ V.P. VE- Pseudomans Ps. Aeruginosa is the commonest human pathogen of the pseudomonas group. It is found in soil, sewage some are commensals others cause UTI wound infection and otitis media. The organism is highly resistant to antibiotics and cause chronic infection in low immune person. Qatar University Biomedical Program 71 Medical Microbiology BIOM 322 Laboratory Manual Morphology: Gram –ve bacilli, motile non capsulated and non sporing. Nutrient agar: aerobes leading to greenish discolouration of the medium due to its diffuse exopigment pyocyanin and fluoricin. Mac conkey:pale non-lactose fermenting colonies are formed. Biochemical activities: Ferment glucose -VE Oxidase test VE+ VP VE - MR VE- Urease test: Some organisms e.g. Proteus produce urease enzyme which split urea with the release of ammonia it causes alkalinity and increase pH of the surrounding medium. Expirement: Growing the organism on a medium containing urea and phenol red indicator urease +ve organisms will turn the medium deep pink after 24 hours. Oxidase test: Some bacteria e.g. Neisseria,Vibrio,Pseudomonas produce oxidase enzyme.the later can reduce the oxidase reagent (tetra methyl-p-phenylene- diamine hydrochloride) to a deep purple colour. Qatar University Biomedical Program 72 Medical Microbiology BIOM 322 Laboratory Manual Expirement: The test is done by picking up a portion of the colony tested and smearing it on a strip filter paper impregnated with oxidase reagent (1% freshly prepared) the immediate development of a deep purple colour indicate a + ve test. Qatar University Biomedical Program 73 Medical Microbiology BIOM 322 Laboratory Manual Characterization of Salmonella&Shigella There are more than 2000 serotypes within genus Salmonella, four of them S.typhi, S.paratyphi A ,B , S, C, cause enteric fever in man other species cause Salmonella food poisoning in man. Morphology: Gram –ve bacilli, motile, non capsulated. Cultural characters: Aerobes and facultative anaerobes grow on nutrient agar and Macconkey produce pale non – lactose fermenting colonies. Biochemical activities: The triple sugar iron (TSI) agar test: Used to differentiate between Entero bacteriaceae on the basis of carbohydrate fermentation and hydrogen sulphide production. TSI agar slants: 1) Contain lactose and sucrose 1% conc. 2) Acid base indicator phenol red which changes from orange to yellow in presence of acids. 3) The slant is inoculated by means of a stab- and streak procedure. Result with Salmonella: Alkaline slant (red) Acid butt (yellow) H2S produce black colour. Only glucose fermentation has occurred acid produced on the slant surface is oxidized rapidly. In the butt the acid reaction is maintained because of reduced O2 tension and slower growth of organism. H2S production is determined by Sodium thiosulfate which is added to the medium determined by blacking in the butt. Because of precipitation of insoluble ferrous sulphide. Shigella Morphology: Gram –ve bacilli non motile non capsulated. Cultural characters: They produce pale non- lactose fermenting colonies on Macconkey Qatar University Biomedical Program 74 Medical Microbiology BIOM 322 Laboratory Manual Biochemical activities: TSI: alkaline (red) &acid butt (yellow) no H2S. Only glucose fermentation has occurred. Qatar University Biomedical Program 75 Medical Microbiology BIOM 322 Laboratory Manual Identification of Enteric micro –organisms using Computer –Assisted Multi test Micro system API -20 Several multitest systems have been developed for differentian and identification of members of the Enterobacteriaceae they use micro techniques that incorporate a number of media in single unit. It employs plastic strip Composed of 10&20&32 individual micro tubes, each contain dehydrated medium in the bottom and an upper cupule. The media become hydrated during inoculation of a suspension of the test organism .The strip is then incubated in a plastic covered tray to prevent evaporation.Following incubation identification of the organism is made by using differential charts supplied by the manufacturer. We must noticed that underlined test is anaerobic must be covered by sterile oil. Test surrounded by U the cupule must be full above the level. Certain test ex. Need special reagents e.g. INDOLE, VP. Following incubation you will make your identification by: 1- The traditional method of noting characteristic color changes and interpreting them according to manufacturer instructions. a-The 21 test are divided into seven groups of three each. b-A value of 1 is assigned to the 1 st+ve test in each group. c-A value of 2 is assigned tu the 2nd +ve test in each group. d-A value of4 is assigned to the 3rd +ve test in each. E-A 7-Digit tulmber is obtained by totaling the +ve values of each of the seven groups of three this number is located in the analytical profile index to identify the organism. 2- The computer assisted method called (mini API). MiniAPI: Theory: I-Spectrophotometric. 2-Nephlometric. 3- Turbidmetry They are colorimetric methods. It is used for assesment of: I-Certain enzyme reaction e.g. urease. 2-Break down of certain intermediate e.g. Indole. Qatar University Biomedical Program 76 Medical Microbiology BIOM 322 Laboratory Manual 3- Turbidity: ability to grow in certain medium e.g. Citrate. 4-Substrate changes e.g. sugar break down& acid production. 5-Biosynthesis of certain intermediates such as metabolism of nitrate. Data handling in this machine depend on: Coloremetric+ Mathematical models. Advantatge: I-Minimal storage space. 2- The use of less media. 3-Minimize time to obtain results. 4-The applicability of results to a computerized system for identification of organism. Disadvantatge: I-Difficulty in obtained a standardized inoculum. 2-Presence of air bubbles during insertion of the sample. PURPOSES: 1. To become familiar with the members of, the family Enterobacteriaceae. 2. To become familiar with laboratory procedures designed to identify enteric pathogens using commercial multi test microsystems. INTRODUCTION: The Enterobacteriaceae are a significant group of bacteria that are endogenous to the intestinal tract or that may gain access to this site via a host's ingestion of contaminated food and water. The family consists of a number of genera whose members vary in their capacity to produce disease. The Salmonella and Shigella are considered to be pathogenic. Members of other genera, particularly Escherichia and Enterobacter and to a lesser extent Klebsiella and Proteus, constitute the natural flora of the intestines and are generally considered to be avirulent. Remember, however, that all can produce disease under appropriate conditions. The Enterobacteriaceae are gram-negative, short rods. They are mesophilic, nonfastidious organisms that multiply in many foods and water sources. They are all non-spore-formers and susceptible to destruction by common physical and chemical agents. They are resistant to destruction by low temperatures and Can therefore frequently survive in soil, sewage, water, and many foods for extended periods of time.From a medical point of view, Qatar University Biomedical Program 77 Medical Microbiology BIOM 322 Laboratory Manual the pathogenic Emerobacteriaceae are salmonellae and shigellae. Salmonellae are responsible for enteric fevers, typhoid and milder paratyphoid and gastroenteritis. In typhoid Salmonella typhi penetrates the intestinal mucosa and enters the blood stream thus infecting organs such as the gall bladder, intestines, liver, kidney, spleen, and heart. Ulceration of the intestinal wall caused by the release of the lipopolysaccharide endotoxin into the blood over a long febrile period, and en-teric symptoms are common. Gastroenteritis is caused by a number of Samonella species. Symptoms associated wirh this type of food poisoning include abdominal pain, nausea, vomiting, and diarrhea which develop within 24 hours of ingestion of contaminated food and last for several days. Several Shigellae are responsible for shigellosis, bacillary dysentery that varies in severity, Ulceration of the large iniestine explosive diarrhea, fever, and dehydration occur in the more severe cases. Isolation and identification of enteric bacteria from feces, urine, blood and fecally contaminated materials are of major importance in diagnosis of enteric infections. Although the Enterobacteriaceae are morphologically a like and in many ways metabolically similar, laboratory procedures for the identification of these bacteria are based on differences in biochemical activities. In the past, several multiest systems have been developed for differentiation and identification of members of the Enterobacteriaceae. They use microtechniques that incorporate a number of media in a single unit. At least six multi test systems are commercially available. The obvious advantages of these units are the need for minimal storage space, the use of less media, the rapidity with which results may be obtainedand the applicability of the results to a computerized system for identification of oganisms, There are also certain disadvantages with these systems,including difficulty in obtaining the proper inoculum size since some media require heavy inoculation while others need to be lightly inoculated, the possioility of media carryover from one compartment to another, and the possibility of using inoculum of improper age. Despite these difficulties, when properly correlated with other properties such as Gram srain and colonial morphology on specialized solid media, these systems are acceptable for the identification of Enterobacteriaceae. The most frequently used systems are discussed. Qatar University Biomedical Program 78 Medical Microbiology BIOM 322 Qatar University Laboratory Manual Biomedical Program 79 Medical Microbiology BIOM 322 Laboratory Manual ENTEROTUBE MULTITEST SYSTEM AND ENCISE ІІ : The Enterotube Multitest System (Roche Diagnostics, Hoffmann-La Roche, Inc., Nutley, New Jersey) consists of a single tube containing 12 compartments (Figure 8.2) and a self enclosed inoculating needle. This needle can touch a single isolated colony and then in one operation be drawn through all 12 compartments, thereby inoculating all of the test media. In this manner, 15 standard biochemical tests can be performed in one inoculating procedure. Following incubation, the color changes that occur in each of the compartments are interpreted according to the manufacturer's instructions to identify the organisms. This method has been further refined to permit identification of the enteric bacteria by means of a computer assisted System called ENCISE (Enterobacteriaceae numerical coding and identification system for enterotube). Qatar University Biomedical Program 80 Medical Microbiology BIOM 322 Laboratory Manual API (ANALYTICAL PROFILE INDEX) SYSTEM The API-20E (Analytab Products 1nc. Plainview,New York) Employs a plastic strip composed of 10 individual microtubes, each containing a dehvdrated medium in the bottom and an upper cupule as shown in Figure 8.3 . The media become hydrated during inoculation of a suspension of the test organism, and the strip is then incubated in a plastic-covered tray to prevent evaporation. In this manner 22 biochemical tests are performed. Following incubation, identification of the organism is made by using differential charts supplied by the manufacturer or by means of a computer-assisted system called PRS (profile recognition system). PRS includes an API coder profile register, and selector. In the following experiment you will inoculate an Enterotube and an API strip with an unknown enteric organism. Following incubation, you wiII make your identification by two methods: (1) The traditional method of noting the characteristic color changes and interpreting them according to manufacturers' instructions. (2) The computer-assisted method illustrated in Figure 8.4. MATERIALS: Cultures: Number- coded. 24-hour trypticase soy agar streak plates of Escherichia coli, Salmonella typhimurium, Klebsiella pneumoniae, Enterobacter aerogenes, Shigella dysenteriae, and Proteus vulgaris. Media: Per designated student group: One Enterotube ІІ one API-20E strip, and one 5-ml tube of 0.85% sterile saline. Qatar University Biomedical Program 81 Medical Microbiology BIOM 322 Qatar University Laboratory Manual Biomedical Program 82 Medical Microbiology BIOM 322 Laboratory Manual Reagents: Sterile mineral oil 10% ferric chloride, Kovac's reagent, V-P reagent for API sestem, nitrate reduction reagents, Barritt's reagent (V-P test reagent for Enterotube system), 1.5% hydrogen peroxide, and 1 % p-aminodimethylanaline oxalate (oxidase reagent). Equipment: Bunsen burner, inoculating loop, 5-ml pipette, mechanical pipetting device, sterile Pasteur pipettes, glassware marking pencil, API profile recognition system and differential identification charts, and Enterotube ENClSE pads and color reaction charts. PROCEDURE: API-20E System 1. Familiarize yourself with the components of the system: Incubation tray, lid, and the strip with its 20 microtubes. 2. Label the elongated flap on-the incubation tray with your name and the number of the unknown culture supplied by the instructor. 3. With a pipette, add approximately 5 ml of tap water to the incubation tray. 4. Using a sterilized loop, touch an isolated colony on the provided streak-plate culture, transfer the inoculum to a 5-ml tube of sterile saline, and mix well to effect a uniform suspension. 5. Remove the API strip from its sterile envelope and place it in the incubation tray. 6. Tilt the incubation tray. Using a sterile Pasteur pipette containing the bacterial saline suspension, fill the tube section of each compartment by placing the tip of the pipette against the side of the cupule: Fill the cupules in the CIT, VP, and GEL microtubes with the bacterial suspension. 7. Using a sterile Pasteur pipette, fill the cupules of the ADH, LDC, ODC, and URE microtubes with sterile mineral oil to provide an anaerobic environment. 8. Cover the inoculated strip with the tray lid and incubate for 13 to 24 hours at 37°C. Qatar University Biomedical Program 83 Medical Microbiology BIOM 322 Laboratory Manual Enterotube System: 1. Familiarize yourself with the components of the system: Screw caps at both ends, mediumcontaining compartments, self enclosed inoculating needle, plastic side bar, and blue taped section. 2. Label the Entrerotube with your name and the number of the unknown culture supplied by the instructor. 3. Remove the screw caps from both ends of the Enterotube. Using the inocubting needle contained in the Enterotube, aseptically pick some inoculum from an isolated colony on the provided streak-plate culture. 4. Inoculate the Enterotube as follows: a. Twist the needle in a rotary motion and withdraw it slowly through all 12 compartments. b. Replace the needle in the tube and with a rotary motion push the needle into the first three companments (GLU, LYS, and ORN). The point of the needle should be visible in the H2S/IND compartment. c. Break the needle at the exposed notch by bending, discard the needle remnant, and replace the caps at both ends. The presence of the needle in the three compartments maintains anaerobiosis, which is necessary for dextrose fermentation, Co2 production, and the decarboxylation of lysine and ornithine. J. Remove the blue tape covering the ADO, LAC, ARB, SOR, VP, DUL/PA, URE, and CIT compartments. Beneath this tape are tiny air vents that provide aerobic conditions in these compartmems. 6. Place the clear plastic slide band over the GLU compartment to contain the wax, which may be spilled by the excessive gas production of some organisms. 7. Incubate the tube on a flat surface for 24 hours at 37°C. Qatar University Biomedical Program 84 Medical Microbiology BIOM 322 Laboratory Manual Table 8.1 Summary of Results: 18-24 Hour Procedure API 20E) System' Interpretation of Reactions Tube Positive Yellow ONPG ADH LOC ODC Negative Incubation 18-24 hours 36-48 hours Colorless Red to orange Yellow Red to orange Red to orange Yellow 36-48 hours Red to orange Yellow 18-24 hours Red to orange Yellow 36-48 hours Red to orange Turquoise to dark blue Yellow Light green to yellow Black Red to orange URE No black deposil deposit H,S 18-24 hours 36-48 hours Red orange Any shade of orange within 18-24 hours is a positive reaction. At 36-48 hours, orange decarboxylase reactions should be interpreted as negative. Orange reactions occurring at 36-48 hours should be interpreted as negative. (1) Both the tube and cupule should be filled. (2) Reaction is read in the aerobic (cupule) area. (1) H,S production may range from a heavy black deposit to a very thin black line around the tube bottom. Carefully examine the bottom of lhe tube before considering the reaction negalive. (2) A "browning" of the medium is a negative reaction unless a black deposit is present. "Browning" occurs wilh TDA-positive organisms. Yellow Yellow to TDA Add 1 drop of 10% ferric chloride. Brown.red Yellow IND Add 1 drop 0f Kovacs' reagent. Red ring Yellow Qatar University (I) Any shade 0f yellow is a posilive reaction. (2) VP tube, before the addilion of reagents, can be used as a negative conlrol. Orange reactions occurring at 36-48 hours should be interpreted as negative. Yellow 18-24 hours CIT Comments Biomedical Program A method 01 lower sensitivily has been chosen. Klebsiella. Proteus and Yersinia. routinely give iJosilive reacticns. (1) Immediate reaction. (2) Indole positive organisms may produce a golden-orange color due 10 indole production. This is a negative reaction. (1) The reaction should be read within 2 minutes after the addition 0f the Kovacs' reagent and the results recorded. (2) After several minules, the HCI present in Kovacs' reagent may react with the plastic 0f the cupule resulting in a change from a negative (yellow) color to a brownish red. This is a negative reaction. 85 Medical Microbiology BIOM 322 Laboratory Manual Table 8.1 Continued Interpretation of Reactions Tube Posltive VP GEL GLU Negative Comments Add 1 drop 0f 40% polassium (1) Wait 10 minutes belore considering the reaction negative. hydroxide,then 1 drop of 6% alpha. (2) A pale pink color (after 10 minutes) naphthol should be interpreted as negative. A pale pink color that appears Red Colorless immediately after the addition of reagents but turns dark pink or red after 10 minutes should be interpreted as positive. Motility may be observed by hangingdrop or wet mount preparation. (1) The solid gelatin particles may Diffusion of the No diffusion spread throughout the tube pigment after inoculation. Unless di/lusion occurs, the reaction is negative. (2) Any degree 0f dilfusion is a positive reaction. Blue to blue- C Yellow gray Fermentation (Enterobacteriaceae, O green M M E N T S F O R Aeromonas, Vibrio) (1) Fermentation of the carbohydrates begins in the most anaerobic portion (bollom) 01 the tube. Therefore, these reactions should be read from the bollom of the tube to the lop. (2) A yellow col or al the botlom of Ihe lube indicates a weak or delayed positive reaclion. A MAN INO Yellow Blue to blue- green L L C SOR A RHA R B SAC O MEL H Y Qatar University Biomedical Program Oxidation (other gram-negatives) . (1) Oxidalive utilization of the carbohydrates begins in the most aerobic portion (top) of the tube. Therefore. these reactions should be read from the top to the botlom 01 the tube. (2) A yellow color in the upper portion of the tube and a 86 Medical Microbiology BIOM 322 Laboratory Manual D AMY R ARA A T E S GLU NITRATE REDUCTION After reading GLU reaclion, add 2 drops of 0.8% sul/anilic acid and 2 drops 01 0.5% N, N-dlmelhyl.alpha naphlhylamine NO2 Red Yellow N2 gas Bubbles : yellow Orange after After reagents reagents and And zinc zinc MAN INO. or After reading carbohydrate reaction, add 1 drop of 1.5% H2O,. SOR fOR Bubbles Calalase bubbles Qatar University No Biomedical Program blue in the bottom of the tube indicates oxidative utilization of the sugar. This reaction should be considered positive only for non.Enterobacteriaceae gram.negative rods. This is a negative reaction for fermentative organisms such as Enterobacteriaceae. (1) Belore addition of reagenls, observe GLU t\.lbe (positive or negative) for bubbles. Bubbles are Indir-a!ive of reduction or nitrate 10 the nitrogenous (N2) slat A pOSitive reaction may take 2-3 minutes for Ihe red color 10 appear. (3) Confirm a negalive lest by adding zinc dust 01 20 mesh granular zinc. A pink to orange color aller 10 minules confirms a negative reaction. A yellow color indicates reduction 01 nitrates to the nitrogenous (N,) slate. (1) Bubbles may take 1-2 minut.es to appear (2) Best results will be obtained if the lest is run in tubes thal have no gas from lermentation. 87 Medical Microbiology BIOM 322 Laboratory Manual Table 8.2 Summary of Chemical and Physical Principles of the Tests on the API 20 E System: Tube ChemIcal/Physical Principles Reactive Ingredients ONPG Hydrolysis 0F ONPG by beta.galactosidase releases yellow orthonitrophenol from the colorless ONPG; IPTG (isopropylthio- galactopyranoside) is used as the inducer. ONPG IPTG AOH Arginine dihydrolase transforms arginine into ornithine,ammonia, and carbon dioxide. This causes a pH rise in the aci-.buffered system and a change in the indicalor from yellow to red. Arginine LOC Lysine decarboxylase transforms lysine into a basic primary amine, cadaverine. This amine causes a pH rise in the acid, buffered system and a change in the indicator from yellow to red. Lysine OOC Ornithine decarboxylase transforms ornithine into a basic primary amine, putrescine. This amine causes a pH rise in the acid,buffered system and a change in the indicator from yellow to red. Ornithine CiT - Carate is the sole carbon source. Citrate utilization resulls in a pH rise and a change in the indicator from green to blue. Sodium cltrate H2S Hydrogen sulfide is produced from thiosuffale. The hydrogen sulfide reacts with iron salts to produce a black precipitate. SodiumThiosulfale URE Urease releases ammonia From urea; ammonia causes the pH to rise and changes the indicator from yellow to red. Urea TDA Tryptophan deaminase forms indolepyruvic acid from tryptophan. Indole pyruvic acid produces a brownish-red calor in the presence of ferric chloride. Tryptophan IND Metabolism 0F tryptophan results in the formation of indole. , Kovacs' reagent forms a colored complex (pink to red) with indole. Tryptophan VP Acetoin, an intermediary glucose melabolile, is produced from sodium pyruvate and indicated by the formation of a colored complex. Conventional VP tesls may take up 104 days, but by using sodium pyruvate, API has shortened the required test lime. Creatine intensifies the color when lests are positive. Sodium pyruvale, Creatine GEL Liquefaction of gelatin by proteolytic enzymes releases a black pigment that diffuses throughout the tube. . Kahn charcoal, gelatin GLU MAN INO SOR RHA SAC MEL AMY ARA Utilization of the carbohydrate results in acid formation and a consequent pH drop. The indicator changes from blue to yellow. GLU Nitrate reduction Nitrites form a red complex with sulfanilic acid and N, N-dimethyl- alpha-naphthylamine. In case of a negative reaction, addition 01 zinc confirms the presence of unreduced' nitrates by reducing them to nitrites (pink to orange calor). If Ihere is no calor change after the addition of zinc, this is indicalive of the complete reduction of nitrates through nil riles 10 nitrogen gas or 10 ananaerogenic amine. MAN, INO, or SOR for Catalase Catalase releasEs oxygen gas from hydrogen peroxide. Qatar University Biomedical Program Glucose Mannitol Inositol Sorbitol Rhamnose Sucrose Melibiose Amygdalin Arabinose Potassium nitrale 88 Medical Microbiology BIOM 322 Laboratory Manual OBSERVATIONS AND RESULTS API-20E System: 1. Observe all reactions in the API strip that do not require addition of a test reagent, and interpret your observations using the manufacturer's instructions. Record your observations and results in the chart. 2. Add the required test reagents in the following order: Kovac's reagent to IND, VP reagent to VP (read the result after 15 minutes), ferric chloride to TDA. nitrate reagents to GLU, and oxidase reagent to OXI. Note color changes and interpret your observations according to the manufacturer's instructions. Record your observations and results in the chart. 3. Based on your results, identify your unknown organism using the differential identification chart. 4. Determine and record in the chart the seven-digit profile number as described in Figure 65.4. Identify your unknown organism by referring to the profile recognition system. Enterotube II System : 1. Observe all reactions in the Enterotube except IND and VP, and interpret your observations using the manufacturer's instructions. Record your obsenvations and results in the chart. 2. Perform the IND and VP tests as follows: a. Place the Enterotube in a rack with the GLU and VP compartments facing downward. b. With a needk and a syringe, gently pierce the plastic film of the H2S/IND compartment and add2 or 3 drops of Kovac's reagent. Read the results after 1 minute. c. As in step 2b, add 2 drops of Barritt's reagent to the VP compartment and read the results after 20 minutes. d. Record your IND and VP observations and results. 3. Based on your results, identify your unknown organism using the manufacturer's color identifica tion charts. 4. Determine and record in the chart the five-digit ID value as described in Figure 65.4, Identify your unknown organism by referring to the computer coding manual. Qatar University Biomedical Program 89 Medical Microbiology BIOM 322 Laboratory Manual Ap1-20E Appearance (color) Code Name OPNG Beta-galactosidase AHD Arginine dihydrolase LDc/LYS Lysine decarboxylase ODC/ORN Enterotube Result (+) or (-) Appearance (color) Result (+) or (-) Orinithine decarboxylase ClT Citrate H2S Hydrogen sulfide URE Urease Tryptoptl_an TDA deaminase IND Indole VP Acetonin GEL Gelatin GLU Glucose MAN Mannitol INO Inositol SOR Sorbitol RHA Rhamnose SAC Sucrose ME Melibiose AMY Amygdalin. ARAlARB Arabinose OXI Oxidase ADO Adonitol fermentation GAS Gas production PHElPA Phenylalanine LAC Lactose DUL Dulcitol Organism Qatar University Biomedical Program 90 Medical Microbiology BIOM 322 Laboratory Manual Demonstration of the following items: 1-Mycobacterium tuberculosis slide: by Ziel –Neelsen stain thin pink rods singly or in small groups. 2-Clostridium titani: Gram +ve bacilli swollen at one end due to terminal spherical projecting spores (drum stick appearance). 3-Loffler´s serum: It is enriched media useful for growth of Diphtheria bacilli it is composed of three parts sterile ox sheep or horse serum and one part glucose broth the medium is rendered solid by heating it in the inspissator at 80 ْc for 2 hrs. This leads to coagulation of the serum the medium is opaque white. Qatar University Biomedical Program 91 Medical Microbiology BIOM 322 Laboratory Manual 4-Lowenstien Jensen medium (L.J.): Selective medium used for cultivation of Tubercle- bacilli. The medium is mainly composed of beaten egg, mineral salts and malachite green. the later inhibits the growth of bacteria other than T.B. the medium is rendered solid by heating it in the inspissator at 80ْ c for 1 h .it is opaque green in colour. 5-Cooked meat broth medium: This is an anaerobic culture medium which consists of minced meat to which broth is added the medium is sterilized in the autoclave. The meat contains reducing substances e.g. .haematin and glutathione .which maintain anaerobic conditions at the depth of fluid medium it is suitable for clostridium group. 6-Anaerobic cultivation: Anaerobic cultivation is essential for some bacteria which cannot grow in presence of O2e.g. Clostridia, anaerobic streptococci, actinomyces, bacteroids,… Anaerobiosis can be achieved either by removal of O2 by combining it with hydrogen to form water in the presence of a palladium catalyst or by the addition of reducing substances to culture media. Anaerobic gas packs system: An especial jar with a tightly fitting lid is used. Suspended from the lid is a cold catalyst which consists of alumina pellets coated with palladium and contained a gauze sachet. In this system hydrogen is generated inside the jar by placing a special gas pack envelops to which 10 ml of water is added it will release Co2 and hydrogen. Qatar University Biomedical Program 92 Medical Microbiology BIOM 322 Laboratory Manual Campylobacter: C. jejuni and C.coli are now among the commonest cause of enterocolitis especially in children. Morphology: Small Gram negative rods comma or S-shaped. Motility is of the darting type with cork screw like movement. Laboratory diagnosis: Cultural characters: In case of diarrhea, a stool sample is inoculated on blood agar containing antibiotics Skirrow´s medium containing; vancomycin, polymyxin and trimethoprim is a selective medium used for their isolation from stools. Campylobacter are microaerophilic; grow best in presence of 5% oxygen and 10%CO2. Better growth is obtained at 42ْcْ .they are non haemolytic on blood agar. Biochemical reactions: They are oxidase and catalase positive but urease negative non –proteolytic and unable to attack carbohydrates. Haemophilus-influenzae This organism is often found in normal throats, however it may cause meningitis and epiglotitis in children and it also causes respiratory disease complications (bronchitis, pneumonia, otitis media, and sinusitis) in patients with viral Influenza. Morphology: Gram –ve small cocco bacilli 1.5 u by 0.5u long filamentous forms occur. Cultural characters: Aerobes require for their growth blood containing media ,blood agar better chocolate agar to provide haematin (x factor) and diphosphopyridine nucleotide (v factor) colonies are small and transparent. Neisseria Many of members in the genus Neisseria occur as commensals in the mouth , throat , pharynx and vagina. Two members N.mengitidis and N.gonorrhoeae occur intracellular in pus cells. Morphology: Gram –ve diplococci intracellular is diagnostic and extra cellular. Cultural characters: Neisseria are fastidious and require blood for growth as in blood agar or chocolate agar Theyer-martin is a selective medium used for isolation of pathogenic Neisseria. Qatar University Biomedical Program 93 Medical Microbiology BIOM 322 Laboratory Manual Identifecation Scheme of Isolated unknown Bacteria The main lines of identification are: when you handled the sample start by doing culture keep in the incubator then take smear. 1-Culturel appearance: This includes the colony morphology size, shape, margin, elevation, colour, opaque or translucent, mucoid or dry, pigment producing. 2-Microscopic examination: a- Examination of unstained preparation will help in demonstrating motility. b- Examination of Gram stained preparations: will determine the staininig reaction of the organism whether Gram +ve or Gram –ve, their morphology (cocci, bacilli) size and arrangement. 3-Biochemical reactions: a- Sugar fermentation b- IMVC C- Urease test d- Catalase test e- Oxidase test f- API-20 system 4- Serological identification 5- Animal inoculation 6- Bacteriophage typing: This used for identification and typing of several species of bacteria e.g Staphylococci. 7- Molecular identification and typing methods: These involve detection of microbial nucleic acid by PCR. Qatar University Biomedical Program 94 Medical Microbiology BIOM 322 Laboratory Manual Species Identification of, Unknown Bacterial Cultures PURPOSE: To identify an unknown bacterial species by the use of dichotomous keys and Bergey´s .Manual of Systematic Bacteriology. PRINCIPLE: At this point in the course, you have developed the manipulative skills and the cognitive microbiological knowledge to Identify microorganisms beyond their genus classification to the Ievel of their species identification. Therefore in this experiment, you will use dichotomous keys. Bergey's Marwal of Systematic Bactcriology, and information accrued from prcviously performed laboratory procedures to help identify the species of an unknown culture. In Experiment 31. "Genus Identification of Unknown Bacterial Cultures," you were required to use a varietv of biochemical tests to successfully accomplish the experimental purpose; Your review of the required procedures and ensuing results should indicate that only a few of these tests were actually necessary, in most instances, for the identification of the unknown culture. Similarly, species identification can be accomplished by using a limited number of carefully selected laboralory procedures. Notice that what appears to be a spurious result in some cases, one that departs from the expected norm for a particular species, may be attributable to strain differences within the given species. These nonconforming results may be verified by the use of Bergey´s Manual to ascertain the existence of variable biochemical test results for the particular species being studied. In this experimental procedure, you will receive a mixed culture containing a gram positive and a gram-negative organism. The protocol will require: (1) Gram staining. (2) streak-plating for observation of colonial characteristics. (3) Use of selective media for the preparation of pure culture. (4) The performance of appropriate biochemical tests s indicated in the dichotomous keys outlined in Figures 15.1 and 15.2 and(5) information in Bergey's Manual. Qatar University Biomedical Program 95 Medical Microbiology BIOM 322 Laboratory Manual MATERIALS: Cultures: Per student: Number-coded , 24- to 48 – hour mixed trypticase soy broth cu1ltures each containing a gram-positive and a gram-negative organism selected from the species listed in figures 15.1 and 15.2 Media: Per Student One trypticase soy agar plate, two trypticas soy agar slants, one trypticase soy broth, one phenylethyl alcohol agar plate, and one MacConkey's agar plat. Required media for the biochemical tests listcd in Figures15.land 15.2should be available on your request. Reagents: Crystal violet, Gram's iodine. 95% ethyl alcohol. safranin. and required reagents for the interpretation of the biochemical reactions listed in Figures 15.l and 15.2 Equipment: Bunsen burner, inoculating loop and needle, staining tray, immersion oil , lens paper, bibulous paper. microscope, and glassware marking pencil. PROCEDURE: Session 1: Separation of the Bacteria in Mixed Unknown Culture: 1. Prepare a trypticase soy agar broth subculture of the unknown and refrigerate following incubation. You will use this culture if contamination of the test culture is suspected during the identification procedure. Qatar University Biomedical Program 96 Medical Microbiology BIOM 322 Laboratory Manual 2. Prepare a Gram-stained smear of the original unknown culture. 3. Prepare four-way streak inoculations on the following media for the separation of the microorganisms in the mixed cultures: a. Trypticase soy agar for observation of colonial characteristics. b. Phenyl ethyl alcohol agar for isolation of gram-positive bacteria. c. MacConke׳s agar for isolation of gram negative bacteria. 4. Incubate all the plates in an inverted position and the subculture for 24 to 48 hours at 37°C. Session 2: Preparation of Pure Cultures: I. Isolate a discrete colony on both the phenylethyl alcohol agar plate and the MacConkey's agar plate and aseptically transfer each onto a trypticase soy agar slant .Incubate the trypticase soy agar slants for 24 to 48 hours at 37°C. Session 3: Identification of Unknown Bacterial Species : 1. Prepare a Gram-stained smear from each of the trypticase soy agar slant cultures to verify their purity by means of the Gram reaction and cellular morphology. 2. If each Gram-stained preparation is not solely gram-positive or gram-negative, repeat the steps in Sessions 1 and 2 using the refrigerated trypticase soy agar subculture as the test culture. 3. If the isolates are deemed to be pure on the basis of their cultural and cellular morphologies, continue with the identification procedure. During this period and in subsequent sessions, use the dichotomous keys in Figures 15.1 and L5.2to select and perfonn the necQatar University Biomedical Program 97 Medical Microbiology BIOM 322 Laboratory Manual essary biochemical tests on each of your isolates for identification of their species. Incubate all cultures for 24 to 48 hours at 37°C prior to making your observations. Qatar University Biomedical Program 98 Medical Microbiology BIOM 322 Qatar University Laboratory Manual Biomedical Program 99 Medical Microbiology BIOM 322 Qatar University Laboratory Manual Biomedical Program 100 Medical Microbiology BIOM 322 Laboratory Manual Name --------------------------------Lab section -------------------------Experiment 12 species Identification of Unknown Bacterial Cultures ---------------------------------------------------------------------------------------------------------Report Sheet Unknown Tube No. -----------------------Unknown # 1 Unknown # 2 Gram reaction and shope: --------------------- ----------------------- Results on BAP: ----------------------------------- ----------------------- Results on MacConkey / Emb: ---------------- ----------------------- Unknown # 1 Unknown # 2 Tests performed Results Tests performed Results Conclusions :-------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------Unknowns are: #1 ----------------------------#2 ----------------------------- Qatar University Biomedical Program 101 Medical Microbiology BIOM 322 Laboratory Manual MYCOLOGY There are thousand species of fungi. Most of them are saprophytes. Few species cause disease in man or animals. Fungi can be classified morphologically or clinically. 1-Morphological classification: A-Yeasts: These are oval or round cells that reproduce by budding e.g.Candida and Cryptococcus neoformans. b- Filamentous fungi: These are branching filaments (hyphae) which may be septate or non-septate e.g. the dermatophytes ;( Microsporum, Tricophyton and Epidermophyton) and Aspergillus. c-Dimorphic fungi: These occur in 2 forms ; a yeast form in tissues or when grown at 37ْc; and a filamentous from when grown at 22ْc,e.g.Histoplasma, Blastomyces, Coccidioides. 2- Clinical classification: a-The superficial mycoses: These are fungal infections that are confined to the stratum corneum without tissue invasion e.g. tinea versicolor (Malassezia furfur). b -Cutanneous mycoses: These are fungal infections that involve the skin, nail or hair with tissue destruction and immunological reaction e.g. dermatophytes and cutaneous candidiasis. c- The subcutaneous mycoses: These are infections confined to the subcutaneous tissue without dissemination to distant sites e.g.mycetoma. d- Systemic mycoses: These are primary pulmonary lesions that may disseminate to any organ e.g. dimorphic fungi. They also include a group of opportunistic mycoses e.g. systemic candidiasis and cryptococcosis. Fungi may also be involved in allergic conditions due to aspergillus spores. Mycoses: fungal infection which lead to diseases. Mycotoxicosis: fungi may elaborate toxic substances e.g. afla toxin from Aspergillus flavus which is carcinogenic and hepatotoxic. Candida albicans C. albicans , is the most important species of Candida. Other species include C.tropicalis,C.parapsilosis, C.krusei. Qatar University Biomedical Program 102 Medical Microbiology BIOM 322 Laboratory Manual C.albicans are gram positive oval budding yeast which produce pseudohyphae.It is part of the normal flora of mucous membranes of the upper respiratory, gastrointestinal, and female genital tracts.In these site it may predominate and cause superinfection. Pathogenesis and clinical findings: Predisposing factors to Candida infections are diabetes mellitus, general deplitity, immunodeficiency, indwelling urinary cathters, intravenous drug abuse, prolonged treatment with broad-spectrum antibiotics (which alter normal flora) and corticosteroids. Clinical affection includes: 1-In the mouth, overgrowth of C.albicans produces white patches i.e. oral thrush or moniliasis. 2-Valvovaginitis with itching and discharge which is favoured by high pH, diabetes, or prolonged use of antibiotics. 3-Skin invasion occurs in warm, moist areas, which become red and weeping such as the axilla, intergluteal folds, or inframammary folds most common in obese and diabetics. 4-Nails become involved when repeatedly immersed in water; as in persons involved in dish washing. Painful redness and swelling of nail folds, thickening and loss of nails i.e. paronychia. 5-Candida may disseminate to many organs or cause chronic mucocutaneous candidiasis specially in debilitated children, diabetics, immunosuppressed patients or drug addicts. Qatar University Biomedical Program 103 Medical Microbiology BIOM 322 Laboratory Manual Laboratory diagnosis: 1-Direct microscopic examination: large oval gram positive budding yeast cells with pseudohyphae. 2-Cultures are done on blood agar and Sabourd,s dextrose agar with actidione (cycloheximide) to inhibit saprophytic fungi and chloramphenicol to inhibit bacteria. Large cream coloured colonies develop after 2-3 days incubation at room temperature or 37ْc .Colonies are identified by: a) Gram stain film b) Germ tube test: is done for confirmation the test is done by inoculating a light inoculum from the colony in 0.5 ml human or animal serum which is incubated at 37ْc for 1-2 hr. On microscopic examination, pseudo- germ tubes will be seen as extensions from the yeast cells (drum stick appearance) if the organism is C.albicans. c) Biochemical reactions may be used for species differentiation. Candida albicans ferment glucose with production of acid and gas. API system is available. Treatment: Anti- fungal drugs. Cryptococcus neoformans C.neoformans is yeast cells with a gelatinous capsule. It is found in the excreta of birds specially pigeons feaces. It is an opportunistic pathogen affecting mainly immunosuppressed patients. Infection occurs by inhalation where it causes sub clinical lung infection. It may spread systemically to the meninges causing meningitis. Laboratory diagnosis: 1-Direct microscopic examination of CSF after staining with India ink reveals large gelatinous capsule around budding yeast cells. 2-Cultures done on Sabourd׳s without acitidione, at 20-37 ْc show mucoid colonies which are identified by India ink staining, biochemical reactions (urease positive). 3-Capsular antigens are detected in CSF by using anticapsular antibodies by a latex agglutination test. 4-Antibodies are detected in patients, sera. Qatar University Biomedical Program 104 Medical Microbiology BIOM 322 Laboratory Manual Dermatophytes The dermatophytes include 3 genera Epidermophyton ,Microsporum and Triciphyton. These organisms affect the keratinized tissues; skin, hair and nails. They spread peripherally from foci to produce ring – like lesions. Hence the name ringworm or tinea. Diagnosis of ringworm: 1-Skin scales, nail and hair clippings are examined microscopically after digestion using 10% KOH Branching hyphae are detected among epithelial cells in skin or nails. In hairs, hyphae or spores are detected. The latter may be outside and inside the hair (ectothrix) or inside the hair (endothrix). 2- Cultures are done on Sabourad׳s dextrose agar containing actidion and chloramphenicol and incubated at room temperature for up to 4 weeks. Colonies are identified by: -Morphology and colour on surface. -Microscopic examination using lacto phenol cotton blue. Tinea versicolor It is a skin infection characterized by superficial brownish scaly areas on light- skinned persons and lighter (depigmented) areas on dark –skinned persons. It has a worldwide distribution .It is caused by Malassezia furfur. Qatar University Biomedical Program 105 Medical Microbiology BIOM 322 Laboratory Manual Antiglobulin agglutination test =Coomb's test This test is used to determine the presence of Rh incompatibility which cause (erythroblastosis fetalis). About 80% of individuals have Rh antigen on their red cells i.e. they are Rh positive. Those who do not have Rh antigen on their cells are Rh negative; and to this group the Rh antigen is considered foreign to which they will respond by antibody formation. The clinical importance of Rh antigen lies in the ability of the red cells of an Rh positive fetus (inherited from Rh positive father) to induce anti-Rh antibodies in his Rh negative mother. Fetal RBC,S enter the maternal circulation in small numbers during separation of the placenta .The Rh negative mother will respond to these Rh positive cells by forming anti-Rh antibodies. These antibodies will pass through the placenta to the Circulation of the fetus during the next pregnancy, and will cause haemolysis of his RBC׳s. This; condition is known as haemolytic disease of the new born, or (erythroblastosis foetalis). The first child usually escapes this condition. The condition can be prevented by injecting the Rh negative mother with a small dose of a potent anti-Rh serum within 3 days after delivery of an Rh -positive infant. Most probably, the injected antibody combines with the Rh positive cells in in the mother's circulation, and diverts them from the antibody forming tissues. Most anti-Rh antibodies are IgG incomplete antibodies which can only coat the Rh positive RBC׳s, but cannot bridge between two RBC׳S to cause agglutination. These antibodies can be detected by the antiglobulin Comb's test which is performed in two ways: 1) Indirect Comb's test: The mother's serum - containing incomplete anti – Rh antibodies -is mixed with Rh positive RBC׳S (GROUP O). After incubation at 37ْ C for 30 min. 1 h the mixture is centrifuged, the deposit containing red cells coated with incomplete antibodies is washed, and antihuman globulin (prepared in rabbits) is added, and the tubes incubated. The antihuman globulin causes agglutination by linking together the incomplete antibody molecules. 2) Direct Comb's test: This test can detect incomplete Rh antibodies coating the RBC׳s of the new born in erythroblastosis foetalis. Qatar University Biomedical Program 106 Medical Microbiology BIOM 322 Laboratory Manual The antihuman globulin is added directly to a washed suspension of the new born RBC׳s Agglutination occurs. Both the direct and indirect Comb's test are also used to detect incomplete antibodies in autoimmune haemolytic anemias. Virus haemagglutination Some viruses e.g. influenza, Para influenza, mumps, adeno and yellow fever viruses can cause agglutination of red blood cells of man ,chicken, guinea pig, rat and other animals. This reaction is used for the detection and titration of haemagglutination viruses in culture materials. Enzvme - Linked Immuno Sorbant Assay (ELISA) This technique is very sensitive and does not require' specialized equipment and avoids the hazards of radioactivity. The method depends on conjugation of an enzyme to either antigen or antibody, and then the enzyme activity on a substrate is used as a quantitative measure. Solid - phase ELISA is widely used to measure antigen or antibody. To measure antibody the indirect method is used .A known antigen is fixed to a solid phase (e.g. plastic cup or microplate) incubated with the test serum dilution,then washed to remove excess unattached antibody and reincubated with antiglobulin labeled with a suitable enzyme (e.g.horseradish peroxidase).the labeled antiglobulin will attach to the antibody bound to the fixed antigen. After washing the enzyme activity is measured by adding a specific substrate and measuring the degree of colour change. To measure an antigen, the double antibody technique (Sandwich technique or Direct method) is used; a known antibody is fixed to the solid phase. The test material containing antigen is added and the excess washed.a specific known antibody labeled with enzyme is added .after washing a substrate is added and the enzyme activity measured colourimetrically and related to antigen concentration. Qatar University Biomedical Program 107 Medical Microbiology BIOM 322 Qatar University Laboratory Manual Biomedical Program 108 Medical Microbiology BIOM 322 Qatar University Laboratory Manual Biomedical Program 109