Notes filled
advertisement

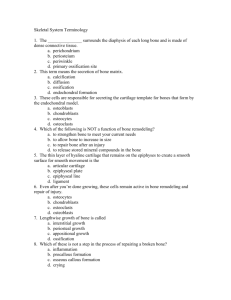
Skeletal Tissues Skeletal tissues Functions 1) support •Frame; muscles, organs and CT attach. 2) protection •Brain, spinal cord, thoracic organs; heart and lungs. 3) movement •Aids muscle contraction; generate leverage. 4) mineral stores Calcium •~2500 gm; also used for cell signaling Phosphorus •For many molecules; ATP for example 5) blood producing •Red and whites blood cells •Within red marrow 6) energy stores •Shafts of bones; filled with fatty material; yellow marrow Histology of skeletal tissue consists of several types of tissues Cartilage •Covers the ends of bones; part of the joint. •Hyaline cartilage dense CT: •periosteum; covers bones •Anchors tendons and ligaments bone •Hard matrix- consisting of hydroxyapatite cells •4 cell types 1-Osteoprogenitor •Ancestral cells (stem cells) •Change (differentiate) into... 2-Osteoblasts •Make bone- fibers and ground substance 3- Osteocytes •Mature bone cells- maintain bone •reserve cells for bone repair 4- Osteoclasts •Erode bone- required for bone remodeling. •Derived from hemocytoblasts matrix •GS + fibers Ground substance •Hard, rock-like material •Brittle, can break easily Hydroxyapatite •Pizoelectric crystal, formed from calcium phosphate •Dense hard minerals, form crystals calcium carbonate collagen fibers •Gives the matrix strength; prevents fractures; made by osteoblasts proximal epiphysis Epiphysis •Ends of bone •Both a proximal and distal epiphysis diaphysis diaphysis •Bone shaft; between the two epiphyses •Has an inner marrow cavity; yellow marrow. distal epiphysis 1) compact bone •Hard and dense bone; most of the diaphysis •Thin layer over each epiphysis 9 Osteon (Haversian system) •Fundamental living unit of bone; consists of cells, layers of matrix and vessels. concentric lamellae •Layers of matrix around a central canal. Haversian canal •Central canal; blood vessels; supply energy and nutritional needs of the osteon. Lacunae •Open spaces; “room”; between lamellae. •Contains a single osteocyte Canaliculi •Tiny channels; interconnect central canal, lacunae, osteocytes. •Nutrient delivery and waste removal. 2) Spongy or cancellous bone •Location: epiphysis. •No distinct organization Trabeculae •Functional unit •Bone extensions project into red marrow. •Lacunae, osteocytes, canaliculi and lamellae; no central canal. red marrow •Red and white blood cell formation. •Nutrients can enter the trabeculae here. Physiology of ossification Ossification (osteogenesis) Bone formation. •Starts in either cartilage model or CT layers •Involves 2 cell types Chondroblasts •Form cartilage model for bone structure Osteoblasts •Produce bone within cartilage model. Two types of ossification •Intramembranous •Endochondral Intramembranous ossification •Within a CT layer during fetal development Ossification center •Initiated by blood vessel •Penetrates middle of CT layer. •Precursor cells become osteoblasts •Form a collagenous matrix- non-calcified •Matrix becomes calcified later forming trabeculae. Trabeculae fuse •Forms the meshlike structure of spongy bone. Apposition •Layers of osteoblasts on both sides of the CT. •Make matrix on the surface of the CT model; bone increases in thickness. •Adds to pervious bone Osteocytes •Osteoblasts become trapped in the growing matrix •Matrix becomes calcified; these cells become osteocytes nucleating seeds How are the hydroxyapatite crystals organized within the matrix? •Collagen fibers act as templates; guide hydroxyapatite deposition •gives matrix strength along certain directions. •Collagen fibers are nucleating seeds endochondral ossification •Endo= within; chondral=cartilage •Bone formation within a cartilage model Diaphysis •Ossification starts within the shaft of the bone. hyaline cartilage model •Covered by a CT layer called the perichondrium •Def: “near cartilage membrane” Endochondral Ossification Step 1: •Chondrocytes in hyaline cartilage enlarge •form struts --> calcify •chondrocytes die, leave cavities Step 2 •Blood vessels around cartilage periphery •Perichondrium; become periosteum; find osteoblasts •Produce bone around diaphysis; subperiosteal collar •Continue to grow --> compact bone (appositional growth). Endochondral Ossification Step 3. •Blood vessels enter cartilage •Deliver osteoblasts. •Spongy bone develop; primary ossification center. Step 4. •Remodeling creates a marrow cavity •Bone replaces cartilage in the epiphyseal plate. Endochondral Ossification Step 5. •Capillaries,osteoblasts enter epiphyses •Secondary ossification centers. Step 6. •Epiphyses fill with spongy bone •Articular cartilage: •Within joint •Epiphyseal plate •Between epiphysis and diaphysis. Physiology of bone growth •Bone continues to grow. •Requires two processes: •1) Epiphyseal plate; bone elongation. •2) Appositional growth; increasing bone thickness. Epiphyseal plate •Aka, growth plate. •Starts as hyaline cartilage Before plate fusion After plate fusion 4 zones of the epiphyseal plate 4 zones of the epiphyseal plate Zone of reserve cartilage •First zone •Next to the epiphysis; hyaline cartilage. •Provides cells for the next zone. Anchor •Anchors the plate to the epiphysis Nutrients •Provides nutrients and cartilage cells to the other zones Zone of proliferating cartilage •Second zone replacement •Cells supplied by the first zone multiply here. •Cartilage proliferates •Plate growth occurs here (small amount). Zone of hypertrophy •Zone three maturation •Cartilage cells increase in size; reach maturity. Expansion •Most growth continues here. zone of calcified matrix •Zone four •Cartilage cells convert the cartilage matrix into a calcified matrix (not bone) Dead •Chondrocytes die Erosion •Matrix erodes •Forms pockets and spaces; merge to form marrow cavity; yellow marrow Osteoclasts •Erode matrix. Rate of growth Human growth hormone (hGH) •One of several; regulates bone growth •Lack of hGH during development; e.g., pituitary dwarfism •Too much hGH before puberty; gigantism Sex hormones •Testosterone and estrogens also play a role in normal bone development. epiphyseal line •Epiphyseal plate fuses late in adolescence; female, 16-18 years; male, 18-20 years. •Called closure. •An epiphyseal line. •Not cartilage; bone. •Too much hGH after closure •Bones thicken; appositional growth • Acromegaly. Rhondo Hatton Film actor, early 20th Cen. Homeostasis of bone remodeling •Bone; dynamic equilibrium between growth and erosion. •Bones can remodel to adapt to new stresses. •During development; bone growth > erosion •Osteoblasts are more active than osteoclasts. Osteoporosis •Osteoclasts are more active than osteoblasts •Osteoblasts; less active with age •Bone looses mass; porous; easy to break. •Due to aging; changes in normal hormone levels. Osteoporotic bone Normal bone