Structure of long bones in mammals
advertisement

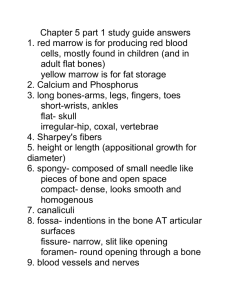
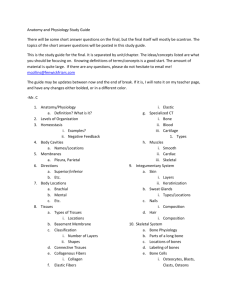
JOURNAL OF MORPHOLOGY 262:546 –565 (2004) Structure of Long Bones in Mammals Michael Locke* Department of Biology, University of Western Ontario, London, Ontario N6A 5B7, Canada ABSTRACT Techniques for staining (silver, osmium, metal sulfides, ink) and microphotography (epiillumination) of polished bone surfaces have been developed to visualize the three-dimensional structure of the shafts of mammalian long bones. Bone is a twocompartment system with capillaries and some kinds of connective tissue in one compartment separated from fibers of bone collagen, often forming lamellae, in the other. Laminar bone consists of stacks of lamellae separated by vascular spaces containing capillary network sheets. It is deposited at the periosteal and endosteal surfaces. Osteonic bone, well described in the literature, consists of cylinders of lamellae with central vascular spaces. The primary structure of the shafts of mammalian long bones is laminar and laminae often remain as the main component. Secondary osteons are a replacement within laminae. As laminar bones mature, some of the irregular longitudinal capillary spaces in the network sheets enlarge and become less crooked to form secondary osteons. Parts of the random networks become ordered longitudinal ones, resulting in collapse of those network spaces not converted to osteons. The residual capillaries become bloodless, making the surviving network spaces difficult to resolve. This may account for them being overlooked in descriptions of bone structure. For example, laminar bone occurs with osteonic bone in the human femur, although it is rarely figured. Nearly mature bones switch the kind of primary bone deposited at the peripheral (periosteal) surface from laminar to primary osteonic. J. Morphol. 262: 546 –565, 2004. © 2004 Wiley-Liss, Inc. KEY WORDS: bone structure and staining; bone as a two-compartment system; laminar bone; osteon This study is concerned with the structure of the shafts of mammalian long bones at the low microscopic level. It supplements the prevailing view that bone is constructed from osteons by showing that compact bone is formed primarily from laminae. In the young growing animals examined (beef, sheep, pigs), the shaft is completely made from circumferentially oriented laminae without osteons. In older or even mature animals much of the shaft is still laminar (human, buffalo, deer, horse, oxen, as well as beef, sheep, and pigs). Enlow and Brown’s (1956, 1957, 1958) often-quoted but perhaps rarely examined classical comparative study of bones describes what we now call laminar bone in many mammals. In spite of this, descriptions of osteons with no mention of laminae were found in a survey of more than 40 textbooks of general biology, comparative mor© 2004 WILEY-LISS, INC. phology, veterinary, medical, and functional histology. Longitudinal profiles of laminae have sometimes even been labeled osteons (Locke and Dean, 2003, in a note aimed at biology teachers). Most research articles follow this tradition, which has changed little since Todd and Bowman’s description of Haversian bone in 1845 (Martin and Burr, 1989b), ignoring the capillary network sheets that separate layers of bone lamellae. Enlow and Brown (1958, p. 211) noted this almost 50 years ago, saying “Most vertebrates do not possess the classic pattern of bone tissue structure described in modern textbooks of histology. The descriptions of bone tissue in current texts are concerned primarily with human bone.” Laminar and osteonic structure is well known to those studying physical properties (Wainwright et al., 1976; Weiner et al., 1999; Currey, 2002), but many researchers are not aware of the complexity of bone structure and its variation with species, kind, orientation, and developmental stage that was described by Enlow and Brown. For example, Halstead (1974, p. 68) follows Currey, by commenting that laminar bone has “received scant attention” compared to “Haversian systems,” but still figures the two kinds of bone incorrectly. Some literature error has resulted from a confused use of terms: for example, circumferential lamellae rather than laminae have been described as smoothing off the endosteal and periosteal surfaces. Lamella is the diminutive of lamina. Laminar bone is made from 4 –20 lamellae. This article is concerned with the shape of the bone compartment, which is usually some variation of a sheet (laminar bone) or a cylinder (osteonic bone). It does not discuss fiber orientation within these compartments, which contributes another layer of definitions at a finer order of microscopy. A brief glossary of the terms used here clarifies terminology (see Appendix). Contract grant sponsor: NSERC; Contract grant number: A6607. *Correspondence to: Michael Locke, Department of Biology, University of Western Ontario, London, Ontario N6A 5B7, Canada. E-mail: mlocke@uwo.ca Published online 16 September 2004 in Wiley InterScience (www.interscience.wiley.com) DOI: 10.1002/jmor.10282 Fig. 1. The primary structure of compact bone is laminar. A: Vascular compartments cut transversely and separated from one another by layers of bone in a transverse profile at 90° to the long axis. Vc, Volkmann’s canals. Silver-stained 3-year-old buffalo humerus. B: The vascular compartments form an intricate reticular network in a tangential profile (face view parallel to the surface). Ink-injected 2-year-old beef humerus. C: Three layers of reticular compartments in a slightly oblique tangential profile. Ink-injected giraffe radius. D: Layers of bone alternate with obliquely or transversely cut vascular compartments connected by Volkmann’s canals (Vc) in a radial profile (longitudinal view from center to periphery). Silver-stained 3-year-old buffalo humerus. Scale bars ⫽ 1 mm. 548 M. LOCKE Figure 2 STRUCTURE OF LONG BONES IN MAMMALS 549 ciation is that studies on bone have traditionally been either anatomical or have relied on grinding thin sections (Enlow and Brown, 1956). Grinding sections is a tedious and difficult process appropriate for high-resolution light microscopy (Yuehue et al., 2003), but at high resolution it is often difficult to determine the plane of section and threedimensional arrangement. There has also been a reluctance to observe profiles other than transverse (as in Enlow and Brown, 1956, 1957, 1958). Modern techniques of scanning electron microscopy of resin casts of the vascular system are time-consuming (Moller et al., 1997), although the results are exceptionally beautiful (Pannarale et al., 1997). Microangiography is restricted to those with specialized X-ray units (Berry, 1979). This article uses simple stereo observation at intermediate magnifications to study the relationships between osteons and laminae in mammalian long bones at different stages of development. It introduces ways to stain carefully oriented samples for viewing by epi-illumination in order to describe the most common compartment patterns and microvasculature of the bone matrix in three dimensions. Fig. 2. Compartments forming laminae contain capillary network sheets. A: Unstained blood-filled capillaries form reticular networks in the plane of the lamina. Natural unstained blood in a tangential profile of cleared beef humerus close to the periosteal surface. B: Staining of the capillary lumens confirms their reticular pattern in capillary sheets. The black speckles are osteocytes. Olive oil-injected and osmium-stained tangential profile of beef humerus. 3D observations in A and B show that some of the denser spots are connections between adjacent sheets. Single connections are more common than Volkmann’s canals uniting several laminae. C: General staining of the vascular compartment shows a coarser reticulum than the capillary network that it encloses. The white speckles are unstained osteocytes. Iron sulfide staining of tangential profile of beef humerus. D: The vascular compartment is probably the prime mover in forming new laminae at the periosteal surface. The vascular compartment (V, blue) is at first much wider (top, younger bone at the periosteal surface) than the compartment destined to contain bone (B, brown to black). Below the forming layer the vascular compartment is reduced to a thin darkly staining layer. Silverstained transverse profile of 2-month-old pig humerus. E: The vascular compartments (V) are at first flat sacs connecting across the bone compartment (B) to the older and newer vascular compartments on each side. Tangential views near the bone surface show profiles of the tubular connections as circles. Each circle contains a brown-stained fiber (3), perhaps concerned in its genesis. These connecting fibers have the topological position of Sharpey’s fibers described in mature bone. Silver-stained tangential profile of a femur of a 6-month-old calf. F: The bone compartment (B) connections enlarge, reducing the vascular compartment (V) to the reticulum that comes to contain the capillary network. Silver-stained tangential profile of a lamb femur further from the periosteal surface than E. Scale bars ⫽ 1 mm. G: Laminar bone is a connective tissue system of two compartments, one containing mineral reinforced collagen fibers (and perhaps Sharpey’s fibers), the other, capillaries and a different class of fibrous components (see also fig. 5.14 in Wainwright et al., 1976; fig. 10.10 in Fawcett, 1994; fig. 1.5 in Currey, 2002). Information on laminar bone is scattered though the literature, but rarely with the clarity and detail that it deserves. One reason for this lack of appre- MATERIALS AND METHODS Sample Preparation Bone samples were prepared from many different sources— new kills, with and without aldehyde fixation, slaughterhouses, mortuary specimens, worn museum preparations, subfossils, and fossils. The periosteum and endosteum were pulled from fresh bone with pliers where necessary. Only the central shaft of long bones, uncomplicated by the cancellous bone at the ends, was studied. Bone blocks were cut on a bandsaw with radial, transverse, and tangential faces. Blanks 1–2 mm thick were then cut from these faces using a fine bandsaw or a jeweler’s saw. Test samples were prepared as billets measuring about 10 ⫻ 10 ⫻ 1 mm or less, depending on the type of bone. It is important to make the main faces parallel to one another to obtain uniformly flat fields for photography. The blanks were ground flat on a wet 220 grit diamond lap followed by a wet 600 grit lap to give a surface finish fine enough for microscopy. Impregnation Infiltration methods show spaces formerly occupied by blood vessels or the spaces around them even in subfossil specimens. Ink. Ink has been used to study blood circulation in bone (De Saint-Georges and Miller, 1992) and to show sutures or the spaces in trabecular bone. It is an easy way to display the spaces in bone occupied in life by blood vessels. Clean dry bone samples were left overnight in a jar of black carbon Indian ink with a few drops of dishwasher detergent. Impregnation was helped by allowing infiltration at reduced pressure in a vacuum oven for 1–24 h before slowly (5 min) returning to atmospheric pressure. Surface ink was then washed off. Either the lumina of blood vessels or the spaces left in the bone formerly occupied by blood vessels and osteocytes, depending on age and preservation, stand out in clear black patterns against the white bone (Figs. 1B,C, 6B). Other colored inks gave similar results. Olive oil and osmium black. Clean dry bone samples were allowed to take up olive oil for hours to days in the reduced pressure of a vacuum oven before a slow (1 h) return to atmospheric pressure. The bones had then become translucent light yellow. They were wiped clean and left for 2–24 h in 1% osmium 550 M. LOCKE tetroxide in phosphate buffer, pH 7.5. The osmium was reduced to a black mass of suboxides (osmium black) by the double bonds of the oleic acid in the olive oil, leaving the blood vessels and/or the spaces they occupied in the bone standing out in sharp black relief (Figs. 2B, 6A). Direct Observation of Blood-Filled Capillaries Most fine blood vessels in bone samples fill with air (see Results), but some, particularly in osteons and in newly formed laminar bone, may contain red blood. After infiltrating the sample with glycerol for a few days, the surface layer becomes translucent or even transparent, allowing blood-filled vessels to be resolved in three dimensions (Figs. 2A, 11A,B). salts is that they penetrate through and across the walls of the capillaries, binding to most of the contents of the vascular compartment but not mature bone itself (iron does stain the bone surface, which may have to be polished away). Hydrogen sulfide penetrates easily, so that all cells and tissues adsorbing the metals become dense black. Conventional staining. Several stains (Coomassie blue, hematoxylin) gave satisfactory colored representations of bone cell components, but not the sharp, dark contrasts most useful to show vascular distribution by low-magnification microscopy. Ground sections. Conventional ground sections viewed by transmitted illumination were also prepared for comparison with the procedures above. Microscopy and Photography Staining Staining techniques require the survival of some organic material and are not suitable for very old bones. Bones were fixed in formaldehyde both for preservation and safety from infectious agents in bone dust. Silver impregnation and reduction. Bone samples were equilibrated in 3–5% silver nitrate on a rotator in the dark for 1–24 h before being washed in water and fixed in 5% sodium thiosulfate. Aldehyde-fixed material showed black silver staining of blood, blood vessels, osteocytes, and epithelia. This makes it ideal for distinguishing different types of bone— osteonic or laminar—at a glance. Although it does not stain mature bone, it does react with preosseus tissue or osteoid, i.e., bone lamellae, as they are being deposited, before calcification. There is a gradient from black in the youngest, outermost, newly forming bone laminae, to brown and yellow in those inner laminae formed earlier. Bone being absorbed during osteoporosis or bone reconstruction stained brown to black, as did recently deposited bone. Silver staining is useful for quickly mapping areas of bone genesis or osteoporosis. The expanded matrix around blood vessels in forming bones stained light blue to orange. Exposure to diffuse light developed more silver after weak impregnation. It is important not to overstain in the silver nitrate. Too long an exposure stained everything black, with no components resolved. In some overstained preparations the thin black surface crust was ground away on a wet 600 or 1800 grit lap to reveal the impregnated capillary systems beneath. The best results were obtained with bone that had been stored in weak formaldehyde, allowing complete penetration and fixation. Unreduced silver was washed out in 5% sodium thiosulfate to make permanent preparations (Figs. 1A,D, 2D,E,F, 3F–H, 4A,B, 5A–I, 6D, 7A,B, 10A). For the purposes of this article, dark silver staining is taken to be a marker for osteoid bone as it is being formed or resorbed. Osmium fixation and staining. Bone samples were left in 1% osmium tetroxide in phosphate buffer at pH 7.2 for 2–24 h. Osmium tetroxide fixes most tissues and prolonged fixation adds more precipitated osmium black. The blackness was further accentuated in some preparations by reacting for 1 h in 1% ethyl gallate. New bone, osteocytes, and cells of the capillary lining were contrasted in black against the unstained mature white bone matrix (Figs. 3I, 11C). Impregnation With Metal Salts Billets were exposed to saturated solutions of metal salts for 1– 4 h, with and without a vacuum. They were then washed and the adsorbed metals converted to black sulfides by treatment with dilute yellow ammonium sulfide. After cleaning, and in some cases repolishing, they were cleared in glycerol. The following salts all gave excellent results: ferrous sulfate (Figs. 2C, 6C, 9A), mercurous acetate (Figs. 7C–F, 8A,B, 9B, 11D,E), bismuth subnitrate, lead acetate, cobalt acetate. The general result resembles osmium black staining, but with a greater tendency to stain the cement sheath. The advantage of metal Stained test samples were observed after glycerol infiltration. This had a dual purpose for photography. It allowed deeper visualization by increasing the transparency of the surface, and it eliminated reflections from surface scratches. This method of tissue preparation and observation is useful for immunofluorescence (tetracyclines and antibodies) in addition to the staining procedures described here. Photographs were taken with a Zeiss photomicroscope and a ⫻1, ⫻2.5, or ⫻10 objective lens with epi-illumination provided by two side lamps. Infiltration and epi-illumination also allowed for 3D observation with a stereomicroscope. The conclusions illustrated by the photographs are based on these 3D observations of several hundred preparations, including those of beef (Bos taurus), sheep (Ovis aries), giraffe (Giraffa camelopardalis), pig (Sus domesticus), human (Homo sapiens), buffalo (Bison bison), deer (Odocoileus virginianus), horse (Equus caballus), and goat (Capra hircus), some involving several different stains and stages of development. Most preparations were made from the central shaft of the humerus or femur, occasionally from other long bones. Because of their simplicity, the techniques may be useful for anyone who works with bone— biologists, gerontologists, archaeologists, physical anthropologists, or forensic scientists. The page orientation has been standardized for all illustrations. Transverse profiles have the periosteal edge to the top. Tangential and radial profiles orient the length of the bone with the length of the page. RESULTS Primary Structure of the Shafts of Mammalian Long Bones Is Laminar The diaphyses or shafts of long bones are made of compact bone, the primary structure of which is laminar. In all young growing animals examined (beef, sheep, pigs), the shaft is completely made from circumferentially oriented laminae without osteons. In older or even mature animals much of the shaft is still laminar (human, buffalo, deer, horse, oxen). Staining showed transverse profiles resembling tree rings. Circumferentially arranged bone laminae, about 200 m wide, separate endothelium-lined vascular compartments, 10 –50 m across (Fig. 1A). This is the primary lamellar or mature plexiform bone of Martin and Burr (1989b). Viewed tangentially, i.e., facing the surface, each vascular compartment sheet is resolved as a reticulum (Fig. 1B,C) very similar to the scanning electron microscope images of resin casts of cow laminae (Arsenault, 1990). Radial profiles (longitudinal cuts from center to periphery) show the capillaries and their com- STRUCTURE OF LONG BONES IN MAMMALS 551 partments cut with all orientations from longitudinal to transverse and oblique (Fig. 1D). The shape and orientation of the osteocytes show that the bone lamellae are layered parallel to the vascular compartment sheets, not in cylinders around capillaries, as in osteons. Layers of bone alternate with obliquely or transversely cut compartments connected by Volkmann’s canals, venous escape routes from pooled blood in the marrow to the network at the periosteal surface (Seliger, 1970; Oni and Gregg, 1990). Laminar bone, i.e., stacks of vascular sheets separated by bone laminae, with each lamina being a plywood-like composite of several lamellae, is the common, basic structure of compact bone. It is the primary structure of most bones. Capillary Network Sheets in the Vascular Compartment of Laminar Bone To understand the images seen in profiles of developing laminar bone it is necessary to visualize them in three dimensions. There are two compartments, one containing bone lamellae, and the other capillaries (and also nerves and connective tissue). The capillaries form a reticular sheet within the reticular vascular compartment. Capillaries form a very fine reticular network in the plane of the lamina. They are easily visualized in tangential profiles of cleared, unstained preparations of bone that has not been exsanguinated and that contains blood-filled capillaries (Fig. 2A). Injection of the capillary lumens (olive oil and osmium) confirms the reticular nature of the capillary sheets (Fig. 2B). Both kinds of preparation allow 3D views under the stereomicroscope. Stereo-views show the arrangement of the short connecting capillaries between adjacent sheets that had been visualized in radial profiles (Fig. 1D). The pattern of capillaries resembles that in a rabbit tibia observed intravitally (Winet, 1989) or in rats by corrosion casting (Ohtani et al., 1982). Staining of the vascular compartment shows a coarser reticulum than the capillary network that it encloses (Fig. 2C). The vascular compartment is probably the prime mover in forming new laminae at the osteal surface. In young animals there may be 5– 8 enlarged vascular compartments forming new laminae. These make up the plexiform bone described by Martin and Burr (1989b), the laminar bone described in the beagle by Jee et al. (1970), or the lamellar bone in fig. 5.13 of Wainwright et al. (1976). Even in older, mature animals there are usually some regions with newly forming laminae. The vascular compartment is at first much wider than the compartment destined to contain bone. It declines in width as the lamellae are deposited in the bone layer, eventually shrinking to contain little more than the capillary network (Fig. 2D). The vascular compartment changes its form as well as its thickness. It is at Fig. 3. The distribution of laminar and osteonic bone in an adult human femur. A: Transverse profiles were cut at seven levels along the length of the femur, 11, 14 (B), 19 (C), 23 (D), 25 (E), 29, and 33 cm from the proximal end. Mainly laminar bone, with its characteristic vasculature, survives into the adult in a layer below the periosteum. Within this is a layer of mainly osteonic bone. Bone on the endosteal surface is cancellous. The core consists of marrow. Right femur 42 cm long from a 52-yearold woman. B–E: The appearance of laminar and osteonic bone marked in A at positions 14 (B), 19 (C), 23 (D), and 25 (E) cm from the proximal end. Silver stained. Scale bar ⫽ 1 cm. Transverse (F:), radial (G), and peripheral H tangential profiles at 23 cm from the proximal end illustrate the histology. The structure was similar at other levels, with osteons predominating over laminae. Silver stained. I: The osteonic layer (O) still contains some fine network capillaries (nc) surviving from its primary laminar structure. Conversely, some capillaries (o) in subperiosteal laminae (L) have become osteons (see Osteons Occur Within Laminae and Osteons Form by Erosion…). Thus, laminar (L) and osteonic layers (O) each contain both kinds of bone. Osmium-stained transverse profile at 23 cm. Scale bars ⫽ 1 mm. first a flat sac with tubular connections between the two sides that appear as circles in face view. Each circle is a window on the bone compartment and contains a brown-stained fiber (Fig. 2E). The fibers are inside the bone compartment and could be concerned in its genesis, making connections between adjacent sheets. They are in the same topological position inside the bone compartment as Sharpey’s fibers (Bloom and Fawcett, 1975). They are noted here because of their topological position in the bone compartment, but with an 552 M. LOCKE Figure 3. (Continued) orientation normal to that of the bone collagen. The windows through the forming vascular compartment should not be confused with the connections across the bone (Volkmann’s canals) that unite adjacent vascular compartments. These circular windows enlarge to leave the remainder of the vascular compartment as the reticulum holding the capillaries (Fig. 2F). The structure of laminar bone and its development is most easily understood if it is thought of as a system of two compartments, one containing bone lamellae and their associated osteocytes, and the other capillaries, nerves, and connective tissue (Fig. 2G). The vascular compartment of laminar bone is a reticulum and its bone a sheet. The vascular compartment of an osteon is a tube and its bone a cylinder. Both kinds of bone compartment are organized in lamellae having various orientations. As Weiner says: “…lamellar bone is present in two forms, namely, as parallel arrays or as cylinders…” (Weiner et al., 1999, p. 253). The lamellae may be interwoven fibers alternating with collagen-rich and collagen-poor regions (Marotti, 1993). Currey (2002, figs. 1.4, 1.5) distinguishes woven from lamellar bone by the woven orientation of some of its fibers in the laminae. The collagen fiber orientation in lamellae suggests a plywood-like structure (Giraud-Guille, 1988; Wiener et al., 1997, 1999; Weiner and Wagner, 1998), as in insect cuticle lamellae. STRUCTURE OF LONG BONES IN MAMMALS 553 Figure 3. (Continued) Laminar and Osteonic Bone in the Human Femur Human histology textbooks, e.g., Bargmann (1967), Elias and Pauly (1966), Han and Holmstedt (1981), Cormack (1984), Krstic (1978, 1984, 1991), figure transverse sections of long bones made only from osteons, sometimes with peripheral layers labeled “circumferential lamellae.” The work of Enlow and Brown (1958) showing laminae and osteons has been forgotten. Published photographs of human 554 M. LOCKE Fig. 4. Osteons occur within laminae. A: Although there are relict laminae, the mature human femur is mainly composed of osteons, as the textbooks propose for a typical diaphysis. Transverse profile of a silver-stained human femur. B: The formation of osteons (o) in laminar bone. Some buffalo bone can be entirely laminar (Fig. 1A) but other regions contain numerous osteons. Silver-stained transverse profile of a 3-year-old buffalo femur. Scale bars ⫽ 1 mm. bone are not easy to interpret. Typically, as in di Fiore (1981), they show osteons and circumferentially arranged “lamellae” averaging 5 m in thickness. A Neanderthal bone (Schultz, 1999, 2001) shows osteons and “basic lamellae” in a subperiosteal peripheral layer in transverse section. The following study of the shaft of a human femur shows that these peripheral circumferential lamellae are probably unrecognized laminar bone. Transverse profiles were cut and prepared for microscopy at seven levels along the length of a human femur (Fig. 3A). Four regions were easily distinguished. Laminar bone, with its characteristic vasculature, survived into the adult in a layer below the periosteum. In some positions there were only one or two laminae; in others, as many as 10 laminae constituted up to a quarter of the shaft thickness. The laminar region was often stained a darker shade of brown by silver or osmium, suggesting that it had a different composition from the layer below it (Fig. 3B–D). The main thickness of the shaft was largely osteonic. Many of the osteons had wide, darkly stained lumens, as if their bone lamellae were being resorbed, perhaps to be expected from osteoporosis in a 52-year-old woman. The endosteal surface had a variable ragged edge of cancellous bone, as though much of it had been eroded, also suggesting osteoporosis. There was no endosteal laminar surface. The core consisted of marrow. Transverse, radial, and peripheral tangential profiles show the human femur has the typical features of laminar and osteonic bone (Fig. 3F–H). The circumferential lamellae so often described are therefore laminae in which the vascular compartments Fig. 5. Osteons form in the vascular compartments of laminar bone. Transverse (A) and radial (B) profiles. Osteons (o) in laminar bone line up exactly with capillaries in the surviving network sheets as though they have replaced them. Some capillaries and their cavities in the bone laminae have enlarged. These are presumed to be forming osteons because their dense staining resembles that in laminar bone deposition and resorption in osteoporosis and endosteal erosion. Silver-stained 3-year-old buffalo femur. Scale bar ⫽ 1 mm. C–I: Transverse profiles of osteons can be arranged in series suggesting stages in their development from capillary network sheets. C: There is no synchrony within a region. All stages of development are found together. A capillary beginning to enlarge is adjacent to an almost completely formed osteon. D: A vascular compartment enlarges locally, resorbing laminar bone as it does so. E,F: A cylinder of osteonic lamellae begins to replace the space carved in the laminar bone. The newly deposited bone stains intensely at first like that during the deposition of laminae. G,H: Osteonic bone continues to be deposited until only a space large enough for a small blood vessel remains. I: The end result is a cylinder of lamellae around a blood vessel little larger than that in the original capillary network but with few lateral connections. The bone is only distinguishable from the original laminar bone by the concentric orientation of its osteocytes and lamellae and the cement sheath. Transverse profiles of silver-stained 3-year-old buffalo femur. Scale bar ⫽ 0.1 mm. STRUCTURE OF LONG BONES IN MAMMALS Figure 5 555 556 M. LOCKE have been reduced or made difficult to resolve (see Why Bones Are White…). The structure was similar at other levels, with osteons predominating over laminae. The details of structure may be idiosyncratic to this particular bone, but we may conclude that human compact bone contains laminae as well as osteons. Separation of the osteonic and laminar layers is not absolute with respect to their constituents (Fig. 3I). Some large osteons occurred among the capillaries of the laminar layer (see following two sections). Conversely, some capillaries in the osteonic layer had the small cross section characteristic of capillary networks and lacked concentric bone lamellae. They are presumably relicts from the primary laminar structure after its replacement by osteons. Osteons Occur Within Laminae The presence of osteons among laminae is a general feature of mature bones. Some bones, as in the human femur, are almost entirely composed of osteons (Fig. 4A). The shaft structure in a 3-year-old buffalo femur shows the replacement of laminar by osteonic bone even more clearly. Much of it is entirely laminar (Fig. 1A), but other regions contain numerous osteons. (Fig. 4B). All the mature bones studied contained osteons. Descriptions of mature bones, as if they represent the typical situation, may account for laminar bone being so often overlooked. they replace parts of the capillary network sheets of laminar bone rather than carving new pathways. The most probable sequence is shown in Figure 5C–I. It begins with enlargement of the vascular cavity around one of the more axially oriented capillaries. Bone eroded from the surrounding lamina begins to stain brown. The space enlarges as much as 10-fold before deposition takes over from resorption. Osteonic lamellae continue to be deposited until only a space large enough for a small blood vessel remains. The new circumferential lamellae progressively lose their dense staining from the outside to the inside, until the only difference from laminar bone lies in the orientation of lamellae and the osteoblasts that have secreted them. The faintly stained density separating the new tubular lamellae from the old flat lamellae may be traces of a cement sheath like that found in other secondary osteons. The result is a less crooked space (see also Fig. 11D), and a blood vessel little larger than that in the original capillary network, but with fewer lateral connections. The loss of lateral connections confirms a micrograph of a resin cast of osteons that have separated from the reticular network but retained connections to Volkmann’s canals (Arsenault, 1990). Straightening and loss of lateral connections is a general property of all osteons observed. The change from radially connected stacks of network sheets, to longitudinal vessels connected to other longitudinal vessels, could result in a significant change in blood flow (see Why Bones Are White…). Osteons Form by Erosion of Laminae and Secretion of Cylindrical Lamellae Folded and Irregular Laminae Primary bone is entirely laminar, growing at the periosteal surface (Fig. 2D,E). Osteons arise later (Fig. 4A,B). By this time the volume of bone may be fixed, so that new bone can only arise in the space created by resorption of the old. New osteons stained strongly with silver, as would be expected if bone is being deposited and/or resorbed. These new osteons in the laminar bone lined up exactly with capillaries in the surviving network sheets, as though they had replaced them (Fig. 5A,B). They did not have the irregular distribution of the basic multicellular units (BMUs) of Martin and Burr (1989a), believed to be the basic mechanism for replacing older bone with new osteons. The new osteons in Figure 5 were at all stages of development, from barely discernable dark brown swellings in the profiles of the reticular spaces, to large concentric cylinders of unstained lamellae (Fig. 5C–I). There was no synchrony within a region. All stages were found together (Fig. 5C). Longitudinal profiles of these forming osteons (Fig. 5B) were each at a particular stage of development, suggesting that the transverse profiles (Fig. 5C–I) represent stages rather than different levels in the length of newly forming osteons. These new osteons resemble the BMUs of Martin and Burr (1989c), or the remodeling osteons of Parfitt (1994), except that In some regions, the shape of the bone compartment is not in flat laminar sheets but may be folded or distorted, creating an irregular 3D network. (The fiber orientation within these compartments creates a further subdivision of categories, such as woven [Stover et al., 1992], fibrolamellar, parallel fibered, or plexiform [Martin and Burr, 1989c]). Lateral connections between capillaries are then oriented in all directions (Fig. 6A). The 3D arrangement is most clearly seen in tangential profiles (Fig. 6B). This 3D network is very different from the stacked network sheets of standard laminar bone (Fig. 1B,C). The switch from flat to distorted laminae is often abrupt, without a smooth transition from flat 2D laminae into folded 3D structures (Fig. 6C). Regular and irregular laminae may alternate. The positioning of irregular layers shows that they have been created in this way by changes in deposition at the periosteal surface, not by distortion of previously deposited regular laminae. (They may also be deposited at the endosteal surface; see Endosteal Laminae Form…). Vascular chambers in these irregular laminae can also become osteons, as they do in flat laminae (Figs. 4, 5). They enlarge and resorb laminar bone before redepositing lamellae in winding osteonic cylinders (Fig. 6D). STRUCTURE OF LONG BONES IN MAMMALS 557 Fig. 6. Laminae may be folded or distorted as well as flat. A: Sheets of laminar bone may be deposited as 3D networks with lateral connections between capillaries oriented in all directions. Olive oil-injected and osmium-stained transverse profile of a deer cannon bone. B: The 3D arrangement is most clearly seen in tangential profiles. This 3D network is very different from the stacked network sheets of standard laminar bone (Fig. 1B,C). Tangential profile of ink-injected beef femur. C: The switch from flat to distorted laminae is often abrupt, without a smooth transition from flat 2D laminae into folded 3D structures. The outer layers are regular laminae, while the inner layer formed earlier is irregular. Iron sulfide-stained radial profile of young beef humerus. D: Vascular chambers in these irregular laminae also become osteons in the same way as in flat laminae (Figs. 4, 5). They enlarge and resorb laminae before redepositing lamellae in winding osteonic cylinders. Silver-stained transverse profile of the endosteal surface of a young beef humerus. Scale bars ⫽ 1 mm. Fig. 7. Some vascular compartments are radially rather than circumferentially oriented. A,B: In a common variant of laminar structure, the vascular chambers and their capillaries extend radially (Rl). The regions are often bounded by circumferential laminae (Cl) but may extend to either surface. Silver-stained transverse profile of a humerus from a young pig. C: Radially arranged components are usually diagonal to the long axis. Infolds from the surface continue as irregular vascular chambers resembling laminae. Mercury sulfide-stained radial profile of a young pig humerus. D: Radial chambers often begin at the surface as continuations of tendon insertions, containing connective tissue as well as or instead of capillaries. They are often interspersed with radial laminae. Mercury sulfide-stained transverse profile of a young pig humerus. E: Tendon insertions may also continue into distorted laminae. Mercury sulfide-stained transverse profile of a young pig humerus. F: Volkmann’s canals (Vc) are often radial-diagonally oriented especially near tendon insertions like A–D. Mercury sulfide-stained radial profile of a young pig humerus. Scale bars ⫽ 1 mm. STRUCTURE OF LONG BONES IN MAMMALS 559 Fig. 8. At the surface of mature bones there may be a switch from deposition of laminae to longitudinal tubes. A: Forming vascular compartments below the periosteum of some mature bones are exactly axially oriented, forming a regular array in transverse profile. Below them each completed compartment has cylindrical lamellae like an osteon. The exact orientation extends for several rows below the surface. Mercury sulfide-stained mature deer cannon bone. B: Tangential profile close to the surface shows longitudinally arrayed vascular compartments with few lateral connections, unlike laminar bone. Some have cylindrical lamellae like osteons. Mercury sulfide-stained mature deer cannon bone. Scale bar ⫽ 1 mm. Some Laminae Are Radially Oriented In a common variant of the folded laminar structure, some laminae are radially oriented. Their vascular chambers and capillaries not only extend radially but also diagonally in the axial direction (Fig. 7A–D). In transverse profile they are leaf-like, flattened radially (Fig. 7B). They may be sandwiched between circumferential laminae (Fig. 7A), or extend to either surface. Radial laminae begin at the surface as tendon insertions and contain connective tissue fibers in addition to blood vessels (Fig. 7D). They pass diagonally across from the periosteal surface, continuing as irregular vascular chambers resembling laminae. (Fig. 7C). Tendon insertions may also continue into distorted laminae (Fig. 7E). Radial laminae overlap in structure with Volkmann’s canals, which are often radial-diagonally oriented, especially near tendon insertions (Fig. 7F). These radial-diagonal orientations show the complexity of bone structure and demonstrate the need for study in all planes before 3D reconstruction. Longitudinal Tubes in Peripheral Laminae Not all bone formed at the periosteal surface is laminar. Late in development, when the size of the bone has been determined, the reticular form may become predominantly axial (Fig. 8A,B). Transverse profiles show that these axial vascular spaces have cylindrical lamellae like osteons. Developmentally, they are primary osteons in the sense that laminar bone is primary, osteons developing within laminae being secondary (Currey, 1982). They have been described as primary osteons in transverse profiles of horse metacarpals (Stover et al., 1992) and are assumed to be the main source of osteons by Ham (1974) in fig. 15.36. Endosteal Erosion With Periosteal Deposition Is a Mechanism for Size and Shape Change The primary consequence of the deposition of circumferential laminae at the surface is increase in girth. If lamellae continue to be deposited around distorted and radially oriented vascular compartments as they are covered over below the surface, there is also the possibility of a lateral increase in area. However, the main cause of growth in the cylinder of bone forming the shaft is periosteal deposition. At the endosteal surface many osteons and all kinds of lamina may be eroded to different de- 560 M. LOCKE Fig. 9. Changes in bone size and shape come from periosteal deposition coupled with endosteal erosion. A: The endosteal surface of growing bones is often irregular, as though erosion has followed a different pattern from deposition. Iron sulfide-stained transverse profile of young beef humerus. B: In some mature bones the endosteal surface cuts diagonally across circumferentially oriented layers of laminae. This suggests that the final shape of a bone depends on specific patterns of erosion as well as outer surface deposition. Mercury sulfide-stained transverse profile of deer cannon bone. Scale bar ⫽ 1 mm. C: Increase in bone diameter with enlargement of the marrow core comes from erosion of the endosteal face coupled with deposition at the periosteal surface. Transverse profiles traced from the middle of the femur and humerus of pigs about 2 and 6 months old. Bone deposited early in development may be largely replaced during growth. Scale bar ⫽ 1 cm. grees at the same time, allowing for a change in shape from that originally mandated by the periosteal deposition (see fig 2.22 in Martin and Burr, 1989c). Change in bone size and shape come from periosteal deposition coupled with endosteal erosion, perhaps related to the lack of load on bone closest to the core. The endosteal surface of growing bones has an irregular surface, as though bone of all kinds is constantly being eroded (Fig. 9A, see also Fig. 4A). The endosteal face of mature bones often cuts diagonally across circumferentially oriented layers of laminae, showing that erosion follows a different pattern from deposition (Fig. 9B). The final shape of a bone therefore depends on specific patterns and extent of erosion as much as growth on the outer surface. Most bone deposited early in develop- ment may be replaced during growth. For example, transverse profiles from the middle of the femur and humerus of pigs about 2 months old can fit completely inside the bones at 6 months (Fig. 9C). Endosteal Laminae Form in Mature Bones Periosteal laminae form continually to make a cylinder of increasing diameter. Endosteal laminae deposited on the inner face at the same time would progressively occlude the lumen. However, endosteal bone is not at first deposited where it is found, but is derived from periosteal laminae. Laminae are only deposited at the endosteal surface at the conclusion of growth (Fig. 10A). They often appear to tidy up the irregular surfaces sur- STRUCTURE OF LONG BONES IN MAMMALS 561 Fig. 10. A: Endosteal laminae of old bones form in situ, covering over secondary osteons and the eroded surface of laminae formed earlier at the periosteal surface. O, osteonic layer; L, endosteal laminae. Silver-stained transverse profile of a 3-year-old buffalo femur. Scale bar ⫽ 0.1 mm. viving erosion. Thus, although endosteal and periosteal bone cylinders may be structurally similar, their genesis can be different. Endosteal laminae may be the remains of periosteal laminae that have survived erosion, but in older bones they are a late-stage deposition on the inner surface after erosion and osteon insertion is complete. These observations confirm the very beautiful photomicrograph of late-stage endosteal deposition in fluorescently labeled horse bones by Stover et al. (1992). Why Bones Are White Rather Than Red or Pink In spite of their relatively rich blood supply, compact bones are white rather than red or pink. There are two obvious reasons for this. Although even very fine capillaries can be clearly resolved as pink threads (e.g., Fig. 2A), the proportion of the profile displaying blood vessels is small. Second, many bones have been partially exsanguinated, although even such bones contain many vessels with blood. Bones from animals chosen because they had not been exsanguinated were still not very pink. Cleared but unstained bone showed blood restricted to only a few vessels. While blood was usually present in capillaries of peripheral laminae and in osteons, it was often absent from more centrally located laminae containing osteons. Blood loss and the small diameter of capillaries may therefore not be the whole reason for white bones. To test whether parts of the vascular compartment were intact but bloodless, unstained bones known not to be exsanguinated and bones with clearly observable blood were studied. Typically, capillary networks in newly formed outer laminae contained blood, as did osteons. Capillaries in central laminae lacked blood and shone white and empty, especially around newly forming osteons (Fig. 11A). Unstained preparations of a human femur showed blood in osteons, but little or none in surviving laminae (Fig. 11B). This was not because the vascular compartments of the laminae had disappeared. Subsequent staining of the same preparation showed laminar structure all around the osteons (Fig. 11C). The idea that not all vascular compartments contain blood-filled capillaries agrees with the observations that osteons lose their connections with the capillary sheets from which they have been derived (Fig. 11D, see Osteons Form by Erosion…). Blood might be expected to be absent from such capillaries. The flow of blood to all bones in the rat, rabbit, dog, and man has been estimated to be 4 –10% of cardiac output (Shim, 1968). It would therefore be an economy to reduce the flow through mature laminar bone that had minimal metabolic activity. Blood is readily observed in the capillaries of new network sheets (Fig. 1A) and in the center of osteons of older bone (Fig. 11B), but not in both where they occur together (Fig. 11A). The question is not whether capillary network sheets cease to be functional, but when. In many mature bones, the only relict of primary laminar structure lies in the arrangement of osteons that follows that of the capillary network sheets into which they have been inserted (Fig. 11E). All blood has been transferred to the osteons. The absence of blood in old capillary network sheets may correlate with local degeneration of the vascular compartment, explaining why 562 M. LOCKE Figure 11 STRUCTURE OF LONG BONES IN MAMMALS laminar bone has so often been overlooked, why lamellae but not laminae have been described between osteons. DISCUSSION AND CONCLUSION The human bone most intensively examined in this study was from an older woman. The expectation that she would have had osteoporosis (Thompson, 1980) was confirmed by the endosteal erosion. There were also forming osteons, as well as a high frequency of degenerate ones, i.e., osteons enlarged by resorption. The formation of osteons in laminar bone throws a new light on osteoporosis. Most growing bones have all stages of osteon development, with resorption followed by cylindrical lamellar deposition. Osteoporotic bone has more in the resorptive phase, as if the message to complete a normal sequence has been blocked. The problem for osteoporosis may not only be increased resorption but a block to resecretion. Manzke et al. (1982) report cases of increased bone formation coupled with normal resorption that might be explained by increased conversion of laminar to osteonic bone. The seemingly great variety of compact bone described here can be resolved as the patterns made by a two-compartment system. Bone is topologically a tubular connective tissue compartment extending into a bone collagen compartment. The simplification should bring its study into the range of developmental biology and genetics, like the studies of tube growth in tracheal systems (Locke, 2001), or lung and kidney development (Metzger and Krasnow, 1999; Lubarsky and Krasnow, 2003). The bone two-compartment system may also be thought of as a functional response to the need for a separate environment that is both massive and locally controlled. Within it, collagen fibers can be oriented in lamellae under conditions that allow hydroxyapatite crystals to be deposited. The varied Fig. 11. Blood is often missing from laminar capillaries in some regions. A: Cleared but unstained bone shows blood (b) in newly forming laminae (l) at the surface and in osteons, but missing from older capillary networks around osteons. The empty capillaries (ecn) shine silvery white. Unstained transverse profile of pig humerus. B: Cleared, unstained human bone shows blood (b) in osteons but not in nearby laminae (L). Transverse profile of an unstained human femur. C: Osmium staining of the preparation in B showed that laminar vascular compartments continued to be present, suggesting that these parts of the vascular system survive but are bloodless. D: Osteons (o) forming from capillaries in laminae lose connections with capillary network sheets (cn). This could cause capillaries like those in A to be bloodless. Mercury sulfide-stained tangential profile of 3-year-old buffalo femur. A–D is the same magnification. Scale bar ⫽ 1 mm. E: In many mature bones the only relict of primary laminar structure lies in the arrangement of osteons that follows that of the capillary network sheets from which they have been derived. All blood has been transferred to the osteons. Mercury sulfide-stained transverse profile of horse femur. Scale bar ⫽ 1 mm. 563 patterns of laminae show the versatility of the system. Sheets of bone can be deposited with any orientation, transverse radial and diagonal radial as well as axial circumferential. The idea of bone as a two-compartment system also has implications for its electrical properties. Conduction could be different in each compartment, as well as along the membrane that separates them. An important difference between laminar and osteonic organization lies in the size of their bone compartments. Although only lamellae in the immediate vicinity of a laminar capillary are eroded when an osteon forms, laminar bone is essentially continuous, with a reticular blood supply. This might make it difficult to effect local morphogenesis. Secondary osteonic bone, on the other hand, forms small local compartments bounded by cement sheaths that lend themselves to resorption and redeposition. During osteoporosis, osteons can be resorbed one by one. Capillary network sheets are ideally patterned for the function of supplying precursors for rapid bone deposition. However, functional capillary network sheets would cause a purposeless resistance to blood flow were they to be retained after the completion of a lamina. It is therefore perhaps not surprising that they cease to contain blood at maturity, when the osteonic capillaries flowing in straight cylinders would give much less resistance. It may be significant that the network sheet capillaries are easily infiltrated with oil, suggesting that they have lipophilic linings. A lipophilic lining could have the dual property of low surface drag, giving reduced resistance to aqueous fluid flow while functional, combined with easy filling of the lumen with air, as seems to happen after nearby osteon formation. Capillaries with hydrophilic linings would have difficulty emptying blood or lymph due to their capillarity. The results suggest that there is still a need for descriptive work on different kinds of bone, their development, structure in relation to function and bone type, and phylogeny. A detailed inventory of bone microstructure of the kind begun by Enlow and Brown (1956, 1957, 1958) might make it possible to identify species, kind of bone, region, and stage of development from fragments, information of interest to systematists, archeologists, and forensic scientists. We may conclude by agreeing with von Ebner (1875) that “the major difficulty of skeletal analysis lies in the heterogeneity of bone, so that its distinctive structure and function may be understood only when every component has been analyzed in all its ontogenetic aspects…” (quoted in Ascenzi, 1983, p. 233). ACKNOWLEDGMENTS I thank Drs. B.A. Flumerfelt and P. Haase, Anatomy Department, University of Western Ontario, for supplying the human bone; Professors J.D. Currey, 564 M. LOCKE R. Dean, B. Hall, D. McMillan, and S. Weiner for careful review and very helpful comments on the manuscript; and R. Nichol and P.C. Gould for invaluable help with literature searches. LITERATURE CITED Aarden EMB, Burger EH, Nijweide PJ. 1994. Function of osteocytes in bone. J Cell Biochem 55:287–299. Arsenault AL. 1990. Vascular canals in bovine cortical bone studied by corrosion casting. Calc Tissue Int 47:320 –325. Ascenzi A. 1983. Microscopic dissection and isolation of bone constituents. In: Kunin AS, Simmons DJ, editors. Skeletal research: an experimental approach, vol. 2. New York: Academic Press. p 185–236. Bargmann W. 1967. Histologie und Mikroskopische Anatomie des Menschen. Stuttgart: Georg Thieme. Berry JL. 1979. A technique for microangiographic analysis of bone. Calc Tissue Int 29:179 –180. Bloom W, Fawcett DW. 1975. A textbook of histology. Philadelphia: W.B. Saunders. Cormack DH. 1984. Introduction to histology. Philadelphia: J.B. Lippincott. Currey JD. 1982. ’Osteons’ in biomechanical literature. J Biomech 15:717. Currey JD. 2002. Bones: structure and mechanics. Princeton, NJ: Princeton University Press. De Saint-Georges L, Miller SC. 1992. The microcirculation of bone and marrow in the diaphysis of the rat hemopoietic long bones. Anat Rec 233:169 –177. di Fiore MSH. 1981. Atlas of human histology. Philadelphia: Lea and Febiger. Ebner von. 1875. Quoted in Ascenzi A. 1983. Microscopic dissection and isolation of bone constituents. In: Kunin AS, Simmons DJ, editors. Skeletal research: an experimental approach, vol. 2. New York: Academic Press. p 185–236. Elias HE, Pauly JE. 1966. Human microanatomy. Philadelphia: F.A. Davis. Enlow DH, Brown SO. 1956. A comparative histological study of fossil and recent bone tissues. Part I. Tex J Sci 8:405– 443. Enlow DH, Brown SO. 1957. A comparative histological study of fossil and recent bone tissues. Part II. Tex J Sci 9:186 –214. Enlow DH, Brown SO. 1958. A comparative histological study of fossil and recent bone tissues. Part III. Tex J Sci 10:187–230. Fawcett DW. 1994. A textbook of histology. New York: Chapman and Hall. Giraud-Guille MM. 1988. Twisted plywood architecture of collagen fibrils in human compact bone osteons. Calc Tissue Int 42:167–180. Halstead LB. 1974. Vertebrate hard tissues. London: Wykeham. Ham AW. 1974. Histology. Philadelphia: J.B. Lippincott. Han SS, Holmstedt JOV. 1981. Human microscopic anatomy. New York: McGraw Hill. Jee WSS, Bartley MHJ, Cooper RR, Dockum NL. 1970. Bone structure. In: Andersen AC, Good LS, editors. The beagle as an experimental dog, vol. 1. Ames: Iowa State University Press. p 162–187. Krstic RV. 1978. Die Gewebe des Menschen und der Saugetiere. Berlin: Springer. Krstic RV. 1984. Illustrated encyclopedia of human histology. Berlin: Springer. Krstic RV. 1991. Human microscopic anatomy. An atlas for students of medicine and biology. Berlin: Springer. Locke M. 2001. Insects for studying fundamental problems in biology. J Insect Physiol 47:495–507. Locke M, Dean RL. 2003. Vascular spaces in compact bone. Am Biol Teacher 65:701–707. Lubarsky B, Krasnow MA. 2003. Tube morphogenesis: making and shaping biological tubes. Cell 112:19 –28. Manzke E, Gruber HE, Hiness RW, Baylink DJ. 1982. Skeletal remodeling and bone related hormones in two adults with increased bone mass. Metabolism 31:25–32. Marotti G. 1993. A new theory of bone lamellation. Calc Tissue Int 53:S47–S56. Martin RB, Burr DB. 1989a. The historical development of concepts surrounding the structure and function of bone. In: Structure, function and adaptation of compact bone. New York: Raven Press. p 1–17. Martin RB, Burr DB. 1989b. The microscopic structure of bone. In: Structure, function and adaptation of compact bone. New York: Raven Press. p 18 –56. Martin RB, Burr DB. 1989c. The formation of secondary osteons. In: Structure, function and adaptation of compact bone. New York: Raven Press. p 105–142. Metzger RJ. Krasnow MA. 1999. Genetic control of branching morphogenesis. Science 284:1635–1639. Moller JF, Robertsen K, Bunger C, Hansen ES. 1997. Improved method for examination of microvascular structures in bone tissue. Clin Orthop Res 334:15–23. Ohtani O, Gannon B, Ohtsuka A, Murakami T. 1982. The microvasculature of bone and especially of bone marrow as studied by scanning electron microscopy of vascular casts—a review. Scan Elect Microsc 1:427– 434. Oni OO, Gregg PJ. 1990. The relative contribution of individual osseous circulations to diaphyseal cortical blood supply. J Orthopaed Trauma 4:441– 448. Pannarale L, Morini S, D’Ubaldo E, Gaudio E, Marinozzi G. 1997. SEM corrosion-casts study of the microcirculation of the flat bones in the rat. Anat Rec 247:462– 471. Parfitt AM. 1994. Osteonal and hemi-osteonal remodeling: the spatial and temporal framework for signal traffic in adult human bone. J Cell Biochem 55:273–286. Schultz M. 1999. Microscopic investigation in fossil hominoidea: a clue to taxonomy, functional anatomy, and the history of diseases. Anat Rec 257:225–232. Schultz M. 2001. Paleohistopathology of bone: a new approach to the study of ancient diseases. Phys Anthropol 44:106 –147. Seliger WG. 1970. Tissue fluid movement in compact bone. Anat Rec 166:247–255. Shim SS. 1968. Physiology of blood circulation of bone. J. Bone Joint Surg 50A:812– 824. Stover SM, Pool RR, Martin RB, Morgan JP. 1992. Histological features of the dorsal cortex of the third metacarpal bone middiaphysis during postnatal growth in thoroughbred horses. J Anat 181:455– 469. Thompson DD. 1980. Age changes in bone mineralization, cortical thickness, and Haversian canal area. Calc Tissue Int 31:5–11. Wainwright SA, Biggs WD, Currey JD, Gosline JM. 1976. Mechanical design in organisms. London: Edward Arnold. Weiner S, Wagner HD. 1998. The material bone: structuremechanical function relations. Annu Rev Mat Sci 28:271–298. Weiner S, Arad T, Sabany I, Traub W. 1997. Rotated plywood structure of primary lamellar bone in the rat: orientations of the collagen fibril array. Bone 20:509 –514. Weiner S, Traub W, Wagner HD. 1999. Lamellar bone: structurefunction relations. J Struct Biol 126:241–255. Winet H. 1989. A horizontal intravital microscope-plus-bone chamber system for observing bone microcirculation. Microvasc Res 37:105–114. Yuehue H, Kylie A, Martin L. 2003. Handbook of histological methods for bone and cartilage. Totowa, NJ: Humana Press. APPENDIX Glossary Basic multicellular unit (BMU) The collection of cells involved in creating secondary osteons in bone remodeling (Martin and Burr, 1989a; Parfitt, 1994). Bone compartments The flat stacks (laminar) or cylinders (osteonic) of bone separated from one another by vascular compartments. STRUCTURE OF LONG BONES IN MAMMALS Capillary network sheets The vasculature between bone laminae. Cement sheath The boundary of uncertain composition and permeability that separates secondary osteons from their surroundings. Circumferential lamellae Lamellae at the endosteal and periosteal surfaces surviving from stacks of laminae after the loss of their capillary network sheets. Circumferential system Laminae and/or lamellae at the endosteal and periosteal surfaces surviving from stacks of laminae after varying degrees of loss of their capillary network sheets. Endosteum The layer of cells, connective tissue and blood vessels lining the inner face of hollow bones. Haversian system The older word for groups of osteons (American journals) or osteones (British journals). Secondary osteon (Currey, 1982). Interstitial lamellae Derived from laminar bone, filling some of the space between osteons after the loss of capillary network sheets. Lamellae Bone layers in both laminar and osteonic bone, each consisting of a 20 –50-m thick layer of collagen fibers on which calcium salts may be deposited. The fiber orientation varies, often changing from lamella to lamella like the layers in plywood or interspersed with nonlamellar orientations. The orientation determines the different kinds of bone (woven, parallel fibered, lamellar, fibrolamellar) described at the ultrastructural level by Weiner et al. (1999), Currey (2002), and others. 565 Laminae Primary bone made from 4 –20 lamellae laid down between capillary network sheets and surviving as interstitial lamellae between osteons and in endosteal and periosteal layers. Laminar bone is always primary. Osteoblast Cell concerned with bone deposition. Osteoclast Cell concerned with bone resorption. Osteocyte Bone cell formed by the incorporation of an osteoblast into the bone matrix (Aarden et al., 1994). Osteoid Preosseous tissue, lamellae before ossification. Osteon A cylinder of concentric lamellae around a tubular space containing blood vessels. Primary osteons form at the periosteal surface of bones nearing maturity and lack a cement sheath. Secondary osteons are a replacement of laminar bone forming around blood vessels derived from capillary networks (Currey, 1982), or the basic multicellular unit (BMU) in bone remodeling (Parfitt, 1994). They have a cement sheath. Periosteum The layer of cells, connective tissue, and blood vessels that protects the outer surface of bones. Vascular compartment The compartment containing capillary networks or osteonic blood vessels and connective tissue, separated by an epithelium from the bone compartment. Volkmann’s canals The radially oriented spaces with blood vessels connecting capillary sheets and to a lesser extent, osteons. They are often diagonal to the long axis.