ARTICLE IN PRESS
Appetite 48 (2007) 145–153
www.elsevier.com/locate/appet
Research report
Vagus nerve stimulation acutely alters food craving
in adults with depression
Jamie S. Bodenlosa,, Samet Koseb, Jeffrey J. Borckardtb, Ziad Nahasb,
Darlene Shawc, Patrick M. O’Neild, Mark S. Georgeb
a
Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, 165 Cannon Street,
3rd Floor, P.O. Box 250852, Charleston, SC 29425, USA
b
Brain Stimulation Laboratory, Institute of Psychiatry, Medical University of South Carolina, 5-North, 67 President Street, Charleston, SC 29425, USA
c
Counseling and Psychological Services Center, Medical University of South Carolina, Charleston, SC 29425, USA
d
Weight Management Center, Medical University of South Carolina, Charleston, SC 29425, USA
Received 21 June 2006; received in revised form 17 July 2006; accepted 19 July 2006
Abstract
Vagus nerve stimulation (VNS) is now available as a treatment for epilepsy and treatment-resistant depression. The vagus nerve plays
a central role in satiety and short-term regulation of food intake and research suggests a relationship between VNS and weight loss. The
underlying mechanisms of this relationship are unknown. The purpose of the current study was to determine whether acute cervical VNS
might temporarily alter food cravings. Thirty-three participants were recruited for three groups; depression VNS, depression non-VNS,
and healthy controls. Participants viewed 22 computerized images of foods twice in one session and completed ratings for food cravings
after each image. The VNS participants’ devices were turned on for one viewing of an image and off for the other (randomized order).
Participants were blind to VNS condition (on versus off). Acute VNS device activation was associated with a significant change in
cravings-ratings for sweet foods. A significant proportion of variability in VNS-related changes in cravings was accounted for by
patients’ clinical VNS device settings, acute level of depression, and body mass. Further studies are warranted addressing how acute or
chronic VNS might modify eating behavior and weight.
r 2006 Elsevier Ltd. All rights reserved.
Keywords: Vagus nerve stimulation; VNS; Obesity; Food cravings; Brain stimulation; Depression
Introduction
Vagus nerve stimulation
Clinicians are investigating several new brain stimulation
techniques, such as vagus nerve stimulation (VNS), to treat
psychiatric disorders including depression, anxiety, and
bipolar disorder (Marangell et al., 2002; Mu et al., 2004;
Nadkarni, LaJoie, & Devinsky, 2005; Rush et al., 2000;
Sackeim et al., 2001). The vagus nerve, one of 12 cranial
Corresponding author. Tel.: +1 508 856 6542.
E-mail addresses: jamie.bodenlos@umassmed.edu (J.S. Bodenlos),
kose@musc.edu (S. Kose), borckard@musc.edu (J.J. Borckardt), nahasz@musc.edu (Z. Nahas), shawd@musc.edu (D. Shaw), oneilp@musc.edu (P.M. O’Neil), georgem@musc.edu (M.S. George).
0195-6663/$ - see front matter r 2006 Elsevier Ltd. All rights reserved.
doi:10.1016/j.appet.2006.07.080
nerves, carries information to and from the brain to major
organs including the heart, stomach, lungs and esophagus.
Electrical stimulation of the vagus afferents (information
traveling to the brain from the body) results in activation
and/or inhibition of brain stem structures such as the
medulla and the nucleus of the tractus solitarius (NTS)
(George et al., 2000). These inputs are then conveyed to
widespread bilateral areas of the cerebral cortex, diencephalon and limbic lobe (Bohning et al., 2001; Chae et al.,
2003; Henry, 2002; Lomarev et al., 2002; Mu et al., 2004).
VNS involves implantation of a small generator under
the skin overlying a patient’s chest. An electrode is
threaded from the generator subcutaneously and attached
to the left-cervical vagus nerve. By placing a computercontrolled magnetic wand over the chest of a patient with a
VNS implant, a clinician can adjust various parameters of
ARTICLE IN PRESS
146
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
the stimulation including the output current intensity
(mA), the frequency (Hz), the pulse-width (ms), stimulus
on-time (seconds) and stimulus off-time (minutes). Various
VNS stimulation parameters have been associated with
activation of different brain areas (Lomarev et al., 2002;
Mu et al, 2004).
VNS was initially approved by the Federal Drug
Administration (FDA) as a treatment for intractable
epilepsy (Tecoma & Iragui, 2006; Uthman, 2000). Since
its approval, VNS has been investigated for several other
clinical applications including depression (Marangell et al.,
2002; Mu et al., 2004; Rush et al., 2000; Sackeim et al.,
2001), and chronic pain (Borckardt, Kozel, Anderson,
Walker, & George, 2005). VNS has recently received FDA
approval as a treatment for treatment-resistant depression
(George et al., 2000; Rush et al., 2000, 2003; Sackeim et al.,
2001).
Few studies examining cervical VNS and weight have
been conducted in humans. In patients who received
cervical VNS for the treatment of epilepsy, 62% experienced significant weight loss. In this sample (N ¼ 27), the
patients with higher output settings for the VNS device
were more likely to lose weight (Burneo et al., 2002). It is
not known whether this VNS-related weight-loss was
caused by changes in metabolism, decreases in fat stores,
changes in hunger and/or satiety signaling in the brain,
changes in food cravings, or by some other mechanism. In
the pivotal study of VNS in treatment-resistant depression,
there was no effect on weight (Rush, Marangell et al., 2005;
Rush, Sackeim et al., 2005). More research is needed to
understand the relationship between VNS and weight
change in humans.
Vagus nerve stimulation and weight change
The relationship between mood and eating behaviors has
long been of interest to researchers (Canetti, Bachar, &
Berry, 2002). Studies have sought to examine how mood
affects not only the amount of food consumed but also the
types of foods eaten. Lyman (1982) found that individuals
were more likely to consume healthy foods during positive
emotions and more likely to consume unhealthy foods
when experiencing negative emotions. Other research
suggests that the meals eaten when experiencing positive
or negative moods are larger in portion than those eaten
during a neutral mood (Patel & Schlundt, 2001). More
recent research has focused on understanding the role of
specific mood states in eating and food cravings. Certain
moods, such as anger or joy, have been found to have a
greater influence on eating than sadness or fear (Macht,
1999). Depressive symptoms in individuals are associated
with higher BMIs, more eating concerns, and lower selfesteem (Werrij, Mulkens, Hospers, & Jansen, 2006).
Recently, Killgore & Yurgelun-Todd (2006) found that
affect differentially predicted regional cerebral responses to
high versus low calorie foods. Their research suggests that
there may be a neurobiologic substrate underlying the
tendency for increased food cravings found for high-calorie
foods during heightened negative emotions. In summary,
this research demonstrates that mood affects food cravings
and the amount and types of food consumed.
There has been a growing interest in the use of VNS to
study and treat obesity (Roslin & Kurian, 2001; Sobocki et
al., 2001). This is an especially important area of research
given that 65% of Americans are overweight or obese
(Hedley et al., 2004). VNS is a logical choice for study
because the vagus nerve has long been linked to
neurological systems associated with hunger and satiety
and it plays a central role in the short-term regulation of
food intake (Havel, 2001). There is evidence, in animals
and humans, that neurostimulation interventions (like
VNS) can be used to impact eating behavior and weight
loss (Burneo, Faught, Knowlton, Morawetz, & Kuzniecky,
2002; Cigaina, 2002; Roslin & Kurian, 2001; Sobocki,
Krolczyk, Herman, Matyja, & Thor, 2005).
Experimental research with animals has found that
stimulation of the vagus nerve, both through thoracotomy
and laparotomy access, has an influence on food intake and
body weight (Sobocki et al., 2005). In a study with normal
weight mongrel dogs, chronic intermittent high-dose VNS
within the thorax resulted in substantial weight loss. The
dogs took longer to consume their food and failed to finish
the food on their plate, an unusual phenomenon for this
type of dog (Roslin & Kurian, 2001). In another study with
animals, Sobocki and colleagues found VNS (stimulation
of the abdominal part of the vagus nerve) was associated
with a significant difference in body mass in a sample of
non-obese pigs. There was a significantly different change
in the ratio of fat for the pigs that received VNS versus the
pigs that did not, but no effect on metabolism was found.
Results of this study suggest that VNS reduces body mass
in animals specifically through its influence on decreasing
fat stores (Sobocki, Fourtanier, Estany, & Otal, 2006).
Overall, the past research examining VNS in animals
demonstrates that VNS affects eating behaviors, weight,
and body composition, although the majority of these
studies stimulated the vagus closer to the stomach than is
done with cervical VNS used in humans.
Mood and eating behaviors
Purpose and aims of the current study
The current project sought to investigate whether acute
left cervical VNS might temporarily affect food cravings in
patients with chronic, treatment-resistant depression. As
past research with animals and humans demonstrates, VNS
is associated with changes in eating behaviors and weight
(Burneo et al., 2002; Sobocki et al., 2005). However, does
left cervical VNS altering metabolism or decrease food
cravings? Currently, there are no published studies that
have systematically investigated the effects of left cervical
VNS on food cravings in humans. Examining the acute
ARTICLE IN PRESS
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
147
Table 1
Individual participants’ clinical VNS settings and number of months each subject had been undergoing VNS therapy for depression at the time of study
enrollment
Subject
Output current (mA)
Frequency (Hz)
Pulse width (ms)
On-time (s)
Off-time (min)
Time with VNS (months)
1
2
3
4
5
6
7
8
9
10
11
0.50
1.25
1.25
0.75
1.25
1.00
1.00
0.50
1.50
0.75
1.25
20
20
20
20
20
20
20
20
20
20
20
250
250
500
500
250
250
250
250
250
250
250
14
7
30
30
30
30
21
30
30
30
30
3
3
3
5
5
3
5
3
5
5
3
78.0
0.5
60.0
72.0
60.0
84.0
66.0
60.0
63.0
1.0
60.0
effects of VNS on food cravings in a laboratory setting may
provide insights into possible mechanisms of action of
VNS for weight-loss. As VNS has recently been approved
as a long-term therapy for treatment-resistant depression,
studying the acute effects of VNS on cravings in individuals
receiving VNS for depression is a logical place to begin.
The specific aims of the current study were to: (1) assess
differences between three groups of patients (depression
VNS, depression non-VNS, healthy controls) on food
cravings for different types of foods (proteins, fruits/
vegetables, sweets), after controlling for time of last meal,
(2) determine the effects of acute VNS device-activation
(on versus off) on food cravings in adults with depression
and (3) understand whether participants’ clinical VNS
device settings, depression level and BMI would affect the
amount of VNS-related change in food cravings. It was
hypothesized that acute VNS device-activation would be
associated with detectable changes in food cravings in
patients receiving VNS for depression.
Method
Participants
Thirty-three participants were recruited to participate in
the study from the Brain Stimulation Laboratory and
Mood Disorders Clinic at the Medical University of South
Carolina. Eleven participants were recruited for each of
three groups; participants receiving VNS therapy for
depression; non-VNS patients with depression; and healthy
controls (without VNS or depression). Depressed participants were recruited from the Mood Disorders Clinic
where participants received treatment for treatment-resistant depression. The participants were contacted to provide
information about the study and were scheduled for an
appointment if they expressed interest. The requirement
was that the individuals had a past diagnosis of depression,
specifically treatment-resistant type. Groups were then
subdivided based on VNS treatment. Healthy controls were
recruited from the medical university community. All VNS
participants had the device implanted for treatment-
resistant depression, and the background device-settings
employed in this study (i.e., output current, frequency,
pulse-width, on-time, off-time) were the clinical settings
determined by the treating psychiatrist (and thus were
different for each subject). The clinical settings employed
for each individual along with the time they had been
receiving VNS therapy for depression are listed in Table 1.
Of the 33 participants, 18 were women (54.5%) and 15
(45.5%) were men. The majority of participants were
Caucasian (81.8%), and the mean age was 43.55 years
(range ¼ 23–64). Most had a body mass index (BMI) in the
normal range (42.4%) and did not smoke (87.9%). Scores
from the Beck Depression Inventory suggest that 18.2%
(N ¼ 2) of VNS participants with depression, 60% (N ¼ 6)
of non-VNS with depression participants, and 0.09%
(N ¼ 1) of healthy controls had moderate to severe
depressive symptoms (BDI score greater than 19) at the
time of participation in the study. Self-reported antidepressant use obtained from all participants. Eighty-two
percent (N ¼ 9) of VNS participants with depression were
taking antidepressants versus the 55% (N ¼ 6) of nonVNS participants with depression. No healthy control
participants reported taking antidepressants. See Tables 2
and 3 for participant information for the overall sample
and specific groups (depression VNS, depression non-VNS,
and controls).
Measures
Beck depression inventory-II (BDI-II)
The BDI-II consists of 21 items assessing symptoms of
depression experienced during the past 2 weeks (Beck,
Steer, & Brown, 1996). Each item contains four statements
reflecting varying degrees of symptom severity, and
respondents are instructed to circle the number (ranging
from zero to three, indicating increasing severity) that
corresponds with the statement that best describes them.
Ratings are summed to calculate a total BDI-II score,
which can range from 0 to 63. The BDI-II has demonstrated high internal consistency, good test-retest reliability, and good construct and concurrent validity with other
ARTICLE IN PRESS
148
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
Table 2
Participant characteristics by group (mean and standard deviation)
Age*
Hours last meal
Weight
BMI*
BDI score*
WSI event
WSI impact
EBI
EES A/F
EES dep
EES anxiety
PAR activity level
Weekday sleep
Weekend sleep
Depression VNS
Depression non-VNS
Controls
52.45 (8.78)
3.59 (2.92)
194.00 (29.27)
30.95 (3.58)
13.3 (8.88)
8.72 (4.54)
17.09 (11.73)
71.70 (11.47)
13.72 (10.23)
8.90 (4.86)
10.54 (8.72)
3.45 (3.73)
8.04 (3.26)
8.72 (3.06)
46.18
6.45
189.86
27.09
26.10
12.55
38.45
75.44
9.72
8.54
10.00
14.88
6.15
6.27
32.00
4.91
159.00
23.43
7.81
13.90
27.36
71.40
4.63
5.09
3.90
20.59
6.45
6.77
(11.57)
(5.98)
(61.87)
(6.14)
(16.19)
(5.56)
(33.74)
(12.95)
(11.03)
(5.22)
(7.98)
(18.53)
(2.58)
(2.89)
(8.40)
(2.89)
(30.36)
(3.43)
(6.83)
(7.27)
(18.35)
(10.35)
(5.76)
(3.91)
(4.43)
(21.84)
(0.93)
(1.12)
*Significant difference between the groups, po0.05.
Table 3
Parameters from exploratory regression analyses predicting VNS-related changes in cravings for sweet foods among participants undergoing VNS therapy
for depression at the time of the study (adjusted R2 ¼ 0.975)
Variable
Beta
Std. error
Std. beta
t-Value
Sig.
(Constant)
Clinical VNS output current setting
Clinical VNS stimulation on-time
Clinical VNS stimulation off-time
Body mass index
Depression emotional eating
Beck Depression Inventory total score
72.381
13.572
0.843
0.039
1.990
1.281
0.287
6.589
1.915
0.068
0.008
0.177
0.107
0.059
0.582
0.886
0.306
0.941
0.803
0.318
10.97
7.09
12.45
4.71
11.25
12.01
4.84
0.002
0.006
0.001
0.018
0.002
0.001
0.017
common measures of depression in clinical and non-clinical
samples (Beck et al., 1996; Whisman, Perez, & Ramel,
2000).
emerge: Anger/Frustration, Anxiety, and Depression. The
EES has been found to have good internal consistency for
the entire scale (coefficient alpha ¼ 0.81) and for the three
factors Anger/Frustration, Anxiety, and Depression subscales with coefficient alphas of 0.78, 0.78, and 0.72,
respectively, and adequate test–retest reliability (r ¼ 0.79;
Arnow et al., 1995).
The eating behavior inventory (EBI)
O’Neil and colleagues (1979) developed the EBI to assess
specific behaviors that have been found to be theoretically
linked to weight management. Both positive and negative
behaviors are assessed through the 26-item scale. Items are
ranked on a 5-item frequency scale, ranging from ‘‘never or
hardly ever’’ engage in a particular behavior to ‘‘always or
almost always’’. The range of scores is from 26 to 130, with
higher scores indicating more positive eating behaviors that
are likely conducive to weight loss. A recent review of over
20 studies utilizing the EBI, suggests that it is a valid tool in
measuring changes in weight management behavior and
correlates positively with weight loss (O’Neil & Reider,
2005).
Seven-day physical activity recall (PAR)
The PAR (Sallis et al., 1985) is a self-report measure with
eight items concerning the duration, intensity, and volume
of physical activity over the past week. Participants
reported the number of hours spent sleeping, and engaging
in moderate, hard, and very hard activity. The 2-week
test–retest reliability (r ¼ 0.69) and concurrent validity
(r’s ¼ 0.82–0.94) of the PAR were satisfactory (Rauh,
Hovell, Sallis, & Hofstetter, 1992; Dishman & Steinhardt,
1988).
The emotional eating scale (EES)
The EES is a 25-item scale that measures urges to eat
when experiencing different emotions (Arnow, Kenardy, &
Agras, 1995). The scale utilizes a 5-point Likert response
format from ‘‘no desire to eat’’ to ‘‘a strong desire to eat’’.
Out of the 25 emotions listed on the measure, three factors
Weekly stress inventory short-form (WSI-SF)
The WSI-SF (Bodenlos et al., 2006) is a 25-item
inventory of daily unpleasant events, in which respondents
report events that occurred over the past week. Participants
indicate if each item occurred, and they rate the impact of
each event on a scale ranging from 1 (happened but not
ARTICLE IN PRESS
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
stressful) to 7 (extremely stressful). The WSI-SF reports
both an event score (i.e., number of events that occurred)
and an impact score (i.e., total perceived stressfulness of
endorsed items). The WSI-SF has shown high internal
consistency, with coefficients ranging from 0.91 to 0.92,
and good convergent validity with the WSI (Bodenlos
et al., 2006).
Procedure
All participants
Participants arrived at the Brain Stimulation Laboratory
at the Medical University of South Carolina and written
informed consent was obtained. Height of the participants
was obtained via self-report and a scale was used to attain
the participants’ weights. Body mass index (BMI) was
calculated based on this information. Participants were
asked when their last meal was consumed and the content
of that meal.
After completing the initial assessment and the questionnaires, the participants were taken to a laboratory
room in the Brain Stimulation Laboratory. Participants
were seated at a computer where a series of standardized
color food images from the International Affective Picture
System (IAPS) were shown on the screen. The use of twodimensional food pictures in cravings studies is a widely
used methodology and has been shown to produce unique
cortical and subcortical activation relative to pictures of
non-food items (Killgore et al., 2003). Twenty-two images
of foods (e.g., ice cream, cake, cheese-burgers, pizza, fruits,
meats, vegetables) were presented for four seconds each.
Each of the pictures was presented to each participant for
two separate viewings within one session. That is,
participants viewed the first 22 food images (presented in
a random order), and then viewed the same pictures over
again (a total of 44 food images) in the same order, in one
block of time (close to 1 h) without interruption. Participants used a computerized visual analog scale (CVAS) to
rate how much they ‘‘would like to eat each food right
now’’ if it were actually available to them. The CVAS was
anchored with ‘‘not at all’’ and ‘‘very much’’, and the
computer converted the visual ratings to numbers ranging
from 0 to 100. Additionally, for each food, participants
were asked to indicate how well they would ‘‘be able to
resist tasting it’’ using a CVAS anchored with ‘‘no trouble
resisting it at all’’ and ‘‘very challenging to resist’’. These
visual ratings were also reverted to numbers ranging from 0
to 100 by the computer. There was a screen between
pictures of the foods to prevent differential lengths of
viewing of particular foods. Participants viewed and
completed ratings for each picture immediately after it
was presented. The software for presenting the pictures,
randomizing picture order, collecting VAS ratings and
randomizing VNS-on/off condition was custom-developed
using RealBasic5.5.5 on the Macintosh Platform and the
program was run on a Macintosh G5 using the Mac OSX.4
operating system.
149
After completion of the questionnaires and laboratory
part of the study, all participants received a $50 reimbursement.
VNS participants
For VNS participants, information about clinical
settings of the VNS device was obtained and the
participants’ VNS device on-time was set to 7 s for the
duration of the study. VNS participants’ devices were
turned on for one viewing of the food images and turned
off for the other (randomly ordered). Participants were
blind to whether their devices were on or off for each trial.
Dependent variables
CVAS scores, for food cravings and confidence in
resisting food were compared for all VNS-on versus
VNS-off trials for VNS participants. Since the other
participants did not have VNS devices, ratings for subjects
in the other two groups were compared between the first
viewing and the second viewing of the food images.
Because the VNS on/off conditions were randomized for
subjects in the VNS group it was it was necessary to use the
absolute value of the change scores for statistical analyses
that involved between-group comparisons in order to
ensure a common metric. The changes scores between
viewings were calculated as the absolute value of trial1 minus trial-2 for non-VNS subjects and the absolute
value of each VNS-on trial minus the VNS-off trial for
subjects in the VNS group. Additionally, change scores
were further divided into each food grouping of interest
(proteins, fruits/ vegetables, sweets).
Results
Group characteristics
In order to assess the groups on overall differences
ANOVAS were performed (see Table 2 for means and
standard deviations for measures). Groups differed on age,
(F (2, 30) ¼ 12.87, p ¼ 0.000), score on the BDI, (F (2,
28) ¼ 7.21, p ¼ 0.003), and BMI, (F (2, 30) ¼ 7.47,
p ¼ 0.002). LSD post-hoc analyses revealed significant
differences for age between control (M ¼ 26.36) and
depression VNS (M ¼ 46.56) groups as well as control
and depression non-VNS (M ¼ 38.41) groups. Individuals
in the control group were significantly younger than those
in the depression non-VNS and depression VNS groups.
No significant differences between depression non-VNS
and depression VNS groups were found for age. For BDI
score, individuals in the depression non-VNS group
(M ¼ 26.1) had significantly higher scores on the BDI
(measure of depression) than those in the depression VNS
(M ¼ 13.3) and control groups (M ¼ 7.81). Significant
differences were not found between the depression VNS
and control groups. Individuals in the control group
(M ¼ 23.42) had significantly lower BMIs than those in
the depression VNS (M ¼ 30.94) or depression non-VNS
ARTICLE IN PRESS
150
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
groups (M ¼ 27.09). No differences were found between
depression VNS and depression non-VNS groups for BMI.
25
Sweets
Proteins
Vegetables
20
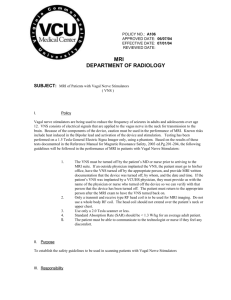
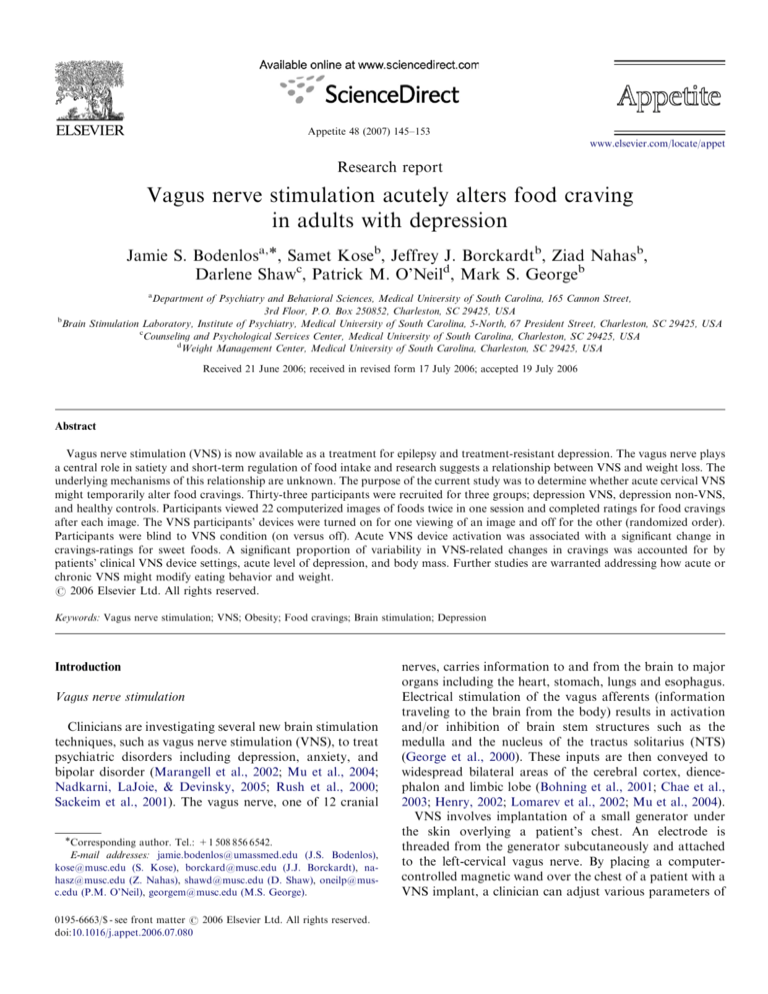
Differences in cravings between groups
15
Changes in cravings between food picture viewings (VNS on
versus off)
Changes in ratings (cravings and ability to resist the
foods) between paired pictures across food groups (sweets,
vegetables/fruits, proteins) were assessed using MANCOVA controlling for time since last meal (in hours). The
absolute values of the change scores between the two
viewings of the food images were used to assess whether the
differences were random or related to turning the VNS
device on or off. With respect to cravings-ratings for
‘‘sweets’’, there was a significant main effect for group, (F
(2, 250) ¼ 3.36, p ¼ 0.05). Post-hoc analyses revealed that
there were significant differences between depression VNS
(M ¼ 17.09) and depression non-VNS (M ¼ 8.77) groups,
and between the depression VNS and healthy control
(M ¼ 7.73) groups. Individuals in the depression VNS
group had significantly higher absolute values for change
scores for cravings of ‘‘sweets’’ between viewings of food
images than did those individuals in the depression and
non-depression group suggesting that activation of the
VNS device was related to an acute change in cravings. Out
of the eleven participants in the depression VNS group,
54.5% (6 participants) had a decrease in food cravings,
from the on to off trials, and 45.5% had an increase in food
cravings (5 participants), from the on to off trials, for
sweets. No significant differences between depression nonVNS and control groups were found. No significant
between-group effects were found for proteins F(5,
26) ¼ 2.05, p ¼ ns, and vegetable/fruit groups F(5,
26) ¼ 2.05, p ¼ ns (see Fig. 1).
Next, exploratory regression analyses were conducted to
determine if variability in VNS-related changes in food
cravings for sweets could be accounted for by participantlevel variables including clinical VNS device settings,
depression-level and BMI. The exploratory model was
significant (F(3, 9) ¼ 59.37, p ¼ 0.003). The majority of
individual variability in VNS-related changes in food
cravings was accounted for by clinical VNS output current,
clinical VNS on-time, clinical VNS off-time, total score
from the Beck Depression Inventory, the Depression factor
10
5
S
N
V
ss
D
ep
re
ea
H
ed
lth
y
S
N
V
ss
ep
re
D
ea
H
ed
lth
y
S
N
V
ed
ss
D
ep
re
ea
lth
y
0
H
Multiple analysis of covariance (MANCOVA) was used
to assess whether there were differences between groups
(VNS, non-VNS depression, and healthy controls) with
respect to mean food cravings ratings and/or ratings of
confidence in ability to resist eating sweet foods, vegetables, and proteins (controlling for hours since last meal).
No effects were found (F(6, 12) ¼ 0.81, ns) suggesting that
groups did not differ with respect to their overall mean
cravings ratings or confidence in ability to resist eating
sweets, vegetables or proteins.
Group
Fig. 1. Absolute values for change in cravings between viewings of foods.
All participants saw each food image twice (randomly ordered), but
participants in the VNS group had their VNS devices turned on for one
viewing and off for the other (also randomly ordered).
from the Emotional Eating Scale, and BMI (adjusted
R2 ¼ 0.975). See Table 3 for parameters from the model.
Lower clinical output current, device on-time and BMI
were associated with VNS-related increases in sweets
cravings, whereas higher clinical device off-time, depression scores from the Beck Depression Inventory and
depression factor scores from the Emotional Eating Scale
were associated with VNS-related decreases in sweets
cravings.
Discussion
This was the first study to examine the effects that acute
left cervical VNS might have on food cravings in adults
with major depression. Our study found that the depression VNS group had greater differences in food cravings
between viewings of images in the sweet food category than
the other two groups (depression non-VNS and healthy
controls). As the VNS device was turned on for one
viewing and off for the other, the order of the VNS
condition was randomized, and the participants were blind
to VNS condition, it is likely that acute VNS had an impact
on food cravings. Significant differences in food cravings
between groups, for other food categories (proteins and
vegetables/fruits) were not found. No between group
differences were found for overall mean ratings for sweets,
vegetables or proteins. A significant proportion of the
variability in VNS-related changes in cravings for sweet
foods was accounted for by clinical VNS device settings,
depression scores and BMI.
Our hypothesis that the change scores between viewings
of food images would be larger in the VNS group than the
other two was partially supported in our study. Specifically, VNS participants demonstrated significantly different change scores for cravings of the ‘‘sweets’’, than both of
the other groups. While there is a substantial amount of
research in animal models that demonstrates that thoracic
ARTICLE IN PRESS
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
or abdominal VNS has an affect on weight and food intake
(Sobocki et al., 2005), this is the first study to demonstrate
the impact that acute VNS device activation has on food
cravings in humans. Food cravings are related to eating
behaviors and therefore they may have influence weight
change over time. This study provides initial evidence that
food cravings, at least for sweet foods, may be one
mechanism underlying the relationship between VNS and
eating behaviors and weight.
Interestingly, VNS had a differential impact on food
cravings for sweets in this sample. That is, approximately
half of the group experienced increases in cravings and the
other half experienced decreases in cravings when the VNS
device was on. Further analyses revealed that several
participant-level variables could explain 97.5% of the
variability in VNS-related changes on food cravings for
sweets. Specifically, decreased levels of VNS output
current, decreased VNS device on-time, and lower BMIs
were associated with increased food cravings for sweets. On
the other hand, increased device on-time, higher levels of
depression, and higher levels of emotional eating when
depressed were associated with decreased food cravings for
sweets. These variables may explain a majority of the
variability for the acute effects of VNS activation on food
cravings for sweets, but further investigation is necessary to
understand the impact of these variables and VNS on
eating behaviors and obesity in the long-term.
To understand how VNS may impact food cravings it is
useful to examine research with VNS and pain. Some
recent data on the effects of VNS on pain perception
suggest that during device activation, patients experience
an acute hypersensitivity to painful stimuli. However, in
the long-term, pain thresholds and pain tolerance are
increased (Borckardt et al., 2005; Kirchner, Birklein,
Stefan, & Handwerker, 2000; Ness, Fillingim, Randich,
Backensto, & Faught, 2000). This has led to the hypothesis
that VNS patients experience repeated periodic hypersensitivity to painful stimuli (when the VNS is actively
firing) which leads to down-regulation of central painperception mechanisms over time (Borckardt et al., 2005).
The same process may be involved in long-term VNS
effects on depression and obesity. It is possible that in the
short-term, VNS device activation (typically 30 s of
activation every 5 min in depression adults) is associated
with subtle increases in food cravings which, in the longterm, leads to a system-wide down-regulation of food
cravings and a subsequent change in eating behavior (i.e.,
weight loss). This relationship may be mediated by some of
the participant-level variables including VNS device
settings, depression level, BMI, and emotional eating
during depressed moods.
We did not find any differences in change scores between
the groups for resistance to eating the foods. It may be that
resistance to eating food is affected by other behavioral and
cognitive factors such as self-efficacy, body image, impulsiveness, conscientiousness of diet, and stimulus control
(only eating at certain times or in particular environments).
151
Although a person may endorse experiencing food cravings, it does not mean that this person will eat those foods.
Food cravings may be the underlying biological mechanism
that increases the likelihood of eating and resistance to
tasting food is affected by a multitude of factors.
Research has found that cravings for sweet foods are
associated with depression in both animals and humans
(Willner et al., 1998). This makes sense intuitively as sweets
taste good and are reinforcing. It is likely that when a
person is depressed, they seek out things that will make
them feel better, even if the effect is temporary. Sweets are
also high in sugar and calories and consumption of large
amounts, will likely lead to weight gain. What role did
VNS play in cravings for sweets? It may be that VNS had
an effect on areas of the brain that are associated with
reward and increased desire for high calorie foods. Pelchat
(2002) hypothesizes that the same brain areas associated
with alcohol and drug addiction may be related to food
cravings as well since there are many overlaps in
characteristics of these ‘‘cravings’’. As more investigators
are studying the neuroanatomical substrates related to
food cravings and hunger using fMRI (Killgore et al., 2003;
Killgore & Yurgelun-Todd, 2005; Pelchat, Johnson, Chan,
Valdez, & Ragland, 2004; St-Onge, Sy, Heymsfield, &
Hirsch, 2005), research incorporating fMRI and VNS may
be necessary to understand the brain areas that link VNS
and food cravings.
Limitations
There are several limitations to the current study that
should be noted. First, the samples used in the current
study were small with only eleven individuals in each
group. Second, the participants were not randomly selected
for this study or randomized to groups, which raises
selection bias threats. These groups were significantly
different from each other with respect to depression, BMI
and age. It would be more desirable to use homogenous
groups to study the variables in question in order to
control for the effects that these differences could have on
food cravings. However, individuals did serve as their own
control for depression, BMI, and age when examining
changes between viewings. It also important to note that
because the recruitment of participants was through the
Mood Disorders Clinic or the medical university community, generalizability of these findings is limited. Although
not significant, there were differences in activity levels
(based on the PAR) between the groups. The small sample
size likely decreased the power and ability to detect a
significant difference. In addition, several psychological
and behavioral variables that may have influenced eating
behavior/food cravings were not assessed including anxiety, mania, and substance use disorders. Further, it may
have been beneficial to obtain information on medical
conditions that may have influenced food intake and
cravings, such as diabetes mellitus where changes in diet
are necessary.
ARTICLE IN PRESS
152
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
Another limitation of the current study is that the
categorization of patients into groups was based on past
diagnoses of depression and not current depressive
symptoms. The groups were categorized based on assessments including the use of SCID interviews that were
conducted prior to participation in the current study (in the
VNS trials). It is likely that the differences in BDI scores
for several participants in the VNS and non-VNS
depressed groups were a result of their treatment response
to VNS and/or antidepressants. Lastly, we cannot say what
effect antidepressant treatment, the combination of antidepressants and VNS, and the chronic use of VNS has on
eating behavior/food craving in patients. Therefore, it
should be acknowledged that these variables might have
influenced our findings.
Future directions
More studies are needed to examine the effects that VNS
has on food cravings, eating behavior and weight-loss both
acutely and over time in depressed adults. As VNS is
beginning to be used more widely for patients with
treatment-resistant depression, research can examine how
VNS impacts not only food cravings but also eating
behaviors and weight throughout the course of treatment
for depression. It is important to assess depressed
individuals’ weight, food cravings, and eating behaviors
prior to implantation of the VNS device and obtain
baseline data before VNS treatment begins. Given that
depression is not the only psychological variable that may
affect food cravings, it would be beneficial to examine
other psychological (anxiety and substance use disorders)
and medical conditions that may impact this relationship
between VNS and food cravings. Studies are needed to
examine differences between obese and non-obese patients,
as cravings may be different in these groups. Further data
on the effects that cravings have on different brain areas
for VNS patients using fMRI data will aid in understanding the mechanisms that underlie the relationship
between food cravings and acute vagus stimulation. Future
research may also want to examine the effects of presenting
real food in a laboratory setting (not computer images of
food), as this is a way to objectively measure resistance to
eating certain foods. Real food would also allow expansion
of the cues an individual is presented with, combining both
olfactory and visual cues. Lastly, more control over the
hunger state and last meal eaten by participants may also
be addressed in future research.
Conclusion
As this is a new area of research, there are many studies
that can be conducted to examine how VNS relates to food
intake, eating behaviors and ultimately, obesity. Brain
stimulation techniques are being used in many disciplines
to aid in treatment of various disorders. The findings
presented in this paper demonstrate the impact that VNS
can have on immediate food cravings, especially with
sweets. Our study lends support for the need of further
research and examination of the use of these techniques,
like VNS, in the ongoing battle with obesity.
Acknowledgements
This study was funded in part by an intramural grant
through the University Research, Committee at the
Medical University of South Carolina.
References
Arnow, B., Kenardy, J., & Agras, W. S. (1995). The emotional eating
scale: The development of a measure to assess coping with negative
affect by eating. International Journal of Eating Disorders, 18(1), 79–90.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). BDI-II, Beck Depression
Inventory: Manual (2nd ed.). Boston, San Antonio, TX: Psychological
Corporation, Harcourt, Brace & Company.
Bodenlos, J. S., Cowles, M., Whitehead, D., Phadtre, M., Ancona, M.,
Jones, G., et al. (2006). Development and validation of the weekly
stress inventory—short form. Annals of Behavioral Medicine, 31, S103.
Bohning, D. E., Lomarev, M. P., Denslow, S., Nahas, Z., Shastri, A., &
George, M. S. (2001). Feasibility of vagus nerve stimulationsynchronized blood oxygenation level-dependent functional MRI.
Investigative Radiology, 36, 470–479.
Borckardt, J. J., Kozel, F. A., Anderson, B., Walker, A., & George, M. S.
(2005). Vagus nerve stimulation affects pain perception in depressed
adults. Pain Research and Management, 10(1), 9–15.
Burneo, J. G., Faught, E., Knowlton, R., Morawetz, R., & Kuzniecky, R.
(2002). Weight loss associated with vagus nerve stimulation. Neurology, 59(3), 463–464.
Canetti, L., Bachar, E., & Berry, E. M. (2002). Food and emotion.
Behavioural Processes, 60, 157–164.
Chae, J. H., Nahas, Z., Lomarev, M., Denslow, S., Lorberbaum, J. P.,
Bohning, D. E., et al. (2003). A review of functional neuroimaging
studies of vagus nerve stimulation (VNS). Journal of Psychiatry
Research, 37, 443–455.
Cigaina, V. (2002). Gastric pacing as a therapy for morbid obesity:
Preliminary results. Obesity Surgery(Suppl. 1), 12S–16S.
Dishman, R., & Steinhardt, M. (1988). Reliability and concurrent validity
for a 7-day recall of physical activity in college students. Medicine &
Science in Sports & Exercise, 20, 14–25.
George, M. S., Sackeim, H. A., Rush, A. J., Marangell, L. B., Nahas, Z.,
Husain, M. M., et al. (2000). Vagus nerve stimulation: A new tool for
brain research and therapy. Biological Psychiatry, 47, 287–295.
Havel, P. J. (2001). Peripheral signals conveying metabolic information to
the brain: Short-term and long-term regulation of food intake and
energy homeostasis. Experimental Biological Medicine, 226, 963–977.
Hedley, A. A., Ogden, C. L., Johnson, C. L., Carroll, M. D., Curtin, L. R.,
& Flegal, K. M. (2004). Prevalence of overweight and obesity among
US children, adolescents, and adults, 1999–2002. Journal of the
American Medical Association, 291, 2847–2850.
Henry, T. R. (2002). Therapeutic mechanisms of vagus nerve stimulation.
Neurology, 59(Suppl. 4), S3–S14.
Killgore, W. D. S., Young, A. D., Femia, L. A., Bogorodzki, P., Rogwska,
J., & Yurgelun-Todd, D. A. (2003). Cortical and limbic activation
during viewing of high versus low-calorie foods. Neuroimage, 19,
1381–1394.
Killgore, W. D. S., & Yurgelun-Todd, D. A. (2005). Body mass predicts
orbitofrontal activity during visual presentations of high-calorie foods.
Neuroreport, 16(8), 859–863.
Killgore, W. D. S., & Yurgelun-Todd, D. A. (2006). Affect modulates
appetite-related brain activity to images of food. International Journal
of Eating Disorders, 39, 1–7.
ARTICLE IN PRESS
J.S. Bodenlos et al. / Appetite 48 (2007) 145–153
Kirchner, A., Birklein, F., Stefan, H., & Handwerker, H. O. (2000). Left
vagus nerve stimulation suppresses experimentally induced pain.
Neurology, 55, 1167–1171.
Lomarev, M., Denslow, S., Nahas, Z., Chae, J. H., George, M. S., &
Bohning, D. E. (2002). Vagus nerve stimulation (VNS) synchronized
BOLD fMRI suggests that VNS in depressed adults has frequency/
dose dependent effects. Journal of Psychiatry Research, 36, 219–227.
Lyman, B. (1982). The nutritional values and food group characteristics of
food preferred during various emotions. Journal of Psychology, 112,
121–127.
Macht, M. (1999). Characteristics of eating in anger, fear, sadness and joy.
Appetite, 33, 65–71.
Marangell, L. B., Rush, A. J., George, M. S., Sackeim, H. A., Johnson, C. R.,
Husain, M. M., et al. (2002). Vagus nerve stimulation for major depressive
episodes: One-year outcomes. Biological Psychiatry, 51, 280–287.
Mu, Q., Bohning, D. E., Nahas, Z., Walker, J., Anderson, B., Johnson, K., et
al. (2004). Acute vagus nerve stimulation using different pulse widths
produces varying brain effects. Biological Psychiatry, 55(8), 816–825.
Nadkarni, S., LaJoie, J., & Devinsky, O. (2005). Current treatments of
epilepsy. Neurology, 64(12 Suppl. 3), S2–S11.
Ness, T. J., Fillingim, R. B., Randich, A., Backensto, E. M., & Faught, E.
(2000). Low intensity vagal nerve stimulation lowers human thermal
pain thresholds. Pain, 86, 81–85.
O’Neil, P. M., Currey, H. S., Hirsch, A. A., Malcom, R. J., Sexauer, J. D.,
Riddle, F. E., et al. (1979). Development and validation of the eating
behavior inventory. Journal of Behavioral Assessment, 1, 123–132.
O’Neil, P. M., & Reider, S. (2005). Utility and validity of the eating
behavior inventory in clinical obesity research: A review of the
literature. Obesity Reviews, 6, 209–216.
Patel, K. A., & Schlundt, D. G. (2001). Impact of moods and social
context on eating behavior. Appetite, 36(2), 111–118.
Pelchat, M. L. (2002). Of human bondage: Food craving, obsession,
compulsion, and addiction. Physiology and Behavior, 76(3), 347–352.
Pelchat, M. L., Johnson, A., Chan, R., Valdez, J., & Ragland, J. D. (2004).
Images of desire: Food-craving activation during fMRI. Neuroimage,
23, 1486–1493.
Rauh, M., Hovell, M., Sallis, J., & Hofstetter, C. (1992). Reliability and
validity of self reported physical activity in Latinos. International
Journal of Epidemiology, 21, 966–971.
Roslin, M., & Kurian, M. (2001). The use of electrical stimulation of the
vagus nerve to treat morbid obesity. Epilepsy and Behavior, 2, S11–S16.
Rush, A. J., Crismon, M. L., Kashner, T. M., Toprac, M. G., Carmody,
T. J., Trivedi, M. H., et al. (2003). Texas Medication Algorithm
Project, phase 3 (TMAP-3) Rationale and study design. Journal of
Clinical Psychiatry, 64, 357–369.
Rush, A. J., George, M. S., Sackeim, H. A., Marangell, L. B., Husain, M.
M., Giller, C., et al. (2000). Vagus nerve stimulation for treatment-
153
resistant depressions: A multicenter study. Biological Psychiatry, 47,
276–286.
Rush, A. J., Marangell, L. B., Sackeim, H. A., George, M. S., Brannan, S.
K., Davis, S. M., et al. (2005). Vagus nerve stimulation for treatmentresistant depression: A randomized, controlled acute phase trial.
Biological Psychiatry, 58, 347–354.
Rush, A. J., Sackeim, H. A., Marangell, L. B., George, M. S., Brannan, S.
K., Davis, S. M., et al. (2005). Effects of 12 months of vagus nerve
stimulation in treatment-resistant depression: A naturalistic study.
Biological Psychiatry, 58, 355–363.
Sackeim, H. A., Rush, A. J., George, M. S., Marangell, L. B., Husain, M.
M., Nahas, Z., et al. (2001). Vagus nerves stimulation for treatmentresistant depression: Efficacy, side effects and predictors of outcome.
Neuropsychopharmacology, 25(5), 713–728.
Sallis, J., Haskell, W., Wood, P., Fortmann, S., Rogers, T., Blair, S., et al.
(1985). Physical activity assessment methodology in the five-city
project. American Journal of Epidemiology, 121, 91–106.
Sobocki, J., Fourtanier, G., Estany, J., & Otal, P. (2006). Does vagal nerve
stimulation affect body composition and metabolism? Experimental
study of a new potential technique in bariatric surgery. Surgery, 139(2),
209–216.
Sobocki, J., Krolczyk, G., Herman, R. M., Matyja, A., & Thor, P. J.
(2005). Influence of vagal nerve stimulation on food intake and body
weight—results of experimental studies. Journal of Physiology and
Pharmacology, 56(6), 27–33.
Sobocki, J., Thor, P. J., Uson, J., Dmaz-Guemes, I., Lipinski, M., Calles,
C., et al. (2001). Microchip vagal pacing reduces food intake and body
mass. Hepatogastroenterology, 48, 1783–1787.
St-Onge, M. P., Sy, M., Heymsfield, S. B., & Hirsch, J. (2005). Human
cortical specialization for food: A functional magnetic resonance
imaging investigation. Journal of Nutritional Neurosciences, 135,
1014–1018.
Tecoma, E. S., & Iragui, V. J. (2006). Vagus nerve stimulation use and
effect in epilepsy: What have we learned? Epilepsy and Behavior, 8,
127–136.
Uthman, B. M. (2000). Vagus nerve stimulation for seizures. Archives of
Medical Research, 31, 300–303.
Werrij, M. Q., Mulkens, S., Hospers, H. J., & Jansen, A. (2006).
Overweight and obesity: The significance of a depressed mood. Patient
Education and Counseling, 62(1), 126–131.
Whisman, M. A., Perez, J. E., & Ramel, W. (2000). Factor structure of the
Beck Depression Inventory-Second Edition (BDI-II) in a student
sample. Journal of Clinical Psychology, 56, 545–551.
Willner, P., Benton, D., Brown, E., Cheeta, S., Davies, G., Morgan, J.,
et al. (1998). ‘‘Depression’’ increases ‘‘craving’’ for sweet rewards in
animal and human models of depression and craving. Psychopharmacology, 136(3), 272–283.