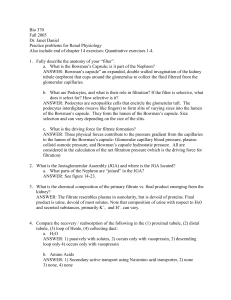
Chapter 26
advertisement

Chapter 26 Urinary System consists of paired kidneys paired ureters one urinary bladder one urethra functions of the urinary system 1. regulation of blood volume and blood pressure control of water lost in urine release of erythropoietin release of renin 2. regulates plasma concentrations of ions sodium, potassium, chloride calcium - site of calcitriol synthesis (vit D) 3. controls blood pH (acid base balance) controls acid and bicarbonate loss from blood 4. eliminates organic wastes especially nitrogenous wastes ammonia, urea and uric acid 5. detoxifies poisons and drugs (along with liver) 6. deaminates amino acids so can be converted to glucose ect general kidney anatomy nephron each kidney contains over one million nephron these are the blood filtering units parts of the nephron each nephron is composed of a blood supply called the renal corpuscle and a long tube called the renal tubule I) renal corpuscle is the blood supply of the nephron called the glomerulus and the tissue that surrounds the glomerulus called the Bowman’s capsule 1 1. glomerulus tuft of 50 intertwining fenestrated capillaries receives blood from the afferent arteriole and is drained by the efferent arteriole efferent goes on to produce the peritubular capillaries have very high blood pressure for a capillary due to small efferent arteriole thus a great quantity of fluid and solutes are pushed out this fluid is called the filtrate very similar to plasma but very little protein thus has lots of good stuff the body needs back over 90% of filtrate is reabsorbed in the peritubular capillary beds which surround the nephron tube 2. mesangila cells between neighboring capillaries there are mesangila cells mesangila cell function 1. are resident macrophages that remove materials that exits the cap but can not enter the renal tube 2. provide some physical support for cap. 3. contain actomyosin and can contract or relax changing cap diameter and may regulate filtration rate 2 3. Bowman’s or glomerular capsule surrounds the glomerulus has two layers (like a fist pushed into a balloon) 1. visceral layer (inner most layer) made of podocytes that are in contact with glomerulus podocytes form foot processes (pedicels) on the glomerulus which form filtration slits or slit pores so that filtrate can exit the capillaries the filtration slit, the fenestrated endothelium, and the lamina densa between the two make up the filtration membrane which determines what can leave the capillary and enter the capsule as a filtrate filtration membrane is affected during glomerulonephritis or inflammation of the glomeruli 2. parietal layer outer layer of simple squamous epithelium contains the filtrate passing from the glomerulus capsular space a space between the two layers fluid pressure will build here and force the filtrate down the renal tubule the Bowman’s capsule has a vascular pole or end where the capillaries enter and a 3 tubular pole or end where the renal tubule starts II) renal tubule 1 proximal convoluted tubule arises from tubular pole of the capsule constructed of cuboidal epithelial cells have numerous microvilli for absorption and large concentration of mitochondria functions: reabsorbs most nutrients most ions any plasma proteins that escape fluid by osmosis follows nutrients and ions reabsorption is by active and passive mechanisms epithelium also secretes substances into PCT lumen from blood 2. loop of Henle 1. descending limb 2. ascending limb each limb has a thick and thin segment (cells size different tube diameter the same) functions: thick ascending limb pumps out NaCl but not permeable to water important in concentrating urine 3. distal convoluted tubule passes between afferent and efferent arterioles smaller diameter then PCT and cells lack microvilli 4 function 1. active secretion of ions, acid drugs and toxins 2. selective reabsorption of Na and Ca 3. the selective reabsorption of water Collecting system DCT empties into a collecting duct several collecting ducts empty into papillary ducts papillary ducts empty into minor calyx minor calyx empty into major calyx major calyx empty into renal pelvis collecting system adjusts the finial composistion of the filtrate controlling the final osmotic concentration and volume of urine juxtaglomerular apparatus located where the distal tubule lies against the afferent and efferent arteriole 1. juxtaglomerular cells specialized smooth muscle cells located in the wall of the afferent arteriole functions: the release of renin JG cells function as a blood pressure receptor which releases renin when pressure drops JG cells also are innervated by the sympathetic nervous system which triggers the release of renin JG cells also releases erythropoietin in response to low pressure and low O2 2. macula densa cells of the distal convoluted tubule are taller columnar cells 5 functions as chemoreceptors sensitive to changes in the solute levels (sodium) of the filtrate in the distal convoluted tubule a decline in osmolarity of fluid in DCT triggers renin release occurs when fluid moves through nephron tubule to slow (more time to absorb sodium, and potassium) types of nephron 1. cortical nephron- 85% are located almost entirely in the cortex of the kidney except small part of the loop of Henle they have a short loop of Henle 2. juxtamedullary nephrons- are located near the cortex medulla junction loop of Henle plunges deeply into the medulla have a longer loop then the cortical nephrons important in producing a concentrated urine Urine formation kidneys filter entire blood volume 60 times per day entire volume every 40 minutes are 1% of body weight but consume 20-25% of oxygen at rest the object is to regulate the volume and composition of the blood to maintain homeostasis of particular importance is the clearance of three organic waste products urea: 21 grams/day from the breakdown of amino acids (actually is converted from ammonia) creatinine: 1.8 grams/day from the breakdown of creatinine phosphate by the skeletal muscle uric acid: 480 mg/day formed from the breakdown of RNA and DNA urine formation involve three processes 1. glomerular filtration 2. tubular reabsorption the removal of water and solutes from the filtrate eventually inter the peritubular capillaries 6 3. secretion transport of solutes from the peritubular fluid across the tubular epithelium and into the filtrate common for many drugs and toxins 1) glomerular filtration is a passive process in which fluids and solutes are forced across the wall of the glomerulus by hydrostatic pressure filtration membrane: the filtration slit, the fenestrated endothelium, and the lamina densa between the two it is the barrier that the filtrate crosses passing from the glomerulus to the Bowman’s capsule determines what can leave the capillary and enter the capsule as a filtrate fenestrated endothelium prevents cells from passing lamina densa blocks all but the smallest plasma proteins filtration slits block small plasma proteins only allowing ions nutrients and water to cross glomerular filtration rate (GFR) total amount of filtrate formed per minute by the kidneys 125 ml per minute 10% of the fluid delivered to the kidneys leaves the blood stream into the capsular spaces rate is 180 (50 gal) liters per day or 70 times the blood volume everyday average adult will reabsorb 99% of the filtrate volume excrete 1 to 2 liters of urine per day GFR is controlled by the same forces that control filtration/reabsorption at capillary beds (balance between hydrostatic pressures and osmotic pressures) Hydrostatic pressures Bp of 50 subtract capsular hydrostatic pressure of 15 = 35mmHg(out) Osmotic pressures Cap osmotic of 25 subtract capsular hydrostatic pressure of 0 = 25 mmHg (in) 7 Filtration pressure = 35(out) – 25 (in ) or 10mmHg(out) two factors that result in glomerular filtration being high 1. filtration membrane is 1000 times more permeable (fenestrated) 2. glomerular blood pressure is higher then at a cap bed (50 verses 15 mmHg) due to small diameter of the efferent arteriole GFR must be carefully controlled If filtrate flow is to fast, can’t reabsorb sufficient solutes and water (loss of nutrients and blood volume) If too slow, blood levels of wastes increase and results in reabsorption of wastes that should be eliminated regulating GFR the normal way to adjust GFR is to change the blood pressure at the glomerulus this is achieved by three mechanisms 1. autoregulation of GFR 2. hormonal regulation 3. sympathetic regulation autoregulation is the ability of the kidneys to maintain a relatively stable GFR in spite of changes in arterial blood pressure the nephron maintains glomerular blood pressure and thus GFR by 1. changing the diameter of the afferent arteriole 2. changing the diameter of the efferent arteriole The changes in diameter are the result of the effect that stretch has on smooth muscle contractions in the wall of the vessel increase in glomerular blood pressure 1. afferent arteriole wall is stretched by pressure which stimulates smooth muscle contraction 2. constriction of mesangial cells 3. relaxation of efferent arterioles decline in glomerular blood pressure results in 1. dilation of the afferent arterioles 8 2. relaxation of mesangial cells 3. constriction of efferent arterioles hormonal regulation of GFR renin – angiotensin works to increased systemic blood volume and blood pressure and the restoration of normal GFR 1. renin from the juxtaglomerular cells is released by a drop in glomerular blood pressure due to low blood volume fall in systemic blood pressure fall in renal blood pressure due to renal artery blockage 2. low osmolarity of fluid in DCT occurs when GFR is very slow and fluid moves through nephron tubule to slow 3. sympathetic activity to the JG apparatus effects of renin -AII renin - angiotensin I - angiotensin IIaldosterone a) peripheral capillary beds AII causes vasoconstriction of arterioles will elevate pressure in renal arteries direct fast effect on GFR b) at nephron AII constricts efferent arterioles Direct fast effect of GFR Triggers the release of aldosterone stimulates reabsorption of Na and water by DCT and collecting system increased blood volume and increased systematic blood pressure indirect and slow effect on GFR c) CNS 9 AII triggers releases of ADH which increases water reabsorption from DCT and collecting system Indirect and slow effect on GFR AII stimulates thirst which will increase blood volume and blood pressure indirect and slow effect on GFR atrial natriuretic peptide main role is to lower blood volume and pressure released by stretch on the atrial wall by high BP ANP triggers dilation of afferent arteriole and constriction of efferent arteriole This will increase GFR so produce more urine and thus lower blood volume and blood pressure ANP blocks the affects of ADH so lose water and sodium sympathetic regulation of GFR most nerve fibers are sympathetic fibers are activated during high levels of sympathetic activity especially by acute drastic fall in blood pressure will override all other forms of GFR regulation effects on GFR fibers produce powerful vasoconstriction of afferent arterioles decreases GFR and slows the production of filtrate moderate sympathetic activity, like during prolonged strenuous exercise, alters the pattern of blood flow and the kidney see less flow. 10 If autoregulation and hormonal regulation can’t oppose this change renal damage may occur due to hypoxia Common in endurance events Proteinuria (protein in urine) Hematuria (blood in urine) conversion of the filtrate to urine involves the recovery of useful substances by tubular reabsorption and the disposal (tubular secretion) of undesirable solutes that did not leave the blood stream during filtration 2) tubular reabsorption Typically almost 99% of the filtrate volume and salts content, and almost 100% of the glucose and amino acids will be reabsorbed by the renal tubule This material is returned to the peritubular capillaries by diffusion movement into the peritubular capillaries is easy to do 1. have high colloid osmotic pressure 2. very low blood pressure due to narrow efferent arteriole 3. slow flow rate Tubular reabsorption of PCT Major chemicals reabsorption at PCT 1. sodium (65%) is 140 mEq/L in filtrate only 12 in tubule cell cells are relatively permeable to Na so much enters by simple diffusion once inside the cell it is pumped out the other side by the sodium/potassium ATP-ase sodium is also reabsorbed by cotransport with other nutrients 2. glucose (100%) transported into the cell by glucose-sodium cotransport proteins is a transcellular route (through the cells) glucose uses the large concentration gradient of sodium to be pulled in glucose is more concentrated inside 11 the tubule cell once inside the cell it diffuses out the other side by facilitated diffusion it is a case of secondary active transport no ATP directly used must use ATP to maintain the sodium gradient 3. amino acids (100%) moved the same way as glucose amino acid-sodium cotransport proteins are more concentrated inside the cell so will diffuse out of tubule cells both amino acids and sugars require a transport protein which are limited in number thus there is a transport maximum if filtrate moves too fast (high GFR) or levels of sugars or amino acids are too high the transporters will become saturated and the nutrients will pass out in the urine diabetes mellitus = sugar in the urine 4. reabsorption of water(65%) as nutrients and ions reabsorbed the filtrate becomes more concentrated with water water will then flow by osmosis 5. reabsorption of other cations ions K, Ca, Mg, ect. As water leaves remaining ions become concentrated so move in by diffusion called solvent drag solvent drag also used to reabsorb lipidsoluble materials and vitamins 6. Chloride and other anions negative chloride tends to follow positive 12 sodium also reabsorb by solvent drag 7. nitrogenous wastes urea is absorbed by solvent drag (60%) kidneys remove less then half of the urea in each pass uric acid is 100% reabsorbed but secreted back in the distal convoluted tubule creatinine is not reabsorbed at all Tubular reabsorption of loop of Henle Primary function is to enable the collecting duct to concentrate the urine by conserving water what happens here? reabsorb half the remaining water and two-thirds the remaining Na, K, and Cl remember: the two parallel segments of the loop are separated only by peritubular fluid and have different permeability characteristics facts: 1. filtrate concentration entering the loop is 300 mosm 2. concentration increases to 1200 at the bottom of the loop 3. concentration drops from 1200 to 100 as the filtrate enters the DCT remember the surrounding tissue will have similar osmolarity as the filtrate 1. sodium, potassium and chloride are pumped out of the thick ascending limb by a sodium, potassium, 2 chloride cotransporter this area is not permeable to water 13 the concentration of salts within the loop goes from 1200 down to 100 DCT receives a solution of 100mosm most solutes are now wastes the pumping of Na, K, Cl results in a concentrated salt fluid in the tissues around the descending limb with the bottom being most concentrated 1200 mosm 2. the thin descending limb is permeable to water but not salts so water flows out of the thin descending limb attracted to the salt pumped out by the thick ascending limb this increases the concentration of the salts in the filtrate as you move alone the thick ascending limb toward the bottom 300 to 1200 mosm at the bottom makes it easier to pump out Na,K and Cl in the ascending limb the vasa recta, with is a part of the peritubular capillary bed, parallels the loop so that the salt gradient is established in the vasa recta so not to disturb the salt gradient and yet it picks up the excess water and salts called countercurrent multiplication countercurrent exchange occurs between fluids moving in opposite directions multiplication effect of exchange increases as fluid movement continues the fluid entered the loop at 300 mosm. Only half of this volume will enter the DCT and it will be at 100mosm due to the reabsorption of NaCl and K by the ascending limb. This solution will also have high concentrations of urea and other wastes that were not transported out Tubular reabsorption and secretion of distal convoluted tubule filtrate is only 15-20% of original volume 14 electrolyte and waste concentration are no longer similar to plasma selective reabsorption along the DCT makes adjustmenst in the composition and volume of the filtate reabsorption 1. sodium reabsorption Sodium is actively transported out of filtrate in exchange from potassium more sodium gained then potassium lost so increases water absorption this sodium transport is selectively controlled based on the bodies needs by the hormone aldosterone aldosterone is released in response to AII Low blood sodium High blood potassium (weak) aldosterone’s affects include 1. trigger the production and insertion of a sodium channel in the basal membrane 2. stimulate the synthesis and activity of the sodium-potassium ATPase thus aldosterone triggers sodium reabsorption but also potassium loss so can cause hypokalemia atrial natriuretic factor inhibits the effects of aldosterone (don’t forget ADH too) on sodium and water reabsorption in DCT thus reduces blood volume and pressure 15 2. also site of calcium reabsorption regulated by parathyroid and calcitriol affects 1. stimulate the production of a calcium channel 2. stimulate the production and activity of a calcium pump (Ca-H ATPase) Tubular reabsorption of collecting system sodium- in cortical region aldosterone-sensitive sodium reabsorption occurs same as DCT water reabsorption occurs if ADH is present filtrate has a osmolarity of 100 as it enters the collection system passes by the loop of Henle where tissue has aosmolarity of up to 1200 if ADH present the system becomes permeable to water and it moves by osmoses thus with out ADH urine will be 100 mosm or dilute diabetes insipidus with max ADH urine will be near 1200 mosm or very concentrated natriuretic ADH effects are opposed by atrial peptide ANF effects 1. elevates GFR 2. blocks aldosterone effects along DCT and collecting system 3. blocks ADH effects on collecting system 4. blocks release of aldosterone and ADH 16 Urea reabsorption The distal portion of the collecting system is permeable to urea which is concentrated by the movement of water out of the collecting system Now urea will travel down its contrition gradient and collects here the bottom of the loop 2) tubular secretion movement of substances from the peritubular capillaries into the tubule occurs if have a concentration gradient most occurs in the distal convoluted tube potassium is secreted in exchange for sodium hydrogen ion occurs when blood and filtrate pH is low low pH (high hydrogen ion ) results in formation of CO2 this diffuses into kidney cells which have carbonic anhydrase this converts CO2 to H2CO3 breakdown to H + HCO3 DCT cells pump out H in exchange for sodium thus acidify the urine the bicar will enter the blood and buffer pH ammonium ion when blood pH drops DCT and PCT will be stimulated to deaminate amino acids producing NH3 (ammonia) the ammonia will bind to H from the break down of H2CO3 (or other sources) and produce NH4 (ammonium ion which will be transported into the tubule by sodium cotransport the bicarb will enter the blood to buffer pH 17 18