has been - Mayo Clinic Health Letter

MAYO CLINIC HEALTH LETTER
Reliable Information for a Healthier Life
VOLUME 30 NUMBER 8 AUGUST 2012
Inside this issue
HEALTH TIPS
. . . . . . . . . . . . . . . . . . .
3
Protect your hearing.
NEWS AND OUR VIEWS
. . . . . .
4
Mayo creates heart drug from snake venom. Managing traumatic nightmares.
CONCUSSION
. . . . . . . . . . . . . . . . .
4
The brain in crisis.
ROSACEA
. . . . . . . . . . . . . . . . . . . . . .
6
Treating facial redness.
PLANTAR FACIITIS
. . . . . . . . . . .
7
Focus on the basics.
SECOND OPINION
. . . . . . . . . . .
8
Preventing type 2 diabetes
Stop prediabetes in its tracks
It’s estimated that up to 1 in 4 Americans has developed or has been diagnosed with prediabetes (insulin resistance). Many more are at risk. Having insulin resistance means that your blood sugar (glucose) levels are higher than normal, but not high enough to be considered type 2 diabetes.
Insulin resistance usually causes no symptoms, but can lead to worsening of cholesterol levels and high blood pressure — and it increases your risk of heart disease and stroke. Moreover, once you develop prediabetes, research indicates that within 10 years, you’re likely to go on to develop type
2 diabetes. That is, unless you do something about it.
Thankfully, you can. By losing around 7 percent of your body weight with improved diet and exercise, it’s very likely that you can prevent type 2 diabetes — and maybe even return your glucose levels to normal.
Losing weight may sound like a lot of work, but when you consider the hassle, expense and discomfort of dealing with type 2 diabetes and its many
Coming in August
BLOOD CLOTS IN THE LUNGS
Prompt treatment may be lifesaving.
DEVICES FOR PAIN
When all else fails.
BASIC PAIN RELIEVERS
It’s wise to use caution.
CORE MUSCLES
Strengthen and maintain for stability.
Every time you eat, your body converts a portion of the digested food into glucose.
Your blood carries the glucose to your body’s tissues, where the cells use it as fuel.
Glucose enters your cells with the help of insulin, which is produced by the pancreas. Insulin acts as a master key, unlocking the doors of your cells and allowing glucose inside.
consequences, it’s a worthwhile investment for better health and a better life.
Insulin resistance
Every time you eat, your body converts a portion of the digested food into glucose. Your blood carries the glucose to your body’s tissues, where the cells use it as fuel.
Glucose enters your cells with the help of insulin, which is produced by the pancreas. Insulin acts as a master key, unlocking the doors of your cells and allowing glucose inside.
In people with insulin resistance, cells don’t respond normally to insulin, and glucose can’t enter the cells as easily. Levels of glucose in your bloodstream increase, and your body produces more insulin to overcome the resistance. Over time, cells of your body become even more resistant to insulin and your body can’t keep increasing insulin production. Unchecked, blood glucose levels continue to rise and you develop type 2 diabetes.
Development of insulin resistance appears to be caused by a complex interaction between genetic and lifestyle factors. People with a family history of type 2 diabetes are at increased risk, as are blacks, Native Americans, Asian-
Americans, Hispanics and Pacific Islanders. Women who have had gestational diabetes, which develops during pregnancy (gestation), are at risk of future type 2 diabetes.
And keep in mind, being overweight — especially with excess body fat around the abdomen — is by far the greatest modifiable risk factor for progressing to type 2 diabetes if you already have insulin resistance. A sedentary lifestyle also is a major risk factor.
In addition, several commonly prescribed drugs can impair glucose tolerance and may increase risk of type 2 diabetes. Among these drugs are cholesterol drugs called statins. But don’t stop taking statins or any other drugs without discussing with your doctor the risks and benefits as they relate to your chances of developing diabetes.
2 www .HealthLetter .MayoClinic .com August 2012
The power of less
Body fat is an agent that causes cells to become resistant to insulin. But, as you lose weight or body fat, your cells become more responsive to insulin.
The change is often remarkable.
One large study found that for adults 60 and older, modest lifestyle changes reduced the risk of progressing from prediabetes to type 2 diabetes by
71 percent. In this study, called the
Diabetes Prevention Program, participants who reduced their risk of developing type 2 diabetes the most:
■
Ate in a healthier way, including eating less fat and fewer calories.
■
Performed exercise equivalent to brisk walking for 150 minutes a week
— an average of 30 minutes a day for five days a week.
■
Aimed to lose 7 percent of their body weight. For someone weighing
200 pounds, that’s 14 pounds.
A healthy diet that can lead to weight loss and prevention of type 2 diabetes involves:
■
An emphasis on eating minimally
processed foods — These include fruits, berries, vegetables, beans and other legumes, and whole grains. In addition to high amounts of fiber, these foods offer a vast array of beneficial nutrients
— not to mention an array of delicious flavors. Importantly for weight loss, fruits and nonstarchy vegetables have low energy density, meaning they contain relatively few calories for a given portion size. Whole grains contain more fiber than do refined grains and help you feel full on fewer calories.
Apart from their role in weight loss, consuming whole grains and fiber — whether the fiber is from whole grains or other sources — has also been strongly associated with improved insulin sensitivity and reduced risk of type 2 diabetes.
■
Moderate portions of low-fat dairy,
fish and other protein sources — Picture the size of a deck of cards and limit your daily intake of meat, poultry and fish to that amount. Consume skim milk and low-fat dairy products in moderation. These foods can be calorie dense, meaning small portions provide lots of calories. You’ll still get plenty of protein if you eat a wide variety of plant foods and consume adequate calories.
Saturated fat — found in meat, poultry and dairy products containing fat — appears to promote insulin resistance beyond its contribution to high calorie intake. Fats found in fish or in plant oils such as canola or olive oil don’t appear to have this effect and may even be slightly protective.
■
Minimal amounts of sweets, sugary beverages and processed baked goods
such as cookies and pastries — These foods have high levels of sugar, fat and calories with little in the way of nutritional value. It’s easy to rapidly consume high amounts of calories with these
MAYO CLINIC HEALTH LETTER
Managing Editor
Aleta Capelle
Associate Editors
Carol Gunderson
Joey Keillor
Medical Illustration
Michael King
Customer Service Manager
Ann Allen
Administrative Assistant
Beverly Steele
Medical Editor
Robert Sheeler, M.D.
Associate Medical Editor
Amindra Arora, M.B,
B.Chir
Editorial Research
Deirdre Herman
Proofreading
Miranda Attlesey
Donna Hanson
Julie Maas
EDITORIAL BOARD
Shreyasee Amin, M.D., Rheumatology; Amindra
Arora, M.B., B.Chir., Gastroenterology and Hepatology;
Brent Bauer, M.D., Internal Medicine; Julie Bjoraker,
M.D., Internal Medicine; Lisa Buss Preszler, Pharm.D.,
Pharmacy; Bart Clarke, M.D., Endocrinology and
Metabolism; William Cliby, M.D., Gynecologic
Surgery; Clayton Cowl, M.D., Pulmonary and Critical
Care; Mark Davis, M.D., Derma tology; Michael
Halasy, P.A.-C., Emergency Medicine; Timothy
Moynihan, M.D., Oncology; Suzanne Norby, M.D.,
Nephrology; Norman Rasmussen, Ed.D., Psychology;
Daniel Roberts, M.D., Hospital Internal Medicine;
Robert Sheeler, M.D., Family Medicine; Phillip
Sheridan, D.D.S., Perio don tics; Peter Southorn, M.D.,
Anes thesiology; Ronald Swee, M.D., Radiology;
Farris Timimi, M.D., Cardiology; Matthew Tollefson,
M.D., Urology; Debra Zillmer, M.D., Orthopedics;
Aleta Capelle, Health Information. Ex officio: Carol
Gunderson, Joey Keillor.
Mayo Clinic Health Letter (ISSN 0741-6245) is published monthly by Mayo Foundation for Medical
Education and Research, a subsidiary of Mayo
Foundation, 200 First St. SW, Rochester, MN 55905.
Subscription price is $29.55 a year, which includes a cumulative index published in December. Periodicals postage paid at Rochester, Minn., and at additional mailing offices . POSTMASTER: Send address changes to Mayo Clinic Health Letter, Subscription Services,
P.O. Box 9302, Big Sandy, TX 75755-9302.
items — especially soda — without realizing that you’re doing so. Moreover, some of these products contain trans fats, which have been linked to increased insulin resistance.
■
Overall portion control — Strategies for portion control include eating slowly so your brain has time to register fullness, stopping eating when you feel satisfied, serving food in smaller amounts or using smaller plates and bowls, not eating from a container, and focusing on eating rather than being distracted by television or work.
■
A few indulgences — Some of the great delights of life — namely a cup or two of coffee, a square or two of dark chocolate, and no more than one alcoholic beverage a day — have in some small studies been modestly associated with better insulin sensitivity.
Get moving
Physical activity helps prevent type
2 diabetes in many ways. Aerobic activity — such as brisk walking — or strengthening exercises are each beneficial, but a plan that includes both offers the greatest benefit.
Exercise is an important component of any weight-control plan. Exercise burns calories directly — but it also burns calories indirectly by increasing your muscle mass. Since muscle tissue burns more calories than does fat tissue, increased muscle mass causes you to burn more calories, even when you are at rest.
Exercise also promotes the transfer of glucose from your blood to your cells. The more you exercise, the more glucose you use, thus lowering the amount of glucose left in your blood.
Exercise also makes your cells more responsive to insulin.
The best exercise is the exercise that you’ll actually do. Planned exercises — such as walking, bicycling or swimming — are good choices. Physical activity such as gardening, dancing or mowing the lawn with a push mower can count, too. Whatever you choose, aim for an intensity level in which you feel yourself working and maybe even breaking a sweat — but you can still say a sentence out loud without having to pause to catch your breath. Gradually building up to doing
30 minutes of exercise on most days is a great benchmark for preventing type
2 diabetes. If you already exercise, you can gradually make your exercise more intense or increase the amount of time you spend exercising.
Intervals are a great way to add intensity. These involve repeated bursts of relatively intense activity separated by short recovery periods. With walking, this may involve walking faster than usual for two minutes, followed by one minute of ordinary walking pace, then repeating that pattern several times. More intense exercise can lead to an increased level of insulin sensitivity for 12 to 48 hours after the exercise session is over.
Physical activity helps prevent type 2 diabetes in many ways.
Aerobic activity
— such as brisk walking — or strengthening exercises are each beneficial, but a plan that includes both offers the greatest benefit.
Isn’t there a drug?
Several medications have been shown to reduce the risk of type 2 diabetes. The best of these appears to be metformin (Glucophage).
However, studies indicate that metformin — when used to prevent type 2 diabetes — is least effective in adults over the age of 45. Furthermore, it’s generally not recommended for use to prevent type 2 diabetes in adults age
60 or older. Even for adults under age
45, metformin isn’t nearly as effective for prevention of type 2 diabetes as is losing weight and exercising.
❒
Health tips
Protect your hearing
Even if you already have hearing loss, avoid further damage. Additional damage may lead to — or worsen — problems such as ringing in the ears (tinnitus). Protect your hearing by:
■
Wearing well-fitting earplugs or earmuffs around loud noises
— Noises that are often more than 85 decibels include those from chain saws, power tools, tractors, snowmobiles, motorcycles and stock car races.
Duration of exposure is equally important. The longer the exposure to noises above 85 decibels, the higher the risk of hearing damage. Some noise exposures, such as gunfire, are so loud that even extremely brief exposure can damage hearing.
Generally, if you must raise your voice to be heard by someone an arm’s length away, the surrounding noise is loud enough to be potentially damaging.
■
Turning down the volume
when you can — The same arm’slength rule applies to sound from radios, TVs or sound systems. If it’s loud enough to interfere with a conversation, turn it down.
Wear snug-fitting headphones or earphones. This will decrease the interference of other sounds, allowing you to listen comfortably to your music without being tempted to turn up the volume to potentially dangerous levels.
■
Giving your ears a rest — Alternate noisy activity with quiet activity. A noise that’s lower on the decibel scale, but continues for a longer period, may be more harmful than a higher intensity noise that’s intermittent.
❒
August 2012 www .HealthLetter .MayoClinic .com
3
News and our views
Mayo creates heart drug from snake venom
Mayo Clinic doctors and researchers have invented a new drug that may one day help relieve symptoms of heart failure — and help prevent damage to the heart muscle and kidneys that can occur during heart attack.
The drug was created in part from molecules from the venom of the
African green mamba snake. The molecules act in concert with receptors in the cardiovascular system to keep fluids and toxins moving when the heart is struggling to pump effectively. The molecules help prevent fluid buildup than can occur with heart failure or heart attack. The venom molecules also help support kidney function so that the body can better rid itself of water and salt. The molecules also prevent heart muscle from dying.
The venom molecules are attached to molecules of a naturally occurring hormone produced in the cells that line the walls of human blood vessels.
These molecules signal blood vessels to dilate, further facilitating blood flow and the processing of waste. By attaching select hormone and venom molecules together, Mayo researchers created the drug cenderitide, which essentially exploits the best properties of each substance.
Cenderitide has undergone several promising, but early tests in humans with heart failure. A study will soon begin to test the effectiveness of cenderitide when given to people who are having a heart attack. It takes time and much research before a promising drug makes it to the marketplace.
Not all drugs survive this arduous process. However, Mayo Clinic doctors and researchers are hopeful that their efforts to merge the best of science and the best of nature will result in a helpful therapy.
❒
Managing traumatic nightmares
A drug that has been used to treat high blood pressure appears to help manage traumatic nightmares associated with post-traumatic stress disorder
(PTSD). Mayo Clinic researchers came to that conclusion after reviewing a number of small studies that evaluated the use of prazosin (Minipress) to treat PTSD-related nightmares.
Severe nightmares that seem extremely real are a common feature of
PTSD. Although prazosin isn’t specifically approved for treatment of PTSD, it has been used off-label to reduce or suppress nightmares in many people with PTSD. Prazosin blocks the brain’s response to an adrenaline-like brain chemical called norepinephrine, which can play a role in sleep disruption.
Researchers say the evidence supports this use of prazosin. Those treated with the drug showed consistent improvement and the drug was generally well tolerated, even among older adults. The most common side effects were dizziness and lightheadedness.
Other than prazosin, there’s not much in the way of drugs available yet with a good evidence base for treating nightmares associated with PTSD.
Mayo Clinic doctors say prazosin’s potential benefits may outweigh possible side effects. People taking prazosin should have their blood pressure monitored regularly — low blood pressure can be a side effect of the medication.
Mayo doctors add that when treating nightmares, behavior therapy, including treatments such as cognitive behavioral therapy, can be as effective as medications and that the best treatment frequently involves both.
❒
Concussion
The brain in crisis
Concussion injury — which is a form of traumatic brain injury — is commonplace on playing fields. Recent estimates indicate head trauma due to contact sports occurs nearly 3.8 million times a year in the U.S.
Concern has grown over concussion brain injuries in professional athletes as well as in teens and children. Youngsters — whose brains are still developing — are competing at ever-earlier ages in concussion-prone contact sports.
The concern spotlights the need for more awareness of concussion dangers and how to prevent them.
A concussion occurs when there’s a blow to the head or a sudden jolt that shakes the head and causes the brain’s gelatin-like cortex to rapidly collide into or bounce off the inside of your skull or to rotate within it. When it occurs, the brain’s function is altered. Loss of consciousness may or may not happen, which is one of the reasons some concussions go unrecognized.
No matter the cause, when a firsttime concussion brain injury is identified and the brain is given adequate rest and time to heal properly, most recover completely. However, changes that occur in the brain due to concussion make it potentially vulnerable to repeat injury and possibly even permanent damage.
For someone who’s had multiple concussions, recovery becomes less certain with each concussion.
Inside matter
According to the Centers for Disease
Control and Prevention, concussions make up the majority of traumatic brain injuries each year. Among adults 65 and older, falls are the number one cause of traumatic brain injury. For all age groups, motor vehicle accidents are the second-leading cause. Part of the concussion conundrum is that the brain has no pain receptors. So, during a concussion — when the brain is slung
4 www .HealthLetter .MayoClinic .com August 2012
through its cushion of cerebrospinal fluid and crashes full force into the cranium — that impact registers indirectly.
Initially, or within several minutes, you may experience confusion and memory loss. This may or may not be preceded by loss of consciousness.
Although you may appear to be fine immediately after a concussion, it’s a different story inside the brain. The instant after a concussion the brain is in crisis. Many brain cells (neurons) can become activated all at once. This can cause a sudden release of brain chemicals (neurotransmitters). Within minutes to hours after a concussion, the brain’s power drain produces signs and symptoms that may include headache, dizziness, imbalance, nausea or vomiting, slurred speech, fatigue and being unaware of your surroundings.
While some symptoms are more immediate, others may show up in the hours and days that follow, including:
■
Difficulty concentrating or remembering things
■
Sensitivity to light and noise
■
Persistent headache
■
Unexplained irritability or other personality changes
■
Sleep disturbances
■
Depression and problems adjusting psychologically
■
Altered senses of taste and smell
As long as symptoms are present, it’s critically important to avoid a second concussion. During this time, the brain is vulnerable to a rare but fatal brain-swelling complication.
Long-term changes from a brain concussion are more uncertain. Although symptoms due to concussion may no longer be apparent, structural damage to the brain may be slower to recover. Recent studies using specialized magnetic resonance imaging (MRI) scans show changes in certain brain structures even at six months.
Medical care matters
A head injury should be evaluated by a medical professional. That person may be your care primary doctor or any other member of your primary health care team capable of giving you advice and assuring follow-up. Young athletes or children should be removed from play for any suspected concussion.
Typically, a neurological exam is done for a head injury. This may include evaluation of your memory and ability to concentrate, vision and hearing, pupils, strength and sensation, balance, coordination, and reflexes.
Although brain imaging isn’t always done, depending on your symptoms, a computerized tomography (CT) scan or
MRI may be done to assess the brain right after injury. However, the findings are usually normal. Imaging is also likely if you’re 65 years of age or older or are taking medicines that affect blood clotting.
Depending on the findings, you may need to be hospitalized overnight for observation. Monitoring is important in the hours after a concussion because brain injury may lead to more-serious problems, including bleeding in or around the brain.
If your doctor says home observation is reasonable, you’ll need to have someone check on you every few hours for at least 24 hours to be sure that your symptoms don’t get any worse. Emergency care is needed if your symptoms get worse or you experience any of the following:
■
Repeated vomiting
■
Severe headache
■
Loss of consciousness
■
Difficulty with mental function or physical coordination
“tough it out” — doing so can make symptoms worse. Instead:
■
Take time to rest — Get plenty of sleep at night and rest during the day.
■
Moderate how much and how in-
tensely you think — Special imaging scans show that thinking causes the brain to use energy, which is fine when the brain isn’t in the process of healing.
But after a concussion, energy use from thinking takes away from the brain’s efforts to heal and recover. Concentration slows recovery and can even make symptoms worse. That’s why it’s important to avoid activities that require a lot of concentration.
■
Avoid physically demanding activi-
ties — Put your workout aside for now.
Let someone else mow the lawn or clean the house. Save the energy you have each day for activities that are most important to you.
If your doctor says you can ease into some regular activities, see how you do. If your symptoms return or you get new symptoms, more rest is needed.
When concussion recovery is managed properly, most people recover completely within a week or two and have no further symptoms. However, for those whose recovery from concussion takes longer, persistent headache can be a common challenge.
❒
Time for recovery
Because the brain is fragile after a concussion, the focus during recovery is rest — both physical and mental. It takes time for the brain to restore itself.
And how much time varies. Several factors can influence how quickly you recover, including your age, severity of the concussion and whether you have other health conditions.
Recovering from a concussion is no time to ignore your symptoms and
A concussion occurs when a blow to the head or a sudden jolt shakes the head and causes the brain’s cortex to bounce off the inside of your skull or to rotate within it.
August 2012 www .HealthLetter .MayoClinic .com
5
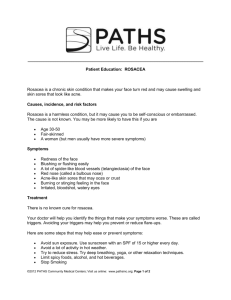
Rosacea
Treating facial redness
You’ve always blushed easily. But in the last months, it seems you’re always blushing. At first you thought it might be due to the warm summer weather.
But even on days spent in air conditioning, your face maintains its redness, especially your cheeks and nose. And lately, a few pimple-like bumps have started to appear.
Changes such as these may indicate a common inflammatory skin condition called rosacea (roe-ZAY-she-uh). An estimated 14 million Americans have rosacea, which can be mistaken for other skin disorders, such as acne and skin allergies. The good news is that the pimple-like bumps of rosacea generally respond well to prescribed treatment and to efforts to avoid triggers that can aggravate the condition.
of your face — especially the nose — due to expanding (dilating) blood vessels close to the skin’s surface. With time, small blood vessels on the nose and cheeks may swell and become more visible. Skin tends to be overly sensitive
— for some, oily skin and dandruff are part of the mix. The inflammatory phase of rosacea is marked by the appearance of small red bumps or pustules, which aren’t the same as whiteheads or blackheads associated with ordinary acne.
More than half of people with rosacea experience a burning or gritty eye sensation called ocular rosacea. The inner skin of the eyelids may become inflamed or appear scaly A rare occurrence — mainly in men — may occur late in the course of rosacea where tissue builds up on or around the nose, giving the nose a large, bulbous appearance (rhinophyma).
First blush
Although anyone can develop rosacea, it’s more likely to occur in people with fair skin and light eye and hair color. The condition typically appears between the ages of 30 and 60. Women are more likely than men to develop rosacea, especially when going through menopause. However, rosacea tends to be more severe in men. Frequent blushing (flushing) may indicate a greater risk of the condition, as does a family history of rosacea. Its cause is unknown, but researchers believe rosacea is likely due to a combination of hereditary and environmental factors.
Rosacea can begin with a tendency for facial flushing. But if that’s your only sign and nothing further develops on your face, it may not be rosacea. Some people have a naturally ruddy complexion or even chronic sun damage, which may give the appearance of rosacea but not actually be rosacea.
Generally, signs and symptoms of rosacea are progressive. Persistent red areas may develop on the center area
Time for solutions
True rosacea rarely clears up on its own. If you have persistent facial redness, see your doctor for diagnosis and proper treatment. You may notice that some of the following factors may make your face turn red (flush). If that’s the case, avoid:
■
Temperature extremes
■
Sunlight exposure
■
Hot foods or beverages
■
Spicy foods
■
Alcohol
■
Stress, anger or embarrassment
■
Hot baths, saunas
■
Medications that dilate blood vessels, including some blood pressure medications
Other than avoiding potential flushing triggers, there aren’t good treatments to address the problem of flushing on its own. However, if the flushing produces dilated vessels on your skin, laser surgery may help reduce the visibility of those blood vessels.
Gentle skin care practices are important to avoid irritating sensitive facial skin and to protect your skin from needless damage. Your doctor can recom-
6 www .HealthLetter .MayoClinic .com August 2012 mend specific skin care products best suited for your skin type.
If your rosacea includes pimple-like bumps, there are very effective treatments.
Topical medications may help reduce these blemishes. Commonly used prescription topicals include antibiotics such as metronidazole (Metrocream,
Metrogel, others), tretinoin (Retin-A,
Renova, others), benzoyl peroxide, azelaic acid (Azelex, Finacea) and sulfacetamide (Klaron).
Topicals may be used alone or in combination with oral antibiotics, which also help reduce inflammation. Oral antibiotics tend to work faster than topical ones. Commonly prescribed antibiotics include tetracycline, doxycycline, erythromycin and minocycline. Once symptoms improve, you may be taken off the oral antibiotics and use just topical medication to help keep rosacea in remission.
Ocular rosacea is typically treated with oral antibiotics. If needed, your doctor may prescribe steroid eyedrops.
In the rare instances of rhinophyma, treatments such as laser surgery can be used to remove tissue buildup.
Treatment for rosacea varies depending on the severity of your symptoms.
Although there’s no cure for rosacea, you can often suppress symptoms and keep rosacea under control with medications and self-care.
❒
Rarely, late in the course of rosacea, tissue can build up on or around the nose, which can give the nose a large, bulbous appearance.
Plantar fasciitis
Focus on the basics
Your plantar fascia is a fibrous band of tissue on the bottom of your foot. It connects your heel bone to your toes and acts like a shock-absorbing bowstring that supports your foot arch and keeps the foot from collapsing.
Plantar faciitis is an injury caused by placing too much tension on the plantar fascia. The injury causes microscopic tears in the plantar fascia, which can lead to inflammation and moderate to piercing pain where your foot arch meets your heel.
The pain often comes on gradually and affects one foot but can affect both feet. It’s usually worse in the morning because the plantar fascia has had a chance to tighten up during the night while the foot was relaxing.
Most people with plantar fasciitis experience improvement with basic care steps — but healing can be slow and frustrating. Still, it’s important to persevere with basic care — and investigate additional forms of therapy if those aren’t enough.
Aggravation
For older adults, the risk of fasciitis can increase because the plantar fascia loses some of its flexibility with age, and the fat pads on the bottom of the feet become thinner and less shock absorbing. Being overweight also puts more strain on the plantar fascia.
Additional strain can be caused by going barefoot or wearing shoes or slippers without much padding or arch support, routinely wearing 2-inch or higher heels, suddenly increasing your activity such as walking a lot on a vacation, standing on your feet for extended periods of time, or lifting heavy objects.
Having high arches, flat feet or an abnormal walking pattern also may lead to increased strain on the fascia.
First line treatment for plantar fasciitis aims to reduce pain and stresses on the heel with steps including:
■
Wearing the right shoes — Indoors or outdoors, wear supportive, cushioned footwear at all times. Low- to medium-heeled shoes are best. Replace worn-out shoes. Keep footwear by your bed so you can slip into them first thing.
■
Providing extra cushion — A lowcost, silicone heel cup can be effective, as can semirigid prefabricated shoe inserts that cup the heel, extend to the ball of the foot and provide arch support.
■
Limiting aggravating activities —
You may need to limit exercises that involve foot strain, such as jogging or stair stepping. Find alternatives such as swimming or cycling. Find ways to avoid standing for long periods, such as bringing a stool to areas where you would ordinarily need to stand.
■
Getting physical therapy — This may include basic stretching and strengthening exercises or more-advanced therapies as directed by a physical therapist.
■
Cooling your heel — Soaking your heel in cold water or applying a clothcovered gel pack to the heel for 15 minutes helps reduce pain and inflammation. If you have vascular disease, diabetes or decreased sensation, talk with your doctor before applying ice.
■
Taking pain medication for flare-ups
— Ibuprofen (Advil, Motrin IB, others) and naproxen (Aleve, others) may help
Plantar fasciitis is an injury caused by too much tension on the plantar fascia.
Basic stretching and strengthening exercises can help relieve plantar fasciitis.
ease pain and inflammation. Using pain medications for more than two weeks isn’t recommended without talking to your doctor.
■
Losing weight — This won’t happen overnight, but over the long term, weight loss through improved diet and exercise helps ease strain on your feet.
When it’s not enough
When the low-cost methods above don’t seem to be helping, additional therapies may include:
■
Custom-molded shoe inserts — A custom, semirigid shoe insert that cups your heel and provides arch support may provide more comfort and support than can be found with similar prefabricated devices.
■
Corticosteroid injection at tender
points — This can knock back inflammation, relieve pain and facilitate healing, but the effect is temporary and basic care is still necessary to provide long-term healing. Multiple injections usually aren’t recommended because they can weaken the fascia and raise the risk of rupture.
■
Night splint — This brace keeps the foot at 90 degrees while sleeping so that the plantar fascia doesn’t tighten at night.
■
Last-resort options — Wearing a cast or walking boot for several weeks can immobilize the fascia to allow healing.
Rarely, surgery may be considered when conventional treatments haven’t helped. Extracorporeal shock wave therapy may be considered, but its effectiveness remains controversial.
❒
August 2012 www .HealthLetter .MayoClinic .com
7
Second opinion
Q Does coconut oil improve cholesterol by raising good cholesterol, or should I use fish oil?
A Limited research suggests that eating higher amounts of coconut oil may be associated with increased levels of high-density lipoprotein (HDL) cholesterol — the “good” cholesterol.
However, coconut oil is high in saturated fats, and reliable scientific evidence on its use to treat high cholesterol so far isn’t conclusive.
In terms of oil supplements that may influence HDL, there’s better evidence for fish oil. Studies show some people taking fish oil have a slight increase in
HDL, but low-density lipoprotein (LDL) cholesterol — the “bad” cholesterol — also tends to increase slightly. More importantly, there’s strong evidence supporting the use of fish oil to lower elevated triglycerides, another type of fat (lipid) in the blood. Triglycerides can increase risk of heart disease.
Fish oil is a natural source of omega-3 fatty acids, in particular eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). EPA and DHA benefit heart health and are important for people at high risk of cardiovascular disease. For people with known cardiovascular disease, adequate EPA and
DHA can reduce the risk of death, heart attack, dangerous abnormal heart rhythms and strokes.
In 2004, the Food and Drug Administration approved a prescription omega-3 fatty acid supplement (Lovaza) as a therapeutic way to reduce high triglycerides. Lovaza contains a high concentration of omega-3 fatty acids EPA and DHA similar to levels shown to be effective in clinical trials.
Fish oil is also available in nonprescription dietary supplements, although some don’t have as high a concentration of EPA and DHA as does prescription Lovaza.
Talk with your doctor before you start using nonprescription fish oil supplements. Excessive amounts may cause bleeding. Taking more than 3 grams of omega-3 fatty acids from supplements should be done only under your doctor’s care.
❒
Q Is agoraphobia the same thing as social anxiety disorder?
A Agoraphobia is a type of anxiety disorder, but it’s not the same as social anxiety. Social anxiety causes excessive anxiety or fear of situations in which you believe others will watch or judge you.
Agoraphobia is a disorder in which you avoid situations that you’re afraid might cause you intense fear (panic attack). These can include a fear of being alone, a fear of leaving your home or a fear of being in any place in which you might feel trapped, embarrassed or helpless if you had a panic attack.
When in these situations, tremendous distress and anxiety are experienced.
Agoraphobia is usually a complication of a panic disorder, which is characterized by panic attacks that occur for no apparent reason and trigger physical symptoms. Panic attacks can make you feel as if you’re losing control, having a heart attack or even dying. Signs and symptoms might include such things as having a rapid heart rate, sweating, shortness of breath, hyperventilation, chest pain and dizziness.
Agoraphobia can develop if a connection is made between panic attack experiences and the situations in which the attacks occurred.
Treatments may include cognitive behavioral therapies and medication.
In therapy, you may learn to recognize and change certain thinking patterns that otherwise play into your anxieties and fear. Behavior therapy may include therapy in which you learn to safely face places or situations that cause distress (exposure therapy). Medications may include the use of antidepressants
— particularly selective serotonin reuptake inhibitors (SSRIs), such as paroxetine (Paxil, others) and fluoxetine (Prozac, others) — and short-acting, anti-anxiety medications.
❒
Have a question or comment?
We appreciate every letter sent to Second
Opinion but cannot publish an answer to each question or respond to requests for consultation on individual medical conditions. Editorial comments can be directed to:
Managing Editor, Mayo Clinic Health Letter,
200 First St. SW, Rochester, MN 55905, or send email to HealthLetter@Mayo.edu
For information about Mayo Clinic services, you may telephone any of our three facilities:
Rochester, Minn., 507-284-2511;
Jacksonville, Fla., 904-953-2000;
Scottsdale, Ariz., 480-301-8000 or visit www.MayoClinic.org
Check out Mayo Clinic’s consumer health website, at www.MayoClinic.com
Copyright
© 2012 Mayo Foundation for Medical
Education and Research. All rights reserved.
MAYO, MAYO CLINIC, the triple-shield Mayo logo, and TOOLS FOR HEALTHIER LIVES are marks of Mayo Foundation for Medi cal
Education and Research.
Mailing lists
We make our Mayo Clinic Health
Letter mailing list available to carefully selected companies and organizations. If you do not wish to receive such mailings, please write us at the address shown at right and enclose your mailing label.
Customer Services
For subscription information from locations within United States and Canada, call Customer Services at: 866-516-4974.
From other countries call: 903-636-9029.
Subscription prices in United States:
$29.55; in Canada: $45; all other countries:
$55 (U.S.). Single copies are available for
$4 plus shipping, handling and taxes.
Purpose
To help our subscribers achieve healthier lives by providing useful, reliable, easy-to-understand health information that’s timely and of broad interest.
Mayo Clinic Health Letter supplements the advice of your personal physician, whom you should consult for personal health problems.
Correspondence
Send subscription inquiries to:
Mayo Clinic Health Letter
Subscription Services
P.O. Box 9302
Big Sandy, TX 75755-9302
MC2019-0812
100812
Printed in the USA
8 www .HealthLetter .MayoClinic .com August 2012