Prognostic value of left ventricular volume response during
advertisement
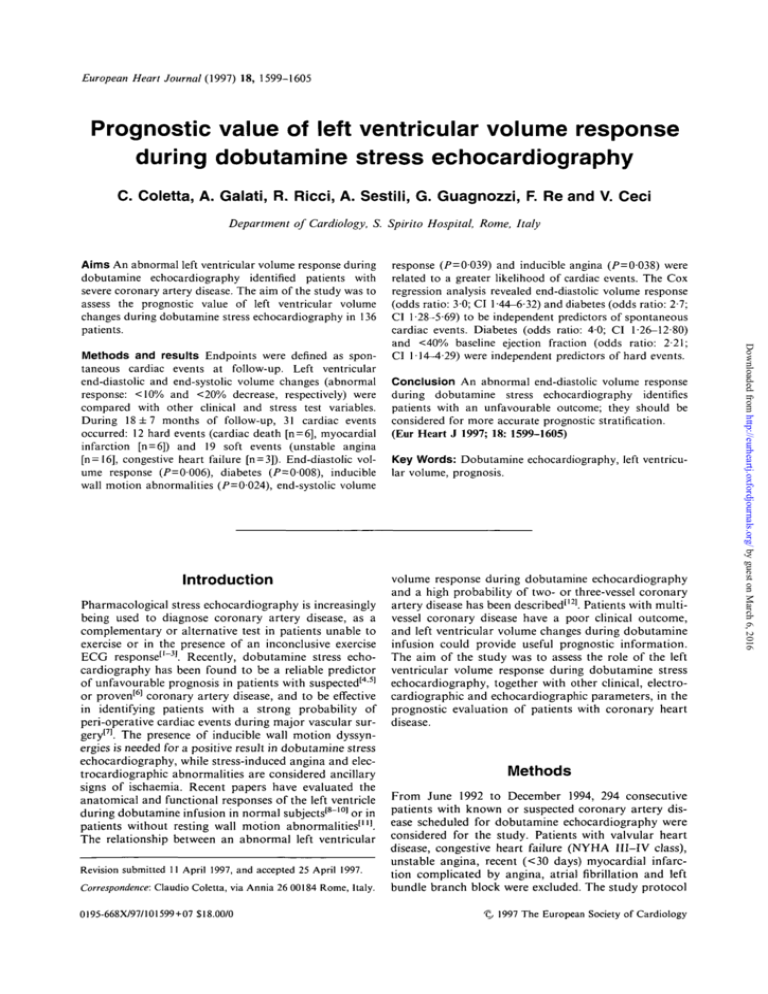
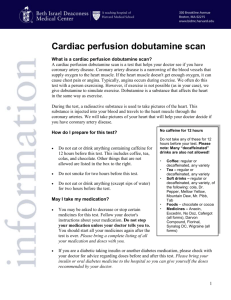
European Heart Journal (1997) 18, 1599-1605 Prognostic value of left ventricular volume response during dobutamine stress echocardiography C. Coletta, A. Galati, R. Ricci, A. Sestili, G. Guagnozzi, F. Re and V. Ceci Department of Cardiology, S. Spirito Hospital, Rome, Italy Aims An abnormal left ventricular volume response during dobutamine echocardiography identified patients with severe coronary artery disease. The aim of the study was to assess the prognostic value of left ventricular volume changes during dobutamine stress echocardiography in 136 patients. Introduction Pharmacological stress echocardiography is increasingly being used to diagnose coronary artery disease, as a complementary or alternative test in patients unable to exercise or in the presence of an inconclusive exercise ECG response1'"3'. Recently, dobutamine stress echocardiography has been found to be a reliable predictor of unfavourable prognosis in patients with suspected'45' or proven'6' coronary artery disease, and to be effective in identifying patients with a strong probability of peri-operative cardiac events during major vascular surgery'7'. The presence of inducible wall motion dyssynergies is needed for a positive result in dobutamine stress echocardiography, while stress-induced angina and electrocardiographic abnormalities are considered ancillary signs of ischaemia. Recent papers have evaluated the anatomical and functional responses of the left ventricle during dobutamine infusion in normal subjects'8"101 or in patients without resting wall motion abnormalities'"'. The relationship between an abnormal left ventricular Revision submitted 11 April 1997, and accepted 25 April 1997. Correspondence: Claudio Coletta, via Annia 26 00184 Rome, Italy. 0195-668X/97/101599+07 S18.00/0 Conclusion An abnormal end-diastolic volume response during dobutamine stress echocardiography identifies patients with an unfavourable outcome; they should be considered for more accurate prognostic stratification. (Eur Heart J 1997; 18: 1599-1605) Key Words: Dobutamine echocardiography, left ventricular volume, prognosis. volume response during dobutamine echocardiography and a high probability of two- or three-vessel coronary artery disease has been described'12'. Patients with multivessel coronary disease have a poor clinical outcome, and left ventricular volume changes during dobutamine infusion could provide useful prognostic information. The aim of the study was to assess the role of the left ventricular volume response during dobutamine stress echocardiography, together with other clinical, electrocardiographic and echocardiographic parameters, in the prognostic evaluation of patients with coronary heart disease. Methods From June 1992 to December 1994, 294 consecutive patients with known or suspected coronary artery disease scheduled for dobutamine echocardiography were considered for the study. Patients with valvular heart disease, congestive heart failure (NYHA III—IV class), unstable angina, recent (<30 days) myocardial infarction complicated by angina, atrial fibrillation and left bundle branch block were excluded. The study protocol 1997 The European Society of Cardiology Downloaded from http://eurheartj.oxfordjournals.org/ by guest on March 6, 2016 Methods and results Endpoints were defined as spontaneous cardiac events at follow-up. Left ventricular end-diastolic and end-systolic volume changes (abnormal response: <10% and <20% decrease, respectively) were compared with other clinical and stress test variables. During 18 ±7 months of follow-up, 31 cardiac events occurred: 12 hard events (cardiac death [n = 6], myocardial infarction [n = 6]) and 19 soft events (unstable angina [n = 16], congestive heart failure [n = 3]). End-diastolic volume response (/>=0006), diabetes (P=0008), inducible wall motion abnormalities (/>=0024), end-systolic volume response (P=0039) and inducible angina (/>=0-038) were related to a greater likelihood of cardiac events. The Cox regression analysis revealed end-diastolic volume response (odds ratio: 30; CI 1-44-6-32) and diabetes (odds ratio: 2-7; CI 1-28-5-69) to be independent predictors of spontaneous cardiac events. Diabetes (odds ratio: 40; CI 1-26-12-80) and <40% baseline ejection fraction (odds ratio: 2-21; CI 1 -14—4-29) were independent predictors of hard events. 1600 C. Coletta et al. The test was considered positive when wall motion deteriorated one grade in at least two segments or two grades in at least one segment; akinesia deteriorating to dyskinesia was not considered for the result of the test'14'. Agreement between the two observers was required for test results to be interpreted as positive. In case of disagreement, the judgement of a third observer was conclusive. For each patient, the wall motion score index (total score/16) at rest and peak stress and the difference between the two values, as an index of severity of ischaemia, were considered; in case of improvement, the score of a resting abnormal segment was calculated as unmodified. Finally, the rate-pressure product at the onset of ischaemia was considered. Dobutamine electrocardiography The dobutamine stress ECG was interpreted as positive for ischaemia if horizontal or downsloping ST segment depression or elevation > 0 1 mV in at least two leads with a normal baseline ST segment occurred. In case of >0-5mV resting ST segment depression or elevation, the ECG response was considered abnormal in the presence of an increased ST segment shift >0-2 mV in at least two leads. In patients with myocardial infarction, ST segment elevation in Q leads was not considered a positive criterion. Dobutamine-atropine stress test In resting conditions, a two-dimensional echocardiographic examination of the left ventricle was performed using a wide-angle phased-array imaging system (Hewlett Packard 77020, Sonos 1500 system) equipped with a 2-25- or 3-5-MHz transducer and recorded on SVHS videotape (Panasonic 7350 AG). A 12-lead ECG was also recorded with the patient at rest. Dobutamine was administered intravenously with an infusion pump, starting at 5 ug . kg" ' body weight per min (stage I) and increasing to 10 ug . kg" ' per min after 3 min (stage II) and then incrementally every 3 min to 20 (stage III), 30 (stage IV) and 40 ug . kg" ' per min, and continued for 6 min (stage V). Atropine (0-25 to l-0mgi.v.) was administered if heart rate at the 3rd min of stage V was lower than the target level. During the test, the 12-lead ECG was continuously monitored and recorded at the end of each stage. Blood pressure was non-invasively measured at rest and at each stage of the test. The two-dimensional echocardiogram was continuously monitored and recorded at rest and during the last minute of each stage. As a rule, the infusion of dobutamine was stopped in the presence of new wall motion abnormalities. Off-line analysis of echocardiographic images was performed by two investigators in blind conditions. The left ventricle was divided into 16 segments, and wall motion in each was subjectively scored on a four-point scale: 1= normal; 2 = hypokinetic; 3 = akinetic; 4=dyskinetic[13]; a reduction of systolic thickening was considered the only criterion for wall motion dyssynergy. Eur Heart J, Vol. 18, October 1997 Left ventricular volume measurements The apical two- and four-chamber views were reviewed off-line for volume analysis by a single investigator in blind conditions. End-diastolic and end-systolic volumes were calculated at rest and at peak dobutamine infusion using the biplane modified Simpson's formula'131 in the frame coincident with the R wave (end-diastole) and in the last frame before mitral valve opening (end-systole); the procedure was performed on three consecutive beats and the mean value was drawn. The percent changes from baseline to peak infusion of end-diastolic and end-systolic volumes were considered. Ejection fraction values at rest and at peak dobutamine infusion and the relative percent change were calculated. An abnormal volume response was defined as a less than 10% decrease in end-diastolic volume and as a less than 20% decrease in end-systolic volume at peak dobutamine infusion; the ejection fraction response was defined as abnormal in the presence of a < 10% increase during the test. Alternative cut-off values were considered where defined normality criteria were absent (end-diastolic volume: <20% decrease; end-systolic volume: <30% decrease; ejection fraction: <5% increase). Variability analysis Intra-observer variability, as regards calculation of left ventricular volume, was assessed by the investigator in the first 40 dobutamine stress tests of this study. At baseline, mean percent variability values in two different Downloaded from http://eurheartj.oxfordjournals.org/ by guest on March 6, 2016 was approved by the Hospital Ethics Committee, and all patients gave written informed consent. In all patients, beta-adrenergic blocking agents were withdrawn 48 h and nitrates and calcium antagonists 24 h before the study. Fifty-five patients had a prematurely interrupted test in the absence of new wall motion abnormalities (repetitive ventricular arrhythmias, >0-3 mV ST depression, systolic blood pressure fall >30mmHg, systolic arterial pressure >220 mmHg, severe chest pain or palpitations) and were excluded. Two hundred and thirty-nine patients had a negative dobutamine stress test at the end of the last stage or at the target heart rate (220 - age x 0-85 in men; 200 - age x 0-85 in woman), or a positive test for inducible wall motion abnormalities. In order to minimize technical problems, the echocardiographic examinations, routinely recorded on a SVHS tape, were reviewed by an experienced observer: only 147 patients (62%) with a clear, complete endocardial definition in apical views were considered as having optimal image quality and were admitted to the follow-up study. In each patient, age, gender, clinical history (myocardial infarction, angina), presence of diabetes (need of long-term therapy), presence of hypertension (need of long-term treatment with antihypertensive drugs) and angina during the dobutamine stress test were considered for subsequent analysis. LV volume response during stress echo blind evaluations performed 30 days apart for enddiastolic and end-systolic volumes were, respectively, 5 ± 4% and 5 ± 5%. At peak stress, mean percent values were, respectively, 6 ± 4% and 7 ± 5%. Follow-up data Statistical analysis Results are given as mean value ± SD. Relative differences were compared using the chi-square test with Yates' correction, or the McNemar test when indicated. Cumulative survival curves were calculated by means of the product-limit method of Kaplan and Meier. Statistical differences between curves were assessed with the log-rank or Mantel-Haenszel test. The individual effect of variables on event-free survival was evaluated with the use of the Cox regression model (BMPD 2L, Department of Biomathematics, University of California-Los Angeles, revised 1987), with an unmodified forward-selection stepwise procedure. Variables selected were: age (continuous value), gender (male/female), hypertension (yes/no), diabetes (yes/no), history of myocardial infarction (yes/no), rest ejection fraction (<40%; <50%), presence of rest wall motion abnormalities (yes/no), rest wall motion score index (<15; <2), inducible angina (yes/no), inducible ECG abnormalities (yes/no), inducible wall motion abnormalities (yes/no), inducible wall motion abnormalities at < 20-000 rate-pressure product (yes/no), >0-3 wall motion score index peak-rest difference (yes/no), enddiastolic volume decrease (<10%; <20%), end-systolic volume decrease (<20%; <30%) and ejection fraction increase during the test (>10%; >5%). For multivariate analysis, results are expressed as risk odds ratio. A P value < 0-05 was considered statistically significant. When appropriate, 95% confidence intervals (CI) are described. Results One hundred and forty-seven patients had high-quality echocardiograms and complete clinical and stress test information. Of these, four were lost at follow-up and seven underwent a coronary revascularization procedure less than 6 months after admission to the study. Definite follow-up information was available in 136 patients (116 men, 20 women, mean age 61 years, range 33 to 75). A history of myocardial infarction was present in 87 patients (64%): in 48 patients the myocardial infarction was recent (35%; mean 18 ± 9 days); 49 patients (36%) had stable angina. Hypertension was present in 60 patients (44%) and diabetes in 26 (19%). Dobutamine stress echocat-diography One hundred and three patients (76%) had wall motion abnormalities at baseline echocardiography. Atropine was administered in 43 patients (32%). New wall motion abnormalities occurred in 68 patients (50%). Angina during the test occurred in 41 patients (30%), and inducible ECG abnormalities were observed in 31 patients. Left ventricular volume response An abnormal end-diastolic volume response was observed in 54 patients (40%); in 27 (20%) the volume increased during the test. An abnormal end-diastolic volume response was present in 43/68 patients with, and in 11/68 patients without, inducible wall motion abnormalities (63% vs 16%; P<0001). An abnormal endsystolic volume response was observed in 47 patients (35%); in 18 (13%) the volume increased during the test. An abnormal end-systolic volume response was present in 29/68 patients with, and in 18/68 patients without, inducible wall motion abnormalities (43% vs 26%; Cardiac events Spontaneous cardiac events During 18 ± 7 months of follow-up (range 1-44 months) events occurred in 31 patients: 12 hard events (cardiac death [n = 6], myocardial infarction [n = 6]) and 19 soft events (unstable angina [n=16], congestive heart failure [n = 3]). Revascularization procedures Twenty one revascularization procedures occurred during the follow-up (CABG: 15, PTCA: 6). Of these, eight procedures (CABG: 6, PTCA: 2) were planned in the absence of any spontaneous event. Clinical and stress test variables vs events at follow-up: univariate analysis All events Diabetes was the only clinical variable correlated with spontaneous cardiac events. Eleven of 26 patients with Eur Heart J, Vol. 18, October 1997 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on March 6, 2016 Follow-up data were obtained from at least one of three sources: (1) review of the patient's hospital record; (2) communication with the patient's physician and review of the patient's chart; (3) periodic outpatient clinical evaluation. The outcome events were denned as: cardiac death and non-fatal myocardial infarction for 'hard' event-free survival; cardiac death, non-fatal myocardial infarction, congestive heart failure with a >2 NYHA class increase and unstable angina with ischaemic ECG changes requiring hospital admission for spontaneously occurring event-free survival. Only one event, the worst, was considered in each patient. To avoid any possible interference between test results and elective revascularization procedures, the follow-up times of patients who had coronary revascularization procedures were censored at the time of intervention. In the absence of events, the minimum follow-up period accepted for the study was 6 months. 1601 1602 C. Coletta et al. Table 1 Sensitivity, specificity, positive predictive value and negative predictive value of clinical and stress test variables for spontaneous cardiac events Variable Diabetes Inducible WMA Inducible Angina EDV Dec <10% ESV Dec <20% Sensitivity Specificity PPV NPV 35% 68% 45% 65% 52% 86% 55% 75% 68% 70% 42% 31% 34% 37% 34% 82% 85% 82% 87% 83% Dec=decrease; EDV=end-diastolic volume; ESV = end-systolic volume; NPV = negative predictive value; PPV=positive predictive value; WMA = wall motion abnormalities. Hard events Death or myocardial infarction occurred in five of 26 patients with, and in seven of 110 without, a history of diabetes (P-0037; relative risk: 3-2). Five of 23 patients with <40% and seven of 113 patients with >40% baseline ejection fraction (P=Q-05; relative risk: 31) had a hard event at follow-up. No other considered variables were correlated with a higher probability of subsequent hard events. Cox stepwise regression analysis All events At stepwise regression analysis, an abnormal enddiastolic volume response during dobutamine stress test Hard events A history of diabetes (odds ratio: 402; 95% CI: 1-2612-80) and a less than 40% baseline ejection fraction (odds ratio: 2-21; 95% CI: 1-14-4-29) were independent predictors of cardiac death and non-fatal myocardial infarction (Table 2). Cardiac death No clinical, baseline echocardiographic or stress test variables were independent predictors of cardiac death at follow-up. Survival tables Kaplan-Meier life tables of cardiac event-free survival in relation to the response of end-diastolic volume and to the presence of new wall motion abnormalities during dobutamine stress tests are represented in Fig. 1. The event-free survival rate at 36 months was significantly higher in patients with a normal end-diastolic volume response (a) and in patients without inducible wall motion abnormalities (b). Discussion Several studies using dipyridamole or dobutamine stress echocardiography have demonstrated that stressinduced ischaemia is associated with an adverse longterm outcome'15"201. The presence of inducible wall motion abnormalities was always considered a positive test result. In the present study, an abnormal decrease in left ventricular end-diastolic volume during dobutamine stress echocardiography was the most accurate predictor of spontaneous cardiac events, both at univariate and Cox multivariate regression analysis. A left ventricular volume decrease during exercise echocardiography in normal subjects is a wellknown phenomenon'2'1, and a relationship between an abnormal volume response during exercise and the presence of residual coronary disease was observed in revascularized patients'22'. In patients with multivessel Table 2 Significant predictors of spontaneous cardiac events according to the Cox stepwise regression model All events Variable EDV Dec <10'Vo Diabetes Hard events Odds Ratio 95% CI Variable Odds Ratio 95% CI 3 02 2-70 1-44-6-32 1-28-5-69 Diabetes EF <40% 402 2-21 1-26-12-80 1-14-^-29 CI=confidence intervals: EF = baseline ejection fraction: other abbreviations as in Table 1. Eur Heart J. Vol. 18, October 1997 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on March 6, 2016 diabetes had a spontaneous cardiac event, in comparison with 20/110 without (P=0008; relative risk: 2-3). An adverse outcome was present in 20/54 patients with an abnormal and in 11/82 patients with a normal enddiastolic volume response (/>=0006; relative risk: 2-8). Twenty-one of 68 patients with, and 10/68 patients without, new wall motion abnormalities (/*=0-025; relative risk: 21) had events at follow-up. An abnormal end-systolic volume response (/>=0-039; relative risk: 20) and angina during dobutamine infusion (/>=OO38; relative risk: 1-9) were the other variables related to a higher probability of cardiac events. Values of sensitivity, specificity, positive and negative predictive values of the aforementioned variables for spontaneous cardiac events are represented in Table 1. (odds ratio: 302; 95% CI: 1-44-6-32) and a history of diabetes (odds ratio: 2-70; 95% CI: 1-28-5-69) were independent predictors of spontaneous cardiac events (Table 2). L V volume response during stress echo 1603 (a) 100 90 • • • • • • • • • • • • • • • • • • • • • a * 80 l AAA 70 AA AAAAAAAAAAA 60 50 'AAAAA A 43% 40 30 20 10 18 24 30 36 42 (b) GO 100 90 80 # ^AA A * A # # # VVWVVVVVV A 85% AA A 70 AAAAAAAAAA A AAAAAAAAA AAAAAAAAA 60 - 58% 50 40 30 20 10 1 , , , , , 1 12 1 18 1 24 Time (months) 1 30 1 36 | ,, 42 Figure 1 (a) Kaplan-Meier event-free survival curves in relation to normal/abnormal left ventricular end-diastolic volume decrease during dobutamine stress echocardiography. •=end-diastolic volume decrease >10%, A = end-diastolic volume decrease <10%, / > <0-01. (b) Kaplan-Meier event-free survival curves in relation to the presence/absence of inducible wall motion abnormalities during dobutamine stress echocardiography. • = negative dobutamine stress echocardiography; • = positive dobutamine stress echocardiography, /><0-01. coronary disease, Aroesty et a/.'231 found an increase in left ventricular end-diastolic pressure with abnormal diastolic volume reduction preceding the appearance of new wall motion abnormalities during pacing-induced ischaemia. Perez et al.[24] first described an abnormal decrease in left ventricular areas (end-diastole: <15%; end-systole: <33%) during dobutamine stress test in a group of patients with coronary artery disease. Olson et al. found an abnormal end-diastolic volume change during dobutamine stress echocardiography to be 100% sensitive and 68% specific in the identification of patients with multivessel disease'121. More recently, Dagianti et al. failed to find a relationship between diastolic/ systolic volume index changes during dobutamine stress tests and the presence of coronary disease'251, while in patients with left main coronary disease Attenhofer et al. observed a preserved volume reduction during dobutamine infusion'261. Therefore data are controversial, but an abnormal response in left ventricular volume seems more frequent in patients with multivessel disease, and it could precede the onset of wall motion abnormalities during provocative stress tests. In a preliminary report, Olson et al.l27\ in patients referred for dobutamine echocardiography, found that an abnormal (<20%) decrease in end-diastolic volume at peak infusion was the only predictor of cardiac events (/>=0-02) and cardiac death (P=0-004) at Cox multivariate regression analysis. In our study, an abnormal end-diastolic Eur Heart J. Vol. 18, October 1997 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on March 6, 2016 12 1604 C. Coletta et al. volume response during dobutamine echocardiography was significantly more frequent in patients with spontaneous cardiac events, while an abnormal end-systolic volume response was a weak prognostic indicator. Endsystolic volume is related to the extension of inducible wall motion abnormalities: the interruption of dobutamine infusion in the presence of new wall motion abnormalities prevented further extension of ischaemia and probably limited the value of such a variable as a prognostic marker. Hard events Diabetes and baseline ejection fraction were significantly predictive of cardiac death or myocardial infarction, both at univariate and at Cox regression analysis, while no stress test result was predictive of future hard events. The reliability of the dobutamine stress test as an indicator of death or reinfarction is controversial: Kamaran et al.m found positive dobutamine echocardiography to be predictive of cardiac death in a group of 210 patients. Poldermans et a/.[5] described the absence of correlation between a positive dobutamine stress test and hard events in 430 patients, but in the subgroup of patients with a normal resting wall motion the test was predictive of cardiac death alone. Finally, in our study no variable was predictive of cardiac death, but the low number of events is the likely reason for this result. Limitations of the study Many patients were excluded from the study and the results cannot be extrapolated to a general, unselected population. However, a suboptimal acoustic window was the prevailing criterion of exclusion, and this should not constitute a selection bias. A high-quality echo image was mandatory to minimize problems of left ventricular volume calculation. The variability of our study data were low enough for clinical application, but the results need to be confirmed in patients whose echo image quality is unselected. Coronary angiography was performed in some patients, and the prognostic impact of coronary artery disease was not analysed. However, the aim of the study was to evaluate the prognostic value of various non-invasive parameters; indications for coronary angiography were questionable in the majority of patients. Eur Heart J, Vol. 18, October 1997 Dobutamine-atropine stress echocardiography has a proven prognostic value and is a reasonable first-line option in patients unable to exercise or with controversial ECG results. Our study demonstrated that an abnormal left ventricular diastolic volume response during dobutamine stress echocardiography has an independent prognostic value, and could be helpful in predicting cardiac events in patients with coronary heart disease. We are grateful to Fulvia Seccareccia, MSc, for the invaluable help in statistical analysis. References [1] Picano E. Stress echocardiography: from pathophysiological toy to diagnostic tool. Circulation 1992; 85: 1604-12. [2] Sawada SG, Segar DS, Ryan T et al Echocardiographic detection of coronary artery disease during dobutamine infusion. Circulation 1991; 83: 1605-14. [3] Marcovitz PA, Armstrong WF. Accuracy of dobutamine stress echocardiography in detecting coronary artery disease. Am J Cardiol 1992; 69: 1269-73. [4] Kamaran M, Teague SM, Finkelhor RS, Dawson N, Bahler RC. Prognostic value of dobutamine stress echocardiography in patients referred because of suspected coronary artery disease. Am J Cardiol 1995; 76: 887-91. [5] Poldermans D, Fioretti PM, Boersma E et al. Dobutamineatropine stress echocardiography and clinical data for predicting late cardiac events in patients with suspected coronary artery disease. Am J Med 1994; 97: 119-25. [6] Williams MJ, Odabashian J, Lauer MS, Thomas JD, Marwick TH. Prognostic value of dobutamine echocardiography in patients with left ventricular dysfunction. J Am Coll Cardiol 1996; 27: 132-9. [7] Poldermans D, Fioretti PM, Forster T et al. Dobutamine stress echocardiography for assessment of perioperative cardiac risk in patients undergoing major vascular surgery. Circulation 1993; 87: 1506-12. [8] Borges AC, Pingitore A, Cordovil A, Sicari R, Baumann G, Picano E. Heterogeneity of left ventricular regional wall thickening following dobutamine infusion in normal human subjects. Eur Heart J 1995; 16: 1726-30. [9] Carstensen S, Ali SM, Stensgaard-Hansen FV et al. Dobutamine-atropine stress echocardiography in asymptomatic healthy individuals. The relativity of stress-induced hyperkinesia. Circulation 1995; 92: 3453-63. [10] Tanimoto M, Pai RG, Jintapakorn W. Normal changes in left ventricular filling and hemodynamics during dobutamine stress echocardiography. J Am Soc Echo 1995; 8: 488-93. [11] Pellikka PA, Roger VL, McCully RB et al. Normal stroke volume and cardiac output response during dobutamine stress echocardiography in subjects without left ventricular wall motion abnormalities. Am J Cardiol 1995; 76: 881-6. [12] Olseon CE, Porter TR, Deligonul U, Xie F, Anderson JR. Left ventricular volume changes during dobutamine stress echocardiography identify patients with more extensive coronary artery disease. J Am Coll Cardiol 1994; 24: 1268-73. [13] Schiller N, Shah P, Crawford M et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. J Am Soc Echo 1989; 2: 358-67. [14] Arnese MR, Fioretti PM, Cornel JH, Postma-Tjoa J, Reijs AE, Roelandt JRTC. Akinesis becoming dyskinesis during high-dose dobutamine stress echocardiography: a marker of myocardial ischemia or a mechanical phenomenon? Am J Cardiol 1994; 73: 896-9. Downloaded from http://eurheartj.oxfordjournals.org/ by guest on March 6, 2016 Inducible wall motion abnormalities The presence of new, or the worsening of pre-existing, wall motion abnormalities during dobutamine stress tests was of significant prognostic value only at univariate analysis. The presence of a large ischaemic area or low-level positivity of the test were not related to a poor outcome, either at univariate or multivariate analysis. Pharmacological therapy could have been intensified in the presence of stress-induced wall motion abnormalities; six of eight patients in whom an elective revascularization procedure was planned had new wall motion abnormalities during dobutamine echocardiography. Conclusions LV volume response during stress echo [22] [23] [24] [25] [26] [27] with exercise two-dimensional echocardiography: description of a clinically applicable method and comparison with radionuclide ventriculography. Circulation 1983; 67: 1211-18. Mertes H, Erbel R, Nixdorff U, Mohr-Kahaly S, Kruger S, Meyer J. Exercise echocardiography for the evaluation of patients after nonsurgical coronary artery revascularization. J Am Coll Cardiol 1993; 21: 1087-93. Aroesty JM, McKay RG, Heller FV, Royal HD, Als AV, Grossman W. Simultaneous assessment of left ventricular systolic and diastolic dysfunction during pacing-induced ischemia. Circulation 1985; 71: 889-900. Perez JE, Waggoner AD, Davila-Roman VG, Cardona H, Miller JG. On-line quantification of left ventricular function during dobutamine stress echocardiography. Eur Heart J 1992; 13: 1669-76. Dagianti A. Penco M, Agati L et al. Stress echocardiography: comparison of exercise, dipyridamole and dobutamine in detecting and predicting the extent of coronary artery disease. J Am Coll Cardiol 1995; 26: 18-25. Attenhofer CH, Pellikka PA, Oh JK, Roger VL, Sohn DW, Seward JB. Comparison of ischemic response during dobutamine echocardiography in patients with left main coronary artery disease. J Am Coll Cardiol 1996; 27: 1171-7. Olson CE, Porter TF, Xie F. Abnormal left ventricular volume response during dobutamine stress predicts adverse outcome. (Abstr). Circulation 1994; 90: Eur Heart J, Vol. 18, October 1997 Downloaded from http://eurheartj.oxfordjournals.org/ by guest on March 6, 2016 [15] Severi S, Picano E, Michelassi C et al. Diagnostic and prognostic value of dipyridamole echocardiography in patients with suspected coronary artery disease. Circulation 1994; 89: 1160-73. [16] Picano E, Pingitore A, Sicari R et al. Stress echocardiography results predict risk of reinfarction early after uncomplicated acute myocardial infarction: large-scale, multicenter study. J Am Coll Cardiol 1995; 26: 908-13. [17] Coletta C, Galati A, Greco G et al. Prognostic value of high dose dipyridamole echocardiography in patients with chronic coronary artery disease and preserved left ventricular function. J Am Coll Cardiol 1995; 26: 887-94. [18] Mazeika PK, Nadazdin A, Oakley CM. Prognostic value of dobutamine echocardiography in patients with high pretest likelihood of coronary artery disease. Am J Cardiol 1993; 71: 33-9. [19] Afridi I, Quinones MA, Zoghbi WA, Cheirif JB. Dobutamine stress echocardiography: sensitivity, specificity and predictive value for future cardiac events. Am Heart J 1994; 127: 1510-15. [20] Poldermans D, Arnese M, Fioretti PM et al. Improved cardiac risk stratification in major vascular surgery with dobutamineatropine stress echocardiography. J Am Coll Cardiol 1995; 26: 648-53. [21] Limacher MC, Qinones MA, Poliner LR, Nelson JG, Winters WLJ, Waggoner AD. Detection of coronary artery disease 1605