Dobutamine Stress Echocardiography (DSE) Information for Patients
advertisement
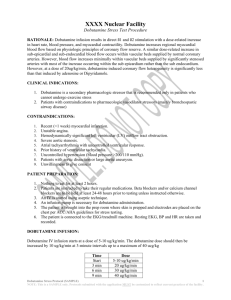
You can find further information on the following websites: www.nhsdirect.nhs.uk (or telephone NHS Direct on 0845 4647) www.bse.org British Society of Echocardiography www.bhf.org.uk Or you may telephone the British Heart Foundation Heart Information Line on 08450708070 Dobutamine Stress Echocardiography (DSE) If you require translation for this Leaflet, please contact: The Cardiology Department, Wycombe Hospital, Queen Alexandra Rd, High Wycombe, Bucks HP11 2TT. Contact details: Gemma Bennett 01494 425902 or Sandra Francis 01494 425903 Information for Patients www.buckinghamshirehospitals.nhs.uk Date of Publication: August 2008 Review Date: August 2010 Leaflet code: Disclaimer This leaflet explains the principles behind DSE and what you may experience during the procedure. It is not, however, comprehensive and should be used in conjunction with consultation with your doctor. Leaflet produced by Melanie Kirk, Cardiology Department, Wycombe Hospital Department of Cardiology Cardiac Imaging Version 1.0 Introduction Dobutamine Stress Echocardiography (DSE) is a test that will allow your cardiologist (heart specialist) to assess the function of your heart and whether it receives an adequate blood supply under stress. It can be used to diagnose or assess coronary artery disease. It is also useful in assessing whether certain parts of the heart are permanently damaged after a heart attack or whether some recovery is possible. The test involves performing an echocardiogram (heart scan) and giving a drug into a vein (dobutamine) that mimics the effects of exercise on the heart. A DSE is helpful in evaluating existing coronary artery disease. It is often used on patients who cannot perform a treadmill test due to arthritis or other physical limitations. It is also useful when the results of the treadmill test do not give us the answers we need. In this leaflet we explain some of the aims, benefits and risks of this procedure. We want you to be fully informed about the procedure and your choices so that you can be involved in making any decisions. Please ask about anything you do not understand or wish to have explained in more detail. You can change your mind about having the procedure at any time. What preparation do I need? If you are on any of the following medications they should be stopped 48 hours before the appointment time. This is because all these medications slow the heart. Bisoprolol Cardicor, Emcor, Monocor Sotalol Beta-cardone, Sotacor Atenolol Tenorim, Co-tenidone, Kalten, Tenoret 50 Tenoretic, Beta-adelat,Tenif. Acebutol Sectral, Secadrex Metoprolol Beatloc, Lopresor, Co-betaloc Carvedilol Eucardic Celiprolol Celectol Labetolol Trandate Pindolol Viskaldix Propranolol Inderal, Inderal LA, Cardinol, Cardinol LA Nadolol Corgard Nebivolol Nebilet Oxprenolol Trasicor, Trasidex, Slow-Trasicor Timolol Betim, Moducren, Prestim Diltiazem Tildiem, Adizem-SR, Adizem-XL, Antigel SR, What is an echocardiogram (heart scan)? An echocardiogram is a diagnostic test that uses ultrasound to take images of your heart. You will be asked to remove all clothing from the waist up and asked to lie on your left-hand side on a special couch. Gel will be applied to your chest and a small probe moved over the skin to view your heart from different angles. High frequency sound waves are transmitted into the body and “echoes” are received back onto the monitor showing the internal structure of your heart. Ultrasound does not use X-rays and it can be safely performed on adults, children and babies. There is no risk to unborn babies. Antigil-XL, Calcocard CR, Dilcardia SR, Dilzem SR Dilzem XL, Slowzem, Tildiem, Viazem, Zemtard Verapamil Cordilox, Securon, Half-Securon, Secron SR, Univer, Verapress MR, Vertab SR Ivabradine Procoralan You should not eat for 2 hours prior to the test. You may take your regular medications (with the exception of those mentioned above) at their usual time with a little water. If you use a nitrolingual (GTN spray) you should take this with you to the appointment. Bring a list of your medications. Wear loose and comfortable clothes and dress so you can easily remove all clothing from the waist up. You may like to bring a newspaper or book. Your blood pressure will be checked on arrival and monitored throughout the test. If it is too high the doctor may decide to postpone the test until it is at an acceptable level. What happens when I arrive at the hospital? On arrival you should report to the Cardiac Day Unit which is located on the upper ground floor of Wycombe Hospital. Go through the double-doors and the nurse’s station is on your righthand side. Hand your appointment letter to a member of staff and you will be shown where to wait. What does the procedure involve? How long does it last? What does it feel like? It is possible to mimic the effects of exercise on the heart by injecting a medicine called dobutamine into a vein. Before the dobutamine is administered you will have an echocardiogram (see above). After the echocardiogram the dobutamine will be given by continuous infusion (drip) through a vein in your arm. This will slowly increase your heart rate in a controlled way. The rate of the dobutamine infusion will be increased every three minutes until you have reached your target heart rate which is determined by your age. Your blood pressure and heart rate will be carefully monitored throughout the test. It is sometimes necessary to give an additional drug called atropine to help you reach your target heart rate. Once you have attained your target heart rate a further scan will be performed. Following this the infusion of dobutamine will be stopped. Depending on the reason for the test you may have an additional scan performed soon after the infusion of dobutamine has begun. The procedure may take up to one hour to complete. However factors such as schedule delays or emergencies may delay the start of your procedure or prolong the length of it. What happens after the procedure? Once the procedure has been completed you will continue to be monitored until your heart rate returns to normal. A cardiac nurse will check on you regularly. We will then remove the cannula (small tube) from your arm and you may get dressed. Do I need someone with me when I go home? Although the effects of the test should have worn off by the time you leave the hospital, it is recommended that you should have a friend or relative drive you home. You may resume your usual diet and activities after the test. The medication may leave you feeling weak for a short period. This will soon pass. Are there any potential risks or complications? A small number of patients may experience minor side-effects. These include headache, nausea and tingling (in fingers, feet or head). These effects usually wear off two to three minutes after the drug has been stopped. If atropine was administered you may experience some blurred vision and a dry mouth. You may also notice symptoms that you would have otherwise developed during normal exercise such as chest pain, palpitations or breathlessness. These usually go away once the test is terminated. If you experience any chest pain (or tightness), breathing difficulties or palpitations during the test, you should notify staff immediately. Potential risks from the procedure are rare, but include complications from the cannula site (bruising or infection), rhythm disturbances of the heart (fewer than 1% of cases), heart attack or stroke (rare: fewer than 1 in 1000 cases). The test is performed regularly in this hospital and the likelihood of a serious event occurring is very low. How can I help to reduce Healthcare Associated Infections? Keeping you hands clean is an effective way of preventing the spread of infections. We ask that you, and anyone accompanying you, use the hand rub (special gel) available at the main entrance of the hospital and at the entrance to every ward before coming into and after leaving the hospital. In some situations hands may need to be washed at a sink using soap and water rather than the hand rub. Staff will let you know if this is the case. For infection control purposes and to keep you safe and well visitors are requested not to: Accompany you if they are unwell Sit on your bed or use the patient toilets Touch your wounds, or any medical devices, drips or catheters. When will I be told the results? We will explain the results of the test as soon as the procedure is completed. It may be that you will need to attend an outpatient appointment in order to discuss the treatment options. A full copy of the report will be sent to the doctor who asked for the test. Who can I contact if I have any more questions? If you have any questions or worries about the procedure, please contact Gemma Bennett in the first instance. Her direct line is 01494 425902.