Overview of CV: Heart and Blood Vessels (BV) Main Path of Blood in
advertisement

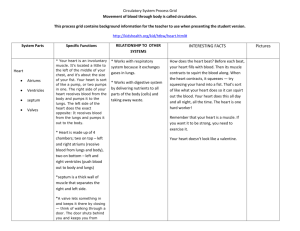
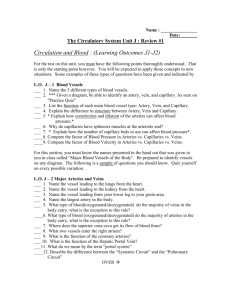
Cardiovascular System: Heart and Blood Vessels Overview of CV: Heart and Blood Vessels (BV) Overview of cardiovascular (CV) system Structure and function of blood vessels Anatomy of heart and path of blood flow Cardiac cycle Control of heart beat and the ECG Pulses and blood pressures Pulmonary and systemic circuit Disorders of cardiovascular system Lymphatic system Components The heart pumps blood The blood vessels are conduits through which blood flows Overall functions Transportation of blood which contains gases, nutrients, wastes… Defend against disease Helps control body temperature, fluid, and pH balance 1 2 Main Path of Blood in the Body Anatomy of Blood Vessels 3 4 Capillaries Arteries Carry blood away from the heart Walls have 3 layers (tunica) Simple squamous epithelium - endothelium Thick smooth muscle layer Outer connective tissue Smallest blood vessels Aorta is the largest artery Arterioles are small arteries that regulate blood pressure and blood flow to capillaries One cell thick with a basement membrane Connect arterioles to venules 5 Microscopic Endothelium Arteriole end—exit of O2, water, and nutrients Venus end—entrance of CO2, water, and wastes 6 1 Exchange at the Capillary Beds… …is primarily a result of diffusion, osmosis, and blood pressure 8 Nutrient Exchange Animation 7 9 10 Venules and Veins Venules receive blood from the capillaries Veins carry blood toward the heart Veins that carry blood against gravity have valves to keep blood flowing toward the heart Veins act as a blood volume reservoir Walls have three layers: ~2/3 of all blood in the body Simple squamous epithelium - endothelium Smooth muscle and CT layers are thinner than arteries but lumen is larger Allow veins to hold a large volume of blood 12 11 2 External View of the Heart and its Vessels Heart is a Muscular Pump 13 14 Two Circulatory Pathways Internal View of the Heart The right side of the heart pumps blood through the pulmonary circuit, which carries blood to and from the lungs The left side of the heart pumps blood through the systemic circuit, which conducts blood to and from the body tissues Heart Function Animation 15 Passage of Blood Through the Heart Superior and Inferior vena cava (O2-poor) Æ Right Atrium Right Atrium Æ Tricuspid Valve Æ Right Ventricle Right Ventricle Æ Pulmonary Semilunar valve Æ Pulmonary Arteries Æ Lungs 4 Pulmonary veins (O2-rich) Æ Left Atrium Left Atrium Æ Atrialventricular valve Æ Left Ventricle Left Ventricle Æ Aortic Semilunar valve Æ Aorta Æ ALL body tissues 16 Valves of the Heart 17 18 3 Coronary Circulation Cardiac Cycle… …is the sequence of heart muscle contraction and relaxation Heart contracts ~70 bpm and lasts 0.85 secs Normal adults rate 60-80 bpm Heartbeat and heart sounds Systole—when ventricles contract and pump blood out of the heart Diastole—when ventricles relax and receive blood from atria Lub = AV valves closing Dup = louder semilunar valves closing Heart murmur—swishing sound from blood flow back into atria due to ineffective valves Can usually be corrected surgically Heart requires 1/20 of body’s total blood flow at rest Cardiac Cycle Animation 19 20 Specialized Cardiac Muscle Cells and the Heart’s Conduction System 21 Sinoatrial (SA) node serves as the pacemaker that determines HR Electrical signal from the SA node spreads through atrial walls causing them to contract - every 0.85 sec Signals stimulate the AV node which in turn sends signals to AV bundle and finally to Purkinje fibers in walls of ventricles causing them to contract Conduction System of the Heart Slight delay at AV node 22 Control of the Heartbeat Internal control External control Cardiac Conduction System Animation 23 The SA node (pacemaker) initiates the heartbeat and causes the atria to contract This impulse reaches the AV node, also in the right atrium, to send a signal down the AV bundle and finally the Purkinje fibers that cause ventricular contraction These impulses travel between gap junctions at intercalated disks Autonomic nervous system (cardiovascular center) and hormones can modify the rate of the heartbeat Other factors are age, gender, fitness level 24 4 Baroreceptors Maintain Arterial Blood Pressure (BP) Electrocardiogram (ECG) Located in aorta and carotid arteries and detect changes in BP When BP rises, arterial BVs are stretched Stretch of baroreceptors causes them to send nerve signals to cardiovascular (CV) center in medulla oblongata CV center responds by sending nerve signals to heart and BV Reduces cardiac output, vasodilates arterioles Net effect is return of BP to normal A record of the electrical changes in cardiac muscle The atria produce an electrical current when stimulated by the SA node called the P wave The contraction of the ventricles is the QRS complex The recovery of the ventricles is called the T wave Used to detect abnormalities Opposite sequence of events occurs if baroreceptors 25 detect drop in BP 26 Blood Pressure Pressure that blood exerts against the walls of blood vessels The highest pressure is during blood ejection from the heart Systolic pressure The lowest pressure is when the ventricles relax Diastolic pressure Highest in aorta and lowest in venae cavae Average blood pressure is recorded at about 120/80 mmHg (systolic/diastolic) 28 27 Blood Pressure Values in Adults Blood pressure varies with age, weight, race, mood, etc… 29 30 5 Pulse Blood Flow Blood flow is under the highest pressure in the arteries Blood flow is slower in the capillaries Alternating expansion and recoil of an arterial wall Pulse rate = heart rate because the arterial walls pulse whenever the left ventricle contracts Some other vital signs Allows time for exchange between cells Blood pressure is minimal in the veins and venules yet blood flow increases Respiratory rate, body temperature 31 32 More on Blood Flow and Pressures Hepatic Portal System Venus return depends on A system that brings blood from the digestive tract to the liver Skeletal muscle contraction One-way valves Pressures associated with breathing Gets first claim to the nutrients in the blood Also removes any bacteria or toxins before they can move on in the body The blood will return to the heart via the inferior vena cava 33 34 Cardiovascular Disorders are Leading Cause of Death in Western Countries Disorders of the Blood Vessels Hypertension Hypertension Atherosclerosis Stroke Heart attack Aneurysm AKA high blood pressure Results when blood moves through vessels at a rate higher than normal A silent killer because there are few symptoms Can lead to a heart attack, stroke or kidney failure Prevention 35 Often due to arterial plaque or atherosclerosis 140/90 mmHg or greater Lower salt intake, control weight, exercise, don’t smoke, limit alcohol intake, don’t abuse drugs such as cocaine and amphetamines, sleep, limit stress 36 6 Atherosclerosis A build up of plaque in blood vessels that reduces blood flow and results in progressive occlusion Result of accumulation of fatty materials beneath inner linings of the arteries and inflammatory response Plaque that is stationary is called a thrombus and an embolus if it detaches and can move to distant sites Associated with stroke, heart attack, and aneurysm Begins in early adulthood and develops progressively during middle age Prevention Atherosclerosis Animation Diet low in saturated fat and cholesterol and rich in omega37 3-polyunsaturated fats; exercise 38 “Good” vs “Bad” Cholesterol Most cholesterol in blood is found bound to carrier proteins- lipoprotein “Good” = High Density Lipoprotein (HDL) “Bad” = Low Density Lipoprotein (LDL) 39 Targets cholesterol for removal in the liver 60 mg/dl and above considered protective against heart disease Carries cholesterol to all body cells and makes it available to them Less than 100 mg/dl is optimal Total cholesterol 40 Less than 200 mg/dl is desirable; 200-239 mg/dl borderline Stroke AKA cerebrovascular accident (CVA) Usually occurs when a cranial artery is blocked or bursts Myocardial Infarction (MI) Part of the brain dies dues to lack of oxygen AKA heart attack Part of the heart dies due to lack of oxygen Symptoms may occur including numbness of hands or face, difficulty speaking, and inability to see in one eye Blockage of a coronary artery or arteries Most common cause is coronary thrombosis Scar tissue replaces dead cardiac muscle 41 Results in diminished pumping ability Can begin with angina pectoris Pain that radiates down the left arm due to partial blockage of a coronary artery Nitroglycerin or nitric oxide dilate BV and helps relieve pain Coronary angiography Procedure to determine if and where there are blockages42 7 Aneurysm A ballooning of a blood vessel Atherosclerosis and hypertension can weaken a vessel and cause ballooning Occurs most commonly in abdominal artery or the arteries leading to the brain 43 44 Dilated and Inflamed Veins Varicose veins Develop when the valves of the veins become weak and ineffective Abnormal and irregular dilations apparent Congestive Heart Failure Superficial veins of leg When occur in the rectum—hemorrhoids Symptoms include shortness of breath, fatigue, weakness, and fluid retention Treatment can include Inflammation of a vein Blood clots may form Condition in which the heart is no longer an efficient pump Phlebitis Heart attack damage, faulty valves, lung disease… Medications to strengthen heart contractions, diuretics, vasodilators If clot blocks a pulmonary vessel, it can kill 45 46 Medical Treatments Dissolving blood clots Gene therapy Vascular endothelial growth factor (VEGF) Injected into area of heart that needs improved blood flow forming collateral BV 60% patients show signs of vessel growth 2-4wks Coronary bypass surgery Tissue plasminogen activator (t-PA) Vein taken and is stitched with one end to aorta and other to end to a coronary artery past the blockage Angioplasty and coated stent Plastic tube with balloon that is inflated and forces vessel open Stent with small metal mess cylinder inserted and is coated with drug that discourage cells growth 47 Recipients need anti-clotting measures due to possibility of clotting Coronary Artery Bypass Graft 48 8 Tips for Prevention of Cardiovascular Disease Do not smoke Do not abuse drugs Keep your weight down to decrease chances of hypertension and Type II diabetes Eat a healthy diet 49 Benefits of Exercise to the Cardiovascular System Know your blood cholesterol Exercise Avoid chronic stress and get adequate sleep 50 Lymphatic System Increases amount of hemoglobin, numbers of RBCs, and blood volume Lowers blood pressure Shifts balance of lipids in blood to “good” form (HDLs) Need to elevate HR to target zone for at least 20 minutes, 3 times/week Low in saturated and trans fats Low in cholesterol Consists of lymph, lymphatic vessels, and lymphoid organs Functions 222 minus age = maximum attainable HR Target zone = 70 to 85% of maximum attainable HR No more than 2 days between sessions 51 53 Lymph vessels also have valves Return the interstitial fluid to the blood stream Transport products of fat digestion Helps defend the body against disease-causing organisms and abnormal cells CV system + lymphatic system = circulatory system 52 54 9 55 10