Usefulness of Macroscopic Urinalysis as a Screening Procedure
advertisement

Usefulness of Macroscopic Urinalysis as a Screening
Procedure
A Preliminary Report
G. BERRY SCHUMANN, M.D., AND NANCY F. GREENBERG, B.S.
Schumann, G. Berry, and Greenberg, Nancy F.: Usefulness
of macroscopic urinalysis as a screening procedure. A preliminary report. Am J Clin Pathol 71: 452-456, 1979. The
macroscopic examination (physicochemical testing) is a sufficient laboratory screening procedure for routine urinalyses
when accurately assessed. Only in those patients for whom
routine urine specimens are macroscopically positive or in
symptomatic patients with or without known renal or urinarytract disease should a microscopic examination be necessary.
Results of this study of more than 900 consecutive routinely
screened urine specimens indicate that there is less than a
3% diagnostic yield when the urine sediment is examined
after a negative macroscopic examination. (Key words: Macroscopic and microscopic urinalysis.)
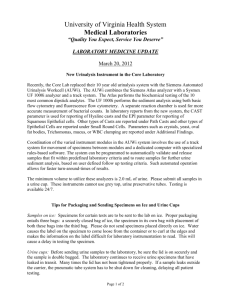
Materials and Methods
Initially, 910 fresh, early-morning, clean, voided,
midstream urine specimens were examined within one
hour after being received in the microscopy section
at Upstate Medical Center. In this study clean-catch
urine specimens were not refrigerated after collection,
and preservatives or fixatives were not used. The
majority of the patients were from hospital admissions,
clinics, or the emergency room. Patients under the care
of the nephrology, urology, or renal transplant services
were excluded, since the majority of these urine specimens were from symptomatic patients and were examined by their own physicians. A reagent-strip* was
used for chemical testing (glucosuria, proteinuria, etc.),
and urinary color, appearance, and specific gravity
were evaluated by the microscopy technologists. A
conventional unstained brightfield microscopy examination was performed after centrifugation of 10 ml of
the urine specimen (2,000 rpm x 5 min).'
In a second study, 102 consecutive clean-catch urine
specimens from both asymptomatic and symptomatic
subjects were evaluated for accuracy in describing
urinary appearance (turbidity). Samples of the original
102 urine specimens were reexamined for turbidity
after results of microscopic examination were recorded.
Turbidity was determined by the ability to read newspaper print through the urine while it was in a transparent, conical centrifuge tube.
In a third study, 220 reagent-strip-negative urine
specimens from asymptomatic and symptomatic subjects were examined by microscopy after their appearance (turbidity) was determined by nephelometry.t
The purpose of this study was to correlate various
amounts of urinary sediment with an accurate measurement of turbidity. The majority of these 220 urine
specimens were visually clear or slightly cloudy.
"Normal" values for formed elements vary from one
laboratory to another. The morphojogic criteria used
Received June 27, 1977; accepted for publication April 6, 1978.
Technical assistance funded by Ames Co. (Division of Miles
Laboratories), Elkhart, Indiana 46514.
Address reprint requests to Dr. Schumann: Director of Cytopathology, University of Cincinnati Medical Center, Cincinnati,
Ohio 45229.
* Multistix, Ames Co. (Division of Miles Laboratories), Elkhart,
Indiana 46514.
t Amylase and Lipase Analyzer, Perkin-Elmer, Coleman Instrument Division, Oak Brook, Illinois 60521.
0002-9173/79/0400/0452 $00.75 © American Society of Clinical Pathologists
452
Downloaded from http://ajcp.oxfordjournals.org/ by guest on March 6, 2016
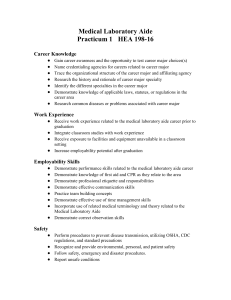
THE EXAMINATION OF URINE is the most common
screening laboratory procedure utilized for the early
detection of renal or urinary-tract disease in asymptomatic subjects. The complete urinalysis 1 involves (1)
macroscopic evaluation of color, appearance (turbidity),
specific gravity, reagent-strip and tablet chemical tests,
and (2) microscopic examination. The latter analysis
is tedious and requires experience, and many times a
more detailed evaluation is necessary. 3 - 7
A major question concerning all routine urinalysis
laboratories is the diagnostic yield of a procedure in
screening urine specimens from asymptomatic individuals. We feel that macroscopic examination is a sufficient screening test for routine urinalyses, and in this
study we evaluate the need of a routine microscopic
analysis on a macroscopically negative urine.
Division of Clinical Pathology, Department of Pathology,
Upstate Medical Center, Syracuse, New York
Vol. 71 . No. 4
453
SCREENING MACROSCOPIC URINALYSIS
Table 3. Positive Findings by Microscopy in 54/555
Urine Specimens Negative by Multistix
Reagent Strip Tests
Table I. Criteria for Classification of Positive
Microscopic Results Using Brightfield
Microscopy 1,2
Urine sediment must contain one of the following:
(1) >5 erythrocytes, leukocytes, or renal tubular cells per highpower field (x 430)
(2) > 3 hyaline casts, > 1 granular cast or presence of any other type
of cast per low-power field (x 100)
(3) > 1 + bacteria per high-power field (x 430)
(4) Presence of fungi, parasites, or viral inclusions
(5) Presence of significant crystals (e.g., cystine) or a large number
of crystals (e.g., uric acid)
to establish positivity or abnormality of a urine sediment by unstained brightfield microscopy is shown in
Table l.1-2
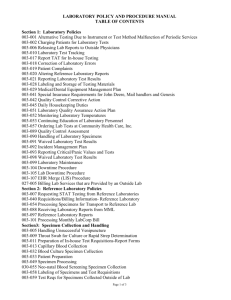
The percentages of urine specimens with proteinuria,
hemoglobinuria, glucosuria, or bilirubinuria that also
had positive microscopic findings are presented in
Table 2. Of the 910 urines examined, 20% (184) had
proteinuria. The distribution of the amounts of proteinuria was: 95 (trace); 41 (1+); 29 (2+); 23 (3+); 2 (4+).
Of these 184 urines with proteinuria, 6 1 % (112) had
positive microscopic findings.
Seven per cent (62/910) had glucosuria and 45% (28/
62) had positive microscopic results. The distribution
of the amounts of glucosuria as measured by the Ames
Clinitest was: 20 (trace); 10 (1+); 8 (2+); 8 (3+);
15 (4+).
Hemoglobinuria was present in 107 (12%) of the urine
specimens (Ames Hemastix), and 65% (70/107) of these
had positive microscopic findings. Two urine specimens
(0.2%) had bilirubin (Ames Icotest), and for both of
these microscopic findings were also positive.
Approximately 10% (54/555) of the routinely screened
urinary specimens yielded positive results on microscopic examination with a negative macroscopic examination (Table 3). Bacteriuria and pyuria were the most
common abnormalities. None of the 54 urine specimens
had more than eight erythrocytes or renal epithelial
Table 2. Percentage of Positive Brightfield Microscopy
Results (910 Routine Urine Specimens)
Positive Findings
Reagentstrip
Results
Macroscopic
Microscopic
No.
%
No.
%
Proteinuria
Glucosuria
Hemoglobinuria
Bilirubinuria
184/910
62/910
107/910
2/910
20
7
12
0.2
112/184
28/62
70/107
2/2
61
45
65
100
Erythrocytes*
Castst
Bacteriuria and pyuria
Renal epithelial cells
Trichomonads and yeasts
3
12
27
9
3
* No specimen had more than 8 erythrocytes per high-power field; 99ft of the urine
specimens with >5 erythrocytes per high-power field were detected by Ames Hemastix.
t in most of the 12 specimens, the casts were hyaline type; rarely, granular type.
cells per high-power field. Most of the 12 specimens
with casts were of hyaline type or a rare granular type.
The specimens with trichomonads and yeasts present
had scant to few numbers of these organisms.
In the second study describing urinary appearance,
21/102 (21%) of the specimens were reported as clear,
but upon reexamination in a transparent, conical centrifuge tube, they were, in fact, turbid. Furthermore, 3/102
(3%) urines that we considered clear were reported as
turbid by the microscopy section. Turbidity was
attributed to pyuria and/or bacteriuria in 13/21 (62%)
Table 4. Correlation of Positive Microscopic Urinalysis
Results from 220 Reagent-strip-negative Urine Specimens with Various Degrees of Turbidity by
Use Nephelometry
(%)
Distribution
of 200 Urine
Specimens
Distribution of
39 Microscopically
Positive
Urine Specimens
3
4
5
6
7
8
9
10
11
12
13
14
8
24
35
36
35
23
11
9
7
3
4
5
0
0
2
2
3
7
4
2
3
0
2
1
3
2
2
2
2
1
0
2
3
4
2
1
3
3
1
0
Turbidity
Visual detection
of turbidity
15
16
17
18
19
20-25
25-50
50-75
75-100
Downloaded from http://ajcp.oxfordjournals.org/ by guest on March 6, 2016
Results
Microscopic Finding
Urine
Specimens
(No.)
A.J.C.P. • April 1979
SCHUMANN AND GREENBERG
454
Table 5. Interpretations of 39 Positive Microscopic Results Following Turbidity Determi nations
Microscopic Results
Urine
Specimens
(No.)
Turbidity
<%)
1
5.0
2
5.5
3
6.0
4
Epithelial
Cells
Mucus
Bacteria
Leukocytes
Erythrocytes
Per HPF*
1+
6.0
Casts
Miscellaneous
Per LPFt
10 hyaline
15
2
7
4
1
1
Interpretation
Dehydration
1 spermatozoon;
1 trichomonad
vet
Nonspecific
J 4 hyaline
( 1 granular
Dehydration
12
4
VC
Trace
5
7
VC
1+
1+
15
3
1+
Trace
1
1
8.0
2+
10
12
10
8.0
1+
20
11
8.0
2+
1+
10
2
VC
12
8.0
2+
1+
15
1
VC
13
10
1
VC
1+
30
2
VC
2+
10
1
UTI
7.0
7.5
7
7.5
8
8.0
9
1+
1+
1+
VC
1 hyaline
Trace yeast
1 2 granular
| 1 epithelial
VC
UTI§
UTI
8.5
1+
14
8.5
1+
15
9.0
16
9.0
2+
10
2
VC
17
9.0
1+
20
1
VC
18
9.0
1+
3
1
2 hyaline
j 1 epithelial
VC
Trace yeast
19
10.0
1+
2+
5
2
VC
20
10.0
1+
2+
7
2
VC
21
11.0
1+
30
8
Pyuria
22
11.0
8
2
23
11.0
1+
50
1
Pyuria
24
13.0
2+
15
5
VC
25
13.0
2+
1
6
26
14.0
1+
10
2
VC
27
15.0
3+
2
4
UTI
28
15.0
Trace
1
1
29
16.0
Trace
3+
3
0
VC
30
18.0
3+
2+
2
2
VC
31
18.5
2+
1+
5
8
1+
2+
2+
Amorphous urates
j 1+ Calcium
)
( oxalate crystals |
J 1 hyaline
j 1 granular
VC
VC
Dehydration
1 hyaline
j 1 granular
VC
TrichomonadsJ
32
19.0
2+
1+
1
1
VC
Downloaded from http://ajcp.oxfordjournals.org/ by guest on March 6, 2016
5
6
455
SCREENING MACROSCOPIC URINALYSIS
Vol. 71 • No. 4
Table5.
{Continued)
Microscopic Results
Urine
Specimens
(No.)
Turbidity
(%)
33
20.5
34
22.0
35
23.0
36
27.0
35.0
37
38
39
Epithelial
Cells
Mucus
Bacteria
Leukocytes
Erythrocytes
Casts
Miscellaneous
50
2+
Pyuria
UTI
25
7 granular
I epithelial
3+
4+
15
20
39.0
1+
80
55.0
3+
20
1+
' HPF, high-power field.
!" LPF, low-power field.
? Renal disease
UTI
UTI
UTI
UTI
$ VC. vaginal contamination.
§ UTI, urinary-tract infection.
tive, 9.7% were microscopically positive by the
criteria in Table 1. When turbidity is considered a
positive macroscopic index, the results of our study
showed that in 16/155 (2.9%) findings were positive
on microscopic examination after negative macroscopic
results.
Discussion
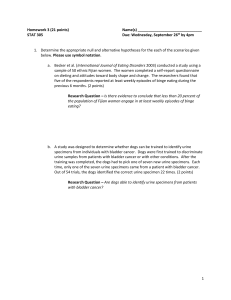
Studies of the diagnostic usefulness and efficiency
of screening routine urine specimens are scant to nonexistent. 26 Development of a new approach for evaluating urinary sediment as a special procedure and complementary diagnostic tool has been of interest to us.
Recently, we have become concerned with the amount
of time spent examining essentially negative urine
specimens.
Macroscopic examinations should be utilized for
screening of specimens to be submitted for microscopic
analysis. Only those specimens with turbidity, proteinuria, glucosuria, hemoglobinuria, or bilirubinuria should
Table 6. Calculation of the Diagnostic Yield of a Routine
Microscopic Urine Examination Following a
Negative Macroscopic Analysis
Total
Number
Routine urines
Reagent-strip* positive urine specimens
Reagent-strip negative urine specimens
Microscopically positive urine specimens
from Multistix reagent-strip negative specimens
Microscopically positive urine specimens from
Multistix reagent-strip and visually clear
negative urine specimens
1
910
355
555
54/555 (9.77r)
16/555 (2.97r)
Multistix, Ames Co. (Division of Miles Laboratories), Elkhart, Indiana 45414.
Downloaded from http://ajcp.oxfordjournals.org/ by guest on March 6, 2016
and amorphous urates or phosphates in 6/21 (29%) of
the specimens.
Results of the third study involving the microscopic
examination of the 220 reagent-strip-negative urine
specimens following nephelometric determinations of
turbidity are presented in Table 4. The majority of
specimens had turbidometric measurements between 4
and 11%. In total, 39 had positive urinary sediment
findings (Table 5).
Below the 8% turbidity level, there were 138/220
(63%) specimens with negative reagent-strip reactions.
Of the 138 specimens, only seven had positive results
on microscopic examination. Of these seven, two represented dehydration by the increased numbers of
hyaline casts; the others represented vaginal contamination. Above the 8% turbidity level, the number of positive
sediment findings increased. Between 8 and 15%
turbidity level, there were 17 positive sediment
findings. We found evidence of urinary tract infection in
three, pyuria in two, and the remainder represented
vaginal contamination. The criteria for vaginal contamination were based on the presence of superficial
squamous epithelial cells, mucus, and cellular debris in
a female patient.' Above the 15% turbidity level (the
level where turbidity is visually detectable), 11/17
specimens (65%) had positive urinary findings. After
discarding specimens interpreted as vaginal contamination, 7/11 (64%) were probably diagnostic of renal or
urinary-tract disease.
The diagnostic yield or false-negative rate of a positive microscopic examination of urine following a negative macroscopic examination is shown in Table 6.
Thirty-nine per cent (355/910) of the routine urines in
this study were reagent-strip (Multistix)-positive. Of
the remaining specimens that were reagent-strip-nega-
Interpretation
456
SCHUMANN AND GREENBERG
The development of strict guidelines for urine specimen collection and processing can reduce problems
such as vaginal contamination and bacterial overgrowth.
Use of (1) a more comprehensive reagent-strip that
tests for nitrite (bacterial growth) and microhematuria
and (2) an accurate measurement of turbidity would
significantly improve the usefulness of the macroscopic
examination as a screening tool. By defining clinically
significant abnormalities, a better assessment of falsenegative results can be obtained.
From the results of this preliminary study, we conclude that there is less than a 3% false-negative rate
(Table 6) when the urine is examined microscopically
after a negative macroscopic examination. Urinarytract infection, pyuria, and dehydration were the only
suggested diagnoses, and probably these patients were
symptomatic at the time (Table 5). Furthermore, urine
cultures and antibody-coated bacterial studies3,8 would
have been more helpful in establishing the correct
diagnosis. At present, it appears that the macroscopic
analysis in itself is a sufficient screening method.
References
1. Bradley GM, Benson ES: Examination of the urine, Todd-Sanford Clinical Diagnosis by Laboratory Methods. 15th edition.
Edited by Davidsohn I, Henry JB. Philadelphia, W. B. Saunders, 1974, pp. 15-81
2. Heimann GA, Forhlich J, Bernstein M: Physician's response
to abnormal results of routine urinalysis. Can Med Assoc J
115:1094-1095, 1976
3. Jones SR, Smith JW, Sanford JP: Localization of urinary-tract
infections by detection of antibody-coated bacteria in urine
sediment. N Engl J Med 290:591-593, 1974
4. Musher DM, Thorsteinsson SB, Airula UM: Quantitative urinalysis, Diagnosing urinary tract infection in men. JAMA 236:
2069-2072, 1976
5. Schumann GB, Harris S, Henry JB: An improved technic for
examining urinary casts and a review of their significance.
Am J Clin Pathol 69:18-23, 1978
6. Schumann GB, Henry JB: An improved technique for the evaluation of urine sediment. Lab Management 15:18-24, 1977
7. Sternheimer R: A supravital cytodiagnostic stain for urinary
sediments. JAMA 231:826-832, 1975
8. Thomas U, Shelokov A, Forland M: Antibody-coated bacteria
in the urine and the site of urinary-tract infection. N Engl
J Med 290:588-590, 1974
Downloaded from http://ajcp.oxfordjournals.org/ by guest on March 6, 2016
be examined microscopically. Microscopic analysis
should also be done on those specimens from symptomatic patients or those with known renal disease even
when a macroscopic examination is negative. Since
many of these patients are monitored daily, urinary
sediment evidence of progressive urinary system disease or response to therapy can be evaluated.
An accurate assessment of turbidity must be made
for each urine specimen. Nephelometry was used to
determine turbidity objectively. Although not routinely
used in the microscopy laboratory, we found it to be
of great value in predicting the amounts of formed
elements in urine. Inspection of urine specimens in
the original containers explained many turbidity misinterpretations. We found that 21/102 (21%) of the urines
were reported as clear, but were indeed cloudy. If an
accurate assessment of turbidity had been made in our
initial study, many of the 54 urines called negative
macroscopically would have been classified as positive
macroscopically. The five most common causes of
turbidity in these urines were leukocytes, erythrocytes,
epithelial cells, bacteria, and amorphous material.
Prospective studies (unpublished data) comparing
unstained brightfield microscopy with a new cytocentrifugation/Papanicoloau stain technic have consistently
shown discrepancies in the morphologic interpretation
of 10-25% of the urines.6 In examining more than 3,000
urine sediments, we have found the latter to be diagnostically superior.6 Although we are not recommending this particular technic for routine screening, we
feel that further evaluation of the urine by "special"
procedures is needed.
In random screenings such as those in physical examinations for insurance purposes, hospital admissions,
etc., much time and expense could be saved by omitting
the microscopic examination on those urine specimens
that are yellow and clear and have a negative chemical
reaction to the reagent strip.
Currently, we are continuing to evaluate the efficacy
of accurate physicochemical testing in screening routine clean-catch urines from asymptomatic subjects.
A.J.C.P. • April 1979