Nucleated Red Blood Cells in Preterm Infants With Retinopathy of
Prematurity
Ronit Lubetzky, MD*‡§; Chaim Stolovitch, MD§㛳; Shaul Dollberg, MD*§;
Francis B. Mimouni, MD, FAAP*§; Mazal Salomon, RN*; and Dror Mandel, MD, MHA*§
ABSTRACT. Objective. The aim of this retrospective
study was to examine hematologic indices of potential
intrauterine hypoxia, including circulating nucleated red
blood cells, lymphocytes, and platelets in preterm infants
who developed retinopathy of prematurity (ROP) compared with suitable controls. We hypothesized that
higher neonatal absolute nucleated red blood cell
(ANRBC) and lymphocyte counts and lower platelets
would be found in infants who developed ROP, compared with control infants.
Methods. Each of 23 infants with ROP was pair
matched for gestational age and Apgar scores with a
control without ROP. Criteria for exclusion in both
groups included factors that may influence the ANRBCs
at birth. Venous ANRBC counts were obtained within 1
hour of life. Statistical analyses used paired t tests, a
paired Wilcoxon test, and backward stepwise-regression
analysis.
Results. Groups did not differ in birth weight, gestational age, Apgar scores, or hematocrit, white blood cell,
or platelets counts. The ANRBC counts at birth were
significantly higher in infants who developed ROP than
in controls.
Conclusions. Infants who develop ROP have higher
ANRBC counts at birth than matched controls. We suggest that increased fetal erythropoiesis exists in preterm
infants who later on will develop ROP. If correct, our
interpretation supports the theory that long-lasting
fetal hypoxia and/or ischemia may play a role in the
pathogenesis of ROP. Pediatrics 2005;116:e619–e622.
URL: www.pediatrics.org/cgi/doi/10.1542/peds.2005-0915;
retinopathy of prematurity, fetal hypoxia.
ABBREVIATIONS. ROP, retinopathy of prematurity; RBC, red
blood cell; WBC, white blood cell; ANRBC, absolute nucleated red
blood cell; IVH, intraventricular hemorrhage.
R
etinopathy of prematurity (ROP) is a developmental vascular disorder that occurs in the
incompletely vascularized retina of premature
infants; it is a major cause of blindness in children in
the developed and developing world. Progress in
neonatal intensive care has led to an increased survival of small preterm infants and, subsequently, to
an increasing incidence of ROP.1,2 In a populationbased cohort study, Chiang et al3 reported that the
overall incidence of ROP among newborn infants in
New York State during the study period was 0.2%.
Although many theories exist about the pathogenesis
of ROP, the mechanisms by which preterm infants
develop ROP are still unclear, and the cause of ROP
is widely considered to be multifactorial.4–6 Hypoxia
of retinal cells, secondary to any one of a variety of
noxious perinatal events, is one of the possible culprits.5 In support of an ischemic-hypoxic theory are
the facts that an increased rate of severe ROP has
been found in infants suffering from fetal growth
restriction7 and neonatal asphyxia,8 conditions
known to potentially compromise blood flow and/or
oxygen supply.
One of the well-described consequences of intrauterine hypoxia is increased compensatory erythropoiesis caused by increased erythropoietin secretion.9–11 In situations associated with intrauterine
hypoxia, such as intrauterine growth restriction, maternal pregnancy-induced hypertension, or maternal
diabetes or smoking, there is an elevation of nucleated red blood cell (RBC) counts at birth, presumably
caused by increased compensatory erythropoiesis.9,12
The aim of this study was to examine hematologic
indices of potential intrauterine hypoxia, including
circulating nucleated RBCs, lymphocytes, and platelets in preterm infants who developed ROP compared with suitable controls. We hypothesized that
higher neonatal absolute nucleated RBC (ANRBC)
and lymphocyte counts and lower platelets would be
found in infants who developed ROP, compared
with control infants.
PATIENTS AND METHODS
Patients
From the Departments of *Neonatology, ‡Pediatrics, and 㛳Ophthalmology,
Tel Aviv Sourasky Medical Center, Tel Aviv, Israel; and §Sackler Faculty of
Medicine, Tel Aviv University, Tel Aviv, Israel.
Accepted for publication Jun 16, 2005.
doi:10.1542/peds.2005-0915
No conflict of interest declared.
Reprint requests to (D.M.) Department of Neonatology, Lis Maternity Hospital, Tel Aviv-Sourasky Medical Center, 6 Weizman St, Tel Aviv 64239,
Israel. E-mail: dmandel@post.tau.ac.il
PEDIATRICS (ISSN 0031 4005). Copyright © 2005 by the American Academy of Pediatrics.
We retrospectively analyzed the charts of all infants who were
admitted to our NICUs, born at the Lis Maternity Hospital, Tel
Aviv Sourasky Medical Center between January 1, 2002, and December 31, 2004, and who were diagnosed with ROP. During that
period a strict protocol of ROP screening, which was consistent
with the 1997 American Academy of Pediatrics guidelines,13,14
was followed. Briefly, all infants who were born with a birth
weight of ⱕ1500 g or a gestational age of ⱕ28 weeks and sick
infants (sick enough to require supplemental oxygen therapy,
mechanical ventilation, or continuous positive airway pressure or
blood pressure support) of ⬎1500 g in birth weight underwent a
dilated indirect ophthalmoscopic examination to detect ROP. The
www.pediatrics.org/cgi/doi/10.1542/peds.2005-0915
PEDIATRICS Vol. 116 No. 5 November 2005
Downloaded from by guest on March 6, 2016
e619
examination was conducted in all infants by a single experienced
pediatric ophthalmologist (C.S.). The examination was performed
in all infants between 4 and 6 weeks’ chronological age or between
31 and 33 weeks’ postmenstrual age.14 Scheduling of follow-up
examinations was determined by the findings at the first examination, using the International Classification of Retinopathy of
Prematurity.13,14 Follow-up examination was continued until vascularization had proceeded to zone 3. Infants with threshold disease were considered candidates for ablative surgery of at least 1
eye within 72 hours of diagnosis.
Each infant with ROP of any stage was pair matched with the
infant admitted immediately after him or her who did not develop
ROP and had the same gestational age (⫾1 week) and 1- and 5minute Apgar scores (⫾1). In an attempt to control for the various
variables known to affect neonatal nucleated RBC counts, we
excluded from the study infants in both groups who were born to
women with gestational or insulin-dependent diabetes15; pregnancy-induced hypertension16; intrauterine growth retardation
(defined as a birth weight below the 10th percentile using the
Lubechenco curves12,17); placental abruption or placenta previa18;
any maternal heart, kidney, lung, or other chronic condition; drug,
tobacco, or alcohol abuse19; perinatal infections (eg, maternal fever, maternal leukocytosis [white blood cells (WBCs) ⬎ 15.0 ⫻
103/mm3], clinical signs of chorioamnionitis such as fever and
abdominal tenderness)20; any abnormality in electronic intrapartum monitoring18; or infants with low Apgar scores (⬍6 at 1 or 5
minutes).21 We also excluded infants with perinatal blood loss,
hemolysis (blood-group incompatibility with positive Coombs test
or hematocrit of ⬍45%),22 or chromosomal anomalies.23 Because of
these exclusion criteria, we had to exclude 10 potential controls
who were each replaced by the appropriate control infant born
immediately after it. Follow-up data were available from the medical charts in our pediatric ophthalmology clinic, when available,
or by telephone interview with the parents.
Hematologic Methods
In our institution, all preterm infants admitted to the NICU
undergo a routine complete blood count with differential count
within the first hour of life. Venous blood samples for complete
blood cell counts were analyzed according to laboratory routine
using an STK-S counter (Coulter Corporation, Hialeah, FL). Differential cell counts were performed manually, and nucleated RBC
counts were counted per 100 WBCs. We showed previously that
leukocyte counts and ANRBC numbers are not independent.24
Thus, traditional expression of nucleated RBCs as their number
per 100 WBCs might introduce a significant bias. Therefore, we
expressed the number of nucleated RBCs as ANRBCs rather than
per 100 leukocytes, and the WBC count was expressed as corrected
for the presence of nucleated RBCs. We also corrected the absolute
lymphocyte count, another potential index of fetal hypoxia.25
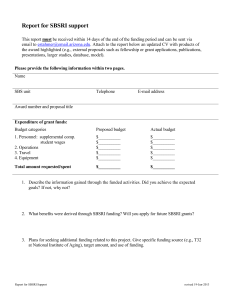
TABLE 1.
Statistical Methods
Data are reported as mean ⫾ SD, n (%), or, for non-normally
distributed variables (such as ANRBCs or Apgar scores) as median (range). Statistical analysis included the 2-tailed paired t test
for normally distributed variables and paired Wilcoxon test for
ANRBCs or Apgar scores. Backward stepwise-regression analysis
was used to assess the effect of gestational age (or birth weight), 1or 5- minute Apgar scores, intraventricular hemorrhage (IVH)
status, and ANRBC count (independent variables) on the ROP
status (dependent variable). We also used Pearson ranked-regression analysis to study the correlation between ROP severity (defined by its stage from 0 [no ROP] to 4, whichever the zone) and
the ANRBC count. P ⬍ .05 was considered significant.
Our local institutional review board approved the study. Because all preterm patients in our institution receive a routine
complete blood count after birth, including nucleated RBC count,
the requirement for informed consent was waived.
RESULTS
A total of 23 infants with ROP were retained for
analysis and compared with 23 controls. Four additional infants with ROP were excluded because of
maternal diabetes (n ⫽ 2), neonatal polycythemia (n
⫽ 1), and maternal asthma (n ⫽ 1). Table 1 depicts
some major demographic and clinical characteristics
of infants with ROP and controls. There were no
significant differences between groups in all clinical
or demographic parameters considered, to the inclusion of infant birth weight, gestational age, major
diagnoses such as respiratory distress syndrome,
patent ductus arteriosus, IVH, and periventricular
leukomalacia, and major treatments and procedures
such as umbilical artery and vein catheters, mechanical ventilation, antibiotic treatment, indomethacin
for patent ductus arteriosus closure, and endotracheal administration of surfactant. By design, infants
with ROP did not differ from controls in terms of
gestational age and Apgar scores.
Table 2 shows the highest stage of ROP (most
severe stage diagnosed in either of the eyes) of children with ROP, the need for laser therapy, and the
outcome. Follow-up data at the age of at least 1 year
were available on 18 patients: 10 from the medical
charts in our ophthalmology clinic and 8 by tele-
Demographic and Perinatal Characteristics of Infants With ROP and Matched Controls
Gestational age, wk, mean ⫾ SD (range)
Birth weight, g, mean ⫾ SD (range)
Prolonged rupture of membranes (24 h), n (%)
Administration of prenatal antibiotics, n (%)
Administration of prenatal betamethasone, n (%)
1-min Apgar score, median (range)
5-min Apgar score, median (range)
Presence of respiratory distress syndrome, n (%)
Endotracheal surfactant administration, n (%)
Duration of ventilation, d, mean ⫾ SD
Maximal oxygen delivered, %, mean ⫾ SD
Duration of oxygen delivered, d, mean ⫾ SD
Patent ductus arteriosus, n (%)
Indomethacin for patent ductus arteriosus, n (%)
IVH, n (%)
Periventricular leukomalacia, n (%)
Umbilical artery catheter, n (%)
Umbilical vein catheter, n (%)
Duration of total parenteral nutrition, d, mean ⫾ SD
Infants With ROP
(n ⫽ 23)
Controls
(n ⫽ 23)
P
28.3 ⫾ 2.3 (24–33)
1097 ⫾ 451 (570–2245)
11 (47.8)
10 (43.5)
15 (65.2)
8 (7–9)
8 (6–10)
15 (65.2)
13 (56.5)
5.4 ⫾ 8.3
27.5 ⫾ 10.38
10.8 ⫾ 12.8
17 (73.9)
13 (56.5)
5 (21.7)
3 (13.04)
9 (39.1)
9 (39.1)
7.3 ⫾ 5.8
28.8 ⫾ 2.8 (24–34)
1186 ⫾ 546 (530–2625)
11 (47.8)
10 (43.5)
14 (60.9)
8 (7–9)
8 (6–10)
16 (69.5)
15 (65.2)
5.3 ⫾ 5.2
24.9 ⫾ 12.15
9.8 ⫾ 10.4
18 (78.3)
15 (65.2)
6 (26.1)
3 (13.04)
7 (30.4)
8 (34.8)
7.4 ⫾ 4.8
.10
.16
.77
.72
.30
.42
.30
.33
.67
.41
.56
.41
.19
.16
.43
.67
.18
.19
.39
None of the differences were statistically different.
e620
NUCLEATED RED BLOOD CELLS AND RETINOPATHY OF PREMATURITY
Downloaded from by guest on March 6, 2016
TABLE 2.
Characteristics of the Infants With ROP
n (%)
Stage
1
2
3
4
Laser treatment
Plus disease
Outcome at ⱖ1 y of age
Visual acuity: central, steady, maintained
Muscle balance: orthophoria
Refractive error: myopic astigmatism
13 (56.6)
5 (21.7)
5 (21.7)
0 (0)
2 (8.7)
1 (4.3)
14 (61.0)
13 (56.5)
4 (17.4)
phone interview of the parents. All 8 patients had
been examined by a pediatric ophthalmologist. All
the parents interviewed over the telephone reported
that no visual problems had been diagnosed.
Table 3 depicts the hematologic data obtained in
both groups. The ANRBC counts at birth were significantly higher in infants with ROP than in control
infants (paired Wilcoxon test: P ⫽ .02). There were no
differences between the 2 groups in terms of hematocrit or WBC, lymphocyte, or platelets counts. In
backward stepwise logistic-regression analysis, taking into account gestational age (or birth weight), the
1- or 5- minute Apgar scores, the IVH status, and the
ANRBC count as independent variables and the ROP
status as the dependent variable, only the ANRBC
was a predictor of ROP (P ⫽ .02). Figure 1 depicts in
a graphic manner the relationship between ANRBC
and ROP stage. Because ANRBCs are not normally
distributed, we used the log ANRBC as the predictor
for stage of ROP. A best-fit cubic-regression equation
was developed: ROP stage ⫽ ⫺9.74 ⫹ 11.23 (log
ANRBC) ⫺ 4.14 (log ANRBC)2 ⫹ 0.52 (log ANRBC)3
(R2 ⫽ 0.122; P ⬍ .001).
DISCUSSION
In a retrospective study, we found that the development of ROP was associated with an increase in
ANRBCs. In our study we excluded small-for-gestational-age infants, which is an important confounding variable.26 We also excluded infants with other
factors associated with potentially increased ANRBC
counts, including hemolysis,22 chromosomal anomalies,23 maternal diabetes,15,27 and neurologic insults.28,29 It is important to note that the 2 groups in
our study (infants with ROP and controls) ended up
being very similar in birth weight, gestational age,
Apgar scores (by design), and major neonatal complications. Thus, we believe that our study confirms
our hypothesis that as a group, preterm infants with
ROP have increased neonatal ANRBC counts.
TABLE 3.
Fig 1. The relationship between ANRBCs and ROP stage.
The mechanism by which ROP is associated with
increased circulating neonatal ANRBC counts is unknown. A likely explanation is relative fetal hypoxia.15,25,30 In favor of a contribution of hypoxia/ischemia in the pathogenesis of ROP are the facts that an
increased rate of ROP has been found in conditions
known to potentially compromise retinal blood flow
and/or oxygen supply, such as fetal growth restriction7 and severe neonatal asphyxia.8 In our study,
the lymphocyte count, also believed to be an indicator of fetal hypoxia,25 was not elevated, and the
platelet count was not decreased, but these hematologic parameters might indicate acute rather than
chronic hypoxia.25 In this retrospective study, cord
blood gases, which theoretically might have helped
in the diagnosis of fetal hypoxemia, were not routinely obtained in all infants. However, cord blood
gases are indicative of the acute oxygenation status
of the fetus in contrast with ANRBCs, which are
indicative of the oxygenation status of the fetus at
least a few days before delivery.31 In terms of timing,
if the elevation of ANRBC counts in the ROP group
is indeed related to fetal hypoxia, as we speculate,
this hypoxia must have been of sufficient duration to
stimulate erythropoietin secretion. The relationship
between hypoxia and ROP is not yet completely
investigated but might involve an increase in vascular endothelial growth factor production induced by
hypoxia, which in turn may stimulate neovascularization.5,32,33 Another possibility under investigation
is hypoxia-induced stimulation of insulin-like
growth factor-binding protein-1 production, which
in turn may decrease free insulin-like growth factor
concentrations, which may prevent normal vessel
growth.5,33–35
Hematologic Characteristics of the Infants With ROP and Matched Controls
Hematocrit, %
WBCs (corrected), ⫻ 109/L
Platelets, ⫻ 109/L
Absolute lymphocyte count, ⫻ 109/L
ANRBCs, ⫻ 106/L
Infants With ROP
Controls
P
49 ⫾ 9/49 ⫾ 6
12.4 ⫾ 5.8
245.1 ⫾ 67.0
7.2 ⫾ 3.5
1785 (122–8550)
0.49 ⫾ 0.06
11.7 ⫾ 5.9
243.9 ⫾ 51.6
6.1 ⫾ 3.6
789 (50–3063)
NS
NS
NS
NS
.02
Data are expressed as mean ⫾ 1 SD except the non-normally distributed ANRBCs, which are
expressed as median (range). NS indicates not significant.
www.pediatrics.org/cgi/doi/10.1542/peds.2005-0915
Downloaded from by guest on March 6, 2016
e621
We suggest that increased fetal erythropoiesis exists in preterm infants who later on will develop
ROP. If correct, our interpretation supports the theory that fetal hypoxia and/or ischemia may play a
role in the pathogenesis of ROP. Although the retrospective aspect of our study requires a replication of
results in a prospective manner, we speculate that
elevated ANRBCs at birth may help to define a subgroup of preterm infants at increased risk for ROP.
REFERENCES
1. Silverman WA. Retrolental Fibroplasia: A Modern Parable. New York, NY:
Grune and Stratton; 1980
2. Kim TI, Sohn J, Pi SY, Yoon YH. Postnatal risk factors of retinopathy of
prematurity. Paediatr Perinat Epidemiol. 2004;18:130 –134
3. Chiang MF, Arons RR, Flynn JT, Starren JB. Incidence of retinopathy of
prematurity from 1996 to 2000: analysis of a comprehensive New York
state patient database. Ophthalmology. 2004;111:1317–1325
4. Campbell K. Intensive oxygen therapy as a possible cause of retrolental
fibroplasia; a clinical approach. Med J Aust. 1951;2(2):48 –50
5. Smith LE. Pathogenesis of retinopathy of prematurity. Semin Neonatol.
2003;8:469 – 473
6. Mccolm JR, Fleck BW. Retinopathy of prematurity: causation. Semin
Neonatol. 2001;6:453– 460
7. Bardin C, Zelkowitz P, Papageorgiou A. Outcome of small-forgestational age and appropriate-for-gestational age infants born before
27 weeks of gestation. Pediatrics. 1997;100(2). Available at: www.pediatrics.
org/cgi/content/full/100/2/e4
8. Arroe M, Peitersen B. Retinopathy of prematurity in a Danish neonatal
intensive care unit, 1985–1991. Acta Ophthalmol Suppl. 1993;210:37– 40
9. Finne PH. Erythropoietin levels in cord blood as an indicator of intrauterine hypoxia. Acta Paediatr Scand. 1966;55:478 – 489
10. Vatansever U, Acunas B, Demir M, et al. Nucleated red blood cell
counts and erythropoietin levels in high-risk neonates. Pediatr Int. 2002;
44:590 –595
11. Ostlund E, Lindholm H, Hemsen A, Fried G. Fetal erythropoietin and
endothelin-1: relation to hypoxia and intrauterine growth retardation.
Acta Obstet Gynecol Scand. 2000;79:276 –282
12. Minior VK, Bernstein PS, Divon MY. Nucleated red blood cells in
growth-restricted fetuses: associations with short-term neonatal outcome. Fetal Diagn Ther. 2000;15:165–169
13. Fierson WM, Palmer EA, Biglan AW, Flynn JT, Petersen RA, Phelps DL.
Screening examination of premature infants for retinopathy of prematurity. A joint statement of the American Academy of Pediatrics, the
American Association for Pediatric Ophthalmology and Strabismus,
and the American Academy of Ophthalmology. Pediatrics. 1997;100:273
14. American Academy of Pediatrics, Section on Ophthalmology. Screening
examination of premature infants for retinopathy of prematurity. Pediatrics. 2001;108:809 – 811
15. Green DW, Mimouni F. Nucleated erythrocytes in healthy infants and
in infants of diabetic mothers. J Pediatr. 1990;116:129 –131
e622
16. Sinha HB, Mukherjee AK, Bala D. Cord blood haemoglobin (including
foetal haemoglobin), and nucleated red cells in normal and toxaemic
pregnancies. Indian Pediatr. 1972;9:5490 –5493
17. Lubchenco LO, Hansman C, Dressler M, Boyd E. Intrauterine growth as
estimated from live-born birth weight data at 24 to 42 weeks gestation.
Pediatrics. 1963;32:793–799
18. Korst LM, Phelan JP, Ahn MO, Martin GI. Nucleated red blood cells: an
update on the marker for fetal asphyxia. Am J Obstet Gynecol. 1996;175:
843– 846
19. Halmesmaki E, Teramo KA, Widness JA, Clemons GK, Ylikorkala O.
Maternal alcohol abuse is associated with elevated fetal erythropoietin
levels. Obstet Gynecol. 1990;76:219 –222
20. Leikin E, Garry D, Visintainer P, Verma U, Tejani N. Correlation of
neonatal nucleated red blood cell counts in preterm infants with histologic chorioamnionitis. Am J Obstet Gynecol. 1997;177:27–30
21. Hanlon-Lundberg KM, Kirby RS. Nucleated red blood cells as a marker
of acidemia in term neonates. Am J Obstet Gynecol. 1999;181:196 –201
22. Thomas RM, Canning CE, Cotes PM, et al. Erythropoietin and cord
blood haemoglobin in the regulation of human fetal erythropoiesis. Br J
Obstet Gynaecol. 1983;90:795– 800
23. Oski FA, Naiman JL. Hematologic Problems in the Newborn. 2nd ed.
Philadelphia, PA: WB Saunders Co; 1972:15–17
24. Green DW, Khouri J, Mimouni FB. Neonatal hematocrit and maternal
glycemic control in insulin-dependent diabetes. J Pediatr. 1992;120:
302–305
25. Phelan JP, Korst LM, Ahn MO, Martin GI. Neonatal nucleated red blood
cell and lymphocyte counts in fetal brain injury. Obstet Gynecol. 1998;
91:485– 489
26. Snijders RJM, Abbas A, Melby O, Ireland RM, Nicolaides KH. Fetal
plasma erythropoietin concentration in severe growth retardation. Am J
Obstet Gynecol. 1993;168:615– 619
27. Mimouni F, Miodovnik M, Siddiqi TA, Butler JB, Holroyde J, Tsang RC.
Neonatal polycythemia in infants of insulin-dependent diabetic mothers. Obstet Gynecol. 1986;68:370 –372
28. Green DW, Hendon B, Mimouni F. Nucleated erythrocytes and intraventricular hemorrhage in preterm neonates. Pediatrics. 1995;96:475– 478
29. Naeye RL, Localio R. Determining the time before birth when ischemia
and hypoxemia initiated cerebral palsy. Obstet Gynecol. 1995;86:713–719
30. Hermansen MC. Nucleated red blood cells in the fetus and newborn.
Arch Dis Child Fetal Neonatal Ed. 2001;84:F211–F215
31. Sheffer-Mimouni G, Mimouni FB, Lubetzky R, Kupferminc M, Deutsch
V, Dollberg S. Labor does not affect the neonatal absolute nucleated red
blood cell count. Am J Perinatol. 2003;20:367–371
32. Leske DA, Wu J, Fautsch MP, et al. The role of VEGF and IGF-1 in a
hypercarbic oxygen-induced retinopathy rat model of ROP. Mol Vis.
2004;10:43–50
33. Smith LE. Pathogenesis of retinopathy of prematurity. Growth Horm IGF
Res. 2004;14(suppl A):S140 –S144
34. Kajimura S, Aida K, Duan C. Insulin-like growth factor-binding protein-1 (IGFBP-1) mediates hypoxia-induced embryonic growth and developmental retardation. Proc Natl Acad Sci USA. 2005;102:1240 –1245
35. Ozen S, Akisu M, Baka M, et al. Insulin-like growth factor attenuates
apoptosis and mucosal damage in hypoxia/reoxygenation-induced intestinal injury. Biol Neonate. 2004;87:91–96
NUCLEATED RED BLOOD CELLS AND RETINOPATHY OF PREMATURITY
Downloaded from by guest on March 6, 2016
Nucleated Red Blood Cells in Preterm Infants With Retinopathy of Prematurity
Ronit Lubetzky, Chaim Stolovitch, Shaul Dollberg, Francis B. Mimouni, Mazal
Salomon and Dror Mandel
Pediatrics 2005;116;e619; originally published online September 30, 2005;
DOI: 10.1542/peds.2005-0915
Updated Information &
Services
including high resolution figures, can be found at:
/content/116/5/e619.full.html
References
This article cites 29 articles, 6 of which can be accessed free
at:
/content/116/5/e619.full.html#ref-list-1
Subspecialty Collections
This article, along with others on similar topics, appears in
the following collection(s):
Ophthalmology
/cgi/collection/ophthalmology_sub
Permissions & Licensing
Information about reproducing this article in parts (figures,
tables) or in its entirety can be found online at:
/site/misc/Permissions.xhtml
Reprints
Information about ordering reprints can be found online:
/site/misc/reprints.xhtml
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned, published,
and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk
Grove Village, Illinois, 60007. Copyright © 2005 by the American Academy of Pediatrics. All
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on March 6, 2016
Nucleated Red Blood Cells in Preterm Infants With Retinopathy of Prematurity
Ronit Lubetzky, Chaim Stolovitch, Shaul Dollberg, Francis B. Mimouni, Mazal
Salomon and Dror Mandel
Pediatrics 2005;116;e619; originally published online September 30, 2005;
DOI: 10.1542/peds.2005-0915
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
/content/116/5/e619.full.html
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned,
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2005 by the American Academy
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on March 6, 2016