CRRT Guideline - Alfred Intensive Care Unit
advertisement

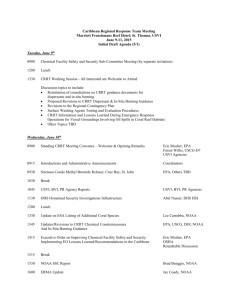
GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) TARGET AUDIENCE ICU Nursing Staff ICU Medical Staff PURPOSE This guideline describes the medical & nursing management of patients receiving renal replacement therapy as a patient in the Intensive Care Unit (ICU). If the patient is simultaneously receiving ECMO, the ECMO guideline should also be consulted. This guideline does NOT describe the management of patient receiving: Hepatic Support using the MARS therapy, OR Plasma Exchange using the Prismaflex TPE therapy, OR Charcoal Filtration using the Prismaflex. GUIDELINE This guideline should be read in conjunction with the Bayside Clinical Care Standards Policy Mutual Obligations for Patient Safety & Quality of Services at Bayside Health [ICU] CRRT Initial Settings CRRT Initial settings.pdf [ICU] Anticoagulation in CRRT (Heparin) CRRT Anticoagulation (Heparin).pdf [ICU] Anticoagulation in CRRT (Citrate) CRRT Regional Anticoagulation (Citrate).pdf [Drug Guideline] LEPIRUDIN INFUSION Lepirudin.pdf [ICU] Recirculation procedure on the Prismaflex CRRT Recirculation on the PrismaFlex.pdf REFERENCES (In APA citation style - for style see: http://www2.liu.edu/cwis/cwp/library/workshop/citapa.htm) Need to add references KEYWORDS Continuous Renal Replacement Therapy (CRRT) CVVHDF CVVH CVVHD AUTHOR / CONTRIBUTORS * denotes key contact Name *Nat Adams Geik Lim Bianca Levkovich Dr Owen Roodenburg Dr Ashley Crosswell ICU Nurses Position ICU Clinical Nurse Educator ICU Clinical Nurse Specialist Clinical Pharmacist ICU Consultant ICU Registrar ICU Renal Special Interest Group Service / Program Need to populate footer Endorsed by: Name/Title: Date: Approved by: Name/Title: Date: Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 1 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) Disclaimer: This guideline has been developed within the context of Alfred Health service delivery. Alfred Health shall not be responsible for the use of any information contained in this document by another organisation outside of Alfred Health. CONTENTS 1. Indications for Continuous Renal Replacement Therapy (CRRT)..…………………….. 3 2. Establishing Vascular Access for CRRT ...................................................................... 4 3. “Heparin-lock” for Vascular Access …................................................................. ……. 5 4. Commencing CRRT using Prismaflex… ............................................................. ……. 6 4.1 Priming Equipment........................................................................................................ 6 4.2 Priming Fluid ................................................................................................................ 6 4.3 Priming Machine .......................................................................................................... 6 4.4 Attaching Machine to the Patient (via vascath) ............................................................ 7 4.5 Settings for CRRT using Prismaflex (non-citrate)........................................................ 9 4.6 Disconnecting from Prismaflex ..................................................................................... 10 4.7 Recirculation on Prismaflex…………………………………………………………………. 12 5. Anticoagulation for CRRT.............................................................................................. 12 5.1 General Anticoagulation Rules ..................................................................................... 12 5.2 Monitoring and Adjusting Anticoagulation in CRRT………………………………………. 14 6. Nursing Management of Patient on CRRT using Prismaflex……….…………………… 15 6.1 Nursing Management - Cannula (vascath)………………………………………………… 15 6.2 Nursing Management - Machine (Prismaflex)…………………………………………….. 15 6.3 Nursing Management - Circuit………............................................................................ 15 6.4 Nursing Management - Patient…………………………………………………………..…. 16 6.5 Nursing Management - Documentation …………………………………………………… 16 6.6 Nursing Management - Troubleshooting ………………………………………….……… 16 6.7 Nursing Management - Waste management & safety…………………………………… 16 7.0 Management of Renal Replacement Therapy (CRRT)................................................ 17 7.1 Management of Patient‟s Electrolytes.......................................................................... 17 7.1.1 Calculating potassium chloride concentration in CRRT 5L fluid bags…………………. 17 7.2 Management of Patient‟s Fluid Balance....................................................................... 18 7.3 Management of Patient‟s Acid-Base Balance.............................................................. 18 7.4 Management of Patient‟s Toxin Removal..................................................................... 19 Appendix 1: Glossary of Terms Used with CRRT ............................................................... 20 Appendix 2: Prismaflex Controls........................................................................................... 25 Appendix 3: Molecular Weights ........................................................................................... 26 Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 2 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 1. Indications for Continuous Renal Replacement Therapy 1.1 Primary goal of CRRT To compensate for loss of renal function, & correct its associated sequelae, including: Accumulation of nitrogenous waste products Electrolyte disturbance Metabolic acidosis Volume overload 1.2 Indications for commencing CRRT Currently there is no measurable parameter, or marker of renal function that mandates commencement of CRRT. Instead, CRRT may be initiated to treat the adverse sequelae mentioned above. A reasonable, but by no means exclusive approach would be: Development of uraemic signs or symptoms Management of fluid overload Electrolyte disturbance o Hyperkalaemia not responding to pharmacological therapy, or causing physiologic disturbance o Other less common - Na+, Ca2+, PO43-,Mg2+, & uric acid Metabolic acidosis Dialyzable or filterable toxins (aspirin, lithium, methanol, ethylene glycol, methotrexate, & theophylline, myoglobin metabolites etc) Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 3 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 2. Establishing Vascular Access for CRRT 2.1 Equipment Standard tray Antiseptic solution (e.g. chlorhexidine) / * betadine only for ECMO circuits Local anaesthetic (e.g. lignocaine) Sterile gown & gloves Mask & protective goggles Cannula (e.g. vascath ) 10 ml ampoule of 0.9% sodium chloride (x2) Syringes - 5 ml & 10 ml Needles - 19 g & 21 or 25 g Leur-lock IV caps (x2) Transparent film dressing (e.g. Tegaderm) Suture material (2/0 silk) Scalpel blade Biopatch +/- Heparin 5000 units in 5ml (x1) [if heparin-lock required] 2.2 Procedure Refer to insertion guidelines within the ICU Central Venous Catheter Guideline Central Line Catheter (CVC) in ICU.pdf 2.3 Site Site of vascath cannulation may affect filter performance, it is preferable to gain access via either Femoral vein > R) Internal Jugular > Subclavian >L) Internal jugular. Note: If long-term haemodialysis is likely, subclavian vascath access should be avoided due to the risk of subclavian vein stenosis. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 4 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 3. “Heparin-lock” for Vascular Access When vascath lumens are not being used, each lumen should be “heparin-locked” with undiluted heparin (ampoule 5000 units in 5 ml) to the volume of the lumen. The volume of the lumen is specified on each of the 2 lumens on the vascath (e.g. red lumen 1.7ml, blue lumen 1.8ml) This remains in situ until the vascath is next used for CRRT or for other IV access Heparin-lock must be aspirated before vascath is used For patients with a heparin sensitivity (i.e. HITS), six hourly 0.9% sodium chloride 10 ml flush should be used instead. 3.1 Equipment Dressing pack Sterile huck towel Antiseptic solution (e.g. chlorhexidine) / * betadine only for ECMO circuits Sterile gloves & protective goggles Syringe - 10 ml (x4), to aspirate & then flush each lumen 0.9% sodium chloride 10ml (x2) Syringe - 2 ml (x2) Needle - 19 g (x2) Heparin 5000 units in 5ml (x1) Leur-lock IV caps (x2) or Positive Pressure Valves (PPV) if 0.9% sodium chloride flushes to be used. 3.2 Procedure 1. Apply goggles, perform hand hygiene, open & add equipment to sterile field 2. Perform hand hygiene & apply sterile gloves 3. Draw up 2 x 10ml 0.9% sodium chloride 4. Using 2ml syringes & needles, draw up Heparin to the specified volume printed on each vascath lumen 5. Place sterile drape from dressing pack underneath vascath 6. Remove leur-lock caps (or PPV‟s if in situ) 7. “Scrub the hub” of each lumen with antiseptic solution & allow to dry 8. Place sterile huck towel underneath newly cleaned vascath 9. Aspirate 10ml blood from each lumen, then flush with 10ml 0.9% sodium chloride to ensure that vascath lumen is clear of blood 10. Instil heparin (gently) according to volume specified on vascath 11. Attach leur-lock caps or PPV (as above) and apply lumen clamp. 12. Label vascath with heparin stickers & drug label to indicate “heparin-lock” in situ. Sign drug order. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 5 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 4. Commencing CRRT using Prismaflex 4.1 Priming Equipment Prismaflex machine Prismaflex Set (standard set ST 100), (need to add section on ST 150 sets) Wide-bore, thermal blood warmer tubing 50 ml leur-lock syringe + 50mls of 0.9% sodium chloride Priming solutions: o 0.9% sodium chloride 1L bag (x2) o Heparin 5000units in 5mls (x2) Dialysate, PBP & Replacement fluids (refer to guideline below) o CRRT Initial settings.pdf Additives for CRRT 5L fluid bags if required (e.g. potassium chloride) If using anticoagulation, collect chosen drugs & delivery devices ICU Renal Replacement Record (CRRT Orders) MR M31 4.2 Priming Fluid The Prismaflex CRRT circuit is primed twice. The first facilitates heparin bonding to the filter membrane, while the second removes excess heparin from the priming solution. Do not use heparin in patients diagnosed with HITS. (Prime once with sodium chloride) Priming solutions: 1st Prime: 0.9% sodium chloride 1000ml with heparin 10,000units (unless HITS) 2nd Prime: 0.9% sodium chloride 1000ml Note: if machine is to be idle for > 30 minutes, leave 2 nd prime until about to connect to patient, otherwise a 3rd prime will be required prior to connecting to patient. 4.3 Priming Machine 1. Follow instructions on screen CLOSELY (read the screen) 2. Choose CVVHDF mode (this ensures all other modes are available) 3. Enable syringe, add 50mL syringe primed with 0.9% sodium chloride 4. Add warming coil to blood circuit (via blue leur-lock connections, post filter), wrap coil around blood warmer 5. Check all connections are secure 6. Prime TWICE, (1st heparin, 2nd 0.9% sodium chloride) 7. Perform Prime Test 8. Accept patient fluid gain/loss 400 mls / 3 hours; unless patient is 30kg or less (consider decreasing accepted value in lighter patients) 9. If machine idle for > 30 minutes prior to attaching to patient – perform another prime. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 6 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 4.4 Attaching Machine to the Patient (via vascath) 4.4.1 Equipment 2 people Dressing pack Sterile huck towel Antiseptic solution (e.g. chlorhexidine) / * betadine only for ECMO circuits Sterile gloves & protective goggles Syringes, 10ml (x 4) 10ml 0.9% sodium chloride (x 2) Leur-lock IV cap 4.4.2 Preparation This procedure requires 2 people o Person 1 (sterile) - accessing vascath o Person 2 (scout) - managing lines, machine & patient Explain procedure to patient & provide reassurance Position of comfort, preferably supine to monitor patient‟s haemodynamic status Consider potential for hypotension on commencement of CRRT. Assess patient‟s haemodynamic status PRIOR to attachment to Prismaflex. Ensure ICU registrar present or readily available when connecting patient Discuss options for management of haemodynamic instability with ICU registrar prior to connecting the patient. o Consider fluid loading & availability of vasopressors (e.g. noradrenaline, metaraminol) o Consider increasing inotropes prior to connecting patient Position patient supine if possible to facilitate monitoring & management of haemodynamics prior to, & during commencement of CRRT. Ensure continuous & accurate blood pressure monitoring Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 7 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 4.4.3 Procedure Person 1(Using aseptic technique & holding non-sterile lines with antiseptic soaked gauze, ascertain patency of both access (red) & return (blue) lumens of vascath): o Apply goggles, perform hand hygiene, open & add equipment to sterile field o Perform hand hygiene & apply sterile gloves o Draw up 2 x 10ml 0.9% sodium chloride o Place sterile drape from dressing pack underneath vascath o Remove leur-lock caps (or PPV‟s if in situ) o “Scrub the hub” of each lumen with antiseptic solution & allow to dry o Place sterile huck towel underneath newly cleaned vascath o Aspirate 10 mls of blood from each vascath lumen & discard – address any patency / flow issues, (see 6.1 Nursing Management of Cannula) o Flush each vascath lumen with 10mls of 0.9% sodium chloride – address any patency / flow issues, (see 6.1 Nursing Management of Cannula) o Clamp both lumens Person 2 – (Pass lines to person 1, ensuring they are clamped, not tangled or contaminated & attend to Prismaflex flow rates) o Hand Access line (red) to Person 1, who takes hold of it with sterile antiseptic soaked gauze & connects it directly to the access lumen (red) of vascath. o Swap Effluent line (yellow) & Return line (blue), so that effluent line (yellow) is now directly connected to effluent bag & return line (blue) is connected to one lumen of the “Y” connector (still attached to the priming bag). o If spare limb of “Y” connector is not being used (e.g. for protamine or calcium), clamp spare limb closest to bifurcation, to minimise blood backflow into lumen during treatment & add leur-lock IV cap o Detach “Y” connector from priming bag & hand to Person 1, who takes hold of it with sterile antiseptic soaked gauze & connects it directly to vascath return lumen (blue). Persons 1 & 2 o Ensure that all lines are unclamped. Person 2 o o o o o Start blood flow rate at 50ml/min & assess patient for any compromise in haemodynamic status. Increase blood flow rate to target rate, (see section 4.5) ideally within 5 minutes. Do not start PBP, Dialysate or Fluid Removal until CRRT blood flow has been safely increased to target; patient is haemodynamically stable and anticoagulation has been commenced. Once blood flow target rate is reached & patient is stable, enter dialysate, PBP, replacement & fluid removal rates (see section 4.5) Ensure that de-aeration chamber level is adequate (blood–fluid interface) 4.4.4 Post procedure Ensure current, signed, valid IV orders for all priming & treatment fluids (MR M31) Continue to observe for & address any haemodynamic instability Secure all lines, ensuring tension relieving secondary anchor dressing in situ Ensure blood warmer turned on Ensure emergency blood return pack available at back of Prismaflex machine Need to add link to photos of line securing Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 8 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 4.5 Settings for CRRT using Prismaflex (non-citrate) Note: For patients being treated using citrate anticoagulation, see Citrate/Calcium guideline CRRT Regional Anticoagulation (Citrate).pdf For all other anticoagulation (e.g. Heparin), or no anticoagulation – the set up is as follows: 4.5.1 CVVHDF (Pre Dilution) on Prismaflex Provides solute removal by both convection & diffusion. Allows patient fluid removal if required. Parameter Blood Flow Dialysate Flow Initial Setting 50mls/min 0 ml/hr until Blood flow at target 0 ml/hr until Blood flow at target Target Setting 250ml/min 30x Patient Weight (in kg) to maximum 3000mls or (100kgs) 200 ml/hr (to reduce clotting in deaeration chamber) 1250 ml/hr Replacement Flow (Post) PBP Flow (used for fluid replacement as Pre-Dilution) Fluid Removal Rate Anticoagulation 0 ml/hr until Blood flow at target 0 ml/hr until Blood flow at target as per Protocol (if used) as per ICU Medical Orders as per Protocol (if used) 4.5.2 CVVHDF (Post Dilution) on Prismaflex Provides solute removal by both convection & diffusion. Allows patient fluid removal if required. Parameter Blood Flow Dialysate Flow Initial Setting 50ml/min 0 ml/hr until Blood flow at target Replacement Flow (Post) PBP Flow Fluid Removal Rate Anticoagulation 0 ml/hr until Blood flow at target (not used) 0 ml/hr until Blood flow at target as per Protocol (if used) Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 9 of 26 Target Setting 250ml/min 30x Patient Weight (in kg) to maximum 3000mls or (100kgs) 1250 ml/hr (used for fluid replacement as Post-Dilution) (not used) as per ICU Medical Orders as per Protocol (if used) Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 4.5.3 CVVHD on Prismaflex Provides solute clearance by diffusion. Allows patient fluid removal if required. Parameter Blood Flow Dialysate Flow Initial Setting 50mls/min 0 ml/hr until Blood flow at target Replacement Flow (Post) PBP Flow Fluid Removal Rate Anticoagulation 0 ml/hr until Blood flow at target (not used) 0 ml/hr until Blood flow at target as per Protocol (if used) Target Setting 250ml/min 30x Patient Weight (in kg) to maximum 3000mls or (100kgs) 200 ml/hr (to reduce clotting in deaeration chamber) (not used) as per ICU Medical Orders as per Protocol (if used) 4.5.4 CVVH on Prismaflex Provides solute removal by convection. Allows patient fluid removal if required. Note: CVVH is not routinely used in Alfred ICU 4.5.5 SCUF on Prismaflex Provides fluid removed by ultrafiltration. Note: SCUF is not routinely used in Alfred ICU Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 10 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 4.6 Disconnecting from Prismaflex (either cessation of treatment or for recirculation) 4.6.1 Equipment 2 people Dressing pack Sterile huck towel Antiseptic solution (e.g. chlorhexidine) / * betadine only for ECMO circuits Sterile gloves & protective goggles 500mls 0.9% sodium chloride Bag spike x1 for cessation, x 2 for recirculation [for lumen aspiration, flush & heparin-lock] o Syringe - 10 ml (x4), to aspirate & then flush each lumen o 0.9% sodium chloride 10ml (x2) o Syringe - 2 ml (x2) o Needle - 19 g (x2) o Heparin 5000 units in 5ml (x1) o Leur-lock IV caps (x2) or Positive Pressure Valves (PPV) if 0.9% sodium chloride flushes to be used. Consider adding extra gauze pieces to aid sterility when accessing multiple lumens Note: The above equipment is available in a pre-made pack (located in ICU equipment store) & should be available at the back of the Prismaflex at all times. This ensures equipment is readily available if blood needs to be returned urgently 4.6.2 Preparation This procedure requires 2 people o Person 1 (sterile) - accessing vascath, o Person 2 (scout) - managing lines, machine & patient Explain procedure to patient & provide reassurance Position of comfort, preferably supine to monitor patient‟s haemodynamic status Turn off anticoagulant infusions (if applicable) 4.6.3 Procedure Person 1 o o o o o Place sterile huck towel underneath vascath “Scrub the hub” of each lumen & allow to dry Ask 2nd person to press “Stop” via Prismaflex screen Using sterile antiseptic soaked gauze - clamp access (red) lumen & limb of access (red) circuit. Disconnect access (red) limb of circuit & add spike, then pass to person 2 who: will connect to 0.9% sodium chloride 500ml unclamp access (red) circuit limb choose „End Treatment‟ or „Change Circuit‟ via Prismaflex screen follow instructions on Prismaflex screen to return blood, (if not clotted) if filter clotted, disconnect without returning blood Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 11 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) Person 1 (continued) o o o o o o o Aspirate access (red) lumen to remove remnant clots, then flush lumen with 10ml of 0.9% sodium chloride Wait until blood in circuit has been returned via return (blue) lumen, then Using sterile chlorhexidine soaked gauze - clamp return (blue) lumen & limb of return (blue) circuit Disconnect & pass to 2nd person to discard in yellow clinical waste bin Aspirate return (blue) lumen to remove remnant clots, then flush lumen with 10ml of 0.9% sodium chloride Heparin lock vascath lumens (see section 3 “Heparin-lock”). Label vascath with heparin stickers & drug label to indicate “heparin-lock” in situ. Sign drug order Either person o o o Ensure all blood circuit lines are clamped before unloading Unload circuit from Prismaflex & discard in yellow clinical waste bin Discard effluent bag fluid into pan room sluice & other remaining fluids into sink NOTE: If treatment ceased due to any Prismaflex malfunction; clearly describe incident & all alarms preceding, providing as much information as possible to help Equipment Nurse / Gambro mechanics to troubleshoot issues. 4.7 Recirculation on Prismaflex Utilised when patient requires temporary disconnection (< 120 mins) from CRRT (e.g. troubleshooting of access issues, transport, short procedure, physiotherapy), to preserve circuit & prolong filtration time. For procedure see “CRRT Recirculation” CRRT Recirculation on the Prismaflex.pdf For Prismaflex screen prints demonstrating the recirculation procedure, see Prismaflex Recirculation Slides.pdf Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 12 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 5. Anticoagulation for CRRT 5.1 General Anticoagulation Rules Anticoagulation is required to prevent clotting of the extracorporeal circuit during CRRT, with the aim being to anticoagulate the circuit, but not necessarily the patient. This anticoagulation can be achieved in a number of ways depending on which is most appropriate for the patient, & preference of the treating team. NOTE: Unless contraindicated or choosing non-standard anticoagulation, most patients should default to having low dose heparin added to the CRRT circuit. CRRT Anticoagulation (Heparin).pdf Other options: No anticoagulation Heparin low dose (circuit) Heparin / Protamine (circuit) Systemic therapeutic anticoagulation o Heparin o Lepirudin o Bivalirudin Citrate / Calcium (circuit) Other anticoagulation (please discuss with ICU pharmacist prior to commencement): o Epoprostenol (circuit) In most cases, anticoagulation infusions should be attached to the filter syringe line. If anticoagulant reversal is used (e.g. Protamine, Calcium), it should be connected via a 'Yconnector‟ at the return cannula of the vascath. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 13 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 5.2 Monitoring and Adjusting Anticoagulation in CRRT Check anticoagulation as per specific protocol. Monitoring times vary, dependant on type of anticoagulation being utilised. Options for Patient sample: o o o Arterial line (preferable) CVC lumen (this sample must be labelled clearly). First sample port of (red) component of circuit, between the vascath access lumen & the PBP fluid entering the circuit (for patients without alternate access as per above) The Circuit sample to be taken from the (red) pre-filter sample port. o o o o o “Scrub the hub” of pre filter port with alcohol swab Use a 5ml syringe (with 21g or smaller needle) or ABG syringe (for citrate) & insert into the rubber port of sample site Aspirate blood slowly to avoid disrupting pressure pod membranes: 2.7mls for APTT 0.5 -1ml in ABG syringe for ionized calcium Pull back on syringe plunger when pulling out needle as there will be pressure behind it & it may spray blood Inject blood into appropriate blood tube Adjust dosage of anticoagulation according to relevant ICU protocol. o CRRT Anticoagulation (Heparin).pdf o CRRT Regional Anticoagulation (Citrate).pdf If restarting treatment after filter has clotted (< 24 hrs), refer to protocols above for anticoagulation dose guidance. If restarting CRRT after more than 24 hours since last filter, start anticoagulation as for new filter circuit. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 14 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 6. Nursing Management of Patient on CRRT using Prismaflex 6.1 Cannula Access site: o Monitor for signs of bleeding or disconnection o Monitor for signs & symptoms of infection Dressing: o Maintain dressing integrity, ensure Biopatch correctly placed o Ensure tension relieving secondary anchor dressing in situ o Change dressing weekly / prn & document on ICU Active. Limb observations: o 8/24 + prn (if femoral approach) o Colour, warmth, movement, sensation & pedal pulses present Assessing patency o Assess patency of cannula lumens prior to attaching to circuit o Removal of blood or return of sodium chloride (10 mls in 3 secs) suggests good access. o If removal or return is difficult or sluggish, don‟t connect to circuit until these access issues are resolved – this may result in a new vascath. 6.2 Machine (Prismaflex) Don‟t prime CRRT circuit until vascath is in situ & patent Consider position of machine before connecting circuit to patient: o Ensure safe access around room o Adequate circuit line length available to reach patient‟s vascath o No fluid bags resting on any equipment or patient‟s bed (as this will affect the machine‟s weight system to adjust fluids) Plug into blue UPS power point (if possible) Lock brake Unless attaching immediately, label circuit with date & time of priming. 6.3 CRRT circuit: Circuit o o o o Ensure blood warmer turned on Ensure all connections are tight If primed circuit idle > 30mins (&<24hours) reprime with 1L 0.9% sodium chloride prior to attachment to patient. If primed circuit idle > 24 hours – discard (or keep for teaching) Returning blood o o o Ensure emergency equipment for return of blood available at back of Prismaflex machine (see 4.6 Disconnecting from Prismaflex) Consider elective return of blood & change of circuit when TMP rises significantly over a period of time. Note: sudden rises are likely to be access-related issues which may be resolved with troubleshooting. Prismaflex machine will prompt user to change the circuit after 72 hours of use or 780L of blood exchange - whichever occurs first. This is a company recommendation & they will not guarantee the integrity of the membrane fibres after this time. This alarm can be overridden, but a yellow alarm will remain present on the machine. Please discuss with medical staff if you are considering leaving the same circuit running after this alert. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 15 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 6.4 Patient: Monitor total patient input & output to assess fluid status, (See 7.2 Management of Patient’s Fluid Balance) Ideally, avoid hip flexion > 30° if femoral cannula in situ check if possible to go higher Ensure lines are secured & tension relieving anchor dressing in situ Monitor coagulation & adjust as per anticoagulation protocols o CRRT Anticoagulation (Heparin).pdf o CRRT Regional Anticoagulation (Citrate).pdf add single link to stickers Monitor patient's core body temperature add further warming options as required. (Note: May mask septic febrile event), 6.5 Documentation: Ensure ALL CRRT fluids are documented & signed on MR M31 Hourly documentation on ICU chart as per stickers: o CRRT Sticker 2012 (non-Citrate).pdf o CRRT Sticker 2012 (Citrate).pdf Document any interruption or cessation of treatment, including a reason, on the bottom of the ICU chart 6.6 Troubleshooting: Have a 2nd person (line manager) present for patient turns to prevent movement of cannula & reduce potential for “access” alarm issues If trouble with “access” alarms, consider: o Using “change bags” option just prior to moves / turns o Rotating cannula at the hub to move it off the wall of the vessel (if appropriate vascath) o Adding 1-2mls 0.9% sodium chloride into circuit via an access pod, to make circuit less negative & allow blood pump to recommence 6.7 Waste management & safety Ideally have only 2 bags of 5L CRRT fluid made up at any one time Ensure cytotoxic stickers on both circuit & effluent bags if patient in cytotoxic precautions. If discarding cytotoxic effluent in sluice, nurse is responsible for removal of emptied bags. Maximum of 2 effluent bags to be left in a cubicle at a time. Don‟t pile effluent bags on top of each other as this may lead to leakage. Adhere to “Safemove”, back smart principles when moving, attaching & disconnecting any CRRT fluid bags. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 16 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 7. Management of Renal Replacement Therapy (CRRT) The primary role of the kidneys is to maintain the composition & volume of the extra cellular fluid, thereby ensuring a constant environment in which normal cellular functions can take place. The kidneys accomplish this by: Regulating plasma composition with regard to electrolytes & osmolality Regulating fluid balance to maintain circulating volume & total body water Maintaining the acid-base balance by excreting hydrogen ions & conserving HCO3Excreting the toxic waste products of metabolism while conserving substances needed by the body During CRRT, these renal functions are managed by the ICU medical & nursing staff. Note that CRRT can also mask signs of other organ systems in failure (e.g. the temperature in a febrile patient, or the serum lactate in patients with an ischaemic bowel). 7.1 Management of Patient‟s Electrolytes The healthy kidney regulates serum electrolyte concentrations. CRRT principally regulates electrolytes by establishing a diffusion gradient across the semi-permeable membrane. The dialysis solutions contain many electrolytes at concentrations (mmol/L) equivalent / close to the desired plasma concentration (mmol/L). Solutions may or may not contain potassium, As the patient‟s blood passes along the membrane, electrolytes diffuse down the concentration gradient across the semi-permeable membrane until the levels equilibrate on each side. However, other processes in the body may also be increasing or reducing the serum level of these electrolytes, (e.g. vomiting, diarrhoea, multiple blood transfusions, bleeding, severe acidosis, endocrine dysfunction, TPN) Plasma electrolytes must be regularly monitored whilst patient is receiving CRRT 7.1.1 Calculating potassium chloride concentration in CRRT 5L fluid bags Note: ALWAYS check whether there is potassium preloaded into bag (e.g.: PrismOcal) Final 5L bag potassium chloride concentration = added potassium chloride (mmols/L) / 5L For example, if you add: o 20 mmol/L potassium chloride to 5 L bag = (20 mmol/L / 5 Litres) = 4 mmol/L o 10 mmol/L potassium chloride to 5 L bag = (10 mmol/L / 5 Litres) = 2 mmol/L Note: Add the same potassium chloride amount to both the dialysate & PBP 5L bags (unless using PrismOcal which already contains potassium) Serum potassium level may fall quite rapidly if no potassium is added to CRRT fluid bags Take into account patient‟s clinical condition when considering what potassium amount to add to CRRT fluid bags o Patient may have large amounts of potassium loss, e.g. Diarrhoea o Patient may have alternate sources of potassium delivery, e.g. TPN o Patient may require higher serum potassium level; e.g. Cardiac issues Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 17 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 7.2 Management of Patient‟s Fluid Balance During CRRT, the patient‟s fluid balance is determined by the net effect of fluids prescribed to the patient, & fluid removed by the machine. The daily fluid balance is prescribed during the ICU medical rounds. This balanced is achieved by altering the hourly fluid removal by the CRRT machine. When setting the hourly fluid removal it is important to consider: the prescribed 24 hour fluid balance goal the obligatory fluid inputs including nutrition (TPN, oral & enteral), infusions, drug administration additional occasional fluid inputs including blood products fluid losses including urine, faecal, wounds, drains & insensible losses Total fluid balance should be calculated & assessed at least 4 hourly, to ensure hourly CRRT fluid removal rate will support 24 hour fluid removal goal E.g. Target Daily Fluid Balance = minus 2000mL Hourly Fluid Balance = minus 2000/24 = minus 83mL Hourly Fluid Removal = hourly input + 83mL The patient's haemodynamic stability (BP, CVP, etc) should be assessed prior to altering CRRT fluid removal rate. 7.3 Management of Patient‟s Acid-Base Balance In acute kidney injury (AKI), organic & inorganic acids are retained leading to metabolic acidosis. During a polyuric phase of AKI, the renal tubules fail to reclaim the bicarbonate (HCO3-) from glomerular filtrate. Thus, a patient with AKI may have either an excess of acids or a deficit of total body HCO3-. Additionally, the patient‟s primary pathology may increase circulating acids including lactic or ketotic acids. During CRRT, HCO3- diffuses into the patient‟s blood across the filter membrane, while acids are removed through convection & diffusion. Severely acidotic patients with AKI may require urgent filtration to assist with management of an acute metabolic acidosis. Caution should be used when the patient‟s primary pathology is being monitored via plasma acid levels (e.g. Lactic acid to monitor bowel ischaemia). CRRT will lower serum acid levels & may falsely imply an improvement in the underlying pathology. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 18 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) 7.4 Management of Patient‟s Toxin Removal Provided their molecular weight is small enough to pass through the pores of the filter membrane, toxins will be removed through CRRT. The rate at which toxins are removed is affected by their protein binding; the CRRT flow rates & the amount of clotting that has occurred within the filter. Daily monitoring of serum urea & creatinine levels provides a method of measuring the effectiveness of the CRRT. Consider a filter circuit change if urea & creatinine have increased during the previous 24 hour period. Other agents that may be removed during CRRT: Inotropes: o inotropes are usually titrated to effect, the inotropic effect should be closely monitored when starting or ending CRRT; as serum levels may be affected by inotrope loss through the filter or sudden cessation of CRRT Antibiotics: o consideration should be given to antibiotic loss through the filter o alert pharmacist when CRRT is commenced or to be ceased Drugs: o close monitoring of therapeutic drugs should be maintained, dosing may need to increase whilst on the filter, but also importantly dose reduction may be required if CRRT is ceased for extended periods without return of native kidney function Electrolytes: o see above for potassium management, however CRRT will influence total body gains or losses of other electrolytes o phosphate supplementation will usually be required after the first few hours of CRRT Nutrition: o water soluble vitamins & smaller amino acids can be lost during CRRT Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 19 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) Appendix 1: Glossary of Terms Used with CRRT Access Pressure The pressure measured by the blood circuit‟s Access Pressure Pod just after the blood flow exits from the patient, but before the blood pump & haemofilter. Convection The movement of solutes during ultrafiltration (UF), in the direction of the flow of the water. Convection rates are greatly increased when replacement fluid is used due to the increased flow across the filter membrane. Also called “solvent-drag”. Counter-Current The process by which two fluids flow in opposite direction, on either side of a semi-permeable membrane. During CRRT the blood flow & dialysate flow run as counter-currents. This means that the differing solute concentrations are maintained for the length of the haemofilter, optimising solute exchange across the membrane. CVVH (Continuous Veno-Venous Haemofiltration) Continuous haemofiltration with the aid of a blood pump provides solute removal by convection. It offers high volume ultrafiltration using replacement fluid, which can be administered pre-filter or postfilter. The pump guarantees adequate blood flow to maintain required UF rates. CVVHD (Continuous Veno-Venous Haemodialysis) Continuous haemodialysis with the aid of a blood pump, using venous access via dual lumen vascath. It provides solute removal by diffusion, & fluid removal by osmosis. Dialysate is pumped in counter-current flow to the blood. As the blood progresses along the semipermeable membrane, the composition of the plasma approaches that of the dialysate. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 20 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) CVVHDF (Continuous Veno-Venous Haemo-Diafiltration) Continuous haemodiafiltration with the aid of a blood pump provides solute removal by diffusion & convection simultaneously. It offers high volume ultrafiltration using replacement fluid, which can be administered pre-filter or post-filter. Simultaneously, dialysate is pumped in counter-current flow to the blood. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 21 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) Diffusion Movement of solutes from an area of high concentration to an area of low concentration. In CRRT, solutes will only diffuse across the semipermeable membrane if they are smaller than the size of the filter pores. (see Molecular Weights Table below) Filter Gradient (ΔP) (also called „Pressure Drop‟) Pressure used to determine micro-clotting in the hollow fibres of the filter. As resistance within the filter increases so too does the pressure gradient required to maintain the same flow. Measures the pressure difference between blood at the top & bottom of the filter to determine micro-clotting within the filter. ΔP = Filter Pressure – Return pressure Filter Pressure The highest pressure in the blood flow. It is measured after the blood pump & prior to the filter. Thus, it reflects the force required to pump the blood through the filter. Filtration / Ultrafiltration In ultrafiltration, plasma water with solutes is pulled from the patient‟s blood across the semi-permeable membrane in the filter. The effluent pump automatically controls the ultrafiltration rate by adjusting the hydrostatic pressure gradient (TMP) across the filter membrane. Only solutes that are smaller than the pore size of the filter will pass through the membrane. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 22 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) Osmosis / Oncotic Attraction Movement of water from an area of low solute concentration to an area of high solute concentration. In CRRT, different blood & dialysate solute volumes are maintained by the semi-permeable membrane. Plasma proteins, being larger than the filter pore size, remain on the blood side of the membrane. PBP (Pre Blood Pump) If required, the PBP infuses sterile replacement solution into the blood circuit, at the beginning of the Access Line. Post-Dilution Haemofiltration circuit where replacement is added after the blood has passed through the filter. The blood becomes highly concentrated due to fluid removal through the filter membrane. Pre-Dilution Haemofiltration circuit where replacement is added prior to the blood entering the filter. The bloods solutes, clotting factors, & osmotic pull are diluted prior to entering the filter. Return Pressure Pressure measured in blood circuit just prior to return to patient. Provides information about the patency of the blood return line & cannula. Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 23 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) SCUF (Slow Continuous Ultrafiltration) Continuous process of fluid removal across a semipermeable membrane, providing patient fluid removal by ultrafiltration. No substitution fluid or dialysate is used. TMP Pressure exerted across the filter membrane during operation. Pressure difference between the blood & fluid compartments. Predicts the risk of haemolysis within the filter. TMP = Filter Pressure + Return Pressure - Effluent Pressure 2 Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 24 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) Appendix 2: Prismaflex Controls Appendix 3: Molecular Weights Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 25 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet. GUIDELINE Title CONTINUOUS RENAL REPLACEMENT THERAPY (CRRT) IN ICU (DRAFT ONLY) Prompt Doc No: <#doc_num> v<#ver_num> Approval Date: <#issue_date> Page 26 of 26 Review & Update by: <#next_review_date> The hard copy of this document may be out of date. To ensure you are reading the current version, check the policy & guideline site on the Alfred Health Intranet.