Depigmenting and Bleaching Agents:
Coping with Hyperpigmentation
ANDREAS D. KATSAMBAS, MD
ALEXANDER J. STRATIGOS, MD
S
ince the introduction of hydroquinone as a skinlightening agent in 1961, several products with
bleaching properties have been used for the treatment of pigmentary disorders of the skin.1 The most
important medical indications for the use of these
agents are melasma and postinflammatory hyperpigmentation, although they have also been used as alternative options for the treatment of ephelides, solar lentigenes, nevi, and lentigo maligna. This article reviews
the most commonly used bleaching agents, discusses
their mechanism of action, and focuses on their efficacy
and safety in treating unwanted skin pigmentation.
Based on our current knowledge, the ideal bleaching
agent has to fulfill certain pharmacologic criteria. It
should have a potent bleaching effect with a rapid time
of onset (less than 2 to 3 months), carry no short- or
long-term side effects, and lead to a permanent removal
of undesired pigment. Most of the currently available
bleaching or depigmenting agents cause a temporary
removal of hyperpigmentation, which usually recurs
after discontinuation of therapy. Presently, there are
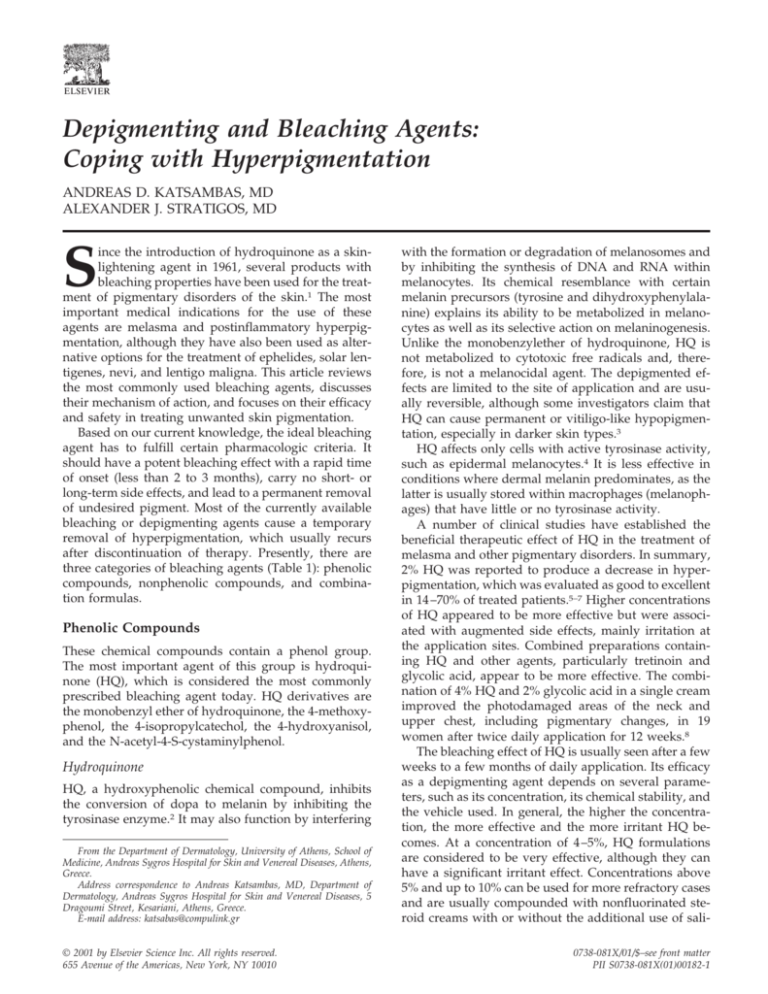
three categories of bleaching agents (Table 1): phenolic
compounds, nonphenolic compounds, and combination formulas.
Phenolic Compounds
These chemical compounds contain a phenol group.
The most important agent of this group is hydroquinone (HQ), which is considered the most commonly
prescribed bleaching agent today. HQ derivatives are
the monobenzyl ether of hydroquinone, the 4-methoxyphenol, the 4-isopropylcatechol, the 4-hydroxyanisol,
and the N-acetyl-4-S-cystaminylphenol.
Hydroquinone
HQ, a hydroxyphenolic chemical compound, inhibits
the conversion of dopa to melanin by inhibiting the
tyrosinase enzyme.2 It may also function by interfering
From the Department of Dermatology, University of Athens, School of
Medicine, Andreas Sygros Hospital for Skin and Venereal Diseases, Athens,
Greece.
Address correspondence to Andreas Katsambas, MD, Department of
Dermatology, Andreas Sygros Hospital for Skin and Venereal Diseases, 5
Dragoumi Street, Kesariani, Athens, Greece.
E-mail address: katsabas@compulink.gr
© 2001 by Elsevier Science Inc. All rights reserved.
655 Avenue of the Americas, New York, NY 10010
with the formation or degradation of melanosomes and
by inhibiting the synthesis of DNA and RNA within
melanocytes. Its chemical resemblance with certain
melanin precursors (tyrosine and dihydroxyphenylalanine) explains its ability to be metabolized in melanocytes as well as its selective action on melaninogenesis.
Unlike the monobenzylether of hydroquinone, HQ is
not metabolized to cytotoxic free radicals and, therefore, is not a melanocidal agent. The depigmented effects are limited to the site of application and are usually reversible, although some investigators claim that
HQ can cause permanent or vitiligo-like hypopigmentation, especially in darker skin types.3
HQ affects only cells with active tyrosinase activity,
such as epidermal melanocytes.4 It is less effective in
conditions where dermal melanin predominates, as the
latter is usually stored within macrophages (melanophages) that have little or no tyrosinase activity.
A number of clinical studies have established the
beneficial therapeutic effect of HQ in the treatment of
melasma and other pigmentary disorders. In summary,
2% HQ was reported to produce a decrease in hyperpigmentation, which was evaluated as good to excellent
in 14 –70% of treated patients.5–7 Higher concentrations
of HQ appeared to be more effective but were associated with augmented side effects, mainly irritation at
the application sites. Combined preparations containing HQ and other agents, particularly tretinoin and
glycolic acid, appear to be more effective. The combination of 4% HQ and 2% glycolic acid in a single cream
improved the photodamaged areas of the neck and
upper chest, including pigmentary changes, in 19
women after twice daily application for 12 weeks.8
The bleaching effect of HQ is usually seen after a few
weeks to a few months of daily application. Its efficacy
as a depigmenting agent depends on several parameters, such as its concentration, its chemical stability, and
the vehicle used. In general, the higher the concentration, the more effective and the more irritant HQ becomes. At a concentration of 4 –5%, HQ formulations
are considered to be very effective, although they can
have a significant irritant effect. Concentrations above
5% and up to 10% can be used for more refractory cases
and are usually compounded with nonfluorinated steroid creams with or without the additional use of sali0738-081X/01/$–see front matter
PII S0738-081X(01)00182-1
Clinics in Dermatology
484 KATSAMBAS ET AL.
Table 1.
Y
2001;19:483– 488
Main Categories of Bleaching or Depigmenting Agents
Phenolic compounds
Nonphenolic compounds
Hydroquinone
Monobenzyl ether of hydroquinone
4-methoxyphenol
4-isopropylcatechol
N-acetyl-4-S-cystaminylphenol
Azelaic acid
Tretinoin
L-ascorbic acid
Kojic acid
N-acetylcystein
cilic acid or tretinoin.9 Most commercially available
formulations in Europe contain 2% of HQ, which is
considered safe and effective. Many dermatologists,
however, may choose to begin treatment with higher
HQ concentrations and use a 2% concentration as maintenance therapy.
A number of different vehicles can be used for HQ
formulations, although several clinical studies have
suggested a hydroalcoholic vehicle as more suitable,
e.g., equal parts of propylene glycol and absolute ethanol.10 The addition of antioxidants, such as ascorbic
acid or sodium bisulphate, enhances the stability of
hydroquinone as it can be easily oxidized— even in a
tube or bottle—and become ineffective.
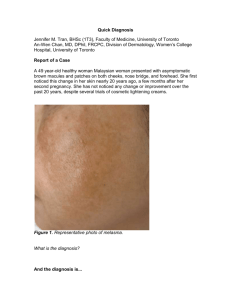
The side effects of hydroquinone can be categorized
as acute and chronic. Acute side effects include allergic
and irritant contact dermatitis, nail discoloration, and
postinflammatory hyperpigmentation.11 High concentrations of HQ (above 5 to 6%) have been associated
with persistent hypopigmentation or depigmentation, a
condition that has been termed “leukoderma en confetti.” Exogenous ochronosis is the most important chronic
side effect of HQ. It presents in the form of reticulated,
ripplelike, sooty pigmentation affecting common sites
of HQ application, such as the cheeks, the forehead, and
the periorbital areas. Histologically these lesions show
banana-shaped yellow-brown pigment globules in and
around collagen bundles in conjuction with giant cells
and melanophage-containing granulomas in the upper
dermis.12 These pigmentary changes are irreversible
and there is no effective treatment. The cause of ochronosis is unknown, but there is a strong correlation
between the occurrence of this condition and the duration of HQ application. In an epidemiological study that
was conducted in South Africa, there were no cases of
exogenous ochronosis observed after application duration of less than 6 months, whereas there was an incidence rate of 92% in individuals who used the product
for more than 16 years.13 These data have raised concern about the long-term safety of HQ, especially in the
context of chronic unsupervised use of over-thecounter, high-concentration products. Even the 2% concentration of HQ contained in most commercially available formulations may carry a small, yet considerable
risk of this irreversible exogenous pigmentation. For
these reasons, the use of HQ has been banned in Japan
Combination
formulas
Kligman’s formula
Pathak’s formula
Westerhof’s formula
and has been severely restricted in South Africa and
Europe.
Contraindications of HQ use include a proven allergy to the agent and past therapeutic resistance. It is
not known whether the drug is able to pass the placenta
and, thus, most physicians do not recommend the use
of HQ during pregnancy or lactation.
Monobenzyl Ether of Hydroquinone
The monobenzyl ether of hydroquinone (MBEH), also
known as monobenzone, has a similar mechanism of
action to HQ on pigmented cells. Moreover, MBEH is
subjected to selective uptake by melanocytes and is
metabolized into reactive free radicals that are capable
of permanently destroying melanocytes.14 This explains
why MBEH causes permanent depigmentation, even
after discontinuation of its use. Interestingly, the loss of
pigmentation is also observed at sites distant to the site
of MBEH application. For this reason, MBEH is primarily used an agent for generalized depigmentation in
patients with extensive vitiligo. The process of depigmentation is long and may require 9 to 12 months of
daily application to achieve total depigmentation.15
Mild irritation usually occurs during application.
Other Phenolic Compounds
Additional phenol compounds are now used in many
countries; for example 4-methoxyphenol, which is usually applied as a 20% cream for the depigmentation of
vitiligo universalis and has a similar mechanism of
action to MBEH.16 4-isopropylcatechol and 4-hydroxyanisole are cytotoxic to pigmented cells and show variable results in the treatment of pigmented disorders.17
Recently, a combination product of 2% 4-hydroxyanisole (Mequinol) and 0.01% tretinoin was tested in a
double-blind multicenter study and was found to improve significantly the solar lentigenes and related hyperpigmented lesions of the face and hands after a
twice-daily application of up to 24 weeks.18 Finally,
N-acetyl-4-S-cystaminylphenol is a phenolic-thio-ether
that acts as a substrate for tyrosinase and selectively
targets cells with active melanin synthesis. It is much
more stable and less irritant than hydroquinone. In a
study of 12 patients with melasma, N-acetyl-4-S-cystaminylphenol produced marked improvement or complete clearing with minimal side effects in 75% of cas-
Clinics in Dermatology
Y
2001;19:483– 488DEPIGMENTING AND BLEACHING AGENTS: COPING WITH HYPERPIGMENTATION 485
es.19 The long-term side effects of the above compounds
are unknown, largely because of the limited experience
in their use.
B Nonphenolic Compounds
Azelaic Acid
Azelaic acid (AZA) is a naturally occurring 9-carbon
dicarboxylic acid that was isolated recently from cultures of Pityrosporum ovale and was associated with
the hypomelanosis seen in tinea versicolor.20 It has been
shown to have beneficial therapeutic effects in acne
vulgaris and certain pigmentary disorders, such as
melasma and lentigo maligna. AZA interferes with the
function of tyrosinase in vitro and may also inhibit
DNA synthesis and mitochondrial oxidoreductase.21 It
does not appear to affect normal melanocytes, and
treatment of constitutively pigmented normal skin,
freckles, lentigenes, and nevi with AZA did not produce a significant therapeutic result.22 The drug, however, appears to exert an antiproliferative and cytoxic
effect on hyperactive and abnormal melanocytes and
may halt the progression of lentigo maligna to lentigo
maligna melanoma.23,24
AZA has been used at concentrations of 15–20% for
the treatment of melasma and postinflammatory hyperpigmentation.25 In double-blind comparative studies,
topical AZA achieved a good-to-excellent response in
60 –70% of melasma patients, and was found to be more
effective than 2% HQ and of equivalent efficacy to 4%
HQ.7,26 A combination regimen of AZA with topical
tretinoin 0.05% for the treatment of melasma produced
similar results after 6 months compared with AZA
monotherapy (approximately 73% of good-to-excellent
improvement), although the addition of tretinoin was
associated with an earlier and more pronounced lightening of melasma pigmentation and a greater percentage reduction of lesion size during the early phase of
treatment.27 These results suggest that tretinoin augments the efficacy of AZA.
In another clinical study, the addition of 15–20%
glycolic acid lotion to AZA cream 20% was as effective
as 4% HQ cream for the treatment of facial hyperpigmentation in darker-skinned individuals.28
At the usual concentrations, AZA is well tolerated in
humans. Adverse reactions such as pruritus, transient
erythema, scaling, and irritation are usually mild and
subside within 2 to 4 weeks.22 Allergic sensitization and
phototoxic reactions can occur, but are rare. No systemic toxicity has been reported.
Tretinoin
The use of tretinoin for the treatment of cutaneous
hyperpigmentation was introduced by Kligman in 1975,
stemming from his observation that acne patients receiving tretinoin developed lighter skin after months of
treatment.29 Tretinoin has been shown in vitro to inhibit
both constitutive and induced melanin formation in
melanoma cell lines.30 In vivo, tretinoin enhances the
epidermal cell turnover, decreasing the contact time
between keratinocytes and melanocytes and promoting
the rapid loss of pigment through epidermopoesis.
Tretinoin has been used in concentrations from
0.025– 0.1% to treat a variety of pigmentary disorders.
The bleaching action is usually very protracted and
occurs anywhere within 12 to 44 weeks of continuous
daily application. Comparative studies in melasma patients have shown a 68 –73% degree of improvement by
tretinoin at 40 weeks of treatment compared with a
control group.31,32 Moderate cutaneous side effects,
such as erythema and desquamation, are observed in
the majority of patients, and in some cases a more
severe dermatitis as well as distressing hyperpigmentation have been reported.33 When prescribing tretinoin, the use of sunscreen is rather important to counteract the possibility of sunburn and photo damage.
L-ascorbic Acid
Vitamin C, or L-ascorbic acid (AsA), interferes with
pigment production at various oxidative steps of melanin synthesis, for example 5,6 dihydroxyindole oxidation.34 AsA has a reducing effect on o-quinones and
oxidized melanin and it can alter melanin from jet black
to light tan. A disadvantage of AsA is its chemical
instability in aqueous solution where it becomes
quickly oxidized and denatures. AsA esters have been
tested in an effort to overcome this problem. A stable
derivative of AsA, magnesium L-ascorbyl-2-phosphate
(VC-PMG), was used in a 10% cream base and produced a significant lightening effect in 19 of 34 patients
with melasma after 3 months of twice daily application.35
Kojic Acid
Kojic acid (5-hydroxy-2-hydroxymethyl-4-H-pyran-4one) is a fungal metabolic product that is structurally
related to maltol. It is a potent tyrosinase inhibitor and
functions by chelating copper at the active site of the
enzyme. It also acts as an antioxidant and prevents the
conversion of the o-quinones of DL-DOPA, norepinephrine, and dopamine to their corresponding melanin.36,37
Kojic acid is used in a 1– 4% cream base, alone or in
combination with tretinoin, hydroquinone, and/or a
corticosteroid. It appears to act synergistically with glycolic acid. The addition of 2% kojic acid in a gel containing 10% glycolic acid and 2% HQ was superior to
the same gel without kojic acid in improving the epidermal melasma of 40 women after 12 weeks of treatment.38 Compared with 2% HQ, kojic acid alone appears to be less effective. There are scant data from the
literature with regard to its long-term side effects, al-
Clinics in Dermatology
486 KATSAMBAS ET AL.
Table 2.
2001;19:483– 488
Westerhof’s Formula
Bleaching Formulas
Name of
formula
Y
Active ingredients
Kligman’s formula Hydroquinone 5%
Tretinoin 0.05–0.1%
Dexamethasone or betamethasone valearate 0.1%
In Hydro-alcoholic base cream or ointment base
Pathak’s formula
2% HQ
Tretinoin 0.05–0.1%
In Hydro-alcoholic base cream or ointment base
Westhorf’s
N-acetylcysteine 3%
formula
HQ 2%
Hydrocortisone 1%
In Ointment base
though some investigators have reported a high frequency of contact sensitivity to this product.39
Combination Formulas
The above agents have been used in combination formulas with the purpose of augmenting the efficacy of
each of these separate active ingredients, of shortening
the duration of therapy and of reducing the risk of
adverse effects. In general, combination therapies have
a more effective bleaching effect than monotherapies
and most physicians commence treatment with one of
these formulas applied once daily (at night) and continue with 2% HQ treatment for maintenance. The most
commonly used combination formulas are listed in Table 2.
Kligman’s Formula
Kligman and Willis used a combination regimen of 5%
HQ, 0.1% tretinoin, and 0.1% dexamethasone in a hydrophilic ointment and demonstrated an efficacy in the
treatment of melasma, ephelides, and postinflammatory hyperpigmentation.29 In this formula, tretinoin
functions as an irritant to facilitate epidermal penetration of HQ, and it also plays an antioxidative role to
prevent oxidation of HQ. Dexamethasone, on the other
hand, is used to decrease the irritation caused by HQ or
tretinoin and to inhibit melanin synthesis by decreasing
cellular metabolic activity. Depigmentation occurs rapidly beginning within 3 weeks after twice-daily application of the formula and maximizing in 5 to 7 weeks.
Pathak’s Formula
Pathak and colleagues conducted a clinical trial of this
formula on 300 Hispanic women with melasma and
showed superior results with creams or lotions that
contained 2% HQ and 0.05– 0.1% tretinoin.5 The authors
suggested that topical steroids are not necessary to
achieve rapid clearance and that they should be preserved for patients who suffer irritation from tretinoin
or HQ.
The combination of 4.7% N-acetylcystein (NAC), 2%
HQ, and 0.1% triamcinolone acetonide improved
melasma after 4 to 8 weeks of application in a left–right,
placebo-controlled clinical study of 12 female patients.40
The bleaching effect of NAC probably relates to the
increase of intracellular glutathion that stimulates
pheomelanin rather than eumelanin synthesis after
binding with dopaquinone, clinically producing a
lighter pigment. As sulfur-containing moeties, NAC
and glutathion exert an inhibitory effect on tyrosinase,
which may also account for their bleaching properties.
There are several variations of the above combination formulas that pertain to the concentration of the
different ingredients and the type of topical steroid. For
example, the use of a lower concentration of tretinoin
(0.05%) and the substitution of dexamethasone with 1%
hydrocortisone acetate or 0.1% betamethasone valerate
in Kligman’s formula reduces the tretinoin-induced irritation and diminishes the risk of steroid side effects
that are often seen with fluorinated steroids, e.g., telangiectasia, atrophy, or hypertrichosis.41
Basic Principles of Bleaching Therapy
Pretreatment Considerations
Before initiating therapy with bleaching agents, physicians should inform patients that the treatment is directed toward improving pigmentation rather than resolving its cause. Patients should also be instructed that
the results will not be permanent and that, despite
initial improvement, recurrence of the hyperpigmentation can occur after a period of time. In this case, the
bleaching treatment may need to be repeated in the
future. It is also important to define the nature and
anatomic localization of the pigmentary process before
starting patients on bleaching therapy. Melasma and
postinflammatory hyperpigmentation may occur in the
epidermis, dermis, or both. The Wood’s light examination can help locate the site of pigmentation, as it intensifies epidermal pigment but not dermal pigment.
However, it is not always a reliable method, particularly in black skin where the differentiation between
epidermal and dermal pigment can be rather difficult.
The most reliable method is a skin biopsy, which determines histologically the cause of the pigment disorder and the depth of melanin deposition. The latter is
probably the most important factor in determining therapeutic responses to bleaching therapy. Epidermal pigmentation as well as certain types of mixed dermal/
epidermal pigmentation respond favorably to topical
bleaching therapy, while dermal pigmentation is usually resistant to depigmented agents and requires other
therapeutic options, e.g., lasers or camouphlage.
Clinics in Dermatology
Y
2001;19:483– 488DEPIGMENTING AND BLEACHING AGENTS: COPING WITH HYPERPIGMENTATION 487
General Measures
References
The success of topical bleaching therapy largely depends on patient compliance and the avoidance of factors that can provoke cutaneous hyperpigmentation.
The avoidance of sun exposure is essential to prevent
the stimulatory effect of ultraviolet light on melaninogenesis. Sun protection can be achieved using appropriate clothing as well as a potent sun block with a sun
protection factor (SPF) of at least 15 to 30. Sunscreen
application should be continued even after the cessation
of therapy and/or the disappearance of skin pigmentation due to the risk of pigment recurrence.
The role of sex hormones such as estrogens and
progesterone in the pathogenesis of melasma has been
well established. There is no consensus, however, of
whether oral contraceptives should be discontinued,
mainly because of the lack of strong evidence that stopping them or changing to a lower concentration contraceptive regimen will significantly alter the clinical outcome of melasma.
In patients with postinflammatory hyperpigmentation, topical steroids represent important adjuncts of
the therapeutic regimen. They are used to treat the
underlying inflammatory reaction. Hydrocortisone, triamcinolone acetonide, or betamethasone valerate are
the most widely used corticosteroids that can be prescribed alone or in combination bleaching formulas.
1. Spencer MC. Hydroquinone bleaching. Arch Dermatol
1961;84:131– 4.
2. Palumb A, d’Ischia M, Misuraca G, Prota G. Mechanism
of inhibition of melaninogenesis by hydroquinone. Biochem Biophys Acra 1991;1073:85–90.
3. Fisher AA. Leukoderma from bleaching creams containing 2% hydroquinone. Contact Dermatitis 1982;8:272–3.
4. Jimbow K, Obata H, Pathak MA, Fitzpatrick TB. Mechanism of depigmentation by hydroquinone. J Invest Dermatol 1974;62:436 – 49.
5. Pathak MA, Fitzpatrick TB, Kraus EW. Usefulness of retinoic acid in the treatment of melasma. J Am Acad Dermatol 1986;15:894 –9.
6. Glenn M, Grimes PE, Pitt E, et al. Evaluation of clinical
and light microscopic effects of various concentrations of
hydroquinone. Clin Res 1991 (abstract);39:83A.
7. Verallo-Rowell VM, Verallo V, Graupe K, et al. Double
blind comparison of azelaic acid and hydroquinone in the
treatment of melasma. Acta Dermatol Venereol (Stockh)
1989;143:58 – 61.
8. Gladstone HB, Nguyen SL, Williams R, et al. Efficacy of
hydroquinone cream (USP 4%) used alone or in combination with salicylic acid peels in improving photodamage
on the neck and upper chest. Dermatol Surg 2000;26:
333–7.
9. Grimes PE. Melasma. Etiologic and therapeutic considerations. Arch Dermatol 1995;131:1453–7.
10. Sanchez JL, Vazques M. A hydroquinone solution in the
treatment of melasma. Int J Dermatol 1982;21:55– 8.
11. Engasser PE, Maibach HI. Cosmetics and dermatology:
Bleaching creams. J AM Acad Dermatol 1981;5:143–7.
12. Snider RI, Thiers BH. Exogenous ochronosis. J Am Acad
Dermatol 1993;28:662– 4.
13. Findley GH, Morrison JGL, Simon IW. Exogenous ochronosis and pigmented millium from hydroquinone bleaching creams. Br J Dermatol 1975;93:613–22.
14. Frenk E, Ott F. Evaluation of the toxicity of the monoethyl
ether of hydroquinone for mammalian melanocytes and
melanoma cells. J Invest Dermatol 1971;56:287–93.
15. Mosher DB, Parrish JA, Fitzpatrick TB. Monobenzylether
of hydroquinone. Br J Dermatol 1977;9:669 –79.
16. Njoo MD, Vodegel RM, Westerhof W. Depigmentation
therapy in vitiligo universalis with topical methoxyphenol and the Q-switched ruby laser. J Am Acad Dermatol
2000;42:760 –9.
17. Bleehen SS. The treatment of hypermelanosis with 4-isopropylcatechol. Br J Dermatol 1976;94:687–94.
18. Fleischer AB, Schwartzel EH, Colby SI, Altman DJ. The
combination of 2% 4-hydroxyanisole (Mequinol) and
0.01% tretinoin is effective in improving the appearance of
solar lentigines and related hyperpigmented lesions in
two phase double-blind multicenter clinical studies. J Am
Acad Dermatol 2000;42:459 – 67.
19. Jimbow K. N-acetyl-4-S-cystaminylphenol as new type of
depigmenting agent for the melanoderma of patients with
melasma. Arch Dermatol 1991;127:1528 – 4.
20. Nazzaro-Porro M. Azelaic acid. J Am Acad Dermatol
1987;17:1033– 41.
21. Schallreuter KU, Wood JM. Azelaic acid as a competitive
Duration of Therapy
Because of the risk of exogenous ochronosis, any
bleaching product should be used for no longer than 2
years. If there is no improvement after 6 months of
application, the use of bleaching agents should be
stopped and alternative modalities should be pursued.
Combined Use with Chemical Peeling
Bleaching agents can be combined with superficial or
medium-depth chemical peels, such as 50 –70% glycolic
acid or 30% trichloroacetic acid peels. HQ or a combined regimen of HQ, tretinoin, and a topical corticosteroid can be used before and/or after a chemical peel
to augment the therapeutic response and decrease the
risk of postinflammatory hyperpigmentation that is frequently seen in melasma patients.42
Conclusions
A fair number of bleaching agents is presently available
to treat hyperpigmentation disorders. Although beneficial for many patients, the majority of these medicaments do not permanently eliminate the abnormal
pigmentation and are frequently associated with significant side effects. Each patient should be assessed individually and a risk/benefit ratio should be established
for each therapeutic approach.
Clinics in Dermatology
488 KATSAMBAS ET AL.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
inhibitor of thioredoxin reductase in human melanoma
cells. Cancer Lett 1987;36:297–305.
Robins EJ, Breathnach AS, Bennet D, et al. Ultrastructural
observations on the effect of azelaic acid on normal human melanocytes and human melanoma cells. Br J Dermatol 1985;113:687–97.
Fitton A, Goa KL. Azelaic acid. Drugs 1991;41:780 –98.
Nazzaro-Porro M, Passi S, Balus L, et al. Effect of dicarboxylic acids on lentigo maligna. J Invest Dermatol 1979;
72:296 –305.
Breathnach AS, Nazzaro-Porro M, Passi S, Zina G. Azelaic
acid therapy in disorders of hyperpigmentation. Clin Dermatol 1989;7:106 –19.
Balina LM, Graupe K. The treatment of melasma 20%
azelaic acid versus 4% hydroquinone cream. Int J Dermatol 1991;30:893–5.
Verallo-Rowell VM, Verallo V, Zaumseil RP, Graupe K.
Combined use of 20% azelaic acid cream and 0.05% tretinoin in topical treatment of melasma. J Dermatol Treat
1996;7:235–7.
Kakita LS, Lowe NJ. Azelaic acid and glycolic acid combination therapy for facial hyperpigmentation in darkerskinned individuals: A clinical comparison with hydroquinone. Clin Ther 1998;20:960 –70.
Kligman AM, Willis I. A new formula for depigmenting
human skin. Arch Dermatol 1975;111:40 – 8.
Ortonne JP. Retinoic acid and pigment cells: a review of
in-vitro and in-vivo studies. Br J Dermatol 1992;41:43–7.
Griffiths CE, Finkel LT, Ditre CM, et al. Topical tretinoin
(retinoic acid) improves melasma: A vehicle-controlled,
clinical trial. Br J Dermatol 1993;129:415–21.
Kimbrough-Green CK, Griffiths CE, Finkel LJ, et al. Top-
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
Y
2001;19:483– 488
ical retinoic acid (tretinoin) for melasma in black patients.
Arch Dermatol 1994;130:727–33.
Tadaki T, Watanabe M, Kumasaki K, et al. The effect of
topical tretinoin on the photodamaged skin of the Japanese. Tohoku J Exp Med. 1993;169:131–9.
Tomita Y, Hariu A, Mizuno C, Seiji M. Inactivation of
tyrosinase by dopa. J Invest Dermatol 1980;75:379 – 82.
Kameyama K, Sakai C, Kondoh S, et al. Inhibitory effect of
magnesium L-ascorbyl-2-phosphate (VC-PMG) on melanogenesis in vitro and in vivo. J Am Acad Dermatol
1996;34:29 –33.
Niwa Y, Akamatsu H. Kojic acid scavenges free radicals
while potentiating leukocyte functions including free radical generation. Inflammation 1991;15:303–15.
Kahn V. Effect of kojic acid on the oxidation of DL-DOPA,
norepinephrine, and dopamine by mushroom tyrosinase.
Pigment Cell Res 1995;8:234 – 40.
Lim JT. Treatment of melasma using kojic acid in a gel
containing hydroquinone and glycolic acid. Dermatol
Surg 1999;25:282– 84.
Nakagawa M, Kawai K, Kawai K. Contact allergy to kojic
acid in skin care products. Contact Dermatitis 1995;32:9 –
13.
Westerhof W, Njoo MD. Bleaching agents. In: Katsambas
AD, Lotti TM, editors. European handbook of dermatological treatments. Berlin: Springer 1999: 766 –77.
Katsambas A, Antoniou C. Melasma. Classification and
treatment. J Eur Acad Dermatol 1995;4:217–23.
Katsambas A. Melasma. A combined treatment with trichloroacetic acid 35% chemical peeling and a hydroquinone treatment scheme. 3rd Congress of the European
Academy of Dermatology and Venereology, 1993:(abstract);230.