Sat_Sportsdrome_1730_Duck PN Presentation update v4
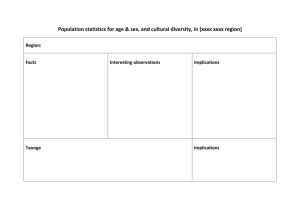
advertisement

Doctors, Nurses ... and pharmacists - why this threesome works. Vanessa Brown Brendan Duck RNZCGP GPCME 2014 What is a clinical pharmacist? Specialist Pharmacist Practitioner Post Graduate education and/or significant clinical experience Undertakes Medicine Review = Medicine Therapy Assessment (MTA) Provides medicine and clinical information services What's different about a Clinical Pharmacist? Focus on risk vs benefits for individual patients for each medicine Applying most recent evidence to specific patient medicine related problems Recommendations on how to implement treatment plan Unbiased assessment of emerging medicine evidence and guideline updates Mrs F.J. 76yr female Her current issues: • Tiredness, cramps + twitchy legs • Constipation, renal function changes • Falling regularly • BP 120/58mmHg Calc CrCl= 21.5mL/min • HbA1c 37mmol/mol Cholesterol levels good • Liver function good Current meds • • • • • • • • Furosemide 80mg mane Amitrip 25mg nocte Ezetrol 10mg daily Aspirin 100mg daily Quinine 300mg BD Simvastatin 40mg nocte Omeprazole 20mg mane Cholecalciferol 1.25mg monthly Recommendations • Change simvastatin 40mg to atorvastatin 10mg • Stop omeprazole • Stop quinine Follow-up • Feeling much better no longer tired. Birth of clinical pharmacist facilitation? $1.06 million year on year increase in combined pharmaceutical budget – CPB = community pharmaceuticals + pharmaceutical cancer treatments + vaccines (from 1 July 2013) Haw kes Bay pharm aceutical expenditure (12 m onth rolling totals) Data source: Pharmac Drug expenditure report for DHB for year ending Sep-10 $36,500,000 $31,500,000 $26,500,000 $21,500,000 $16,500,000 $11,500,000 $6,500,000 $1,500,000 Feb-04 Apr-04 Jun-04 Aug-04 Oct-04 Dec-04 Feb-05 Apr-05 Jun-05 Aug-05 Oct-05 Dec-05 Feb-06 Apr-06 Jun-06 Aug-06 Oct-06 Dec-06 Feb-07 Apr-07 Jun-07 Aug-07 Oct-07 Dec-07 Feb-08 Apr-08 Jun-08 Aug-08 Oct-08 Dec-08 Feb-09 Apr-09 Jun-09 Aug-09 Oct-09 Dec-09 Feb-10 Apr-10 Jun-10 Aug-10 Not sustainable No ‘low hanging fruit’ ‘Unmet need’ 12 months to Aging Population Items Dispensed per Capita by Age Rate (crude) per 1000 population Comparison of dispensing rates by age group (items), January to December 2010 120000.0 100000.0 80000.0 60000.0 40000.0 20000.0 0.0 0-14 years 15-24 years 25-44 years 45-64 years Haw ke's Bay 65-84 years 85+ years Total (all ages) New Zealand Source: Pharmaceutical Claims Data Mart, Ministry of Health (Extracted: 22/4/2011). Note data subject to change over time. Dr Info The model Clinical pharmacist facilitators (1.5 FTE) Focus on best practice – not cost To complement the population based clinical pharmacist facilitator (1.0 FTE) Proof-of-concept Funded by Hawke’s Bay DHB – working out of Health Hawke’s Bay PHO – in specific practices (0.5 FTE x 3) Aims Interventions targeted at polypharmacy – ≥ 65 years – would not disadvantage Māori, Pacific or NZDep 9/10 Polypharmacy – patient harm / ADRs Improve chronic disease outcomes (CV risk, diabetes) Fulton & Allen 2005 Practice Focuses Patients >65 years residing in Age Related Residential Care (ARRC) facilities Patients who are over 65 years living independently in the community Practice - with high needs population (Māori, Pacific or NZDep 9/10) The Practices TE MATA PEAK PRACTICE GREENDALE FAMILY HEALTH CENTRE TOTARA HEALTH Location Havelock North Taradale Hastings & Flaxmere Targeted population Patients 65 years and over, living in Age Related Residential Care Facility Patients, 65 years and over, living independently in the community Patients with high needs including Māori, Pacific and NZDep 9/10 Enrolled Population 9800 6000 11000 Target Population 1200 7029 175+ Evolution of role Relationship building Initially focus was on patients taking >10 meds Medicines rather than people Development of tools to generate referrals Quality activities Demand for services Practice Nurse Quote “Resource for education of nurses, patients, GPs. Can't imagine not having CP here now as I probably access CP expertise daily…” Totara Health Individual vs Population Focus – Individual reviews = large benefit for individuals ≠ large benefit for high needs population – Focus on population with chronic disease with poor outcomes – Smaller review of medicines treating chronic disease and recommendations to General Practitioner Adherence Number of risk factors for nonadherence per patient 2 22% 3 or more 9% 1 37% 0 32% Mr T.J. Male, 63 year old, Cook Island Māori Labels – ‘Non-compliant’ – ‘Poor diabetes control due to religious beliefs’ Problem – Poor understanding of medication – Strong beliefs in value of nutrition and ‘living off the land’ Mr T.J. Type 2 diabetes Recent admission for heart failure Recent admission for cellulitis Cancellation of cataract surgery – Poorly controlled hypertension and diabetes HbA1c 123 mmol/mol BP 195/110 mmHg LDL 4.5 mmol/L Mr T.J. Intervention – Improve understanding of medicines – Sustained adherence to medicines (BP, Lipid and Diabetes) BP 120/70 mmHg HbA1c 56mmol/mol LDL 2.5 mmol/L No recent HF symptoms – Teaching other about the benefits of medicines Te Mata Peak Practice Primarily Aged Related Residential Care Aims: – Reduction in polypharmacy – Improve medicine safety Medicine reconciliation on admission Medicine Therapy Assessment prior to 3/12 review Medicine quality initiatives Digoxin administration and monitoring Vitamin D Prescribing Medicines and Falls Risk ARC Registered Nurse – how has the CP helped? “Education. Medication Reviews. Input into Best Practice projects. Liaison between GP and facility when required”. Greendale Family Health Focused on ≥ 65 years living at home Medicine therapy assessments Co-ordination of multiple prescribers! Medicine reconciliation Clinical guidelines and standing orders Tools used – Multi-Med Survey Tools Used – S.I.M.P.L.E. Linkages • • • • • • • • Health Hawke’s Bay Care cluster Home services District nurses Local specialists Hospital pharmacists Community pharmacist Allied health; OT, PT, dietitian, social worker Medicine reconciliation Update medical record Required clarification Required a medicine review as multiple issues Other interventions 37% 29% 23% 11% – E.g. advice on syringe driver medicine doses medicine information queries Special Authority number follow up Greendale: 1 December 2012 – 18 January 2013 Benefits to GP High quality unbiased advice Different set of eyes/focus Collaborative decision making Source of information on constantly changing evidence and guidelines Availability of medicine information Coordination of multiple prescribers MOPS audits Benefits to Practice Collaboration to manage chronic disease Increased practice confidence in managing polypharmacy Contribution to quality improvement of the practice Review of medicine policies and standing orders Cornerstone accreditation support Benefits to patients Patient centered approach Different focus, asks different questions Address medicine benefits vs harm Improved outcomes Reduced medicine complexity Coordination of multiple prescribers GP Quote “Initially I had no idea what a clinical pharmacist would do for our practice, now I don’t know how I could live without them.” Cost reduction / avoidance Category 1. Community pharmaceuticals 2. Falls 3. Reduction in BP § Cost $ Number of events Total DHB savings p.a. or per event* Known / estimated* Known / estimated* ¥$500,000 $0 to $47,000 4. Delayed admission to ARRC 5. ED transfer avoided 64 $149,400 *3 *$100,000 $24,000 2 $48,000 $450 *1 *$450 Total ~$800,000 Hawke’s Bay CPB September 2012 to August 2013 Reduction in sBP by 10mmHg (1 each renal failure, myocardial infarction, stroke) ¥ § Hawkes Bay Future Direction Clinical Pharmacist Facilitators add value to general practice 1 FTE per 20,000 patients Ensure access to all areas within DHB At 1 July 2014, HBDHB is rolling out this service Hawke’s Bay wide (8 FTE) We Can Help You Evidence to support clinical pharmacist role Experience of implementation Hawke’s Bay team is happy to put together a proposal Contact: - Billy Allan, Chief Pharmacist, HBDHB William.Allan@hawkesbaydhb.govt.nz - Di Vicary, Health Hawke’s Bay pharmacist@healthhb.co.nz Acknowledgments Di Vicary, Clinical Pharmacist Facilitator Team Leader Billy Allan, Chief Pharmacist Hawke’s Bay DHB Health Hawke’s Bay Greendale Family Health Te Mata Peak Practice Totara Health Any Questions?