Biol1406 Lab Biotechnology
advertisement

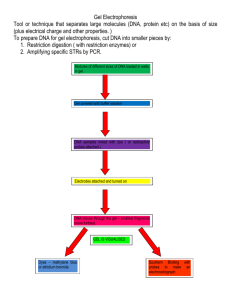
Biol1406 Lab Biotechnology Recombinant DNA In 1970, Hamilton Smith discovered restriction enzymes in bacteria. These enzymes act as scissors, cutting DNA molecules at specific sites. Smith put bacteria and a bacteriophage (virus) together. The bacteria destroyed the viral DNA by cutting it into small pieces; thereby destroying the invading virus. This discovery has led to recombinant DNA technology. To begin, restriction enzymes are placed with DNA so that it can be cut. The DNA is then isolated and polymerase chain reactions (PCR), produces multiple copies of the DNA. The replicated material is then used for study, analyses or recombination. Restriction Endonucleases (Enzymes) By cutting (also termed restricting or digesting) DNA with restriction enzymes or restriction endonucleases, we separate DNA into smaller fragments, restriction fragments. Restriction endonucleases recognize a specific DNA sequence wherever (and however many times) it occurs in a DNA molecule and cuts the DNA at or near that site, each restriction enzyme is named for the species of bacteria from which it was isolated. Digesting DNA requires energy and involves a physical cleavage of chemical bonds. The specific recognition sites are often palindromes; sequences of complimentary DNA that can be read the same backward as forward. In nature, bacteria use restriction enzymes to recognize and metabolize foreign DNA. Bacteria utilize restriction enzymes as a “primitive” immune system. A plasmid is a relatively small extra-chromosomal circular DNA molecule found in bacteria and yeasts. pUC 19, is found in E. coli and one of the most widely used plasmids for cloning due to its size and DNA sequence. Restriction enzymes recognize particular DNA base sequences and cut the DNA at that sequence in a particular pattern (blunt or sticky ends). The illustration below shows the recognition sequence (palindromes) for three restriction enzymes and the pattern they produce. Eco RI G-A-A-T-T-C C-T-T-A-A-G Hha I G-C-G-C C-G-C-G Sma I C-C-C-G-G-G G-G-G-C-C-C Study the DNA sequence below and draw lines through it where each enzyme would cut it producing restriction fragments. Be sure to label which enzyme would make which cut. C-G-G-T-A-A-T-G-C-G-A-A-T-T-C-A-A-G-C-G-C-A-G-A-T-G-C-G-C-G-A-T-C-C-C-G-G-G-G-A-T-A-G-C G-C-C-A-T-T-A-C-G-C-T-T-A-A-G-T-T- C-G-C-G-T-C-T- A-C-G-C-G-C-T-A-G-G-G-C-C-C-C-T-A-T-C- G 1 Biol1406 Lab Biotechnology Gel Electrophoresis/ RFLP Analysis By cutting DNA with restriction enzymes we separate DNA into smaller fragments, restriction fragments. We can then do a comparative analysis on restriction fragments (using the same restriction endonucleases) of DNA from different samples. Due to individuality of DNA, polymorphism (different structure) should exist. By comparing the restriction fragment length polymorphism (RFLP) we can determine the likelihood of whether two pieces of DNA came from the same individual (species) or different individuals (species). We will employ agarose gel electrophoresis as our analytical tool. The DNA molecules will range from 500 to 30,000 base pairs. DNA is negatively charged at neutral pH. The migration rate of the DNA molecules of the same shape through the microscopic pores of the agarose gel is inversely proportional to their size. Therefore, DNA will travel through the gel based on size, charge and shape. In the experiment, DNA fragments of unknown size and Standard (known) DNA fragments will be submitted to electrophoresis. The Standard is a size ladder. Because of variables including preparation of gels, voltage, and individual electrophoresis units, run time, etc; a Standard must be run with each gel of unknowns. The unknowns will travel relative to their sizes and can be compared to the known fragment sizes and the distance they traveled. Following electrophoresis the gel is to be stained for DNA band visualization. Methylene Blue is used for staining the DNA bands. It covalently binds to the DNA (chemical bonding characterized by the sharing of pairs of electrons between atoms of similar electronegativity). Cancer Gene Detection Many contributory factors have been identified to cause the onset of cancers including exposure to certain carcinogens in our diets and environment. Several forms of cancer have familial predispositions. These cancers appear to be linked to inherited mutation of suppressor genes, such as p53. Familial cancers constitute a very small fraction of the total reported cancers and they occur in dominant inherited patterns. Mutations that are directly inherited are referred to as germline mutations. Such mutations can be detected in familial pedigrees. A second type of mutation, known as somatic mutations, does not have direct genetic links and are acquired during the life of the individual. Patterns of typical hereditary and sporadically acquired nonhereditary pedigrees appear in Figure 1. In a germline with an inherited mutation, a single somatic mutation within a suppressor gene will result in the inactivation of both alleles. By contrast, normal inherited suppressor genes, that are free of mutations, will require two sequential mutations to initiate tumors. This model is referred to as the "Two-hit" hypothesis. 2 Biol1406 Lab Biotechnology Background Information Some of the first genes identified include the retinoblastoma (RB) gene, Wilm's’ tumor (WTI), neurofibromatosis type II gene and Li-Fraumeni syndrome (LFS). In Li-Fraumeni syndrome, a notable feature in family pedigrees, include a sarcoma (bone, muscle, vascular cancers) patient and at least two immediate relatives with other cancers before the age of 45, as well as multiple cancers in other family members. This is illustrated in Figure 2. With the advent of molecular biology applications to medicine, gene maps and the chromosomal locations of genes are becoming available as tools for the identification of predisposition for various diseases. The procedures used to obtain such information include DNA isolation and the analysis of point mutations in hot spot areas in cancer-related genes, such as p53. Several methods of analysis for the detection of point mutations in genes include DNA sequencing. The Human genome project has provided information to link to the identification of many various cancers and other diseases to DNA sequence information. This information needs to be handled cautiously to assure confidentiality of patients’ genetic profiles. The study of inherited cancers has given cancer molecular biologists the opportunity to search for genes that are critical in normal cell development and carcinogenesis. At the molecular level, cancer formation is characterized by alterations in both dominant oncogenes and tumor suppressor genes, such as p53. Suppressors are normal cellular proteins that are involved in limiting cell growth. By contrast, oncogenes are involved in promoting the growth of cells. In recent years, the p53 tumor suppressor protein has become the center of many cancer biology studies. Because it appears to be of major significance, there is great impetus to study how this gene functions in normal cells compared to cancer cells. The gene for the p53 protein is located on the short arm of chromosome 17. Wild type (normal) p53 functions as a cell regulator as it is a sequence-specific DNA-binding protein that acts as a transcriptional regulator. Upon introduction of mutations, p53 loses its ability to bind to DNA. By contrast, p53 that have mutations in specific hot spots promote uncontrolled cell growth and therefore function as oncogenes genes with potential to cause cancer). For a tumor suppressor gene such as p53 to play a role in transformation in cancer, both alleles need to be altered, as shown Figure 2. The p53 protein can be divided into three domains. Of interest to us is the central region within the protein where the majority of critical "hot spot" mutations are located. These "hot spots" are sites where mutations are detected in high frequencies. They are between exons 5 through 8 where 95% of the mutations occur. There are five subregions in this region where point mutations are detected in human cancers. Examples of hot spots include codons 165 and 175 in exon 5; 196 and 213 in exon 6; 245 and 248 in exon 7; 273 and 282 in exon 8; all are within the p53 protein. Several of these mutations result in an altered p53 protein conformation. In turn, these changes can result in increased stability of the mutant protein and the ability to bind to the normal p53 protein and inactivate it. It is of interest to note that there are correlations 3 Biol1406 Lab Biotechnology between the mutation and tumor tissue. One such example is the mutation at amino acid 175 which is common in colon carcinoma but is rarely observed in lung carcinoma. The inherited Li-Fraumeni syndrome as it has become to be known is rare. When it does occur it affects young family members and results in high mortality rates. Further analysis showed more than 50% of the affected families had extended phenotypes that included brain, breast cancers and leukemias. Cells in the individuals with LFS have a single wild type p53 allele. Examination of the p53 has shown a correlation to mutations in the protein as described above. Constructing the Family Pedigree A first step in the search and assignment of Li-Fraumeni syndrome is to establish the family pedigree of the patient. The first part of the experiment is based on the information made available as part of a diagnosis by the family physician and the oncologist. The pedigree information that you will develop is for a young woman who is suspected to have the Li-Fraumeni syndrome. Upon monthly breast self-examination, Valerie Brown, age 36, found a small irregular mass. She was concerned because she knew that her mother had a mastectomy when she was in her late thirties. Valerie made an appointment with her physician, who referred her to a specialist at a local cancer center, where she was diagnosed as having breast cancer. As part of the medical work-up, the oncologist had inquired about her family history of cancer. Upon consultation with her mother, Valerie learned that her father and his family appeared to be free of cancer. However, in Valerie's mother's family, several cases of cancer have occurred. With the information given below, chart the family pedigree. • Her mother, Diane, was diagnosed and treated for breast cancer at the age of 39. • Valerie did not know that Diane had a sister, Mabel, who died at age 2 of a brain tumor. • Diane's brother, James underwent surgery, followed by chemotherapy for colon cancer. • Her maternal grandmother, Elsie, died at age 42 from bilateral breast cancer. • Her maternal grandfather, Elmer, was free of cancer and is 88 years old. • Her maternal cousin, Patrick (son of James), died of brain cancer at 14. • Her cousin, Jane, aged 2 who is Patrick's sister was diagnosed with childhood leukemia and subsequently died. • Patrick's two other brothers, Robert, 28 and Curtis, 30, are in good health and free of cancer. • Valerie's sister, Nancy is free of cancer. • Nancy's son, Michael was diagnosed at the age of 3 as having sarcoma. Recently, at the age of 18, he was diagnosed as having osteosarcoma. • Nancy's other son, John, and daughter, Jessica, are free of cancer. 4 Biol1406 Lab Biotechnology Valerie has five children: Justin (16), Sheila (14), Robert (10), Angela (8), and Anthony (6), none of whom show any signs of cancer at this time. She was interested in the p53 diagnostic test to determine if she inherited mutations. The familial pedigree strongly suggests Li-Fraumeni syndrome. In such a case, a secondary diagnostic test is normally conducted. In this scenario, Valerie provides a sample of blood and tumor tissue to conduct DNA analysis for the p53 gene. Normally the procedure is to amplify the gene using polymerase chain reaction. This is followed by one of several methods to detect the presence of a point mutation at the hot spots. In the simulation experiment which follows, Valerie's DNA has already been digested with a restriction enzyme that recognizes the mutant sequence at the simulated hot spot site at nucleotide 165 which is the palindrome CAGCTG. A restriction enzyme was used as a probe to cut the simulated amplified gene for Valerie’s DNA sample, together with a normal control and a set of standard DNA marker fragments. Digestion of the normal amplified DNA will give a characteristic DNA fragment banding pattern. The DNA obtained from blood lymphocyte will give an altered band pattern representing one normal allele and the second which is the mutant. The DNA analysis from the tumor tissue will show only the pattern for the tumor allele. The predigested samples with the control wild type and DNA markers will be separated by agarose gel electrophoresis and stained. 5 Biol1406 Lab Biotechnology Edvotek 6 Biol1406 Lab Biotechnology Procedure 1. An 0.8% agarose gel has been prepared and is being maintained at 55oC 2. Prepare your casting tray, placing it on a work space that will be undisturbed. 3. Pour gel into tray. Fill to the top of the casting tray. 4. Immediately insert a 6 tooth comb into center of casting bed. 5. Allow the gel to cool approximately 20 minutes. 6. Remove the comb by pulling straight up. 7. Set up your electrophoresis chamber. Place the gel tray into the chamber, center and level on platform. DNA is negatively charged, so place your wells nearest the negative electrode (opposites attract- the DNA will be pulled toward the positive charge). Weight with stabilizing bar, Fill the apparatus chamber with prepared buffer (pH 7.8). Make sure the gel is completely submerged. 8. Practice delivering sample to well. Use 35 µl practice solution. The practice solution will become diluted in the buffer and will not affect your experiment. set the micropipette to 35 µl press the button to the first stop immerse into sample once immersed, slowly release the button, drawing sample into the tip position pipette tip into well, without puncturing well deliver the sample by slowly pressing the button to the first stop, continue pressing to the second stop do not release the button remove the pipette from the well; once the tip is removed from the well you may release the button press the eject button to discard tip 9. Judging from the practice dye, adjust amount as necessary (micropipette). 10. Load 35-38µl DNA samples into the wells in consecutive order. Refer to table 1 for identification of DNA samples. 7 Biol1406 Lab Biotechnology Table 1. Electrophoresis Cancer Gene Detection Gel Lane 1 Standard DNA Fragments Loading well Lane 2 Control DNA Loading well Lane 3 Patient Peripheral Blood DNA Loading well Lane 4 Patient Breast Tumor DNA Loading well Lane 5 Patient Normal Breast Tissue DNA Loading well 11. Run the gel Place the cover on apparatus chamber- make sure the tray is level. Check that negative and positive indicators are properly oriented Insert negative (black) and positive (red) inputs. Plug in the power source Check that the current is flowing by identifying bubble curtains at the electrodes. 12. Allow approximately 60-90 minutes for separation to occur. Stop the process when a sample has traveled 1-2 cm from the gel’s edge. At this stage DNA cannot be visualized, but you should see a “lead” band of color called tracking dye. Tracking dye is a small molecule that travels in front of the DNA to indicate distance traveled. 13. Formulate a hypothesis with predicted outcomes. 14. Draw and label a diagram (see Table 1). 15. After electrophoresis, place the agarose gel in a plastic dish. 16. Use one of the two methods for staining your DNA bands. Method 1- Wearing gloves completely submerse the gel with ~ 75 ml diluted Methylene Blue stain. Stain the gel for 5 minutes. Longer than 5 minutes may necessitate extended destaining time. Or Method 2- Wearing gloves, place the blue dye side of the Methylene blue card faces down on the gel. Firmly run your fingers over the entire surface of the card and gel to ensure contact between them. Place an empty boat on top of the gel and card and weight down. Allow stain to sit for 10 minutes. Remove card. If gel appears very light, wet surface with buffer and place card back on gel for 5 minutes. 8 Biol1406 Lab Biotechnology 17. The gel must now be destained. Drain the stain into the appropriately labeled flask. 18. Destain by covering the gel with 37°C distilled water. Warm water is not necessary, but it speeds the process. Water that is too hot will deteriorate the gel. 19. Gently agitate the gel container every few minutes and change the distilled water every ten minutes. The large bands will become visible when the gel is still light blue. Continue to destain until the large bands are sharp and the small bands become visible. 20. Carefully remove the gel from the container and place on a paper towel for inspection. References Edvotek 2009. Cancer Gene Detection. The Biotechnology Education Company. Accessed 19 October 2011. http://www.edvotek.com. 9 The Electrocardiogram: Heart Sounds & the Cardiac Cycle Background Structure and Organization of the Heart In lab we have already covered where the heart is located in the body, the structure of the heart regarding blood flow through the heart and the histological composition and organization of the heart wall. If you are not familiar with any of the material listed above, take the time to go back and learn it now. I will not go over any of that material here, but it is the foundation for the material we are covering and you are expected to know it. Conduction System of the Heart When we covered the muscular system in lecture, histology and the heart in the lab, we briefly mentioned that cardiac muscle is autorhythmic. This means the basic rhythm of the contraction of cardiac muscle is set by specialized cells in the myocardium of the heart. It is NOT dependent upon the nervous system. This characteristic is often used by Hollywood to create drama when a character displays the still beating heart of their enemy/victim. Now the while the basic rhythm and the coordination of the contraction of the myocardium is generated by the heart itself, you should already know that the nervous system can modify the rate and force of this contraction. Under the influence of the sympathetic branch of the autonomic nervous system, heart rate and force of contraction can increase. This will lead to elevated blood pressure and more blood to the tissues with higher oxygen demands: the skeletal and cardiac muscle tissues. You have experienced this, yourself, when you have been frightened or are exercising. The opposite effect is created as a result of the parasympathetic branch of the autonomic nervous system. This branch will return your heart rate to normal resulting in lower blood pressure. While both of these branches influence the rate and force of contraction of the heart, the basic rhythm and coordinated contraction of the myocardium are the result of the conduction system of the heart; a network of modified and specialized cardiac muscle fibers. Let’s go through the components of the conduction system and discuss each in turn. The first component of the conduction system of the heart is known as the sinoatrial node (or SA Node). This is a collection of specialized cardiac muscle cells located in the myocardium of the superior, posterior wall of the right atrium just inferior to the orifice of the superior vena cava. While all cardiac muscle is autorhythmic, this collection of cells tends to depolarize at a faster rate than the surrounding cells of the myocardium. As a result, the SA node is responsible for setting the frequency of the contraction of the myocardium. This is why the SA node is commonly referred to as the “pacemaker” of the heart. The SA node will pass this wave of depolarization into the next portion of the conduction system of the heart: the internodal fibers. The internodal fibers, like all of the cells involved in the conduction system of the heart, is modified cardiac muscle fibers located in the myocardium. The intermodal fibers extend from the SA node through the atria to the atrioventricular node (AV node). (The etymology reflects this relationship: “inter” meaning between.) These internodal fibers also extend throughout the myocardium of the atria and aid in spreading the wave of depolarization through the myocardia of both the right and the left atria. This results in the coordinated contraction of both the atria at the same time from the base of the heart towards the apex forcing the blood through the AV valves into the ventricles. The internodal fibers propagate the action potential more rapidly than the surrounding myocardium. As a result, the wave of depolarization will arrive at the atrioventricular node (AV node) before the myocardia of the atria have finished contracting. As a result, the fibers in the AV node propagate the action potential very slowly. The AV node is located in the inferior portion of the interatrial septum just anterior to the coronary sinus. By the time the atria have finished contracting, the wave of depolarization has passed through the AV node and will move into the atrioventricular bundle (AV bundle or bundle of His). From the AV bundle the wave of depolarization will move into the left and right bundle branches traveling down the interventricular septum and up the lateral Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts walls of the ventricles. Unlike the internodal fibers of the atria, the AV bundle and bundle branches do NOT send the wave of depolarization into the surrounding cardiac fibers of the myocardia. (If it did this would result in a wave of contraction from the base of the heart to the apex pushing the blood in the ventricles the wrong direction.) We want the ventricles to contract from the apex towards the base forcing the blood through the semilunar valves into the pulmonary artery and aorta. To ensure the action potential moves into the myocardium in the correct place is the job of the purkinje fibers. These are, once again, modified cardiac muscle fibers. These are also the only fibers that will pass the action potential, or wave of depolarization, into the myocardia of the ventricles ensuring a contraction from the apex of the heart towards the base. When the myocardia of the ventricles is finished contracting, the SA node will once again spontaneously depolarize starting the entire process over again. This occurs approximately 76 times per minute in a resting adult – wow! Pretty cool! Electrocardiogram The combined electrical activity of the myocardial cells produces electrical currents that spread through the body fluids. These electrical currents are large & can be detected by recording electrodes placed on the skin. When this activity is recorded it is called an electrocardiogram (ECG or EKG). (ECG is derived from Latin name and EKG is derived from German. Other than that, there is no difference between the two.) An ECG has five distinct features and these are designated in alphabetical order as P, Q, R, S, & T. This is very convenient for us. Typically these features constitute three “waves”: the P wave, the QRS wave or complex, the T wave. Each of these waves is recorded as a direct result of the electrical activity of the heart. The P wave indicates depolarization of the atria. The QRS complex is the result of both the repolarization of the atria and the depolarization of the ventricles. The T wave is created by repolarization of the ventricles. While an ECG is recording the electrical activity of the heart, we can infer what is happening regarding contraction and relaxation of the atria and ventricles. Before we do that let’s discuss the cardiac cycle in detail. Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts The Cardiac Cycle The cardiac cycle encompasses all of the events associated with one “heart beat” (lub-dub). This includes the contraction of the myocardia of the atria while the myocardia of the ventricles are relaxing followed by the contraction of the myocardia of the ventricles while the myocardia of the atria are relaxing. Contraction of the myocardium is known as systole. Often we want to designate which chambers of the heart are involved. As a result, contraction of the atria is called atrial systole and contraction of the ventricles is called ventricular systole. Relaxation of the myocardium is called diastole. Again we may want to designate atrial diastole or ventricular diastole. When the chambers are not actively contracting they are in diastole. We can correlate the features of the ECG with atrial and ventricular systole. Before we do so, let’s go over the cardiac cycle in detail. Since this is a cyclic event, we need to start somewhere. So we will pick up when both the atria and the ventricles are relaxing (diastole). When the ventricles are ~ 75% full, atrial systole will start (from the base towards the apex) and the ventricles will be filled to capacity. This is followed by ventricular systole (while the atria relax - atrial diastole). Remember, during ventricular systole the wave of contraction will start at the apex and move towards the base. This forces the AV valves to slam shut preventing the blood from back flowing into the atria. At almost the same time, the semilunar valves will be forced open and the blood will flow into the pulmonary artery and the aorta. After the ventricles are finished contracting they will also relax (ventricular diastole). The pressure gradient created by the expanding ventricles will cause blood in the arteries to backflow into the ventricles. To prevent this, the semilunar valves will slam shut. The AV valves will open allowing blood from the atria to move into the ventricles. Viscosity of the blood also plays a role in filling the ventricles. Heart Sounds The sounds typically attributed to the heart are created when the valves in the heart slam shut preventing the backflow of blood. They are described clinically as two sounds: lub and dub. (Some people describe them as lup and dup). The first sound (lub) is created at the beginning of ventricular systole when the AV valves slam shut preventing the backflow of blood from the ventricles into the atria. The second heart sound (dub) is created by the semilunar valves slamming shut at the beginning of ventricular diastole preventing the backflow of blood from the arteries into the ventricles. Ventricular systole is happening in the time between the lub and the dub. Correlating the Cardiac Cycle with the Features of the ECG Even though the ECG only measures and records the electrical activity of the heart, we can infer what is happening regarding the cardiac cycle. The P wave is caused by atrial depolarization and the presence of a P wave indicates that atrial systole has occurred. The QRS complex is the result of both atrial repolarization and ventricular depolarization. If there is a QRS complex, you can infer ventricular systole has occurred. My favorite feature on the ECG is known as the P-Q interval. This is the stretch of the ECG between the P wave and the Q wave when the action potential is moving through the AV node allowing the atrial systole to reach completion before the action potential is passed on to the myocardium of the ventricles! Pretty cool. If you refer to the ECG figure in your Text and look at the top of the figure, you will notice a yellow and a blue bar. These bars indicate ventricular and atrial systole, respectively. When the chambers are not actively contracting they are in diastole. Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts Getting Started Setting up the Computer 1. From your group one student will need to logon to the computer using their VC username and password. They must be someone willing to stay the entire lab period. 2. The iWorx unit should already be hooked to the computer. You will need to turn this on before opening any of the associated software. To turn the box on, flip the switch on the back of the box (on the right hand side). You will know the box is on when the red indicator light on the front of the box lights up. 3. Once you are logged onto the computer you must open the file named “Labscribe” You can find this by going through the computer files. I simply do a file search for the name “Labscribe.” Once you find the file, open it by double clicking on the icon. 3. Allow your lab instructor to get you set up with the software. While waiting, you can finish setting up the volunteer and the equipment. Setting up the Volunteer/Equipment 1. Everyone needs to turn their cell phones off! The signals will interfere with the ECG reading and cause poor results. This is the number one cause of problems in this lab. 2. From your group one student will need to be equipped with ECG leads. Again, they must be willing to stay the entire lab session. 3. Gently place the event marker in the Channel 3 input of the iWorx unit. Do NOT force it. 4. The volunteer should remove all jewelry from their wrists and ankles. 5. Use an alcohol swab to clean and scrub a region of each wrist and the right ankle (that has little or no hair). Let the areas dry. 6. Remove the plastic covering from a disposable electrode and apply the electrode to the scrubbed area on each wrist and the ankle. Leave these electrodes in place until the end of the lab. 7. Attach the AAMI connector on the end of the gray patient cable to the isolated Channel 1 & 2 inputs of the iWorx unit (see below). 8. Snap the lead wires onto the electrodes, such that: The red (+1) lead is attached to the right wrist The black (-1) lead is connected to the left wrist The green (C or ground) lead is connected to the right leg 9. The subject must sit quietly with their hands uncrossed in their lap. If the subject moves, the ECG trace will move off the top or bottom of the screen. If the subject moves any muscles in the arms or upper body, the electromyograms (EMGs) from the muscles will appear on the ECG recording as noise. Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts Exercise 1: The ECG in a Resting Subject Goal: to measure the ECG in a resting individual Procedure 1. Click on the Record button, located on the upper right side of the LabScribe Main window. The signal should begin scrolling across the screen. 2. Click on the Autoscale button at the upper margin of the ECG channel. If the signal on the ECG channel is upside down (the R wave is going down), click on the downward arrow to the left of the channel title and select the Invert function. The trace should now look similar to the one in the figure. If a larger signal is required, the electrodes should be moved from the wrists to the skin just below each clavicle. 3. Have the volunteer open and close their fists, or move their arms across their chest. Notice that the trace moves around the screen and the ECG is distorted. This should exemplify why it is necessary to keep still and relaxed when recording the ECG. 4. When you have a suitable trace, record for a minute or two. 5. Click Stop to halt recording. Data Analysis 1. Using the arrow tabs at the bottom of the trace, scroll through the recording and find a section of data with four to six good ECG cycles in succession. 2. Click the Double Cursor icon so that the two blue vertical lines (cursors) appear over the recording window. Drag the lines to the left and the right of your four to six good cycles. (You can adjust the time display by pressing the Half Display Time, Double Display Time or the Zoom between Cursors buttons on the LabScribe Toolbar [shown below]). 3. Once you have your four to six good cycles between the cursors, click the Analysis button on the toolbar. 4. Look at the Function Table that is above the uppermost channel displayed in the Analysis window. The names of the mathematical functions used in the analysis appear in this table: V2-V1 and T2-T1. We will be using V2-V1 to measure the amplitude (height) of each feature and T2-T1 to measure the time interval between features. Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts 5. Use the mouse to click on and drag the cursors to specific points on the ECG recording to measure the following: R wave amplitude o Place one cursor on the Q wave that preceded the R wave and the second cursor on the peak of the R wave. The value for V2-V1 on the ECG channel is this amplitude. Record the measurement below. Measure and record the amplitudes of two additional R waves. Figure the average amplitude of the R wave. ___________________ _____________________ ___________________ Average R wave amplitude ___________________ P wave amplitude o Place one cursor on the baseline that precedes the P wave and the second cursor on the peak of the P wave. The value for V2-V1 on the ECG channel is this amplitude. Record the measurement below. Measure and record the amplitudes of two additional P waves. Figure the average amplitude of the P wave. ___________________ _____________________ ___________________ Average P wave amplitude ___________________ T wave amplitude o Place one cursor on the baseline that precedes a P wave and the second cursor on the peak of the T wave in the same cycle as the P wave. The value for V2-V1 on the ECG channel is this amplitude. Record the measurement below. Measure and record the amplitudes of two additional T waves. . Figure the average amplitude of the T wave. ___________________ _____________________ ___________________ Average T wave amplitude ___________________ The beat period (the time interval between two adjacent R waves) Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts o Place one cursor on peak of an R wave and the second cursor on the peak of the adjacent R wave in the same cycle as the P wave. The value for T2-T1 on the ECG channel is the beat period. Record the measurement below. Measure and record the amplitudes of two additional beat periods. . Figure the average beat period. ___________________ _____________________ ___________________ Average beat period (seconds/beat) ___________________ Using this number calculate the heart rate of the subject using the following equation: Heart Rate (beats/minute) = 60 seconds/minute # seconds/beat Questions 1. Is the amplitude of each wave (P, QRS, T) always the same in different cardiac cycles? 2. Which wave has the largest amplitude? 3. What is the average resting heart rate of the subject? 4. Would the P waves of different subjects have the same amplitude? The QRS complexes? The T waves? Why? 5. For each subject, would the wave with the largest amplitude be the same for all individuals? 6. Would the heart rate be the same for all individuals? 7. How do you think resting heart rate would be affected by gender, apparent fitness or diet? Exercise 2: Heart Sounds & the ECG Goal: To study the phasing of heart sounds to the ECG. Procedure: 1. Obtain a stethoscope and wash the ear pieces with an alcohol swab to prevent the spread of pathogens. 2. Be sure to place the stethoscope earpieces in the ear such that they are oriented towards the external auditory canal. 3. Place the head of the stethoscope on the left side of the subject’s chest and listen for heart sounds. Move the stethoscope head to different positions until heart sounds are clearly heard. 4. If you have not already done so, go back to the main window by clicking the Main window icon on the toolbar. When you are ready to record, click the Record button. 5. Hold the stethoscope on the subject’s chest in one hand and the event marker in the other hand. Press the event marker when you hear the “lub” or first heart sound, and release it when you hear the “dub” or second heart sound. 6. After recording for 20 seconds, click Stop to halt the recording. Data Analysis 1. Scroll through the recording and find a section of data with four to six exemplary ECG waveforms and consistent responses in succession on the event marker channel. 2. Use the Display Time icons to adjust the Display Time of the Main Window to show at least four complete ECG/heart sounds cycles. 3. Click the Analysis icon to go to the Analysis window. 4. Use the mouse to click on and drag the cursors to measure the following: The R-Lub interval o This is the time interval between the peak of a R wave and the onset of the event mark. The onset of the event mark indicates the occurrence of the first heart sound. Record the value for T2-T1 of either channel. Measure this time interval for two additional channels. Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts ______________ ___________________ ________________ Average R-lub interval ___________________ The T-Dub internal o This is the time interval between the peak of a T wave and the offset of the event marker. The offset of the event marker indicates the occurrence of the second heart sound. Record the value for T2-T1 of either channel. Measure this time interval for two additional channels. ______________ ___________________ ________________ Average T-dub interval ___________________ Questions 1. Why does the lub sound occur around the peak of the R wave? 2. Is the time delay between the R wave and the lub sound always the same? Explain. 3. Why does the dub sound occur around the peak of the T wave? 4. Is the time delay between the T wave and the dub sound always the same? Explain. Prepared by M.E. Janowski-Bell, Ph.D. Modified from iWorx Handouts