Human Pathology (2009) 40, 1112–1121
www.elsevier.com/locate/humpath
Special Section on Telepathology
Virtual microscopy in pathology education
Fred R. Dee MD ⁎
Department of Pathology, Carver College of Medicine, University of Iowa, Iowa City, IA 52242, USA
Received 23 March 2009; accepted 9 April 2009
Keywords:
Virtual microscopy;
Virtual slides;
Pathology education
Summary Technology for acquisition of virtual slides was developed in 1985; however, it was not until
the late 1990s that desktop computers had enough processing speed to commercialize virtual microscopy
and apply the technology to education. By 2000, the progressive decrease in use of traditional microscopy
in medical student education had set the stage for the entry of virtual microscopy into medical schools.
Since that time, it has been successfully implemented into many pathology courses in the United
States and around the world, with surveys indicating that about 50% of pathology courses already have
or expect to implement virtual microscopy. Over the last decade, in addition to an increasing ability to
emulate traditional microscopy, virtual microscopy has allowed educators to take advantage of the
accessibility, efficiency, and pedagogic versatility of the computer and the Internet. The cost of virtual
microscopy in education is now quite reasonable after taking into account replacement cost for
microscopes, maintenance of glass slides, and the fact that 1-dimensional microscope space can be
converted to multiuse computer laboratories or research. Although the current technology for
implementation of virtual microscopy in histopathology education is very good, it could be further
improved upon by better low-power screen resolution and depth of field. Nevertheless, virtual microscopy is beginning to play an increasing role in continuing education, house staff education, and evaluation
of competency in histopathology. As Z-axis viewing (focusing) becomes more efficient, virtual microscopy will also become integrated into education in cytology, hematology, microbiology, and urinalysis.
© 2009 Elsevier Inc. All rights reserved.
1. Introduction
Virtual microscopy is in the process of revolutionizing the
teaching of microscopic pathology. Multiple medical schools
have implemented this novel technology, and virtual
microscopy is being introduced into the continuing educational and self-assessment programs of pathology educational organizations. Virtual microscopy is very attractive to
educators because it nearly perfectly emulates the pan and
zoom features of traditional microscopy, with the added
advantages of the efficiency, accessibility, and versatility of
⁎ 100 Medical Laboratories, University of Iowa, Iowa City, IA 52242,
USA.
E-mail address: fred-dee@uiowa.edu.
0046-8177/$ – see front matter © 2009 Elsevier Inc. All rights reserved.
doi:10.1016/j.humpath.2009.04.010
computer-assisted education. This article aims to provide an
overview of the following: (1) technological development of
virtual microscopy for education, (2) advantages and
disadvantages of virtual microscopy in education, (3)
implementation of virtual microscopy in education (20002008), and (4) future challenges and opportunities for virtual
microscopy in education.
2. Technological development of virtual
microscopy for education
Web-based virtual microscopy requires multiple technical
steps for optimal educational implementation: (1) acquisition
Virtual microscopy in pathology education
of digital information equivalent to hundreds of high power
fields of view; (2) creation a seamless giant montage, called a
virtual slide or whole slide image; (3) converting the virtual
slide into a file format that allows panning in the x-y axis and
zooming from one magnification to another; (4) serving the
virtual slide file (over a network or the Web) in a pan and
zoom viewer; and (5) integrating virtual slides and editors via
databases that facilitate superimposed annotations and
accompanying text.
Early technology for acquisition of multiple microscopic
fields of view (called digital tiles) with a precision motorized
microscope stage and creation of a digital montage (now
called a virtual slide) was initially described in 1985-1993
[1,2]. Then in the late 1990s, when desktop computers had
enough processing speed and RAM to acquire a digital
facsimile of the majority of the information on a glass
slide, virtual slide acquisition technology using digital
tiles was improved upon and commercialized by BacusLabs
(www.bacuslabs.com) and MicroBrightField (www.microbrightfield.com). Another technologic advance in acquisition
of virtual slides came several years later when 2 novel
methods of acquisition that did not rely on creating digital
1113
tiles with a traditional microscope were developed and
commercialized in the United States. Aperio (www.aperio.
com) released a linear scanner that rapidly acquired digital
stripes across the whole slide, and Dmetrix (www.dmetrix.
net/) released an array microscope for rapid simultaneous
digital capture of the whole slide by multiple microlenses [3].
In the late 1990s, simultaneous with the commercialization of virtual slide acquisition solutions, Kodak and others
introduced a multiresolution pyramidal file format called
FlashPix, and Live Picture/MGI developed a FlashPix image
file converter and server to stream virtual slides over the Web
to a pan and zoom viewer [4]. At about the same time,
BacusLabs adapted a method for transmission of digital tiles
over the intranet, which were then assembled into a montage
(called a WebSlide) in a pan and zoom client viewer.
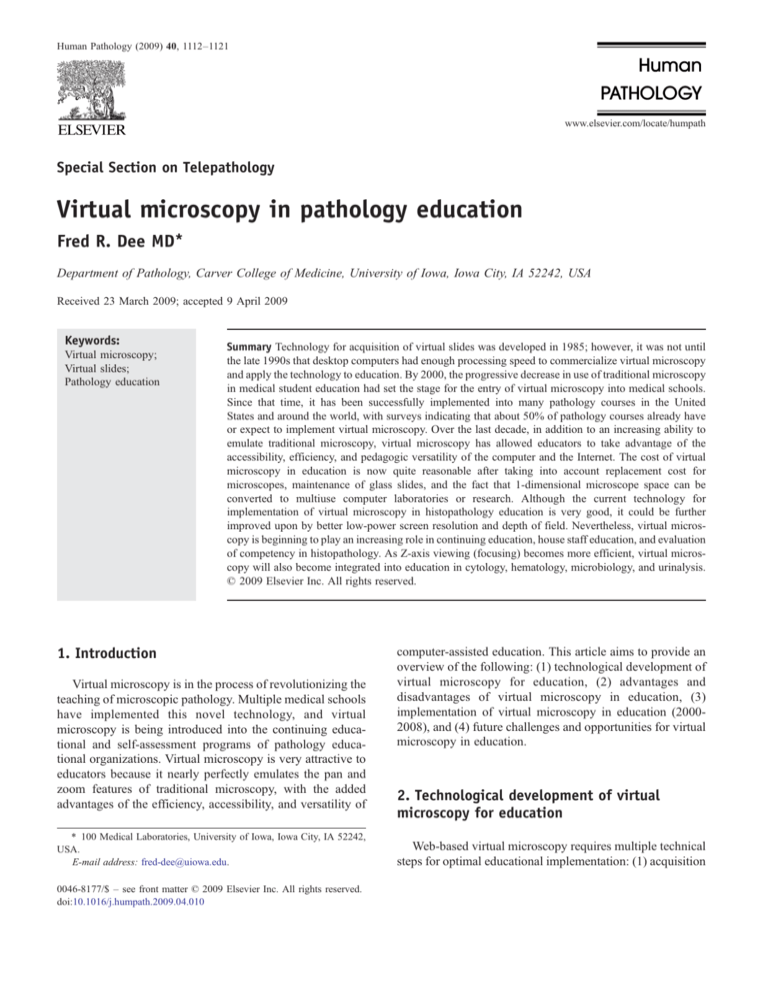
Another major innovation that further increased the
educational value of virtual microscopy came in 2001
when developers began to integrate virtual slides with an
annotator applet in a database structure. This educational
model provided educators the ability to label virtual slides
with arrows, circles, and text labels using overlays. Integration with a database structure also allowed educators to
Fig. 1 This screen shot from the Virtual Slidebox/Human Histopathology Atlas demonstrates text and arrow overlays that are activated by
clicking on annotation buttons and text in the left frame. The entire content of the browser window is dynamically generated via a Perl scripted
MySQL database and editor interface. Note that the location and navigation box (upper right) provides a thumbnail for orientation to the whole
slide. This virtual slide is a fortuitous cut through a bronchus showing transition from normal to invasive carcinoma shown at a traditional
microscope magnification equivalent of ×1.25. Areas of interest can be zoomed to the equivalent of ×20.
1114
F. R. Dee
easily link descriptive text specific to the virtual slide in a
separate browser window, as well as create links to supplemental gross images and normal virtual slides. Some of these
features are illustrated in Fig. 1, which is a screen shot of an
annotated slide in the Virtual Slidebox / Human Histopathology Atlas (www.path.uiowa.edu/virtualslidebox).
Manipulation of an annotator via a scripted database
editor can also be used to provide initially hidden feedback to
trainees via instructor-generated labels after they independently examine the slide or allow trainees to add their own
labels to the virtual slide. These functions are particularly
important in teaching and evaluating locator and identification skills of trainees who will use the traditional microscope
in their future practice.
The standard virtual slide technology described above
does not provide the ability to focus because only 1 focal
plane (in the x-y axis) is acquired. Multiple planes of focus
are not needed for most histopathologic applications in
education; however, as will be pointed out later in this
article, the ability to focus up and down is critical for
education in disciplines such as cytology, hematology,
microbiology, and urinalysis that use smears and liquidbased preparations [5-8]. On these preparations, the cells
Table 1
do not all lay flat on the slide, and in some cases, 3dimentional (3-D) clusters of cells or objects need to be
visualized. Focusing can also occasionally be important in
histologic sections where the depth of focus afforded by
only 1 plane of focus cannot adequately visualize microbes
or other small objects [9]. “Virtual focusing” can be
accomplished by 3-D scanning (also called z-axis scanning), which consists of acquiring the equivalent of 6 or
more virtual slides separated by several microns of focus
perfectly aligned in the z-axis, sometimes called z-stacks.
In the 3-D viewer, panning and focusing are carried out by
jumping from 1 virtual slide focus level in the z-stack to
another using up-down arrows or the mouse roller bar;
simultaneously, each virtual slide level in the z-stack can be
panned in the x-y plane similar to standard virtual slides.
Currently, 3-D scanning of multiple perfectly aligned focal
planes over the whole slide is possible, but is technically
complex and time consuming. In addition, efficient viewing
of 3-D slides, which requires the ability to simultaneously
pan and focus over the whole slide at several magnifications, is much slower than examining a standard virtual
slide, especially over the Web. Unfortunately, 3-D solutions
that have been well evaluated for efficiency of synchronous
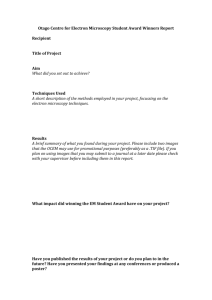
Advantages and disadvantages of virtual microscopy versus traditional microscopy
Advantages
Disadvantages
Accessibility
Access can be anywhere anytime there is a computer (and
the Web) available.
One slide can be viewed by many or duplicated and shared.
Multiple recuts are not needed.
One-of-a-kind slides that cannot be recut can be duplicated
into an unlimited number of copies and shared with others,
eg, the fortuitous cut in Fig. 1.
Efficiency
Focus, proper condenser adjustment, and lighting are not required.
Pedagogic
Trainees do not learn how to use a traditional microscope
if virtual microscopy is used exclusively.
Technology:
Technical competence in viewing is easier to achieve and
less frustrating for trainees who do not have an aptitude for
traditional microscopy.
There is rapid access to the next slide in the slide box.
Pedagogic
Very-low-power overview (≪ ×4) allows trainee to better
visualize relationship of pathologic to normal tissue.
A thumbnail and location box allows trainee to remain oriented
to the whole slide while viewing at high magnification.
Marking x-y and magnification coordinates of multiple key
areas and movement among these areas at the click of the mouse
is possible.
Side-by-side viewing, annotation overlays, and integration with
descriptions, case scenarios, gross and radiological images or digital
photomicrographs is possible.
Group discussion is enhanced as each computer screen can serve as a
multihead microscope.
Cost
Cost may be significantly less depending on the educational venue.
Low magnification has less resolution when viewed on
a standard computer screen.
Refractile objects do not refract well.
Original glass slide tissue artifact and imperfections are
difficult to scan.
Virtual focus acquisition and viewing is inefficient,
especially over the Web.
Virtual microscopy in pathology education
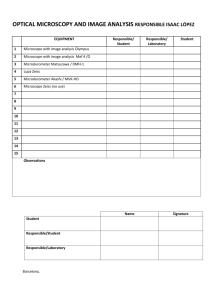
Table 2 Advantages and disadvantages of virtual microscopy
versus digital photomicrographs
Advantages
1115
3. Advantages and disadvantages of virtual
microscopy in education
Disadvantages
Pedagogic
Cost
Ability to pan and zoom.
Cost is significantly more.
Very-low-power overview
Technology
(≪ ×4) allows trainee to
better visualize relationship
of pathologic to normal tissue.
A thumbnail and location box
Transmission speed,
allows trainee to remain
reliability of acquisition
oriented to the whole slide
and serving, and relative
while viewing at high
lack of standards all add
magnification.
complexity to
implementation.
Marking x-y and magnification
coordinates of multiple key
areas and movement among
these areas at the click of the
mouse is possible.
simultaneous panning and focusing (CytoView and a
MicroBrightField solution) are primarily intended for
proficiency testing and research applications, respectively,
and are not being distributed for education [5,6,8]. A recent
report using a Hamamatsu system showed promising
results for educational application, but speed and efficiency
of viewing were not reported [9]. Other vendors (including
BacusLabs and Aperio in the United States) also have 3-D
solutions. Zeiss (www.zeiss.com) has developed a variation
on the above called “extended focus,” in which z-stacks are
acquired as described above. Then, the sharp contrast
details from each focal plane are extracted and collapsed
into a single virtual slide where the best focused detail
derived from each of the multiple focal planes is viewed.
The acquisition and processing are still technically complex
and time consuming, but transmission over the Web is as
fast as with a standard virtual slide (personal observation/
communication). Thus, cells laying on the slide at different
levels are all in focus, and 3-D objects are in focus top to
bottom; however, the sensation of being able to focus
through a 3-D cell cluster or object is missing.
Although early development and implementation were
driven primarily by educators and research applications,
more recent commercial development has been driven by
the potential applications in service pathology. Subsequent
to the early development described above, there has been
an explosion in virtual slide technology in both quality and
quantity. For example, in 2006, it was reported that there
were 31 commercial vendors in the field virtual microscopy
[10]. Scanning and serving of virtual slides are now much
more rapid, of higher quality, of higher resolution, of larger
file size, and more versatile than was even conceivable
when virtual microscopy was first implemented in education in 2000.
Tables 1 and 2 outline the advantages and disadvantages
of virtual microscopy for teaching microscopic pathology,
compared with traditional (real) microscopy and digital
photomicrographs, respectively. The advantages and disadvantages listed are recurrent themes derived from articles
describing implementation of virtual slides in education
(Table 3) and from personal communication among
educators at education and informatics meetings.
3.1. Virtual microscopy versus traditional
(real) microscopy
Because virtual microscopy can nearly perfectly emulate
traditional microscopy, it can be applied to almost any
discipline or educational venue where traditional microscopy
is currently used. Plus, computerization adds the accessibility, efficiency, and pedagogic advantages of virtual
microscopy, which are detailed in Table 1.
The cost of virtual microscopy in medical student
education may be quite comparable with traditional
microscopy. For example, when we at Iowa cost-accounted
virtual microscopy versus traditional microscopy, taking
into account the replacement cost for microscopes,
generation of and maintenance of multiple sets of glass
microscope slides, and the fact that microscope space can
be converted to multiuse computer laboratories or research
space, we estimated that startup costs, including acquisition
equipment and computer software and hardware, could be
recouped. Although the cost for virtual microscopy remains
high, the cost should eventually come down with
innovation and competition among vendors. In addition,
there can be cost sharing as virtual microscopy becomes
integrated into education, clinical service, and research in
the same institution. Finally, for continuing education
Table 3
Venues for virtual microscopy implementation
Education in pathology
3.1 Medical student education
3.1.1 Pathology small group teaching
3.1.2 Histopathology laboratories/large groups
3.1.3 Integrated and problem-based curricula
3.1.4 Repositories for sharing among
institutions
3.2 Cytology
3.3 Hematology
3.4 House staff education and evaluation
3.5 Continuing medical education
3.6 Veterinary pathology and comparative
pathology
3.7 Histology—as a prerequisite for pathology
education
References
[11-13]
[12,16,17]
[15]
[13]
[6,8,18-21]
[7]
[22]
[23-25]
[26-29]
[30-36]
1116
(and competency evaluation), costs saved by not having to
create and mail glass slides can offset acquisition and
serving costs.
3.2. Virtual microscopy versus
digital photomicrographs
Because virtual slides are single (although complex)
giant images, they can be placed on a server with a URL
and thus can be used in Web-based education as you
would a photomicrograph, but with the added pedagogic
advantages detailed in Table 2. Although photomicrographs can be nested to provide the semblance of pan and
zoom, and annotations can be added, these functions are
much more readily performed with virtual slides and
associated annotation editors.
The disadvantages of virtual microscopy versus digital
photomicrographs are primarily cost related. Cost is a
minimum of about $80,000 for scanner, and serving and
viewing software. Cost for serving and viewing software,
with commercial scanning of slide sets at approximately $40/
slide, can be less than $10,000 startup. Compared to teaching
with digital photomicrographs, the transmission speed,
technical complexity, reliability, and relative lack of
standards in the virtual microscopy industry are still
somewhat of an issue, but these have significantly improved
over the last 8 years.
4. Implementation of virtual microscopy in
education 2000-2008
Table 3 lists the variety of educational venues in which
virtual microscopy has been implemented. The references
point to articles describing implementation and evaluation
[6-8,11-36].
4.1. Medical student education in pathology
Results of a small survey of pathology chairs in 2007
showed little difference between the United States Medical
Licensing Examination (USMLE) pathology scores from
institutions with or without microscopes in their curricula
[37]. Based on this finding, the authors suggested that “a
possible conclusion is that the microscope is now irrelevant
for teaching pathology to medical students,” although
indicating that a larger study would be needed to test the
validity of their suggested conclusion. The suggestion in this
article was already preceded by a progressive devaluation of
the microscope in medical student education. Before the
early 1990s, most pathology courses relied on lectures and
laboratories or pathology case–based exercises built around
traditional microscopy [38]. Over the last several decades, a
number of curricular reforms have impacted this old
paradigm [37-41]: (1) decreased time has been allotted for
F. R. Dee
pathology and other basic sciences because of the need to
introduce more student contact to foundations of clinical
practice in the first 2 years of medical school; (2) accrediting
bodies recommended a move away from department-based
didactic teaching with lectures and laboratories toward more
centrally managed integrated curricula, with an emphasis on
problem-based or case-based learning and self-directed
study; (3) traditional microscopy has been progressively
augmented and in some cases replaced by digital photomicrographs because of the efficiency, accessibility, and
flexibility provided by computer-assisted education; (4) there
is a perception that practicing physicians (other than
pathologists) do not need to know how to use a microscope
(especially for histopathology); (5) single-dimensional
microscope laboratories are expensive to maintain and
occupy valuable space that could be used for computer
laboratories or research.
A limited survey of pathology chairs presented at the
Association of Pathology Chairs (APC) meeting in 2007
indicated that only about 45% of medical school curricula
have pathology laboratories or large groups for teaching
histopathology, and only about 18% used glass slides in their
curricula (personal communication from Patricia Thomas).
Another limited survey in 2007 indicated that up to 40% of
medical schools still used traditional microscopes and glass
slides in their teaching of pathology [37]. Combining this
2007 data, and comparing it with 1997 survey data reported
by Kumar et al, suggests that the number of curricula with
pathology laboratories has decreased over the last decade
from 98% to less than 50% and that the use of glass slides has
decreased from 85% in 1997 to about 30% in 2007 [37,38].
This progressive decrease in use of traditional microscopy set the stage for the entry of virtual microscopy into
education of medical students in 2000. Since that time, this
new technology, with its promise to expand on the pedagogic
advantages of traditional microscopy, has been successfully
implemented into many pathology courses in the United
States and around the world. A survey in 2004 indicated
that virtual microscopy in US medical student education
had increased from its inception in 2000 to 22% in 2004
[42]. This survey also indicted that of those course directors
not using virtual microscopy at that time, 50% expected to
implement virtual microscopy within 3 to 5 years. In 2007,
based on a combination of 2 limited surveys presented at
the APC meeting (by PatriciaThomas) and the data from
the Group for Research in Pathology Education (GRIPE;
personal communication), it appears that as of 2007, perhaps
up to 33% of medical schools in the United States had
integrated virtual microscopy into their pathology curricula.
In addition to US medical schools, there is also increasing
international implementation. Personal communication with
several educators outside the United States indicates 4 of
5 medical schools in Switzerland, 4 of 12 medical schools in
Poland, and 3 of 18 medical schools in Australia are using
virtual microscopy in their pathology courses (Kathrin Glatz,
Janusz Szymas, and Rakesh Kumar, respectively).
Virtual microscopy in pathology education
A wide variety of settings can be used to teach histopathology to medical students, ranging from large laboratories (up to 150 or more students), to smaller laboratories or
large groups (15-50 students), to small group settings (6-10
students). Virtual microscopy can be implemented in any of
these educational settings, assuming computer access and
space is available. Weather a medical school decides to
implement virtual microscopy depends on a number of
factors, not the least of which is computer availability.
The following 3 sections discuss several implementations
of virtual microscopy in medical student education.
Although no outcomes research has been done to prove
that the pedagogic advantages of virtual microscopy make it
superior to traditional microscopy or digital photomicrographs for teaching histopathology to medical students, it is
clear that virtual microscopy provides an efficient, accessible, and enjoyable way to do so.
4.1.1. Pathology small group teaching
At Iowa in our second-year pathology course for medical
students, we converted from traditional pathology microscope laboratories to small group teaching (called pathology
case analysis) in the early 1970s. Each week in preparation
for pathology case analysis, students examine 4 microscope
slides with associated patient scenarios and gross and
radiographic images during independent learning time.
Then, during a 2-hour case analysis small group session
(8 students), they present the gross and microscopic
pathology, clinical pathologic correlation, and pathogenesis
to their classmates under the guidance of a pathology faculty
or resident facilitator. Before implementation of virtual
microscopy in case analysis, students had 60 h/wk access to a
laboratory equipped with double-headed microscopes, and
histopathology was presented by the students to the small
group using a microscope equipped with a video camera and
monitor. In 1999, we purchased virtual slide acquisition and
delivery hardware and software and digitized our 67 caseassociated glass slides. In 2000, we implemented the virtual
slides into our pathology case analysis exercises and
integrated them via a database with other case materials
[11,13]. These case analysis materials can be viewed on the
Web (www.path.uiowa.edu/cgi-bin-pub/vs/case_analysis/
cases.cgi). After implementation, students were given the
option of preparing for small group presentation using glass
slides or using virtual microscopy. In the first year of
implementation, use of traditional microscopy by students
decreased to 25% of that in 1999, which was 100%. Over the
next 3 years, the use of traditional microscopy in case
analysis fell to near zero, where it has remained. On
formative evaluations, students indicated that image quality
of virtual slides was nearly equal to that of traditional
microscopy and felt that they learned better using the virtual
slides because of efficiency and accessibility. Facultysubjective evaluations indicated an increase in students'
skill in demonstrating histopathology in small group. In
addition, faculty found the virtual slides very useful in their
1117
own preparation for small group because they could prepare
to facilitate case analysis small group in their office or at
home. There was no change in student scores on pathology
examinations. Over the last 8 years, we have upgraded both
our scanner and our delivery software several times. Our
large single-use microscope room has become a multipurpose laboratory with computers, microscopes, and bench
top space for point of care and venipuncture training. In the
near future, this laboratory will be downsized and moved to
another site, and the large laboratory will be converted to
research space.
4.1.2. Pathology laboratory or large group teaching
Most medical student pathology courses, when microscope slides are used in the curriculum, use a variety of
permutations on the “pathology laboratory” rather than the
pathology case analysis model described above, although
smaller laboratories (sometimes called “large groups”)
frequently have associated cases scenarios.
A very successful incorporation of virtual microscopy was
carried out in 2003 at the University of New South Wales
(UNSW) [12]. Their weekly sessions (45-55 students) use
2 to 3 cases with 4 to 5 microscope slides. In the large group
room, before implementation of virtual microscopy, each
student had a microscope and slides, and the tutor would
supervise the learning process. In 2002, they digitized their
glass slides and added 32 computers (side-by-side with
microscopes) with 2 students per computer. In addition, the
tutor could project the virtual slide and move to key areas of
the slide with premarked coordinates. No other component of
the course was changed. Evaluation of the implementation
indicated most students preferred using virtual slides.
Formative evaluations pointed out that virtual slides were
always in focus, faster to use, and efficient and were
especially appreciated by students with low aptitude for
using traditional microscopy. In addition, everyone sees the
same slide, the computer facilitated more student-to-student
and student-to-faculty interaction, and students could review
at home. They also implemented virtual microscopy into
their progress examinations and found no difference in
performance from previous years using glass slides.
At the other end of the spectrum of large group/pathology
laboratory teaching is a recent report from the Seoul National
University College of Medicine [16]. They implemented
virtual microscopy into a previously traditional pathology
laboratory consisting of 160 students with 3 tutors.
Implementation of virtual microscopy was carried out by
having students download the digitized class slide set and a
viewer on to their personal laptops from the university server.
In the same laboratory setting as before, students used their
laptops. After implementation, students were asked to
compare virtual microscopy with traditional microscopy.
Students (142 respondents) strongly preferred virtual microscopy. Formative evaluations showed a range from 79%
to 98% affirmative responses to each of the following
statements concerning virtual microscopy: “less stressful…
1118
better image quality…less time to find lesions…better for
changing magnification…easier to use...had better focus…
better for group discussion…easier to switch to another
slide…more enjoyable…and better to find artifacts.” Students
also appreciated the ability to review slides at home.
Virtual microscopy was implemented into the annual
Pathobiology of Cancer Workshop laboratories in 2002 [17].
After implementation, students (18 per laboratory) continued
to study a set of glass slides using a traditional doubleheaded microscope; however, the facilitator projected a
virtual slide acquired from the slide being studied by the
students. Although this workshop is for bioscience trainees,
the implementation provides a model for implementation in
medical student laboratories that might use a similar format.
This model allows students to continue to learn from
traditional microscopy, whereas virtual slides are used to
facilitate classroom instruction. The advantage of this model
is that students can more easily find areas of interest on the
glass slide as the instructor points them out on the virtual
slide. It also allows the students to study on the Web outside
of laboratory time.
4.1.3. Virtual microscopy in an integrated curriculum
Integration of pathology with other disciplines can take
a variety of forms, ranging from integration with basic
science courses to integration with introduction to clinical
medicine, or totally integrated with both, and the pathology
teaching can be in a large or small group.
Integration of pathology and histology into a large group
setting using virtual slides was carried out at UNSW in
2004-2005, 1 year after implementing it into their standalone pathology course [15]. Based on the success of virtual
slides the year before, they abandoned traditional microscopes and used virtual slides only. Both histologists and
pathology tutors were in attendance. The results of this
integration had a similar positive outcome to the pathology
implementation the year before.
There are no articles describing implementation of virtual
microscopy into a fully integrated preclinical curriculum or a
Problem-Based Learning (PBL) curriculum; however, it is
likely that some programs are doing so. There is no logistic
reason why virtual slides cannot be integrated with PBL if
the cases are online and small group rooms have computer
access. Learning issues could then be developed that require
students to study and present histopathology via virtual
slides along with clinical and pathophysiologic correlations.
4.1.4. Repositories for sharing among institutions
The University of Iowa Department of Pathology
obtained a grant from the National Library of Medicine
(2000-2003) to develop a virtual slide database for sharing
among medical schools. The data set is composed of a
comprehensive set of slides for use in general and systemic
pathology. The slides were initially selected based a list of
core morphologic concepts of disease for second-year
medical students [43]. Using the Iowa course data set as a
F. R. Dee
foundation, we have added slides from institutions around
the world, thus creating an open source virtual slide box. A
histology data set is also included. The approximately 1000
virtual slides in the data set are in a nonproprietary file
format, which can be converted for use with a wide variety of
virtual slide server and viewer combinations. Slides in the
data set can be viewed in the Virtual Slidebox at www.path.
uiowa.edu/virtualslidebox. Directions for acquisition of the
data set can be found in the Copyright and Fair Use link on
the Virtual Slidebox home page. The entire data set and
associated metadata, which are available to course directors
for the cost of processing and mailing, has now been shared
with more than 30 institutions in the United States and
around the world.
In Australia, UNSW has developed a repository of virtual
slides, with associated worksheets illustrating approaches to
teaching with these slides (personal communication from
Rakesh Kumar). This repository has been funded by the
Australian Learning & Teaching Council. The slides include
teaching sets for not only anatomy (histology) and
pathology but also botany and zoology. The virtual slide
collections are available without charge to Australian tertiary
education institutions.
Data sets for sharing among institutions provide distinct
advantages, not the least of which is decreasing the high
cost of acquisition. In addition, slides with exceptional education value can be used by all. As has occurred with
photomicrographs, creation of virtual slide data sets by
educational organizations or consortia of medical schools
should also be feasible Although it is also technically and
logistically possible for consortia of institutions to share
a server, given the uncertainty of the Web and the fact
that serving and viewing software still has variable performance, institutions should still purchase their own serving
and viewing software, if virtual microscopy is to be a
required part of their curriculum.
4.2. Cytology
As outlined in Section 2, the standard virtual slide, with
only one focal plane, does not work as well for cytologic
preparations as it does for histologic sections. Evaluation of
two 3-D solutions indicated that they have diagnostic
accuracy and acceptable viewing efficiency [6,8]. These
solutions allowed simultaneous panning and focusing in a
continuous seamless manner, as is done in real microscopy by
cytologists. Efficiency of viewing was facilitated by bringing
all of the z-stacks in a field of view into RAM and ready to
focus as soon as new fields are panned into view. When this
was done directly off of a desktop hard drive or DVD, it still
took cytologists 4 times as long to carefully examine the same
surface area of a slide with virtual microscopy as with
traditional microscopy; however, cytologists thought this
level of viewing efficiency tolerable for cytology education
[8]. Viewing over the Web is even slower and would not be
acceptable for clinical work. Finally, there have been a
Virtual microscopy in pathology education
number of other reports describing virtual microscopy for
cytology, including description of software interfaces to teach
locate and identify skills [18-21]. The above activity, and the
fact that a number of vendors appear to be working on
efficient 3-D solutions, offers promise for the future of virtual
microscopy in cytology education.
4.3. Hematology
Hematology (as well as microbiology and urinalysis)
microscopic preparations have some of the same focus issues
as cytology; however, there has been less activity among
educators in these areas as evidenced by a paucity of reports
in the literature [7].
1119
interact over glass slides at a multiheaded microscope.
Krupinsky et al [44] have recently shown that virtual slides
can be used to facilitate study of eye movement of trainees and
experts as they look at a slide and thus objectively document
the approach experts take as they evaluate a microscopic slide.
An expansion of this type of educational research may
facilitate construction of computerized self-assessment exercises that compare trainees' eye movement and panning and
zooming actions with experts and thus provide trainees
objective feedback for improvement. In addition, software
solutions with an interface to teach cytology locator skills
described by Stewart et al [21] have application not only in
cytology but also in histopathology and hematology.
4.5. Continuing education
4.4. House staff education and evaluation
The American Board of Pathology has been augmenting
the practical component of their examination with virtual
microscopy for a number of years, and as of 2006, 15 of
75 microscopic questions used virtual slides [22]. Their
continued use in board examinations suggests that virtual
microscopy should be an efficient and reliable way to train
and evaluate pathology house staff. In addition, as discussed
elsewhere in this issue, there are studies showing a high level
of agreement between virtual slides and the original glass
slides in diagnostic telepathology and competency testing.
Thus, there is tremendous opportunity in house staff
education to create virtual slide sets, annotate them, develop
atlases and self-assessment exercises, and develop consortia
for sharing among training programs.
In compliance with the Accreditation Council for
Graduate Medical Examination (ACGME) requirement for
programs to implement objectively measurable performancebased education and assessment, we at Iowa developed an inhouse exercise designed to measure progress in development
of competency in morphologic skill in general surgical
pathology. We administered a Web-based extended multiplechoice examination with 20 virtual slides and minimal
clinical information to our 20 residents. This examination
showed very high internal reliability, as well as significant
validity as measured by strong correlation with months in
training in surgical pathology and performance on the
surgical pathology section of the Resident In-Service
Examination (RISE) examination. This study was presented
at the 2008 APC meeting, and is published in this issue of
Human Pathology (Bruch L, DeYoung B, Dee FR). It is
also of interest that in Europe, the first progress test for
trainees and pathologists called European Pathology Learning System was administered on October 1, 2008 (personal
communication from JG van den Tweel).
In addition, virtual slides may make it possible to more
objectively measure and improve the skills that house staff
need to examine a microscopic slide. Up to this point,
subjective methods have been used as a trainee and expert
Virtual microscopy appears to be well established in
histopathology continuing education. The diagnostic concordance with glass slides, cost savings provided by Web
accessibility, and the need for only 1 original glass slide to
provide virtual slide viewing to all participants underline the
impact that virtual microscopy can have on continuing education in pathology. Several articles have described the use of
virtual slides in continuing education-like activities [23-25].
In addition, a number of major pathology organizations have
recently implemented virtual microscopy into their offerings,
including the American Society for Clinical Pathology
(ASCP), the College of American Pathologists, and the
United States and Canadian Association of Pathologists. The
ASCP uses virtual slides to “supplement instruction during
meetings and self-assessment activities: meetings focusing on
in-depth topics will use virtual microscopy during the session
to illustrate morphology, and then provide participants with a
DVD with the images as a reference; online self-assessment
activities will incorporate virtual microscopy to allow further
study of the images used in the case studies” (personal
communication from Becky Harris, ASCP). Finally, on
an international level, virtual microscopy is being used by
the European Virtual Microscopy Network (www.webmicroscope.net/default.asp) and the Canadian Association of
Pathologists (www.cap-acp.org/whatsnew.html).
4.6. Veterinary and comparative pathology
Similar to human pathology, there is a role for virtual
microscopy in veterinary pathology teaching and comparative pathology [26-29]. Simms et al [29] described the
successful implementation in an undergraduate veterinary
medical curriculum. Virtual microscopy is also prominent on
several comparative pathology Web sites [26]. These include
the Comparative Pathology link on the Iowa Virtual Slidebox
home page (www.path.uiowa.edu/virtualslidebox) and a
University of California at Davis Web site, which has
many human cancers and mouse models of human cancer
(http://imagearchive.compmed.ucdavis.edu/).
1120
4.7. Histology—a prerequisite for
pathology education
Virtual microscopy is applicable to the study of histology,
as it is to histopathology [30-36]. In addition, the same
curricular pressures that apply to pathology also apply to the
teaching of histology in medical schools. Thus, it is not
surprising that a review of trends in histology teaching in US
medical schools indicated that as of 2005, approximately
25% of schools had implemented virtual microscopy into
their histology teaching with an additional 25% indicating
that they would implement virtual microscopy by the
following year [34]. Thus, virtual microscopy implementation in histology is probably at least as prevalent as in
pathology, and the 2 disciplines frequently share hardware
and software in the same institution.
Harris et al [30] described implementation of virtual
microscopy into histology in the medical school curriculum
at the University of Iowa in 2000, simultaneous with its
implementation in pathology [31]. The first step in this
implementation was to put the existing histology syllabus on
line side-by-side with virtual slides of the entire histology
glass slide set. After carrying out introductory laboratories in
a traditional laboratory to orient students to the use of the
microscope, students were then allowed to choose among 4
different venues for learning for the balance of the semester:
(1) the old microscope-only laboratory, (2) a laboratory
equipped with both computers and traditional microscopes,
(3) a computer-only laboratory, and (4) self-study on the
computer. Most students opted for the combined laboratory,
probably in part because the final practical examination
continued to be given using traditional microscopy. The
following year, extensive annotations were added to the
virtual slides. In addition, virtual slide practice exercises
were added in which the trainee was first given an unknown
slide. They were asked to identify the tissue, then an arrow
appeared pointing at a structure to identify, then an answer
followed. The annotations and exercises increased self-study
and markedly increased student satisfaction. Performance
levels on examinations have been maintained. Subsequently,
a number of other novel implementations of virtual
microscopy in histology have been described [32,33,35,36].
5. Future opportunities and challenges for
virtual microscopy in education
Commercial vendors and advancing technology have had
and will probably continue to have an impact on the
development of virtual microscopy for education in the
United States. The proprietary nature of some systems and
the lack of interchangeability of file formats among the
products continue to be of concern; however, these appear to
be less significant an impediment to innovation in education
than in the early years of virtual microscopy.
F. R. Dee
The literature devoted to virtual microscopy innovation
and implementation in education is small but rapidly
expanding. Excluding repeat discipline-specific articles
from the same institution, there were 3 articles in 2000 to
2002, 8 articles 2003 to 2004, and already 12 articles in 2006
to 2008 as of September 2008 on the reference list for this
review. In addition, there are increasing numbers of
presentations and abstracts at education and informatics
meetings; for example, at the most recent International
Association of Medical Science Educators meeting in July
2008, there were 5 virtual microscopy articles, a 6-hour
faculty development course, and a focus session devoted to
virtual microscopy for student teaching in histology and
pathology (www.iamse.org).
Although initial implementation of virtual microscopy in
pathology education was in medical student education, there
is little doubt that virtual microscopy will have an increasing
role in continuing education and house staff education. The
technology for implementation in continuing education in
histopathology is already quite good; however, it could be
improved upon by better low-power screen resolution.
Virtual focus (3-D, Z-axis viewing) will need to become
more efficient before virtual microscopy becomes fully
integrated into continuing education in cytology, hematology, microbiology, and urinalysis.
The American Board of Pathology implementation, the
diagnostic concordance with glass slides, the positive results
of the competency study at Iowa, and the potential to
develop novel ways to use the computer to teach microscopic skills suggest there is tremendous opportunity for the
use of virtual slides for training and self-assessment for
pathology house staff.
Given the estimate that perhaps only 30% of medical
schools still use glass slides sets to teach microscopic
pathology, that only about 45% still have laboratories and
large groups, and that virtual microscopy may already be
incorporated in at least 33% of curricula, the incorporation
into pathology medical school curricula may begin to level
off unless virtual microscopy is incorporated in novel ways
into small group teaching and/or independent learning
exercises. Apart from local circumstances in a medical
school, a decision to implement virtual microscopy will
depend on the level of commitment that pathology chairs and
their faculty have to the proposition that active learning
of histopathology by panning and zooming whole (virtual)
slides, and the associated ability to develop innovative
computer-assisted educational programs, have an important
role in the education of future physicians.
References
[1] Silage DA, Gil J. Digital image tiles: a method for the processing of
large sections. J Microsc 1985;138:221-7.
[2] Westerkamp D, Gahm T. Non-distorted assemblage of the digital
images of adjacent fields in histological sections. Anal Cell Pathol
1993;5:235-47.
Virtual microscopy in pathology education
[3] Weinstein RS, Descour MR, Liang C, et al. An array microscope for
ultrarapid virtual slide processing and telepathology. Design, fabrication, and validation study. HUM PATHOL 2004;35:1303-14.
[4] Jao CS, Hier DB, Brint SU. The display of photographic-quality
images on the Web: a comparison of two technologies. IEEE Trans Inf
Technol Biomed 1999;3:70-3.
[5] Taylor RN, Gagnon M, Lange J, Lee T, Draut R, Kujawski E.
CytoView: a prototype image-based Papanicolaou smear proficiency
test. Acta Cytol 1999;43:1045-51.
[6] Gagnon M, Inhorn S, Hancock J, et al. Comparison of cytology
proficiency testing: glass slides vs. virtual slides. Acta Cytol 2004;
48:788-94.
[7] Lee SH. Virtual microscopy: applications to hematology. Lab Hematol
2005;11:38-45.
[8] Dee F, Donnelly A, Radio S, Leaven T, Kreiter C, Zaleski MS. Utility
of 2-D and 3-D virtual microscopy in cervical cytology education and
testing. Acta Cytol 2007;51:523-9.
[9] Kalinski T, Zwonitzer R, Sel S, et al. Virtual 3-D microscopy using
multiplane whole slide images in diagnostic pathology. Am J Clin
Pathol 2008;130:259-64.
[10] Rojo MG. Critical comparison of 31 commercially available digital
slide systems in pathology. Int J Surg Pathol 2006;14:285-305.
[11] Dick(Dee) FR. Web-based Virtual Microscope Laboratories. Pathol
Educ 2000-2001;25:58-62 [http://peir.path.uab.edu/griper/journals/
v25n2.pdf].
[12] Kumar RK, Velan GM, Korell SO, Kandara M, Dee FR, Wakefield D.
Virtual microscopy for learning and assessment in Pathology. J Pathol
2004;204:613-8.
[13] Dee FR, Heidger P. Virtual slides for teaching histology and pathology.
In: Gu J, Ogilvie RW, editors. Virtual Microscopy and Virtual Slides
in Teaching, Diagnosis and Research, Taylor & Francis Group. Boca
Raton: CRC Press; 2005. p. 141-9 [Chapter 9].
[14] Glatz-Krieger K, Spornitz U, Spatz A, Mihatsch MJ, Dieter Glatz D.
Factors to keep in mind when introducing virtual microscopy.
Virchows Arch 2006;448:248-55.
[15] Kumar RK, Freeman B, Velan GM, De Permentier PJ. Integrating
histology and histopathology teaching in practical classes using virtual
slides. Anat Rec B New Anat 2006;289:128-33.
[16] Kim MH, Park Y, Seo D, et al. Virtual microscopy as a practical
alternative to conventional microscopy in pathology education. Basic
Appl Pathol 2008;1:46-8.
[17] Dee FR, Lehman JM, Consoer D, Leaven T, Cohen M. Implementation
of virtual microscope slides in the annual Pathobiology of Cancer
Workshop Laboratory. HUM PATHOL 2003;34:430-6.
[18] Steinberg DM, Syed ZA. Application of virtual microscopy in clinical
cytopathology. Diagn Cytopathol 2001;25:389-96.
[19] Grant KL. Virtual microscopy as a tool for proficiency testing in
cytopathology. Arch Pathol Lab Med 2003;127:1320-4.
[20] Marchevsky AM, Khurana R, Thomas P, Scharre K, Farias P, Bose S.
The use of virtual microscopy for proficiency testing in gynecologic
cytopathology: a feasibility study using ScanScope. Arch Pathol Lab
Med 2006;130:349-55.
[21] Stewart J, Bevans-Williams K, Bhattacharya A, Ye C, Miyazaki K,
Kurtycz D. Virtual microscopy: an educator's tool for the enhancement
of cytotechnology student's locator skills. Diagn Cytopathol 2008;36:
363-8.
[22] Bennett B. Certification from the American Board of Pathology:
getting it and keeping it. HUM PATHOL 2006;37:978-81.
[23] Romer D. Use of virtual microscopy for didactic live-audience
presentation in anatomic pathology. Ann Diagn Pathol 2003;7:67-72.
1121
[24] Lundin M, Lundin J, Helin H, Isola J. A digital atlas of breast
histopathology: an application of Web based virtual microscopy. J Clin
Pathol 2004;57:1288-91.
[25] Helina H, Lundin M, Lundin J, et al. Web-based virtual microscopy
in teaching and standardizing Gleason grading. HUM PATHOL 2005;
36:381-6.
[26] Dee FR. Virtual microscopy for comparative pathology. Toxicol Pathol
2006;34:966-7.
[27] Ward JM. So many Web sites, so little time! Toxicol Pathol 2006;34:
314-5.
[28] Dee F, Meyerholz D. Teaching pathology in the 21st century—virtual
microscopy applications. J Vet Med Educ 2007;34:431-6.
[29] Simms MH, Mendis-Handagama C, Moore RN. Virtual microscopy
in a veterinary curriculum. J Vet Med Educ 2007;34:416-22.
[30] Harris T, Leaven T, Heidger P, Kreiter C, Duncan J, Dick(Dee) FR.
Comparison of a virtual microscope versus a regular microscope
laboratory for teaching histology. Anat Rec (New Anat) 2001;265:
10-4.
[31] Heidger P, Dee FR, Consoer D, Leaven T, Kreiter C. An integrated
approach to teaching and testing in histology with real and virtual
imaging. Anat Rec (New Anat) 2002;269:107-12.
[32] Blake CA, Lavoie HA, Millette CF. Teaching medical histology at
the University of South Carolina School of Medicine: transition
to virtual slides and virtual microscopes. Anat Rec (New Anat) 2003;
275:196-206.
[33] Krippendorf BB, Lough J. Complete and rapid switch from light
microscopy to virtual microscopy for teaching medical histology. Anat
Rec (New Anat) 2005;285:19-25.
[34] Bloodgood RA, Ogilvie RW. Trends in histology laboratory teaching
in United States medical schools. Anat Rec (New Anat) 2006;289B:
169-75.
[35] Goldberg HR, Dintzis R. The positive impact of team based virtual
microscopy on student learning in physiology and histology. Adv
Physiol Educ 2007;31:261-5.
[36] Scoville SA, Buskirk TD. Traditional and virtual microscopy
compared experimentally in a classroom setting. Clin Anat 2007;20:
565-70.
[37] Taylor CR, DeYoung BR, Cohen MB. Pathology education: quo
vadis? HUM PATHOL 2008;39:1555-61.
[38] Kumar K, Daniel J, Doig K, Agamanolis D. Teaching pathology in
United States medical schools, 1996/1997 survey. HUM PATHOL
1998;29:750-5.
[39] Kumar K, Indurkhya A, Nguyen H. Curricular trends in instruction of
pathology: a nationwide longitudinal study from 1993 to present. HUM
PATHOL 2001;32:1147-53.
[40] Marshall R, Cartwright N, Mattick K. Teaching and learning in
pathology: a critical review of the English literature. Med Educ
2004;38:302-13.
[41] Burton J. Teaching pathology to medical undergraduates. Curr Diagn
Pathol 2005;11:308-16.
[42] Roullet M, Feldman M, Shea J, Phillips (Cambor) CC. The use of
virtual slides in North American Medical Schools. Presented at the
Slice of Life Meeting in Portland; 2005.
[43] Dick(Dee) F, Leaven T, Dillman D, Torner R, Finken L. Core
morphologic concepts of disease for second-year medical students.
HUM PATHOL 1998;29:1017-20.
[44] Krupinsky EA, Tillack AA, Richter L, et al. Eye-movement study and
human performance using telepathology virtual slides. Implications for
medical education and differences with experience. HUM PATHOL
2006;37:1543-56.