The influence of stiffness of the fixator on maturation of callus after
advertisement

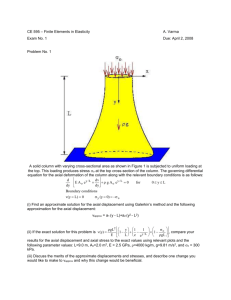
The influence of stiffness of the fixator on maturation of callus after segmental transport L. Claes, J. Laule, K. Wenger, G. Suger, U. Liener, L. Kinzl From the University of Ulm, Germany he treatment of large bony defects by callus distraction is well accepted, but the duration of treatment is long and the rate of complications increases accordingly. We have examined the effect of the stiffness of the axial fixator on reducing the time for maturation of callus. We created a mid-diaphyseal defect of 15 mm in the metatarsal bone in sheep and stabilised it with a ring fixator. After four days a bony segment was transported for 16 days at 1 mm per day. After 64 days the animals were divided into four groups, three with axial interfragmentary movement (IFM) of 0.5, 1.2 and 3.0 mm, respectively, and a control group. The 3.0 mm IFM group had the smallest bone density (p = 0.001) and area of callus and the largest IFM after 12 weeks; it also had typical clinical signs of hypertrophic nonunion. The most rapid stiffening of the callus was in the 0.5 mm group which had the smallest IFM (p = 0.04) after 12 weeks and radiological signs of bridging of the defect. These results indicate that suitable dynamic axial stimulation can enhance maturation of distraction callus when the initial amplitude is small, but that a large IFM can lead to delayed union. T J Bone Joint Surg [Br] 2000;82-B:142-8. Received 21 July 1998; Accepted after revision 5 March 1999 Callus distraction is widely used for the treatment of 1,2 defects of tubular long bones. At the end of the distraction the young callus has low mechanical stiffness and L. Claes, PhD, Professor and Director J. Laule, DVSc, PhD, Research Fellow K. Wenger, PhD, Research Fellow Department of Orthopaedic Research and Biomechanics G. Suger, MD, Orthopaedic Surgeon U. Liener, FRCS, Orthopaedic Surgeon L. Kinzl, MD, Professor Department of Surgery University of Ulm, Helmholtzstrasse 14, D-89081 Ulm, Germany. Correspondence should be sent to Professor L. Claes. ©2000 British Editorial Society of Bone and Joint Surgery 0301-620X/00/19332 $2.00 142 strength; adequate time must then be allowed for maturation before the fixator can be removed. At least two-thirds of this time is dedicated to passive maturation and most complications such as loosening or infection of the pins 3,4 occur during this phase if external fixation is used. Loosening of the pins results in reduced mechanical stability and increased movement in young regenerate bone. In experimental studies on callus distraction, both deleterious and advantageous effects have been demonstrated on movement, depending on the amount. A small degree 5 will induce regeneration and maturation of callus, but if it exceeds a certain limit in the regenerate bone, maturation decreases and osseous bridging of the defect is inhibited, 6 resulting in hypertrophic nonunion. The specific range of movement which effectively stimulates young distraction callus is unknown. The movement which occurs normally in this tissue during the maturation phase can be estimated from in vitro measurements of fixators used in distraction osteogenesis. In a tibial Ilizarov fixator consisting of four rings, axial movement is in the range of 3 to 6 mm when axially loaded to 300 N, depending on the amount of 7,8 pretension in the wires. When pretension is reduced or the wires loosened the 9 axial movements are correspondingly higher. It is not possible to ensure that patients do not exceed the proposed load limits. More information, generated from the more finely-incremented interfragmentary movements (IFM), is still needed to estimate the degree of axial movement may be optimal or critical for the maturation of callus. Studies have shown that in sheep, when pulsed distraction of an amplitude of 0.08 mm was applied for 250 cycles, the ultimate torsional strength of the regenerate 10 improved, but this was not significant. Similar results were obtained when axial dynamisation was applied two 11 weeks after the end of distraction, indicating a diminished sensitivity of distraction callus for axial movement during advanced maturation. To investigate the effect of axial IFM in young regenerate bone and to determine how much may be optimal, we developed an animal model which approximated to the healing conditions in the human tibia. It had the following criteria: 1) stable, rigid fixation allowing distraction of callus over at least 15 mm; 2) purely axial-guided movement in the regenerate bone; and 3) adjustable and wellTHE JOURNAL OF BONE AND JOINT SURGERY THE INFLUENCE OF STIFFNESS OF THE FIXATOR ON MATURATION OF CALLUS AFTER SEGMENTAL TRANSPORT 143 Fig. 1 Diagram of the operative procedure: left, creation of the mid-diaphyseal defect; middle, adjustment of the length of the defect to 15 mm; and right, daily segmental bone transport of 1 mm in two steps. controlled amplitude, with monitoring of the movement and stiffness during maturation of the callus. We used this model to study our hypothesis that dynamisation of the fixation device with sufficient axial IFM enhances the maturation of newly-formed callus, whereas large axial movements inhibit it. Material and Methods We used 32 skeletally-mature female sheep, aged three years or older, with a mean weight of 80 ± 10 kg. Approval for the experiment was granted by a German governmental scientific review board (Regierungsprasidium, Tübingen, No. 485). Using general halothane anaesthesia, we performed a standardised operation. To prevent plantar flexion 11 of the foot, which can occur during lengthening, we used a segmental bone-transport model. The fixator was first applied to the intact metatarsal. We drilled holes for four Steinmann pins, 4.5 mm in diameter, using a 4 mm drill bit. The drill and stabilising pins were inserted over a guide 75° apart. Schanz screws 5 mm in diameter were inserted distally in a medioplantar and proximally in a mediodorsal direction after predrilling with a 3.5 mm bit (Fig. 1). Two Steinmann pins, 3 mm in diameter, were inserted 8 mm apart in the transportable bony segment in a mediolateral direction after predrilling with a 2 mm bit through a drill guide. With the fixator applied to the metatarsal, a defect 10 mm in length was created in the distal diaphysis by two osteotomies using an oscillating saw and a guide (Fig. 1). A bony segment 25 mm in length was resected from the proximal diaphysis by a third osteotomy, using a Gigli saw trained along a guide. Before the osteotomies VOL. 82-B, NO. 1, JANUARY 2000 were performed, the periosteum was resected for 2 mm around the planned site of the osteotomy. All drilling and sawing were performed under cooling irrigation with 0.9% NaCl solution. When all the osteotomies were completed, sawdust and bone chips were carefully removed to prevent undesired osseoinduction. The bony segment was then transported proximally to close the saw gap, and the defect was adjusted to 15 mm using a distance gauge. After four days distraction of the callus was begun at 1 mm per day in two increments, morning and evening, and continued over 16 days, resulting in compression of 1 mm at the docking site. In a pilot study in vitro with a washershaped loading cell at the docking site (Typ 9031; Kistler, Winterthur, Switzerland) a compressive force of 170N was produced. Before docking the axial telescoping system was locked and the two rings further stabilised by two connecting rods in the sagittal plane. In one group the IFM was restrained by an axially stiff fixator (control group) and in the three dynamised groups the fixators were equipped with a telescopic system allowing axial IFMs of 0.5, 1.2 or 3.0 mm after completion of the distraction 21 days after operation. The decrease in axial IFM was measured in vivo by displacement transducers mounted to the external fixator. During load-bearing the young regenerate bone was compressed initially by the designed displacement amplitude, then during unloading the original defect of 15 mm was recovered by the recoil of the springs. After 12 weeks the sheep were killed and the metatarsals removed and investigated morphologically. External fixator. The fixator consisted of two circular aluminium frames, one of which was fixed distally on the metatarsal by two Steinmann pins and one Schanz screw 144 L. CLAES, J. LAULE, K. WENGER, G. SUGER, U. LIENER, L. KINZL (Stratec, Waldenburg, Switzerland) and the other proximally. The free clamp length of the transfixing pins was 80 mm. The two frames, nominally 60 mm apart, were fitted to each other by two pairs of mating titanium cylinders (Fig. 1), each pair consisting of an inner and an outer tube. The inner tube contained a steel spring. The two symmetrial springs were preloaded to 60 N each so that loading forces higher than 120 N would initiate an IFM. Any loads lower than 120 N would not move the ends of the osteotomy together. The axial movement allowed during loading could be adjusted between 0 and 4 mm. At unloading the original gap size was recovered by the release of the springs. Additionally, the cylinders were equipped to transfix a bony segment with two Steinmann pins and to transport it over 15 mm by advancing a nut (Fig. 1). Immediately after the operation and during the period of distraction, two additional rods connected the rings in both the stabilised and stimulated groups to increase further the stiffness of the fixator. The full weight of the experimental ring fixator was about 2.1 kg. The isolated biomechanical characteristics of the external fixator system were determined by testing it mounted to a Pertinax plastic tube similar in dimensions to the metatarsal bone. The length of the defect was adjusted to 15 mm and the complete system tested in free bending, compression and torsion in the configurations corresponding to before and at docking of the bony segment. Bending and compression tests were performed on a materials testing machine (Zwick 1454, Einsingen, Germany). For compression testing, ball mounts were used at both the distal and proximal ends of the tube to ensure that there was a purely axial force. The fixator-Pertinax system was loaded to a maximum of 300 N and movement in the area of the defect was 12 measured by an electronic goniometer system. All displacements in the defect, the deflection angles in the frontal and sagittal planes and the torsional angles around the long axis of the bone were determined. The bending stiffness was measured in a combined free bending and axial compression test with a length of lever arm of 50 mm and an applied force of 300 N resulting in a bending movement of 15 Nm. It was calculated as the ratio of the bending moment to the degree of flexion. Torsional stiffness was measured in a customised torsional testing machine with the Pertinax tube mounted proximally and distally. A torsional moment of 5 Nm was applied and the rotation angle recorded. The torsional stiffness was defined as the ratio of the applied torsional moment to the measured rotation angle of the ends of the osteotomy in the defect. In vivo measurement of the interfragmentary movement. The decrease in the IFM over the healing period as a result of the progressive bridging and calcification of the distraction callus was monitored once a week using an inductive LVDT (Type SS 102; Collins, Long Beach, California) placed between the distal and proximal frames of the fixators; the electrical signals of the device were trans- mitted telemetrically (Biotel 33; Glonner, Planegg, Germany) to a personal computer. As the sheep walked, displacement curves were generated. The IFM was defined as the maximum displacement recorded after at least five steps. Movements smaller than 0.05 mm were not considered to be valid since the accuracy of the LVDT device and telemetry is in the range of 0.03 mm. Since this had been previously noted for a stable fixed metatarsal, weekly IFM was not monitored in this group (control). Just before dynamisation of the fixator on day 21 after operation, the inherent displacement of the system was evaluated by monitoring the deflection of the complete, locked fixation device as the animal walked. The fixator was then unlocked and the initial axial movement in the distraction callus determined from the difference in movement between the locked and unlocked states. Weekly measurements were then made until the animals were killed on days 81 to 84, using always the inherent displacement at day 21 as null. The adjusted values were then normalised to the maximum measured for the given animal during the study. CT studies. After all the sheep had been killed at about 84 days after operation the metatarsals were excised, and the fixator removed. The healing area was scanned by computed tomography (pQ-CT 960; Stratec, Pforzheim, Germany) with a voxel size of 0.590 0.590 mm and slice thickness of 1.0 mm. Fourteen slices were taken along the axis of the regenerate bone area with a slice distance of 1.5 mm, including two in the proximal and distal cortices and ten in the area of regenerate bone. Tissue with a threshold above 3 0.45 l/cm or density greater than 218 mg/cm was considered as bone. Bone density and bone area were calculated with software provided by the manufacturer. The precision of the bone density measurements is better than 3%. Statistical analysis The variable of interest is the proportion of sheep with an IFM below 0.3 mm (bony healing) on the twelfth week. The groups were compared using Fisher’s exact test. First, an overall test for all three groups was performed and the variables of density and area were analysed by analysis of variance. Post-hoc tests within an analysis of variance were adjusted for multiple comparisons appropriately with Tukey’s HSD test. Results In the first three weeks after operation, load-bearing on the limb was tentative as assessed by daily observation, but then appeared to become normal after docking. Stiffness of the external fixator. From the in vitro testing of the rigidity of the fixator, the maximal axial deformation of the tube and fixator in the stable, locked position was 0.3 mm under an axial load of 300 N. The displacement of the ends of the osteotomy at the defect in the sagittal and frontal plane was always less than 0.18 mm if loaded axially as measured by the goniometer system. THE JOURNAL OF BONE AND JOINT SURGERY THE INFLUENCE OF STIFFNESS OF THE FIXATOR ON MATURATION OF CALLUS AFTER SEGMENTAL TRANSPORT Axial stiffness was 989 N/mm. Under dynamised fixation the load-displacement curve showed three distinct slopes. From 0 to 120 N the axial stiffness of the fixator system was 915 N/mm. From 120 N to approximately 130 N it equalled that of the springs, 7.69 N/mm, which allowed full axial movement within a small load range. At 130 N the bolts prohibited further axial displacement of the rings and the stiffness returned to 989 N/mm. The axial stiffness of the fixator used in the control group with two additional connecting rods in the sagittal plane and 1 mm of compression at the docking site was 1065 N/mm. In free bending, the angular stiffness of the locked fixator at docking was 112 Nm/° in the sagittal plane and 50 Nm/° in the frontal plane. Torsional stiffness measured at the osteotomy gap in a fixator with locked, stable fixation was 12.3 Nm/°. Interfragmentary movement. The mean postoperative IFM under stable fixation was 0.17 mm (0.06 to 0.29), reflecting the inherent displacement due to elastic deformation of the external fixator and pin-bone contact (Table I). Thus, measurements below 0.3 mm may occur after bony bridging. The IFM decreased in all dynamised groups during the healing period (Table I). The slowest reduction of the IFM, normalised to individual initial values corrected for the inherent displacement of the fixator frame, was found in the 3.0 mm group (Fig. 2). The value in the 0.5 and 1.2 mm groups was 9% and 24%, respectively, of the initial IFM value after 12 weeks, but in the 3.0 mm group it 145 was 42%. Only the 0.5 mm group reached an IFM as low as the inherent displacement of the fixator (0.2 mm) at week 12 of monitoring. Radiologically, these specimens were bridged and were stable. This bridging appears to have started in the tenth week and was mainly in the 0.5 mm group. Only one sheep in the 0.5 mm group had an IFM of 0.3 mm or larger after ten weeks compared with five in the 1.2 mm group and seven in the 3 mm group. At the end of the study at 12 weeks, all of the 0.5 mm group had an IFM smaller than 0.3 mm whereas in four of the 1.2 mm group and seven of the 3 mm group it was larger than 0.3 mm. The number of sheep with an IFM below 0.3 mm was significantly larger in the 0.5 mm group than in the 1.2 mm (p = 0.04) and 3 mm groups (Fisher’s exact test, p = 0.001). This indicates that maturation of callus was most rapid in the group with 0.5 mm of initial axial movement. In the 3 mm group the mean movement after ten weeks was 1.5 mm and after 12 weeks it was 1.4 mm which indicates no significant improvement in stiffening and signs of nonunion. CT findings. In the 0.5 mm group the distribution of callus was nearly circular whereas in the 3 mm group it was irregular (Figs 3 to 5). All animals showed the highest density of callus next to the proximal and distal cortices. Toward the middle zone the density decreased in every group to its lowest value (Fig. 6a) which was significantly lowest in the 3 mm group (p = 0.001, Fig. 6a, Table II) and highest in the 0.5 mm group. The mean density of the 3 corresponding intact metatarsal bone was 1199 mg/cm . There were no statistical significant differences in the area of callus among the groups in the centre of the defect (p = 0.86). The area of callus in the 3.0 mm group was lowest in the middle of the defect and increased towards the cortices to values significantly larger than the cross2 sectional area of the adjacent diaphysis (160 mm ; Fig. 6b, Table III). Such a distribution of callus indicates hypertrophic pseudarthrosis as has been described by 13,14 others. Discussion Fig. 2 Correlation of interfragmentary movement (IFM) in the distraction callus with healing time. For comparison of the groups, the IFM is normalised to the maximum values at the start of the measurements corrected for the inherent displacement of the fixator frame. The worst maturation of distraction callus occurred when 3 mm of IFM were allowed when there was a significantly smaller density and area of callus than for the other groups at 12 weeks after operation. There were no significant differences in the density and area of the callus in the groups with 0, 0.5 and 1.2 mm of axial movement. The larger IFM stimulated more callus near the zones of the Table I. The inherent displacement of the fixator and the mean (SD) IFM (mm) over the healing time for the dynamised groups Inherent Group (mm) displacement Day 21 0.5 1.2 3 Weeks after operation 4 5 6 7 8 9 10 11 12 0.155 (0.069) 0.559 (0.204) 0.507 (0.242) 0.452 (0.204) 0.437 (0.204) 0.357 (0.109) 0.262 (0.079) 0.271 (0.116) 0.206 (0.104) 0.245 (0.128) 0.202 (0.074) 0.190 (0.100) 1.379 (0.198) 1.104 (0.352) 0.891 (0.365) 0.772 (0.365) 0.646 (0.335) 0.644 (0.454) 0.567 (0.372) 0.577 (0.428) 0.501 (0.373) 0.476 (0.379) 0.156 (0.053) 2.829 (0.471) 2.565 (0.593) 2.193 (0.741) 2.118 (0.741) 2.061 (0.758) 1.880 (0.915) 1.771 (0.857) 1.525 (0.946) 1.559 (0.939) 1.433 (0.996) VOL. 82-B, NO. 1, JANUARY 2000 146 L. CLAES, J. LAULE, K. WENGER, G. SUGER, U. LIENER, L. KINZL Fig. 3 CT scans from the middle of the defect (left) and the corresponding scout view (top, 0.5 mm group; bottom, 3.0 mm group). cortical defect but not in the middle of the area of callus distraction. The fastest stiffening was seen in the 0.5 mm group after ten weeks which had still not been achieved in the other groups at 12 weeks. In this model, the more IFM allowed initially, the higher it was at the end of the study and the lower the resulting callus density (D) in the middle of the defect (D = 630-50*IFM; r = 0.59). The early bony bridging of the fibrous interzone in the 0.5 mm group indicated early maturation of the newly formed callus in the middle of the defect. In the 3 mm group the IFM was too large to allow bridging and stabilisation of the defect. One reason was a movement-induced inhibition of cell and 15 vessel proliferation into the defect. The new external fixator for segmental bone transport provides standardised and controlled distraction and maturation of callus, with accurate settings of the telescopic 7,8,16-18 the axial movement. In contrast to other systems new ring fixator has a very high bending, torsional and axial stiffness in all planes, minimising uncontrolled IFM. The initial, designed axial telescopic movement can be monitored telemetrically and thus used to determine the rate of maturation over any selected period of study. The lengthening index, the ratio of the total fixation time to the length of new bone obtained, was 56 days/cm in our study which corresponded to segmental bone transport in the 19 tibia of adult men. The lengthening indices of an absolute lengthening in the femur or tibia of young sheep are between 11,20-22 25 and 43 days/cm. This is generally lower than values for patients which are between 33 and 63 days/ 19,23,24 The muscle and other soft-tissue cover of the cm. sheep metatarsal is notably less than that of the sheep tibia and femur which decreases its influence on bone healing. There are two notable limitations to our study. First, the measurement of the IFM was complicated by loosening of pins in the late maturation period which must affect the accuracy of the IFM data. Measurements of loosening of pins on removed bones at the end of the study showed an effect of up to 0.1 mm of axial movement for the 0, 0.5 mm and 1.2 mm groups and up to 0.3 mm for the 3 mm group. These movements, however, did not significantly influence the mean values of interfragmentary movements measured at this time. Secondly, there was notable variability in the amount of weight-bearing tolerated by each sheep at the observation period which must affect the constancy of the test conditions. These two factors together probably explain the relatively high scatter in the IFM data. Figure 4 – High resolution radiograph of an animal in the 3 mm group taken after killing. Figure 5 – High resolution radiograph of an animal in the 0.5 mm group taken after killing. Fig. 4 Fig. 5 THE JOURNAL OF BONE AND JOINT SURGERY THE INFLUENCE OF STIFFNESS OF THE FIXATOR ON MATURATION OF CALLUS AFTER SEGMENTAL TRANSPORT Fig. 6a 147 Fig. 6b Density of callus (a) and area of distraction callus (b) at various locations according to axial movement. 3 Table II. Mean (SD) callus density (mg/cm ) for various locations. Two slices were taken in the proximal and distal cortices Group (mm) 0 0.5 1.2 3.0 Slice Proximal cortex 1 2 3 4 Middle of defect 7 8 9 10 Distal cortex 1111.6 (99.2) 1168.6 (77.9) 1068.3 (75.9) 984.4 (69.3) 839.0 (77.4) 864.9 (94.3) 848.2 (86.1) 785.9 (64.5) 768.6 (58.3) 779.4 (54.0) 743.5 (35.4) 700.5 (44.1) 744.8 (43.2) 760.3 (54.9) 717.7 (36.6) 659.3 (35.8) 726.2 (41.0) 729.7 (41.8) 694.4 (33.4) 638.3 (38.0) 699.4 (38.1) 704.1 (32.2) 675.3 (36.8) 620.1 (39.8) 722.9 (32.9) 758.3 (56.7) 708.9 (26.7) 636.1 (35.0) 755.3 (28.1) 771.0 (58.2) 721.8 (24.3) 663.5 (19.2) 774.1 (39.2) 792.8 (70.0) 746.8 (50.2) 687.0 (32.2) 817.6 (98.1) 893.3 (151.7) 841.2 (119.9) 767.7 (107.8) 950.2 (132.6) 1075.1 (164.8) 980.9 (106.0) 844.1 (158.4) 1033.9 (117.3) 1082.6 (99.3) 988.2 (104.4) 899.8 (63.2) 692.1 (37.5) 726.6 (53.5) 685.8 (37.7) 619.1 (41.2) 1146.0 (67.5) 1188.1 (83.5) 1074.3 (70.3) 913.8 (146.3) 2 Table III. Mean (SD) callus area (mm ) for various locations. Two slices were taken in the proximal and distal cortices Group (mm) 0 0.5 1.2 3.0 Slice Proximal cortex 1 2 3 4 Middle of defect 7 8 9 10 Distal cortex 231.5 (56.2) 226.8 (48.3) 256.8 (55.6) 338.1 (94.8) 250.5 (75.9) 249.3 (68.5) 303.1 (87.2) 389.1 (148.5) 243.7 (106.3) 250.3 (76.6) 290.4 (116.0) 352.3 (161.6) 249.8 (117.5) 260.4 (82.2) 281.0 (141.2) 295.3 (165.5) 253.5 (130.0) 255.8 (99.0) 265.1 (142.9) 238.4 (94.8) 235.6 (123.0) 224.4 (120.7) 244.6 (139.2) 192.3 (184.7) 239.4 (115.0) 264.1 (88.5) 288.6 (139.1) 237.4 (142.4) 233.39 (0.8) 248.5 (71.4) 294.6 (131.9) 280.7 (160.0) 210.3 (69.5) 220.3 (56.0) 289.1 (11.50) 312.4 (155.3) 196.3 (55.4) 219.7 (50.9) 274.6 (84.5) 342.1 (140.4) 200.0 (40.3) 214.4 (43.5) 278.4 (70.9) 360.4 (129.5) 244.5 (57.1) 248.0 (59.4) 283.2 (70.5) 385.5 (112.8) Our findings have shown that dynamisation of a distraction callus during maturation with 0.5 mm of initial axial amplitude in the sheep metatarsal bone stimulates maturation as compared with either no or large IFMs. By contrast, large IFMs of 3 mm led to large formation of callus at the cortical defect zone but delayed maturation, showing typical signs of 6 hypertrophic nonunion. Such large deformations of approximately 20% of the length of the defect can often be seen under clinical conditions. Taking the axial stiffness of stand8 ard ring fixators and a partial loading bearing of 300 to 500 N into consideration, defects up to 60 mm will often VOL. 82-B, NO. 1, JANUARY 2000 225.9 (129.0) 249.5 (100.0) 255.7 (139.7) 193.3 (166.3) 199.3 (30.5) 198.8 (32.0) 247.1 (61.0) 366.5 (121.0) produce corresponding axial movements. Additional loosen9 ing of wires can lead to a decreased axial stability. Fixators with low axial stiffness and loosening of wires may result in delayed nonunion. Callus distraction may therefore benefit from the use of stiffer fixators and half 9 pins in addition to or instead of wires. Although none of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but are directed solely to a research fund, foundation, eduational institution, or other non-profit institution with which one or more of the authors is associated. 148 L. CLAES, J. LAULE, K. WENGER, G. SUGER, U. LIENER, L. KINZL References 1. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part I: the influence of stability of fixation and soft-tissue preservation. Clin Orthop 1989:249-81. 2. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II: the influence of the rate and frequency of distraction. Clin Orthop 1989:263-85. 3. Bonnard C, Favard L, Sollogoub I, Glorion B. Limb lengthening in children using the Ilizarov method. Clin Orthop 1993;293:83-8. 4. Levine SE, Davidson RS, Dormans JP, Drummond DS. Distraction osteogenesis for congenitally short lesser metatarsals. Foot Ankle Int 1995;16:196-200. 5. Pflüger G, Rahn BA, Fischerleitner F, Thoma H, Wolner C. Osseous bridging of the distraction gap in leg lengthening procedures. Arch Orthop Unfallchir 1976;86:45-60. 6. Aronson J. Experimental and clinical experience with distraction osteogenesis. Cleft Palate-Craniofac J 1994;31:473-81. 7. Podolsky A, Chao EYS. Mechanical performance of Ilizarov circular external fixators in comparison with other external fixators. Clin Orthop 1993;293:61-70. 8. Schneider E, Sasse S, Schmidt HG, Schümann U. Biomechanics of the ring fixator: contributions of individual structural elements. Unfallchirurg 1992;95:580-7. 9. Suger G, Dürselen L, Claes L, Kinzl L. Biomechanical evaluation of gap motion in the Ilizarov external fixator with combined use of half pins and original Ilizarov wires. Trans International Society of Fracture Repair, Brussels 1992:81-2. 10. Figueiredo UM, Watkins PE, Goodship AE. The effects of micromotion in distraction osteogenesis. 39th Trans Orthop Res Soc, San Francisco, California, 1993:130. 11. Steen H, Fjeld TO, Bjerkreim I, et al. Limb lengthening by diaphyseal corticotomy, callus distraction and dynamic axial fixation: an experimental study in the ovine femur. J Orthop Res 1988;6:730-5. 12. Wilke H-J, Ostertag G, Claes L. A three dimensional goniometer linkage system for the analysis of movement with six degrees of freedom. Biomed Tech Berl 1994;39:149-55. 13. Stürmer KM. Histomorphologie der gestüorten Knochenbruchheilung. OP-Journal 1988;4:4-11. 14. Catagni MA. Classification and treatment of nonunion. In: Bianchi Maiocchi A, Aronson J, eds. Operative principles of Ilizarov. Baltimore, etc: Williams and Wilkins, 1991:191-8. 15. Ippolito E, Peretti G, Bellocci M, et al. Histology and ultrastructure of arteries, veins and peripheral nerves during limb lengthening. Clin Orthop 1994;308:54-62. 16. Aronson J, Harrison BH, Stewart CL, Harp JHJ. The histology of distraction osteogenesis using different external fixators. Clin Orthop 1989:106-16. 17. Caja VL, Larsson S, Kim W, Chao EYS. Mechanical performance of the Monticelli-Spinelli external fixation system. Clin Orthop 1994;309:257-66. 18. Paley D, Fleming B, Catagni M, Kristiansen T, Pope M. Mechanical evaluation of external fixators used in limb lengthening. Clin Orthop 1990:50-7. 19. Green SA, Jackson JM, Wall DM, Marinow H, Ishkanian J. Management of segmental defects by the Ilizarov intercalary bone transport method. Clin Orthop 1992:136-42. 20. Windhager R, Grossschmidt K, Sigl H, Tsuboyama T, Plenk H. Knochentransport mit einem neuen internen Distraktionssystem. Osteologie 1995:136-42. 21. Steen H, Fjeld TO. Lengthening osteotomy in the metaphysis and diaphysis: an experimental study in the ovine tibia. Clin Orthop 1989:297-305. 22. Gil-Albarova J, de Pablos J, Franzeb M, Canadell J. Delayed distraction in bone lengthening: improved healing in lambs. Acta Orthop Scand 1992;63:604-6. 23. Hamanishi C, Yasuwaki Y, Kikuchi H, Tanaka S, Tamura K. Classification of the callus in limb lengthening: radiographic study of 25 limbs. Acta Orthop Scand 1992;63:430-3. 24. Mitchell GP. L'elongation du tibia. Rev Chir Orthop Reparatrice Appar Mot 1963;49:205-11. THE JOURNAL OF BONE AND JOINT SURGERY